Beruflich Dokumente
Kultur Dokumente
Clinical Contributions To Addressing The Social Determinants of Health
Hochgeladen von
1234chocoOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Clinical Contributions To Addressing The Social Determinants of Health
Hochgeladen von
1234chocoCopyright:
Verfügbare Formate
CMJ1002-Patel.
qxd
3/12/10
9:47 AM
Page 130
PROFESSIONAL ISSUES
Clinical Medicine 2010, Vol 10, No 2: 1303
Clinical contributions to addressing the social determinants
of health
Kiran CR Patel, Peter Spilsbury and Rashmi Shukla
ABSTRACT The drive to address social determinants of health
is gaining momentum. Appreciating that health outcomes are
only partly affected by healthcare, clinicians and clinical communities can play a significant role in this crusade by action at
local, regional, national and global levels. A concerted and systematic focus on integrating and industrialising upstream interventions at every healthcare encounter is essential to prevent
future illness, thus enabling a paradigm shift in the healthcare
service from being one of illness management to health preservation. The evidence base demonstrates the cost efficacy of
upstream interventions. The challenge is how this evidence is
utilised to implement these interventions in everyday healthcare. Today, with a global economic crisis and challenged public
sector funding, the need to address prevention has never been
more pressing. Clinical engagement at all levels, from the front
line to the boardroom is vital. Clinicians must address access,
communication, strategy and commissioning to fulfil a professional responsibility to become and remain the corporate
memory of a health service focused on preventing illness while
simultaneously delivering cost-effective healthcare.
KEY WORDS: health inequalities, social determinants
Determinants of health outcomes
Introduction
The review on tackling social determinants of health by Sir
Michael Marmot has challenged all individuals and organisations
to assess their contributions to this agenda, in its quest to ameliorate health inequalities.1 Broadly, the commission from the World
Health Organization (WHO) highlights three areas for action:
to improve daily living conditions
to tackle the inequitable distribution of power, money and
resources
Kiran CR Patel, consultant cardiologist and honorary senior lecturer
in cardiovascular medicine, Sandwell and West Birmingham NHS
Trust and University of Birmingham; clinical lead for Staying Healthy,
NHS West Midlands Strategic Health Authority; chair of trustees,
South Asian Health Foundation; trustee, National Heart Forum;
Peter Spilsbury, director of strategy and regulation, NHS West
Midlands; Rashmi Shukla, regional director of public health, NHS
West Midlands/Department of Health West Midlands
This paper is based on a presentation given by Kiran CR Patel at
the Royal College of Physicians on 13 July 2009 during a policy
dialogue on social determinants of health and chronic disease
130
to measure and understand the problem and assess the
impact of action.
It is the third area in which clinicians may be able to contribute as well as implement practical reforms to address the
consequent inequalities which clinicians manage on a daily
basis.
At a macro level, the UK government has established a review
with four tasks. It must firstly identify the evidence most relevant to underpinning future policy and action. Secondly, it
must show how this evidence could be translated into practice.
Thirdly, it must advise on possible objectives and measures,
building on the experience of the current Public Service
Agreement targets on infant mortality and life expectancy.
Finally, it must publish a report of the review's work to contribute to a post-2010 health inequalities strategy. It is clear that
a wide range of clinical partnerships involving public health
and social care professionals are essential to deliver an optimal
strategy with realistic aspirations, transforming rhetoric into
practice.
It is important for clinicians to appreciate that functionally, the
current healthcare system contributes downstream by dealing
with health outcomes consequent to a combination of societal
and environmental factors. The NHS spends considerable
resource and effort in dealing with the health consequences of
inequalities, somewhat neglecting its potential contribution in
preventing those health consequences. Differential exposure to
these determinants or causes of causes, in conjunction with
differential vulnerability attributed by differential living conditions and access to healthcare, determines disparate health outcomes and the health inequalities witnessed by the medical profession and society at large.2 The aspiration of the NHS Next
Stage Review for the health service to transform from an illness
management to a health preserving service is not only beneficent to the individual, but makes considerable economic sense,
particularly in the impending economic climate of fiscal
famine.3 Maintaining health not only delivers individual wellbeing but maintains their contribution to society and the
economy, thus avoiding the fiscal consequences of illness and
subsequent dependence upon the welfare state.
