Beruflich Dokumente
Kultur Dokumente
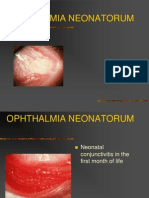
Ophthalmia Neonatorum
Hochgeladen von
Ejay BautistaOriginalbeschreibung:
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Ophthalmia Neonatorum
Hochgeladen von
Ejay BautistaCopyright:
Verfügbare Formate
CLINICAL MANAGEMENT GUIDELINES
Ophthalmia neonatorum
Aetiology
Ophthalmia Neonatorum (ON) (conjunctivitis of the newborn) occurs
within the first 30 days of life. It may be infective or non-infective
Infective
Bacterial, chlamydial or viral infection acquired during passage through
an infected birth canal
Historically, the commonest agent was Neisseria gonorrhoeae
(gonococcus) and the use of silver nitrate drops as prophylaxis was
introduced in the C19, although abandoned in the UK in the 1950s.
Nowadays the usual agent is Chlamydia trachomatis. The prevalence of
ON differs in different parts of the world and is dependent mainly upon
socioeconomic conditions, level of knowledge about general health,
standard of maternal healthcare as well as the type of prophylactic
programme used. In the UK, the incidence in 2003 was as follows:
C. trachomatis: 6.9 per 100,000 live births
N. gonorrhoeae: 3.7 per 100,000 live births
In developing countries, very much higher incidences have been
reported
Other bacteria that can cause ON include Haemophilus, Streptococcus,
Staphylococcus and Pseudomonas species. ON can also complicate
generalised neonatal Herpes simplex infection
The neonatal conjunctiva is particularly vulnerable to infection because
of the lack of immunity and the absence of local lymphoid tissue at birth
The incubation period is usually as follows:
C. trachomatis: 5-14 days
N. gonorrhoeae: 3-5 days
Predisposing factors
Symptoms
Signs
Opthalmia neonatorum
Version 8 22.07.13
Non-infective
Usually chemical conjunctivitis, induced by agents used for prophylaxis
Infection of the maternal birth canal as the result of sexually-transmitted
disease
This infection may be asymptomatic, especially in the case of C.
trachomatis
Symptoms (usually described by mother):
Redness
Discharge (may be profuse in gonococcal infection)
Swelling of lids (may be severe)
Symptoms usually bilateral
Lids
Oedema (may impede examination of ocular surfaces)
Conjunctival features
Mucopurulent conjunctivitis discharge may be profuse in C.
trachomatis infection. Danger of infection of clinician when
prising open lids
NB: in neonatal C. trachomatis infection there are no follicles as
in adults, because of the neonates lack of lymphoid tissue
Conjunctival oedema (chemosis)
Conjunctival membrane in severe cases
Corneal features
Cornea can be involved, especially in N. gonorrhoeae infection.
This organism can pass through intact corneal epithelium.
