Beruflich Dokumente
Kultur Dokumente
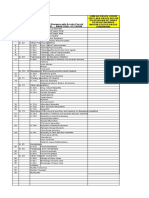
ATI - Unit 3 Chapters 44-46
Hochgeladen von
lisaOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
ATI - Unit 3 Chapters 44-46
Hochgeladen von
lisaCopyright:
Verfügbare Formate
Flashcards - ATI: Unit 3 chapters 44-46
Home > Print Preview
What would you like to do?
Get the free Flashcards app for iOS
Get the free Flashcards app for Android
Learn more
ATI: Unit 3 chapters 44-46
10/9/15, 1:14 PM
Author:
ID:
Filename:
Updated:
Tags:
Folders:
Description:
kelc
78933
ATI: Unit 3 chapters
44-46
2011-04-13 01:08:55
ati flashcards
ati flashcards basic
nursing care
Show Answers:
1. Who are the healthcare providers legally permitted to write prescriptions in the US?
Physicians
Advanced practice nurses
Dentists
Physician assistants
2. What are the five legal responsibilities of the healthcare providers who can write prescriptions?
1. Obtaining the client's medical history and physical examination
2. Diagnosing
3. Prescribing medications
4. Monitoring response to therapy
5. Modifying medication orders as necessary
3. What are the responsibilities of the nurse in relation to legal responsibilities of safe medication administration and error prevention?
- Preparing, administering, and evaluating client responses to medications
- Developing and maintaining an up-to-date knowledge base of medications administered, including uses, mechanisms of action, routes of
administration, safe dosage range, adverse/toxic responses, precautions, and contraindications
- Skill competency
- Knowledge of acceptable practice
- Determining accuracy of medication orders
- Reporting of all medication errors
- Safeguarding and storing medications
4. What controls the prescribing, dispensing and administering of medications?
Federal, state and local laws
Health care agency policies
Each state's nurse practice act
5. What are the types of medication orders?
Routine/standard order
Single/one-time order
Stat order
PRN order
Standing order
6. What type of medication order may or may not have a termination date?
Routine/standard order - will stay in effect until the PCP discontinues it or the client is discharged
7. What type of medication order is to be given once at a specified time or as soon as possible?
Single/one-time order
8. What type of medication order is only given once and given immediately?
Stat order
9. What type of medication order stipulates at what dosage, what frequency, and under what conditions a medication may be given?
PRN order
10. What type of medication order would the nurse use clinical judgment with which to determine the client's need for the medication?
PRN order
http://www.freezingblue.com/flashcards/print_preview.cgi?cardsetID=78933
Page 1 of 11
Flashcards - ATI: Unit 3 chapters 44-46
10/9/15, 1:14 PM
11. What type of medication order may be written for specific circumstances and/or for specific units?
Standing order
12. What are the components of a medication order?
- Name of client
- Date and time of order
- Name of medication
- Dosage
- Route of administration
- Time and frequency
- Signature of prescribing provider
13. What are the physiological variables affecting medication responses?
Age
Gender/body build
Chronic disease
Concurrent medication use
First-pass effects
Nutritional status
Pregnancy
Genetic factors
14. How does age affect medication responses?
Infants immature liver function limits the ability to metabolize medications
Aging process can alter liver and kidney function and decrease metabolism and excretion of medications
Decreased circulation can negatively affect medication distribution
15. How does gender/body build affect medication responses?
Differences in hormones
Distribution of fat and water
Weight
Height
Lean body mass
- All of the above affect medication absorption, distribution, metabolism and excretion 16. How does chronic disease affect medication responses?
Body organ dysfunction influences how medications are absorbed, distributed, metabolized and excreted
17. How does concurrent medication use affect medication responses?
Different medications used together can lead to unexpected and/or unpredictable metabolism, interference with intended therapeutic effect and an increased
risk of adverse medication reactions and interactions
18. What is the first-pass effect of medication and how does it affect medication responses?
Certain medications, when taken orally, are inactivated on their first pass through the liver and must be given by an alternate route
If they are inactivated they have no therapeutic effect on the body
19. What affect does nutritional status have on medication responses?
Presence or absence of food in the stomach can alter medication absorption.
