Beruflich Dokumente
Kultur Dokumente
Pediatric Pneumonia Death Caused by Community-Acquired Methicillin - Resistant Staphylococcus Aureus, Japan
Hochgeladen von
M ZumrodinOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Pediatric Pneumonia Death Caused by Community-Acquired Methicillin - Resistant Staphylococcus Aureus, Japan
Hochgeladen von
M ZumrodinCopyright:
Verfügbare Formate
LETTERS
Pediatric
Pneumonia Death
Caused by
Communityacquired
MethicillinResistant
Staphylococcus
aureus, Japan
To the Editor: Community-acquired methicillin-resistant Staphylococcus aureus (CA-MRSA), which
carries genes for Panton-Valentine
leukocidin (PVL), has become a major
concern worldwide (13). CA-MRSA
is mainly associated with skin and soft
tissue infections in young, otherwise
healthy, persons in the community (3)
and also with life-threatening sepsis
and community-acquired pneumonia (preceded by influenza) (1,3,4).
The role of PVL in the pathogenesis
of staphylococcal infections is controversial. Whereas Labandeira-Rey
et al. (5) provided data that PVL, in
combination with staphylococcal
protein A, destroys respiratory tissue
and bacteria-engulfing immune cells,
Voyich et al. (6) and Bubeck Wardenburg et al. (7) showed that PVL was
not essential for the pathogenesis of
skin disease, sepsis, or pneumonia in
a mouse model.
Several types of CA-MRSA
clones exist, e.g., CA-MRSA belonging to multilocus sequence type (ST)
1 (called the USA400 clone) and ST8
(called the USA300 clone), which have
been major clones in North America
(recently, USA300 is becoming more
prominent); CA-MRSA belonging to
ST80, which has been a major clone in
Europe; and CA-MRSA belonging to
ST30, which is distributed worldwide,
including Japan (2,8). MRSA carrying
the PVL gene (a marker of CA-MRSA
[ST30]) comprises 0.1% of MRSA
isolated in hospitals in Japan (9).We
describe a fatal case of pediatric pneu1312
monia and septic shock from CA-MRSA in Japan.
A 16-month-old, previously
healthy boy was admitted to the hospital for fever and shortness of breath
on August 30, 2006. He had had coldlike symptoms for 14 days and fever
for the 2 previous days. On examination, hordeolum of the right eyelid and
cyanosis were observed; the patients
blood pressure was 106/ (undetectable) mm Hg, tachycardia 185 beats/
min, tachypnea 72 breaths/min, and
temperature 39.8C. He had bilateral
coarse breath sounds, and bronchovesicular breath sounds over the right
lung. Chest radiography indicated lobar consolidation and pleural effusion
on the right side. Laboratory analysis
showed leukocytopenia, thrombocytopenia, elevated C-reactive protein
level, and hypoxemia.
Intravenous administration of
sulbactam/ampicillin and cefotaxime,
and oxygen inhalation was started.
Oxygen saturation did not improve,
and laboratory values of disseminated
intravascular coagulation (DIC) were
observed: platelet count 121 K/mm3,
fibrinogen level 528 mg/dL, fibrin
degradation products 37.7 g/mL,
prothrombin time 1.86 international
normalized ratio, and D-dimer 37.7
g/mL. The condition was considered
septic shock, and consequently the boy
was transferred to the pediatric intensive care unit, where he required intubation and mechanical ventilation.
Sulbactam/ampicillin was switched
to meropenem, and cefotaxime was
continued. On day 2 after admission,
chest radiography showed bilateral
consolidation. On day 3, blood culture
yielded MRSA, and cefotaxime was
changed to vancomycin. Meropenem
therapy was continued to cover possible mixed bacterial infection. Immunoglobulin therapy and DIC syndrome
treatment (nafamostat mesilate, ulinastatin, freeze-dried concentrated human
antithrombin III) were also started.
On day 4, computed tomographic examination detected pneumothorax and
athelectasis. Because laboratory data
confirmed the presence of only MRSA,
meropenem was changed to flomoxef
(which belongs to the oxacephem family of -lactam antimicrobial agents)
on the expectation that a possible synergistic effect of flomoxef and vancomycin might occur. No major changes
occurred on days 5 and 6. On day 7, in
addition to bilateral infiltrates on chest
radiography, the oxygen index was 65
(partial pressure of arterial oxygen/
fraction of inspired oxygen), and the
patient was considered to have acute
respiratory distress syndrome. A percutaneous cardiopulmonary support
system (a portable heart-lung machine
that provides temporary circulatory
support) was used, but in spite of treatment, there was no improvement, and
the child died on day 10 after admission (September 8). An autopsy was
not performed.
Molecular characterization of
MRSA isolated from the blood was
performed as described previously
(8,9). Isolated MRSA (strain NN32)
was positive for PVL, belonging to
ST30:spa19:staphylococcal cassette
chromosome mec (SCCmec)IVa, and
was resistant to only -lactam antimicrobial agents (Table).
