Beruflich Dokumente
Kultur Dokumente
Campylobacter IMRA
Hochgeladen von
Adriana Rivera PosadaCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Campylobacter IMRA
Hochgeladen von
Adriana Rivera PosadaCopyright:
Verfügbare Formate
CAMPYLOBACTER
THE ORGANISM/TOXIN
This organism causes the most commonly reported
gastrointestinal disease in New Zealand. The two
species Campylobacter jejuni and C. coli are most
often associated with disease. Grows best in reduced
oxygen atmospheres and only at temperatures
exceeding room temperature.
GROWTH AND ITS CONTROL
Growth:
Temperature: Optimum 42C, range 30.5 to 45C. Is
comparatively slow growing (fastest generation time
approximately 1 hour) even under optimum
conditions.
pH: Optimum 6.5 to 7.5, range 4.9 to 9.
Atmosphere: Normally requires reduced levels of
oxygen optimum growth at 3-5% oxygen and 210% carbon dioxide. Can be adapted to aerobic
growth, although the significance of this in
transmission of the disease is unclear.
Water activity: Optimum growth is at aw = 0.997
(0.5% NaCl), minimum aw 0.987 (2.0% NaCl)
Survival:
Temperature: Survival in food is better under
refrigeration than at room temperature, up to 15
times as long at 2oC than at 20oC. Can survive up to
an hour on hands and moist surfaces. Numbers
decline slowly at normal freezing temperatures after
an initial reduction. Freezing therefore does not
instantly inactivate the organism in food.
Atmosphere: Survives well in modified atmosphere
and vacuum packaging. Usually survives poorly at
atmospheric oxygen concentrations.
Viable but Non-Culturable (VNC) Cells: Under
adverse conditions Campylobacter is said to undergo
a transition to a VNC state. The ability for
Campylobacter to produce VNC cells is becoming
widely accepted.
Inactivation (CCPs and Hurdles):
Temperature: Rapidly inactivated by heating at 55oC
and above.
D50 = 1-6.3 min. D55 = 0.6-2.3 min. D time at 60oC =
0.2-0.3 min.
pH: Growth inhibited in foods at less than pH 4.9
and above pH 9. Rapid death in foods at pH <4.0
especially at above refrigeration temperatures.
Water activity: Thought to be sensitive to drying but
under certain refrigeration conditions can remain
viable for several weeks.
Preservatives: Sensitive to NaCl concentrations
above 1%, and death occurs slowly at 2% (D time is
5-10 hours). Ascorbic acid and several spices inhibit
growth.
Sanitisers/Disinfectants: (These products must be
used as advised by the manufacturer).
Sensitive to sanitisers, e.g. chlorine, used in the food
industry. Equally or more sensitive than E. coli to
water disinfection processes (monochloroamine, free
chlorine).
(N.B. The absence of a sanitiser/disinfectant from
this section does not necessarily imply that it is
ineffective).
Radiation: Sensitive to irradiation. An estimated 6
D reduction would result from exposure to 2 kGy, 10
D would result from 2.5 kGy. A 2-3 kGy dose is
sufficient to decontaminate meat. D values reported
are 0.18 kGy in refrigerated product, 0.24 kGy in
frozen product.
More sensitive to ultraviolet radiation than E. coli
and commercial UV water treatment units producing
30 mWs/cm2 are considered adequate.
THE ILLNESS
Incubation: 1 to 10 days (usually between 2 and 5
days) following ingestion of the bacteria.
Symptoms: Typically muscle pain, headache and
fever (known as the febrile prodrome) followed by
watery or bloody diarrhoea, abdominal pain and
nausea. Symptoms may last 1 day to 1 week or
longer (usually 5 days). Excretion of the organism in
stools occurs on average for 2 to 3 weeks and is
mostly self-limiting. Hospitalisation has been
reported in 13% of cases. The attack rate is around
45%.
Condition: Campylobacteriosis. Campylobacter
colonises the gut and damages the intestine. The
exact mechanisms of this remain unclear.
Toxins: Toxins are not produced in foods.
At Risk Groups: Can affect any age group but most
often isolated from infants (< 1 year) and young
(twenties) adults. Incidence higher in males (up to 45
years of age).
