Beruflich Dokumente
Kultur Dokumente
Acute Lymphocytic Leukemia
Hochgeladen von
Wendy EscalanteCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Acute Lymphocytic Leukemia
Hochgeladen von
Wendy EscalanteCopyright:
Verfügbare Formate
1 ACUTE LYMPHOCYTIC LEUKEMIA TO PROTEIN S DEFICIENCY (escalante-saac)
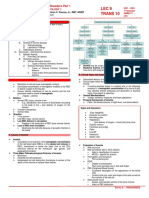
ACUTE LYMPHOCYTIC
LEUKEMIA
75%,25 %
Boys ,girls, 4
Results from an uncontrollable proliferation of immature cells
(lymphoblast), derived from the lymphoid stem cells.
the cell of origin is the precursor of b lymphocytes, in approximately _ of
all, & _ in t-lymphocytes.
all is most common in young children w/ _affected more than_.; the peak
incidence is _yrs. of age.
CLINICAL MANIFESTATIONS:
Immature leukocytes
_proliferate in the bone marrow & impede the development of normal
myeloid cells.
leukocytes, erythrocytes, &
as a result, normal hematopoiesis is inhibited , resulting in reduced
platelets.
number of _
low or high
Leukocyte count may either be _but there is always increased proportion
in immature cells.
liver and spleen
leukemic cell infiltration to other organs include from enlarged_; and
bone pain.
headache and vomiting
Infiltration of leukemic cells into the cns, patient may exhibit _from
meningeal involvement.
MEDICAL MANAGEMENT:
-complete remission
Expected outcome:
1. Chemotherapy
2. In adult all, allogenic
transplant
3. bmt or pbst offers a
chance for prolonged
remission, or even cure.
CHRONIC LYMPHOCYTIC
is a common malignancy in adults; the average age of diagnosis is 72
LEUKEMIA ( CLL)
yrs.
Europe
most common form of leukemia in _and us affecting more than 120,000
people.
asian
15
PATHOPHYSIOLOGY
b-lymphocytes.
fully mature
apoptosis
infrequent in _descent
people w/ cll may survive for _ yrs.
-cll is derived from malignant clone of _
- most of the leukemia cells are _
- these cells can escape _( progammed cell death), resulting in an
excessively accumulation of the cells in the bone marrow & circulation.
- early stage of cll, an elevated lymphocyte is seen w/c can exceed to_,
- _occurs as the lymphocytes are trapped w/in the lymph nodes.
- _can develop
- in later stages of the disease, _may develop.
- _can also occur at any stage.
100,000/mm3
Lymphadenopathy
hepatomegaly and
splenomegaly
anemia and
thrombocytopenia
autoimmune disease
CLINICAL MANIFESTATIONS:
Asymptomatic
- many clients are _and are diagnosed incidentally during p.e. or during
treatment for other disease.
Lymphocyte
- increased in _count is always present.
Lymph nodes
- enlargement of the _is common.
herpes zoster
- life threatening infections are common such as viral infection like_.
MEDICAL MANAGEMENT:
fludarabine (fludara), and
1. Chemotherapy agents _are often given in combination w/ the
cyclophospamide(cytoxan)
monoclonal antibody rituximab(rituxan).
5 yrs
- this chemotherapeutic agent can give_ Remissions in 70% of pts.w/ cll.
anviral agents and
2. Prophylactic use of _is important and need to continue for several
antibiotics
months after treatment ends.
3. _is given to selected patients w/ recurrent infection.
Immunoglobulin iv
ASSEESMENT:
1. Taking the health history identifying risk factors causing the disease.
2. Weakness & fatigue are common manifestations
3. Thorough systematic assessment of the patient (p.e.)
4. Analyze laboratory results: low platelet count can be dangerously low to cause active bleeding.
Baseline findings are compared to current results to determine progression of the disease.
5. Culture results should be reported immediately for prescribing specific antibiotics can be started or
revised
2 ACUTE LYMPHOCYTIC LEUKEMIA TO PROTEIN S DEFICIENCY (escalante-saac)
NURSING DIAGNOSIS:
1. Risk/ or actual infection & bleeding
2. Risk for impaired skin integrity r/t toxic effects of chemotherapy; alterd nutrition; immobility
3. Impaired gas exchange.
4. Acute pain and discomfort r/t mucositis, leukocyte infiltration of systemic tissues, fever, infection
5. Altered nutrition, less than body requirements, r/t hypermetabolic state, anorexia,pain & nausea.
6. Hyperthermia r/t infection
7. Impaired physical mobility r/t anemia, protective isolation, fatigue.
8. Self-care deficit r/t fatigue, malise, and protective isolation.
9. Anxiety r/t knowledge deficit or uncertaintenty about future.
10. Disturbed body image r/t change in appearance, function, and role.
11. Grieving r/t anticipatory loss, and altered role functioning.
12. Knowledge deficit about the disease process.
PLANNING AND GOALS
Patient is free from complications and pain; attainment and maintenance of adequate nutrition, activity
tolerance, ability to provide self-care
NURSING INTERVENTIONS
1. Preventing or managing infection and bleeding.
2. Managing mucositis
3. Improve nutritional intake
- provide oral care before and after eating.
- administer pain reliever before meal.
- encourage small frequent feedings w/ food in moderate temperature.
- monitor daily body weight for evaluation of food intake.
- encourage nutritional supplements.
- tpn is required for adequate nutrition.
4. Easing pain and discomfort
- analgesics/antipyretics are given to relieve pain and fever.
- sponging w/ cool water is useful, compared to ice packs w/c should be avoided.
- gentle back and shoulder massage may be provided for comfort.
- nurses should implement creative strategies that permit uninterrupted sleep for at least few hrs.while still
administering
medication on time.