Decreased nutritional status impairs the client's ability to produce specific medication-metabolizing enzymes, leading to impaired medication
metabolism
20. How does pregnancy affect medication responses?
Circulatory changes, hormonal changes, and presence of fetus may influence how medications are absorbed, distributed, metabolized and excreted by the
body
21. How do genetic factors affect medication responses?
Inherited traits may have specific influence on metabolism of medications
22. What are the psychosocial variables affecting medication response?
Health illness beliefs
Previous experiences with medications
Knowledge base
Cultural beliefs
Developmental stage
Social support/financial status
Potential for medication dependence and misuse
23. What are the six rights of safe medication administration?
http://www.freezingblue.com/flashcards/print_preview.cgi?cardsetID=78933
Page 2 of 11
Flashcards - ATI: Unit 3 chapters 44-46
10/9/15, 1:14 PM
Right client
Right medication
Right dose
Right route
Right time/frequency
Right documentation
24. How do you verify the client's identification for medication administration?
Check ID band, name, and/or photograph with the medication record
25. How many times do you read the medication label to verify it's the right medication?
3 times - when the container is selected, when removing the dose from container and when container is replace
26. True or false: leave unit-dose medication in its package until administration
True
27. Why is giving medication on time important?
To maintain a consistent therapeutic blood level
28. what is the time period in which a medication can be given?
1/2 hour before or after the scheduled time
29. What do you do if the route is not designated or the route designated is not recommended?
Contact the primary care provider for clarification
30. What are some resources for medication information?
Nursing drug books
Pharmacology textbooks
Professional journals
Physician's Desk Reference (PDR)
Professional websites
31. How are medications organized?
Pharmacologic action
Therapeutic use
Body system
Chemical makeup
Safe use during pregnancy
32. What is a medication's mechanism of action?
How the medication produces the desired therapeutic effect
33. This is the primary action for which the medication is administered to a specific client.
Therapeutic effect
34. These are undesired and sometimes dangerous effects of the medication - usually identified according to body system
Adverse effects
35. What is toxicity of medication?
The specific risks and manifestations of toxicity
36. Medication interactions can cause _________ and _________ effects.
Desired; undesired
37. What is a precaution for medication administration?
Caution for use in some clients
38. What are some contraindications for medication administration?
Specific disease
Condition
Age
Allergy
39. What are the nursing implications for medication administration?
How to monitor for therapeutic effects
How to prevent and treat adverse effects
How to provide for comfort
How to instruct clients in the safe use of medications
http://www.freezingblue.com/flashcards/print_preview.cgi?cardsetID=78933
Page 3 of 11
Flashcards - ATI: Unit 3 chapters 44-46
10/9/15, 1:14 PM
40. What are common medication errors?
- Wrong medication or IV fluid
- Incorrect dose or IV rate
- Wrong client, route or time
- Administration of known allergic medication
- Omission of dose
- Incorrect discontinuation of medication or IV fluid
41. How are therapeutic responses monitored with medication administration?
Change dosages gradually
42. Who should administer medications?
A. The patient's physician
B. Only A and C
C. The patient's nurse
D. Individual who prepared the medication
D. Individual who prepared the medication
43. Where does self-administration of medications take place?
In the home and community-based settings
In a facility/agency setting when clients wish to so their home medications and the ability to do so safely
44. What instructions should be given to a client who is going to be self-administering medication?
Written and verbal instructions for each medication regarding dosage, expected responses, and side/adverse effects
45. A nurse prepares an injection of an opiod to give to a client who reports pain. Prior to administering the medication, the nurse is called to
another room to assist another client onto a bedpan. This nurse then asks a second nurse to give the injection to that she can help the client
needing the bedpan. Which of the following actions is the most appropirate for the second nurse to take?
