Beruflich Dokumente
Kultur Dokumente
Baby Massage Ameliorates Neonatal Jaundice in Full-Term Newborn Infants
Hochgeladen von
gladeva yugi antariOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Baby Massage Ameliorates Neonatal Jaundice in Full-Term Newborn Infants
Hochgeladen von
gladeva yugi antariCopyright:
Verfügbare Formate
Tohoku J. Exp. Med.
, 2011, 223, 97-102 Baby Massage Ameliorates Neonatal Jaundice
97
Baby Massage Ameliorates Neonatal Jaundice in Full-Term
Newborn Infants
Jun Chen,1 Mieko Sadakata,2 Mayumi Ishida,2 Naoto Sekizuka3 and
Mitsuko Sayama2
1
Division of Information Science and Biostatistics, Niigata University Graduate School of Medical and Dental
Sciences, Niigata, Japan
2
Division of Nursing, School of Health Sciences, Faculty of Medicine, Niigata University, Niigata, Japan
3
Sekizuka Hospital of Shibata, Niigata, Japan
Neonatal jaundice is a common physiological problem affecting over half of all full term and most preterm
infants. Thus, newborn infants must be monitored for signs of hyperbilirubinemia to prevent acute bilirubin
encephalopathy or kernicterus. Evidence exists supporting the benefits of baby massage as a form of mild
hand to skin contact, to increase neonatal physical and mental development. In the present study, the
effects of gentle baby massage on neonatal jaundice in full term newborn infants were evaluated by a
controlled clinical trial. The inclusion criteria of newborn neonates were as follows: (1) gestational age of
37 ~ 41 weeks, (2) birth weight of 2,800 ~ 3,600 g, (3) Apgar score at birth of 8 ~ 10, and (4) being a
healthy neonate without neonatal asphyxia and hemolytic condition. Breastfed newborns without
phototherapy were included: 20 in the massage group and 22 in the control group. We found the mean
stool frequency of the massaged infants on day 1 and day 2 (4.6 and 4.3) was significantly higher than that
of the control group (3.3 and 2.6) (p < 0.05). The transcutaneous bilirubin levels on the second to fifth day
and serum total bilirubin levels on fourth day were significantly decreased in the massage group, compared
to the control group. In conclusion, baby massage at an early stage after birth could reduce neonatal bilirubin levels. We suggest baby massage is beneficial for ameliorating neonatal jaundice.
Keywords: baby massage; neonatal jaundice; transcutaneous bilirubin level; enterohepatic circulation; vagus nerve
Tohoku J. Exp. Med., 2011, 223 (2), 97-102. 2011 Tohoku University Medical Press
Neonatal jaundice is a common physiological problem
affecting over half of all full term and most preterm infants.
Although most jaundice is harmless, newborn infants must
be monitored for signs of hyperbilirubinemia and acute bilirubin encephalopathy or kernicterus. According to the
American Academy of Pediatrics (AAP) recommendation,
the clinical intervention on jaundice includes observation,
evaluation, diagnosis or phototherapy (American Academy
of Pediatrics 1994). Both for treatment and prevention, the
mainstay of intervention is phototherapy, a safe and widely
available therapy when compared with exchange transfusion and medication. There are however potential sideeffects attributable to phototherapy, including watery diarrhea, increased insensible water loss, skin rashes, blue baby
syndrome and transient bronzing of the skin. There is also
controversy surrounding whether phototherapy treatment
for jaundice may increase the risk of developing melanoma
later in life (Matichard et al. 2006; Dennery and Lorch
2007; Newman and Maisels 2007). Furthermore, the baby
and mother could suffer mental and emotional pressure
induced by separation when phototherapy is performed.
Therefore, it is necessary to find some way to newborn
jaundice and control bilirubinemia to within normal range
whilst avoiding more harmful treatments.
In many areas of the world, especially in the African
and Asian continents, Indigenous South Pacific cultures and
the former Soviet Union, baby massage is a traditional
practice. There have been many studies on the effect of
baby massage over the past several decades. These studies
have demonstrated the beneficial effects of baby massage
for neonatal physical development such as weight, length,
head circumference, bone mineral density, sleep duration,
respiration and the elimination and reduction of colic and
wind (Field 2002; Field et al. 2010). Baby massage is also
thought to reduce infant stress and promote positive parentinfant interaction (Underdown et al. 2006; Hernandez-Reif
et al. 2007). Based on our clinical experience, baby massage would promote early-stage defecation of neonates,
which may accelerate bilirubin excretion with the possibility of reducing neonatal jaundice. We therefore conducted
Received November 11, 2010; revision accepted for publication December 24, 2010. doi: 10.1620/tjem.223.97
Correspondence: Jun Chen, Department of Medical Informatics, Niigata University Graduate School of Medicine and Dental Sciences,
Asahimachi-Dori 1-754, Niigata 951-8520, Japan.
e-mail: chenjun@med.niigata-u.ac.jp
97
98
J. Chen et al.
a clinical study to reveal the effects of baby massage on
jaundice reduction.