5. Decreasing fatigue and deconditioning
- nursing interventions should focus on assisting the patient to establish a balance between activity and rest.
- at a minimum, patients should be encouraged to sit up on bed, and gradually increased according to tolerance
of the patient.
MAYDA PA INI KUTOB 10 :p
EVALUATION
1. Shows no evidence for infection.
6. Has less fatigue and increased level of activity.
2. Experience no bleeding.
7. Participates in self-care.
3. Has intact oral mucous membrane.
8. Maintains fluid and electrolyte balance.
4. Attains optimal level of nutrition.
9. Discuss hope for peaceful death.
5. Reports satisfaciton with pain and
10.absence of complications.
comfort level.
are neoplasms of cells of lymphoid origin.
LYMPHOMA
lymphoma
lymphoma
1. HODGKIN
LYMPHOMA
Unicentric
reed-stemberg cells
men than in women
chronic immunosuppressive
ETIOLOGY
Unknown
familial
these tumors usually starts in lymph nodes but can involve lymphoid
tissue in the spleen, gi tract,, liver,, or bone marrow.
can be classified as hodgkin lymphoma and non-hodgkin lymphoma.
*is a rare malignancy, _in origin initiates in a single node.
* the disease spreads by contiguous extension along the lymphatic
system.
* the malignant cell of hodgkin lymphoma is the_, a gigantic tumor
& thought to be of immature lymphoid origin.
*more common in_, and has a familial pattern.
*more commonly seen in patients receiving _drugs..
cells
*cause is _
*has a _pattern
* maybe drug-induced risk
PATHOPHYSIOLOGY:
reed-stenberg cell
CLINICAL
MANIFESTATIONS:
*the disease spreads by contiguous extension along the lymphatic
system.
*the pathologic hallmark & essential diagnostic criterion is the_.
*_ enlargement of one or more lymph nodes on one side of the neck, w/c
3 ACUTE LYMPHOCYTIC LEUKEMIA TO PROTEIN S DEFICIENCY (escalante-saac)
Painless
cervical, sub clavicular, &
mediastinal
pruritus, unknown
brief but severe pain
is firm but not hard.
*the most common site for lymphadenopathy are the _nodes.
* a mediastinal mass may be seen on x-ray
*_ is common & cause is_.
*some patients experience _after drinking alcohol at the site of tumor,
and cause is unknown.
* _is the most common hematologic finding.
mild anemia
ASSESSMENT AND
DIAGNOSTIC FINDINGS:
>red-sternberg cell
MEDICAL MANAGEMENT:
*Cure
*Short course chemotherapy
NURSING MANAGEMENT:
*tobacco, alcohol, and
exposure to environmental
carcinogens, and excessive
sunlight.
2. NON-HODGKIN
LYMPHOMAS
*Heterogenous
*b lymphocytes
*immunodeficiencies or
autoimmune d/o
CLINICAL
MANIFESTATIONS:
*Lymphadenopathy
*fever, drenching night
sweats, unintentional weight
loss
ASSESSMENT &
DIAGNOSTIC FINDINGS:
*histopathology
* ct and pet scans
MEDICAL MANAGEMENT:
> Chemotherapy
> cranial radiation or
intrathecalchemo therapy
NURSING MANAGEMENT:
*excisional lymph node biopsy w/ findings of the _
*once diagnosis is confirmed and histologic type is done, it is necessary
to assess the extent of the disease or staging.
*in the p.e.,it is important to assess lymph node chains, as well as the
size of the spleen and liver.
*a chest x-ray, ct scan of the chest, abdomen, and pelvis are crucial to
identify the extent of lymphadenopathy within the regions.
*other lab tests, cbc, platelet count, esr, and liver and function studies.
The genenral goal of treatment of hodgkin lymphoma is_.
1._, (2-4 mos) followed by radiation therapy to the involves site.
2. A combination of abvd is the standard for more advanced disease
( stage iii & iv, & all stages w/ b symptoms); this include
Adriamycin, bleomycin, vinblastin, dacrvacin.
1. The nurse should encourage patient to reduce other factors that
increase the risk of developing second cancers, such as use of _
2. The nurse should provide education about relevant self-care strategies
and disease management.
*are a _group of cancers that originate from the neoplastic growth of
lymphoid tissue.
*most nhls , involve malignant_, the lymphoid tissue involved are largely
infiltrated with malignant cells.
*the incidence of nhl has increased in people with_; prior treatment of ca,
prior organ transplant, viral infections, and exposure to carcinogens.
*_ is the most common
*b symptoms like_.
* lymphomatous masses can compromise organ function like mass at
mediastinum may compromise respiratory function.
*_ of the malignant cells
* _to identify stage and extent of tissue involvement.
treatment is determined by the classification of the disease, the stage of
the disease, prior treatment, and ability of the patient to tolerate
treatment.
1. _
2. For central nervous system involvement, _is used in addition to
systemic
Chemotherapy.
1. Since patients with nhl undergo chemotherapy, nursing mgt is
focused on the side effects of chemo and radiation therapy.
BLEEDING DISORDERS
> trauma
*Results to failure of the hemostatic mechanisms.
*bleeding is commonly provoked by_.
4 ACUTE LYMPHOCYTIC LEUKEMIA TO PROTEIN S DEFICIENCY (escalante-saac)
*When the source is platelet or coagulation factor abnormalities, factor
abnormalities, the site of bleeding can be anywhere in the body.
*When the source is vascular abnormalities, the site of bleeding may be
more localized.
CLINICAL
MANIFESTATIONS:
> petechae
MEDICAL MANAGEMENT:
*abnormalities in the vascular system can give a localized bleeding.
*patients w/ platelets defect develop _w/c could be seen in groups.
