Beruflich Dokumente
Kultur Dokumente
1 Immco
Hochgeladen von
Dyah Ayu PitasariOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
1 Immco
Hochgeladen von
Dyah Ayu PitasariCopyright:
Verfügbare Formate
Bullous pemphigoid (BP) is a chronic,
autoimmune, subepidermal, blistering
disease of the skin. It rarely involves
mucous membranes. BP is characterized
by the presence of (1) immunoglobulin
IgG and complement deposits in the skin
of patients and (2) of the presence in the
serum of immunoglobulin G (IgG)
autoantibodies specific for the basement
membrane zone antigens such as to
BP230 ( BPAg1) and BP180 (BPAg2).
CLINICAL FEATURES
BP is uncommon, and its frequency is
unknown. No racial predilection is apparent.
BP primarily affects elderly individuals
in the fifth through seventh decades of
life, with an average age at onset of 65
years. A few cases of BP of childhood
onset have been reported in the literature.
The cause of BP is not known. Clinically
BP may present with several distinct clinical
presentations such as generalized bullous,
vesicular, vegetative, generalized erythroderma,
urticarial, and nodular. It can
affect any part of the skin surface, with a
predilection on the flexural areas of the
skin. Oral and ocular mucosa involvement
rarely occurs and, when seen, is of minor
clinical significance.
DIAGNOSIS
BP diagnosis is by biopsy and serum
analysis of the presence of autoantibodies
to the basement membrane zone (BMZ).
Biopsy studies include H&E and direct
immunofluorescence (IF). Direct IF studies
show the presence of immunoglobulins
and complement in the BMZ with a linear
pattern. Serum studies detect the presence
of autoantibodies to BMZ antigens by
indirect IF using primate esophagus
and/or split skin. For H&E biopsy should
be taken from the edge of a blister and for
direct IF studies biopsy should be from
normal-appearing perilesional skin.
The H&E examination demonstrates
subepidermal blister. The inflammatory
infiltrate is typically polymorphous, with
an eosinophil predominance. Direct IF
studies demonstrate in vivo deposits of
IgG (70-90% of patients) and complement
C3 deposition (90-100% of patients)
in a linear band at the BMZ. This pattern
of immunoreactants is also observed in
other sub-epidermal bullous diseases such
as mucous membrane pemphigoid
(MMP) and epidermolysis bullosa acquisita
(EBA). In summary, a combination of
clinical, histological, and IF studies are the
most reliable in diagnosis of BP.
BP can be differentiated from EBA by
localizing the site of immunedeposits on
the peri-lesional biopsy split at the lamina
lucida junction by incubating the patient's
skin biopsy in high salt. These antigen
localization studies can be performed
on specimens that have been submitted
for routine IF studies. Similar studies of
antigen localization can also be performed
on serum. Based on the site of localization
of immune deposits differentaiton between
BP and EBA can reliably be made as
summarized to the right.
TREATMENT
Topical steroids are effective however
their use in extensive disease may be
limited by side effects and practical
factors. The effectiveness of the addition
of plasma exchange or azathioprine to
corticosteroids has not been fully
established. Combination treatment with
tetracycline and nicotinamide may be
useful.
IMMCO Diagnostics, Inc.
