Beruflich Dokumente
Kultur Dokumente
Dimero D en Tep
Hochgeladen von
Alvaro Andres Flores JimenezOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Dimero D en Tep
Hochgeladen von
Alvaro Andres Flores JimenezCopyright:
Verfügbare Formate
Clinical Review & Education
JAMA Diagnostic Test Interpretation
D-Dimer for Pulmonary Embolism
Grgoire Le Gal, MD, PhD; Marc Righini, MD; Philip S. Wells, MD, MSc
An 82-year-old woman with bladder cancer and treated hypertension was referred by
her family physician after she reported experiencing a few days history of mild fever,
cough, limited deep inspiration, and left-sided pleuritic chest pain. She had no personal
or family history of venous thrombosis and did not have any recent surgery, trauma, or
admission to hospital. Her long-term medications included fluoxetine, vitamin D, and
hydrochlorothiazide.
On examination, temperature was 38.3C (101F), blood pressure was
157/78 mm Hg, pulse rate was 82 beats per minute, and respiratory rate was 20 breaths
per minute. Oxygen saturation was 97% in room air. She had a regular heart rate with a
mild systolic murmur; her jugular venous pressure was normal; and lung auscultation
revealed reduced air entry at the left base. She had no leg swelling and no pain on calf
palpation. Laboratory testing results are reported in Table 1. The attending physician
raised the diagnosis of a pulmonary embolism (PE) among the differentials. The clinical
probability of PE was unlikely (Wells score).
Table 1. Laboratory Values for Diagnosis of Pulmonary Embolism
Laboratory Test
Patients Values
Reference Range
Hemoglobin, g/dL
12.0
14.0-17.5
White blood cell count, 103/L
7.4
4.5-11.0
Platelet count, 103/L
359
150-350
Serum creatinine, mg/dL
1.26
0.6-1.2
D-dimer, ng/mL
680
<500
HOW DO YOU INTERPRET THESE TEST
RESULTS?
A. D-dimer test result is positive.
Imaging test is required.
B. D-dimer test result is positive. The
diagnosis of PE is confirmed.
C. D-dimer test result is positive but
below her age-adjusted cutoff. PE
is ruled out.
D. D-dimer test result is positive
due to active malignancy. PE is
ruled out.
SI conversion factors: for serum creatinine (mg/dL to mol/L), multiply by 88.4.
Answer
C. D-dimer test result is positive but below the patients ageadjusted cutoff. PE is ruled out.
Test Characteristics
D-dimers result from the fibrinolysis of acute thrombi. Enzymelinked immunosorbent assay (ELISA) and immunoturbidimetric
D-dimer assays are highly sensitive for the diagnosis of PE.
The D-dimer test should be
used in combination with a
pretest clinical probability
Quiz at jama.com
assessment (Table 2). The
D-dimer is useful only in patients with a low-intermediate or
unlikely pretest clinical probability of PE, as assessed by a
validated clinical decision rule.1,2 It should not be used in patients
with a high/likely pretest clinical probability. Systematic reviews
report a sensitivity of greater than 95% and negative likelihood
ratios of 0.10 for ELISA or immuneturbidimetric assays, with a
specificity of 40% and a positive likelihood ratio of 1.64.3 Using
a cutoff value of 500 ng/mL, a negative D-dimer assay safely
rules out the diagnosis of PE in patients with a low-intermediate
or unlikely clinical probability. This was demonstrated in several
outcome studies in which patients with a low-intermediate or
unlikely pretest probability and a negative D-dimer test result
were left untreated and followed up for 3 months (ie, the3-month
risk of venous thromboembolism was 0.14% [95% CI,
1668
0.05%-0.41%], lower than the risk observed after a negative pulmonary angiography).4
Conversely, because D-dimers increase in many other clinical
situations (eg, infection, inflammation, malignancy, postsurgical
status, pregnancy), the specificity of the test is low (approximately 50%) and as a result, a positive D-dimer test is not diagnostic for PE.
