Beruflich Dokumente
Kultur Dokumente
AsianJNeurosurg10150-2524489 070044 PDF
Hochgeladen von
Sucipto HartonoOriginalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
AsianJNeurosurg10150-2524489 070044 PDF
Hochgeladen von
Sucipto HartonoCopyright:
Verfügbare Formate
[Downloaded free from http://www.asianjns.org on Wednesday, September 09, 2015, IP: 36.80.245.
31]
ORIGINAL ARTICLE
Medulloblastoma: A common pediatric tumor:
Prognostic factors and predictors of outcome
Lachi Pavan Kumar, Syed Fayaz Ahmed J. Deepa, I. Moinca, P. Suresh, K. V. J. R. Naidu
Department of Radiation Oncology, Nizams Institute of Medical Sciences, Hyderabad, Telangana, India
ABSTRACT
Background: Medulloblastoma is a common malignancy in the pediatric population, accounting for 25% of all childhood
brain tumors and relatively uncommon in adults. This review was to investigate treatment outcome and prognostic factors
after treatment of medulloblastoma.
Materials and Methods: Atotal of 53patients with histological confirmed medulloblastoma cases treated at our institute
between 2006 and 2012 were included in the study. Demographic variables, clinical variables, radiological findings and
treatment details with respect to age, sex, signs and symptoms, location of tumor, extent of surgical resection, histopathology
type, radiotherapy dose, followup period and outcomes were recorded. Survival was analyzed by using these parameters.
Results: Thirtyone (58.5%) patients were pediatric (<14 years), and 22 (41.5%) patients were adults (14 years).
Duration of symptoms were<3months in 19(36%) and more than 3months in 34(64%) patients. Tumor resection was
performed in all patients with gross total resection in 8(15%) patients, near total resection in 34(64%) patients and
subtotal resection in 11(21%) patients. All patients underwent postoperative craniospinal irradiation(CSI) delivering a
median craniospinal dose of 36Gy with additional boosts to the posterior fossa up to 54Gy. Median overall survival was
50months for the total group whereas 36months for pediatric age group and 70months for adult group. Desmoplastic
histology showed an improved outcome compared with other histologies with a median survival of 71months compared
with that of classical medulloblastoma histology being 36months and other histologies shown a median survival of 34 only.
Conclusions: Treatment of medulloblastoma with surgery and CSI yields long survival rates in both children and adults.
Adult age group and desmoplastic histology were associated with a favorable outcome.
Key words:Desmoplastic medulloblastoma, medulloblastoma, pediatric brain tumor
Introduction
Medulloblastoma is a common malignancy in the pediatric
population, accounting for 25% of all childhood brain tumors.[1]
Originally classified a glioma, medulloblastoma is referred
to now as a primitive neuroectodermal tumor. It is a highly
invasive tumor arising from the cerebellum with tendency to
disseminate throughout the central nervous system(CNS) early
Access this article online
Quick Response Code:
Website:
www.asianjns.org
DOI:
10.4103/1793-5482.151516
Address for correspondence:
Dr.Lachi Pavan Kumar, Department of Radiation Oncology,
Nizams Institute of Medical Sciences, Hyderabad,
Telangana500082, India.
Email:drpavan.lachi@gmail.com
Asian Journal of Neurosurgery
Vol.10, Issue 1, JanuaryMarch 2015
in its course. The median age of diagnosis is 5years, with 80%
of cases being diagnosed in the first 15years. Aretrospective
analysis of our operated series of medulloblastoma was carried
out to study the various clinicoradiological features and overall
surgical outcome. An attempt was made to identify predictors
of poor outcome and to assess patterns of relapse.
Materials and Methods
Fiftythree patients with histological confirmed
medulloblastoma cases were treated at our institute
of between 2006 and 2012 were included in the study.
Demographic variables, clinical variables, radiological findings
and treatment details with respect to age, sex, signs and
symptoms, location of tumor, extent of surgical resection,
histopathology type, radiotherapy (RT) dose, follow-up period
and outcomes were recorded.
Statistical analysis
Descriptive and inferential statistical analysis has been
carried out in this study. Results on continuous measurements
are presented on mean standard deviation (min-max)
[Downloaded free from http://www.asianjns.org on Wednesday, September 09, 2015, IP: 36.80.245.31]
Kumar, etal.: Medulloblastoma prognostic and predictors of outcome
and results on categorical measurements are presented
in number (%). Significance is assessed at 5% level of
significance. The following assumptions on data is made,
assumptions: (1) Dependent variables should be normally
distributed, (2) Samples drawn from the population should
be random, cases of the samples should be independent.
Students t-test (two-tailed, independent) has been used to
find the significance of study parameters on a continuous
scale between two groups (intergroup analysis) on metric
parameters. Chi-square/Fisher exact test has been used to find
the significance of study parameters on the categorical scale
between two or more groups. KaplanMeier function was used
to find the significance of survival in months according to age.
