Beruflich Dokumente
Kultur Dokumente
Neurofibromatoza
Hochgeladen von
Maria Magdalena DumitruOriginalbeschreibung:
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Neurofibromatoza
Hochgeladen von
Maria Magdalena DumitruCopyright:
Verfügbare Formate
Answer
Neurofibromatosis: Neurofibromatosis (NF) is an autosomal dominant disorder
with numerous presentations affecting nearly every organ system. The 2 major
subtypes are NF type 1 (NF1), also known as peripheral NF, and NF type 2
(NF2), referred to as central NF. However, these terms are not completely correct
because NF1 may cause central characteristics.
About 50% of cases of NF are familial, and the other 50% are due to
spontaneous gene mutation. NF1, also known as von Recklinghausen disease, is
a common genetic disorder involving a gene mutation on chromosome 17 that
affects 1 in every 3000-4000 births (Children's Tumor Foundation, 2006). This
disorder affects all races and both sexes equally (Neurofibromatosis, Inc, 2006).
The diagnosis of NF1 requires that the patient present with 2 or more of the
following conditions: 6 or more caf au lait spots (irregularly shaped, evenly
pigmented, brown macules), 2 or more neurofibromas, axillary or inguinal
freckling, Lisch nodules on the iris, optic glioma, various types of osseous
lesions, or a first-degree relative with the condition.
Symptomatic NF1 typically manifests as flesh-colored, benign skin tumors that
appear late in childhood. The patient may have as few as 3 or as many as
thousands of these benign lesions, which consist of Schwann cells, neural
fibroblasts, mast cells, and vascular elements. Neurofibromas may occur
anywhere in the body and potentially lead to marked disfigurement. Lesions
along visual, auditory, or CNS nerve pathways may result in blindness, deafness,
or neurologic deficits. Other findings associated with this condition include
skeletal anomalies, such as fibrous dysplasia, subperiosteal bone cysts, or
vertebral scalloping (Neurofibromatosis, Inc, 2006).
NF2 is a progressive genetic disorder affecting 1 in every 33,000-40,000 births
(Neurofibromatosis, Inc, 2006). Patients with NF2, which results from an
abnormality of chromosome 22, typically present with acoustic neuromas or
vestibular schwannomas. Clinical manifestations include tinnitus, balance
disorders, and progressive hearing loss. Affected patients may also have
meningiomas and juvenile cataracts. The diagnosis is based on a history of the
condition in a first-degree relative and on any 2 of the conditions listed above for
NF1 (Neurofibromatosis, Inc, 2006).
For both NF1 and NF2, the diagnosis is primarily based on physical findings and
a positive family history. Diagnostic tests that may be useful include radiographic
studies, such as CT of the brain, genetic analysis, and psychological or
developmental assessment.
No cure exists for this condition. Recommendations for follow-up include referral
to support groups, psychological counseling, evaluation of learning disorders,
surgical excision of lesions, and regular monitoring by a primary care provider for
any changes that may occur, as patients with NF1 are at somewhat increased
risk of malignancy. Annual ocular examinations are recommended. Genetic
testing is also advocated in patients with NF who wish to have children. Surgery
has been a successful treatment for the lesions themselves; however, recurrence
often occurs, and nerve damage is a risk when tumors are located along neural
pathways (National Institute of Neurologic Disorders and Stroke, 2006).
For more information on neurofibromatosis, see the eMedicine articles
Neurofibromatosis (within the Dermatology specialty), Neurofibromatosis, Type 1
and Neurofibromatosis, Type 2 (within the Neurology specialty), and
Neurofibromatosis Type 1 and Neurofibromatosis Type 2 (within the Radiology
specialty). For other resources and access to support networks, contact the Web
pages of Children's Tumor Foundation and Neurofibromatosis, Inc.
References
Children's Tumor Foundation: Diagnosis of NF1. Available at:
http://www.ctf.org/aboutnf/nf1/diagnosisnf1.htm. Accessed July 29, 2006.