60 Pineview Drive
Buffalo, NY 14228 USA | www.immco.com
toll free North America: 1-800-537-8378
Das könnte Ihnen auch gefallen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Autoimmune Plant Based Cookbook SpreadDokument74 SeitenThe Autoimmune Plant Based Cookbook Spreadskknf7jqpn100% (1)
- DR - Satyen Bhattacharyya Assistant Professor: BIMLS, BurdwanDokument38 SeitenDR - Satyen Bhattacharyya Assistant Professor: BIMLS, Burdwanpraveen kumarNoch keine Bewertungen
- The Diagnosis and Treatment of Autoimmune Encephalitis JCN 2016Dokument13 SeitenThe Diagnosis and Treatment of Autoimmune Encephalitis JCN 2016Alex Del PieroNoch keine Bewertungen
- Autoimmune Polyglandular Syndrome Type 2 - The Tip of An IcebergDokument9 SeitenAutoimmune Polyglandular Syndrome Type 2 - The Tip of An IcebergtoroalfaroNoch keine Bewertungen
- NewsArchives PDFDokument392 SeitenNewsArchives PDFkitty katNoch keine Bewertungen
- Myositis Autoantibodies and Clinical Phenotypes 2104Dokument7 SeitenMyositis Autoantibodies and Clinical Phenotypes 2104Mario SuarezNoch keine Bewertungen
- Anti-TG ARCDokument7 SeitenAnti-TG ARCMariaNoch keine Bewertungen
- Managing Lockjaw Disorders in Dogs: TrismusDokument14 SeitenManaging Lockjaw Disorders in Dogs: TrismusmiloNoch keine Bewertungen
- Associação Da Ingestão de Glúten Nos Primeiros 5 Anos de Vida e A Incidencia de Doença CeliacaDokument10 SeitenAssociação Da Ingestão de Glúten Nos Primeiros 5 Anos de Vida e A Incidencia de Doença CeliacaAna Beatriz SpagollaNoch keine Bewertungen
- Chronic UrticariaDokument40 SeitenChronic UrticariaeeeeewwwwwNoch keine Bewertungen
- Plasmapheresis in Nephrology Voinov V.ADokument13 SeitenPlasmapheresis in Nephrology Voinov V.AEliDavidNoch keine Bewertungen
- Pathogenesis of Type 1 Diabetes MellitusDokument12 SeitenPathogenesis of Type 1 Diabetes MellitusJIEHASMARTNoch keine Bewertungen
- Serum Anti-Myelin-Associated Glycoprotein Antibodies in Egyptian Autistic ChildrenDokument6 SeitenSerum Anti-Myelin-Associated Glycoprotein Antibodies in Egyptian Autistic ChildrenmhabranNoch keine Bewertungen
- Reumatoid ArthritisDokument19 SeitenReumatoid Arthritishenning_mastereid166Noch keine Bewertungen
- Vaccination and Autoimmune Disease: What Is The Evidence?: ReviewDokument8 SeitenVaccination and Autoimmune Disease: What Is The Evidence?: Reviewtito7227Noch keine Bewertungen
- Veterinary Immunology: Fuad Mohammed (DVM, MSC, Assist. Prof.)Dokument36 SeitenVeterinary Immunology: Fuad Mohammed (DVM, MSC, Assist. Prof.)BEKUMA SHIBIRUNoch keine Bewertungen
- CFS - Denigration by DesignDokument246 SeitenCFS - Denigration by Designfatima110Noch keine Bewertungen
- Diseases of ImmunityDokument55 SeitenDiseases of ImmunityMeera ANN AJINoch keine Bewertungen
- Case QuestionsDokument6 SeitenCase Questionsapi-353723892Noch keine Bewertungen
- Reference: Maglumi Tma (Clia)Dokument4 SeitenReference: Maglumi Tma (Clia)Lidia NarbNoch keine Bewertungen
- MR Supple All 2014Dokument429 SeitenMR Supple All 2014Regita Ayu LestariNoch keine Bewertungen
- 5 Immunological DisordersDokument22 Seiten5 Immunological DisordersPaula CárdenasNoch keine Bewertungen
- Disorders of The Immune System: Allergic DiseasesDokument2 SeitenDisorders of The Immune System: Allergic DiseasesElisha RosalynNoch keine Bewertungen
- Autoimmunity Reviews: A. Greco, M. Fusconi, A. Gallo, C. Marinelli, G.F. Macri, M. de VincentiisDokument6 SeitenAutoimmunity Reviews: A. Greco, M. Fusconi, A. Gallo, C. Marinelli, G.F. Macri, M. de Vincentiisronaldyohanesf87Noch keine Bewertungen
- 44 - 75 - Detection of Autoantibodies Against Platelet Glycoproteins in ... HeDokument21 Seiten44 - 75 - Detection of Autoantibodies Against Platelet Glycoproteins in ... HevishnupgiNoch keine Bewertungen
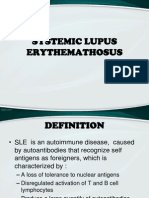
- Systemic Lupus ErythemathosusDokument23 SeitenSystemic Lupus ErythemathosusFransisca HardimartaNoch keine Bewertungen
- Autoimmune Rheumatic DiseasesDokument3 SeitenAutoimmune Rheumatic DiseasesBuat DownloadNoch keine Bewertungen
- Paleo Book PDFDokument679 SeitenPaleo Book PDFsindza100% (17)
- Classification of Rheumatic DiseasesDokument29 SeitenClassification of Rheumatic DiseasesBahaa Shaaban100% (5)
- Deepthi M 3rd Semester, MSC MicrolobiologyDokument23 SeitenDeepthi M 3rd Semester, MSC MicrolobiologyShalini MNoch keine Bewertungen