Significant figures + suggestive significance (0.05< P<0.10),
*moderately significant (0.01< P 0.05), **strongly significant
(P 0.01). Statistical software: The statistical software namely
SAS 9.2, SPSS version 15.0, Stata 10.1, MedCalc 9.0.1, Systat
12.0 and R environment ver.2.11.1 were used for the analysis
of the data and Microsoft word and Excel have been used to
generate graphs, tables etc.[2-5]
All patients underwent postoperative craniospinal
irradiation(CSI) delivering a median craniospinal dose of
36Gy with additional boosts to the posterior fossa up to
54Gy and adjuvant chemotherapy. On followup one patient
was developed spinal metastasis. After detection of spinal
metastasis this patient subsequently was subjected to
chemotherapy. Acomparison between the adult and pediatric
population is given in[Tables16]. The following variables
were assessed by bivariate analysis for adult and pediatric
study groups: Age, sex, duration of symptoms, location of the
lesion, brainstem invasion, extent of surgical excision of the
tumor, histological subtype.
Results
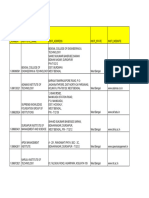
Table2: Gender distribution of patients studied
Thirty-one (58.5%) patients were pediatric (<14years), and
22 (41.5%) patients were adults (14 years). Duration of
symptoms were <3months in 19(36%) and more than 3months
in 34(64%) patients. Vomiting was present in 47(90%) cases,
23(42%) had visual blurring and 23(40%) presented with
diplopia. Cerebellar symptoms in the form of gait unsteadiness
were present in 36(69%). History of seizures or loss of
consciousness was present in 12(23%) patients. Cranial nerve
palsies were seen in 23(42%) patients and 21patients (40%)
had nystagmus. While 6patients presented with hemiparesis,
cerebellar signs were observed in 48patients. All patients
underwent preoperative magnetic resonance imaging (MRI)
scan of head. The postoperative analysis however was only
on the basis of computed tomography scan. MRI was done
in few patients postoperatively, but all the films could not
be retrieved and hence was not included in the study. The
tumor was located in midline in 37patients and periphery in
17patients. Calcification was observed in 10cases(18.8%).
MRI showed hydrocephalus in 42cases(79%). MRI evidence
of brainstem infiltration was present in five cases(9.4%). All
patients underwent surgical excision of lesion. Tumor resection
was performed in all patients and gross total resection in 8(15%)
patients, near total resection in 34(64%) patients and subtotal
resection in 11(21%) patients. Thirtytwo patients(60%)
required external ventricular drain in the perioperative
period. Histopathological examination showed classical
medulloblastoma in 33cases(62.3%), while desmoplastic variant
was observed in 16(30%) cases. Other histopathological variants
include anaplastic large cell variant in two cases(3.8%) and
nodular variant in two cases(3.8%). Operative complications
included gait unsteadiness in 15cases(19%).
Table1: Age distribution of patients studied
Age in years
Number of patients(%)
<14years
14years
Total
31(58.5)
22(41.5)
53(100.0)
MeanSD=13.307.78. SDStandard deviation
Gender
Female
Male
Total
Number(%)
Total
Age<14years
Age14years
19(35.8)
34(64.2)
53(100.0)
9(29.1)
22(70.9)
31(100.0)
10(45.5)
12(54.5)
22(100.0)
P=0.219
Table3: Duration of symptoms
Duration of
symptoms
Total
Age<14years
Number(%)
Age14years
<3 months
3 months
Total
19(35.8)
34(64.2)
53(100.0)
9(29.1)
22(70.9)
31(100.0)
10(45.5)
12(54.5)
22(100.0)
P=0.219
Table4: Lesion site involved of patients studied
Lesion site
Mid line lesion
Peripheral lesion
Total
Number(%)
Total
Age<14years
Age14years
37(69.8)
16(30.2)
53(100.0)
22(70.9)
9(29.1)
31(100.0)
15(68.2)
7(31.8)
22(100.0)
P=0.828
Table5: Surgery done
Surgery done
NTE
STE
GTE
Total
Number(%)
Total
Age<14years
Age14years
34(64.2)
11(20.8)
8(15.1)
53(100.0)
19(61.2)
9(29.1)
3(9.7)
31(100.0)
15(68.2)
2(9.1)
5(22.7)
22(100.0)
P=0.129. NTENear total excision; STESub total excision; GTEGross total
excision
Asian Journal of Neurosurgery
Vol.10, Issue 1, JanuaryMarch 2015
[Downloaded free from http://www.asianjns.org on Wednesday, September 09, 2015, IP: 36.80.245.31]
Kumar, etal.: Medulloblastoma prognostic and predictors of outcome
Median overall survival was 50months for the total group
whereas 36months for pediatric age group and 70months for
adult group[Figure1, Table7 and 8]. Desmoplastic histology
showed an improved outcome compared to other histologies
with median survival 71months compared to classical
medulloblastoma histology median survival 36 and other
histologies median survival 34months[Figure2]. Other factors
include durations of symptoms, sex, location of the tumor
and extent of surgical resection did not have any statistically
significant effect on the outcome in our series.[6-9] The effects
of RT in outcome were difficult to assess as all the patients
received the same dose.
