Beruflich Dokumente
Kultur Dokumente
Exercise. Impaired Sympathetic Vascular Regulation in Humans After Acute Dynamic
Hochgeladen von
nyuwwchocolavaOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Exercise. Impaired Sympathetic Vascular Regulation in Humans After Acute Dynamic
Hochgeladen von
nyuwwchocolavaCopyright:
Verfügbare Formate
Impaired sympathetic vascular regulation in humans after acute dynamic
exercise.
J R Halliwill, J A Taylor and D L Eckberg
J. Physiol. 1996;495;279-288
This information is current as of September 9, 2007
This is the final published version of this article; it is available at:
http://jp.physoc.org/cgi/content/abstract/495/Pt_1/279
This version of the article may not be posted on a public website for 12 months after
publication unless article is open access.
The Journal of Physiology Online is the official journal of The Physiological Society. It has
been published continuously since 1878. To subscribe to The Journal of Physiology Online go
to: http://jp.physoc.org/subscriptions/. The Journal of Physiology Online articles are free 12
months after publication. No part of this article may be reproduced without the permission of
Blackwell Publishing: JournalsRights@oxon.blackwellpublishing.com
Downloaded from jp.physoc.org by on September 9, 2007
Journal of Physiology (1996), 495.1, pp.279-288
52130
279
Impaired sympathetic vascular regulation in humans after
acute dynamic exercise
John R. Halliwill *, J. Andrew Taylor t and Dwain L. Eckberg t
TDepartments of Physiology and Medicine, Medical College of Virginia and Hunter
Holmes MfcGuire Department of Veterans Affairs Medical Center, Richmond, VA 23249,
*Department of Anesthesiology, Division of Research, Mayo Clinic and Foundation,
200 1st Street SW, Rochester, MN 55905 and tHebrew Rehabilitation
Centre for Aged, Beth Israel Hospital, and Harvard Medical School,
Division on Aging, Boston, MA 02131-1097, USA
1.
2.
3.
4.
The reduction in vascular resistance which accompanies acute dynamic exercise does not
subside immediately during recovery, resulting in a post-exercise hypotension. This sustained
vasodilatation suggests that sympathetic vascular regulation is altered after exercise.
Therefore, we assessed the baroreflex control of sympathetic outflow in response to arterial
pressure changes, and transduction of sympathetic activity into vascular resistance during a
sympatho-excitatory stimulus (isometric handgrip exercise) after either exercise (60 min
cycling at 60 % peak aerobic power (V02 peak)) or sham treatment (60 min seated rest) in nine
healthy subjects.
Both muscle sympathetic nerve activity and calf vascular resistance were reduced after
exercise (-29-7 + 8-8 and -25-3 + 91 %, both P < 0 05). The baroreflex relation between
diastolic pressure and sympathetic outflow was shifted downward after exercise (postexercise intercept, 218 + 38 total integrated activity (heartbeat)-'; post-sham intercept,
318 + 51 total integrated activity (heartbeat)-', P< 0 05), indicating less sympathetic
outflow across all diastolic pressures. Further, the relation between sympathetic activity and
vascular resistance was attenuated after exercise (post-exercise slope, 0 0031 + 0 0007 units
(total integrated activity)-' min; post-sham slope, 0 0100 + 0 0033 units (total integrated
activity)-' min, P < 0 05), indicating less vasoconstriction with any increase in sympathetic
activity.
Thus, both baroreflex control of sympathetic outflow and the transduction of sympathetic
activity into vascular resistance are altered after dynamic exercise. We conclude that the
vasodilatation which underlies post-exercise hvpotension results from both neural and
vascular phenomena.
The haemodynamic response to large-muscle, dynamic
exercise is characterized by an increased mean arterial
pressure, despite a profoundly reduced systemic vascular
resistance. Although arterial pressure declines quickly after
an acute bout of exercise, systemic resistance does not
completely recover, resulting in a post-exercise hypotension
(Coats, Conway, Isea, Pannarale, Sleight & Somers, 1989;
Cleroux, Kouame, Nadeau, Coulombe & Lacourciere,
1992a; Isea, Piepoli, Adamopoulos, Pannarale, Sleight &
Coats, 1994) that lasts nearly 2 h in healthy individuals
(Halliwill, Taylor, Hartwig & Eckberg, 1996). This
sustained vasodilatation indicates that sympathetic vascular
regulation may be altered after exercise. There are two
possible sources for an alteration in sympathetic vascular
regulation: arterial baroreflex control of sympathetic outflow
and vascular responsiveness to sympathetic stimulation.
The arterial baroreflex exerts exquisite control over arterial
pressure and should respond to the hypotension by
increasing symnpathetic outflow. HowNTever, despite the
reduction in arterial pressure, sympathetic outflow to the
vasculature is either unchanged or reduced compared with
pre-exercise levels (Floras, Sinkey, A.l)ward, Seals, Thoren &
M\ark, 1989; Hara & Floras, 1992). Thus, baroreflex control
of sympathetic outflow may be altered by prior exercise;
however, it is unclear whether it is changes in gain and/or
resetting of the reflex that are responsible. Further, data
from animals suggest that vascular responsiveness to
adrenergic stimulation is attenuated after exercise (Howard,
DiCarlo & Stallone, 1992; Howard & DiCarlo, 1992; Patil,
DiCarlo & Collins, 1993). If such vascular effects predominate
in humans, a dissociation of vasoconstrictor responses
from sympathetic activity could result in post-exercise
Downloaded from jp.physoc.org by on September 9, 2007
J R. Halliwill, J A. Taylor and D. L. Eckberg
280
h potension evein if sympathetic outflow,were etihan ced.
HowN-ever, there are n1o data on the transduction of
sympathetic nerve activity into vascular resistance after
exercise in hlumcans.
Changes in l)aroreflex control of syimpathetic outflowr acnd
chanues in the trcansdluction of sympatlhetic outflow into
vasoconstriction are not mutually exclusive; therefore, we
investigated both b)aroreflex control of sympathetic nervous
outflow and the transduction of sympathetic outflow into
vascular resistance following moderate-intensity dynamnic
exercise in healthv lhumans. We have found previously that
the baroreflex control of heart rate was augmented after
exercise (Halliwill et al. 1996) and, therefore, hypothesized
that alterations in sympathetic transduction to vascular
resistance would be the predominant factor in generating
post-exercise hypotension. Howev-er, our results indicate that
alterations in both the l)aroreflex control of sympatlhetic
nervous outflowv anid transduction of sympathetic outflow\
into vascular resistance contribute to post-exercise vasodilatation; thus, lost-exercise hypotension appears to result
from 0both neural and vascular nmechanisms.
METHODS
This study was approvedlby the Humiiian Research Committees of
the Aleclical College of Virginia ancl the Hunter Holmes AlcC;uire
Department of Veterans Affaiirs Medical Center. Each sul)ject gave
his or her informeled written consent pIrior to participation.
Subjects
Nine healthy, non-smnoking, normnotensive sul)jects participated in
this study (five imeni and fouir womnen, aged 22-27 years). TI'he
sul)jects' average daily l)hysical activity levels were within tlhe
normal range for a sedentary to moderately active population
(Stanford Physical Activity Questionnaire (Sallis et al. 1985):
365-502 keal day' kgM'). Peak aerol)ic powver (1'2 peak) was
determiined with a uraded I maxi;imal cNcle ergometer test comprising
2 min workload incremients sifficient to achieve exhaustion within
13 mmin, and V w,,peak-as within the normllal range for this
population (36 5-51 (0 ml min-' kg-'). Thwis test was usecl to
determine the exercise workloads used in the following protocol.
Experimental protocol
Subjects underwent l)arallel experiments on two separate days. The
order of the experiments was randomnized )between shani, a 60 min
period of seated upriglht rest: ancl exercise, a 60 min periocl of
seatecl uprighit cycling at 60% 12i)eak (Collins 1edalmate,
WV. E. Collins Inc., B3raintree, AIA, USA). We lhave previously
shown that exer;cise of thi.s intensity ancl dluration produces a
sustained (-2 h) post-exercise hlypotension (Halliwill et al. 1996).
During exercise and slian, subjects were allowed to drink water ad
libi/amo. Ambient temper-atuLe ranged fiomn 22 to 24 C. During
eachi experimiient, hieart rcate, arteriial preisure ancd cardiac output
wele measULiedl in the supine position before and at 60 min postslhamii or -exercise. Heart rate and arterial pressu e were also
recordcled every 1O nin d(uring shalmn or exercise. The haroreflex
Control of syml)pathfetic outfloW was assessed 60 min post-shaim or
-exercise andl svympatlhetic control of vascular resistance was
assessed approximnately 90 mi n post-sham orI -exercise.