Children's Tumor Foundation: Diagnosis of NF2. Available at:
http://www.ctf.org/aboutnf/nf2/diagnosisnf2.htm. Accessed July 29, 2006.
Neurofibromatosis, Inc: What is NF? Available at:
http://www.nfinc.org/what.shtml. Accessed July 29, 2006.
NINDS: National Institute of Neurologic Disorders and Stroke.
Neurofibromatosis Fact Sheet. Available at:
http://www.ninds.nih.gov/disorders/neurofibromatosis/
detail_neurofibromatosis.htm#57453162. Accessed July 29, 2006.
BACKGROUND
A 32-year-old woman presents to the emergency department with several fleshcolored papules on her face, trunk, and upper extremities. She noticed the
lesions at approximately 10 years of age. However, over the past 5 years, the
lesions have increased in number and become uncomfortable. She primarily
complains of irritation from the lesions along her bra line. She previously
underwent excision of other similar skin lesions 5 years ago, but these have
since recurred. She denies having discharge, pain, trauma, contact with
individuals with atypical skin lesions or rashes, travel out of the country, unusual
exposure to animals, or a history of sexually transmitted disease.
The patient's medical and surgical history includes environmental allergies,
frequent episodes of bronchitis, and the aforementioned excisions. She takes
cetirizine HCl (Zyrtec) and fluticasone propionate (Flonase) for allergies and has
no known drug allergies. Her family history is significant for coronary artery
disease, hypertension, diabetes mellitus, and glaucoma. She does not smoke
and drinks alcohol on occasion. The review of systems is otherwise
noncontributory.
Physical examination reveals dozens of fleshy nodules of 0.5-2.0 cm throughout
her trunk, face, and upper extremities. The nodules are nontender to palpation
and nonerythematous, and they produce no discharge, crusting, or scaling.
Several 1.5- to 3-cm, tan, oval macules and patches with well-defined borders
are located on her trunk and upper extremities (see Images). Her vital signs are
within normal limits, and the rest of the physical findings are unremarkable.
What is the diagnosis?
Hint
Tan macules or patches, known as "caf au lait" spots, are characteristic of this
genetic disorder.
Author:
Alyssa D. Abbey, BA, PA-S,
Physician Assistant Student,
Barry University-Miami Shores,
Fla
Martin I. Newman, MD,
Department of Plastic and
Reconstructive Surgery,
Cleveland Clinic Florida, Weston
eMedicine
Editor:
Erik D. Schraga, MD,
Staff Physician,
Kaiser Permanente,
Santa Clara Medical Center, Calif
Das könnte Ihnen auch gefallen
- Neurofibromatosis Type 1: Ontinuing Medical EducationDokument14 SeitenNeurofibromatosis Type 1: Ontinuing Medical EducationMatthew DavisNoch keine Bewertungen
- Neurofibromatosis 1, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsVon EverandNeurofibromatosis 1, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNoch keine Bewertungen
- Neurofibromatosis 1: Diagnosis and ManagementDokument6 SeitenNeurofibromatosis 1: Diagnosis and ManagementCYNTHIA MARLEN HORTA SANCHEZNoch keine Bewertungen
- Neurofibromatosis Type 1 Genetic Testing: MOL - TS.301.ADokument9 SeitenNeurofibromatosis Type 1 Genetic Testing: MOL - TS.301.ASarah QonitahNoch keine Bewertungen
- Review: Pathophysiology of Neurofibromatosis Type 1Dokument9 SeitenReview: Pathophysiology of Neurofibromatosis Type 1monster1225Noch keine Bewertungen