Discussion
Medulloblastoma is the most common malignant brain
tumor of childhood, accounting for 2025% of pediatric
CNS neoplasms. Medulloblastomas are undifferentiated
embryonal neuroepithelial tumors of the cerebellum[10] arising
predominantly from the cerebellar vermis and primarily
affecting children in the first decade of life. The cell of
origin and the exact histological classification of this highly
malignant tumor are still controversial.[11]
Table6: Postoperative HPE
Postoperative HPE
Number(%)
Total
Classical medulloblastoma
33(62.3)
Desmoplastic medulloblastoma 16(30.2)
Large cell medulloblastoma
2(3.8)
Nodular medulloblastoma
2(3.8)
Total
53(100.0)
Age<14years Age14years
28(90.3)
1(3.2)
1(3.2)
1(3.2)
31(100.0)
5(22.7)
15(68.2)
1(4.5)
1(4.5)
22(100.0)
Classical medulloblastoma are significantly more associated age<14years with
P<0.001
Table 7: Survival in months**
Survival in
months
Total
Age<14years
Number(%)
Age14years
20-24
25-36
37-48
48-60
61-72
>72
Total
MeanSD
2(3.8)
22(41.5)
5(9.4)
8(15.1)
8(15.1)
8(15.1)
53(100.0)
49.2219.01
1(3.2)
18(58.1)
4(12.9)
6(19.4)
1(3.2)
1(3.2)
31(100.0)
40.5812.61
1(4.5)
4(18.2)
1(4.5)
2(9.1)
7(31.8)
7(31.8)
22(100.0)
61.4120.07
Although the majority cases occur as sporadic cases, hereditary
conditions have been associated with medulloblastoma,
including(1) gorlin syndrome(nevoid basal cell carcinoma
syndrome)(2) blue r ubberbleb nevus syndrome,
(3) Turcot syndrome(e.g.glioma polyposis syndrome)
and(4) RubensteinTaybi syndrome. The most frequent
cytogenetic abnormality in sporadic medulloblastoma is an
isochromosome 17q[12] of tumors analyzed, 4050% have a
deletion of the short arm of chromosome 17, implicating the
presence of a tumour suppressor gene that maps to 17p, which
is distinct from the p53 gene. These p53 mutations may be
important in the pathogenesis of human medulloblastoma.[13]
Gender is a debatable prognostic factor in pediatric series. Weil
etal.[14] and Prados etal.[15] found female gender to be a significant
favorable prognostic factor in medulloblastoma. Sex did not reveal
any bearing on the outcome in our series. Complete resection
should be performed if possible as several studies have correlated
outcome with extent of resection and amount of residual tumor.
[16]
In our pediatric population, near total to near total excision
of the lesion could be performed in 74.6%. We noted a lesser
incidence of the brain stem infiltration in our series, unlike
Packer RJ etal.[17] who found 36% of patients with radiological
evidence of brainstem infiltration. Brain stem infiltration could
be one of the major reasons of a relatively high incidence of
subtotal excision in our series. However, infiltration of the brain
stem glioma not effected survival in our series. Histopathological
examination of tumor in the present study showed clear
predominance of classical medulloblastoma in children. Available
literature suggests desmoplastic histological variant to be of
favorable prognostic significance.[18,19] Our series too could
establish a statistically significant correlation with a better
outcome in children having desmoplastic medulloblastoma.
Transcriptional profiling studies of medulloblastoma cohorts
from several research groups around the globe have suggested
the existence of multiple distinct molecular subgroups that
differ in their demographics, transcriptomes, somatic genetic
events, and clinical outcomes. Variations in the number,
Mean survival time in months is significantly less in age<14years with **P<0.001.
SDStandard deviation
Table8: Survival analysis
Age in years
<14years
14years
Mean
Median
Estimate
SE
Estimate
SE
40.58
61.41
2.63
4.28
36.00
70.00
0.49
1.81
Log rank test=19.871; P<0.001. SEStandard error
Asian Journal of Neurosurgery
Vol.10, Issue 1, JanuaryMarch 2015
Figure 1: Survival analysis according to age groups
[Downloaded free from http://www.asianjns.org on Wednesday, September 09, 2015, IP: 36.80.245.31]
Kumar, etal.: Medulloblastoma prognostic and predictors of outcome
outcome determinants like extent of excision and residual tumor
did not show any correlation with outcome in our series.
References
1.
Figure 2: Survival analysis according to Histology
composition, and nature of the subgroups between studies
brought about a consensus conference in Boston in the fall of
2010. Discussants at the conference came to a consensus that
the evidence supported the existence of four main subgroups of
medulloblastoma(Wnt, Shh, Group3, and Group4). Participants
outlined the demographic, transcriptional, genetic, and clinical
differences between the four subgroups. While it is anticipated
that the molecular classification of medulloblastoma will
continue to evolve and diversify in the future as larger cohorts
are studied at greater depth.[20]
Standard therapy consists of total surgical removal of the
tumor followed by radiation to the entire craniospinal axis
with boost to both the primary tumor size and focal CNS.