Baroreflex responsiveness. 'T'o assess the baroreflex control of
sympathetic outflow, InLIscle syml)athetic nierve activity was
J. I'hysiol. 495.1
m-neasured during arterial pressure changes indlucedl bw nitroprussicle
andl phenvlephrine (Ebert & Cowley, 1992). After a 5 min baseline
periodl, 100,ug socdium nitroprusside was given intravenously as a
olus, followed 1 min later bi 1,50ug p)lenylephrine HCI. This
piotocol decreases arterial l)ressuLe -15 mmlilHg below baseline
levels and then increases it 1 5 mmnHg above baseline levels, over a
sihort timne course.
Vascular responsiveness. To assess the transduction of the
sympathetic activity into vascular resistance, calf bloo1l flow ancl
muscle srympathetic nerve activity were mneasure(d during isometri
lhandgrip exeicise helcd to fatigue. Isometr-ic exercise elicits a hIighly
rieproducible pressor response mediated by progressive, pairallel
increases in muscle sympathetic nerve activity an(d ascular
resistance (Seals_ 1989) Further there is a causal relation
between muscle sympathetic nerve activ-ity and calf -ascular
resistance, providling a non-pharmacological method to quantify
the transduiction process. All subjects hacl undergone two previous
training sessions in which they leamnecl to perfoirim isomnetric
lhandgrip exercise to fatigue with either lhand. In the training
sessions, subjects were coached to avoid gasping breaths VXalsalva
manoeuvers (forceful breath holding), and contraction of other
limnbs. During the experiments, the maximum v\oluntary contriaction
was determined fiom the best of thIee attemnpts after the subject
had coompleted slhaIm oIr exercise. After recovery fiom the baroreflex
testing and a 5 mmin baseline period, the subject miaintainecl an
isiometric forearmln contraction at 35% of maximnumn voluntary
contraction to the poinit of fatigue. Force fiomi a clynamomiieter
(Carolina Biological Suppl- Co., Burlington, NC, USA) was
displayed to the subject on an oscilloscope withi the target force.
The encl-point of fatigue was identified lw an-i inability to maintain
hlanclgrip force witlhin 10% of the target level for greater than 2 s
and pronouncement of a maximal perceived exertion irating (Borg,
1 970).
Measurements
Heart rate was determ miiledl froim an electrocardiogram recolding,
beat-bl-beat arterial pressure was measurecl in a finger tusilng a
Finapres)blood pressure monitor (AMoclel 2300, Ohmeda, Englewood,
CO, USA), and standard arterial pressure was measured in ani arin
using a Dinamap 1)lood0 pressure monitor (MAlodel 1846SX, Critikon
Inc., Tampa, FL, USA). Respiration was monitored continuously
using a bellows placed across the subject's abdomlien andl linked to a
-
piessure transducer.
Cardiac output. Cardliac oUttput w\as estimllatedI bw the indiIect
Fick imiethod of carbon dlioxidle (CD2) rebreathiing to equilibrium, as
described previously (Collier, 1956; Halliwill ci al. 1996).
Muscle sympathetic nerve activity. Aluscle symnipafltetic nerve
activ'it\y was recorded via micrdoneurogra)hiv, as described b1
Sundl6f & WVallin (1977). Briefly, miiultiunit, postganglionic mlluscle
sy mpatlhetic nerve acti-itv was recoidcled firomn the peroneal nerve
to the fibtular hlead. Recordings were made withi a
miuicrIoelectr'ocde (0-2 ilI diamiueter' insullatedI slhaft, tapered
to an unlinsulatecd tip of -1-5 j/imi) inserted inlto the nerNve blundle
andcl an uninsulatecl reference electrode insertecl near the fibular
hiead (-2-3 cm fiom the recording electrocde). The nerve was
locatedl bwt using the microelectrodle first as a stimuitilatino electrode
to initiate muscle twitches, and then as a iecording electrode to
identify a fascicle which contained imiu.scle svnil)athetic activ ity.
a
Alusele sympathetic nerve activity was distinguishled fiom other
sources of nerve activity bw the following criteria: (1) pr esence of
posterior
tungsten
sl)ontaneouS pulse svnchronous bursts, (2) increased activity
(dturing Valsalva straining, (3) muscle afferenit activity with iliusele
stretch, ancd (4) no chantge of activity during lighlt stroking of the
Downloaded from jp.physoc.org by on September 9, 2007
J. Phys(ol. 495.1
281
Post-exercise vasodilatation
Table 1. Systemic and regional haemodynamics and sympathetic outflow
SYstolic aiterial pressure (mmifHg)
Diastolic pressure (mmHg)
Alean arter ial pressure (inm Hg)
Cardiac output (I mint)
Total peripheral resistance (units)
Calf blood flowr (ml min-1 (100 ml)F1)
Calf -asculair resistance (units)
MIuscle sy unpathetic nerve activity
(bursts min1)
(total integrated activity (min)')
(bur'sts (100 heartbeats)-)
(total integrated activity (100 heartbeats)F')
Post-sham
Post-exercise
131 + 3
71 + 2
91 + 2
5-9 + 0 4
16-3 + 1-5
2-20 + 0 34
47-4 + 5-4
123 + 5*
65 + 3
84 + 3*
7 0 + 0-6*
12-8 + 1.5*
2-86 + 0-36
34-2 + 4-9*
2-7
340
50
620
8-9 + 1-5*
1600 + 300*
14-8 + 2-8*
2660 + 530 *
15-7 +
2290 +
274 +
4000 +
Values are means + S.E.M. * indicates deviations from post-sham (P < 0 05).
skin or with startling the subject with loud noises, indicating lack
of skin nerve activity. The recordecd signal was amplified 70000fold, bandpass filterecl (700-2000 Hz), rectified, and integrated
(resistance-capacitanice integrator circuit, time constant 0 1 s) b)y a
nerve traffic analyser (Model 662C3, Biomnedical Engineering,
University of Iow-a, Iow-a City, IA, USA). The resulting signal was
miionitored on an oscilloscope and loudspeaker througlhout the
experiment. Sympathetic activity was recorded in the leg ipsilatei-al
to the arm pertform)iing lhandgrip exercise and contralateral to tlle
leg used for calf blood-flow measurements. The set-up was reversecl
on the second day of tle experiment.
Calf blood flow. Calf blood flox- was estimnated bsy venous occlusion
plethysmography, as described bY Siggaard-Andersen (19570). An
air-filled, latex plethlnsmographic cuff was placed mid-calf and
connected to a voltumetr'ic pressure transducer (M\odel PT5, Grass
Instrument Co., Quincy, AIA, USA) for recording changes in calf
volume. An arter ial occlusion cuff around the ankle was
continuously inflate(d to suprasystolic pressures (250 mmHg)
during mneasuremenits, wh-lile a veenous occlusion cuff around tlle
thigh was inflated to 60 mmnHg for 715 s out of every 15 s,
p)roviding one calf blood-flow- measurement every 15 s. Calf blood
flow was caliblrate(d at the encl of every experiiment b)y a(dcling
known volumnes of air to the pletlhysm-nographic cuff still in place on
the sulbject. Thiis 1)1ood flow was expressed as millilitres per imiinute
pel one hundclrecl miillilitres of tissue.
Data analysis
t)ata were recorded b)y electrostatic (Gould ES 1000, Gould Inc.,
(Greenbelt, MD, USA) ancl FAI tal)e (Model 3968A, Hewlett
Pacl,kard) recorders. D)ata were ancaly-sed off-line with signal
p)rocessing software (WinDaq, Dataq Instruments, Akron, OH,
LTSA). The electrocardiogran,m beat -lw-b)eat arterial pressure, calf
plethysmogram, i ntegr atecl muscle symlpathetic nerve activity, ancl
respiration signal (bellows) were cligitized at 250 Hz. AMuscle
sympathetic nerve activity was quantifiedI as both the numbll)er of
boursts ancl as total initeg-ratecl activity, (lefinied as the summned area
of bursts. Data foti derivation of venitilation volumnes anid(CO2
concentrations were (ligitized at 100 Hz. 'I'otal periplheral resistance
was calculated 1 w dividing mean arterial pressure by cardiac
outpLut, andl calf \vasCular resistance was calculatecl by lividling
mnean arterial pressure by calf blood flow; both resistances were
expressed as units. Since i-esistance values derived from Finapres
and Dinamap pressures provided analogous results, only those
based on Finapres pressures are presented.