Subjects and Methods
Participants
Subjects consisted of healthy term infants born at the Sekizuka
Hospital of Shibata in Niigata, a metropolitan city in Japan, from
September 2006 to November 2006. Inclusion criteria for study
participation were (1) gestational age of 37 ~ 41 weeks (259 ~
287days), (2) birth weight of 2,800 ~ 3,600 g, (3) Apgar score at birth
of 8 ~ 10, and (4) being a healthy neonate without neonatal asphyxia
and hemolytic condition, and puerpera without maternal obstetric
complications. As standard practice for 1 week all healthy neonates
were breast fed during their admittance to the hospital.
During the selection and trial period, a total of 69 cases were
admitted and these were semi-randomly allocated to a control group
(n = 40) or a treatment group (n = 29): infants born in every two days
enter the control group and one day enter treatment group. An obvious gap between the amounts of two allocated groups because we
predicted that there were more cases in the control group than the
treatment group that needed to be treated with phototherapy and had
to drop out of the trial. As a result of this, the allocation was changed
to accommodate for infants who had been switched to phototherapy
treatment. Finally, there were 22 of 40 in the control group and 22 of
29 in treatment group not requiring phototherapy. In addition,
because of severe skin rashes, 2 subjects in the treatment group were
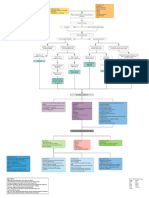
excluded from the trial. The incidence of mild skin rashes was similar between the two groups. Fig. 1 gives the profile of the study and
details of inclusion, exclusion and reasons for non-compliance.
Obstetric data
The main obstetric data related to childbirth were considered as
part of the background information collected from the participating
subjects. This information included infant gender, gestational age,
birth weight, Apgar score, mothers total number of deliveries, blood
loss at delivery, duration of delivery and type of delivery.
Fig. 1. Study flow chart.
99
Baby Massage Ameliorates Neonatal Jaundice
Procedure
For neonates in the treatment group, specialized clinical staff
gave 15-20 minutes of baby massage twice daily, 1 hour after the
morning and midday feed, from the first day to the fifth day postnatal.
For this study, we devised massage methods and procedures based on
Touch Therapy (Field et al. 1986) from the University of Miami,
USA. The room temperature was maintained at between 24-28C.
After thoroughly washing hands and applying baby oil, pressure was
applied to the newborns skin with warm, bare hands. Massage starting on the face, massager use two thumbs gently rubbing the periorbital and cheek regions; and then moving on to the chest, two hands
of performer from the lower margin of chest slide to opposite upper
edge alternately; then to the abdomen, corresponding to the conformation of colon, the performer push a half circle gently; next is on the
limbs, the performer use hand by hand with moderate pressure external side of the upper and lower limbs; and finally the back, the performer slide two hand from vertebra to two sides by neck to buttock.
The staff members performing the massage were trained by the same
licensed massage therapist. Normal care was given to the control
new born infants.
Measures
Stool frequency: stool frequency was checked from the first day
to the fifth day postnatally. The times of defecation were documented
according to the mothers parenting logs and nursing records.
Transcutaneous bilirubin level: Measured before massage treat
ment using a transcutaneous jaundice meter (manufactured by Konica
Minolta, JM-103, Japan) from the first day to fifth day postnatally.
Measurement areas were infants forehead and 2 points on the chest,
measured 3 times each by pressing the meter against the skin
vertically, and the average value was adopted.
Serum bilirubin values: Serum total bilirubin levels and
unbound bilirubin levels were measured from capillary blood exsanguinated from newborn infants planta pedis on fourth day postnatally.
Statistical analysis
We used the Student t-test for assessing the differences between
mean values, and chi-square tests for the difference in ratios between
the treatment and control groups. We also used a repeated measure
ANOVA to compare the difference of body weight, stool frequency
and transcutaneous bilirubin levels between the two groups. The
level of statistical significance was set at p < 0.05. The statistical
analysis was performed using software SPSS14.0 (Chicago, IL,
USA).