The Medicare midpoint reimbursement is $18.77 for a quantitative D-dimer test.5
Application of Test Results to This Patient
The D-dimer test result for this patient was 68 ng/mL. This
result indicates a positive D-dimer test as per most commercial
assays (conventional cutoff value 500 ng/mL). Given the low
specificity of the test, a high D-dimer level never rules in the diagnosis of PE. Patients with positive D-dimer results should undergo
an imaging test, such as a computed tomography pulmonary
angiography (CTPA) or a ventilation-perfusion lung scan.6 However, D-dimer levels increase with age, and as a result, the proportion of patients in whom the diagnosis may be ruled out on the
basis of a negative D-dimer test decreases with ageonly 5% of
patients older than 80 years have a negative D-dimer, as compared with more than 50% of patients aged 40 years or
younger. 7 An age-adjusted D-dimer cutoff value was recently
derived and validated in several retrospective analyses and one
prospective management outcome study.8,9 D-dimer results are
JAMA April 28, 2015 Volume 313, Number 16 (Reprinted)
Copyright 2015 American Medical Association. All rights reserved.
Downloaded From: http://jama.jamanetwork.com/ by a Carleton University User on 05/12/2015
jama.com
JAMA Diagnostic Test Interpretation Clinical Review & Education
What Are Alternative Diagnostic Testing Approaches?
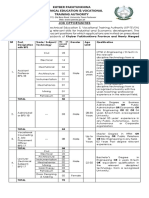
Table 2. The Wells Score for Pulmonary Embolisma
Clinical Variable
Points
Clinical signs of DVT
3.0
Recent surgery or immobilization (<1 mo)
1.5
Heart rate >100/min
1.5
Previous history of PE or DVT
1.5
Hemoptysis
1.0
Malignancy
1.0
An alternative diagnosis is less likely than PE
Pretest Probability Assessment
3.0
Score
PE Prevalence,
% (95% CI)b
3 Categories
Low
<2
Intermediate
6 (4-8)
2-6
High
>6
23 (18-28)
49 (42-56)
2 Categories
Unlikely
8 (6-11)
Likely
>4
34 (29-40)
Abbreviations: DVT, deep venous thrombosis; PE, pulmonary embolism.
a
Data are from Wells et al.2
Data are from Ceriani et al.10
typically reported without providing the age-adjusted upper limit
of normal. However, the age-adjusted cutoff value is easy to compute: in patients aged 50 years or more, a D-dimer level belowthe
product of their age multiplied by 10 (eg, 820 ng/mL in this
82-year-old patient) appears to safely rule out PE without any
imaging test.
ARTICLE INFORMATION
Author Affiliations: Thrombosis Program,
University of Ottawa, Ottawa, Ontario, Canada
(Le Gal, Wells); Division of Hematology, University
of Ottawa, Ottawa, Ontario, Canada (Le Gal, Wells);
Department of Medicine, University of Ottawa,
Ottawa, Ontario, Canada (Le Gal, Wells); Clinical
Epidemiology Unit, Ottawa Health Research
Institute, Ottawa, Ontario, Canada (Le Gal, Wells);
The Ottawa Hospital, Ottawa, Ontario, Canada
(Le Gal, Wells); Division of Angiology and
Hemostasis, Geneva University Hospital, Geneva,
Switzerland (Righini).
Corresponding Author: Philip S. Wells, MD, MSc,
The Ottawa Hospital, General Campus, 501 Smyth
Rd, PO Box 206, Ottawa, Ontario K1H 8L6, Canada
(pwells@toh.on.ca).
Section Editor: Mary McGrae McDermott, MD,
Senior Editor.