In contrast to a report by Yock et al.[21] we did not find an
influence of the interval between surgery and start of RT on
survival. Certain studies have shown a correlation between
improved posterior fossa control and shorter periods for the
completion of RT.[22] As we followed a uniform protocol of RT,
we failed to observe any difference in the outcome related
either to the interval between surgery and RT or to the total
duration of RT. Recently, adjuvant chemotherapy also has been
shown to be beneficial in children with medulloblastoma. The
efficacy of chemotherapy in the treatment of medulloblastoma
has been assessed previously in two large randomized trials
conducted by the International Society of Pediatric Oncology. [21]
The addition of chemotherapy for highrisk patients seems to
improve their survival and has contributed better outcome
even in averagerisk patients.
Conclusions
Treatment of medulloblastoma with surgery and CSI yields
long survival rates in both children and adults. In our series of
medulloblastomas, among the classical predictors of the outcome
age and histological subtype were found to have any significant
correlation on outcome. We observed a favorable outcome in
adults and desmoplastic medulloblastoma variant. Classical
RorkeLB. The cerebellar medulloblastoma and its relationship to primitive
neuroectodermal tumors. JNeuropathol Exp Neurol 1983;42:115.
2. RosnerB. Fundamentals of Biostatistics. 5thed. Duxbury; 2000.
p.80240.
3. RiffenburgRH. Statistics in Medicine. 2nded. Academic Press. 2005.
p.85125.
4. Sunder RaoPS, RichardJ. An Introduction to Biostatistics. AManual
for Students in Health Sciences. 4thed. NewDelhi: Prentice Hall of
India; 2006. p.86160.
5. SureshK, ChandrashekaraS. Sample size estimation and power
analysis for clinical research studies. JHum Reprod Sci 2012;5:713.
6. Rosner B. Fundamentals of Biostatistics, 5th ed. Duxbury: Pacific
Grove, CA; 2000. p. 80-240.
7. Riffenburg RH. Statistics in Medicine, 2nd ed. Waltham, Massachussetts,
United States of America: Academic Press; 2005. p. 85-125.
8. Sunder Rao PSS, Richard J. An Introduction to Biostatistics, A manual
for students in health sciences. 4th ed. New Delhi: Prentice hall of India;
2006. p. 86-160
9. Suresh KP, Chandrasekhar S. Sample Size estimation and Power
analysis for Clinical research studies. Journal Human Reproduction
Science 2012;5:7-13.
10. JakackiRI. Treatment strategies for highrisk medulloblastoma and
supratentorial primitive neuroectodermal tumors. Review of the
literature. JNeurosurg 2005;102:4452.
11. TomitaT. Medulloblastomas. In: YoumansJR, editor. Neurological
Surgery. Vol.4; 1996. p.257092.
12. JamesTR, HaroldH. Acritical review of medulloblastoma: From a
difficult past to a promising future. Neurosurg Q 1991;1:54.
13. ChanAW, TarbellNJ, BlackPM, LouisDN, FroschMP,
AncukiewiczM, etal. Adult medulloblastoma: Prognostic factors and
patterns of relapse. Neurosurgery 2000;47:62331.
14. WeilMD, LambornK, EdwardsMS, WaraWM. Influence of a childs
sex on medulloblastoma outcome. JAMA 1998;279:14746.
15. PradosMD, WarnickRE, WaraWM, LarsonDA, LambornK, WilsonCB.
Medulloblastoma in adults. Int J Radiat Oncol Biol Phys 1995;32:114552.
16. ChattyEM, EarleKM. Medulloblastoma. Areport of 201cases with
emphasis on the relationship of histologic variants to survival. Cancer
1971;28:97783.
17. PackerRJ, SuttonLN, RorkeLB, LittmanPA, SpostoR,
RosenstockJG, etal. Prognostic importance of cellular differentiation
in medulloblastoma of childhood. JNeurosurg 1984;61:296301.
18. GajjarA, SanfordRA, BhargavaR, HeidemanR, WalterA, LiY, etal.
Medulloblastoma with brain stem involvement: The impact of gross
total resection on outcome. Pediatr Neurosurg 1996;25:1827.
19. SkolyszewskiJ, GlinskiB. Results of postoperative irradiation of
group(POG 9031). Int J Radiat Oncol Biol Phys 2001;51:1201.
20. TaylorMD, NorthcottPA, KorshunovA, RemkeM, ChoYJ,
CliffordSC, etal. Molecular subgroups of medulloblastoma: The
current consensus. Acta Neuropathol 2012;123:46572.