*bleeding can be severe, bleeding can be oftenly stopped by application
of pressure at the site of bleeding.
*in contrast, bleeding from coagulation d/o do not tend to cause
superficial bleeding, instead, bleeding occurs deeper within the body.
( subcutaneous or im hematomas, hemorrhage into joint spaces).
- varies based on the underlying cause of the d/o.
- if bleeding is significant, blood products are indicated.
*a patient who is to undergo invasive procedure including tooth
extraction may need a transfusion prior to the procedure.
NURSING MANAGEMENT:
> bleeding
*clients should be closely monitored for signs of _and patient must be
taught on immediate measures to control bleeding.
*they need to understand the importance of avoiding activities that may
increase the risk for bleeding.
> petechiae
*it is necessary to make a routine exam to skin for signs of bleeding
tendencies like_.
*admitted patients are monitored for bleeding by testing all drainage
and excreta for occult blood.
*monitor v/s
1. THROMBOCYTHEMIA ( ESSENTIAL THROMBOCYTHENIA)
>600,000/mm3
* is stem cell d/o w/in the bone marrow, a marked increase in platelet
production, occurs w/ platelet count greater than _
*platelet size may be abnormal, but platelet survival is normal.
>in eryththrocytes,
*occasionaly, increase in platelet is accompanied by increased _
leukocytes both
*cause is _
> unknown
CLINICAL
*many patients are _
MANIFESTATIONS:
>asymptomatic
> platelet count
> exceeds 1 mil/mm3
> burning, warmth, and redness
> headache
> dvt, and pulmonary embolism
> minor or major hemorrhage
>1.5 mil/mm3
ASSESSMENT & DIAGNOSTIC
FINDINGS:
> platelets
> elevated( 600,000 mm3)
MEDICAL MANAGEMENT:
> low-dose aspirin
> Hydroxyurea
> Interferon alfa--2b
> platelet pheresis
NURSING MANAGEMENT:
> hemorrhage and thrombosis
> neurologic manifestations.
*elevated _on cbc
*symptoms most often occur when platelet count_.
when symptoms occur, they result in hemorrhage or vascular occlusion w/c may
affect large blood vessels, as well as microcirculation.
*the toxic effects of platelet substances include _in a localized distal area of the
extremities.
*_ is the most common neurologic manifestation w/c include ischemic attacks.
*most common form of thromboembolism include_.
*because the platelet are dysfunctional, _may occur.
*bleeding does not occur until unless platelet count exceeds_., due to deficiency
in von willebrand factor as the platelet count increase.
*cbc shows markedly large and abnormal _
*platelet count is consistently_.
1. In younger patients w/ no risk factor, _therapy may be sufficient to prevent
thrombotic complications but clients w/ history of gi bleeding asa is
contraindicated.
- asa can relieve the neurologic symptoms, eryththromyalgia, and visual
symptoms of primary thromcythenia.
2. _is effective in lowering the platelet count.
4. _has been shown to lower platelet counts by an unknown mechanism given
sc.
5. If there is the need for immediate reduction of platelet, _is done, to reduce
the amount of circulating platelet.
1. Patients should be taught about the accompanying risks for_.
2. Patient is informed of signs and symptoms of thrombosis, particularly the_
3. Risks factors for thrombosis are assessed, such as obesity, hypertension,
hyperlipidemia, and smoking; measures to diminish these factors are
encouraged.
4. Patients who are taking asa are informed of the risk for bleeding.
5. Patients who are taking inferon are taught on how to self-administer the
medication and manage side effects.
5 ACUTE LYMPHOCYTIC LEUKEMIA TO PROTEIN S DEFICIENCY (escalante-saac)
6. Patients who are taking hydroxyurea should have their cbc be monitored,
dosage is based on the platelet and wbc count.
2. SECONDARY THROMBOCYTOSIS
> platelet production
*inc._ is the primary mechanism of secondary or reactive thrombocytosis.
*platelet count is above normal, but in contrast with throbocythenia, an
inc.of more than 1 mil.is rare.
> rare
*symptoms of hemorrhage or thrombosis is_.
*risk factors/ conditions w/c can cause reactive increase in platelet,
infection, chronic inflammatory disease, ida, acute hemorrhage,
splenectomy.
3. THROMBOCYTOPENIA
> platelet level
*low_, can result from various factors: dec.production of platelets within
the bone marrow, inc.destruction of platelets, or inc.consumption of
platelets.
CLINICAL
MANIFESTATIONS:
*bleeding and petechiae do not occur w/ platelet count greater than_.
>50,000/mm3
*when the platelet count drops to less than_, petechiae can appear with
>20.000/ mm3
nasal and gingival bleeding.
*if platelet count is less than_, spontaneous,, potential fatal cns or gi
>5000
hemorrhage can occur.
ASSESSMENT AND
DIAGNOSTIC FINDINGS:
1. Bone marrow aspiration and biopsy.
2. Numerous genetic causes of thrombocytopenia have been
discovered, including autosomal dominant, autosomal recessive, and x> Peripheral smear
linked mutations.
3. _can easily determine platelet clumping as the cause of
thrombocytopenia.
MEDICAL MANAGEMENT:
1. Treatment of the cause: if due to platelet production is the cause, _may
> platelet transfusions
increase platelet count and stop bleeding. But if excessive destruction
occurs, splenectomy can be useful therapeutic intervention.
1. Prevent complications
NURSING INTERVENTION:
- avoid _containing drugs.