- 81 MantapDokument8 Seiten81 MantapadeNoch keine Bewertungen
- NeurofibromatosisDokument9 SeitenNeurofibromatosisDenny EmiliusNoch keine Bewertungen
- Neurofibromatosis (Von Reklinghausen Disease)Dokument4 SeitenNeurofibromatosis (Von Reklinghausen Disease)kenBusbyNoch keine Bewertungen
- Neurofibromatosis 1: Practical GeneticsDokument8 SeitenNeurofibromatosis 1: Practical GeneticsEccoNoch keine Bewertungen
- Understanding Neurofibromatosis: 3rd EditionDokument14 SeitenUnderstanding Neurofibromatosis: 3rd EditionSucipto HartonoNoch keine Bewertungen
- Diagnostic Review of Neurofibromatosis Type 1: Pathology Case Reviews January 2014Dokument10 SeitenDiagnostic Review of Neurofibromatosis Type 1: Pathology Case Reviews January 2014Xavier PeñaloNoch keine Bewertungen
- Honors Term Paper Neurofibromatosis Type 1 FinalDokument10 SeitenHonors Term Paper Neurofibromatosis Type 1 Finalapi-726936832Noch keine Bewertungen
- Sites You Should See: Did You Know?: By: Stephanie HuDokument3 SeitenSites You Should See: Did You Know?: By: Stephanie HuStephanie HuNoch keine Bewertungen
- Neuro FibromaDokument18 SeitenNeuro FibromaVerli Fajriati NofliNoch keine Bewertungen
- NF 1Dokument5 SeitenNF 1budi rahmawatiNoch keine Bewertungen
- Neurofibromatosis Type 1 Review and Update On.10Dokument11 SeitenNeurofibromatosis Type 1 Review and Update On.10claudio RivasNoch keine Bewertungen
- (03241750 - Acta Medica Bulgarica) Neurofibromatosis Type I (Von Recklinghausen Disease) - A Case Report and Review of The LiteratureDokument4 Seiten(03241750 - Acta Medica Bulgarica) Neurofibromatosis Type I (Von Recklinghausen Disease) - A Case Report and Review of The LiteratureTeodorNoch keine Bewertungen
- About Neurofibromatosis: Neurocutaneous SyndromeDokument4 SeitenAbout Neurofibromatosis: Neurocutaneous SyndromeLili SurianiNoch keine Bewertungen
- Neurofibromatosis-1: CausesDokument4 SeitenNeurofibromatosis-1: CausesKapten Inf Dwi CahyoNoch keine Bewertungen
- Syndromic and Sporadic Pediatric Optic Pathway Gliomas: Review of Clinical and Histopathological Differences and Treatment ImplicationsDokument9 SeitenSyndromic and Sporadic Pediatric Optic Pathway Gliomas: Review of Clinical and Histopathological Differences and Treatment ImplicationsMarco DoradoNoch keine Bewertungen
- 2008 121 633 Joseph H. Hersh and Committee On Genetics: Health Supervision For Children With NeurofibromatosisDokument12 Seiten2008 121 633 Joseph H. Hersh and Committee On Genetics: Health Supervision For Children With NeurofibromatosisMatthew DavisNoch keine Bewertungen
- Sordera SindromicaDokument8 SeitenSordera SindromicaFabian Camelo OtorrinoNoch keine Bewertungen
- NF 2Dokument22 SeitenNF 2Rocio LedesmaNoch keine Bewertungen
- Neurofibromatosis BrochureDokument2 SeitenNeurofibromatosis Brochureapi-251731184Noch keine Bewertungen
- Neurofibromatosis Report CutieDokument8 SeitenNeurofibromatosis Report Cutieaeronh john PurificandoNoch keine Bewertungen
- Orbital Peripheral Nerve SheathDokument15 SeitenOrbital Peripheral Nerve SheathChavdarNoch keine Bewertungen
- Neurofibromatosis Type 1 in Multiple Sclerosis in Saudi Arabia: Case Report and Literature ReviewDokument6 SeitenNeurofibromatosis Type 1 in Multiple Sclerosis in Saudi Arabia: Case Report and Literature ReviewIJAR JOURNALNoch keine Bewertungen
