Beruflich Dokumente
Kultur Dokumente
Acu+Moxi On Insomnia
Hochgeladen von
Madan KumarOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Acu+Moxi On Insomnia
Hochgeladen von
Madan KumarCopyright:
Verfügbare Formate
Online Submissions: http://www.journaltcm.
com
info@journaltcm.com
J Tradit Chin Med 2013 August 15; 33(4): 428-432
ISSN 0255-2922
2013 JTCM. All rights reserved.
CLINICAL STUDY
TOPIC
Curative effect of acupuncture and moxibustion on insomnia: a randomized clinical trial
Xiyan Gao, Cuixiang Xu, Peiyu Wang, Shan Ren, Yanli Zhou, Xuguang Yang, Ling Gao
aa
Xiyan Gao, Cuixiang Xu, Peiyu Wang, Shan Ren, Yanli
Zhou, Xuguang Yang, Ling Gao, College of Acupuncture
and Massage, Henan University of Traditional Chinese Medicine, Zhengzhou 450008, China
Supported by Chinese National Natural Science Foundation 81173335, Research into Effect of Acupuncture on Expression of Protein Difference in Brain Tissue of Rat Model
with Insomnia
Correspondence to: Prof. Xiyan Gao, College of Acupuncture and Massage, Henan University of Traditional Chinese
Medicine, Zhengzhou 450008, China. gaoxiyan@yeah.net
Telephone: +86-18703634802
Accepted: March 16, 2013
groups. However, the reduction in the experiment
group was greater than that in the control group in
sleeping quality, time to fall asleep, sleeping disorder, and daytime function (P<0.05).
CONCLUSION: Acupuncture and moxibustion at
Baihui (GV 20), Sishencong (EX-HN 1), Shenmai (BL
62), and Zhaohai (KI 6) significantly improved insomnia symptoms in the experiment group compared with the control group.
2013 JTCM. All rights reserved.
Key words: Acupuncture; Sleep initiation and maintenance disorders; Treatment outcome; Randomized clinical trials
Abstract
OBJECTIVE: To observe the effect of acupuncture
and moxibustion on insomnia and explore its
mechanism.
INTRODUCTION
Insomnia, a common sleeping disorder, manifests as an
insufficiency of sleep time and a decline in sleep quality. Therefore, insomnia greatly influences the life,
study, and work of patients. Prolonged use of sleeping
pills can bring about drug dependence and hypofunction. We have used acupuncture and moxibustion to
treat insomnia without adverse reactions. Therefore,
we sought to perform a randomized clinical trial to further explore the effect of acupuncture and moxibustion
on insomnia.
METHODS: One hundred and twenty patients
were randomly divided into an experiment group
and a control group. Sixty patients in the experiment group were treated once a day with acupuncture at Baihui (GV 20), Sishencong (EX-HN 1), Shenmai (BL 62), and Zhaohai (KI 6) and with moxibustion at Baihui (GV 20) and Sishencong (EX-HN 1).
Sixty patients in the control group were acupunctured once a day at Shenmen (HT 7), Neiguan (PC
6), and Sanyinjiao (SP 6). The Pittsburgh Sleep Quality Index (PSQI) was used to compare sleep improvement between the two groups.
MATERIALS AND METHODS
Patient data
One hundred and twenty outpatients of the Department of Acupuncture and Moxibustion in the Third
Affiliated Hospital of Henan College of Traditional
Chinese Medicine from January 2010 to December
RESULTS: The total effective rate was 87.7% in the
experiment group and 76.3% in the control group.
The PSQI scores and the total score were lower after treatment than before treatment in both
JTCM | www. journaltcm. com
428
August 15, 2013 | Volume 33 | Issue 4 |
Gao XY et al. / Clinical Study
2011 were randomly divided into an experiment group
and a control group. Among the 60 patients in the experiment group, there were 23 males and 37 females
aged (39 13) years with Pittsburgh Sleep Quality Index (PSQI) scores of 184. Among the 60 patients in
the control group, there were 26 males and 34 females
aged (40 13) years with PSQI scores of 17 4. There
was no statistical difference (P>0.05) in sex, age, or
PSQI score between the two groups.
ed the therapeutic plan in manipulation, (b) suspended
two treatments in the therapeutic period, or (c) used
other methods to help insomnia symptoms.