Conflict of Interest Disclosures: All authors have
completed and submitted the ICMJE Form for
Disclosure of Potential Conflicts of Interest. Dr
Wells reports receipt of personal fees for serving as
a speaker for Bayer Healthcare, Boehringer
Ingelheim, Biomerieux, and BMS/Pfizer, all of which
were outside the submitted work. and none were
reported. Drs Le Gal and Righini report no
disclosures.
In some centers, most patients with suspected PE are directly referred for a CTPA without prior use of pretest probability assessment and D-dimer. The combination of a D-dimer test with a clinical probability assessment allows ruling out PE without undergoing
an imaging test in approximately one-third of outpatients.4 The cost
effectiveness of this approach has been demonstrated.7 Moreover,
there is an increasing concern about the risk of cancer in patients
exposed to radiation from medical imaging.10 The D-dimer test represents a safe and reliable option to avoid the use of CTPA in an important proportion of patients with clinically suspected PE.
Patient Outcome
A chest x-ray film revealed a left inferior lobar consolidation. The patient was treated with antibiotics, discharged home on the same day,
and asked to follow up with her general practitioner. She had a good
and uneventful recovery.
Clinical Bottom Line
In combination with a validated clinical decision rule, a negative
D-dimer assay allows the physician to safely rule out the diagnosis of PE in approximately one-third of outpatients.
A positive D-dimer is not diagnostic for PE. Patients with clinically
suspected PE and positive D-dimer should undergo imaging tests
for PE.
According to recent studies, PE might be ruled out in patients with
a low-intermediate or unlikely pretest probability and D-dimer level
that is less than their age-adjusted cutoff (ie, patients age 10 in
patients aged 50 years or older).
REFERENCES
6. Anderson DR, Kahn SR, Rodger MA, et al.
Computed tomographic pulmonary angiography vs
ventilation-perfusion lung scanning in patients with
suspected pulmonary embolism: a randomized
controlled trial. JAMA. 2007;298(23):2743-2753.
1. Le Gal G, Righini M, Roy P-M, et al. Prediction of
pulmonary embolism in the emergency
department: the revised Geneva score. Ann Intern
Med. 2006;144(3):165-171.
7. Righini M, Nendaz M, Le Gal G, Bounameaux H,
Perrier A. Influence of age on the cost-effectiveness
of diagnostic strategies for suspected pulmonary
embolism. J Thromb Haemost. 2007;5(9):1869-1877.
2. Wells PS, Anderson DR, Rodger M, et al.
Derivation of a simple clinical model to categorize
patients probability of pulmonary embolism:
increasing the models utility with the SimpliRED
D-dimer. Thromb Haemost. 2000;83(3):416-420.
8. Andro M, Righini M, Le Gal G. Adapting the
D-dimer cutoff for thrombosis detection in elderly
outpatients. Expert Rev Cardiovasc Ther. 2013;11(6):
751-759.
Additional Contribution: We thank the patient for
sharing her experience and for granting permission
to publish it.
3. Di Nisio M, Squizzato A, Rutjes AW, Bller HR,
Zwinderman AH, Bossuyt PM. Diagnostic accuracy
of D-dimer test for exclusion of venous
thromboembolism: a systematic review. J Thromb
Haemost. 2007;5(2):296-304.
4. Carrier M, Righini M, Djurabi RK, et al. VIDAS
D-dimer in combination with clinical pre-test
probability to rule out pulmonary embolism:
a systematic review of management outcome
studies. Thromb Haemost. 2009;101(5):886-892.
9. Righini M, Van Es J, Den Exter PL, et al.
Age-adjusted D-dimer cutoff levels to rule out
pulmonary embolism: the ADJUST-PE study. JAMA.
2014;311(11):1117-1124.
10. Ceriani E, Combescure C, Le Gal G, et al. Clinical
prediction rules for pulmonary embolism:
a systematic review and meta-analysis. J Thromb
Haemost. 2010;8(5):957-970.