A. Prepare another syringe and give the injection
B. Tell the client needing the bedpan she will have to wait for her nurse
C. Give the injection prepared by the other nurse
D. Offer to assist the client needing the bedpan
D. Offer to assist the client needing the bedpan
46. C. Remove the medications, discard them, report the error, and document according to facility/agency policy
For a medication that ordered at 0900, which of the following are acceptable administration times? (select all that apply)
- 0905
- 0825
- 1000
- 0840
- 0935
- 0905
- 0840
47. Which of the following nursing actions may prevent medication errors from occurring?
A. Giving the ordered medication and then looking up the usual dosage range
B. Relying on another nurse to clarify a medication order
C. Checking with the PCP when a single dose requires administration of multiple tablets
D. Taking all medications out of the unit-dose wrappers before entering the client's room
C. Checking with the PCP when a single dose requires administration of multiple tablets
48. When implementing medication therapy, the nurse's responsibilities include which of the following? (select all that apply)
- Observing for medication side effects
- Monitoring for therapeutic effects
- Ordering the appropriate dose
- Changing the dose if side effects occur
- Maintaining an up-to-date knowledge base
- Observing for medication side effects
- Monitoring for therapeutic effects
- Maintaining an up-to-date knowledge base
http://www.freezingblue.com/flashcards/print_preview.cgi?cardsetID=78933
Page 4 of 11
Flashcards - ATI: Unit 3 chapters 44-46
10/9/15, 1:14 PM
49. 1 gr = ?
60 mg
50. 1 oz = ?
30 ml
51. 1 tsp = ?
5 ml
52. 1 tbs = ?
3 tsp
53. 1 kg = ?
2.2 lb
54. Round to what place in dosage calculations, unless otherwise indicated?
tenths
55. A client is to receive 300 mg of phenytoin (Dilantin) now and every morning. The pharmacy sends 200 mg tablets. How many tablets
should be given?
1.5 tabs
56. A client is to receive furosemide (Lasix) 80 mg IV q6h for 24 hr. Available is 10 mg/mL. How many mL should be administered for each
dose?
8 mL
57. A client is to be given amicillin (Ampicin) 250 mg orally q6h. Available is 125 mg/5mL. How many mL should be given for each dose?
10 mL
58. A client is to receive aspirin 10 gr every 4 hr when necessary. Available are 325 mg tablets. How many tablets should be given for each
dose?
2 tablets
59. A client is to receive acetaminophen (Tylenol) 320 mg every 3 to 4 hr for fever. Available is 160 mg/5 mL. How many tsp should be given
each dose?
2 tsp
60. A primary care provider prescribes atropine 0.5 mg IV for bradycardia. The vial is labeled atropine 400 mcg/mL. How many mL should be
given?
1.25 mL
61. A child weighs 31 lb. The PCP prescribes ampicillin 100 mg/kg/day in four divided doses. Available is ampicillin 250 mg/2 mL. How
many mL per dose should be given?
2.8 mL
62. Phenytoin (Dilantin) 5 mg/kg/day is prescribed in two divided doses for a child weighing 16 lb. It is available at 50 mg/mL. What is the
total daily dosage in mL for this child?
0.7 mL/day
63. Methylprednisolone (Solu-Medrol) 40 mg/kg/day is ordered every 4 hr for an adult weighing 154 lb. It is available at 40 mg/mL. How
many mL should be given per dose?
11.7 mL
64. A client is to receive 1 L of normal saline over 8 hr. The tubing drop factor is 15 gtt/mL. Calculate how many gtt/min should be delivered
per manual control.
31 gtt/min
65. A client is to receive metronidazole (Flagyl) 500 mg in 100 mL NS IV PB administered over 1 hr. The tubing drop factor is 60 gtt/mL.
Calculate how many gtt/min should be delivered per manual control?
100 gtt/min
66. A client is to receive Zantac 50 mg in 100 mL NS IV PB administered over 20 min. The tubing drop factor is 10 gtt/mL. Calculate how
many gtt/min should be delivered per manual control.