> asa and aspirin
-
do not give im injection
avoid insertion of catheter if possible
use oral laxatives
apply pressure to venipuncture sites for at least 5 mins.or until bleeding stops.
permit no flossing of teeth and no mouthwashes
avoid suctioning if possible.
lubricate lips w/ water soluble lubricant every 2 hrs.when awake.
discourage vigorous coughing and avoid blowing of the nose.
prevent falls by assisting patient during ambulation
4. IDIOPATIC THROBOCYTOPENIC PURPURA (ITP)
> common in children and
young women.
*is a disease that affects people of all ages, but is more _
*there are 2 forms of itp: acute itp occurs predominantly in children,
often appears 1-6 weeks after a viral infection;
Chronic itp is often diagnosed by exclusion of other causes of
thrombocytopenia.
PATHOPHYSIOLOGY:
*in patients w/ itp, antiplatelet autoantibodies that bind to platelets are
found in the blood.
* when the platelets are bound by the antibodies, the res or the
macrophage system ingest the platelets destroying them..
*body tries to compensate by increasing platelet production within the
marrow.
CLINICAL
MANIFESTATIONS:
> easy bruising, heavy menses,
petechiae
> intracranial hemorrhage
ASSESSMENT AND
DIAGNOSTIC FINDINGS:
>20,000/mm3
> h pylori
MEDICAL MANAGEMENT:
*_ appear on trunk and extremities signs of dry purpura.
*patients w/ wet purpura have the tendency to have_.
*decreased platelet count to as low as_.
*some patients may have _
goal of mgt is safe platelet count.
1. Treament is identifying the cause of itp, if it is a drug-induced itp, then
discontinue the drug.
6 ACUTE LYMPHOCYTIC LEUKEMIA TO PROTEIN S DEFICIENCY (escalante-saac)
> Immunosuppressive drugs
> cortecosteroids
> Iv immunoglobulin
> Splenectomy
> Thrombopoiesis-stimulating
protein romiplostin
* platelet transfusion
NURSING
INTERVENTIONS:
2._, block the binding receptors on macrophages so that the platelets are not
destroyed.
Ex. Imuran ( azathioprine).
3. Administration of _like prednisone.
4. _is commonly used to treat itp.
5. _can be done.
6. Administration of anti-d, binds to erythrocytes w/c are in turn destroyed by
the bodys macrophages. Anti-d produces a transient dec in hct.and inc.pletlet
count in many itp, but not to all types of itp.
7. _has been successfully used to treat chronic itp.
* _are to be avoided because the patients antiplatelet antibodies bind with the
transfused platelets causing them to be destroyed.
1. Assessment of patients lifestyle to determine risk of bleeding from activity.
2. A careful medication history is obtained including use of over the counter
drugs, herbs, supplements.
3. The nurse must assess for history of recent viral infections & reports of
headache or visual disturbances w/c may indicate intracranial hemorrhage.
4. All injections or rectal medications should be avoided because they can
stimulate bleeding.
5. Patients admitted to the hospital should be monitored closely of their v/s and
to include neurologic monitoring.
5. HEMOPHILIA
inherited bleeding d/o: hemophilia a and hemophilia b, w/c can be
differentiated by lab tests.
> Hemophilia A
> Hemophilia B
> x-linked traits
A. _- is caused by a genetic defect that results in deficient or
defective factor viii.
B. _, also called Christmas disease stems from deficient or defective
factor ix.
* both types of hemophilia are inherited as_, so almost affected patients
are males, females can be carriers, but are always asymptomatic.
*hemophilia is recognized in early childhood, usually in the toddler stage,
and diagnosed only if client sustained bleeding d/o from trauma.
CLINICAL
MANIFESTATIONS:
> trauma
> hemarthoses and
hematomas
MEDICAL MANAGEMENT:
> transfusion of factor viii
and ix
> plasmapheresis
> desmopressin
NURSING
INTERVENTIONS:
6. VIT K DEFICIENCY
> vit k
> malnourished
> antibiotics
*it is manifested by hemorrhages from various parts of the body.
Bleeding depends on the degree of factor deficiency, and extent of injury.
*hemorrhage may occur secondary to_.
*spontaneous hemorrhage may occur in severe deficiency of factor viii,
w/c may result to_.
*bleeding is also common in the git, kidneys, mucous membrane.
1. Replacement _depending on the deficiency.
*patients are given concentrate when they are actively bleeding and as a
preventive measure before an invasive procedure is done.
2. Patient may require_, or concurrent immunosuppressive therapy,
particularly in in the setting of significant.
3. Administration of_, induces a significant but transient rise in factor
viii levels, mechanism of action is still unknown.
1. Patient and family are help to cope up w/ the disease need to identify positive
aspects of their lives.
2. Patients are encouraged to be self-sufficient & to maintain independence by
preventing unnecessary trauma that can cause acute bleeding episodes and
temporarily affect with normal activities.
3. Patients must be taught for maintaining of optimal health.
4. Safety at home and in the workplace are emphasized in the health teachings.
5. Patients and family are taught on avoidance of drugs that may cause
bleeding as side effect of the drug.
*synthesis of many coagulation factors depends on _
*vit k deficiency is common in _individuals
*Prolonged use of some_ decreases the intestinal flora that produce vit k,
depleting vit.k stores.
*Administration of oral vit k or sc injection can correct the deficiency
quickly, reflected w/ normalization of protrombin time.
6. DISSEMINATED INTRAVASCULAR COAGULATION (DIC)
> sepsis, trauma, ca, shock,
*is not a disease, but a sign of an underlying condition like_.
toxins or allergic reactions
> altered
*in dic, normal hemostatic mechanism is _
* the inflammatory response generated by the underlying disease
initiates the process of coagulation w/in the vasculature.
*the natural anticoagulation pathways w/in the body are simultaneously
7 ACUTE LYMPHOCYTIC LEUKEMIA TO PROTEIN S DEFICIENCY (escalante-saac)
impaired, and fibro lytic system is suppressed so that tiny clots are
formed in the microcirculation.