A measure of baroreflex control of sympathetic outflow was
proxvided byr the relation between muscle sympathetic nerve
activity and diastolic pr essure during vasoactive drug boluses
(Ebert & CowAley, 1992). We used diastolic pressure because muscle
sympathetic nerve actixvity correlates closely wvith diastolic pressure
but not with systolic pressure (Sundl6f & Wallin, 1978). Beat-bybeat values for nerve activity were averagedlover 3 mmHg diastolic
pressure ranges and a weighted linear regression betwN-een nerve
activity and pressure was performed. This pooling procedure
r educes the statistical impact of the inherent beat-by-beat
variability in nerve activity due to non-baroreflex influences
(e.g. respiration; Ebert & Cow-ley, 1992). The mean nerve activity
ancl pressure during the 5 mnin baseline that precedecd nitroprusside
adlministration was included in the regression.
An index of the transdduction of sympathetic activity into -ascular
resistance was derived fiomn the r-elationship between calf vascular
r esistance and muscle sympathetic nerve activity. This was
calculated fiom a weiglhted linear regression of 30 s values foi calf
vascutlar resistance and nerve activity (i.e. the mean of two calf
blood-flow measurieinents were usecl fir each point in the
regression). The reaniesistance ancl nerve activity durinn the
5 mmin baseline that preceded handgrip exercise were included in the
regression.
Since regressions based on total integmatecl activity and burst
niuml)e providlec identical results, only those baseed on total
integrated activitV aie plesented.
Statistics. VTariables which were measured after shamn or exercise
were compared using a paired Student's t test. All variables
measutred during sham ovr exer-cise wrere averaged for the entire
60 itwin period andl comiipared with l)pe-exelcise values by a
repeatedl-measures anialysis of v-ariarnce. The baroreflex ancd
trans(luction relations were analyNsedl b)y multivariate linear
regression modlels witlh rmepeate(d meastures. All values ame repolrtedl
as iimeanls + SE.N1.
Downloaded from jp.physoc.org by on September 9, 2007
J. Physiol. 495.1
J R. Halliwill, J A. Taylor and D. L. Eckberg
282
Phenylephrine
Nitroprusside
-1
--
160-
U)
bLbI
tU) 0)
41800
I1i I LL
II
1-
1u
Electrocardiogram
II
co
11 I iILLLtiIt II
. [II . I
LI
Mon
, .
IL [ILIII
LI Ll IL L L L
tlL IL
IILL LIlL
f~11
h~*
J14
Il
l
'l
II P III II111 III III II llllllllllll lll
Illll-II
I1111
~6W~I
M MMl 1 -l
11 '-1111ll 11l1I
1400
II
II
1111111
lllllv'1-11
III
1200a) 1000-
1a
._.-
cc
800600
Muscle sympathetic
nerve activity
1 min
Figure 1. Representative vascular baroreflex data
Representative data from one subject showing beat-by-beat arterial pressure, electrocardiogram, beat-bybeat R-R interval, and integrated muscle sympathetic nerve activity during nitroprusside and
phenylephrine baroreflex testing.
reserve
RESULTS
is defined
as
resting supine heart rate minus
maximum heart rate achieved during
Exercise
The mean exercise workload was 130 + 10 W. During this
time heart rate increased from 62X0 + 2-2 beats min-' at
rest to 138-2 + 3-1 beats min-' during exercise (mean for
entire 60 min of exercise, P< 0 05). This represented, on
average, 63-0 + 1P9% of heart rate reserve (heart rate
Vo,
peak
160
4-
4-
120
C.)
a)0
C
140
>.
Figure 2. Representative vascular baroreflex relation
100
Representative baroreflex relation derived from data in Fig. 1.
5 min baseline that preceded nitroprusside administration.
*, the mean nerve activity across a 3 mmHg range of pressure.
Regression: muscle sympathetic nerve activity
(MSNTA) = 310 361 diastolic pressure (DBP); r, -0-88.
0,
80 -
E a)
en
a) '
60
40
-)
20
.I-
.
0-
45
50
55
70
60 65
75
Diastolic pressure (mmHg)
test),
indicating the targeted relative workload had been reached.
Systolic pressure increased 34 + 4 mmHg (P < 0 05), while
diastolic pressure was unchanged (0 + 4 mmHg) during
exercise. As a result, mean arterial pressure increased with
exercise (+11 + 3 mmHg, P < 0 05). Neither heart rate nor
arterial pressure changed with sham.
80
Downloaded from jp.physoc.org by on September 9, 2007
J. Ph1ysiol. 495.1
283
Post-exercise vasodilatation
Systemic and regional haemodynamics and
sympathetic outflow
Table 1 shows systemic and regional haemodynamics and
sympathetic outflow at 1 h recovery post-sham and postexercise. Mean arterial and systolic pressures were less postexercise (both P < 0 05). Cardiac output was higher after
exercise (P < 0 05), whereas both total peripheral and calf
vascular resistances were lowrer (-21P7 + 4-9 and -25-3 +
94 %, both P < 0 05) after exercise. Concurrent -with these
haemodynamic changes, muscle sympathetic nerve activity
was lower after exercise, regardless of whether it was
assessed as burst number or total integrated activity.
Baroreflex control of sympathetic outflow
Figure 1 shows data from one subject during injections of
vasoactive drugs. Nitroprusside and phenylephrine elicit a
sequential fall and rise in pressure that provoke reflex
changes in heaIrt period (R-R interval), and muscle
sympathetic outflow. Changes in diastolic pressure were
similar after sham and exercise (mean fall: -13-2 + 1 6 vs.
-15 6 + 2 4 mmHg, P= 0 37; mean rise: 116 + 2 0 vs.
12 0 + 2-4 mmHg, P= 0 79). The relation between muscle
sympathetic nerve activity and diastolic pressure derived
from the data in Fig. 1 is shown in Fig. 2. This relation wNas
used to assess baroreflex control of sympathetic outflow. A
close relation betw een nerve activity and pressure was seen
in each subject (mean correlation coefficient, r = -074 +
0 08). Figure 3 shows the mean baroreflex relations.
Although the slopes of the relations were not different
(-3 96 + 0 72 vs. -3 05 + 0 70 total integrated activity
(heartbeat)-' mmHHg-, P = 0410), the intercept was less
post-exercise (318 + 51 vs. 218 + 38 total integrated
activity (heartbeat)-', P< 0 05), indicating that the entire
relation was shifted downward, and that across all diastolic
pressures, muscle sympathetic nerve activity was less. In
contrast, the relation between heart rate and arterial
pressure was unaltered, as we have found previously
(intercept: 201 + 23 vs. 174 + 17 beats min-', P= 0413;
slope: -1-05 + 0416 vs. -0-91 + 0414 beats min-' mmHg-',
P = 0-36; Halliwill et al. 1996).
Transduction of sympathetic activity into vascular
resistance
Figure 4 shows data from one subject during the handgrip
portion of the protocol. Isometric handgrip exercise elicits a
progressive rise in arterial pressure and parallel increases in
muscle sympathetic nerve activity and vascular resistance.
Handgrip strength and time to fatigue were consistent on
each day of the experiment (35 % maximal voluntary
contraction: 12'3 + 0 9 vs. 12-0 + 1P3 kg, P = 0 70; time to
fatigue: 237 + 24 vs. 252 + 41 s, P = 0 70). The relation
between calf vascular resistance and muscle sympathetic
nerve activity derived from the data in Fig. 4 is shown in
Fig. 5. A close relation between calf vascular resistance and
nerve activity was seen in each individual (mean
r, 0 76 + 0 04). This relation was used to assess the
transduction of sympathetic activity into vascular resistance.
Figure 6 shows the mean transduction relations expressed as
total integrated activity. The slope of the relation was
greatly attenuated post-exercise (0-0100 + 0 0033 vs.
0-0031 + 0 0007 units (total integrated activitvy)-imin,
P < 0 05), but the intercept was unaltered (19 6 + 11 vs.
2641 + 4-2 units, P = 0412), indicating that with any
increase in muscle sympathetic nerve activity, there is less
of an increase in calf vascular resistance after exercise, and
that this disparity becomes more apparent with greater
sympathetic activation.
DISCUSSION
These data provide conclusive evidence for altered
sympathetic vascular regulation after acute dynamic
exercise in humans. Despite strong evidence for a persistent
post-exercise vasodilatation, there are no previous data on
baroreflex control of sympathetic outflow or sympathetic
control of vascular resistance after exercise in humans. Our
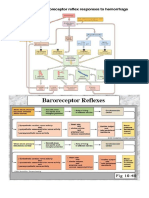
findings are schematically summarized in Fig. 7. First, we
found striking reductions in baseline muscle sy-mpathetic
nerve activity, which w\ere associated with a dowxnward shift
of the sympathetic nerve activity-arterial pressure relation.