Standard of dropout
Patients were considered dropouts of the study if they:
(a) failed to visit, (b) willingly quit the therapeutic process or could not persist in treatment because of unexpected conditions, or (c) had poor obedience with incomplete data during the clinical trial.
Research design
This study was a single-blind randomized controlled
trial. Individuals were randomized by a computer-generated allocation list. The patients and registrar did not
know to which group the patient had been allocated.
This study met the standards of medical ethics and was
approved by the ethics committee of the Third Affiliated Hospital of Henan College of Traditional Chinese
Medicine. All patients signed an informed consent
form.
Standard of suspension
Patients who could not tolerate the treatment or had serious adverse reactions during treatment suspended the
clinical trial. Patients who refused to be treated or continued to use drugs or other treatments during the therapeutic period were also suspended.
Needles
Dispensable Hanyi needles, 0.30 mm in diameter and
25 mm or 40 mm in length, were used for acupuncture (produced by Tianjin Huahong Medical Material
Limited Company, batch number 101201, Tianjin,
China).
Standard of diagnosis
We adopted the insomnia-diagnosing standard from
the third edition of the Chinese Classification of Mental Diseases (CCMD-3)1 and the sleep-detecting method published by the World Health Organization
(WHO). Sleeping efficiency was determined with the
formula (sleeping efficiency=actual time asleep/time
from going to bed to getting up 100% ). All patients
conformed to the insomnia diagnosis standard in the
CCMD-3 and their illness course exceeded half a year.
Patients with insomnia caused by somatic or mental
diseases or by prolonged use of tranquilizers or other
drugs were excluded.
Taking acupoints
Acupoints were taken in the two groups in reference to
Acupuncture and Moxibustion, TCM teaching material for higher education.
Acupoints in the experiment group were: Baihui (GV
20), Sishencong (EX-HN 1), Shenmai (BL 62), and
Zhaohai (KI 6). Xinshu (BL 15) and Pishu (BL 20)
were added for deficiency of both heart and spleen.
Xinshu (BL 15) and Danshu (BL 19) were added for
Qi deficiency of both heart and gallbladder. Xingjian
(LR 2) and Taichong (LR 3) were added for fire-syndrome caused by stagnation of liver-Qi. Taixi (KI 3)
and Taichong (LR 3) were added for hyperactivity of
fire because of Yin deficiency.
Acupoints in the control group were: Shenmen (HT
7), Neiguan (PC 6), and Sanyinjiao (SP 6). Adjunct
acupoints were the same as in the experiment group.
Standard of inclusion
Patients were included if they: (a) conformed to the
standard for diagnosing insomnia, (b) were 18-65 years
old, (c) had no insomnia caused by substantive damage
to internal organs, (d) had not taken Chinese medicines (including Chinese patent drugs and decoctions
for nourishing the heart to calm the mind) or Western
Medicine (including bromide, Librium, or diazepam)
to treat insomnia in the past week, or if they took these
drugs for 3-5 days but stopped taking them for more
than 7 days, and e) signed an informed consent form.
Manipulation
Patients in the experiment group lay in the dorsal position. After the skin was routinely sterilized, needles
were inserted into Baihui (GV 20) and Sishencong
(EX-HN 1) 0.8 cun deep. After the needling sensation,
the uniform reinforcing-reducing method was performed. Needles were inserted into Shenmai (BL 62)
and Zhaohai (KI 6) 0.5 cun deep. After the needling
sensation, the reinforcing method was performed at
Zhaohai (KI 6) and reducing method at Shenmai (BL
62) and adjunct acupoints. After acupuncture, a doctor
held a moxa roll (produced by Nanyang Wolong
Hanyi Mugwort Floss Factory, Nanyang, China) with
one end ignited to perform moxibustion at Baihui
(GV 20) and Sishencong (EX-HN 1) for 40 min. During its retention, the needle was manipulated once ev-
Standard of exclusion
Patients were excluded if they: (a) did not conform to
the standards of diagnosis and inclusion, (b) had accepted other treatments possibly influencing the indexes of effects used in this study, (c) had serious cardio-cerebral blood vessel, liver, kidney, hematopoietic system,
or mental diseases, (d) were pregnant or lactating female patients, and (e) had other factors necessarily excluded.