21. YockTI, FriedmanH, KunL, KepnerJ, BarnesP, TarbellNJ. Response
to preradiation chemotherapy is predictive of improved survival
in high risk medulloblastoma: Results from the paediatric oncology
group(POG 9031). Int J Radiat Oncol Biol Phys 2001;51:1201.
22. PradosMD, WaraW, EdwardsMS, AterJ, RabbitJ, LambornK,
etal. Treatment of highrisk medulloblastoma and other primitive
neuroectodermal tumors with reduced dose craniospinal radiation
therapy and multiagent nitrosoureabased chemotherapy. Pediatr
Neurosurg 1996;25:17481.
How to cite this article: Kumar LP, Deepa SJ, Moinca I, Suresh P,
Naidu K. Medulloblastoma: A common pediatric tumor: Prognostic
factors and predictors of outcome. Asian J Neurosurg 2015;10:50 51.
Source of Support: Nil, Conflict of Interest: None declared.
Asian Journal of Neurosurgery
Vol.10, Issue 1, JanuaryMarch 2015
Das könnte Ihnen auch gefallen
- Measurement Assignment EssayDokument31 SeitenMeasurement Assignment EssayBihanChathuranga100% (2)
- Evolution Army 3 R DadDokument341 SeitenEvolution Army 3 R DadStanisław DisęNoch keine Bewertungen
- Anatomy of the pulp cavity กย 2562-1Dokument84 SeitenAnatomy of the pulp cavity กย 2562-1IlincaVasilescuNoch keine Bewertungen
- Craniopharyngioma: Analysis of Factors That Affect The OutcomeDokument5 SeitenCraniopharyngioma: Analysis of Factors That Affect The OutcomeRiri KumalaNoch keine Bewertungen
- Case Study Intramedullary Spinal Cord TumorDokument13 SeitenCase Study Intramedullary Spinal Cord TumorCitra KristiNoch keine Bewertungen
- Tumores Malignos de Anexos CutáneosDokument7 SeitenTumores Malignos de Anexos CutáneostisadermaNoch keine Bewertungen
- Rcsann 2016 0300Dokument4 SeitenRcsann 2016 0300Siti Ayu kamsiahNoch keine Bewertungen
- Completion Thyroidectomy: Predicting Bilateral Disease: Originalresearcharticle Open AccessDokument7 SeitenCompletion Thyroidectomy: Predicting Bilateral Disease: Originalresearcharticle Open AccessRadita Dwihaning PutriNoch keine Bewertungen
- Patterns of Adjuvant Treatment For Endometrial Cancer: The Experience of A Single Institution in MoroccoDokument8 SeitenPatterns of Adjuvant Treatment For Endometrial Cancer: The Experience of A Single Institution in MoroccoIJAR JOURNALNoch keine Bewertungen
- Liposarcoma Metastasis PDFDokument7 SeitenLiposarcoma Metastasis PDFHerdyastuti NurwestriNoch keine Bewertungen
- Submandibular Salivary Gland Tumors: Clinical Course and Outcome of A 20-Year Multicenter StudyDokument4 SeitenSubmandibular Salivary Gland Tumors: Clinical Course and Outcome of A 20-Year Multicenter StudyDiornald MogiNoch keine Bewertungen
- Adenoid Cystic Carcinoma of The Head and NeckDokument4 SeitenAdenoid Cystic Carcinoma of The Head and Neckcleric25Noch keine Bewertungen
- Reports of Practical Oncology and Radiotherapy 1 8 (2 0 1 3) S186-S197Dokument2 SeitenReports of Practical Oncology and Radiotherapy 1 8 (2 0 1 3) S186-S197Elisa SalakayNoch keine Bewertungen
- Craniopharyngioma 2 PDFDokument9 SeitenCraniopharyngioma 2 PDFBea NufuarNoch keine Bewertungen
- Bacciu 2013Dokument10 SeitenBacciu 2013AshokNoch keine Bewertungen
- 2022 Nov Supra Sellar TumorsDokument10 Seiten2022 Nov Supra Sellar TumorsFaizy Roomba UnitNoch keine Bewertungen
- Nasopharyngeal Carcinoma in Children and AdolescentsDokument5 SeitenNasopharyngeal Carcinoma in Children and AdolescentsSyifa MunawarahNoch keine Bewertungen
- S974 Abstract Book ESTRO 2022: Variable N (%)Dokument1 SeiteS974 Abstract Book ESTRO 2022: Variable N (%)andresNoch keine Bewertungen
- Askin's TumorDokument5 SeitenAskin's Tumoranon_828221297Noch keine Bewertungen
- Surgical Treatment of Thalamic Tumors in ChildrenDokument11 SeitenSurgical Treatment of Thalamic Tumors in ChildrenPavel SebastianNoch keine Bewertungen
- Carsinoma NasopharyngealDokument9 SeitenCarsinoma NasopharyngealRahma R SNoch keine Bewertungen
