Beruflich Dokumente
Kultur Dokumente
Cardio Vascular Diabetes Risk Assessment 6dec13 Summary
Hochgeladen von
JoshVereker-BindonCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Cardio Vascular Diabetes Risk Assessment 6dec13 Summary
Hochgeladen von
JoshVereker-BindonCopyright:
Verfügbare Formate
New Zealand Primary Care Handbook (2012) Update 2013
Cardiovascular and Diabetes
Risk Assessment
Whats new?
The overarching principle is that the intensity
of interventions should be proportional to the
size of the estimated combined cardiovascular
disease (CVD) risk. This recommendation has not
changed.
Relative risk reductions are more or less constant
across the spectrum of combined risk. The higher
the combined risk, the larger the absolute benefit
of treating one or more risk factors.
The majority of patients with:
an estimated five-year combined CVD risk
below 10 percent can generally be well
managed without drug treatment
magnitude of absolute benefits and the harms
of interventions. Individuals will vary in the way
they interpret these risk estimates and in their
desire and willingness to act on them.
Measuring lipids
Non-fasting tests are an appropriate way of
measuring lipids. One non-fasting measurement
is appropriate for risk assessment.
Measuring HbA1c for diabetes
HbA1c is the preferred test for the majority of
people. Any patient with an HbA1c from
41 to 49 requires advice about reducing their risk
of diabetes. Fasting is never required for HbA1c.
an estimated five-year combined CVD risk
between 10 percent and 20 percent will benefit
from shared decision making about the benefits
and harms of blood pressure (BP) and lipidlowering drugs
The Ministry of Health has provided advice about
pre-diabetes at www.hiirc.org.nz (search for
pre-diabetes advice).
a combined CVD risk over 20 percent,
including patients with a personal history of
CVD, are likely to benefit significantly from
blood pressure lowering, lipid-lowering and
antiplatelet medication, over and above
intensive non-pharmacological interventions.
For combined risk over 20 percent, monitoring
of non-fasting lipids every three to six months
until stable and then every one to two years is
recommended.
Clinical judgment and informed patient
preferences (shared decision-making) should
feature in decisions about treatment for
all people, and particularly for those in the
intermediate range of risk and for younger or
older people. Shared treatment decisions should
take into account an individuals estimated
five-year combined1 CVD risk and the
Monitoring lipids
For combined risk under 20 percent, the aim
is to achieve a moderate reduction in LDL-C.
Re-measurement can wait until the next
combined risk assessment.
Following lifestyle management interventions,
non-fasting lipids should be repeated at time of
review, usually after 6 to 12 months.
1 The word combined is used to reflect the calculated risk based on the combined effects of known cardiovascular risk factors.
Non face-to-face cardiovascular risk assessment: It is reasonable to apply blood pressure, non-fasting total cholesterol, HDL-C and HBA1c (or
fasting glucose) measurements that have been recorded during the previous five years if the persons circumstances have not significantly
changed. The higher the risk level that is established in retrospect, the more important it is to establish a current estimate. The result must be
communicated to the patient.
The recommended interventions, goals and follow-up based on cardiovascular
risk assessment
Cardiovascular risk
Established CVD
CVD risk
calculated
>20%
Lifestyle
Drug therapy
Follow-up
Intensive lifestyle advice
(diet, physical activity,
smoking cessation)
simultaneously with
drug treatment
Strong evidence of benefit
from BP-lowering, statins
and antiplatelet therapy in
this group
Risk factor monitoring
initially at 3 months,
then as clinically
indicated
Intensive lifestyle advice
(diet, physical activity,
smoking cessation)
simultaneously with
drug treatment
Strong evidence of benefit
from BP-lowering, statins
and antiplatelet therapy in
this group
Annual review or as
clinically indicated
Specific individualised
lifestyle advice (diet,
physical activity,
smoking cessation)
Good evidence
demonstrating benefit
from BP-lowering and/
or statin therapy in this
group. The absolute benefits
will be smaller at lower
levels of combined risk,
with increasing benefit of
treating both BP and lipids
for those with higher
five-year combined risk
As clinically indicated,
with a more intensive
focus for higher
combined risk patients
10% to 20%
If patient not on drug
treatment, offer CVD
risk assessment at
reassessment at one