- Ojoph 2022111815222395Dokument12 SeitenOjoph 2022111815222395budi rahmawatiNoch keine Bewertungen
- CEP Neurofibromatosis Type I: Points To Be Considered by General PediatriciansDokument8 SeitenCEP Neurofibromatosis Type I: Points To Be Considered by General PediatriciansElison J PanggaloNoch keine Bewertungen
- NeurofibromatosisDokument13 SeitenNeurofibromatosisNadya Kemala AmiraNoch keine Bewertungen
- Neurofibromatosis 1Dokument10 SeitenNeurofibromatosis 1Minelle Sanchez InsoNoch keine Bewertungen
- A Prospective 10 Year Follow Up Study of Patients With Neurofibromatosis Type 1Dokument5 SeitenA Prospective 10 Year Follow Up Study of Patients With Neurofibromatosis Type 1YesicaNoch keine Bewertungen
- Neurofibromatosis Type 1: Ontinuing Medical EducationDokument14 SeitenNeurofibromatosis Type 1: Ontinuing Medical EducationDeysi Blanco CohuoNoch keine Bewertungen
- Neurofibromatosis - Pediatrics - MSD Manual Professional EditionDokument8 SeitenNeurofibromatosis - Pediatrics - MSD Manual Professional Editioncynthiadamayanti_drNoch keine Bewertungen
- Genetics Evaluation of Persons/families With Hearing Loss, Genetic Screening Genetics of Hearing Impairment Gene Database For Hearing LossDokument12 SeitenGenetics Evaluation of Persons/families With Hearing Loss, Genetic Screening Genetics of Hearing Impairment Gene Database For Hearing LosssherinNoch keine Bewertungen
- Clinical and Genetic Basis of Familial Amyotrophic Lateral Sclerosis (Revisión)Dokument12 SeitenClinical and Genetic Basis of Familial Amyotrophic Lateral Sclerosis (Revisión)Francisco Ahumada MéndezNoch keine Bewertungen
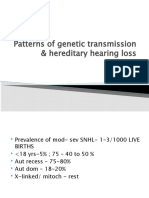
- Patterns of Genetic Transmission & Hereditary Hearing Loss: DR - DivyaDokument60 SeitenPatterns of Genetic Transmission & Hereditary Hearing Loss: DR - DivyavipinNoch keine Bewertungen
- GENBIODokument3 SeitenGENBIOCyra BantilloNoch keine Bewertungen
- From Rare Diseases, Genetic Disorders To Orphan DrugsDokument192 SeitenFrom Rare Diseases, Genetic Disorders To Orphan DrugsShing Ming TangNoch keine Bewertungen
- American Academy of Neurology Key PointsDokument193 SeitenAmerican Academy of Neurology Key Pointszayat13Noch keine Bewertungen
- An Update On Neurofibromatosis Type 1: Not Just Café-au-Lait Spots, Freckling, and Neurofibromas. An Update. Part I. Dermatological Clinical Criteria Diagnostic of The DiseaseDokument11 SeitenAn Update On Neurofibromatosis Type 1: Not Just Café-au-Lait Spots, Freckling, and Neurofibromas. An Update. Part I. Dermatological Clinical Criteria Diagnostic of The Diseasezulfan tmNoch keine Bewertungen
- Enfermedades NeurológicasDokument24 SeitenEnfermedades NeurológicasSritaIves AguilarNoch keine Bewertungen
- Case Report: Vertigo As A Predominant Manifestation of NeurosarcoidosisDokument5 SeitenCase Report: Vertigo As A Predominant Manifestation of NeurosarcoidosisDjumadi AkbarNoch keine Bewertungen
- TextDokument2 SeitenTextAknur JakhanshaNoch keine Bewertungen
- VEM5384 Clincial Neurology DisordersDokument62 SeitenVEM5384 Clincial Neurology DisordersdeadnarwhalNoch keine Bewertungen
- Care GuidelinesDokument12 SeitenCare GuidelinesGloryNoch keine Bewertungen
- Initial Evaluation VertigoDokument8 SeitenInitial Evaluation VertigoTanri Hadinata WiranegaraNoch keine Bewertungen
