Beruflich Dokumente
Kultur Dokumente
Emergency Laparotomy
Hochgeladen von
samm kinhgCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Emergency Laparotomy
Hochgeladen von
samm kinhgCopyright:
Verfügbare Formate
Title of Guideline
Contact Name and Job Title
Directorate & Speciality
Date of submission
Date on which guideline must be reviewed
Explicit definition of patient group to which it
applies
Abstract
Key Words
Statement of the evidence base of the
guideline has the
guideline been peer reviewed by colleagues?
Evidence base: (1-5)
1a
meta analysis of randomised
controlled trials
1b
at least one randomised
controlled trial
2a
at least one well-designed
controlled study without
randomisation
2b
at least one other type of welldesigned quasi-experimental
study
3
well designed nonexperimental descriptive studies
(ie comparative / correlation and
case studies)
4
expert committee reports or
opinions and / or clinical
experiences of respected
authorities
5
recommended best practise
based on the clinical
experience of the guideline
developer
Consultation Process
Target audience
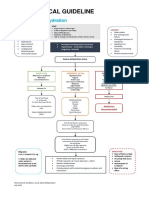
Management of the emergency laparotomy
patient:
A practical guideline
Dr V C Banks Consultant AICU & Anaesthetics,
Dr J Mole Consultant Anaesthetist
Dr G Pipe SPR Anaesthetics
Specialist Support and Digestive Diseases
and Thoracics directorates.
December 2013
December 2016
Patients undergoing an Emergency Laparotomy
The emergency laparotomy patients have a high
mortality and this guideline helps with the
preparation, resuscitation and care of
Emergency Laparotomy patients.
Emergency Laparotomy
Septic surgical patient
Critical Care
Yes,
Evidence base is level 2 as well as national best
practice
Consulted with surgical directorate, anaesthetics
and critical care departments.
Doctors, Anaesthetists and Surgeons involved in
the care of patients undergoing Emergency
Laparotomy
This guideline has been registered with the trust. However, clinical guidelines are guidelines
only. The interpretation and application of clinical guidelines will remain the responsibility of the
individual clinician. If in doubt contact a senior colleague or expert. Caution is advised when
using guidelines after the review date.
Page1of25
EmergencyLaparotomyGuidelineNUHVCBv3
Management of the emergency laparotomy patient: a practical
guideline
Pre-operative care: (see Appendix 1: Emergency Surgery Admission
Booklet)
INITIAL RISK ASSESMENT BY CLINICIAN (A&E/ WARD)
1. Full history, examination and baseline investigations
FBC, U&E, LFTs, Coagulation, Lipase, Glucose and G&S
hcg in ALL females of reproductive age
Blood cultures if febrile
ABG including lactate
ECG, consider troponin
Urinalysis/ MSU
Hourly Early Warning Scores
2. Is this patient HIGH RISK of significant Morbidity/ Mortality?
(any of the risk factors) 1
SIRS >2 + 1 organ dysfunction
Lactate > 2
EWS > 4
Long term steroids/immune-suppressed
Age 70
Age > 50 and;
Creatinine > 130mol or dialysis dependent
Diabetes
Significant CVS/Respiratory disease
Urgent surgery/Re-do laparotomy
Predicted PPOSSUM mortality > 5%
ASA 3 + 1 organ dysfunction
ASA 4/5
Page2of25
EmergencyLaparotomyGuidelineNUHVCBv3
3. Recognise and Treat Sepsis
Septic patients have a much higher mortality than other patients
undergoing emergency surgery 2
Once a patient has been identified as septic, give appropriate
antibiotics within 1 hour of diagnosis of sepsis, every hour delay
in antibiotics increases mortality.3 Consult with microbiology
guidelines as per Intranet.
Source control is very important. Early senior surgical input is
required to decrease time to theatre. In surgery, the longer a septic
patient remains without source control, the higher the mortality.
Reassess the patient regularly - BEWARE LOW RISK patients
can deteriorate rapidly to become HIGH RISK. Review EWS.
Provide analgesia within an hour of first medical assessment if
required.
Consider NG tube if bowel obstruction likely.