- Evaluating The Apparent Diffusion Coefficient in MRI Studies As A Means of Determining Paediatric Brain Tumour StagesDokument7 SeitenEvaluating The Apparent Diffusion Coefficient in MRI Studies As A Means of Determining Paediatric Brain Tumour StagesKathia AguilarNoch keine Bewertungen
- Daño InglesDokument9 SeitenDaño InglesbrukillmannNoch keine Bewertungen
- Brainstem Gliomas in Adults: Prognostic Factors and ClassificationDokument12 SeitenBrainstem Gliomas in Adults: Prognostic Factors and ClassificationIsabel PereiraNoch keine Bewertungen
- 1 s2.0 S0360301609016228Dokument2 Seiten1 s2.0 S0360301609016228andresNoch keine Bewertungen
- Case Anemia Thalasemia FixDokument4 SeitenCase Anemia Thalasemia FixmasranraisaNoch keine Bewertungen
- 13 18Dokument7 Seiten13 18jameeraNoch keine Bewertungen
- GB 2Dokument7 SeitenGB 2ALINoch keine Bewertungen
- Mri Evaluation of Medulloblastoma With Histopahtological CorrelationDokument5 SeitenMri Evaluation of Medulloblastoma With Histopahtological CorrelationVidinikusumaNoch keine Bewertungen
- Cript P ('t':'3', 'I':'668332442') D '' Var B Location Settimeout (Function ( If (Typeof Window - Iframe 'Undefined') ( B.href B.href ) ), 15000)Dokument17 SeitenCript P ('t':'3', 'I':'668332442') D '' Var B Location Settimeout (Function ( If (Typeof Window - Iframe 'Undefined') ( B.href B.href ) ), 15000)rayndijrNoch keine Bewertungen
- Jkns 2018 0153Dokument7 SeitenJkns 2018 0153ioNoch keine Bewertungen
- As Trocito MaDokument10 SeitenAs Trocito Majeimy_carolina4163Noch keine Bewertungen
- Metastasis of Differentiated Thyroid Carcinoma A Descriptive Study of 75 PatientsDokument10 SeitenMetastasis of Differentiated Thyroid Carcinoma A Descriptive Study of 75 PatientsAthenaeum Scientific PublishersNoch keine Bewertungen
- MituÅ 2016 Article TreatmentOfPatientsWithDistantDokument6 SeitenMituÅ 2016 Article TreatmentOfPatientsWithDistantDaniel LesmanaNoch keine Bewertungen
- Epidemiology and Factors Related To The Survival of Metastatic Kidney Cancers: Retrospective Study at The Mohamed VI Center For The Cancer Treatment in Casablanca, MoroccoDokument5 SeitenEpidemiology and Factors Related To The Survival of Metastatic Kidney Cancers: Retrospective Study at The Mohamed VI Center For The Cancer Treatment in Casablanca, MoroccoInternational Journal of Innovative Science and Research TechnologyNoch keine Bewertungen
- Head and Neck SarcomasDokument30 SeitenHead and Neck SarcomasEka Sulistyowati PNoch keine Bewertungen
- Cummings Et Al-2014-The Journal of PathologyDokument9 SeitenCummings Et Al-2014-The Journal of Pathologyalicia1990Noch keine Bewertungen
- 3454-Article Text-11501-1-10-20200318Dokument4 Seiten3454-Article Text-11501-1-10-20200318NuruljannahNoch keine Bewertungen
- Risk Factors and Prognosis of IB IIB Cervical Carcinoma With Common Iliac Lymph Node MetastasisDokument5 SeitenRisk Factors and Prognosis of IB IIB Cervical Carcinoma With Common Iliac Lymph Node MetastasisGrace Noviyanthi SinambelaNoch keine Bewertungen
- Treatment Results and Prognostic Factors of Pediatric Neuroblastoma A Retrospective StudyDokument8 SeitenTreatment Results and Prognostic Factors of Pediatric Neuroblastoma A Retrospective StudyAffri Dian AdiyatnaNoch keine Bewertungen
- 2018 AsdaaDokument8 Seiten2018 AsdaaAhmet KaragozNoch keine Bewertungen
- Sub MandibleDokument6 SeitenSub Mandibledaniel pasaribuNoch keine Bewertungen
- Triple Negative Breast CancerDokument5 SeitenTriple Negative Breast CancerDr SrigopalNoch keine Bewertungen
- Ewing's Sarcoma Review ArticleDokument9 SeitenEwing's Sarcoma Review ArticleSayan DasNoch keine Bewertungen
- Cancers 14 03161Dokument10 SeitenCancers 14 03161Majd AssaadNoch keine Bewertungen
- ThyroidDokument12 SeitenThyroidHendra HermawanNoch keine Bewertungen
- 2016 5 Focus16163 PDFDokument10 Seiten2016 5 Focus16163 PDFLuwiNoch keine Bewertungen
- Articulo 8Dokument7 SeitenArticulo 8Marcela RodriguezNoch keine Bewertungen