To date, all cases of PVL-positive
CA-MRSA infections officially reported in Japan were caused by strains belonging to ST30 (9). All these strains
can be classified into 2 types on the
basis of spa type (Table), for example,
ST30:spa19:SCCmecIVc. This type
includes strain NN1, isolated from an
11-month-old patient with bullous impetigo (8); strain NN12, isolated from a
17-year-old patient with cutaneous abscess/osteomyelitis (8); strain NN31,
isolated from an 18-year-old patient
with pelvic abscesses (9); and strain
EB00449, isolated from a 27-year-old
patient with cutaneous abscesses (9).
Another type is ST765 (single locus
variant of ST30):spa43:SCCmecIVx.
This type includes strain DB00319,
isolated from a 61-year-old hospital
inpatient (9).
Emerging Infectious Diseases www.cdc.gov/eid Vol. 14, No. 8, August 2008
LETTERS
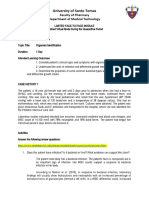
Table. Characteristics of PVL-positive MRSA strains reported in Japan since 2000*
Type, gene, or resistance
Types
CC
ST
spa
agr
SCCmec
Coagulase
Toxins
Leukocidins
Hemolysins
Staphylococcal enterotoxins
Exfoliative toxins
Others
Present strain
NN32
30
30
19
3
IVa
IV
PVL-positive MRSA
Previous strains
NN1
NN12, NN31
EB 00449
30
30
30
30
30
30
19
19
19
3
3
3
IVc
IVc
IVc
IV
IV
IV
DB 00319
30
765
43
3
IVx*
IV
lukS-PV, lukF-PV
lukE-lukD, lukM
hla, hlg, hld
hlb
hlgv
sea
tst, seb, sec,
sed, see, seh,
sej, sek, sep
egc
seu
eta, etb, etd
set
edin
+
+
+
+
+
+
+
+
+
+
+
+
icaA, sdrD, sdrE
icaD, cna,
eno, fnbA,
fnbB, ebpS,
clfA, clfB, fib,
sdrC, bbp
Aminoglycosides
Adhesins
Drug resistance and
penicillinase plasmid
Macrolides
Lincosamides
Tetracycline
Penicillinase plasmid
(kb)
GEN#
KAN#*
+
(33)
+
(33)
TET#
+
(33)
GEN**
KAN**
STR**
ERY**
CLI**
+
(33)
+
(40)**
*PVL, Panton-Valentine leukocidin; MRSA, methicillin-resistant Staphylococcus aureus; SCCmec IVx, staphylococcal cassette chromosome mec type IV
with unknown subtypes; +, positive; , negative; GEN, gentamicin; KAN, kanamycin; STR, streptomycin; ERY, erythromycin; CLI, clindamycin; TET,
tetracycline.
GenBank accession nos. for the PVL gene sequences from strains NN32 and NN1 are AB286959 and AB186917, respectively.
egc, enterotoxin gene cluster, including seg, sei, sem, sen, and seo genes.
cna, gene encoding for collagen binding protein (adhesin).
bbp, gene encoding for bone sialoprotein binding protein (adhesin).
#Drug resistance encoded by a conjugative drug resistance plasmid (pGKT1) (8).
**Multidrug-resistant penicillinase plasmid encoding for resistance to GEN, KAN, STR, ERY, and CLI, in addition to penicillin resistance (9).
The molecular characteristics of
strain NN32 were similar to those of
strain NN1, except for SCCmecIV subtypes (Table). Moreover, pulsed-field
gel electrophoresis patterns (data not
shown) and the PVL gene sequences
of the 2 strains (NN32 and NN1) were
identical (Table).
This case of CA-MRSA ST30 infection in a child represents a progression from common coldlike symp-
toms (occurring outside the influenza
season) to fatal pneumonia, despite
intensive therapy, including the administration of sensitive antimicrobial
agents. CA-MRSA ST30 contains several genes that mediate adhesion (e.g.,
cna and bbp) and toxin genes (PVL
and egc, which encode for at least 5
superantigens, including staphylococcal enterotoxin G, I, M, N, and O).
The gene cluster egc is associated
with septic shock (10). Further studies
are needed to clarify the pathogenesis
of community-acquired pneumonia
caused by CA-MRSA.
Acknowledgments
We thank Yasuhisa Ueda, Yuki Bando, and Keisuke Sunagawa for clinical
suggestions and Wataru Higuchi, Hirokazu Isobe, Soshi Dohmae, Hassan Zaraket,
Shizuka Yabe, Misao Takano, and Kyoko
Ozaki for technical assistance.
Emerging Infectious Diseases www.cdc.gov/eid Vol. 14, No. 8, August 2008
1313
LETTERS
This study was supported by a grant
from the Japan Science and Technology
Agency, Japan.