- P71 NEJM DeliriumDokument10 SeitenP71 NEJM DeliriumGabriel CampolinaNoch keine Bewertungen
- Neurofibromatosis Etiology, Commonly Encountered Spinal Deformities and Surgical TreatmentDokument10 SeitenNeurofibromatosis Etiology, Commonly Encountered Spinal Deformities and Surgical TreatmentChristoforos KampouridisNoch keine Bewertungen
- 662 FullDokument13 Seiten662 FullPaviliuc RalucaNoch keine Bewertungen
- 2008 - Neurofibromatoses - KaufmnanDokument203 Seiten2008 - Neurofibromatoses - KaufmnanPablo Antonio Antonio100% (1)
- Neurofibromatosis Tipo 1 y Gliomas de Vías Ópticas. Una Serie de 80 PacientesDokument7 SeitenNeurofibromatosis Tipo 1 y Gliomas de Vías Ópticas. Una Serie de 80 PacientesHanderson RamirezNoch keine Bewertungen
- Neurofibromatosis Involving The Fibula in An Adult Patient: Case ReportDokument3 SeitenNeurofibromatosis Involving The Fibula in An Adult Patient: Case ReporthardiNoch keine Bewertungen
- Neurosyphilis: The Reemergence of An Historical DiseaseDokument2 SeitenNeurosyphilis: The Reemergence of An Historical DiseaseDrashua AshuaNoch keine Bewertungen
- Ocular Features of Marfan Syndrome: Gordana Stanković-Babić, Milena Vujanović, Jasmina Đorđević-Jocić, Sonja CekićDokument4 SeitenOcular Features of Marfan Syndrome: Gordana Stanković-Babić, Milena Vujanović, Jasmina Đorđević-Jocić, Sonja CekićmongiiiNoch keine Bewertungen
- Prion Disease: Kelly J. Baldwin, MD Cynthia M. Correll, MDDokument12 SeitenPrion Disease: Kelly J. Baldwin, MD Cynthia M. Correll, MDMerari Lugo Ocaña100% (1)
- Neurooncology of Familial Cancer SyndromesDokument10 SeitenNeurooncology of Familial Cancer SyndromesMădălina SimionNoch keine Bewertungen
- Congenital Muscular Dystrophies and Congenital.8 PDFDokument26 SeitenCongenital Muscular Dystrophies and Congenital.8 PDFlithium2203Noch keine Bewertungen
- Disruptions Result From Destruction of A NorDokument6 SeitenDisruptions Result From Destruction of A NorAsri RachmawatiNoch keine Bewertungen
- ECP KIT - Keep in TouchDokument2 SeitenECP KIT - Keep in TouchMaria Magdalena DumitruNoch keine Bewertungen
- Ecnp 2016Dokument3 SeitenEcnp 2016Maria Magdalena DumitruNoch keine Bewertungen
- Plan de Management 2015Dokument14 SeitenPlan de Management 2015Maria Magdalena Dumitru0% (1)
- 4288 8405 1 SMDokument20 Seiten4288 8405 1 SMMaria Magdalena DumitruNoch keine Bewertungen
- Dement ADokument1 SeiteDement AMaria Magdalena DumitruNoch keine Bewertungen
- StahlDokument1 SeiteStahlMaria Magdalena Dumitru100% (1)
- When Death Is Sought - Assisted Suicide and Euthanasia in The Medical ContextDokument5 SeitenWhen Death Is Sought - Assisted Suicide and Euthanasia in The Medical ContextMaria Magdalena DumitruNoch keine Bewertungen
- Physician Brochure 2003 FinalDokument12 SeitenPhysician Brochure 2003 FinalMaria Magdalena DumitruNoch keine Bewertungen
- Extra Tables Statistics Explained 01092015Dokument6 SeitenExtra Tables Statistics Explained 01092015Maria Magdalena DumitruNoch keine Bewertungen
- Isometsa - Psychological Autopsy Studies - Eur Psychiatry 2001Dokument7 SeitenIsometsa - Psychological Autopsy Studies - Eur Psychiatry 2001Maria Magdalena DumitruNoch keine Bewertungen
- Suicide in The Elderly Learning NotesDokument1 SeiteSuicide in The Elderly Learning NotesMaria Magdalena DumitruNoch keine Bewertungen
- BooksDokument1 SeiteBooksMaria Magdalena DumitruNoch keine Bewertungen