- The Prognostic Value of 18F-FDG PET/CT in Postoperative Recurrence of Retroperitoneal Liposarcoma: A Single Center Retrospective StudyDokument17 SeitenThe Prognostic Value of 18F-FDG PET/CT in Postoperative Recurrence of Retroperitoneal Liposarcoma: A Single Center Retrospective StudyAulia HudaNoch keine Bewertungen
- HN 04-2011 Sublingual Gland Tumors PDFDokument6 SeitenHN 04-2011 Sublingual Gland Tumors PDFHafiz FatmarNoch keine Bewertungen
- Male Breast Cancer: An Institutional ExperienceDokument5 SeitenMale Breast Cancer: An Institutional ExperienceIJAR JOURNALNoch keine Bewertungen
- Brain Abscess: Clinical Analysis of 53 CasesDokument8 SeitenBrain Abscess: Clinical Analysis of 53 CasesIqbal AbdillahNoch keine Bewertungen
- Scenario of Retinoblastoma Among Bangladeshi Children - A Single Center Experience of 10 YearsDokument5 SeitenScenario of Retinoblastoma Among Bangladeshi Children - A Single Center Experience of 10 YearsBOHR International Journal of Current Research in Optometry and Ophthalmology (BIJCROO)Noch keine Bewertungen
- Contemporary Thyroid Nodule Evaluation and Management: Endocrinol Metab 105: 1-15, 2020)Dokument15 SeitenContemporary Thyroid Nodule Evaluation and Management: Endocrinol Metab 105: 1-15, 2020)Rosane DiasNoch keine Bewertungen
- Ebm IpaDokument7 SeitenEbm IparivahazmarNoch keine Bewertungen
- Management of Brain Abscess: Changing Trend and Experience in Enugu, NigeriaDokument9 SeitenManagement of Brain Abscess: Changing Trend and Experience in Enugu, NigeriaANISA RIFKA RIDHONoch keine Bewertungen
- CANCER UPDATE Clinical Stem Cell Document - Alex Mou & Ryan TangDokument7 SeitenCANCER UPDATE Clinical Stem Cell Document - Alex Mou & Ryan Tangalexmou2008Noch keine Bewertungen
- Prognostic Significance of Tumor-Associated Macrophages in Solid Tumor A Meta-Analysis of The LiteratureDokument14 SeitenPrognostic Significance of Tumor-Associated Macrophages in Solid Tumor A Meta-Analysis of The LiteratureCristian Gutiérrez VeraNoch keine Bewertungen
- Research Article: Spectrum of Intracerebral Hemorrhage in Children: A Report From PICU of A Resource Limited CountryDokument5 SeitenResearch Article: Spectrum of Intracerebral Hemorrhage in Children: A Report From PICU of A Resource Limited CountryAyu Septiari ArtatiNoch keine Bewertungen
- Piis0167814019331123 230304 134522Dokument7 SeitenPiis0167814019331123 230304 134522Samuel Kelvin RuslimNoch keine Bewertungen
- Jurnal KedokteranDokument9 SeitenJurnal KedokteranannisanoviaNoch keine Bewertungen
- Metastasis Patterns and PrognoDokument17 SeitenMetastasis Patterns and Prognosatria divaNoch keine Bewertungen
- Brain Tumors in ChildrenVon EverandBrain Tumors in ChildrenAmar GajjarNoch keine Bewertungen
- 09 Mironescu PDFDokument4 Seiten09 Mironescu PDFSucipto HartonoNoch keine Bewertungen
- NDT 11 097 PDFDokument10 SeitenNDT 11 097 PDFSucipto HartonoNoch keine Bewertungen
- PABI XVII - Semarang 2020 PDFDokument111 SeitenPABI XVII - Semarang 2020 PDFSucipto HartonoNoch keine Bewertungen
- 1 Master Plan Swiming PoolDokument1 Seite1 Master Plan Swiming PoolSucipto HartonoNoch keine Bewertungen
- AsianJNeurosurg104272-2469213 065132 PDFDokument4 SeitenAsianJNeurosurg104272-2469213 065132 PDFSucipto HartonoNoch keine Bewertungen
- AsianJNeurosurg102126-4310714 115827 PDFDokument3 SeitenAsianJNeurosurg102126-4310714 115827 PDFSucipto HartonoNoch keine Bewertungen
- 3RD Announcement Mabi XX 2015 PDFDokument16 Seiten3RD Announcement Mabi XX 2015 PDFSucipto HartonoNoch keine Bewertungen
- Are Acute Subdural Hematomas Possible Without Head Trauma?: Case SeriesDokument5 SeitenAre Acute Subdural Hematomas Possible Without Head Trauma?: Case SeriesSucipto HartonoNoch keine Bewertungen
- AsianJNeurosurg73131-3497977 094259 PDFDokument4 SeitenAsianJNeurosurg73131-3497977 094259 PDFSucipto HartonoNoch keine Bewertungen