150.5I
Figure 3. Mean vascular baroreflex relations
Mean baroreflex relations after shain (continuous line) ancl after
exercise (dashedl linle; ii = 9). Also sho-wn are the baseline values
for post-shamn (0) and post-exercise (0), and the mean values
from each subject's lowest andc highest diastolic pressures postsham (0) and post-exercise (0). Error bars indicate 5.E.M.
Post-sham regression: AISNA = 318 - 396 DBP; r, -0-88;
post-exercise regression: AISNA = 218 - 305 DBP; r, -0-83.
_
a)
?c
100-
>1
.y :,
cs
Q.
50c0 .: CZ
-)
40
Downloaded from jp.physoc.org by on September 9, 2007
70
80
50
60
Diastolic pressure (mmHg)
90
J. Physiol. 495.1
J R. Halliwill, J A. Taylor and D. L. Eckberg
284
Electrocardiogram
150
125
Co
CL
E
1 00
k-k
Muscle sympathetic
nerve activity
Calf blood flow
Calf vascular
resistance (units)
35-85
4660
82-12
20 s
Figure 4. Representative handgrip data
Representative data from one subject showing electrocardiogram, arterial pressure, integrated muscle
sympathetic nerve activity, calf blood flow, and the derived calf vascular resistance during the handgrip
part of the protocol.
This indicates that an alteration in baroreflex control of
sympathetic outflow does contribute to post-exercise vasodilatation. Second, we found a dramatic attenuation of the
vascular resistance-sympathetic nerve activity relation.
This indicates that an impairment in the transduction of
nerve activity into vascular resistance also contributes to
post-exercise vasodilatation. Thus, the reduced vascular
resistance which underlies post-exercise hypotension results
from both neural and vascular phenomena.
Although we document changes in sympathetic vascular
regulation only to skeletal muscle, these alterations have an
important functional impact on systemic haemodynamics.
120 co
c7
100 -
X
c
.e
80
,c
80-
Figure 5. Representative handgrip transduction relation
Representativ,e transduction relation derived from data in Fig. 4.
0, 5 min baseline that preceded handgrip exercise. 0, the mean nerve
activity and vascular resistance during a 30 s period. Regression: calf
vascular resistance (CVR) = 27-4 + 0 0033 MSNA; r, 078.
.co
c
60-
0.
0
co
Cu
0*
*0
40 20 0
4000
8000
12000
16000
Muscle sympathetic nerve activity
(total integrated activity (min)-')
Downloaded from jp.physoc.org by on September 9, 2007
J. Physiol. 495.1
Post-exercise vasodilatation
285
70 -
c 60C
Figure 6. Mean transduction relations
Mean transduction relations after sham (continuous line) and after exercise
(dashed line; ii = 9). Also shown are the baseline values for post-sham (0)
and post-exercise (@), and the mean values from each maximal nerve
activity post-shain (0) and post-exercise (0). Post-sham
regression: CVR = 19-6 + 00100 MSNA; r, 0 93; postexercise regression: CVR = 26 1 + 0-0031 MSNA; r, 0 93.
a)0
c)
X 400
(0
ir 30-
20 0
Skeletal muscle can receive up to 88 % of systemic blood
flow during exercise (Rowell, 1993) and changes in skeletal
muscle blood flow at rest can profoundly affect systemic
arterial pressure (Rowell, Detry, Blackmon & Wyss, 1972).
Further, we found that total peripheral resistance and calf
vascular resistance changed in parallel, strongly suggesting
that what occurs in the lower leg does indeed reflect what
occurs systemically. Therefore, our findings of regional
neural and vascular changes underlying a vasodilatation
after exercise are likely to have a functional significance in
mediating post-exercise hypotension.
2000 4000 6000 8000 10000
Muscle sympathetic nerve activity
(total integrated activity (min)-')
Neural mechanisms
All our subjects had a decreased sympathetic nerve activity
within the 2 h immediately following acute dynamic
exercise. Previous assessments of sympathetic outflow after
exercise have yielded equivocal results (Floras et al. 1989;
Floras & Senn, 1991; Hara & Floras, 1992), perhaps because
the exercise protocols used did not consistently produce
post-exercise hypotension. In association with the reduced
nerve activity, we also found that the relation between
sympathetic activity and arterial pressure is shifted
downward after exercise. Thus, sympathetic vasoconstrictor
outflow is less at any pressure, contributing to the reduced
.>
0
U)
Resistance
X38 3
(4 6) post-sham
29 5 (3.7) post-exercise
Sympathetic activity
Figure 7. Schematic summary of results
Mtodel of altered vascular regulation after exercise, incorporating shift in baroreflex control of sympathetic
outflow and attenuation of the transduction of sympathetic activity into vascular resistance. Sham relations
are continuous lines; exercise relations are dashed lines.
Downloaded from jp.physoc.org by on September 9, 2007
286
J R. Halliwill, J A. Taylor and D. L. Eckberg
vascular resistance after exercise. This resetting of the
arterial baroreflex to lower pressures could occur either at
the level of the baroreceptors themselves or in the central
nervous system. It is unlikely that the baroreceptors
themselves are reset, since baroreflex control of heart rate is
not altered at the time when our sympathetic recordings
were made (Halliwill et al. 1996). As afferent baroreceptor
activity does not subserve specific efferent outflows, this
excludes baroreflex resetting at the baroreceptor level and
indicates a change in the central nervous system control of
vascular sympathetic outflow. A central opioid pathway,
activated by exercise, has been suggested to mediate postexercise vasodilatation by inhibiting sympathetic vasoconstrictor outflow (Thoren, Floras, Hoffman & Seals, 1990).
However, recent studies have found no role for a central
opioidergic mechanism in mediating post-exercise hypotension (Hara & Floras, 1992; Sebastian, Moran & Tipton,
1995). Nonetheless, it is apparent that some central
alteration in the arterial baroreflex results in a downward
shift in the sympathetic outflow-arterial pressure relation.
It is possible that the alteration is not due to a change in the
arterial barorefl,ex per se, but is due to increased sympathoinhibitory input from cardiopulmonary receptors. Although
exercise usually produces hypovolaemia (sweating and
extravascularization of fluids lead to plasma volume loss),
plasma volume returns to normal and can even increase
during recovery from exercise due to changes in fluidregulating hormones or elevations in plasma protein
(leading to fluid shifts from the extravascular space; R6cker,
Kirsch, Heyduck & Altenkirch, 1989; Gillen, Lee, Mack,
Tomaselli, Nishiyasu & Nadel, 1991). Some volume
expansion may have occurred prior to our measurements
(we did not measure plasma volume); however, volume
expansion of greater than 11 would be required to elicit the
magnitude of symnpatho-inhibition that we found (Vissing,
Scherrer & Victor, 1989) and volume expansion of this
magnitude is unlikely to have occurred as quickly as 1-2 h
post-exercise (Rocker et al. 1989; Gillen et al. 1991).
Nonetheless, the influence of cardiopulmonary reflexes
could be enhanced by a single bout of exercise. Indeed,
Collins & DiCarlo (1993) reversed the post-exercise hypotension in rats by blocking cardiopulmonary afferent nerves.
It is unclear if this mechanism is responsible in humans.
Reductions in central blood volume presumed to unload the
cardiopulmonary baroreceptors have been shown to produce
both unchanged and augmented forearm vascular resistance
responses (Bennett, Wilcox & Macdonald, 1984; Cleroux,
Kouame, Nadeau, Coulombe & Lacourciere, 1992 b).
However, these data are insufficient to derive any conclusions
concerning cardiopulmonary responses in humans due to
methodological limitations (Taylor, Halliwill, Brown,
Hayano & Eckberg, 1995) and to measurement limitations
(i.e. no information on sympathetic responses). Regardless,
it may be that increased cardiac filling pressures secondary
to modest hypervolaemia interact with augmented responsiveness of cardiopulmonary reflexes to inhibit sympathetic
J Phy8iol.495.1
outflow, thus shifting the nerve activity-arterial pressure
relation in humans.
Vascular mechanisms
We found not only a clear sympatho-inhibition, but also a
striking attenuation of the relation between sympathetic
activity and vascular resistance during recovery from
exercise. Thus, even if sympathetic vasoconstrictor outflow
were unchanged, impaired vascular responsiveness would
result in reduced vascular resistance after exercise.
Ineffective transduction of nerve activity into vasoconstriction could result from less neurotransmitter release.
For example, circulating opioids may be increased after a
single bout of exercise (Schwarz & Kindermann, 1992).