- Exercise Guide Dumbells Hantlar - EngDokument1 SeiteExercise Guide Dumbells Hantlar - EngMaria Magdalena DumitruNoch keine Bewertungen
- Global Burden Disease Death Estimates Sex 2008Dokument8 SeitenGlobal Burden Disease Death Estimates Sex 2008Maria Magdalena DumitruNoch keine Bewertungen
- Suicide in The CF 1995 2012Dokument21 SeitenSuicide in The CF 1995 2012Maria Magdalena DumitruNoch keine Bewertungen
- bjpg55 883aDokument1 Seitebjpg55 883aMaria Magdalena DumitruNoch keine Bewertungen
- Prev Youth Jeunes EngDokument179 SeitenPrev Youth Jeunes EngMaria Magdalena DumitruNoch keine Bewertungen
- Exercise Guide Stretch - EngDokument1 SeiteExercise Guide Stretch - EngMaria Magdalena DumitruNoch keine Bewertungen
- Final Version As LodgedDokument21 SeitenFinal Version As LodgedMaria Magdalena DumitruNoch keine Bewertungen
- Martin Barkin: What Makes Run?Dokument1 SeiteMartin Barkin: What Makes Run?Maria Magdalena DumitruNoch keine Bewertungen
- 508 Suicide Prevention Paper FinalDokument46 Seiten508 Suicide Prevention Paper FinalMaria Magdalena DumitruNoch keine Bewertungen
- Epidemiol Rev 2008 Nock 133 54Dokument22 SeitenEpidemiol Rev 2008 Nock 133 54Maria Magdalena DumitruNoch keine Bewertungen
- Bereaved by SuicideDokument2 SeitenBereaved by SuicideMaria Magdalena DumitruNoch keine Bewertungen
- 4754666Dokument7 Seiten4754666Maria Magdalena DumitruNoch keine Bewertungen
- Publicatii 2012Dokument6 SeitenPublicatii 2012Maria Magdalena DumitruNoch keine Bewertungen
- Assessement and Management of Violence Risk in Forensic PsychiatryDokument6 SeitenAssessement and Management of Violence Risk in Forensic PsychiatryMaria Magdalena DumitruNoch keine Bewertungen
- BookDokument157 SeitenBookMaria Magdalena DumitruNoch keine Bewertungen
- Publicatii 2011Dokument3 SeitenPublicatii 2011Maria Magdalena DumitruNoch keine Bewertungen
- Publicatii 2011Dokument3 SeitenPublicatii 2011Maria Magdalena DumitruNoch keine Bewertungen
- Health Optimizing Physical Education 1Dokument22 SeitenHealth Optimizing Physical Education 1Russel MejicoNoch keine Bewertungen
- Reporte 2020 de La Oficina de Asuntos Globales de Estados UnidosDokument72 SeitenReporte 2020 de La Oficina de Asuntos Globales de Estados UnidosAristegui NoticiasNoch keine Bewertungen
- Reading Comprehension Exercise, May 3rdDokument3 SeitenReading Comprehension Exercise, May 3rdPalupi Salwa BerliantiNoch keine Bewertungen
- Equipoise HajjajDokument4 SeitenEquipoise HajjajerrelyoNoch keine Bewertungen
- Mri Emergency Coding Card v2Dokument1 SeiteMri Emergency Coding Card v2Afif AzmiNoch keine Bewertungen
- Science 9 Quarter 1 Week 2 Sim 3Dokument30 SeitenScience 9 Quarter 1 Week 2 Sim 3Jelly FloresNoch keine Bewertungen
- You Will Be Asked To Answer Individually The Questions Below: Answers Should Be Written in A 1/2 Crosswise Sheet of PaperDokument3 SeitenYou Will Be Asked To Answer Individually The Questions Below: Answers Should Be Written in A 1/2 Crosswise Sheet of PaperDummy AccountNoch keine Bewertungen
- Astaxanthin Uses and Effectiveness in Therapy of Acnes Vulgaris Final Revisi 7Dokument12 SeitenAstaxanthin Uses and Effectiveness in Therapy of Acnes Vulgaris Final Revisi 7Desica NatalisaNoch keine Bewertungen
- Blood Glucose MonitoringDokument4 SeitenBlood Glucose MonitoringAman ChaudharyNoch keine Bewertungen