Standard of rejection
Patients were removed from the study if they: (a) violatJTCM | www. journaltcm. com
429
August 15, 2013 | Volume 33 | Issue 4 |
Gao XY et al. / Clinical Study
was used for comparison between two groups. A 2 test
was used to compare enumeration data. P<0.05 is regarded as a statistical difference.
ery 10 min. The treatment was carried out once in the
afternoon every day for 15 days as a course of treatment.
Patients in the control group lay in the dorsal position.
After the skin was routinely sterilized, needles were inserted into Shenmen (HT 7) 0.5 cun deep, Neiguan
(PC 6) 0.8 cun deep, and Sanyinjiao (SP 6) 1.0 cun
deep. After the needling sensation, the uniform reinforcing-reducing method was performed. The reducing
method was practiced at adjunct acupoints. During its
retention, the needle was manipulated once every
10 min. The treatment was carried out once in the afternoon every day for 15 days as a course of treatment.
RESULTS
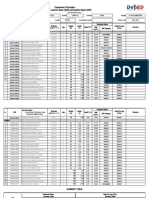
Comparison of clinical curative effects between the
two groups
Among the 60 patients in the experiment group, three
dropped out (two were patients with poor obedience
and one failed to visit), leaving a qualification rate of
95% . The treatment in the experiment group resulted
in cure in 27 patients, an obvious effect in 11 patients,
effectiveness in 12 patients, and ineffectiveness in seven
patients. The total effective rate was 87.7% . Among
the 60 patients in the control group, one dropped out
(failed to visit), a qualification rate of 98.3%. The treatment in the control group resulted in cure in 22 patients, an obvious effect in 13 patients, effectiveness in
10 patients, and ineffectiveness in 14 patients. The total effective rate was 76.3%. A 2 test showed that the
total effective rate in the experiment group was much
higher than that in the control group (P<0.01) (Table 1).
There was a statistical difference (texperiment group=3.12, tcontrol
group=3.22, P<0.01) in the total PSQI score before and
after treatment in the two groups. Both therapeutic
methods had curative effects on insomnia. There was a
statistical difference (t=2.89, P<0.01) in the total PSQI
score after treatment between the two groups. The improvement of the total PSQI score in the experiment
group was greater than that in the control group. The
difference of total PSQI score before and after treatment in the experiment group was better than that in
the control group (Table 2).
There was a statistical difference (P<0.05) in the score
of the various PSQIs before and after treatment in the
two groups. Both therapeutic methods had curative effects on insomnia. There was a statistical difference (P<
0.01) in the score of sleep quality, time to fall asleep,
sleep disorder, and daytime function after treatment between the two groups. There was no statistical difference (P>0.05) in the sleeping time and sleeping efficiency scores, indicating that the curative effect in the
experiment group was better than that in the control
group in sleeping quality, time to fall asleep, sleep disorder, and daytime function. Comparison of differences
in the score of various PSQIs before and after treatment between the two groups showed that the improve-
Measurements
We adopted the scale for evaluating PSQIs,2 including:
sleep quality, time to fall asleep, sleeping time, sleeping
efficiency, daytime functions, and total score. Specially
assigned persons were in charge of enquiring about illness condition and making a record before, 1 week,
and 2 weeks after treatment and a record of patients
who were clinically cured 7 days after the end of treatment.
Standard for evaluating curative effect
In reference to the standard for evaluating curative effects on insomnia in the Principle for Directing Clinical Research into New Chinese Drugs3 published by
the Health Ministry, cured insomnia includes sleeping
time returning to normal, sleeping time at night exceeding 6 h, or patients feeling rested after sound sleep.
An obvious effect means that sleep is clearly improved,
sleeping time increases by more than 3 h, and sleep becomes sounder. Effectiveness means that symptoms are
alleviated and sleeping time increases by less than 3 h.
Ineffectiveness means that insomnia is unimproved or
aggravated and the patient drops out.