Perforation may result
1 of 2
CLINICAL MANAGEMENT GUIDELINES
Ophthalmia neonatorum
Differential diagnosis
Signs usually bilateral; may be asymmetrical
By definition, conjunctivitis occurring within the first 30 days of life
is ON
Congenital obstruction of the nasolacrimal duct(s) is often
associated with epiphora, discharge and recurrent conjunctivitis
(see Clinical Management Guideline on Nasolacrimal Duct
Obstruction)
Management by Optometrist
Practitioners should recognise their limitations and where necessary seek further advice or refer
the patient elsewhere
Non pharmacological
None
Pharmacological
None
Management Category A1: emergency (same day) referral to Ophthalmologist; no intervention
ON may result in a severe and progressive conjunctivitis with corneal
complications and be associated with potentially serious systemic
infection
Possible management by Ophthalmologist
Diagnosis
Conjunctival cultures for bacteria (N. gonorrhoeae requires
special media)
Conjunctival scraping for Gram stain (bacteria) and Giemsa stain
(for C. trachomatis)
Polymerase chain reaction (PCR) studies
Treatment
Bacterial conjunctivitis
Systemic penicillin G or a cephalosporin for N. gonorrhoeae
Topical erythromycin sometimes given in addition
Other topical antibiotics, including azithromycin
Frequent irrigation until discharge ceases
Chlamydial conjunctivitis
Systemic erythromycin
Topical azithromycin
Herpetic conjunctivitis
Systemic aciclovir
Evidence base
Darling EK, McDonald H
A meta-analysis of the efficacy of ocular prophylactic agents used for the
prevention of gonococcal and chlamydial ophthalmia neonatorum
J Midwifery Womens Health 2010;55:319-27
Authors conclusions: Failure rates of universal eye prophylaxis support
reexamination of this policy where the prevalence of maternal infection is
low. (North American practice)
(The Oxford 2011 Levels of Evidence = 1)
Opthalmia neonatorum
Version 8 22.07.13
2 of 2
Das könnte Ihnen auch gefallen
- The Ideal Candida Diet Cookbook; The Superb Diet Guide To Alleviate Candida Symptoms And Restore Gut Health With Nutritious RecipesVon EverandThe Ideal Candida Diet Cookbook; The Superb Diet Guide To Alleviate Candida Symptoms And Restore Gut Health With Nutritious RecipesNoch keine Bewertungen
- Ophthalmia NeonatorumDokument2 SeitenOphthalmia NeonatorumjudssalangsangNoch keine Bewertungen
- ConjunctivitisDokument113 SeitenConjunctivitisHussam AliNoch keine Bewertungen
- Jurnal 2Dokument3 SeitenJurnal 2danna aflahNoch keine Bewertungen
- Gonococcal ConjunctivitisDokument7 SeitenGonococcal ConjunctivitishadijahNoch keine Bewertungen
- Home (/KB/) / Ophthalmia NeonatorumDokument8 SeitenHome (/KB/) / Ophthalmia NeonatorumMohammed Shamiul ShahidNoch keine Bewertungen
- Sindrome Duh Genital GODokument9 SeitenSindrome Duh Genital GOIntan PermataNoch keine Bewertungen
- Ophthalmia NeonatorumDokument30 SeitenOphthalmia NeonatorumLing TaerahkunNoch keine Bewertungen
- Opthalmia UmDokument23 SeitenOpthalmia Umnanu-jenuNoch keine Bewertungen
- Atypicalpneumonia NezDokument22 SeitenAtypicalpneumonia NezNezz AdrianiNoch keine Bewertungen
- Microbial Keratitis Royal College of OphthalmologistDokument2 SeitenMicrobial Keratitis Royal College of OphthalmologistmahadianNoch keine Bewertungen