CLINICAL
MANIFESTATIONS:
ASSESSMENT AND
DIAGNOSTIC FINDINGS:
MEDICAL MANAGEMENT:
NURSING MANAGEMENT:
PROTEIN C DEFICIENCY
>protein c
> thrombosis
> asymptomatic
> purified protein c
concentrate
> warfarin and other anticoagulant
PROTEIN S DEFICIENCY
> protein s
> protein c
>15 yrs.old.
> liver disease, pregnancy,
hiv infection, nephritic
syndrome.
ACQUIRED PROTEIN C
RESISTANCE
NURSING MANAGEMENT:
*patient may bleed from the mucous membrane, venipuncture sites, or gi
and urinary tracts.
*patient usually develop multiple organ dysfunction syndrome and may
develop renal failure as well as pulmonary and cns infarctions as a result
of thromboses or hemorrhages.
*drop in platelet count, increase in protrombin time, elevation in fibrin,
*treat the underlying cause
*correct tissue ischemia by improving oxygenation, fluids replacement,
electrolytes balance, and administration of vasopressors.
*replacement of deficit coagulation factors and platelets
*cryoprecipitate is used to correct fibrinogen and factors v and vii.; fresh frozen
plasma is used to replace other coagulation factors.
*use of heparin infusion, although there is controversy regarding its use. Heparin
may inhibit the formation of microthrombi and thus permits perfusion of the
organs.
*other therapies include recumbenant activated protein c, effective in
diminishing inflammatory responses on the surface of the vessels, as well as
having anti-coagulant properties.
*nurses should be aware of who are patients at risk for dic. ( sepsis and
acute promyelocytic leukemia).
*patients need to be assessed frequently for signs of bleeding and
thrombosis, and monitored progression of these signs.
*assess skin w/ particular attention to bony prominences, and skin folds.
*reposition carefully, use pressure reducing mattress.
*perform careful skin care every 2 hrs, emphasizing the dependent areas,
all bony prominences, perineum.
*use prolonged pressure after injection.
*_ is an enzyme that, when activated, inhibits coagulation.
*when levels of protein c is deficient, the risk of_ increases and may
occur spontaneously.
*people w/ protein c dificiency are _until they reached the age of 20,
signs of thrombosis increases as the individual reaches 30-45 yrs.
*treatment w/ _is sometimes indicated.
*_ drugs maybe used w/ caution.
*_ is another natural anticoagulant normally produced by the liver.
*activated _requires protein s to inactivate certain clotting factors.
*when the level of protein s is deficient, the activation process is
diminished, and the risk of thrombosis can be increased.
*like patients w/ protein c deficiency, these clients have a greater risk
recurrence of venous thrombosis early in life, as early as _.
*thrombosis most frequently occurs in the axillary region, mesenteric,
and cerebral veins.
* Acquired protein s deficiency can also occur like in _
*apc resistance is a condition that can occur w/ other hypercoagulate
states.
*apc is an anticoagulant, and apc resistance increases the risk for
thrombosis.
*a molecular defect in factor v gene has been identified in most patients
w/ apc resistance.
*it is the most common cause of inherited hypercoagulability in
caucasians,
*factor v leiden mutation increase risk of thrombosis in patients using
oral contraceptives, increased in age.
*avoid activates that would cause circulatory stasis.( immobility, crossing
the legs)
*Exercise, like ambulation should be done regularly.
*Anti-embolism stockings are usually prescribed.
8 ACUTE LYMPHOCYTIC LEUKEMIA TO PROTEIN S DEFICIENCY (escalante-saac)
*Some patients may require life-long therapy for anti-coagulants, and
they should be well informed of the side effects of the drug.
*advice patients to avoid risk factors for thrombosis like cigarrete
smoking,
*Patients w/ hereditary d/o should encourage their siblings to be tested
for the disorder.
*For hospitalized patients, they should be monitored frequently for signs
of beginning thrombus formation particularly in the legs, and the lungs.
*Ambulation or rom exercises should be encouraged regularly, and
prophylactic anticoagulant drugs are commonly prescribed.