A real movement to address social determinants of health and
disease has rightly gained momentum. Successive secretaries of
state for health have highlighted that inequalities in health are
Royal College of Physicians, 2010. All rights reserved.
CMJ1002-Patel.qxd
3/12/10
9:47 AM
Page 131
Clinical contributions to addressing the social determinants of health
something we could not afford to ignore, with poverty, unemployment and ill health too often inherited like a gene.
Challenges to the clinician
What are the potential roles of individual clinicians and clinical
communities in addressing social determinants of health? How
might the individual clinician contribute at levels ranging from
the individual to global populations? The clinician has evolved
to accommodate many roles and responsibilities ranging from
healer and pioneer, to that of manager and leader in todays
health service. Many will feel a sense of nihilism at the mere
thought of engaging with the social determinants agenda.
However, it is a challenge which clinicians must rise to. Without
a paradigm shift in the mindset of clinicians to accommodate
the need to be at the very least cogniscent of social determinants, healthcare economies will be slow to make the shift from
a reactive to a predictive health service and slow to reap the
rewards of such a shift.
The evidence base and drivers for tackling
social determinants
An evidence base alone is insufficient to tackle health inequalities and the social determinants of disease (indeed, traditional
studies lauded within evidence-based medicine usually fail to
define social value judgements of interventions), but a robust
review of evidence by organisations such as the National
Institute for Health and Clinical Excellence (NICE) is vital to
guiding policy and strategy. Levers, tools and incentives are
essential to translate evidence into practice. Performance management and impact assessments are equally essential to ensure
implementation is optimal and sustained. The challenge for
clinicians and public health communities is not to replace the
armoury of drugs and allied therapeutic interventions which the
profession is accustomed to providing, but rather complement
these with often neglected upstream interventions to optimise
personal and population health gains. Upstream interventions,
often considerably more cost effective than downstream interventions, may provide the opportunity costing to facilitate
investment within the NHS. Communication and coordinated
action between public health and clinical communities must be
strengthened in order to define, integrate and industrialise
upstream interventions throughout the health service.
Smoking alone accounts for over 50% of the variation in UK
life expectancy and up to 30% of all acute hospital admissions
are tobacco related. As a single brief intervention, plausible for
any healthcare professional to deliver, smoking cessation advice
may potentially have a dramatic impact on healthcare resource
utilisation.
Strategic challenge
Healthcare strategy must be optimally formulated and deployed
to ensure paramount health gains. While NHS targets have
Royal College of Physicians, 2010. All rights reserved.
undoubtedly improved healthcare by removing deleterious situations, such as two-year waiting times to see a specialist, other
targets and drivers can generate perverse incentives with little
health gain. Clinicians should professionally challenge strategies
and policies which are demonstrably inefficient or which divert
attention and resources away from more pressing priorities eg
where services are inversely proportional to need such as palliative care in inner cities.
Over their working careers, clinicians contribute to healthcare delivery for three or more decades and therefore must
accept the function of being the corporate memory of the
health service. Incessant reorganisation of the NHS undoubtedly disrupts focus and communication while creating artificial boundaries obstructive to seamless and equitable healthcare delivery but, with long-term vision, clinicians have an
opportunity to underpin intermittent turbulence with
strategic stability.
Addressing social determinants in acute care
At the coalface of acute care, clinicians clearly impact upon
acute health gains. Coupled to proactive case finding and
upstream interventions, such acute activity delivers the preventative healthcare expected of all healthcare staff. Social determinants of inequalities are often covert and therefore awareness is
necessary to pursue their detection. One example would be a
strategy to ensure that not only cessation of tobacco smoking
but also the reduction of passive smoking and smokeless
tobacco use be proactively sought and addressed, particularly in
areas of deprivation. By leading existing multidisciplinary
teams and extending their roles, clinical teams can detect determinants and impart upstream interventions along an entire
pathway of care. Newer structures and organisations therefore
need not necessarily be developed rather some things should
be done differently and different things should be done.