year for 15% to 20% risk
and every two years for
10% to 15% risk
Shared decision-making
approach to consider
benefits and harms of drug
treatment of modifiable
risk factors
Lifestyle advice (diet,
physical activity,
smoking cessation)
<10%
Evidence of benefit from
BP-lowering and statin
therapy in this group is
unclear; use a shared
decision-making approach
to consider benefits and
harms of treatment of
modifiable risk factors
Offer further CVD
risk assessment in
5 to 10 years
December 2013 HP 5767
Das könnte Ihnen auch gefallen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (119)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- MD AANOADokument21 SeitenMD AANOARizka Dany AfinaNoch keine Bewertungen
- Pharmacology Lab (1) : Routes of Drug AdministrationDokument14 SeitenPharmacology Lab (1) : Routes of Drug AdministrationBotan AbdullahNoch keine Bewertungen
- NS Compounding Set 4 PDFDokument24 SeitenNS Compounding Set 4 PDFJulia BottiniNoch keine Bewertungen
- Staph Lecture MicrococcusDokument30 SeitenStaph Lecture Micrococcussophia salibaNoch keine Bewertungen
- Understanding Hepatic Encephalopathy (HE) Symptoms, Causes and TreatmentDokument3 SeitenUnderstanding Hepatic Encephalopathy (HE) Symptoms, Causes and TreatmentSuhas KandeNoch keine Bewertungen
- A Case of Patient AI, Who Came in Due To Sore ThroatDokument16 SeitenA Case of Patient AI, Who Came in Due To Sore ThroatLovelle LopezNoch keine Bewertungen
- DR Putu Gde Hari WangsaDokument5 SeitenDR Putu Gde Hari Wangsahariwangsa23Noch keine Bewertungen
- Fast Paces Academy - SymptomsDokument21 SeitenFast Paces Academy - SymptomsAdil ShabbirNoch keine Bewertungen
- Upper Extremity Venous Doppler Ultrasound PDFDokument12 SeitenUpper Extremity Venous Doppler Ultrasound PDFLayla Salomão0% (1)
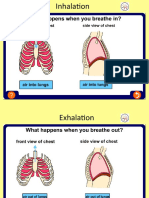
- Asthma Inhale and ExhaleDokument14 SeitenAsthma Inhale and ExhaleNguyen Nhu VinhNoch keine Bewertungen
- Figure 1. New Criteria For AKI Diagnosis Are Displayed. in Order To Diagnose AKIDokument8 SeitenFigure 1. New Criteria For AKI Diagnosis Are Displayed. in Order To Diagnose AKIMayra Alejandra Prada SerranoNoch keine Bewertungen
- Certificate For COVID-19 Vaccination: Beneficiary DetailsDokument1 SeiteCertificate For COVID-19 Vaccination: Beneficiary DetailsAshok KumarNoch keine Bewertungen
- 10kCdz5YW-djkylc0QnB YNo5hs4Vfe9zDokument45 Seiten10kCdz5YW-djkylc0QnB YNo5hs4Vfe9zwangchengching29Noch keine Bewertungen
- Stem Cells and Cancer Stem Cells, Volume 2 - Stem Cells and Cancer Stem Cells, Therapeutic Applications in Disease and Injury - Volume 2Dokument409 SeitenStem Cells and Cancer Stem Cells, Volume 2 - Stem Cells and Cancer Stem Cells, Therapeutic Applications in Disease and Injury - Volume 2ArtanNoch keine Bewertungen
- Winkler - Chapter 8. Khalid AlshareefDokument4 SeitenWinkler - Chapter 8. Khalid AlshareefKhalid Bin FaisalNoch keine Bewertungen
- CLINICAL CHEMISTRY 2 Tumor MarkersDokument3 SeitenCLINICAL CHEMISTRY 2 Tumor MarkersSuzzaine EniazzusNoch keine Bewertungen
- ODC Nursing FormsDokument5 SeitenODC Nursing Formsgyds_17Noch keine Bewertungen
- Amoxicillin Therapy Valid for Pneumonia in ChildrenDokument4 SeitenAmoxicillin Therapy Valid for Pneumonia in ChildrenShofaajiNoch keine Bewertungen
- Slavin 1996Dokument6 SeitenSlavin 1996jahdsdjad asffdhsajhajdkNoch keine Bewertungen
- A Prospective Study On Acute Limb Ischemia - Presentation, Management, Outcome - Our Institutional ExperienceDokument6 SeitenA Prospective Study On Acute Limb Ischemia - Presentation, Management, Outcome - Our Institutional ExperienceIJAR JOURNALNoch keine Bewertungen
- Complete Genetics Disease ChartDokument14 SeitenComplete Genetics Disease ChartJames FlanneryNoch keine Bewertungen
- What Are The Different Types of Stress?Dokument2 SeitenWhat Are The Different Types of Stress?Полина КосьминаNoch keine Bewertungen
- Vet Histology Lecture Notes on Digestive System IDokument62 SeitenVet Histology Lecture Notes on Digestive System IDEV3LLS100% (3)
- He367t R1 RCDokument2 SeitenHe367t R1 RCSedighe VafaieNoch keine Bewertungen
- Group 1 Case Study Chapter 24Dokument10 SeitenGroup 1 Case Study Chapter 24Doneva Lyn MedinaNoch keine Bewertungen
- Assessment of The Thorax and LungsDokument108 SeitenAssessment of The Thorax and LungsJohn Martin Casihan100% (3)
- 2007 MCQDokument67 Seiten2007 MCQTiffani Gutierrez100% (1)
- CV Peneliti UtamaDokument14 SeitenCV Peneliti Utamabidan lidiafNoch keine Bewertungen
- RENBUT BHN LAB 2022 SD Agt 2023Dokument3 SeitenRENBUT BHN LAB 2022 SD Agt 2023ajisNoch keine Bewertungen
- Impaired Gas Exchange NCPDokument1 SeiteImpaired Gas Exchange NCPCj AlconabaNoch keine Bewertungen