Das könnte Ihnen auch gefallen
- Clinical Medicine - Lecture: - Topic: - DateDokument2 SeitenClinical Medicine - Lecture: - Topic: - DateqselmmNoch keine Bewertungen
- Red Blood Cell Anomalies: Elliptocytes & Oval MacrocyteDokument12 SeitenRed Blood Cell Anomalies: Elliptocytes & Oval MacrocyteSHUPATUSSAI100% (1)
- 02 - Examination of Blood and Bone Marrow HematologyDokument3 Seiten02 - Examination of Blood and Bone Marrow Hematologyhamadadodo7Noch keine Bewertungen
- Red Blood Cell Disorders Part 1Dokument6 SeitenRed Blood Cell Disorders Part 1Claire GonoNoch keine Bewertungen
- Leukemia - Pathophysiology of White Cells DisordersDokument10 SeitenLeukemia - Pathophysiology of White Cells DisordersJacecosmozNoch keine Bewertungen
- (CLINPATH) Lipids and DyslipoproteinemiaDokument5 Seiten(CLINPATH) Lipids and DyslipoproteinemiaJolaine ValloNoch keine Bewertungen
- Pediatric ProblemsDokument4 SeitenPediatric ProblemsRencel Hope Bañez100% (1)
- Red Blood Cell Disorders Anemia: Anemia Is A Laboratory DiagnosisDokument3 SeitenRed Blood Cell Disorders Anemia: Anemia Is A Laboratory DiagnosisAnonymous 8hJAATBNoch keine Bewertungen
- Clinical Medicine - Lecture: - Topic: - DateDokument3 SeitenClinical Medicine - Lecture: - Topic: - DateqselmmNoch keine Bewertungen
- Screening Test For Phagocytic Engulfment: DiapedesisDokument2 SeitenScreening Test For Phagocytic Engulfment: DiapedesisBianca ANoch keine Bewertungen
- Hemolytic Disease of The Newborn: (Erythroblastosis Fetalis)Dokument17 SeitenHemolytic Disease of The Newborn: (Erythroblastosis Fetalis)sandeepv08Noch keine Bewertungen
- Protein Metab 2 Dra. SantosDokument7 SeitenProtein Metab 2 Dra. SantosMelissa SalayogNoch keine Bewertungen
- Vitamin B12 and FolateDokument12 SeitenVitamin B12 and FolateAllessandria DimaggioNoch keine Bewertungen
- (MID) IMMUNOSERO - Chapter 13 - Hypersensitivity (Reviewer)Dokument6 Seiten(MID) IMMUNOSERO - Chapter 13 - Hypersensitivity (Reviewer)Aisle Malibiran PalerNoch keine Bewertungen
- Classification of AnemiaDokument33 SeitenClassification of Anemialieynna4996Noch keine Bewertungen
- A. B. C. A. B. C. D.: Clinical Chemistry II - Prelims (Bandala)Dokument19 SeitenA. B. C. A. B. C. D.: Clinical Chemistry II - Prelims (Bandala)IceNoch keine Bewertungen
- Chemical Examination of UrineDokument7 SeitenChemical Examination of UrineStephen YorNoch keine Bewertungen
- Pathology - Chapter 14Dokument14 SeitenPathology - Chapter 14Cory GrayNoch keine Bewertungen
- Unit Viii: The Hematologic SystemDokument1 SeiteUnit Viii: The Hematologic SystemAqi RamenaiNoch keine Bewertungen
- Therapeutics - Gastrointestinal Tract: Heart FailureDokument5 SeitenTherapeutics - Gastrointestinal Tract: Heart FailureDarnell DelgadoNoch keine Bewertungen
- Anemia Type Pathogenesis Clinical Manifestations Diagnosis Peripheral Blood Lab FindingsDokument15 SeitenAnemia Type Pathogenesis Clinical Manifestations Diagnosis Peripheral Blood Lab FindingsDanielle FosterNoch keine Bewertungen
- Lymphoid NeoplasmsDokument52 SeitenLymphoid NeoplasmsAmalia Riska GNoch keine Bewertungen
- Hemophilia Nursing CareDokument10 SeitenHemophilia Nursing CareEla 15Noch keine Bewertungen
- Hemolytic Anemia: MorphologyDokument10 SeitenHemolytic Anemia: MorphologyAlya Putri KhairaniNoch keine Bewertungen
- Pancreatic AdenocarcinomaDokument6 SeitenPancreatic AdenocarcinomafikriafisNoch keine Bewertungen
- Hematology Lectures 1 5 DR - TuyDokument10 SeitenHematology Lectures 1 5 DR - TuyMiguel Cuevas DolotNoch keine Bewertungen
- Hemolytic AnemiaDokument1 SeiteHemolytic AnemiaTeus FatamorganaNoch keine Bewertungen
- HaemoglobinDokument47 SeitenHaemoglobinPreethi AbhilashNoch keine Bewertungen
- RevalidaDokument5 SeitenRevalidaHawkins FletcherNoch keine Bewertungen
- Hemostasis and Thrombosis: OutlineDokument11 SeitenHemostasis and Thrombosis: OutlineManila MedNoch keine Bewertungen
- Clin Path Trans 3.05 Urinalysis (2b)Dokument6 SeitenClin Path Trans 3.05 Urinalysis (2b)Reymart FernandezNoch keine Bewertungen
- Anemia Flow ChartDokument1 SeiteAnemia Flow ChartCynthiaNoch keine Bewertungen
- Hematology: - The Science Dealing With The FormationDokument104 SeitenHematology: - The Science Dealing With The FormationYamSomandarNoch keine Bewertungen
- Classification of The Epilepsies: Purpose: For Clinical DiagnosisDokument25 SeitenClassification of The Epilepsies: Purpose: For Clinical Diagnosisayu rifqiNoch keine Bewertungen
- Acute Lymphoblastic LeukemiaDokument25 SeitenAcute Lymphoblastic Leukemiaapi-396564080Noch keine Bewertungen
- UrinalysisDokument9 SeitenUrinalysisSukma EffendyNoch keine Bewertungen
- Normal Values of CBCDokument1 SeiteNormal Values of CBCCherr NollNoch keine Bewertungen