Statistical analyses
Because the acupuncture and moxibustion practitioner
cannot be double-blinded in clinical experiments, the
single-blind method is used. Specially assigned persons
are independently in charge of manipulation, recording illness condition, and statistic analysis. SPSS 13.0
software (produced by SPSS China Software Shanghai
Limited Company, Shanghai, China) was used to process data. Measurement data are expressed as mean value standard difference ( x s). A t-test of paired data
was used for comparison before and after treatment in
the same group. A t-test of two independent samples
Table 1 Comparison of curative effects on insomnia in patients between two groups (n)
Group
Cure
Obvious effect
Effectiveness
Ineffectiveness
Total effective rate (%)
Control
59
22
13
10
14
76.3
Experiment
57
27
11
12
87.7
P value
0.000
Notes: experiment group were treated once a day with acupuncture at Baihui (GV 20), Sishencong (EX-HN1), Shenmai (BL 62), and Zhaohai (KI 6) and with moxibustion at Baihui (GV 20) and Sishencong (EX-HN1); control group were acupunctured once a day at Shenmen (HT 7), Neiguan (PC 6), and Sanyinjiao (SP 6). The efficiency of two groups were 76.3%, 87.7%; the Experimental group was significantly higher than that in control group (P<0.01).
JTCM | www. journaltcm. com
430
August 15, 2013 | Volume 33 | Issue 4 |
Gao XY et al. / Clinical Study
Table 2 Comparison of total PSQI score before and after treatment in two groups ( x s)
Group
Total score before treatment
Total score after treatment
Difference before and after treatment
Control
59
145
55a
84
Experiment
57
154
43ab
144c
Notes: experiment group were treated once a day with acupuncture at Baihui (GV 20), Sishencong (EX-HN 1), Shenmai (BL 62), and
Zhaohai (KI 6) and with moxibustion at Baihui (GV 20) and Sishencong (EX-HN 1); control group were acupunctured once a day at
Shenmen (HT 7), Neiguan (PC 6), and Sanyinjiao (SP 6). aP<0.01, compared with the total score before treatment in the same group; bP<
0.01, compared with the total score after treatment in the control group; cP<0.01, compared with the difference before and after treatment
in the control group.
ment in the experiment group was more obvious than
that in the control group (Table 3).
balance of the Yin heel vessel and Yang heel vessel can
people gain regular sleep. Consequently, regulation of
the heel vessels and balance of Yin and Yang can treat
insomnia. Shenmai (BL 62) and Zhaohai (KI 6) are
both in the Eight Influential Points. Zhaohai (KI 6) is
a point on the kidney meridian of foot shaoyin, which
links with the Yin heel vessel. Acupuncture should use
the reinforcing method. Shenmai (BL 62) is a point on
the bladder meridian of foot taiyang, which links with
the Yang heel vessel. Shenmai should be stimulated
with the reducing method. These two points can reinforce Yin and reducing Yang, possibly improving sleep.
The governor vessel is also closely related to the brain.
As stated in Su Wen, the governor vessel goes "up to
[the] forehead, reach [es] the top of [the] head, [the]
collateral brain." Baihui (GV 20) is located in the middle of the top of the head, which is at the intersection
of the governor vessel, the meridian of foot taiyang,
hand shaoyang, foot shaoyang, and foot jueyin. Ling
Shu says that the "brain is the sea of marrow, which
conveys up to the cover, down to Fengfu (GV 16)."
The cover in this context means Baihui (GV 20),
which has extensive contact with all parts of the body.