Sympathetic nerve terminals possess presynaptic inhibitory
opioid receptors (Wong-Dusting & Rand, 1989) that may be
occupied after exercise, effectively reducing noradrenaline
release. Although systemic opioid blockade with naloxone
has been shown to reverse post-exercise hypotension in
animals (Shyu & Thoren, 1976; Devine, Sebastian, Monnin
& Tipton, 1991; Sebastian et al. 1995), it has had mixed
results in humans (Boone, Levine, Flynn, Pizza, Kubitz &
Andres, 1992; Hara & Floras, 1992), and the role of opioids
remains controversial (Sebastian et al. 1995). Presynaptic
inhibition can also be caused by neuropeptide Y (Lundberg
& Stjarne, 1984), which is co-released with noradrenaline
during exercise (Pernow et al. 1986). After exercise,
neuropeptide Y may remain bound to presynaptic receptors,
reducing noradrenaline release (Pernow et al. 1986).
The most likely site for ineffective transduction of
sympathetic outflow into vascular resistance is arterial
smooth muscle, through receptor downregulation or local
vasodilatator substances. Post-exercise reductions in
vascular responsiveness to adrenergic stimulation have been
shown in isolated aortic strips (Howard et al. 1992) and in
conscious rabbits (Howard & DiCarlo, 1992) and rats (Patil et
al. 1993). Using nitric oxide synthetase blockade in rats,
Patil et al. (1993) were partially able to reverse the
attenuated adrenergic responsiveness of smooth muscle
after exercise, strongly supporting a role for enhanced nitric
oxide activity in post-exercise vasodilatation. While there
are no analogous data from humans, the strongest effect on
vascular responsiveness may be that of nitric oxide.
In conclusion, we found that persistent vasodilatation
following a single bout of moderate-intensity dynamic
exercise is mediated in two ways. First, baroreflex control of
sympathetic outflow is altered, such that sympathetic
outflow at any given pressure is less. Second, transduction
of sympathetic activity into vascular resistance is also
altered, such that vascular resistance is even further
reduced. Thus, post-exercise hypotension appears to result
from both neural and vascular mechanisms.
Downloaded from jp.physoc.org by on September 9, 2007
J Physiol. 495.1
Post-exercise vasodilatation
BENNETT, T., WILCOX, R. Cl. & AIACDONALD, I. A. (1984). Post-exercise
reduction of blood pressure in hypertensive men is not due to acute
impairment of baroreflex function. Clintical Science 67, 97-103.
BOONE, J. B., LEVINE, AM., FLYNN, M. G., PIZZA, F. X., KUBITZ, E. R.
& ANDRES, F. F. (1992). Opioid receptor modulation of postexercise
hypotension. Mledicine and Science in Sports and Exercise 24,
1108-1113.
BORG, G. (1970). Perceived exertion as an indicator of somatic stress.
Scandinavian Journal of Rehabilitationi and MIedicine 2-3, 92-98.
CLEROUX, J., KOUANME, N., NADEAU, A., COULOMBE, D. &
LACOURCIERE, Y. (1992a). After effects of exercise on regional and
systemic heemodvnamics in hypertension. Hypertension 19,
183-191.
CLEROUX, J., KOUAME, N., NADEAU, A., COULOMBE, D. &
LACOURCIERE, Y. (1992 b). Baroreflex regulation of forearm vascular
resistance after exercise in hyrpertensive and normotensive humans.
A merican Journal of Physiology 263, H1523-1531.
COATS, A. J. S., CONWNAY, J., ISEA, J. E., PANNARALE, G., SLEIGHT, P. &
SOMERS, V. K. (1989). Systemic and forearm vascular resistance
changes after upriglht bicycle exercise in Iman. Journal of Physiology
413, 289-298.
COLLIER, C. R. (1956). Determination of mixed venous CO2 tensions
by rebreathing. Journal of Applied Physiology 9, 25-29.
COLLINS, H. L. & DICARLO, S. E. (1993). Attenuation of
postexertional hypotension by cardiac afferent blockade. American
Journal of Physiology 265, H11179-1183.
DEVINE, M. D., SEBASTIAN, L. A., MONNIN, K. A. & TIPTON, C. AM.
(1991). Training and post-exercise hypotension with hypertensive
rats (SHR). The Physiologist 34, A267.
EBERT, T. J. & COWLEY, A. W. (1992). Baroreflex modulation of
sympathetic outflow during physiological increases in vasopressin
in humans. American Journal of Physiology 262, H1372-1378.
FLORAS, J. S. & SENN, B. L. (1991). Absence of post exercise
hypotension and svmpathoinhibition in normal subjects: additional
evidence for increased sympathetic outflow in borderline hypertension. Canadian Journal of Cardiology 7, 253-258.
FLORAS, J. S., SINKEY, C. A., AYLWARD, P. E., SEALS, D. R., THOREN,
P. N. & MARK, A. L. (1989). Postexercise hypotension and
sympathoinhibition in borderline h-ypertensive men. Hypertension
14, 28-35.
GILLEN, C. M., LEE, R., MIACK, G. W., TOMASELLI, C. M., NISHIYASU,
T. & NADEL, E. R. (1991). Plasma volume expansion in humans
after a single intense exercise protocol. Journal of Applied
Physiology 71, 1914-1920.
HALLIWILL, J. R., TAYLOR, J. A., HARTWIG, T. D. & ECKBERG, D. L.
(1996). Augmented baroreflex heart rate gain after moderateintensity, dynamic exercise. American Journal of Physiology 270,
R420-426.
HARA, K. & FLORAS, J. 5. (1992). Effects of naloxone on
hemody-namics and sympathetic activity after exercise. Journial of
Applied Physiology 73, 2028-2035.
HOWARD, Ml. CT. & DICARLO, S. E. (1992). Reduced v-ascular
responsiveness after a single bout of dynamic exercise in the
conscious rabbit. Journal of Applied Physiology 73, 2662-2667.
HOWARD, AM. G., DICARLO, S. E. & STALLONE, J. N. (1992). Acute
exercise attenuates phenyleplirine-induced contraction of rabbit
isolated aortic rings. Medicine and Science in Sports and Exercise
24,1102-1107.
ISEA, J. E., PIEPOLI, M., ADAMOPOULOS, S., PANNARALE, G.,
SLEIGHT, P. & COATs, A. J. S. (1994). Time course of haemodynamic
changes after maximal exercise. European Journal of Clinical
Inv estigation 24, 824-829.
287
LUNDBERG, J. Al. & STJXRNE, L. (1984). Neuropeptide Y (NPY)
depresses the secretion of 3H-noradrenaline and the contractile
response evoked by field stimulation, in rat vas deferens. Acta
Physiologica Scandinavica 120, 477-479.
PATIL, R. D., DICARLO, S. E. & COLLINS, H. L. (1993). Acute exercise
enhances nitric oxide modulation of vascular response to
phenylephrine. American Journal of Physiology 265, HI 184-1188.
PERNOW, J., LUNDBERG, J. M., KAIJSER, L., HJEMDAHL, P.,
THEODORSSON-NORHEIM, E., MARTINSSON, A. & PERNOW, B. (1986).
Plasma neuropeptide Y-like immunoreactivity and catecholamines
during various degrees of sympathetic activation in man. Clinical
Physiology 6, 561-578.
ROCKER, L., KIRSCH, K. A., HEYDUCK, B. & ALTENKIRCH, H.-U.
(1989). Influence of prolonged physical exercise on plasma volume,
plasma proteins, electrolytes, and fluid-regulating hormones.
International Journal of Sports Medicine 10, 270-274.
ROWELL, L. B. (1993). Control of regional blood flow during dynamic
exercise. In Human Cardiovascular Control, pp. 205-254. Oxford
University Press, New York.
ROWELL, L. B., DETRY, J. R., BLACKMON, J. R. & Wyss, C. (1972).
Importance of the splanchnic vascular bed in human blood pressure
regulation. Journal of Applied Physiology 32, 213-220.
SALLIS, J. F., HASKELL, W. L., WOOD, P. D., FORTMANN, S. P.,
ROGERS, T., BLAIR, S. N. & PAFFENBARGER, R. S. (1985). Physical
activity assessment methodology in the five-city project. American
Journal of Epidemiology 121, 91-106.
SCHWARZ, L. & KINDERMANN, W. (1992). Changes in f-endorphin
levels in response to aerobic and anaerobic exercise. Sports Mledicine
13, 25-36.
SEALS, D. R. (1989). Sympathetic neural discharge and vascular
resistance during exercise in humans. Journal of Applied
Physiology 66, 2472-2478.
SEBASTIAN, L. A., MORAN, Al. M. & TIPTON, C. AMI. (1995). Postexercise hypotension and intra-cerebro-ventricular (ICV) injections
of /1-endorphin and naloxone hydrochloride. FASEB Journial 9,
A361.