50 gtt/min
http://www.freezingblue.com/flashcards/print_preview.cgi?cardsetID=78933
Page 5 of 11
Flashcards - ATI: Unit 3 chapters 44-46
10/9/15, 1:14 PM
67. A nurse is to administer 600 mL of D5W over 8 hr. The IV pump should be set to deliver how man mL/hr?
75 mL/hr
68. An IV medication is to infuse over 20 min on the IV pump. The medication is mixed in 100 mL of normal saline. The IV pump should be
set to deliver how many mL/hr?
300 mL/hr
69. An IV medication is to infuse over 30 min on the IV pump. The medication is mixed in 100 mL of normal saline. The IV pump should be
set to deliver how many mL/hr?
200 mL/hr
70. What are the advantages of IV therapy?
Fast absorption and onset of action
Less discomfort after initial insertion
Maintains constant therapeutic blood levels
Less irritation to subcutaneous and muscle tissue
71. What are the disadvantages of IV therapy?
Circulatory fluid overload is possible if infusion is large and/or too rapid
Immediate absorption leaves no time to correct errors
IV administration can cause irritation to the lining of the vein
Failure to maintain surgical asepsis can lead to local infection and septicemia
72. What are the two types of IV access?
Peripheral
Central
73. Why should some medications be infused on an IV pump instead of IV push?
Medications (like potassium chloride) that can cause serious adverse reactions
74. Should medication be added to an IV container that is already hanging?
No, only add medication to a new IV fluid container
75. True or false: Never administer IV medication through tubing that is infusing blood, blood products, or parenteral nutritional solutions
True
76. What should be done before infusing a medication through tubing that is infusing another medication?
Verify compatibility
77. What are ways to prevent needlesticks?
Be familiar with IV insertion equipment
Avoid using needles when needless systems are available
Use protective safety devices when available
Never recap a needle
Dispose of needles immediately in designated puncture-resistant receptacles
Do not break or bend needles
78. What are the methods of IV medication infusion?
- Mixed in large volumes of fluid and given as continuous IV infusion
- Intermittent IV administration
- Bolus IV administration
79. When giving an IV medication infusions in a large volume of fluid, what amount of fluid is appropriate?
500-1000 mL
80. What amount of solution is used when giving medication through intermittent IV administration?
25-250 mL
81. What is intermittent IV administration?
Medications given intermittently in a small amount of solution through a continuous IV system or with saline or heparin lock systems
82. If given with a continuous IV infusion, what is the term for administering a medication through intermittent IV?
Piggyback
83. What needs to be done before and after medication administration through a saline or heparin lock system?
Flush the access port/tubing
http://www.freezingblue.com/flashcards/print_preview.cgi?cardsetID=78933
Page 6 of 11
Flashcards - ATI: Unit 3 chapters 44-46
10/9/15, 1:14 PM
84. What is bolus IV administration?
Medication in small amounts of solution that is injected over a short time (1 to 2 min) in emergent and nonemergent situations
85. What is one reason why some medications are given as bolus IV?
To achieve an immediate medication level in the bloodstream - pain medication
86. What are some special considerations when giving IV medications to older adult clients, clients taking coagulants or clients with fragile
veins?