Takashi Ito,* Makiko Iijima,*
Takayoshi Fukushima,*
Masato Nonoyama,*
Masahiro Ishii,*
Tatiana Baranovich,
Taketo Otsuka,
Tomomi Takano,
and Tatsuo Yamamoto
*Kitasato University School of Medicine,
Kanagawa, Japan; and Niigata University Graduate School of Medical and Dental
Sciences, Niigata, Japan
DOI: 10.3201/eid1408.070391
References
1.
2.
3.
4.
5.
6.
7.
1314
Centers for Disease Control and Prevention. Four pediatric deaths from
community-acquired methicillin-resistant
Staphylococcus aureusMinnesota and
North Dakota, 19971999. JAMA.
1999;282:11235. DOI: 10.1001/jama.
282.12.1123
Tristan A, Bes M, Meugnier H, Lina G,
Bozdogan B, Courvalin P, et al. Global
distribution of Panton-Valentine leukocidinpositive methicillin-resistant Staphylococcus aureus, 2006. Emerg Infect Dis.
2007;13:594600.
Zetola N, Francis JS, Nuermberger EL,
Bishai WR. Community-acquired methicillin-resistant Staphylococcus aureus:
an emerging threat. Lancet Infect Dis.
2005;5:27586. DOI: 10.1016/S14733099(05)70112-2
Hageman JC, Uyeki TM, Francis JS,
Jernigan DB, Wheeler JG, Bridges CB,
et al. Severe community-acquired pneumonia due to Staphylococcus aureus,
200304 influenza season. Emerg Infect
Dis. 2006;12:8949.
Labandeira-Rey M, Couzon F, Boisset
S, Brown EL, Bes M, Benito Y, et al.
Staphylococcus aureus Panton-Valentine
leukocidin causes necrotizing pneumonia.
Science. 2007;315:11303. DOI: 10.1126/
science.1137165
Voyich JM, Otto M, Mathema B, Braughton KR, Whitney AR, Welty D, et al. Is
Panton-Valentine leukocidin the major
virulence determinant in communityassociated methicillin-resistant Staphylococcus aureus disease? J Infect Dis.
2006;194:176170. DOI: 10.1086/509506
Bubeck Wardenburg J, Bae T, Otto M, Deleo FR, Schneewind O. Poring over pores:
alpha-hemolysin and Panton-Valentine
leukocidin in Staphylococcus aureus
pneumonia. Nat Med. 2007;13:14056.
DOI: 10.1038/nm1207-1405
8. Takizawa Y, Taneike I, Nakagawa S, Oishi
T, Nitahara Y, Iwakura N, et al. A Panton-Valentine leucocidin (PVL)-positive
community-acquired methicillin-resistant
Staphylococcus aureus (MRSA) strain, another such strain carrying a multiple-drug
resistance plasmid, and other more-typical
PVL-negative MRSA strains found in Japan. J Clin Microbiol. 2005;43:335663.
DOI: 10.1128/JCM.43.7.3356-3363.2005
9. Yamamoto T, Dohmae S, Saito K, Otsuka
T, Takano T, Chiba M, et al. Molecular
characteristics and in vitro susceptibility
to antimicrobial agents, including the desfluoro(6) quinolone DX-619, of PantonValentine leucocidin-positive methicillinresistant Staphylococcus aureus isolates
from the community and hospitals. Antimicrob Agents Chemother. 2006;50:4077
86. DOI: 10.1128/AAC.00847-06
10. Ferry T, Thomas D, Genestier AL, Bes
M, Lina G, Vandenesch F, et al. Comparative prevalence of superantigen genes
in Staphylococcus aureus isolates causing sepsis with and without septic shock.
Clin Infect Dis. 2005;41:7717. DOI:
10.1086/432798
Address for correspondence: Tatsuo Yamamoto,
Division of Bacteriology, Department of
Infectious Disease Control and International
Medicine, Niigata University Graduate
School of Medical and Dental Sciences, 757
Ichibanchou, Asahimachidori, Niigata, Japan;
email: tatsuoy@med.niigata-u.ac.jp
Letters
Letters commenting on recent
articles as well as letters reporting cases, outbreaks, or original
research are welcome. Letters
commenting on articles should
contain no more than 300 words
and 5 references; they are more
likely to be published if submitted
within 4 weeks of the original articles publication. Letters reporting cases, outbreaks, or original
research should contain no more
than 800 words and 10 references.
They may have one Figure or Table and should not be divided into
sections. All letters should contain
material not previously published
and include a word count.
Rarity of Influenza
A Virus in Spring
Shorebirds,
Southern Alaska
To the Editor: Knowledge of
avian influenza (AI) virus and its host
epidemiology and ecology is essential
for effective monitoring and mitigation (1). Applicability of global and
continental-scale models will be key
for expanding this knowledge base.