Long Term Effects: Infection may occasionally be
followed by arthritis (e.g. Reiters syndrome) or
Guillain-Barr Syndrome (GBS). 1% of cases suffer
reactive arthritis 7-10 days after onset. 0.1% of cases
develop GBS 1-3 weeks after infection, and of these
15% recover completely, 3-8% die and the rest
recover with varying degrees of impairment. A
number of other less common non-enteric diseases
can occur. Invasion of the bloodstream may occur in
1.5 per 100,000 cases, especially in the elderly. US
data suggests a case-fatality rate of around 3 per
100,000 outbreak associated illnesses.
Dose: Consumption of 800 cells causes infection on
approximately 50% of occasions, but the proportion
Prepared for the Ministry of Health by ESR Ltd.
1
Issued May 2001
These data sheets contain a summary of information available in the literature. Because of the many variables which impact on the survival of organisms in foods,
information in this sheet must be used as a guide only. Specific processes must be checked by the food manufacturer to ensure their product is safe.
of people becoming sick is not as high. Dose
response information for numbers less than this is
not available. Modelling has indicated an optimum
dose for becoming ill is 1,000-10,000 cells.
NZ Incidence: 320 cases/100,000 in 1998, 224.8 in
1999. There is a distinct seasonal trend, with most
cases occurring in Spring and Summer. Since
records were kept the overall trend is that of
increasing annual rates.
Treatment: Usually none, but fluids may be given.
Some cases warrant treatment with antibiotics.
Erythromycin is the drug of choice, although
resistant strains are emerging.
SOURCES
Human: Campylobacter is not one of the organisms
normally found in the human intestine. Faecal-oral
person-to-person transmission (in some cases by
asymptomatic carriers) has been reported.
Animal: Commonly found at high numbers in the
guts of ruminant animals. Some non-ruminant
animals (e.g. dogs and cats) are infected with the
organism and may, or may not, show signs of
disease. Flies have been implicated as vectors. Birds
are considered to be a primary reservoir.
Food: Raw poultry is frequently contaminated (5560% of samples in New Zealand); cooked chicken is
rarely contaminated (0.07%-NZ data). Raw milk,
offal, red meat, mushrooms, garlic butter, salads and
shellfish have all yielded Campylobacter. However
pathogenic species were not detected in New
Zealand commercially harvested shellfish.
Environment: Excreta from infected animals may
contaminate soil or water. Environmental survival is
conventionally considered to be poor but newer
information suggests it may be better than currently
acknowledged. For example Campylobacter has
been detected in dry beach sand. Survival in cold
water is good, but reduced at temperatures above
10oC. Recreational water (i.e. river water) in New
Zealand has been shown to be contaminated by
Campylobacter present at low concentrations.
Campylobacter is present in water and sediments
more frequently and at higher numbers in the winter
months. Environmental survival appears to be the
opposite to human cases, i.e. survival is poorer in the
warmer months.
Transmission Routes: The importance of
undercooked chicken as a source of a proportion of
cases of campylobacteriosis recognised, but the
relative importance of other routes, e.g. other foods,
recreational
unknown.
water,
occupational
exposure
is
OUTBREAKS AND INCIDENTS
Outbreaks: Most cases of disease are sporadic and
outbreaks relatively rare. Because the organism is
unlikely to grow in foods unless they are severely
temperature abused, most outbreaks are caused by
cross contamination or inadequate cooking. Correct
refrigeration serves to aid the survival of the
organism. In general contaminated milk (usually
unpasteurised) and water are considered to be
responsible for most outbreaks. However, any food
that may become contaminated can act as a vehicle.
New Zealand:
Liver Pt: 12 cases. Control point failure:
inadequate cooking of chicken livers.
Water: 19 cases. Control measure failure:
breakdown in chlorination of town supply.
Water: 67 cases. Control point failure; unsafe
drinking water supply.
Overseas:
Garlic butter: 30 cases, 4 hospitalised. Control
measure failure: inadequate heat treatment.
Milk: 23 cases, 0 hospitalised. Control measure
failure: milk unpasteurised.
Tuna salad: 79 cases, 39 cases in infirmary. Control
measure failure: cross contamination.
Cucumber: 78 cases. Control measure failure: cross
contamination.
Water: 257 cases. Control measure failure:
unchlorinated water.
Stir fried chicken: 12 cases, 1 hospitalisation.
Control measure failure: inadequate heat treatment.
Epidemiology: A major New Zealand study
identified recent consumption of raw or undercooked
chicken, and eating chicken in restaurants to be
associated with disease and there was also an
association with recent overseas travel, rainwater as
a source of water at home, consumption of raw dairy
products and contact with puppies and cattle,
particularly calves.