5. Centers for Medicare & Medicaid Services.
Clinical Laboratory Fee Schedule. http://www
.cms.gov/Medicare/Medicare-Fee-for-Service
-Payment/ClinicalLabFeeSched/index.html. Accessed
June 27, 2014.
jama.com
(Reprinted) JAMA April 28, 2015 Volume 313, Number 16
Copyright 2015 American Medical Association. All rights reserved.
Downloaded From: http://jama.jamanetwork.com/ by a Carleton University User on 05/12/2015
1669
Das könnte Ihnen auch gefallen
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Elements of ArtDokument1 SeiteElements of Artsamson8cindy8louNoch keine Bewertungen
- Mcdonald 2016Dokument10 SeitenMcdonald 2016Andrika SaputraNoch keine Bewertungen
- 1.technical Specifications (Piling)Dokument15 Seiten1.technical Specifications (Piling)Kunal Panchal100% (2)
- Turn Around Coordinator Job DescriptionDokument2 SeitenTurn Around Coordinator Job DescriptionMikeNoch keine Bewertungen
- Hey Friends B TBDokument152 SeitenHey Friends B TBTizianoCiro CarrizoNoch keine Bewertungen
- Role of Losses in Design of DC Cable For Solar PV ApplicationsDokument5 SeitenRole of Losses in Design of DC Cable For Solar PV ApplicationsMaulidia HidayahNoch keine Bewertungen
- Maternal Sepsis and Sepsis ShockDokument17 SeitenMaternal Sepsis and Sepsis ShockAlvaro Andres Flores JimenezNoch keine Bewertungen
- Mcom Sem 4 Project FinalDokument70 SeitenMcom Sem 4 Project Finallaxmi iyer75% (4)
- Lactate-Guided Resuscitation Saves Lives: We Are Not Sure: EditorialDokument3 SeitenLactate-Guided Resuscitation Saves Lives: We Are Not Sure: EditorialAlvaro Andres Flores JimenezNoch keine Bewertungen
- 10 1378@chest 09-2690Dokument9 Seiten10 1378@chest 09-2690Alvaro Andres Flores JimenezNoch keine Bewertungen
- Bishnoi2020 Article EvaluationOfFactorsDeterminingDokument6 SeitenBishnoi2020 Article EvaluationOfFactorsDeterminingAlvaro Andres Flores JimenezNoch keine Bewertungen
- Tribute ofDokument10 SeitenTribute ofAlvaro Andres Flores JimenezNoch keine Bewertungen
- Bupropion 2011 Efectos CardiovascularesDokument10 SeitenBupropion 2011 Efectos CardiovascularesAlvaro Andres Flores JimenezNoch keine Bewertungen
- Case 3-2020: A 44-Year-Old Man With Weight Loss, Diarrhea, and Abdominal PainDokument10 SeitenCase 3-2020: A 44-Year-Old Man With Weight Loss, Diarrhea, and Abdominal PainAlvaro Andres Flores JimenezNoch keine Bewertungen
- Pharmacokinetics of Bupropion and Its Metabolites in Haemodialysis Patients Who SmokeDokument8 SeitenPharmacokinetics of Bupropion and Its Metabolites in Haemodialysis Patients Who SmokeAlvaro Andres Flores JimenezNoch keine Bewertungen
- FeverDokument5 SeitenFeverAlvaro Andres Flores JimenezNoch keine Bewertungen
- 2013 34 438 Rani S. Gereige and Pablo Marcelo Laufer: Pediatrics in ReviewDokument21 Seiten2013 34 438 Rani S. Gereige and Pablo Marcelo Laufer: Pediatrics in ReviewAlvaro Andres Flores JimenezNoch keine Bewertungen
- DengueDokument10 SeitenDengueAlvaro Andres Flores JimenezNoch keine Bewertungen
- DeshidratacionDokument14 SeitenDeshidratacionAlvaro Andres Flores JimenezNoch keine Bewertungen