- Caso Clínico - Neisseria GonorrhoeaeDokument7 SeitenCaso Clínico - Neisseria GonorrhoeaeRigobertoNoch keine Bewertungen
- Neonatal Sepsis, Opthalmia Neonatarum & HIV/AIDSDokument15 SeitenNeonatal Sepsis, Opthalmia Neonatarum & HIV/AIDSSAKSHI RANANoch keine Bewertungen
- Bakteri Penyebab IMSDokument67 SeitenBakteri Penyebab IMSuut14Noch keine Bewertungen
- Ophthalmia NeonatorumDokument2 SeitenOphthalmia NeonatorumconcozNoch keine Bewertungen
- Page Two 100509ToxoplasmaGondiinfectsMostSpeciesPage2Dokument2 SeitenPage Two 100509ToxoplasmaGondiinfectsMostSpeciesPage2Ralph Charles Whitley, Sr.Noch keine Bewertungen
- GonorrheaDokument53 SeitenGonorrheaapi-1991639975% (4)
- Ophthalmia NeonatorumDokument5 SeitenOphthalmia NeonatorumDelphy VargheseNoch keine Bewertungen
- Chlamydia TrachomatisDokument7 SeitenChlamydia TrachomatisDewi SetiawatiNoch keine Bewertungen
- Ophthalmia NeonatorumDokument3 SeitenOphthalmia NeonatorumDyraWirasasmitaMirsanNoch keine Bewertungen
- Gram (-) Cocci: NeisseriaceaeDokument8 SeitenGram (-) Cocci: NeisseriaceaeMary Grace RiveraNoch keine Bewertungen
- ConjunctivitisDokument52 SeitenConjunctivitisFiona H.D.100% (2)
- Antibiotics 07 00059 v2Dokument8 SeitenAntibiotics 07 00059 v2alfiraNoch keine Bewertungen
- Ophthalmia neonatorumIIDokument29 SeitenOphthalmia neonatorumIIgopscharanNoch keine Bewertungen
- Chlamydia SPPDokument22 SeitenChlamydia SPPemmarie gwen tanNoch keine Bewertungen
- ChancroidDokument4 SeitenChancroidDaniel Vergara ArceNoch keine Bewertungen
- Sexually Transmitted Infections (Sti) Ii: Return To SyllabusDokument15 SeitenSexually Transmitted Infections (Sti) Ii: Return To SyllabusANGGITA LARASATI PURBANINGRUMNoch keine Bewertungen
- EndometritisDokument6 SeitenEndometritisandriansyah2110% (1)
- Neonatal Conjunctivitis PDFDokument5 SeitenNeonatal Conjunctivitis PDFEskanita Anggun RNoch keine Bewertungen
- Pelvic Infections in Women: Belgian Guidelines: OutlineDokument35 SeitenPelvic Infections in Women: Belgian Guidelines: OutlineJose mauricio PalenciaNoch keine Bewertungen
- Gyne - (Section B) PID-STI-1Dokument45 SeitenGyne - (Section B) PID-STI-1Kailash KhatriNoch keine Bewertungen
- Gonorrhea 1Dokument26 SeitenGonorrhea 1Alessandra Franchesca CortezNoch keine Bewertungen
- Ophthalmia NeonatorumDokument17 SeitenOphthalmia NeonatorumIndranil DuttaNoch keine Bewertungen
- Gonococcal Infection in The Newborn - UpToDateDokument13 SeitenGonococcal Infection in The Newborn - UpToDateCarina ColtuneacNoch keine Bewertungen
- Agranulocytosis FinalDokument17 SeitenAgranulocytosis FinalsanthiyasandyNoch keine Bewertungen
- Endophtalmitis: AnamnesisDokument6 SeitenEndophtalmitis: AnamnesisErlinda AgustinaNoch keine Bewertungen
- Trachoma Assignment On CHNDokument6 SeitenTrachoma Assignment On CHNSovon SamantaNoch keine Bewertungen
- Viral Conjunctivitis AlgorithmDokument8 SeitenViral Conjunctivitis AlgorithmRobert Selvin MNoch keine Bewertungen
- Essentials of Diagnosis: GonorrheaDokument4 SeitenEssentials of Diagnosis: GonorrheaMalueth AnguiNoch keine Bewertungen
- Gonorrhea: SymptomsDokument9 SeitenGonorrhea: Symptomspragna novaNoch keine Bewertungen
- Gynaecology: Gum, Fertility, Contraception, and UrogynaecologyDokument46 SeitenGynaecology: Gum, Fertility, Contraception, and UrogynaecologyOccamsRazorNoch keine Bewertungen