Sishencong (EX-HN 1), located 1 cun anterior, posteri-
DISCUSSION
In this study, we regulated defensive Qi and invigorated brain marrow using acupuncture and moxibustion
to treat insomnia. Compared with conventional methods, this method can improve sleep quality by adjusting the brain's sleep function, improving symptoms of
dreaminess, dizziness, headache, heavy head and poor
memory, and promoting the periodicity from light to
deep sleep. Traditional Chinese Medicine hypothesizes
that there is a close relationship between sleep and
wakefulness and defensive Qi movement in the body
with the alternation of day and night and the balance
of Yin and Yang heel vessels. Ling Shu that, "defensive
Qi moves in the Yang during the day, and Yin during
the night, as Yin corresponds to night, dominating
sleep people fall asleep when Yang Qi ends but Yin
Qi is grand, and vice versa Yin and Yang converge
with each other in the Yin and Yang heel vessels, Yang
joins Yin, Yin leaves Yang. As Yang reaches its limit, the
eyes open, and vice versa." That is, only when there is a
Table 3 Comparison of PSQI scores before and after treatment in two groups ( x s)
Item
Group
Before treatment
After treatment
Difference before and after treatment
Sleep quality
Control
2.40.7
1.00.8
1.60.9
Experiment
2.60.5
0.90.6
2.00.9d
Control
2.20.8
1.00.8a
1.20.9
Experiment
2.00.9
0.80.6ab
1.61.3d
Control
2.10.6
1.00.9a
1.20.7
Experiment
2.00.9
0.80.6
1.41.4d
Control
2.01.0
1.00.8a
1.10.9
Experiment
2.01.0
0.70.3ac
1.61.0d
Control
1.60.5
1.00.5a
0.60.6
Experiment
1.20.4
0.90.3
0.50.3d
Control
1.90.8
1.00.7a
1.20.8
Experiment
2.70.6
0.80.7
2.00.9d
Time to fall asleep
Sleeping time
Sleeping efficiency
Sleep disorder
Daytime function
ab
ac
ab
ab
t
1.19
0.98
0.70
1.77
1.76
2.85
Notes: experiment group were treated once a day with acupuncture at Baihui (GV 20), Sishencong (EX-HN 1), Shenmai (BL 62), and
Zhaohai (KI 6) and with moxibustion at Baihui (GV 20) and Sishencong (EX-HN 1); control group were acupunctured once a day at
Shenmen (HT 7), Neiguan (PC 6), and Sanyinjiao (SP 6). aP<0.01, compared with the data before and after treatment in the same group;
b
P<0.01, cP>0.05, compared with the data after treatment in the control group; dP<0.01, compared with the difference before and after
treatment in the control group.
JTCM | www. journaltcm. com
431
August 15, 2013 | Volume 33 | Issue 4 |
Gao XY et al. / Clinical Study
or and lateral to Baihui (GV 20), has two anterior
and posterior points that are both on the governor
vessel, and two lateral points that adjoin the bladder
meridian, which is collateral to the kidney. The meridian Qi communicates with the primary spirit,
calming the nerves and improving intelligence, reinforcing the brain and regulating the mind. Therefore,
it can promote sleep, uplift the spirit, and strengthen
memory.
5-HT, located at the head end of the raphe nucleus,
plays an important part in the maintenance of
slow-wave-sleep. The bodies of the 5-HT nerve cells
are mainly concentrated at the raphe nuclei. Therefore,
reducing the potency of 5-HT could advance sleep.
Studies have shown that moxibustion can protect the
hippocampal neurons of chronic stress rats, significantly improving the content of brain-derived neurotrophic factor. It can also significantly increase cerebral cortex 5-serotonin levels and its metabolite 5-hydroxyindoleacetic acid in presenium rats, and participate in the
signal transduction of the neurotrophic factor in the
brain. Therefore, moxibustion can resist insomnia, improve sleep quality, reduce awakening at night, reduce
sleep disorder, improve awakening, and ensure normal
functioning in daytime.
10
11
12
REFERENCES
1
13
Mental branch of Chinese Medical Association. Standard
for classifying and diagnosing mental disorder in China
(3rd edition). Jinan: Shandong Press of Science and Technology, 2001: 118-119.
Liu XC, Tang MQ, Hu L, et al. Research into confidence and efficiency of Pittsburgh sleeping quality indexes. Zhong Hua Jing Shen Ke Za Zhi 1996; 29(2):
103-107.
Health Ministry of People's Republic of China. Principle
on directing clinical research into new Chinese drugs. Beijing: Beijing People's Health Press, 1993: 186.
JTCM | www. journaltcm. com
14
15
432
Li XH, Han C, Zhang LF. Effect of moxibustion at point
Dazhui on expression of brain-derived neurotrophic factor
in chronic stress rats. Chin J of Clin Rehabi 2004; 8(1):
194-196.
Zhong L, Lan Q, Chen XL, Liao FZ, Tang Y. Influence of
electric moxibustion with drug on content of neurotransmitter of monoamine type in cerebral cortex of senile rats.