Following the delivery of acute care, clinicians must ensure
that pathways reaching into the community are optimised to
maximise benefits from secondary prevention. More challenging in an era when the healthcare economy aims to deliver
as much healthcare in the community as possible, clinicians
must guarantee that they engage with primary care, public
health and social care teams to ensure prevention is not only
delivered at every opportunity in the acute sector, but also that
appropriate strategies are developed to embed prevention services into mainstream primary care. In primary care, clinicians
must embrace the concept that not only is more acute care
offered closer to home, but entire pathways of care should be
delivered covering primordial and primary prevention in
tandem with health and social care interventions.
Analysis from WHO demonstrates that the top seven contributors to morbidity and mortality from any cause worldwide
are also cardiovascular risk factors and, therefore, cardiovascular disease prevention has much to offer the wider healthcare
economy as a starting point in the quest to ameliorate health
inequalities.
131
CMJ1002-Patel.qxd
3/12/10
9:47 AM
Page 132
Kiran CR Patel, Peter Spilsbury and Rashmi Shukla
Improving communication across clinical pathways
Enhanced communication across clinical pathways is essential to influence the root cause of much morbidity and mortality. Preconceptual health lays the foundation for disparities
and inequalities and therefore clinicians might wish to influence the upstream agenda of maternal and child health.
Childhood, adolescence and early adulthood offer opportunities to entertain primordial and primary prevention strategies across clinical pathways. When treating the consequences
of adverse behaviours in one pathway, eg alcohol-related
harm, does the clinician intervene to reduce the risks of subsequent admission or the psychosocial consequences of
alcohol abuse?
Improving access to healthcare
Simply providing does not ensure access to healthcare, but
rather may foster inequalities in access unless individuals are
made aware of their existence, the services are acceptable and
physically accessible (in time and place) and acquired equitably. Continuous audit and equity impact assessment of services is crucial to ensure inequalities are addressed. Equal
access is not necessarily equitable if healthcare needs are disparate. Commensurately, disparities in disease prevalence do
not necessarily equate to inequalities and this is an important
observation. Disparities may reflect different patterns of disease or presentation. Therefore, informed needs assessment,
audit and service development are key to respond to inequalities data from health outcome reports and regional health profiles demonstrating inequalities in care.4
Influencing service development and strategy
Clinicians and clinical networks can strongly influence healthcare commissioning but should also aspire to influencing local
strategic partnerships to ensure wider determinants of poor
health are addressed in local area agreements developed
between NHS, local authorities and partners. Therein is an
opportunity for clinicians to make a significant impact upon
local social determinants of health.
Clinical influence at a regional level
Clinical engagement engineered by the Next Stage review provides an opportunity for clinicians to influence regional strategies, programmes and partnerships.3 Regions must begin to use
knowledge of inequalities to guide strategic developments and
define the health and social care workforce, along with the skills
required of it to deliver upstream interventions and additionally detect triggers for urgent healthcare utilisation. Peer review
of clinical pathways, services and interagency links must be
facilitated to optimise the impact upon social determinants at a
macro level, cogniscent of the need to focus on mental as well
as physical wellbeing.
132
The current approach in the NHS to improving quality and
ensuring value for money in a time of global recession puts
innovation, productivity, and prevention at the heart of the
healthcare agenda. This is a process underpinned by clinical
engagement. Free of thought constraints, healthcare staff will
shortly enter into dialogue which aims to define and deliver
optimal healthcare in a challenging climate. Concepts of cost
effectiveness and its alignment with capacity (greater investment is not always commensurate with better healthcare),
equity and an appreciation of the overall healthcare economy
within these dialogues will strive to deliver an engaged workforce with wider strategic vision. Collaborative disinvestment
and strategic development has the potential to shape healthcare
without boundaries in a climate where competition and
boundaries have often constrained healthcare development for
the overall healthcare economy.
Clinical influence at a national level
At a national level, firstly there is ample opportunity for clinicians to engage in guideline development, particularly at
NICE where each guideline commendably has a focus on
inequalities and is tailored to meet the needs of groups where
the evidence base dictates a need. Clinicians have much to
contribute to public health programme guidance development by demonstrating opportunities for upstream interventions at each healthcare interaction. Secondly, a clinical contribution to challenging policies damaging economic growth
is essential and communities such as the medical royal colleges and voluntary organisations, by virtue of hosting such
debates, are rightly seizing the initiative to ensure developments in the food and drink, alcohol, tobacco and arms industries are fully aware of their health impact at population level.