Page3of25
EmergencyLaparotomyGuidelineNUHVCBv3
4. Timelines if HIGH RISK PATIENT 1
Refer to Surgical Registrar to review within 30 mins
Discussion with Consultant - within 1 hour of Surgical
Registrar review
Book CT scan (indicate HIGH RISK status)
CT scan reported - within 5 hours of booking
5. If Surgery is indicated for HIGH RISK PATIENT
Calculate estimated PPOSSUM score
(http://www.riskprediction.org.uk/)
Inform Theatre Co-coordinator & 3rd on Anaesthetist QMC/
2nd on NCH
STATE: High Risk status, EWS, PPOSSUM score & Lactate
3rd on call to discuss case with Consultant and Critical Care
Arrival in theatre within 1 hour of decision to operate
6. Timelines for LOWER RISK PATIENT 1
(Beware patients often deteriorate and become HIGH RISK)
Discussed with Consultant - within 12 hours of Surgical
Registrar review
Time CT scan reported within 24 hours of MRCS review
Time reviewed by Consultant within 24 hours of admission
7. If Surgery is indicated for LOWER RISK PATIENT
Calculate estimated PPOSSUM score
(http://www.riskprediction.org.uk/)
Inform Theatre Co-coordinator & on call Anaesthetist
STATE: Lower Risk status, EWS, PPOSSUM score &
Lactate
Arrival in theatre within 12 hours of decision to operate
Page4of25
EmergencyLaparotomyGuidelineNUHVCBv3
Management of the emergency laparotomy patient: a practical
guideline
Anaesthesia
Pre-operative care
1. Emergency anaesthetic service should be consultant led at all
times 4
2.
3.
4.
5.
a. If PPOSSUM score > 10% mortality Consultant
Anaesthetist and Surgeon involvement is mandatory
b. No SHO/CT to anaesthetise an emergency laparotomy
patient on their own
c. High risk patients to have a consultant anaesthetist present
or anaesthetist whom the responsible consultant knows to be
competent to undertake the case
Plan ahead and discuss procedure with surgical team and options
for limiting surgery if instability
If Estimated Blood Loss expected to be > 1.5L cell salvage should
be available
Post-operative care should be planned as far as possible preoperatively
Critical care needs to be involved early, preferably before surgery
or other major interventions, such as prolonged interventional
radiological procedures.
Intra-operative care
1. Ventilation
If likely ITU admission insert size 8 coett tube for females
and size 9 for men (unless unable)
Aim for SaO2 > 94% 5
Consider PEEP of at least 5cmH2O
Aim for Tidal Volume 5-7 ml/kg (Ideal Body weight)
Consider pressure control ventilation to minimise peak
airway pressure
Aim Pmax < 30cmH20
Page5of25
EmergencyLaparotomyGuidelineNUHVCBv3
2. Antibiotics prophylaxis
Consider escalation/addition - (consult microbiology)
Antifungal if re-laparotomy or significant peritoneal soiling
(800mg Fluconazole)
Gentamicin if systemic sepsis (3-5mg/kg) (Check not
already given elsewhere)
3. Please use Goal Directed therapy with a cardiac output monitor &
invasive lines if major Emergency surgery 6
Aim Stroke Volume Variation < 10%
Aim MAP > 65 mmHg
Aim UO + 0.5ml/kg/hr
CVP > 8 mmHg
Haematocrit > 30%
Saturation central venous O2 >70% (ScvO2)
Lactate < 2
BM> 4
Have a low threshold for inotropes/vasopressors to avoid
excessive fluid administration ( Noradrenaline infusion
5mg/40mls Normal Saline)
Page6of25
EmergencyLaparotomyGuidelineNUHVCBv3
LiDCO
O algoritthm
Pagge7of25
ncyLaparoto
omyGuidelin
neNUHVCBv3
Emergen
Oesophageal Dopplerr Algorith
hm
Pagge8of25
ncyLaparoto
omyGuidelin
neNUHVCB v3
Emergen