Avoid tourniquets - use blood pressure cuff instead
Do not slap extremity to visualize veins
87. What are some special considerations when giving IV medications to a client with edema in extremities?
Apply digital pressure over proposed vein to displace edema
Apply pressure with alcohol pad
Cannulation must be quick
88. In what clients may anatomical landmarks need to be used to find veins for IV therapy?
Obese clients
89. What equipment is needed for IV medication administration?
Solution to be infused
Correct size catheter
Correct tubing
Infusion pump - if indicated
Insertion supplies
90. How far above a proposed IV insertion site should the tourniquet be applied?
4 to 6 inches
91. Where should veins first be assessed for IV insertion?
Distal veins on the nondominant hand
92. What veins should be avoided when inserting an IV?
Varicosed veins that are permanently dilated and tortuous
Veins in inner wrist with bifurcations, in flexion areas, near valves, in lower extremities, and antecubital fossa
Veins that are sclerosed or hard
Veins in an extremity with impaired sensitivity
93. How should a vein feel when assessing for an IV insertion site?
Resilient, soft and bouncy on palpation
94. What are methods to enhance venous access?
Gravity, fist clenching, friction with alcohol, heat, percussion by tapping gently, multiple tourniquets and transillumination
95. How should the area be cleansed prior to insertion of IV?
With alcohol, iodine preparation or chlorhexidine apply friction in a circular motion from middle to outward edge
Allow to air dry for 1 to 2 min
96. Where should the vein be anchored when inserting an IV?
Below the site of insertion
97. What should the client be warned of prior to the nurse inserting the IV needle?
Sharp, quick stick
98. True or false: The bevel of the needle should be facing up when inserting an IV
False
99. What angle should an IV be inserted at?
15 to 20 degrees
100. What is an indication of a successful IV insertion?
Flashback of blood into the catheter
101. After advancing the catheter into the vein, what should be done with the needle?
Withdraw the needle
102. When should the tourniquet be released?
http://www.freezingblue.com/flashcards/print_preview.cgi?cardsetID=78933
Page 7 of 11
Flashcards - ATI: Unit 3 chapters 44-46
10/9/15, 1:14 PM
After IV catheter insertion and before attaching the tubing
103. What needs to be documented on the IV catheter dressing?
Catheter size, date/time of insertion, and the initials of the nurse that inserted the catheter
104. What needs to be documented in the patient's chart after inserting an IV?
Date and time of insertion
Insertion site and appearance
Catheter size
Type of dressing
IV fluid and rate (if applicable)
Number, locations and conditions of site-attempted cannulations
Client response
105. How is the patency of an IV maintained?
Do not stop a continuous infusion or allow blood to back up into the catheter
Instruct the client not to manipulate flow rate device, change settings on IV pump and avoid lying on tubing
Make sure the IV dressing is not too tight
Flush intermittent IV catheters
Monitor site and infusion rate at least every hour
106. How often should an intermittent IV catheter be flushed?
After every medication administration
Every 8 to 12 hours when not in use
107. How should IV therapy be discontinued?
Check order/prep equipment
Wash hands
Apply gloves
Remove tape and dressing
Clamp IV tubing
Apply sterile gauze pad over site without putting pressure on vein
Withdraw catheter
Elevate and apply pressure for 2 min
Assess site
Apply tape over gauze
Use pressure dressing if needed
Assess catheter for intactness
Document
108. How do you prevent IV infections?
Use standard precautions
Change IV sites according to policy
Remove catheters as soon as they are no longer clinically indicated
Change catheter is any break in surgical aseptic technique is suspected
Use sterile needle/catheter for each insertion attempt
Avoid writing on IV bags with pens or markers
Change tubing immediately if contamination is known or suspected
Fluids should not hang more than 24 hours unless it is a closed system
Wipe all ports with alcohol before connecting IV lines or inserting a syringe
Never disconnect tubing for convenience or to position the client
Do not allow ports to remain exposed to air
Wash hands before and after handling the IV system
109. Pain, burning
Pallor
Local swelling at the site
Cool skin
Damp dressing
Slowed infusion
These are signs of?