SHYU, B. C. & THOREN, P. (1976). Circulatory events following
spontaneous muscle exercise in normotensive and hypertensive rats.
Acta Physiologica Scandinavica 128, 515-524.
SIGGAARD-ANDERSEN, J. (1970). Venous occlusion plethysmography
on the calf. Evaluation of diagnosis and results in vascular surgery.
Danish M1Iedical Bulletin 17, 1-66.
SUNDLOF, G. & WALLIN, B. G. (1977). The variability of muscle nerve
sympathetic activity in resting recuInbent Inan. Journal of
Physiology 272, 383-397.
SUNDL6F, G. & WALLIN, B. G. (1978). Human muscle nerve
sympathetic activity at rest. Relationship to blood pressure and age.
Journal of Physiology 274, 621-637.
TAYLOR, J. A., HALLIWILL, J. R., BROWN, T. E., HAYANO, J. &
ECKBERG, D. L. (1995). 'Non-hypotensive' lhpovolaemia reduces
ascending aortic dimensions in humans. Journal of Physiology 483,
289-.298.
THOREN, P., FLORAS, J. S., HOFFMAN, P. & SEALS, D. R. (1990).
Endorphins and exercise: physiological mwechanisms and clinical
implications. Medicine and Science in Sports and Exercise 22,
41-7-428.
\'ISSING, S. F., SCHERRER, U. & VTICTOR, R. G. (1989). Relation
between sympathetic outflow and vascular resistance in the calf
during perturbations in central venous pressure: evidence for
cardiopulmonary afferent regulation of calf vascular resistance in
humans. Circulation Research 65, 1710-1717.
Downloaded from jp.physoc.org by on September 9, 2007
288
J R. Halliwill, J A. Taylor and D. L. Eckberg
WX\NG-DUSTING, H. & RAND, Al. J. (1989). Inhibition of sympatlhetic
neurotransmission b)y the opioid 8-receptor agonist DAM1A in the
pithed rat. Cliniical atd( Experimtlenital Pharmitacology antd Physiology
16, 821-827.
Acknowledgements
This study was conclucted by John R. Halliwill in partial fulfilment
of the requirements for the degree of Doctor of Philosophy at the
Miedical College of Virginia and was supported by grants from the
Department of Veterans Affairs, the National Institutes of Health
(HL 22296), and the National Aeronautics and Space Administration
(NAG 2-408 and NAS 10-10285). We thank Larry A. Beightol for
his technical assistance. \Ve especially thank the subjects w-ho
volunteered for this study.
Author's email address
J. R. Halliwill: halliwill.john@mayo.edu
Received 20 Novem ber 1995; accepted 23 April 1996.
Downloaded from jp.physoc.org by on September 9, 2007
J Physiol. 495.1
Impaired sympathetic vascular regulation in humans after acute dynamic
exercise.
J R Halliwill, J A Taylor and D L Eckberg
J. Physiol. 1996;495;279-288
This information is current as of September 9, 2007
Updated Information
& Services
including high-resolution figures, can be found at:
http://jp.physoc.org
Permissions & Licensing
Information about reproducing this article in parts (figures,
tables) or in its entirety can be found online at:
http://jp.physoc.org/misc/Permissions.shtml
Reprints
Information about ordering reprints can be found online:
http://jp.physoc.org/misc/reprints.shtml
Downloaded from jp.physoc.org by on September 9, 2007
Das könnte Ihnen auch gefallen
- Reflex Effect of Skeletal Muscle MechanoreceptorDokument9 SeitenReflex Effect of Skeletal Muscle MechanoreceptorMateus José ArrudaNoch keine Bewertungen
- Acute Effects of Resistance Exercise On Arterial ComplianceDokument6 SeitenAcute Effects of Resistance Exercise On Arterial Complianceramonfonseca051Noch keine Bewertungen
- Reserch VestDokument11 SeitenReserch VestRAMO STEF SZEKERESNoch keine Bewertungen
- Post-Exercise Aortic Hemodynamic Responses To Low-Intensity Resistance Exercise With and Without Vascular OcclusionDokument6 SeitenPost-Exercise Aortic Hemodynamic Responses To Low-Intensity Resistance Exercise With and Without Vascular OcclusionJuanfran Montesinos GarciaNoch keine Bewertungen
- 1985-Cardiac Adaptations To Chronic ExerciseDokument28 Seiten1985-Cardiac Adaptations To Chronic ExerciseJavier Mora BaizNoch keine Bewertungen
- Camarena 2000Dokument10 SeitenCamarena 2000Veronica JanethNoch keine Bewertungen
- Treinamento de Força e Sistema Vascular 2005 J Appl PhysiolDokument6 SeitenTreinamento de Força e Sistema Vascular 2005 J Appl PhysiolDarlan SilvaNoch keine Bewertungen
- Necessity For Vestibulo-Autonomic ResponsesDokument6 SeitenNecessity For Vestibulo-Autonomic ResponseswellytonNoch keine Bewertungen
- The Effect of Gravity Inversion Procedures On Systemic Blood Pressure, Intraocular Pressure, and Central Retinal Arterial PressureDokument5 SeitenThe Effect of Gravity Inversion Procedures On Systemic Blood Pressure, Intraocular Pressure, and Central Retinal Arterial Pressurecookie “cookihakies” anonymeNoch keine Bewertungen
- Chronic Baroreflex Activation Restores Spontaneous Baroreflex Control and Variability of Heart Rate in Obesity-Induced HypertensionDokument10 SeitenChronic Baroreflex Activation Restores Spontaneous Baroreflex Control and Variability of Heart Rate in Obesity-Induced HypertensionCaesar Catalin CaratasuNoch keine Bewertungen
- Am J Physiol Regul Integr Comp Physiol-2000-Daniels-R1849-55Dokument7 SeitenAm J Physiol Regul Integr Comp Physiol-2000-Daniels-R1849-55Dr-Alaa HashimNoch keine Bewertungen
- Cardiovascular Drift and Cerebral and Muscle Tissue Oxygenation During Prolonged Cycling at Different Pedalling CadencesDokument12 SeitenCardiovascular Drift and Cerebral and Muscle Tissue Oxygenation During Prolonged Cycling at Different Pedalling CadencesBob UeckerleleNoch keine Bewertungen
- WongDokument5 SeitenWongtalleresccorporal5Noch keine Bewertungen
- Bove 1979Dokument8 SeitenBove 1979Arthur PiresNoch keine Bewertungen
- Mizushima Et Al. 2000Dokument7 SeitenMizushima Et Al. 2000Hendry SusantoNoch keine Bewertungen
- Cardiovascular Responses To Static ExerciseDokument7 SeitenCardiovascular Responses To Static Exercisesilvio da costa guerreiroNoch keine Bewertungen
- AJP Heart 2008Dokument8 SeitenAJP Heart 2008Rezza FahlevhyNoch keine Bewertungen
- Net Notes CardioDokument9 SeitenNet Notes CardioJess PeltraNoch keine Bewertungen
- Article - N - Gender Differences Responses in Isometric ExerciseDokument6 SeitenArticle - N - Gender Differences Responses in Isometric ExercisePacho ArbelaezNoch keine Bewertungen
- Effects of Walking With Blood Ow Restriction On Limb Venous Compliance in Elderly SubjectsDokument5 SeitenEffects of Walking With Blood Ow Restriction On Limb Venous Compliance in Elderly SubjectsJonathan Alexis Salinas UlloaNoch keine Bewertungen
- Factors Affecting Blood Pressure During Heavy Weight Lifting and Static ContractionsDokument8 SeitenFactors Affecting Blood Pressure During Heavy Weight Lifting and Static ContractionsMumtaz MaulanaNoch keine Bewertungen
- Evaluation of Heart Rate Variability - UpToDateDokument31 SeitenEvaluation of Heart Rate Variability - UpToDateGonçalo MirandaNoch keine Bewertungen
- Postexercise Hypotension in An Endurance-Trained Population of Men and Women Following High-Intensity Interval and Steady-State CyclingDokument10 SeitenPostexercise Hypotension in An Endurance-Trained Population of Men and Women Following High-Intensity Interval and Steady-State Cyclingnuttela ismeNoch keine Bewertungen