Associations
identified
overseas
include;
occupational exposure to raw meat, having a
household pet with diarrhoea, ingesting untreated
water from lakes, rivers and streams, travel abroad,
consumption of poultry liver, consumption of
poultry, consumption of sausages at a barbecue, and
eating poultry that was brought into the house raw.
Prepared for the Ministry of Health by ESR Ltd.
2
Issued May 2001
These data sheets contain a summary of information available in the literature. Because of the many variables which impact on the survival of organisms in foods,
information in this sheet must be used as a guide only. Specific processes must be checked by the food manufacturer to ensure their product is safe.
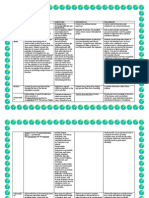
ADEQUATE PROCESSING GUIDELINES
N.B. These guidelines have been derived from published information. Industry is advised to ensure that
processing steps they are using are adequate to meet their particular food safety objectives.
Cook meats to:
Internal temperature reached
Minced meats (beef, veal, lamb, pork) + pork cuts
71oC
Minced poultry
74oC
63oC
Meat cuts (beef, veal, lamb), fish, seafood
77oC
Poultry, breast
82oC
Poultry, whole
Reheat cooked foods to
74oC
Reduce pH of food to 4.9
Avoid cross contamination from raw foods to cooked foods
Avoid direct handling of cooked ready-to-eat foods
Time
15 sec
Instantaneous
REFERENCES
Altekruse, S. F. et al. (1999) Campylobacter jejuni-An emerging foodborne pathogen. Emerging Infectious
Diseases 5;28-35.
Eberhardt-Phillips, J., Walker, N., Garrett, N., Bell, D., Sinclair, D., Rainger, W. and Bates, M. (1997)
Campylobacteriosis in New Zealand:results of a case control study. Journal of Epidemiology and
Community Health 51;686-691.
Lane, L. and Baker, M. (1993) Are we experiencing an epidemic of Campylobacter infection ? Communicable
Disease New Zealand 93;59-62,68.
Solomon, E.B. and Hoover, D.G. (1999) Campylobacter jejuni: A bacterial paradox. Journal of Food Safety
19; 121-136.
The International Commission on Microbiological Specifications for Foods (1996) Campylobacter. In Microorganisms in Foods 5 Microbiological Specifications of Food Pathogens, pp 45-65. Blackie Academic
and Professional, London.
The National Advisory Committee on Microbiological Criteria for Foods. (1995) Campylobacter jejuni/coli.
Dairy, Food and Environmental Sanitation 15; 133-153.
Prepared for the Ministry of Health by ESR Ltd.
3
Issued May 2001
These data sheets contain a summary of information available in the literature. Because of the many variables which impact on the survival of organisms in foods,
information in this sheet must be used as a guide only. Specific processes must be checked by the food manufacturer to ensure their product is safe.
Prepared for the Ministry of Health by ESR Ltd.
4
These data sheets contain a summary of information available in the literature. Because of the many variables which impact on the survival
of organisms in foods, information in this sheet must be used as a guide only. Specific processes must be checked by the food manufacturer
to ensure their product is safe.