Infiltration
110. How is infiltration prevented?
Careful selection of site and catheter
Securing the catheter
111. Stop infusion
http://www.freezingblue.com/flashcards/print_preview.cgi?cardsetID=78933
Page 8 of 11
Flashcards - ATI: Unit 3 chapters 44-46
10/9/15, 1:14 PM
Remove catheter
Elevate extremity
Encourage active ROM
Apply warm compresses 3-4 times/day
Restart IV proximal to site or other extremity
Treatment of infiltration
112. Edema
Throbbing, burning or pain at the site
Warmth
Erythema
May be a red line up the arm with a palpable band at the vein site
Slowed infusion
Signs of phlebitis/thrombophlebitis
113. How is phlebitis prevented?
Rotation of sites
Avoiding lower extremities
Proper handwashing and surgical aseptic technique
114. How is phlebitis treated?
Promptly discontinuing the infusion
Notify the PCP
Elevate extremity
War/moist compresses
Restart with new tubing and fluid
TED hose and/or anticoagulants
Culture the site and cannula if drainage is present
115. What are the signs of a hematoma?
Accumulation of clotted blood in the tissue, causing ecchymosis (bruising)
116. How are hematomas prevented?
Minimize tourniquet time
remove tourniquet before starting IV fluid
Hold pressure after removal of IV
117. How are hematomas treated?
Pressure dressings
Avoiding alcohol
After bleeding stops, using warm compresses and elevation
118. What are the signs of a catheter embolus?
Possibly asymptomatic
With migration there will be severe pain at the site
119. What is done to prevent catheter emboli?
Never reinsert the stylet into the catheter
Avoid joints
120. How are catheter emboli treated?
Pacing the tourniquet high on the extremity to limit venous flow
Preparing for removal under x-ray or surgery
Saving the catheter after removal to determine the cause
121. Tenderness, pain
Warmth
Edema
Induration
Red streaking
Fever, chills, malaise
Signs of cellulitis
122. How is cellulitis prevented?
Rotations of sites
http://www.freezingblue.com/flashcards/print_preview.cgi?cardsetID=78933
Page 9 of 11
Flashcards - ATI: Unit 3 chapters 44-46
10/9/15, 1:14 PM
Avoiding the lower extremities
Proper handwashing and surgical aseptic technique (same as phlebitis)
123. How is cellulitis treated?
Promptly discontinuing the infusion
Notify the PCP
Elevate extremity
War/moist compresses
Restart with new tubing and fluid
TED hose and/or anticoagulants
Culture the site and cannula if drainage is present
Antibiotics
Analgesics
Antipyretics
124. Sudden or gradual rise in temperature, chills and shaking, increased HR and RR, headache, nausea, vomiting, diarrhea and confusion
Bacteria cultured from blood
Signs of septicemia
125. What is the best way to prevent septicemia?
Diligent adherence to maintaining surgical aseptic technique
126. How is septicemia treated?
Monitoring the client's VS and assessing for s/s of infection
Notify PCP of changes in status
Blood cultures
Administering antibiotics as ordered
127. How is fluid overload treated?
Raising HOB
VS
Notifying PCP of changes in status
Possible readjustment of rate
128. How is fluid overload prevented in IV therapy?
Using an infusion pump
Monitoring I & O
129. Distended neck veins
Increased BP
Tachycardia
SOB
Crackles in the lungs
Edema
Signs of fluid overload
130. What are signs of air emoboli?
If in the pulmonary arteries - same as pulmonary embolism
Rarely occurs with peripheral lines
131. How are air emboli prevented?
Priming/flushing all tubing to prevent air from entering the system
Changing the IV solution containers before empty
132. How are air emboli treated?
Immediately
Putting the client in Trendelenburg position on the left side and instructing client to perform the Valsalva maneuver
Notify PCP
Perform frequent assessments
Ventilatory support and IV therapy per orders
133. Which of the following techniques will minimize the risk of catheter embolism?
A. Administer coagulants
B. Once in the vein, never put the stylet back through the catheter
C. Rotate the IV sites at least every 72 hours
D. Use good handwashing technique before and after IV insertion
http://www.freezingblue.com/flashcards/print_preview.cgi?cardsetID=78933
Page 10 of 11
Flashcards - ATI: Unit 3 chapters 44-46
10/9/15, 1:14 PM
B. Once in the vein, never put the stylet back through the catheter
134. The nurse checks for patency of an IV saline lock by
A. asking the client if the site is painful
B. checking the date of insertion
C. flushing the IV with NS and assessing the site
D. assessing the site for redness
C. flushing the IV with NS and assessing the site
USAA
We Now Provide Comprehensive Dental Insurance. Learn More!