- Ajpregu 00151 2015Dokument10 SeitenAjpregu 00151 2015Poring CarnavasNoch keine Bewertungen
- Task Oriented Improves Strength - Stroke PatientsDokument7 SeitenTask Oriented Improves Strength - Stroke PatientsPedro FonsecaNoch keine Bewertungen
- Rapid Increase in Plasma Growth Hormone After Low-Intensity Resistace Exercise With Vascular OcclusionDokument7 SeitenRapid Increase in Plasma Growth Hormone After Low-Intensity Resistace Exercise With Vascular OcclusionFabiano LacerdaNoch keine Bewertungen
- BIOL 0211 - Lab Report 4 - Blood PressureDokument7 SeitenBIOL 0211 - Lab Report 4 - Blood PressureFIYINNoch keine Bewertungen
- Central Mechanisms Cardiovascular System Short and Long TermDokument12 SeitenCentral Mechanisms Cardiovascular System Short and Long Termsilvio da costa guerreiroNoch keine Bewertungen
- Takarada 2000Dokument10 SeitenTakarada 2000Alejandro Albert RequesNoch keine Bewertungen
- Robert D. Foreman Et Al - Modulation of Intrinsic Cardiac Neurons by Spinal Cord Stimulation: Implications For Its Therapeutic Use in Angina PectorisDokument9 SeitenRobert D. Foreman Et Al - Modulation of Intrinsic Cardiac Neurons by Spinal Cord Stimulation: Implications For Its Therapeutic Use in Angina PectorisLuammmNoch keine Bewertungen
- Effects of Exercise On Hypertension - From Cells To Physiological Pescatello 2015Dokument341 SeitenEffects of Exercise On Hypertension - From Cells To Physiological Pescatello 2015Daniel LópezNoch keine Bewertungen
- Central Venous Pressure: Its Clinical Use and Role in Cardiovascular DynamicsVon EverandCentral Venous Pressure: Its Clinical Use and Role in Cardiovascular DynamicsNoch keine Bewertungen
- Petrie 2015Dokument34 SeitenPetrie 2015Sebastian GiovanniniNoch keine Bewertungen
- Effects of Continuous Passive Motion On Reversing The Adapted Spinal Circuit in Humans With Chronic Spinal Cord InjuryDokument7 SeitenEffects of Continuous Passive Motion On Reversing The Adapted Spinal Circuit in Humans With Chronic Spinal Cord InjuryJoy SantosNoch keine Bewertungen
- Strengthening StrokeDokument23 SeitenStrengthening StrokePedro FonsecaNoch keine Bewertungen
- Life Sciences: F.S. Zamo, V.G. Barauna, S. Chiavegatto, M.C. Irigoyen, E.M. OliveiraDokument7 SeitenLife Sciences: F.S. Zamo, V.G. Barauna, S. Chiavegatto, M.C. Irigoyen, E.M. OliveirarodrigodaliascienceNoch keine Bewertungen
- 1996 Nonlinear Control of Heart Rate Variability in Human InfantsDokument6 Seiten1996 Nonlinear Control of Heart Rate Variability in Human InfantsSP507Noch keine Bewertungen
- Chronic Interactions Between Carotid Baroreceptors and Chemoreceptors in Obesity HypertensionDokument14 SeitenChronic Interactions Between Carotid Baroreceptors and Chemoreceptors in Obesity HypertensionCaesar Catalin CaratasuNoch keine Bewertungen
- Ankle Cryotherapy Facilitates SoleusDokument6 SeitenAnkle Cryotherapy Facilitates SoleusRamiro Avendaño RebolledoNoch keine Bewertungen
- Progressive Aortic Stiffness in Aging C57Bl-6 Mice Displays Altered Contractile Behaviour and Extracellular Matrix ChangesDokument11 SeitenProgressive Aortic Stiffness in Aging C57Bl-6 Mice Displays Altered Contractile Behaviour and Extracellular Matrix Changesender000Noch keine Bewertungen
- 2019 Journal of Surgical ResearchDokument8 Seiten2019 Journal of Surgical ResearchFernando ZanoniNoch keine Bewertungen
- Bondgraph Published CardioVascular 5Dokument24 SeitenBondgraph Published CardioVascular 5AhmedNoch keine Bewertungen
- Raven Et Al-2006-Experimental PhysiologyDokument13 SeitenRaven Et Al-2006-Experimental PhysiologyJesus Maturana YañezNoch keine Bewertungen
- The Journal of Physiology - 2000 - Steensberg - Production of Interleukin 6 in Contracting Human Skeletal Muscles CanDokument6 SeitenThe Journal of Physiology - 2000 - Steensberg - Production of Interleukin 6 in Contracting Human Skeletal Muscles CanPia GrzegorczykNoch keine Bewertungen
- Exercise PhysiologyDokument6 SeitenExercise PhysiologyMunazzah IjazNoch keine Bewertungen
- Bahan Inc TranslateDokument8 SeitenBahan Inc TranslateDedi Irawandi Angela NursisNoch keine Bewertungen
- 1 Physiology and Pathophysiology of Thoracic Sympathetic BlockadeDokument7 Seiten1 Physiology and Pathophysiology of Thoracic Sympathetic BlockadeFarid AkbarNoch keine Bewertungen
- Am J Physiol Regul Integr Comp Physiol 2001 - BadrDokument6 SeitenAm J Physiol Regul Integr Comp Physiol 2001 - BadrTony LeeNoch keine Bewertungen
- Transcutaneous Electrical Nerve Stimulation Versus Baclofen in SpasticityDokument9 SeitenTranscutaneous Electrical Nerve Stimulation Versus Baclofen in SpasticityArkar SoeNoch keine Bewertungen
- Cardio-Respiratory Effects of Change of Body Position: The Circulatory SystemDokument14 SeitenCardio-Respiratory Effects of Change of Body Position: The Circulatory SystemCarla Monique SartoNoch keine Bewertungen
- Cardiovascular System: Lecture 5 (Part I-II) September 28, 2005 October 5, 2005 EXS 558 Dr. MoranDokument44 SeitenCardiovascular System: Lecture 5 (Part I-II) September 28, 2005 October 5, 2005 EXS 558 Dr. MoraneliseudesafateNoch keine Bewertungen
- 1 s2.0 S0735109708005676 MainDokument9 Seiten1 s2.0 S0735109708005676 MainAprilleo ViedroNoch keine Bewertungen
- Acute Hypotensive Response To Continuous and Accumulated Isocaloric Aerobic BoutsDokument8 SeitenAcute Hypotensive Response To Continuous and Accumulated Isocaloric Aerobic BoutsLeticia N. S. NevesNoch keine Bewertungen
- Cvs Group4Dokument14 SeitenCvs Group4Lilian EdeniNoch keine Bewertungen
- Near-Infrared Spectroscopy Measures of Sternocleidomastoid Blood Flow During Exercise and HyperpnoeaDokument12 SeitenNear-Infrared Spectroscopy Measures of Sternocleidomastoid Blood Flow During Exercise and HyperpnoeaRobsonBorgesNoch keine Bewertungen
- ESTUDIO - El Vendaje Neuromuscular Reduce La Presion Arterial en La Hipertension Arterial SistemicaDokument3 SeitenESTUDIO - El Vendaje Neuromuscular Reduce La Presion Arterial en La Hipertension Arterial SistemicainfodhNoch keine Bewertungen
- Circulation 1992 Hirsch 1566 74Dokument10 SeitenCirculation 1992 Hirsch 1566 74gunnasundaryNoch keine Bewertungen
- Pathophysiology / Pharmacology: Cardiac PhysiologyDokument6 SeitenPathophysiology / Pharmacology: Cardiac Physiologyjazzdoc007Noch keine Bewertungen
- Parkinsonism and Related Disorders: David A. Low, Ekawat Vichayanrat, Valeria Iodice, Christopher J. MathiasDokument5 SeitenParkinsonism and Related Disorders: David A. Low, Ekawat Vichayanrat, Valeria Iodice, Christopher J. MathiasRafael Yokoyama FecchioNoch keine Bewertungen
- Monitoreo Hemodinamico Funcional PinskyDokument23 SeitenMonitoreo Hemodinamico Funcional PinskyJuan CarrascoNoch keine Bewertungen
- Natural Course of Initially Non-Operated Cases of Acute Subdural Hematoma The Risk Factors of Hematoma Progression (A. Nurul Amiruddin c11109153)Dokument9 SeitenNatural Course of Initially Non-Operated Cases of Acute Subdural Hematoma The Risk Factors of Hematoma Progression (A. Nurul Amiruddin c11109153)nyuwwchocolavaNoch keine Bewertungen