Research in the Delaware Bay area,
eastern United States, suggests an
ecologic and epidemiologic viewpoint
of AI virus in wild birds in which
shorebirds (family Scolopacidae) are
predominant hosts in spring; however,
research in Alberta, Canada, suggests
that waterfowl are such in autumn
(2,3). AI virus surveillance in Europe
(4) suggests that the spring aspect of
this scenario does not apply there. To
increase knowledge of AI transport
among shorebirds in spring in the
North Pacific, we conducted AI virus
surveillance during the springs of 2006
and 2007 at the Copper River Delta
area of Alaska. Millions of birds congregate at this location in the spring,
resulting in the highest spring shorebird concentrations in the New World
(5). We also sampled gulls (Laridae),
which are common and heretofore unsurveyed for AI in this ecosystem.
In 2006 and 2007, 1,050 shorebirds
(Western Sandpiper, Calidris mauri,
and Least Sandpiper, C. minutilla) and
770 Glaucous-winged Gulls (Larus
glaucescens) were sampled during peak
spring migration at Hartney Bay, Cordova, Alaska (6028N 1468W; Table). Fresh fecal samples were obtained
from tidal flats within <1 to 90 min after identified flocks were dispersed, and
samples were placed in sterile medium
(brain heart infusion buffer with 10,000
U/mL penicillin G, 1 mg/mL gentamicin, and 20 g/mL amphotericin B) and
either kept cool (<1 week) before transport to Fairbanks (2006) or placed into
liquid nitrogen within 2 h of collection
Emerging Infectious Diseases www.cdc.gov/eid Vol. 14, No. 8, August 2008
Das könnte Ihnen auch gefallen
- Non-inflammatory immunology: An introduction to the immune system and its pathologiesVon EverandNon-inflammatory immunology: An introduction to the immune system and its pathologiesNoch keine Bewertungen
- Toxic Shock SyndromeDokument13 SeitenToxic Shock SyndromeSrinivas PingaliNoch keine Bewertungen
- Orchitis: A Complication of Severe Acute Respiratory Syndrome (SARS)Dokument7 SeitenOrchitis: A Complication of Severe Acute Respiratory Syndrome (SARS)Arisa RosyadaNoch keine Bewertungen
- 26 Mip CC 29 Teodor Andra C 808-811Dokument4 Seiten26 Mip CC 29 Teodor Andra C 808-811ana2693Noch keine Bewertungen
- 58 1454-18Dokument7 Seiten58 1454-18overmegaNoch keine Bewertungen
- F - CMCRep 1 Assy Et Al - 1405Dokument2 SeitenF - CMCRep 1 Assy Et Al - 1405faegrerh5ju75yu34yNoch keine Bewertungen
- 38 10 1498 PDFDokument5 Seiten38 10 1498 PDFGilbert MenesesNoch keine Bewertungen
- Journal of Infection and Chemotherapy: SciencedirectDokument4 SeitenJournal of Infection and Chemotherapy: SciencedirectRaodatul IstiharohNoch keine Bewertungen
- Inhibition of Bruton Tyrosine Kinase in Patients With Severe COVID-19Dokument19 SeitenInhibition of Bruton Tyrosine Kinase in Patients With Severe COVID-19ANoch keine Bewertungen
- SJMCR-57438-440Dokument3 SeitenSJMCR-57438-440Dwi PascawitasariNoch keine Bewertungen
- Elderly PneumoniaDokument10 SeitenElderly PneumoniaFayne ConaderaNoch keine Bewertungen
- Science Abe4832 FullDokument20 SeitenScience Abe4832 FullsussanNoch keine Bewertungen
- Staphylococcal Toxic Shock Syndrome: M Kare, A DangDokument3 SeitenStaphylococcal Toxic Shock Syndrome: M Kare, A DangAnonymous ALlIo2LNoch keine Bewertungen
- Biomed ..Dokument10 SeitenBiomed ..Romina Molette GonzalesNoch keine Bewertungen
- Elizabeth King I ADokument3 SeitenElizabeth King I AAlba UrbinaNoch keine Bewertungen
- Typhoid Fever Epidemiology and Treatment Outcomes in ChinaDokument17 SeitenTyphoid Fever Epidemiology and Treatment Outcomes in ChinaRafif Abdurrahman WijisaksonoNoch keine Bewertungen
- Disseminated Multifocal Tuberculosis An Unusual Presentation With Macrophagic Activation SyndromeDokument5 SeitenDisseminated Multifocal Tuberculosis An Unusual Presentation With Macrophagic Activation SyndromeInternational Journal of Innovative Science and Research TechnologyNoch keine Bewertungen
- Vol 3. Issue 3Dokument43 SeitenVol 3. Issue 3Diana MargaretaNoch keine Bewertungen