Zhong Guo Zhen Jiu 2004; 24(4): 275-278.
Zhang PL, Gao XY, Wei YL, et al. Multi-centered random control research into treatment of insomnia with acupuncture at Sishencong (EX-HN 1). Zhong Yi Za Zhi
2008; 49(8): 712-714.
Zhang SH, Fu WB. Experience in treating insomnia with
acupuncture and moxibustion. Zhong Yi Za Zhi 2011; 19
(10): 1692-1693.
Zhang Y, Wu XD. Analysis and countermeasure of insomnia factors. Shanxi Zhong Yi Xue Yuan Xue Bao 2002; 25
(5): 12-14.
He ZK. Application of acupuncture at Baihui (GV 20) to
treating diseases in brain. Zhong Yi Yao Dao Bao 2010; 16
(9): 116-117.
Ren S, Gao XY. Clinical research into optimized plan on
selecting acupoints for acupuncture to treat insomnia.
Zhong Yi Za Zhi 2009; 6(11): 46-47.
Ye RF. Assessment of insomnia. Zhong Guo Lin Chuang
Xin Li Xue Za Zhi 2004; 12(2): 207-208.
Yan XQ. Observations on curative effect of moxibustion
at Baihui (GV 20) on 49 patients with obstinate insomnia.
Zhen Jiu Lin Chuang Za Zhi 1999; 15(5): 37-38.
Zhou HQ, Gao XY. Clinical research into treatment of insomnia with moxibustion. Zhong Yi Xue Bao 2011; 26
(4): 505-506.
Zhang HZ, Jia CS, She YF. Clinical observations on treatment of obstinate insomnia with acupuncture mainly at
Zhaohai (KI 6) and Shenmai (BL 62). Sichuang Zhong Yi
2003; 21(6): 75-76.
Chen L, Sun LL, Wang X, Zhang FC. Research into modern articles on law governing acupoint selection for treatment of insomnia with acupuncture and moxibustion.
Zhong Yi Za Zhi 2012; 12(6): 1051-1054.
August 15, 2013 | Volume 33 | Issue 4 |
Das könnte Ihnen auch gefallen
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5795)
- Samkhya PhilosophyDokument1 SeiteSamkhya PhilosophyMadan KumarNoch keine Bewertungen
- MahayogamDokument2 SeitenMahayogamMadan KumarNoch keine Bewertungen
- Padmasana Siddhasana Simhasana Bhadrasana Swasthikasana Gomukasana VirasanaDokument1 SeitePadmasana Siddhasana Simhasana Bhadrasana Swasthikasana Gomukasana VirasanaMadan KumarNoch keine Bewertungen
- Varishtha Pension Bima Yojana Proposal Form - PDF 463333275Dokument5 SeitenVarishtha Pension Bima Yojana Proposal Form - PDF 463333275Madan Kumar50% (2)
- Procedure For Mud TherapyDokument3 SeitenProcedure For Mud TherapyMadan Kumar100% (1)
- Therapist Training ProgramDokument1 SeiteTherapist Training ProgramMadan KumarNoch keine Bewertungen
- Magneto Therapy NotesDokument5 SeitenMagneto Therapy NotesMadan Kumar100% (2)
- Acupuncture - An Anatomical Approach, Second EditionDokument250 SeitenAcupuncture - An Anatomical Approach, Second Editionlisa252Noch keine Bewertungen
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Adjective Clause Ilave Test (Tipdil)Dokument6 SeitenAdjective Clause Ilave Test (Tipdil)İlayda ErdoğanNoch keine Bewertungen
- Ubum FranchiseDokument77 SeitenUbum FranchiseShah PratikNoch keine Bewertungen
- Early Intervention Support and Inclusion For Children With Disability - ADHCDokument4 SeitenEarly Intervention Support and Inclusion For Children With Disability - ADHCMirolz PomenNoch keine Bewertungen
- 5 - Anemias Associated With Abnormal Heme SynthesisDokument24 Seiten5 - Anemias Associated With Abnormal Heme SynthesisSara BakerNoch keine Bewertungen
- Botany (Virus)Dokument48 SeitenBotany (Virus)Madhuri DeviNoch keine Bewertungen