- Hemolytic AnemiaDokument9 SeitenHemolytic AnemiaTheeya QuigaoNoch keine Bewertungen
- Divergent Differentiation, Creating So-Called Mixed Tumors: Seminoma Are Used For Malignant Neoplasms. TheseDokument6 SeitenDivergent Differentiation, Creating So-Called Mixed Tumors: Seminoma Are Used For Malignant Neoplasms. TheseSherwin Kenneth Madayag100% (1)
- Intrinsic RBC DisordersDokument4 SeitenIntrinsic RBC DisordersMartin ClydeNoch keine Bewertungen
- Pharmacology of EthanolDokument5 SeitenPharmacology of EthanolJoshua RemonNoch keine Bewertungen
- Clinical Hematology Lecture on Erythrocyte Disorders and AnemiasDokument6 SeitenClinical Hematology Lecture on Erythrocyte Disorders and AnemiasNel TinduganiNoch keine Bewertungen
- Approach To Anemia: - Reticulocyte Count Is Most Important TestDokument15 SeitenApproach To Anemia: - Reticulocyte Count Is Most Important TestJanella SuerteNoch keine Bewertungen
- Gallstone Case StudyDokument19 SeitenGallstone Case StudyMoNa JbaReenNoch keine Bewertungen
- Fluids and Electrolytes Management in Surgical PatientsDokument4 SeitenFluids and Electrolytes Management in Surgical PatientsJanine Maita BalicaoNoch keine Bewertungen
- Serum ElectrolytesDokument2 SeitenSerum ElectrolytesKervin CablaidaNoch keine Bewertungen
- Anemia NotesDokument6 SeitenAnemia NotesElstella Eguavoen Ehicheoya100% (2)
- Chapter 7 - NeoplasiaDokument23 SeitenChapter 7 - NeoplasiaAgnieszka WisniewskaNoch keine Bewertungen
- Understanding PancytopeniaDokument68 SeitenUnderstanding PancytopeniaThaveeshaLindsayWhiteNoch keine Bewertungen
- RBC DisordersDokument70 SeitenRBC DisordersNdor Baribolo100% (1)
- CCII 8.0 - Clinical EnzymologyDokument2 SeitenCCII 8.0 - Clinical EnzymologyWynlor AbarcaNoch keine Bewertungen
- Hanta Vi Ru S Inf Ection SDokument20 SeitenHanta Vi Ru S Inf Ection Stummalapalli venkateswara rao100% (3)
- Renin Angiotensin Aldosterone SystemDokument1 SeiteRenin Angiotensin Aldosterone Systemgdubs215Noch keine Bewertungen
- Megaloblastic Anemia Testing AlgorithmDokument1 SeiteMegaloblastic Anemia Testing AlgorithmkatNoch keine Bewertungen
- Rabies: Ragina AguilaDokument55 SeitenRabies: Ragina AguilaCharles Lester AdalimNoch keine Bewertungen
- 3 Year CPC October 8, 20202Dokument4 Seiten3 Year CPC October 8, 20202Raian SuyuNoch keine Bewertungen
- Interpretation of Liver Enzyme Tests - A Rapid GuideDokument3 SeitenInterpretation of Liver Enzyme Tests - A Rapid Guidesserggios100% (2)
- Malignancy DR RashaDokument29 SeitenMalignancy DR RashaRasha TelebNoch keine Bewertungen
- Leukaemia LPDokument27 SeitenLeukaemia LPPiyu ShindeNoch keine Bewertungen
- LeukemiaDokument51 SeitenLeukemiaCres Padua QuinzonNoch keine Bewertungen
- Birth Rates and Death Rates Etc Formulas PDFDokument2 SeitenBirth Rates and Death Rates Etc Formulas PDFHafiz Zahid MahmoodNoch keine Bewertungen
- PATHODokument2 SeitenPATHOWendy EscalanteNoch keine Bewertungen
- Course of Automation in IndustrialDokument3 SeitenCourse of Automation in IndustrialWendy EscalanteNoch keine Bewertungen
- Cardiac 1.09 Blood Pressure Normal ValuesDokument1 SeiteCardiac 1.09 Blood Pressure Normal ValuesRandy Mar TagudarNoch keine Bewertungen
- Modifiable and Non-Modifiable Risk Factors for Myocardial InfarctionDokument2 SeitenModifiable and Non-Modifiable Risk Factors for Myocardial InfarctionWendy Escalante100% (1)
- Assessment of Kidneys PDFDokument1 SeiteAssessment of Kidneys PDFWendy EscalanteNoch keine Bewertungen
- PATHODokument2 SeitenPATHOWendy EscalanteNoch keine Bewertungen
- Classification LFDokument34 SeitenClassification LFAnonymous 4tzR698Noch keine Bewertungen
- Drug StudyDokument14 SeitenDrug StudyWendy EscalanteNoch keine Bewertungen
- NCP 2 MiDokument16 SeitenNCP 2 MiWendy EscalanteNoch keine Bewertungen
- NCPDokument3 SeitenNCPWendy EscalanteNoch keine Bewertungen
- Caring For The Bedridden PatientDokument1 SeiteCaring For The Bedridden PatientWendy EscalanteNoch keine Bewertungen
- Nurs1117 AlphaDokument118 SeitenNurs1117 AlphaRappler0% (1)
- Nasogastric Tube Management and CareDokument21 SeitenNasogastric Tube Management and CareWendy EscalanteNoch keine Bewertungen
- Laboratory Exams and ResultsDokument15 SeitenLaboratory Exams and ResultsWendy EscalanteNoch keine Bewertungen
- NCP 2 MiDokument16 SeitenNCP 2 MiWendy EscalanteNoch keine Bewertungen
- Lift CarryDokument7 SeitenLift CarryBianca ThereseNoch keine Bewertungen
- Drug StudyDokument14 SeitenDrug StudyWendy EscalanteNoch keine Bewertungen
- Concept Map in Head and Neck CancerDokument3 SeitenConcept Map in Head and Neck CancerWendy EscalanteNoch keine Bewertungen
- Assessment of KidneysDokument1 SeiteAssessment of KidneysWendy EscalanteNoch keine Bewertungen
- 02 Orig Art 02 PDFDokument3 Seiten02 Orig Art 02 PDFWendy EscalanteNoch keine Bewertungen