- Adult Still's Disease and Respiratory Failure in A 74 Year Old WomanDokument3 SeitenAdult Still's Disease and Respiratory Failure in A 74 Year Old WomanEduardo Romero StéfaniNoch keine Bewertungen
- New-Onset Diabetes in Covid-19: Eloise Baudou, M.D. Anne Lespine, PH.DDokument3 SeitenNew-Onset Diabetes in Covid-19: Eloise Baudou, M.D. Anne Lespine, PH.DMaya Indri LaraswatiNoch keine Bewertungen
- Pneumonia Thesis StatementDokument9 SeitenPneumonia Thesis StatementCollegePapersHelpUK100% (2)
- Delay in Diagnosis of Extra-Pulmonary Tuberculosis by Its Rare Manifestations: A Case ReportDokument5 SeitenDelay in Diagnosis of Extra-Pulmonary Tuberculosis by Its Rare Manifestations: A Case ReportSneeze LouderNoch keine Bewertungen
- MRSADokument7 SeitenMRSAronald marbunNoch keine Bewertungen
- Systemic Inflammatory Response Syndrome (SIRS) & Sepsis: Dr.H.Asril Zahari SP.B.KBDDokument43 SeitenSystemic Inflammatory Response Syndrome (SIRS) & Sepsis: Dr.H.Asril Zahari SP.B.KBDPark ji SangNoch keine Bewertungen
- Case Report: Streptococcus AnginosusDokument4 SeitenCase Report: Streptococcus AnginosusIesanu MaraNoch keine Bewertungen
- Accepted Manuscript: Journal of Critical CareDokument28 SeitenAccepted Manuscript: Journal of Critical CareSyawaluddin sakti maulanaNoch keine Bewertungen
- A Clinical Study On Extrapulmonary TuberculosiDokument10 SeitenA Clinical Study On Extrapulmonary TuberculosinayemamasruraNoch keine Bewertungen
- Pulmonary Tuberculosis Literature ReviewDokument5 SeitenPulmonary Tuberculosis Literature Reviewafdtvwccj100% (1)
- s15010 023 02142 4Dokument29 Seitens15010 023 02142 4denemebakalim72Noch keine Bewertungen
- cc11046 PDFDokument189 Seitencc11046 PDFNurfadhilah YusufNoch keine Bewertungen
- Elife 77345 v1Dokument48 SeitenElife 77345 v1Afandi CharlesNoch keine Bewertungen
- J Clin Pathol 1980 Brook 1099 101Dokument4 SeitenJ Clin Pathol 1980 Brook 1099 101ysh_girlNoch keine Bewertungen
- A Rare Cause of Endocarditis: Streptococcus PyogenesDokument3 SeitenA Rare Cause of Endocarditis: Streptococcus PyogenesYusuf BrilliantNoch keine Bewertungen
- 1 - Science 2020 - Deep Immune Profiling of COVID-19 PatientsDokument29 Seiten1 - Science 2020 - Deep Immune Profiling of COVID-19 PatientsGabrielaNoch keine Bewertungen
- Omi 2017 0070Dokument13 SeitenOmi 2017 0070Heldrian dwinanda SuyuthieNoch keine Bewertungen
- Physiological Reports - 2024 - Theotonio Dos Santos - Antimicrobial Peptides and Other Potential Biomarkers of Critical IllnessDokument12 SeitenPhysiological Reports - 2024 - Theotonio Dos Santos - Antimicrobial Peptides and Other Potential Biomarkers of Critical IllnessLucas TheotonioNoch keine Bewertungen
- Sepsis Update 2011 PDFDokument10 SeitenSepsis Update 2011 PDFIndahK.WardhaniPutriNoch keine Bewertungen
- Jurnal Microsatelit 4Dokument5 SeitenJurnal Microsatelit 4Ieien MuthmainnahNoch keine Bewertungen
- Sepsis and Septic Shock - Critical Care MedicineDokument2 SeitenSepsis and Septic Shock - Critical Care MedicineMihaela MoraruNoch keine Bewertungen
- Organism ID & Types of ShockDokument5 SeitenOrganism ID & Types of ShockAdrian BrillantesNoch keine Bewertungen
- Seq Exercise: By: Dr. Mohammad Saad Abdul-MajidDokument27 SeitenSeq Exercise: By: Dr. Mohammad Saad Abdul-MajidKalichandren ArumugamNoch keine Bewertungen
- Lancet - Septic Shock (Seminars)Dokument16 SeitenLancet - Septic Shock (Seminars)williamsbarriosNoch keine Bewertungen
- Scientific Letters: WWW - Elsevier.es/eimcDokument2 SeitenScientific Letters: WWW - Elsevier.es/eimcfeby1992Noch keine Bewertungen
- Pulmonary Tuberculosis Presenting with ARDSDokument5 SeitenPulmonary Tuberculosis Presenting with ARDSCimol AgustinaNoch keine Bewertungen
- Streptococcus Group A InfectionsDokument13 SeitenStreptococcus Group A InfectionsLidia GotoYourhappyplaceNoch keine Bewertungen
- Apoptosis StxDokument7 SeitenApoptosis StxKarina Fischer SigelNoch keine Bewertungen
- Ijam-3775 CDokument3 SeitenIjam-3775 Carunkumar kumararunNoch keine Bewertungen
- Jurnal PilihanDokument7 SeitenJurnal PilihanNovia khasanahNoch keine Bewertungen
- Presepsin 6Dokument189 SeitenPresepsin 6donkeyendutNoch keine Bewertungen