- Toxoplasmosis AaoDokument28 SeitenToxoplasmosis AaoUNHAS OphthalmologyNoch keine Bewertungen
- Optha SeminarDokument29 SeitenOptha SeminarYoseph DemisseNoch keine Bewertungen
- InfectiousDokument4 SeitenInfectiouszainabd1964Noch keine Bewertungen
- Chlamydia and Nonspecific UrethritisDokument4 SeitenChlamydia and Nonspecific UrethritisErfina BasriNoch keine Bewertungen
- Conjunctivitis - Diagnosis & DDXDokument7 SeitenConjunctivitis - Diagnosis & DDXNabillaMerdikaPutriKusumaNoch keine Bewertungen
- Bahan GonoreDokument7 SeitenBahan GonoreAlzena AkbarNoch keine Bewertungen
- Sexual Transmitted InfectionsDokument44 SeitenSexual Transmitted InfectionsDeshielanny AlagumolyNoch keine Bewertungen
- Biology ProjectDokument17 SeitenBiology ProjectSakti MageswariNoch keine Bewertungen
- Ophthalmia NeonatorumDokument5 SeitenOphthalmia NeonatorumTeresa MontesNoch keine Bewertungen
- Ecthyma Gangrenosum - StatPearls - NCBI BookshelfDokument5 SeitenEcthyma Gangrenosum - StatPearls - NCBI BookshelfSyafira Laila NurulitaNoch keine Bewertungen
- Conjunctivitis 1Dokument8 SeitenConjunctivitis 1Opubo BrownNoch keine Bewertungen
- Notes MICROBIAL DISEASES and EPIDEMIOLOGYDokument12 SeitenNotes MICROBIAL DISEASES and EPIDEMIOLOGYDaniella TupasNoch keine Bewertungen
- Artikan 3Dokument1 SeiteArtikan 3Rivan San JayaNoch keine Bewertungen
- MSD Pro DocumentDokument6 SeitenMSD Pro DocumentMuhammedNoch keine Bewertungen
- BMJ 335 7630 CR 01147 Vaginal DischargeDokument5 SeitenBMJ 335 7630 CR 01147 Vaginal DischargeHassan Abdullah AL-balushiNoch keine Bewertungen
- Mycoplasma Pneumonia DiscussionDokument18 SeitenMycoplasma Pneumonia Discussionmuskaanmir108Noch keine Bewertungen
- Infectious Endophthalmitis After: CataractDokument6 SeitenInfectious Endophthalmitis After: CataractSurendar KesavanNoch keine Bewertungen
- Harper's Textbook of Pediatric DermatologyVon EverandHarper's Textbook of Pediatric DermatologyProf. Dr. Alan D. IrvineNoch keine Bewertungen
- Anxiety CaseDokument2 SeitenAnxiety CaseEjay BautistaNoch keine Bewertungen
- Surgery 3rd Shifting Se 2017Dokument8 SeitenSurgery 3rd Shifting Se 2017Ejay BautistaNoch keine Bewertungen
- Psych Case 2Dokument1 SeitePsych Case 2Ejay BautistaNoch keine Bewertungen
- Psych Case 2Dokument1 SeitePsych Case 2Ejay BautistaNoch keine Bewertungen
- IpfDokument2 SeitenIpfEjay BautistaNoch keine Bewertungen
- Evolution Fern and Low LightDokument14 SeitenEvolution Fern and Low LightEjay BautistaNoch keine Bewertungen
- History of COVID-19Dokument2 SeitenHistory of COVID-19Sahara SoboNoch keine Bewertungen
- Capsicum Frustascens Cayenne Pepper Decoction As An Alternative Killer For CockroachesDokument4 SeitenCapsicum Frustascens Cayenne Pepper Decoction As An Alternative Killer For CockroachesRhitzelynn Ann BarredoNoch keine Bewertungen
- Pancasakti Journal of Public Health Science and ResearchDokument8 SeitenPancasakti Journal of Public Health Science and Researchnabilah dwi nopridaNoch keine Bewertungen
- Trusted Medical Answers-In Seconds.: General MycologyDokument19 SeitenTrusted Medical Answers-In Seconds.: General MycologyntnquynhproNoch keine Bewertungen
- Vis DtapDokument2 SeitenVis DtapBeeco SiboroNoch keine Bewertungen