Das könnte Ihnen auch gefallen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5795)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1091)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Index To SSRI StoriesDokument100 SeitenIndex To SSRI StoriesGaryBurlesonNoch keine Bewertungen
- Review Notes 2000 - Geriatrics PDFDokument12 SeitenReview Notes 2000 - Geriatrics PDFeset5Noch keine Bewertungen
- Chronic Kidney DiseaseDokument12 SeitenChronic Kidney DiseaseRoseben SomidoNoch keine Bewertungen
- Electroconvulsive Therapy ManagementDokument32 SeitenElectroconvulsive Therapy ManagementNaeem KhanNoch keine Bewertungen
- AdultDehydrationGuidelineJuly2015 PDFDokument3 SeitenAdultDehydrationGuidelineJuly2015 PDFmarselamgeNoch keine Bewertungen
- Pulmonary Function TestDokument87 SeitenPulmonary Function TestRiry AmbarsaryNoch keine Bewertungen
- Ortho Pedo Traumatic InjuriesDokument4 SeitenOrtho Pedo Traumatic InjurieschloieramosNoch keine Bewertungen
- Letter To VA From The Quinism FoundationDokument2 SeitenLetter To VA From The Quinism FoundationWUSA9 TVNoch keine Bewertungen
- Character Styles Introduction PDFDokument4 SeitenCharacter Styles Introduction PDFKOSTAS BOUYOUNoch keine Bewertungen
- Dimensions of Anxiety Symptoms in Romanian Young Adult Subjects From Brasov CountyDokument4 SeitenDimensions of Anxiety Symptoms in Romanian Young Adult Subjects From Brasov CountylmplmpNoch keine Bewertungen
- ResumeDokument1 SeiteResumeapi-398428706Noch keine Bewertungen
- Management of Gastric Variceal Hemorrhage: S K Sarin, Sanjay NegiDokument4 SeitenManagement of Gastric Variceal Hemorrhage: S K Sarin, Sanjay NegiSa 'ng WijayaNoch keine Bewertungen
- Internship Assign 1Dokument2 SeitenInternship Assign 1s.raza.a23Noch keine Bewertungen
- Commonly Prescribed Drugs in PakistanDokument15 SeitenCommonly Prescribed Drugs in PakistanMaryam Asif100% (1)
- Acanthosis NigricansDokument32 SeitenAcanthosis NigricansZeliha TürksavulNoch keine Bewertungen
- Preceptor EvaluationDokument2 SeitenPreceptor Evaluationapi-380898658Noch keine Bewertungen
- Kawasaki's DiseaseDokument3 SeitenKawasaki's DiseaseDavid ChengNoch keine Bewertungen
- Leukaemias: A Review: Aetiology and PathogenesisDokument6 SeitenLeukaemias: A Review: Aetiology and PathogenesisCiro Kenidy Ascanoa PorrasNoch keine Bewertungen
- SLIDE03 FluidElectrolyteImbalanceDokument57 SeitenSLIDE03 FluidElectrolyteImbalanceGrace Amato-Moore100% (1)
- Cardiac Function TestDokument8 SeitenCardiac Function Testramanrajesh83100% (2)
- Charka Sutra PDFDokument72 SeitenCharka Sutra PDFsolanki parth100% (6)
- Farmakologi Obat Hemostasis & AntikoagulanDokument19 SeitenFarmakologi Obat Hemostasis & AntikoagulanamirahNoch keine Bewertungen
- Yin and Yang PolaritiesDokument33 SeitenYin and Yang Polaritiesdanielherciu100% (1)
- Rotator Cuff BookDokument37 SeitenRotator Cuff BookAlexandra DimitrakouNoch keine Bewertungen
- Homa TherapyDokument107 SeitenHoma TherapyNicole StevensNoch keine Bewertungen
- Gua ShaDokument41 SeitenGua ShaFerencne Hanis100% (2)
- Pain Free A Revolutionary Method For Stopping Chronic PainDokument2 SeitenPain Free A Revolutionary Method For Stopping Chronic Painmohsin_shaikh200150% (2)
- FILE STOK - OdsDokument162 SeitenFILE STOK - OdsAhmad GupongNoch keine Bewertungen
- Thesis CricketDokument32 SeitenThesis CricketShubham Aggarwal0% (2)
- Stepney, SharylDokument2 SeitenStepney, SharylSharyl Murphy StepneyNoch keine Bewertungen