- Stem Cell Exosomes Show Promise for Treating Severe COVID-19Dokument8 SeitenStem Cell Exosomes Show Promise for Treating Severe COVID-19Alejandro Andrés Salazar GuzmánNoch keine Bewertungen
- Cytokine Storm and Leukocyte Changes in Mild Versus SevereDokument25 SeitenCytokine Storm and Leukocyte Changes in Mild Versus SevereRaffaharianggaraNoch keine Bewertungen
- Rhizomucor Scedosporium: Case ReportDokument6 SeitenRhizomucor Scedosporium: Case ReportPaul ColburnNoch keine Bewertungen
- Endogenous Mediators in Sepsis and Septic Shock: A. Beishuizen, Vecmes, and C. HaanenDokument77 SeitenEndogenous Mediators in Sepsis and Septic Shock: A. Beishuizen, Vecmes, and C. HaanenAlexandra DobriţaNoch keine Bewertungen
- SepsisDokument36 SeitenSepsisWan FaizuddinNoch keine Bewertungen
- Streptococcal Tonsillitis As A Cause of Urticaria Tonsillitis and UrticariaDokument5 SeitenStreptococcal Tonsillitis As A Cause of Urticaria Tonsillitis and UrticariasDamnNoch keine Bewertungen
- Management of Brain AbscessesDokument10 SeitenManagement of Brain AbscessesAnonymous 9dVZCnTXSNoch keine Bewertungen
- Cronobacter Sakazakii in Adults - A Rare Case Report.Dokument4 SeitenCronobacter Sakazakii in Adults - A Rare Case Report.International Organization of Scientific Research (IOSR)Noch keine Bewertungen
- tmp6899 TMPDokument12 Seitentmp6899 TMPFrontiersNoch keine Bewertungen
- Clinical ImmunologyDokument5 SeitenClinical ImmunologyiuventasNoch keine Bewertungen
- Sans titre (1)Dokument9 SeitenSans titre (1)rollinpeguyNoch keine Bewertungen
- Ncbi PDFDokument13 SeitenNcbi PDFM ZumrodinNoch keine Bewertungen
- The UKPDS Risk Engine: A Model For The Risk of Coronary Heart Disease in Type II Diabetes (UKPDS 56)Dokument9 SeitenThe UKPDS Risk Engine: A Model For The Risk of Coronary Heart Disease in Type II Diabetes (UKPDS 56)M ZumrodinNoch keine Bewertungen
- Ncbi PDFDokument13 SeitenNcbi PDFM ZumrodinNoch keine Bewertungen
- Afp PDFDokument8 SeitenAfp PDFM ZumrodinNoch keine Bewertungen
- From Cytokines To TLR and Beyond Current Knowledge and Future Research Needs in BSDokument11 SeitenFrom Cytokines To TLR and Beyond Current Knowledge and Future Research Needs in BSOscar RodriguezNoch keine Bewertungen
- Pediatric Pneumonia Death Caused by Community-Acquired Methicillin - Resistant Staphylococcus Aureus, JapanDokument3 SeitenPediatric Pneumonia Death Caused by Community-Acquired Methicillin - Resistant Staphylococcus Aureus, JapanM ZumrodinNoch keine Bewertungen
- Delay Umbilical 2Dokument6 SeitenDelay Umbilical 2Sisrini Rahayu SammarianNoch keine Bewertungen
- 16-31-1-SM Widiastuti 2014Dokument5 Seiten16-31-1-SM Widiastuti 2014M ZumrodinNoch keine Bewertungen
- S10 1 FullDokument1 SeiteS10 1 FullM ZumrodinNoch keine Bewertungen
- Kaji Ulang Status Gizi Anak 0-59 Bulan AtmaritaDokument16 SeitenKaji Ulang Status Gizi Anak 0-59 Bulan AtmaritaM ZumrodinNoch keine Bewertungen
- Acne VulgarisDokument5 SeitenAcne VulgarisM ZumrodinNoch keine Bewertungen
- Hydrocele Dan SpermatoceleDokument1 SeiteHydrocele Dan SpermatoceleM ZumrodinNoch keine Bewertungen
- JNC 7 ShortDokument14 SeitenJNC 7 ShortFeigan SimarmataNoch keine Bewertungen
- Emerg Medicine For Rural Hospital 2015 BrochureDokument12 SeitenEmerg Medicine For Rural Hospital 2015 BrochureM ZumrodinNoch keine Bewertungen
- Faktor-Faktor Yang Berhubungan Dengan HB0 PDFDokument7 SeitenFaktor-Faktor Yang Berhubungan Dengan HB0 PDFM ZumrodinNoch keine Bewertungen
- Analisis Kebutuhan Dan Selera Balita Terhadap Pemberian Makanan Tambahan Mp-Asi Pada Balita Bawah Garis Merah Di Puskesmas Indralaya TAHUN 2014Dokument15 SeitenAnalisis Kebutuhan Dan Selera Balita Terhadap Pemberian Makanan Tambahan Mp-Asi Pada Balita Bawah Garis Merah Di Puskesmas Indralaya TAHUN 2014M ZumrodinNoch keine Bewertungen
- J Neurol Neurosurg Psychiatry 2001 Kuwabara 560 2Dokument4 SeitenJ Neurol Neurosurg Psychiatry 2001 Kuwabara 560 2M ZumrodinNoch keine Bewertungen
- SpermatoceleDokument2 SeitenSpermatocelemrizkidm2301Noch keine Bewertungen