- A Clinical Report On Partial Pulpotomy and Capping With Calcium Hydroxide in Permanent Incisors With Complicated Crown FractureDokument6 SeitenA Clinical Report On Partial Pulpotomy and Capping With Calcium Hydroxide in Permanent Incisors With Complicated Crown Fractureroy sepNoch keine Bewertungen
- Health 10 4th QDokument4 SeitenHealth 10 4th QLeonilo C. Dumaguing Jr.Noch keine Bewertungen
- Emerging and Re-Emerging Disease in NepalDokument25 SeitenEmerging and Re-Emerging Disease in NepalBinayaNoch keine Bewertungen
- How To Calculate Calories Intake: by Group 6Dokument9 SeitenHow To Calculate Calories Intake: by Group 6Reina Magfirah MokogintaNoch keine Bewertungen
- Infection Control Practice On Vital Signs Equipment: A Survey Among Senior Nursing Students in Iloilo City, PhilippinesDokument7 SeitenInfection Control Practice On Vital Signs Equipment: A Survey Among Senior Nursing Students in Iloilo City, PhilippinesRyan Michael OducadoNoch keine Bewertungen
- Anemia, Acute Bronchitis and Adequate NutritionDokument39 SeitenAnemia, Acute Bronchitis and Adequate NutritionSetiawan DanuNoch keine Bewertungen
- Distaclor Granules For Suspension 125mg/5ml & 250mg/5mlDokument2 SeitenDistaclor Granules For Suspension 125mg/5ml & 250mg/5mlfirdausazinun8684Noch keine Bewertungen
- Biro Administrasi Dan Akademik (Baak) : Berita Acara Kegiatan Belajar Mengajar (KBM)Dokument3 SeitenBiro Administrasi Dan Akademik (Baak) : Berita Acara Kegiatan Belajar Mengajar (KBM)Juventus HuruleanNoch keine Bewertungen
- Accreditation (Summary) December 29, 2017Dokument8 SeitenAccreditation (Summary) December 29, 2017Jacq CalaycayNoch keine Bewertungen
- Medicine PDFDokument385 SeitenMedicine PDFMaheshNoch keine Bewertungen
- Service Learning Reflection PaperDokument3 SeitenService Learning Reflection Paperapi-297614673Noch keine Bewertungen
- BW Health-5Dokument2 SeitenBW Health-5Michael JaballasNoch keine Bewertungen
- CHN 3Dokument5 SeitenCHN 3Lea TanNoch keine Bewertungen
- Global School-Based Student Health Survey: BackgroundDokument2 SeitenGlobal School-Based Student Health Survey: BackgroundU Bagja PutraNoch keine Bewertungen
- Model State Medical Marijuana Bill PDFDokument26 SeitenModel State Medical Marijuana Bill PDFJoseph PreisterNoch keine Bewertungen
- Mrcpsych TipsDokument7 SeitenMrcpsych Tipsmahadev470% (1)
- Viral Infections Part 1 by Nicolle Ann Pancho (Pediatrics Rotation)Dokument67 SeitenViral Infections Part 1 by Nicolle Ann Pancho (Pediatrics Rotation)Nicolle PanchoNoch keine Bewertungen
- AQUALIPODokument16 SeitenAQUALIPOAvalavenia Molina AbadNoch keine Bewertungen
- Antenatal Education For First Time MothersDokument26 SeitenAntenatal Education For First Time MothersPratik Ranjan NayakNoch keine Bewertungen
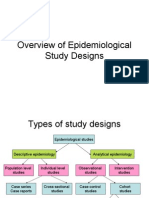
- Overview of Epidemiological Study DesignsDokument16 SeitenOverview of Epidemiological Study DesignsLakshmi Seth100% (2)
- Inventory List at in Emergei (Cy: PrsentDokument1 SeiteInventory List at in Emergei (Cy: PrsentVirginia BennettNoch keine Bewertungen
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsVon EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNoch keine Bewertungen