What would you like to do?
Get the free Flashcards app for iOS
Get the free Flashcards app for Android
Learn more
Home > Print Preview
http://www.freezingblue.com/flashcards/print_preview.cgi?cardsetID=78933
Page 11 of 11
Das könnte Ihnen auch gefallen
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Orem & Roys Nursing Models: A ComparisonDokument4 SeitenOrem & Roys Nursing Models: A ComparisonlisaNoch keine Bewertungen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5795)
- Psych Drugs NursingDokument7 SeitenPsych Drugs Nursinglisa100% (2)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Schizophrenia Care Plan RNDokument8 SeitenSchizophrenia Care Plan RNlisa75% (4)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Sentara NursingDokument166 SeitenSentara NursinglisaNoch keine Bewertungen
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Med Surg Iggy Hypertension NotesDokument6 SeitenMed Surg Iggy Hypertension NoteslisaNoch keine Bewertungen
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- 312 ATI Critical Care MedsDokument34 Seiten312 ATI Critical Care Medslisa100% (1)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Table of Commonly Used IV SolutionsDokument2 SeitenTable of Commonly Used IV SolutionsKelly Diane LigosNoch keine Bewertungen
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Nanda 2015-2017 Nursing DiagnosisDokument3 SeitenNanda 2015-2017 Nursing Diagnosislisa88% (8)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Health Information Technology 2014Dokument641 SeitenHealth Information Technology 2014lisa100% (7)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- Basic Nursing Fundamentals EliminationDokument35 SeitenBasic Nursing Fundamentals Eliminationlisa100% (1)
- ATI IV TherapyDokument8 SeitenATI IV Therapylisa100% (1)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- Handout NSNA Student PresentationDokument14 SeitenHandout NSNA Student PresentationlisaNoch keine Bewertungen
- Dosage Calculations Chapter 3 A T IDokument35 SeitenDosage Calculations Chapter 3 A T Ilisa100% (4)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Ihi PS101Dokument8 SeitenIhi PS101lisa100% (1)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Adrenergic DrugsDokument32 SeitenAdrenergic Drugslisa100% (1)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- M4 - Didactic - NCM 118Dokument4 SeitenM4 - Didactic - NCM 118KARL FESARITNoch keine Bewertungen
- Evaluation and Management of Pediatric Community-Acquired PneumoniaDokument46 SeitenEvaluation and Management of Pediatric Community-Acquired PneumoniaJan Marvin Lichauco MendozaNoch keine Bewertungen
- Lassa Fever: What You Need To Know AboutDokument2 SeitenLassa Fever: What You Need To Know AboutMoses AyoadeNoch keine Bewertungen
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- Original Studies: Originalni Naučni RadoviDokument8 SeitenOriginal Studies: Originalni Naučni RadoviMiroslav JovanovicNoch keine Bewertungen
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Fifth Edition Answers To End-Of-Chapter Questions: GCSE Biology For YouDokument2 SeitenFifth Edition Answers To End-Of-Chapter Questions: GCSE Biology For YouRafia ArmanNoch keine Bewertungen
- Double Stimulations During The Follicular and Luteal Phases of Poor Responders in IVF/ICSI Programmes (Shanghai Protocol)Dokument8 SeitenDouble Stimulations During The Follicular and Luteal Phases of Poor Responders in IVF/ICSI Programmes (Shanghai Protocol)Nirmal KumawatNoch keine Bewertungen