- 1-Coronavirus Covid-19 Test (RT-PCR Technique) - PO1241383262-904Dokument1 Seite1-Coronavirus Covid-19 Test (RT-PCR Technique) - PO1241383262-904RudraNathNoch keine Bewertungen
- END TB by 2025Dokument32 SeitenEND TB by 2025neeta mathurNoch keine Bewertungen
- Sumana Mondal - 6448287517244598Dokument4 SeitenSumana Mondal - 6448287517244598PRONAB MAJHINoch keine Bewertungen
- An Investegatory Project ReportDokument17 SeitenAn Investegatory Project ReportKhushi kapseNoch keine Bewertungen
- WHO Report On Surveillance: of Antibiotic ConsumptionDokument58 SeitenWHO Report On Surveillance: of Antibiotic ConsumptionLeonel Fernandez RamirezNoch keine Bewertungen
- Pelvic Inflammatory DiseaseDokument48 SeitenPelvic Inflammatory DiseaseAnonymouscatNoch keine Bewertungen
- Blood Transfusion FormDokument2 SeitenBlood Transfusion FormGMCH LaboratoryNoch keine Bewertungen
- Materi 1 KLS Xi PersonalDokument4 SeitenMateri 1 KLS Xi Personalakusopo JalNoch keine Bewertungen
- Essential Questions in Paediatrics For MRCPCH v2 PDFDokument208 SeitenEssential Questions in Paediatrics For MRCPCH v2 PDFa4aboo100% (10)
- TOPIC 1 24-Oct-2021 Perjumpaan Bersemuka PJJ Minggu PertamaDokument60 SeitenTOPIC 1 24-Oct-2021 Perjumpaan Bersemuka PJJ Minggu PertamaSleeping BeautyNoch keine Bewertungen
- EPIDEMIC Vs PANDEMICDokument3 SeitenEPIDEMIC Vs PANDEMICRiddhi PansareNoch keine Bewertungen
- Information On Vaccination-Differentiated Safe Management Measures (SMMS)Dokument9 SeitenInformation On Vaccination-Differentiated Safe Management Measures (SMMS)Goh Yong DaNoch keine Bewertungen
- Macdona Masali AssignmentDokument5 SeitenMacdona Masali AssignmentMasali MacdonaNoch keine Bewertungen
- Casey Infectious Disease PamphletDokument2 SeitenCasey Infectious Disease Pamphletapi-552547083Noch keine Bewertungen
- To Promote Good Hygiene and Physical Comfort.: Coli (E. Coli), NormallyDokument2 SeitenTo Promote Good Hygiene and Physical Comfort.: Coli (E. Coli), NormallyFran LanNoch keine Bewertungen
- An Introduction of MalariaDokument19 SeitenAn Introduction of MalariaSomesh GuptaNoch keine Bewertungen
- TB Case StudyDokument2 SeitenTB Case StudyReisabelle LabianoNoch keine Bewertungen
- Management - Guidelines - of - Malaria - in - Malaysia - (Final) v2 PDFDokument63 SeitenManagement - Guidelines - of - Malaria - in - Malaysia - (Final) v2 PDFaiyuanNoch keine Bewertungen
- Timoteo Paez Integrated School (SHS) : Research PlanDokument9 SeitenTimoteo Paez Integrated School (SHS) : Research PlanEzekiel AvisoNoch keine Bewertungen
- CandidiasisDokument6 SeitenCandidiasisNabrazz SthaNoch keine Bewertungen
- Enterobacteriaceae ManualDokument1 SeiteEnterobacteriaceae ManualMukhtiar AliNoch keine Bewertungen
- Operational Guidelines On Limited Face To Face ImplementationDokument36 SeitenOperational Guidelines On Limited Face To Face ImplementationJohn Paul light100% (3)
- Laporan-Diagnosa DesemberDokument421 SeitenLaporan-Diagnosa DesemberPutri Annisa0% (1)
- Pendahuluan: Skin and Soft Tissue Infections (Sstis)Dokument15 SeitenPendahuluan: Skin and Soft Tissue Infections (Sstis)Ribka TheodoraNoch keine Bewertungen
- Maklumat Vaksinasi: Vaccination DetailsDokument2 SeitenMaklumat Vaksinasi: Vaccination DetailsHazadiana ZainalNoch keine Bewertungen