It is a duty of clinical communities to demonstrate the social
injustice of inequitably weighted economic growth. Climate
change is a prime example of how the carbon footprint of
developed countries creates an unequal mortality burden on
developing countries and the poor. Consequently, all global
summits and policies should accommodate health impact
assessments and clinicians, particularly academic clinicians,
are invaluable in developing such assessments. The carbon
footprint of healthcare should begin to challenge individuals
and institutions, starting with the role of the NHS and its
employees.
Clinical influence at global level
Clinical contributions to the social determinants agenda at a
global level are more challenging. India, for example, is an economic powerhouse celebrated by trade sectors and organisations, yet a quarter of the population survive on less than $2 per
day, a third of all deaths occur in children under the age of five
years and almost half of three year olds are malnourished. All
clinical communities and organisations must be cogniscent of
global healthcare challenges and the responsibility developed
Royal College of Physicians, 2010. All rights reserved.
CMJ1002-Patel.qxd
3/12/10
9:47 AM
Page 133
Clinical contributions to addressing the social determinants of health
world governments have in playing their part in addressing
global inequalities.
An awareness of global health inequalities data is often useful
in developing local services. For example, globally, 20% of cardiovascular disease (CVD) deaths occur in south Asians. This is
projected to rise to 40% by 2025. Local outcomes data, which in
England have demonstrated year upon year that proportional
mortality ratios are higher in this ethnic group. How might the
physician use this information to improve health outcomes
locally? An appreciation of such inequalities enables the clinician to tailor not only individual healthcare with a heightened
suspicion of CVD in patients from this ethnic group, but proactive case finding might also be influenced at local, regional or
national levels.5 Risk assessment and interventions for primary
prevention might be influenced by such epidemiological data
too.6,7 Similarly, knowledge that CVD prevalence and outcomes
demonstrate a socioeconomic gradient enables justifiable
strategies for proactive case finding, risk assessment and
upstream interventions in deprived populations, together with
local tailoring of services to improve access and outcomes.
Local challenges are thus informed by global, national and
regional epidemiological data.
challenge of having a greater impact on health outcomes by
embracing opportunities to influence health inequalities by
addressing social determinants of health and disease.
Prevention is everybodys business in 21st-century healthcare
and clinicians are well placed to be the advocates of their most
vulnerable patients.
Conflicts of interest
KP is also chair of trustees for the South Asian Health Foundation
and trustee to the National Heart Forum, which have both contributed to the policy dialogue on social determinants of health.
References
1
2
3
4
Clinician as sociologist
Finally, for those clinicians who lead communities, one must
recognise that while healthcare delivery and social change
movements have been challenged to focus on diversity of the
populations they serve, we must celebrate similarity to the same
extent to which we focus on diversity, to develop more cohesive
rather than divided communities, thereby reducing the mental
strain of marginalised groups being perceived as different or
feeling as such.
Summary
Overall, it is time to appreciate that health outcomes are only
partly determined by health services. Doctors must rise to the
Royal College of Physicians, 2010. All rights reserved.
Marmot M. Closing the health gap in a generation: the work of the
Commission on Social Determinants of Health and its recommendations. Glob Health Promotion 2009;Suppl 1:237.
Whitehead M, Dahlgreen G. What can be done about inequalities in
health? Lancet 1991;338:105963
Darzi A. Quality and the NHS next stage review. Lancet
2008;371:15634.
Department of Health. Health profile of England 2008. London: DH,
2008. www.dh.gov.uk/en/Publicationsandstatistics/Publications/
PublicationsStatistics/DH_093465
Department of Health. Putting prevention first vascular checks: risk
assessment and management. London: DH, 2008. www.dh.gov.uk/en/
Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/
DH_083822
Hippisley-Cox J, Coupland C, Vinogradova Y et al. Predicting cardiovascular risk in England and Wales: prospective derivation and validation of QRISK2. BMJ 2008;336:147582.