- Tufts Opencourseware The Pathophysiology of HypertensionDokument10 SeitenTufts Opencourseware The Pathophysiology of HypertensionaddicaNoch keine Bewertungen
- Cefixime 25may2008Dokument2 SeitenCefixime 25may2008M ZumrodinNoch keine Bewertungen
- SpermatoceleDokument3 SeitenSpermatoceleM ZumrodinNoch keine Bewertungen
- DEPKES RI NEW Pedoman Nasional Penanggulangan TBC 2011Dokument110 SeitenDEPKES RI NEW Pedoman Nasional Penanggulangan TBC 2011familyman8091% (11)
- Acne VulgarisDokument5 SeitenAcne VulgarisM ZumrodinNoch keine Bewertungen
- Tool BoxDokument44 SeitenTool BoxM ZumrodinNoch keine Bewertungen
- Double Unders MasteryDokument13 SeitenDouble Unders MasterySebastian Hurtado100% (2)
- E PortfolioDokument3 SeitenE Portfolioapi-337945337Noch keine Bewertungen
- Understand Glaucoma: Causes, Diagnosis and TreatmentDokument57 SeitenUnderstand Glaucoma: Causes, Diagnosis and TreatmentDarshan SinghNoch keine Bewertungen
- Ananda Zaren - Core Elements of The Materia Medica of The Mind - Vol IDokument101 SeitenAnanda Zaren - Core Elements of The Materia Medica of The Mind - Vol Ialex100% (2)
- Biochem 2 Chapter 1Dokument19 SeitenBiochem 2 Chapter 1Suzaila's SyfaNoch keine Bewertungen
- Understanding Cholesterol Levels and Risks: A Guide to Lipid ProfilesDokument48 SeitenUnderstanding Cholesterol Levels and Risks: A Guide to Lipid ProfilesAnonymous o3Q3QXENoch keine Bewertungen
- The Impact of Life Cycles on Family HealthDokument27 SeitenThe Impact of Life Cycles on Family Healthmarcial_745578124Noch keine Bewertungen
- Understanding Contraceptive Knowledge and Practices Among Breastfeeding WomenDokument286 SeitenUnderstanding Contraceptive Knowledge and Practices Among Breastfeeding WomenAastha JainNoch keine Bewertungen
- Nutritional Care in Respiratory Disease: DR Haerani Rasyid, Mkes, SPPD, K-GHDokument94 SeitenNutritional Care in Respiratory Disease: DR Haerani Rasyid, Mkes, SPPD, K-GHDesywinNoch keine Bewertungen
- Single Best Answer Question-Writing Tips For Clinicians: J L Walsh, B H L Harris, P E SmithDokument6 SeitenSingle Best Answer Question-Writing Tips For Clinicians: J L Walsh, B H L Harris, P E SmithSandro ToninNoch keine Bewertungen
- Annual Health Checkup (Executive) : Package Amt. Package Actual AmtDokument1 SeiteAnnual Health Checkup (Executive) : Package Amt. Package Actual AmtPAWAN KUMARNoch keine Bewertungen
- 2006 Human and Developmental Toxicology - D. Bellinger (Informa, 2006) WW PDFDokument555 Seiten2006 Human and Developmental Toxicology - D. Bellinger (Informa, 2006) WW PDFGiovana BarbosaNoch keine Bewertungen
- Internet Book of Critical Care (IBCC) : Rapid ReferenceDokument1 SeiteInternet Book of Critical Care (IBCC) : Rapid Referenceian porterNoch keine Bewertungen
- Slides 6 - ObturationDokument22 SeitenSlides 6 - Obturationبراءة أحمد السلاماتNoch keine Bewertungen
- PMO - Pasteurized Milk OrdinanceDokument340 SeitenPMO - Pasteurized Milk OrdinanceTato G.k.Noch keine Bewertungen
- Managing Fatigue During PregnancyDokument2 SeitenManaging Fatigue During PregnancyBlanz Irybelle KindomNoch keine Bewertungen
- Types of Feeding TubesDokument8 SeitenTypes of Feeding TubesElda KuizonNoch keine Bewertungen
- Dehorning DisbuddingDokument4 SeitenDehorning DisbuddingAnca AnghelescuNoch keine Bewertungen
- Soal Tes TOEFL Dan Pembahasan Jawaban Written Expression (Complete Test 2 by Longman)Dokument23 SeitenSoal Tes TOEFL Dan Pembahasan Jawaban Written Expression (Complete Test 2 by Longman)Prakoso JatiNoch keine Bewertungen
- JKNKLKLDokument10 SeitenJKNKLKLCyntia AndrinaNoch keine Bewertungen
- Hipospadia, PPT Blok 3.1 (English)Dokument11 SeitenHipospadia, PPT Blok 3.1 (English)weniNoch keine Bewertungen
- 2 1 1000Dokument100 Seiten2 1 1000Dr-Mohammed AdelNoch keine Bewertungen
- MOH Corporate Plan 2022 - 2025Dokument159 SeitenMOH Corporate Plan 2022 - 2025M MNoch keine Bewertungen
- Neuromuscular Facilitation Techniques: Miss Rojaramani Vasamshetty MPT Ii YrDokument24 SeitenNeuromuscular Facilitation Techniques: Miss Rojaramani Vasamshetty MPT Ii YrdeepuphysioNoch keine Bewertungen
- Dagim Firide YimenuDokument138 SeitenDagim Firide Yimenugemu deribaNoch keine Bewertungen