- KP Tevta Advertisement 16-09-2019Dokument4 SeitenKP Tevta Advertisement 16-09-2019Ishaq AminNoch keine Bewertungen
- Global Geo Reviewer MidtermDokument29 SeitenGlobal Geo Reviewer Midtermbusinesslangto5Noch keine Bewertungen
- Mastertop 1230 Plus PDFDokument3 SeitenMastertop 1230 Plus PDFFrancois-Noch keine Bewertungen
- Application of Graph Theory in Operations ResearchDokument3 SeitenApplication of Graph Theory in Operations ResearchInternational Journal of Innovative Science and Research Technology100% (2)
- All You Need To Know About Egg YolkDokument7 SeitenAll You Need To Know About Egg YolkGolden Era BookwormNoch keine Bewertungen
- AntibioticsDokument36 SeitenAntibioticsBen Paolo Cecilia RabaraNoch keine Bewertungen
- Lithuania DalinaDokument16 SeitenLithuania DalinaStunt BackNoch keine Bewertungen
- Residual Power Series Method For Obstacle Boundary Value ProblemsDokument5 SeitenResidual Power Series Method For Obstacle Boundary Value ProblemsSayiqa JabeenNoch keine Bewertungen
- Corrosion Fatigue Phenomena Learned From Failure AnalysisDokument10 SeitenCorrosion Fatigue Phenomena Learned From Failure AnalysisDavid Jose Velandia MunozNoch keine Bewertungen
- Technical Specification For 33KV VCB BoardDokument7 SeitenTechnical Specification For 33KV VCB BoardDipankar ChatterjeeNoch keine Bewertungen
- Biological Beneficiation of Kaolin: A Review On Iron RemovalDokument8 SeitenBiological Beneficiation of Kaolin: A Review On Iron RemovalValentin GnoumouNoch keine Bewertungen
- De Thi Hoc Ki 1 Mon Tieng Anh Lop 5 Co File NgheDokument10 SeitenDe Thi Hoc Ki 1 Mon Tieng Anh Lop 5 Co File Nghetuyen truongNoch keine Bewertungen
- Borang Ambulans CallDokument2 SeitenBorang Ambulans Callleo89azman100% (1)
- Decision Making and The Role of Manageme PDFDokument20 SeitenDecision Making and The Role of Manageme PDFRaadmaan RadNoch keine Bewertungen
- Impact of Advertising On Consumers' Buying Behavior Through Persuasiveness, Brand Image, and Celebrity EndorsementDokument10 SeitenImpact of Advertising On Consumers' Buying Behavior Through Persuasiveness, Brand Image, and Celebrity Endorsementvikram singhNoch keine Bewertungen
- RSA - Brand - Guidelines - 2019 2Dokument79 SeitenRSA - Brand - Guidelines - 2019 2Gigi's DelightNoch keine Bewertungen
- Regions of Alaska PresentationDokument15 SeitenRegions of Alaska Presentationapi-260890532Noch keine Bewertungen
- Comparitive Study ICICI & HDFCDokument22 SeitenComparitive Study ICICI & HDFCshah faisal100% (1)
- Deal Report Feb 14 - Apr 14Dokument26 SeitenDeal Report Feb 14 - Apr 14BonviNoch keine Bewertungen
- Sam Media Recruitment QuestionnaireDokument17 SeitenSam Media Recruitment Questionnairechek taiNoch keine Bewertungen
- Tribal Banditry in Ottoman Ayntab (1690-1730)Dokument191 SeitenTribal Banditry in Ottoman Ayntab (1690-1730)Mahir DemirNoch keine Bewertungen
- B122 - Tma03Dokument7 SeitenB122 - Tma03Martin SantambrogioNoch keine Bewertungen
- g6 - AFA - Q1 - Module 6 - Week 6 FOR TEACHERDokument23 Seiteng6 - AFA - Q1 - Module 6 - Week 6 FOR TEACHERPrincess Nicole LugtuNoch keine Bewertungen