National Institute for Health and Clinical Excellence. Lipid modification: cardiovascular risk assessment and the modification of blood lipids
for the primary and secondary prevention of cardiovascular disease.
London: NICE, 2008. www.nice.org.uk/nicemedia/pdf/
CG67FullGuideline1.pdf
Address for correspondence: Dr KCR Patel, Sandwell
Hospital, Lyndon, West Bromwich, West Midlands B71
4HJ. Email: Kiran.Patel@swbh.nhs.uk
133
Reproduced with permission of the copyright owner. Further reproduction prohibited without permission.
Das könnte Ihnen auch gefallen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5795)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1091)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Language of PreventionDokument9 SeitenLanguage of Prevention1234chocoNoch keine Bewertungen
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Doctor Talk: Communication Practice Role PlaysDokument6 SeitenDoctor Talk: Communication Practice Role Plays1234chocoNoch keine Bewertungen
- Multiplexers DemultiplexersDokument17 SeitenMultiplexers Demultiplexerslvsaru100% (1)
- Code Geass - StoriesDokument5 SeitenCode Geass - Stories1234chocoNoch keine Bewertungen
- Topical Steroids (Sep 19) PDFDokument7 SeitenTopical Steroids (Sep 19) PDF1234chocoNoch keine Bewertungen
- Fairy Tail - Main ThemeDokument3 SeitenFairy Tail - Main Theme1234chocoNoch keine Bewertungen
- Blue BirdDokument7 SeitenBlue Bird1234chocoNoch keine Bewertungen
- Mbs Quick Guide: JULY 2020Dokument2 SeitenMbs Quick Guide: JULY 20201234chocoNoch keine Bewertungen
- PBM Module1 MTP Template 0Dokument2 SeitenPBM Module1 MTP Template 01234chocoNoch keine Bewertungen
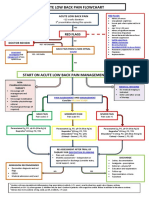
- Acute Low Back Pain Flowchart January 2017Dokument1 SeiteAcute Low Back Pain Flowchart January 20171234chocoNoch keine Bewertungen
- Managing Mental Illness in Patients From CALD Backgrounds: PsychiatryDokument5 SeitenManaging Mental Illness in Patients From CALD Backgrounds: Psychiatry1234chocoNoch keine Bewertungen
- Taking A Social and Cultural HistoryDokument3 SeitenTaking A Social and Cultural History1234chocoNoch keine Bewertungen
- Barrett's Esophagus: Identifying The Squamocolumnar (SC) and Gastroesophageal (GE) Junctions EndoscopicallyDokument10 SeitenBarrett's Esophagus: Identifying The Squamocolumnar (SC) and Gastroesophageal (GE) Junctions Endoscopically1234chocoNoch keine Bewertungen
- Preoperative AssessmentDokument9 SeitenPreoperative Assessment1234chocoNoch keine Bewertungen
- A Conceptual Framework For HealthDokument1 SeiteA Conceptual Framework For Health1234chocoNoch keine Bewertungen
- Acute Post-Op Pain ManagementDokument4 SeitenAcute Post-Op Pain Management1234chocoNoch keine Bewertungen
- Blue Card Declaration PDFDokument1 SeiteBlue Card Declaration PDF1234chocoNoch keine Bewertungen
- Prenatal Screening Test (AUS) PDFDokument24 SeitenPrenatal Screening Test (AUS) PDFshirley_ling_15Noch keine Bewertungen
- Final Test 1 K 2 - KeyDokument10 SeitenFinal Test 1 K 2 - KeyDuy HưngNoch keine Bewertungen
- GP125 - 200s Maintenance Manual-A520180913Dokument170 SeitenGP125 - 200s Maintenance Manual-A520180913paulatclayxNoch keine Bewertungen
- Sheena HSMDokument8 SeitenSheena HSMdesign12Noch keine Bewertungen