- Nasogastric Tube Management and CareDokument21 SeitenNasogastric Tube Management and CareWendy EscalanteNoch keine Bewertungen
- Integrated Management of Childhood Illness3 1 PDFDokument78 SeitenIntegrated Management of Childhood Illness3 1 PDFWendy EscalanteNoch keine Bewertungen
- Carotid Artery Disease ManagementDokument2 SeitenCarotid Artery Disease ManagementWendy EscalanteNoch keine Bewertungen
- At DietDokument8 SeitenAt DietWendy EscalanteNoch keine Bewertungen
- Acid-Ash DietDokument10 SeitenAcid-Ash DietWendy Escalante0% (1)
- Clear Liquid DietDokument6 SeitenClear Liquid DietWendy EscalanteNoch keine Bewertungen
- Concept Map of CKD Gastrointestinal SymptomsDokument4 SeitenConcept Map of CKD Gastrointestinal SymptomsWendy Escalante0% (1)
- Brat DietDokument8 SeitenBrat DietWendy EscalanteNoch keine Bewertungen
- Example of Invitation CardDokument2 SeitenExample of Invitation CardWendy EscalanteNoch keine Bewertungen
- End of Respiration, Beginning of Reproduction TranscriptionDokument7 SeitenEnd of Respiration, Beginning of Reproduction TranscriptionmarthafaragNoch keine Bewertungen
- Zen Wellness Horary Clock Booklet PDFDokument4 SeitenZen Wellness Horary Clock Booklet PDFMila onlyNoch keine Bewertungen
- 10 2 Neonatal TransfusionDokument6 Seiten10 2 Neonatal TransfusionfatmaNoch keine Bewertungen
- Life Process Ki KahaniDokument51 SeitenLife Process Ki KahaniKAMYA BRATA DEBNATHNoch keine Bewertungen
- Mountain Body Methapore in The AndesDokument17 SeitenMountain Body Methapore in The AndesAnna PrzytomskaNoch keine Bewertungen
- Human and Social Biology Graded ClassworkDokument3 SeitenHuman and Social Biology Graded ClassworkMeloney TrimminghamNoch keine Bewertungen
- Hemostasis: Written By: Fayzah Alshammari Date: 06-11-2021Dokument4 SeitenHemostasis: Written By: Fayzah Alshammari Date: 06-11-2021fayzah alshammariNoch keine Bewertungen
- NatokinaseDokument6 SeitenNatokinasefabadioNoch keine Bewertungen
- Haematological Parameters THDokument12 SeitenHaematological Parameters THShalu Bala ArjunNoch keine Bewertungen
- Heart Etheric Fifth ChamberDokument40 SeitenHeart Etheric Fifth Chamberklatifdg100% (1)
- Modul Interna Hom-ImunologiDokument12 SeitenModul Interna Hom-Imunologimuhammad sudrajatNoch keine Bewertungen
- Quennie C Frog DissectionDokument12 SeitenQuennie C Frog DissectionDhovie Mae FernandoNoch keine Bewertungen
- Group 1 - HemoglobinDokument10 SeitenGroup 1 - HemoglobinU WidNoch keine Bewertungen
- Cardio Notes 1Dokument8 SeitenCardio Notes 1Lindsay Grace MandarioNoch keine Bewertungen
- Tawa-Tawa Contains Active Ingredients That May Help Dengue Hemorrhagic Fever (DHF) Patients - StudyDokument2 SeitenTawa-Tawa Contains Active Ingredients That May Help Dengue Hemorrhagic Fever (DHF) Patients - StudyLouiseNoch keine Bewertungen
- The Digestive System Natural 6ºprimariaDokument6 SeitenThe Digestive System Natural 6ºprimariaPatry sanchezNoch keine Bewertungen
- CHAPTER 1.1 Blood PDFDokument25 SeitenCHAPTER 1.1 Blood PDFMuhammad Irfan AmiruddinNoch keine Bewertungen
- 26.4 Acid-Base Balance - Anatomy and PhysiologyDokument17 Seiten26.4 Acid-Base Balance - Anatomy and PhysiologyManjunath Vaddambal100% (1)
- Peripheral Vascular and Lymphatic System AssessmentDokument37 SeitenPeripheral Vascular and Lymphatic System AssessmentSuzanne Rush100% (3)
- MitochondriaDokument6 SeitenMitochondriakevin smithNoch keine Bewertungen
- Human Blood CellsDokument3 SeitenHuman Blood CellscsamarinaNoch keine Bewertungen
- Biology 2A03 Quiz 1 Version 1 Answers Feb 2013Dokument8 SeitenBiology 2A03 Quiz 1 Version 1 Answers Feb 2013JeevikaGoyalNoch keine Bewertungen
- S53 - FPSC NFC Location D-819, Part A, C V Raman Marg, Near Fortis Escort Hospital, New Friends Colon New DelhiDokument8 SeitenS53 - FPSC NFC Location D-819, Part A, C V Raman Marg, Near Fortis Escort Hospital, New Friends Colon New DelhiSohaib DurraniNoch keine Bewertungen
- HemophiliaDokument62 SeitenHemophiliamuhirwa Samuel100% (1)
- Vita KDokument31 SeitenVita KPabitra ThapaNoch keine Bewertungen
- 7A Cells, Tissues and Organs Booklet - Doc-1Dokument16 Seiten7A Cells, Tissues and Organs Booklet - Doc-1Majdoline SadeddineNoch keine Bewertungen
- Temporary Lab Services GuideDokument475 SeitenTemporary Lab Services GuideLorena Ek MaciasNoch keine Bewertungen
- Biology: Paper 9700/11 Multiple ChoiceDokument63 SeitenBiology: Paper 9700/11 Multiple Choicejust1394Noch keine Bewertungen
- How Can Blood Diseases Be IdentifiedDokument4 SeitenHow Can Blood Diseases Be Identifiedllatham0% (1)
- 321efektivitas Bayam Dan Buah Bit Terhadap Kadar Hemoglobin Ibu HamilDokument12 Seiten321efektivitas Bayam Dan Buah Bit Terhadap Kadar Hemoglobin Ibu Hamilsindy marveniaNoch keine Bewertungen