- Algorythm For Metabolic AlkalosisDokument1 SeiteAlgorythm For Metabolic AlkalosisabhivnairNoch keine Bewertungen
- Ventilator-Associated Pneumonia in The ICUDokument8 SeitenVentilator-Associated Pneumonia in The ICUnyuwwchocolavaNoch keine Bewertungen
- Algorythm For Metabolic AlkalosisDokument1 SeiteAlgorythm For Metabolic AlkalosisabhivnairNoch keine Bewertungen
- Diving Medicine For Scuba DiversDokument371 SeitenDiving Medicine For Scuba Diversboca19660% (1)
- Ventilator-Associated Pneumonia in The ICUDokument8 SeitenVentilator-Associated Pneumonia in The ICUnyuwwchocolavaNoch keine Bewertungen
- Severe Atopic DermatitisDokument6 SeitenSevere Atopic DermatitisnyuwwchocolavaNoch keine Bewertungen
- Dis.-2012-De Oliveira-1714-9Dokument6 SeitenDis.-2012-De Oliveira-1714-9nyuwwchocolavaNoch keine Bewertungen
- Baro TraumaDokument4 SeitenBaro TraumanyuwwchocolavaNoch keine Bewertungen
- Dermatitis AtopikDokument7 SeitenDermatitis AtopiknyuwwchocolavaNoch keine Bewertungen
- The Pathogenesis of The Diabetic Foot UlcerDokument29 SeitenThe Pathogenesis of The Diabetic Foot UlcernyuwwchocolavaNoch keine Bewertungen
- Pityriasis Lichenoides Chronica in Black PatientDokument5 SeitenPityriasis Lichenoides Chronica in Black PatientnyuwwchocolavaNoch keine Bewertungen
- Journal of Mycosis FungoidesDokument4 SeitenJournal of Mycosis FungoidesnyuwwchocolavaNoch keine Bewertungen
- Atopic Dermatitis .Dokument7 SeitenAtopic Dermatitis .nyuwwchocolavaNoch keine Bewertungen
- Dis.-2012-De Oliveira-1714-9Dokument6 SeitenDis.-2012-De Oliveira-1714-9nyuwwchocolavaNoch keine Bewertungen
- Fneur 04 00142Dokument7 SeitenFneur 04 00142nyuwwchocolavaNoch keine Bewertungen
- Pityriasis LichenoidesDokument0 SeitenPityriasis LichenoidesnyuwwchocolavaNoch keine Bewertungen
- Dis.-2012-De Oliveira-1714-9Dokument6 SeitenDis.-2012-De Oliveira-1714-9nyuwwchocolavaNoch keine Bewertungen
- Journal of Mycosis FungoidesDokument4 SeitenJournal of Mycosis FungoidesnyuwwchocolavaNoch keine Bewertungen
- BAD Specials BookletDokument12 SeitenBAD Specials BookletzfjasimNoch keine Bewertungen
- Improving Outcomes On Urologic Cancer PatientsDokument148 SeitenImproving Outcomes On Urologic Cancer PatientsMaghfirahEkasariLaitjinaraNoch keine Bewertungen
- Atopic Dermatitis (Eczema)Dokument4 SeitenAtopic Dermatitis (Eczema)nyuwwchocolavaNoch keine Bewertungen
- Severe Atopic DermatitisDokument6 SeitenSevere Atopic DermatitisnyuwwchocolavaNoch keine Bewertungen
- Pityriasis Lichenoides Chronica in Black PatientDokument5 SeitenPityriasis Lichenoides Chronica in Black PatientnyuwwchocolavaNoch keine Bewertungen
- UVa, PUVA PLDokument5 SeitenUVa, PUVA PLnyuwwchocolavaNoch keine Bewertungen
- P e - 1-Prefi PDFDokument12 SeitenP e - 1-Prefi PDFSairah Camille ArandiaNoch keine Bewertungen
- Exercise LabDokument3 SeitenExercise LabJonatan LeflerNoch keine Bewertungen
- PHYED-6101 Physical FitnessDokument65 SeitenPHYED-6101 Physical FitnessJSMMLSNoch keine Bewertungen
- A Review of Fluid and Hydration in Competitive TennisDokument11 SeitenA Review of Fluid and Hydration in Competitive TennisSilvio DantasNoch keine Bewertungen
- Effortless ExerciseDokument148 SeitenEffortless ExerciseTempoShire100% (1)
- PT Karuniajaya Andalan Prima: Stress Test ECGDokument16 SeitenPT Karuniajaya Andalan Prima: Stress Test ECGRay FNNoch keine Bewertungen
- Heart Rate Training Customize Your Training Based On IndividualDokument273 SeitenHeart Rate Training Customize Your Training Based On IndividualAfrizal Fauziansyah100% (4)
- Neonatal Patient Monitor en C60 V1.2Dokument2 SeitenNeonatal Patient Monitor en C60 V1.2Surta DevianaNoch keine Bewertungen
- Aerobic ExerciseDokument10 SeitenAerobic ExerciseGeorge OstNoch keine Bewertungen
- Nursing: Heart DisorderDokument68 SeitenNursing: Heart DisorderJhun Echipare100% (1)
- Especificaciones Monitor N15 MindrayDokument4 SeitenEspecificaciones Monitor N15 MindrayAnielaNoch keine Bewertungen
- Operator Manual Corival V2 English: Lode BV Groningen, The NetherlandsDokument31 SeitenOperator Manual Corival V2 English: Lode BV Groningen, The NetherlandsMauricioDinizNoch keine Bewertungen
- Physical Fitness & Longevity TestsDokument17 SeitenPhysical Fitness & Longevity TestsmrludiNoch keine Bewertungen
- Collins1993 Are Adaptations To Combined Endurance and Strength Training Affected by The Sequence of TrainingDokument8 SeitenCollins1993 Are Adaptations To Combined Endurance and Strength Training Affected by The Sequence of TrainingKatherine Nicole Díaz DelgadoNoch keine Bewertungen
- Immediate Effect of Nadi Shodhana Pranayama On Blood Glucose, Heart Rate and Blood PressureDokument6 SeitenImmediate Effect of Nadi Shodhana Pranayama On Blood Glucose, Heart Rate and Blood PressureDr. Manoranjan TripathyNoch keine Bewertungen
- Accepted: The Copenhagen Soccer Test: Physiological Response and Fatigue DevelopmentDokument37 SeitenAccepted: The Copenhagen Soccer Test: Physiological Response and Fatigue DevelopmentCesar Vinicius Santana MartineNoch keine Bewertungen
- Reformer User ManualDokument26 SeitenReformer User ManualpmurkuteNoch keine Bewertungen
- Design and Fabrication of Arduino BasedDokument145 SeitenDesign and Fabrication of Arduino BasedAndreea IlieNoch keine Bewertungen
- Prep U Exam #1 Adult 1Dokument14 SeitenPrep U Exam #1 Adult 1Adriana RemedioNoch keine Bewertungen
- Direction: Read Each Question Very Carefully. Choose The Best Answer From The Given Choices by Shading TheDokument5 SeitenDirection: Read Each Question Very Carefully. Choose The Best Answer From The Given Choices by Shading TheAe BreyNoch keine Bewertungen
- Jobfit Work Fitness Assessment Protocol - May 2016 PDFDokument16 SeitenJobfit Work Fitness Assessment Protocol - May 2016 PDFsafiyaNoch keine Bewertungen
- Training Zone Calculations: Run Cycle SwimDokument7 SeitenTraining Zone Calculations: Run Cycle SwimMoreno LuponiNoch keine Bewertungen
- Sleep Study Test: PSG Summary ReportDokument12 SeitenSleep Study Test: PSG Summary Reportkuwar palNoch keine Bewertungen
- Neuro-Cardiac-guided TMSDokument11 SeitenNeuro-Cardiac-guided TMSRafael MoreiraNoch keine Bewertungen
- What Tempo Runs and Threshold Running Are All AboutDokument1 SeiteWhat Tempo Runs and Threshold Running Are All AboutCharyyar BayramovNoch keine Bewertungen
- p90x ExcelDokument288 Seitenp90x ExcelCristhian Camilo Gómez NarváezNoch keine Bewertungen
- Benjamin III Bidang - B. Fit Cs - Module 1 Obl - CBLDokument20 SeitenBenjamin III Bidang - B. Fit Cs - Module 1 Obl - CBLBENJAMIN III BIDANGNoch keine Bewertungen
- Manual Work Design: From: Niebel's Methods, Standards, and Work Design, Twelfth EditionDokument147 SeitenManual Work Design: From: Niebel's Methods, Standards, and Work Design, Twelfth EditionzoerydasNoch keine Bewertungen
- Packet 2 Teaching P.E. For Elementary GradesDokument42 SeitenPacket 2 Teaching P.E. For Elementary GradesJia DagandanNoch keine Bewertungen
- Nonstress Test and Contraction Stress Test - UpToDateDokument27 SeitenNonstress Test and Contraction Stress Test - UpToDatekimberlyNoch keine Bewertungen