- SIP Report-PRATYUSH (1950-113) - 1Dokument49 SeitenSIP Report-PRATYUSH (1950-113) - 1LOKESH KUMAR SINHANoch keine Bewertungen
- Eaton Industrial Special Process List (SPL)Dokument5 SeitenEaton Industrial Special Process List (SPL)amirkhakzad498Noch keine Bewertungen
- Lecture On Dictionaries - Jupyter NotebookDokument13 SeitenLecture On Dictionaries - Jupyter NotebookruchikaNoch keine Bewertungen
- How Summer Students Perceive The Closed Summer Program: in The Case of Jimma UniversityDokument17 SeitenHow Summer Students Perceive The Closed Summer Program: in The Case of Jimma UniversityКонстантин НечетNoch keine Bewertungen
- 2001 Daewoo Nubira Service Manual2 PDFDokument685 Seiten2001 Daewoo Nubira Service Manual2 PDFalberto 32100% (1)
- Basiccharge Ev Ftu Superfast Data Sheet 028413Dokument2 SeitenBasiccharge Ev Ftu Superfast Data Sheet 028413Cojoc Constantin-CosminNoch keine Bewertungen
- Good Pitch India 2018 ReviewDokument145 SeitenGood Pitch India 2018 ReviewIndian Documentary FoundationNoch keine Bewertungen
- Parrot: by Alan BrownjohnDokument2 SeitenParrot: by Alan BrownjohnPADUMI SASIKALA50% (2)
- 2020 AMC Years 7-8 JuniorDokument8 Seiten2020 AMC Years 7-8 JuniorTodor DobrevNoch keine Bewertungen
- How To "Revert-Back" To "Previous-Version"???: Build 1 Testing DeploymentDokument19 SeitenHow To "Revert-Back" To "Previous-Version"???: Build 1 Testing DeploymentClaudiu Stefan HaiduNoch keine Bewertungen
- Family Tree Template With DetailsDokument8 SeitenFamily Tree Template With DetailsJude WellsNoch keine Bewertungen
- Blue A Ks2 Test3Dokument6 SeitenBlue A Ks2 Test3Mateo García-PumarinoNoch keine Bewertungen
- Problem Solving Essay Outline - ProcrastinationDokument2 SeitenProblem Solving Essay Outline - ProcrastinationAniqaNoch keine Bewertungen
- Ludo (Sorry) - Game StrategyDokument8 SeitenLudo (Sorry) - Game Strategysuperyoopy100% (1)
- ASLI 02 Supply Air Grilles Set - AIR ConditioningDokument21 SeitenASLI 02 Supply Air Grilles Set - AIR ConditioningAminul Hassan50% (2)
- SPHE8281DDokument35 SeitenSPHE8281Ddiego-tNoch keine Bewertungen
- Quiz 1 Distribusi Plus JawabanDokument6 SeitenQuiz 1 Distribusi Plus JawabandimasfupNoch keine Bewertungen
- Manual: InstructionDokument2 SeitenManual: InstructionBan ZanganaNoch keine Bewertungen
- Image Processing (Rry025)Dokument22 SeitenImage Processing (Rry025)Babasrinivas GuduruNoch keine Bewertungen
- Executive Leadership: Artificial Intelligence Primer For 2021Dokument10 SeitenExecutive Leadership: Artificial Intelligence Primer For 2021ranga.raman100% (1)
- Curriculum Vitae: Alex Gnanamani.KDokument4 SeitenCurriculum Vitae: Alex Gnanamani.KDIJUNoch keine Bewertungen
- RESEARCH FORM and STYLEDokument8 SeitenRESEARCH FORM and STYLEKristian Karl Bautista Kiw-isNoch keine Bewertungen
- Lemon BatteryDokument6 SeitenLemon BatteryMohammed AsifNoch keine Bewertungen
- Black Mirror Analysis: 15 Million Merits (Due 27/04/16)Dokument11 SeitenBlack Mirror Analysis: 15 Million Merits (Due 27/04/16)Will MunnyNoch keine Bewertungen
- Variables That Affect Teachers' Attitudes Towards Disability and Inclusive Education in Mumbai, IndiaDokument12 SeitenVariables That Affect Teachers' Attitudes Towards Disability and Inclusive Education in Mumbai, IndiaSumaiya HossainNoch keine Bewertungen
- Asynchronous ActivityDokument1 SeiteAsynchronous ActivityJoanna Mae MendozaNoch keine Bewertungen