- Department of Hormones: 25 - Hydroxy Vitamin DDokument2 SeitenDepartment of Hormones: 25 - Hydroxy Vitamin DASHWIN .A.S.Noch keine Bewertungen
- Guillain - Barre SyndromeDokument1 SeiteGuillain - Barre SyndromeGrant Kenneth Dumo AmigableNoch keine Bewertungen
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Impaired Swallowing Care PlanDokument5 SeitenImpaired Swallowing Care Planjakifer33% (3)
- Kertas Kerja Program Sayangkan KitaDokument5 SeitenKertas Kerja Program Sayangkan Kitaaknb2702Noch keine Bewertungen
- Summative 2 Renal 2011Dokument8 SeitenSummative 2 Renal 2011Ike Annisa YuwelzaNoch keine Bewertungen
- Module 5 - Formative Assessment 10 - NCM 112 CARE OF CLIENTS WITH PROBLEMS IN OXYGFENATION FLUDokument9 SeitenModule 5 - Formative Assessment 10 - NCM 112 CARE OF CLIENTS WITH PROBLEMS IN OXYGFENATION FLUDharylle CariñoNoch keine Bewertungen
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Headache: Differential Diagnosis of HeadacheDokument139 SeitenHeadache: Differential Diagnosis of Headachemero1983Noch keine Bewertungen
- PMLS LecDokument4 SeitenPMLS LecAlyana GabiniNoch keine Bewertungen
- DipSlide For Environmental Monitoring in HospitalDokument6 SeitenDipSlide For Environmental Monitoring in HospitalIwan RidwantoNoch keine Bewertungen
- Questionnnaire 1Dokument3 SeitenQuestionnnaire 1Franz Sobrejuanite GuillemNoch keine Bewertungen
- Icd-10 Oktober 2021Dokument9 SeitenIcd-10 Oktober 2021Nia KurniawatiNoch keine Bewertungen
- Diagnosis of Midface Fractures With CT: What The Surgeon Needs To KnowDokument24 SeitenDiagnosis of Midface Fractures With CT: What The Surgeon Needs To KnowMohammad AdhityaNoch keine Bewertungen
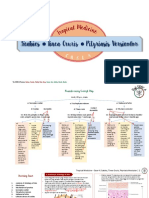
- Scabies Tinea Cruris Pityriasis Versicolor: Semangat!Dokument11 SeitenScabies Tinea Cruris Pityriasis Versicolor: Semangat!Fitriah Nur SyamiatiNoch keine Bewertungen
- LoadVoucher AspxDokument4 SeitenLoadVoucher AspxEdnalyn CasasNoch keine Bewertungen
- Pharmacology of Phenadoxone dN-Morpholino 4:4 Diphenyl: HydrochlorideDokument17 SeitenPharmacology of Phenadoxone dN-Morpholino 4:4 Diphenyl: Hydrochlorideisaev201Noch keine Bewertungen
- Ivt BTDokument3 SeitenIvt BTAB AlmazoraNoch keine Bewertungen
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- 4th Meeting of GTFCC Working Group On Surveillance 2019 List of ParticipantsDokument4 Seiten4th Meeting of GTFCC Working Group On Surveillance 2019 List of ParticipantsSteve NjengaNoch keine Bewertungen
- Dr. Naitik D Trivedi & Dr. Upama N. Trivedi: Pharmacology and Toxicology PracticalDokument2 SeitenDr. Naitik D Trivedi & Dr. Upama N. Trivedi: Pharmacology and Toxicology PracticalAnjali RaulNoch keine Bewertungen
- Obg FormatDokument17 SeitenObg Formatarchana vermaNoch keine Bewertungen
- Art Therapy What Is Art Therapy?Dokument2 SeitenArt Therapy What Is Art Therapy?rohit singhNoch keine Bewertungen
- Faculty List2019Dokument6 SeitenFaculty List2019suyashsahu2505Noch keine Bewertungen
- Cytology Uri Prost RespDokument7 SeitenCytology Uri Prost RespDavid FelmeriNoch keine Bewertungen
- Safety Data Sheet: Section 1. Chemical Product and Company IdentificationDokument17 SeitenSafety Data Sheet: Section 1. Chemical Product and Company IdentificationEngr Qaisar NazeerNoch keine Bewertungen
- Allergies or Food Intolerances.: Therapeutic DietDokument3 SeitenAllergies or Food Intolerances.: Therapeutic DietBryan Mae H. DegorioNoch keine Bewertungen