Issued May 2
Das könnte Ihnen auch gefallen
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5795)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1091)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- Food Safety Presentation by SerSafeDokument372 SeitenFood Safety Presentation by SerSafeDeVillaM100% (2)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Haccp Butter ChickenDokument27 SeitenHaccp Butter ChickenAYMAN ZEHRA75% (4)
- CampylobacteriosisDokument34 SeitenCampylobacteriosisDoinaPendusNoch keine Bewertungen
- FSM Haccp Butter ChickenDokument26 SeitenFSM Haccp Butter ChickenAYMAN ZEHRANoch keine Bewertungen
- Food Borne Diseases Associated With Foods of Animal OriginDokument60 SeitenFood Borne Diseases Associated With Foods of Animal OriginWan SyarifuddinNoch keine Bewertungen
- Oral Fecal Route Diseases Oral Fecal Route Diseases: Afroz Lakhani RN, BSCNDokument74 SeitenOral Fecal Route Diseases Oral Fecal Route Diseases: Afroz Lakhani RN, BSCNafrozlakhaniNoch keine Bewertungen
- Risk Analysis - 2005 - Cox - Some Limitations of Qualitative Risk Rating SystemsDokument12 SeitenRisk Analysis - 2005 - Cox - Some Limitations of Qualitative Risk Rating SystemsSung Woo ShinNoch keine Bewertungen
- Food Poisoning - Causes, Symptoms, Treatments, RecoveryDokument9 SeitenFood Poisoning - Causes, Symptoms, Treatments, RecoveryJeyShidaNoch keine Bewertungen
- Campylobacter Food PoisoningDokument4 SeitenCampylobacter Food PoisoningVishnu Reddy Vardhan PulimiNoch keine Bewertungen
- Laboratory Diagnosis of Bacterial Gastroenteritis: Romney M. Humphries, Andrea J. LinscottDokument29 SeitenLaboratory Diagnosis of Bacterial Gastroenteritis: Romney M. Humphries, Andrea J. LinscottFatah Jati PNoch keine Bewertungen
- DiseasesDokument13 SeitenDiseasesJaypee SaturnoNoch keine Bewertungen
- 30 Chicken Diseases Every Farmer Should KnowDokument104 Seiten30 Chicken Diseases Every Farmer Should KnowHadrien FaryalaNoch keine Bewertungen
- PTS 60.1501.08 HSE Food Water SafetyDokument55 SeitenPTS 60.1501.08 HSE Food Water SafetyAmeerHamzaNoch keine Bewertungen
- Phenotypic and Molecular Characterization of Erythromycin Resistance in Campylobacter Jejuni and Broiler ChickensDokument6 SeitenPhenotypic and Molecular Characterization of Erythromycin Resistance in Campylobacter Jejuni and Broiler ChickensjavelezhNoch keine Bewertungen
- Campylobacteriosis DiseaseDokument10 SeitenCampylobacteriosis DiseasejannahNoch keine Bewertungen
- Diseases With Diarrhea SyndromeDokument19 SeitenDiseases With Diarrhea SyndromeManishNoch keine Bewertungen
- Birao Sas 13 Microbiology and ParasitologyDokument9 SeitenBirao Sas 13 Microbiology and ParasitologyFrancis Jacob Dejecacion GarcesNoch keine Bewertungen
- Thesis CampylobacterDokument6 SeitenThesis Campylobacterfc5wsq30100% (2)
- Clinical Manifestations, Diagnosis, and Treatment of Campylobacter Infection - UpToDateDokument19 SeitenClinical Manifestations, Diagnosis, and Treatment of Campylobacter Infection - UpToDateNedelcu MirunaNoch keine Bewertungen
- Pathogens and Pathways, and Small Drinking-Water SuppliesDokument22 SeitenPathogens and Pathways, and Small Drinking-Water SuppliesZari Sofia Leviste100% (1)
- BB Book 1Dokument149 SeitenBB Book 1Nilam Sa'diyahNoch keine Bewertungen
- Public Health MicrobiologyDokument39 SeitenPublic Health MicrobiologyBenyam ZenebeNoch keine Bewertungen
- Campylobacter OutlineDokument7 SeitenCampylobacter OutlineShania DawnNoch keine Bewertungen
- Unit 2 - The MicroworldDokument63 SeitenUnit 2 - The MicroworldVJ PelisigasNoch keine Bewertungen
- Midterm 1 (Test 1-10)Dokument34 SeitenMidterm 1 (Test 1-10)Priya SalunkeNoch keine Bewertungen
- EFSA Journal - 2022 - The European Union One Health 2021 Zoonoses ReportDokument273 SeitenEFSA Journal - 2022 - The European Union One Health 2021 Zoonoses ReportJulio San MartinNoch keine Bewertungen
- FSANZ FoodborneIllness 2013 WEBDokument120 SeitenFSANZ FoodborneIllness 2013 WEBBrandon EdwardsNoch keine Bewertungen
- SR0183, Bolton Broth Selective Supplement - Oxoid - Product Detail PDFDokument2 SeitenSR0183, Bolton Broth Selective Supplement - Oxoid - Product Detail PDFSadiya RhasyaNoch keine Bewertungen
- Bacterial Pathogens in Chicken Meat-444Dokument7 SeitenBacterial Pathogens in Chicken Meat-444bhawana bhattNoch keine Bewertungen
- Healthmedicinet Com II 2014 MayDokument381 SeitenHealthmedicinet Com II 2014 MayHeal ThmedicinetNoch keine Bewertungen