- The Age of Magical Overthinking: Notes on Modern IrrationalityVon EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityBewertung: 4 von 5 Sternen4/5 (27)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsVon EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsBewertung: 5 von 5 Sternen5/5 (1)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeVon EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeBewertung: 2 von 5 Sternen2/5 (1)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedVon EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedBewertung: 5 von 5 Sternen5/5 (81)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionVon EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionBewertung: 4 von 5 Sternen4/5 (404)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisVon EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisBewertung: 4.5 von 5 Sternen4.5/5 (42)
- The Obesity Code: Unlocking the Secrets of Weight LossVon EverandThe Obesity Code: Unlocking the Secrets of Weight LossBewertung: 4 von 5 Sternen4/5 (6)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDVon EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDBewertung: 5 von 5 Sternen5/5 (1)
- The Comfort of Crows: A Backyard YearVon EverandThe Comfort of Crows: A Backyard YearBewertung: 4.5 von 5 Sternen4.5/5 (23)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsVon EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsBewertung: 3.5 von 5 Sternen3.5/5 (3)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisVon EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisBewertung: 3.5 von 5 Sternen3.5/5 (2)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Von EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Bewertung: 4.5 von 5 Sternen4.5/5 (110)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaVon EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsVon EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsBewertung: 4.5 von 5 Sternen4.5/5 (170)
- Why We Die: The New Science of Aging and the Quest for ImmortalityVon EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityBewertung: 4 von 5 Sternen4/5 (3)
- Gut: the new and revised Sunday Times bestsellerVon EverandGut: the new and revised Sunday Times bestsellerBewertung: 4 von 5 Sternen4/5 (392)
- Sleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningVon EverandSleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningBewertung: 4 von 5 Sternen4/5 (3)
- 12 Rules for Life by Jordan B. Peterson - Book Summary: An Antidote to ChaosVon Everand12 Rules for Life by Jordan B. Peterson - Book Summary: An Antidote to ChaosBewertung: 4.5 von 5 Sternen4.5/5 (207)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisVon EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisBewertung: 4 von 5 Sternen4/5 (1)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryVon EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryBewertung: 4 von 5 Sternen4/5 (44)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessVon EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessBewertung: 4.5 von 5 Sternen4.5/5 (328)
- The Marshmallow Test: Mastering Self-ControlVon EverandThe Marshmallow Test: Mastering Self-ControlBewertung: 4.5 von 5 Sternen4.5/5 (58)
- A Brief History of Intelligence: Evolution, AI, and the Five Breakthroughs That Made Our BrainsVon EverandA Brief History of Intelligence: Evolution, AI, and the Five Breakthroughs That Made Our BrainsBewertung: 4.5 von 5 Sternen4.5/5 (6)