- Boaz Gobera (NsambyaHospitalReport2021)Dokument62 SeitenBoaz Gobera (NsambyaHospitalReport2021)GOBERA BOAZNoch keine Bewertungen
- Health Promotion and Primary Health CareDokument51 SeitenHealth Promotion and Primary Health CareBhawna JoshiNoch keine Bewertungen
- GinaDokument59 SeitenGinasigitNoch keine Bewertungen
- Poodle Papers Spring 2004Dokument36 SeitenPoodle Papers Spring 2004PCA_website100% (6)
- Hendra - EKGDokument34 SeitenHendra - EKGRINANoch keine Bewertungen
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionVon EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionBewertung: 4 von 5 Sternen4/5 (402)
- The Age of Magical Overthinking: Notes on Modern IrrationalityVon EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityBewertung: 4 von 5 Sternen4/5 (13)
- How to Talk to Anyone: Learn the Secrets of Good Communication and the Little Tricks for Big Success in RelationshipVon EverandHow to Talk to Anyone: Learn the Secrets of Good Communication and the Little Tricks for Big Success in RelationshipBewertung: 4.5 von 5 Sternen4.5/5 (1135)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsVon EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsBewertung: 3.5 von 5 Sternen3.5/5 (3)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeVon EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeNoch keine Bewertungen
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsVon EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsNoch keine Bewertungen
- Breaking the Habit of Being YourselfVon EverandBreaking the Habit of Being YourselfBewertung: 4.5 von 5 Sternen4.5/5 (1454)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsVon EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsBewertung: 4.5 von 5 Sternen4.5/5 (169)
- Why We Die: The New Science of Aging and the Quest for ImmortalityVon EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityBewertung: 3.5 von 5 Sternen3.5/5 (2)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedVon EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedBewertung: 5 von 5 Sternen5/5 (78)
- The Comfort of Crows: A Backyard YearVon EverandThe Comfort of Crows: A Backyard YearBewertung: 4.5 von 5 Sternen4.5/5 (23)
- Deep Sleep Hypnosis: Guided Meditation For Sleep & HealingVon EverandDeep Sleep Hypnosis: Guided Meditation For Sleep & HealingBewertung: 4.5 von 5 Sternen4.5/5 (103)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisVon EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisBewertung: 4 von 5 Sternen4/5 (1)
- The Ultimate Guide To Memory Improvement TechniquesVon EverandThe Ultimate Guide To Memory Improvement TechniquesBewertung: 5 von 5 Sternen5/5 (34)
- The Obesity Code: Unlocking the Secrets of Weight LossVon EverandThe Obesity Code: Unlocking the Secrets of Weight LossBewertung: 5 von 5 Sternen5/5 (3)
- Techniques Exercises And Tricks For Memory ImprovementVon EverandTechniques Exercises And Tricks For Memory ImprovementBewertung: 4.5 von 5 Sternen4.5/5 (40)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessVon EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessBewertung: 4.5 von 5 Sternen4.5/5 (327)
- The Happiness Trap: How to Stop Struggling and Start LivingVon EverandThe Happiness Trap: How to Stop Struggling and Start LivingBewertung: 4 von 5 Sternen4/5 (1)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingVon EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingBewertung: 5 von 5 Sternen5/5 (4)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingVon EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingBewertung: 3.5 von 5 Sternen3.5/5 (31)
- The Tennis Partner: A Doctor's Story of Friendship and LossVon EverandThe Tennis Partner: A Doctor's Story of Friendship and LossBewertung: 4.5 von 5 Sternen4.5/5 (4)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaVon EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- The Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsVon EverandThe Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsNoch keine Bewertungen