- Visual Diagnosis and Traditional Chinese Medicine: Face Reading - What Your Face SaysDokument8 SeitenVisual Diagnosis and Traditional Chinese Medicine: Face Reading - What Your Face SaysTaniaNoch keine Bewertungen
- Notes On Maternal & Child Care (Pregnancy)Dokument3 SeitenNotes On Maternal & Child Care (Pregnancy)Oink TopusNoch keine Bewertungen
- Sample I-Search Paper: Living With AsthmaDokument7 SeitenSample I-Search Paper: Living With AsthmaputriNoch keine Bewertungen
- MCQ Internal MedicineDokument16 SeitenMCQ Internal Medicinemohamed mowafey100% (2)
- E360 Operating ManualDokument180 SeitenE360 Operating Manualpablo_ramirez_32Noch keine Bewertungen
- ANAPHY Lec Session #19 - SAS (Agdana, Nicole Ken)Dokument7 SeitenANAPHY Lec Session #19 - SAS (Agdana, Nicole Ken)Nicole Ken AgdanaNoch keine Bewertungen
- Exams MedsurgDokument29 SeitenExams MedsurgUy Jezrielle MicahNoch keine Bewertungen
- Introduction Clinical Pharmacology 9th Visovsky Test BankDokument6 SeitenIntroduction Clinical Pharmacology 9th Visovsky Test BanksonyaaaqNoch keine Bewertungen
- Meningococcemia: Neisseria Meningitidis - Is An EncapsulatedDokument19 SeitenMeningococcemia: Neisseria Meningitidis - Is An EncapsulatedcarolinecayasaNoch keine Bewertungen
- Pharmacotherapy of TuberculosisDokument31 SeitenPharmacotherapy of TuberculosisjabirNoch keine Bewertungen
- Diabetes Mellitus & HypertensionDokument12 SeitenDiabetes Mellitus & HypertensionMisbah KhanNoch keine Bewertungen
- Disfunctional Vascular Endothelium As A Driver of Atherosclerosis - Emergind Insights Into Pathogenesis and Treatment 2021Dokument18 SeitenDisfunctional Vascular Endothelium As A Driver of Atherosclerosis - Emergind Insights Into Pathogenesis and Treatment 2021Camila VidigalNoch keine Bewertungen
- G4 HealthDokument10 SeitenG4 HealthrinjoicecasilNoch keine Bewertungen
- Vaccine: Greg G. WolffDokument5 SeitenVaccine: Greg G. WolffRennan Lima M. CastroNoch keine Bewertungen
- Nursing Care Plan HyperthyroidismDokument2 SeitenNursing Care Plan Hyperthyroidismderic76% (17)
- Energy Balance WorksheetDokument3 SeitenEnergy Balance Worksheetsara wilsonNoch keine Bewertungen
- Teste de Proficiência Da Cultura Inglesa-SPDokument9 SeitenTeste de Proficiência Da Cultura Inglesa-SPLarissa AzevedoNoch keine Bewertungen
- Sex Linked Inheritance Pedigree 2016Dokument37 SeitenSex Linked Inheritance Pedigree 2016Krisburt Delos SantosNoch keine Bewertungen
- Sf8 Nutritional-Stat-Baseline 6 Pearl 2022Dokument8 SeitenSf8 Nutritional-Stat-Baseline 6 Pearl 2022Dante Maligsa BautistaNoch keine Bewertungen
- Living DonorDokument21 SeitenLiving DonorquecarajoqueresNoch keine Bewertungen
- Sweet DeathDokument5 SeitenSweet DeathJBNoch keine Bewertungen
- Carol Rivers'board Review FlashcardsDokument440 SeitenCarol Rivers'board Review FlashcardsJennelle CadoganNoch keine Bewertungen
- List of Important World International DaysDokument32 SeitenList of Important World International DaysYassir ButtNoch keine Bewertungen
- Food Poisoning N AMOEBIASIS - LECTUREDokument60 SeitenFood Poisoning N AMOEBIASIS - LECTUREpriyanka100% (1)
- Case Study Number FourDokument5 SeitenCase Study Number FourYessamin Paith RoderosNoch keine Bewertungen