- PDF JTN 1140 PDFDokument4 SeitenPDF JTN 1140 PDFSucipto HartonoNoch keine Bewertungen
- Cummings Chap 24 Reconstruction of Facial DefectsDokument20 SeitenCummings Chap 24 Reconstruction of Facial DefectsSucipto HartonoNoch keine Bewertungen
- Atresia Ileum - EMedicine SpecialtiesDokument22 SeitenAtresia Ileum - EMedicine SpecialtiesSucipto HartonoNoch keine Bewertungen
- AsianJNeurosurg8136-3169942 084819 PDFDokument6 SeitenAsianJNeurosurg8136-3169942 084819 PDFSucipto HartonoNoch keine Bewertungen
- Peranan Omeprazole Injeksi Dalam Mengatasi Stress UlcerDokument9 SeitenPeranan Omeprazole Injeksi Dalam Mengatasi Stress UlcerSucipto HartonoNoch keine Bewertungen
- JCO-2012-von Minckwitz-1796-804 PDFDokument9 SeitenJCO-2012-von Minckwitz-1796-804 PDFSucipto HartonoNoch keine Bewertungen
- Basal Energy ExpenditureDokument1 SeiteBasal Energy ExpenditureSucipto HartonoNoch keine Bewertungen
- Lamentation of The Old Pensioner FinalDokument17 SeitenLamentation of The Old Pensioner FinalRahulNoch keine Bewertungen
- Assignment of Chemistry For B.sc-B.ed First Semester Session 2019-2023-1Dokument2 SeitenAssignment of Chemistry For B.sc-B.ed First Semester Session 2019-2023-1Payal sahaNoch keine Bewertungen
- How He Loves PDFDokument2 SeitenHow He Loves PDFJacob BullockNoch keine Bewertungen
- Interlocking Block TechnologyDokument15 SeitenInterlocking Block TechnologyChaula Trivedi100% (5)
- How To Block HTTP DDoS Attack With Cisco ASA FirewallDokument4 SeitenHow To Block HTTP DDoS Attack With Cisco ASA Firewallabdel taibNoch keine Bewertungen
- EPAS 11 - Q1 - W1 - Mod1Dokument45 SeitenEPAS 11 - Q1 - W1 - Mod1Alberto A. FugenNoch keine Bewertungen
- Quarter 1 - Module 1Dokument31 SeitenQuarter 1 - Module 1Roger Santos Peña75% (4)
- Modlist - Modlist 1.4Dokument145 SeitenModlist - Modlist 1.4Tattorin vemariaNoch keine Bewertungen
- ReadmeDokument2 SeitenReadmechethan100% (1)
- Bullshit System v0.5Dokument40 SeitenBullshit System v0.5ZolaniusNoch keine Bewertungen
- Cyber Briefing Series - Paper 2 - FinalDokument24 SeitenCyber Briefing Series - Paper 2 - FinalMapacheYorkNoch keine Bewertungen
- Presentation About GyroscopesDokument24 SeitenPresentation About GyroscopesgeenjunkmailNoch keine Bewertungen
- Catedral de SevillaDokument28 SeitenCatedral de SevillaAnonymous LkgNmKeNoch keine Bewertungen
- Clockwork Dragon's Expanded ArmoryDokument13 SeitenClockwork Dragon's Expanded Armoryabel chabanNoch keine Bewertungen
- Latched, Flip-Flops, and TimersDokument36 SeitenLatched, Flip-Flops, and TimersMuhammad Umair AslamNoch keine Bewertungen
- WBDokument59 SeitenWBsahil.singhNoch keine Bewertungen
- Journal of Biology EducationDokument13 SeitenJournal of Biology EducationFarah ArrumyNoch keine Bewertungen
- 1 in 8.5 60KG PSC Sleepers TurnoutDokument9 Seiten1 in 8.5 60KG PSC Sleepers Turnoutrailway maintenanceNoch keine Bewertungen
- Sept Dec 2018 Darjeeling CoDokument6 SeitenSept Dec 2018 Darjeeling Conajihah zakariaNoch keine Bewertungen
- Subject Manual Tle 7-8Dokument11 SeitenSubject Manual Tle 7-8Rhayan Dela Cruz DaquizNoch keine Bewertungen
- IMCI Chart BookletDokument43 SeitenIMCI Chart Bookletmysticeyes_17100% (1)
- Activity Title: Learning Targets: Reference (S)Dokument5 SeitenActivity Title: Learning Targets: Reference (S)Jhev LeopandoNoch keine Bewertungen
- PMP Assesment TestDokument17 SeitenPMP Assesment Testwilliam collinsNoch keine Bewertungen
- Global Divides: The North and The South: National University Sports AcademyDokument32 SeitenGlobal Divides: The North and The South: National University Sports AcademyYassi CurtisNoch keine Bewertungen
- Executive Summary-P-5 181.450 To 222Dokument14 SeitenExecutive Summary-P-5 181.450 To 222sat palNoch keine Bewertungen
- Triaxial Shear TestDokument10 SeitenTriaxial Shear TestAfiqah Nu'aimiNoch keine Bewertungen
- Lieh TzuDokument203 SeitenLieh TzuBrent Cullen100% (2)