Ethical Considerations
This study was approved by the Ethics Committee of Niigata
University Graduate School of Health Sciences and informed consent
was obtained from the guardians of the neonates.
Results
Subject characteristics
Table 1 shows the demographic characteristics of a
total of 69 newborn infants who enrolled for this trial.
There were no differences in birth conditions between the
treatment and control groups. The subjects gestational age
was approximately 278 days (39 weeks), Apgar score was 9,
and there was no percentage difference in the type of delivery (vaginal delivery or cesarean section). There was also
no difference in the birth weight: control group 3,146 199
g vs. treatment group 3,188 207 g. There were also no
significant differences in mothers total number of deliveries, blood loss at delivery and duration of delivery. As there
were no differences in birth and delivery conditions, we
could confirm that these two groups were homogeneous
groups prior to beginning the study. We also show in Table
2 the background factors in both groups who completed
trial; it is similar to the table 1 and shows no significant difference.
Table 1. Subject characteristics of cases enrolled in the trial.
Control group (N = 40)
Infants
Gender
Male
Female
Gestational Age (Days)
Birth weight (g)
Apgar Score
Mothers
Total number of deliveries
Blood loss at delivery(ml)
Duration of delivery(h)
Type of delivery:
Vaginal delivery
Cesarean-section
Treatment group (N = 29)
P Value
0.39
15 (37.5)
25 (62.5)
277.6 7.0
3,164.5 199.4
9.0 0.2
13 (48.1)
14 (51.9)
278.3 7.9
3,188.5 207.9
9.0 0.2
1.5 0.7
306.6 146.8
7.7 6.19
1.6 0.8
380.8 203.5
7.1 6.6
36 (90.0)
4 (10.0)
20 (74.1)
7 (25.9)
0.94
0.41
0.78
0.67
0.09
0.69
0.11
For subjects gender and type of delivery for mothers and Phototherapy, we showed the differences in
ratios (P Value found by chi-square test). For gestational age (in days), birth weight and Apgar score, etc.,
differences in the mean values are shown (P Values found by t-test).
100
J. Chen et al.
Table 2. Background Factors of newborns who completed the trial.
P Value
Control group (N = 22)
Treatment group (N = 20)
8 (36.4)
14 (63.6)
278.1 6.8
8 (40.0)
12 (60.0)
278.9 7.8
18 (81.8)
4 (18.2)
9.0 0.2
15 (75)
5 (25)
9.0 0.2
0.95
3,164.5 197.0
3,028.1 192.3
2,953.2 195.5
2,964.6 208.8
3,005.3 219.5
3,037.5 223.3
3,190.2 200.0
3,065.5 179.2
2,996.5 179.5
2,984.5 210.7
3,001.0 214.8
3,018.5 228.3
0.68
0.52
0.46
0.76
0.95
0.79
Gender
0.81
Male
Female
Gestational Age (Days)
Type of delivery:
Vaginal delivery
Cesarean-section
Apgar Score
Weight (g)
Birth weight
Day 1
Day 2
Day 3
Day 4
Day 5
0.68
0.71
For subjects gender, we showed the differences in ratios (P Value found by chi-square test). For
gestational age (in days), birth weight and Apgar score, etc., differences in the mean values are shown
(P Values found by t-test). Analyzed by ANOVA, the weight was no difference between the two
groups (F value = 0.078, P = 0.782).
Table 3. Comparison of Daily Stool Frequency.
Day 1
Day 2
Day 3
Day 4
Day 5
Control (N = 22)
Treatment (N = 20)
T Value
P Value
3.3 2.0
2.6 1.9
4.1 2.7
4.7 2.5
3.9 2.0
4.6 1.7
4.3 2.0
4.8 1.5
5.5 2.6
4.7 1.6
2.27
2.77
0.96
0.97
1.49
0.03*
0.008*
0.35
0.34
0.15
All values are means standard error of the. Mean (SD). *p < 0.05. Analyzed by ANOVA,
the frequency of stools was difference between the two groups (F value = 6.301, P = 0.016).
Stool frequency
Table 3 shows the frequency of stools per day from the
first to the fifth day. The mean stool frequency of the
treatment group on day 1 and day 2 (4.6 and 4.3) were
significantly higher than that of the control group (3.3 and
2.6) (p < 0.05, < 0.01 respectively). On days 3, 4 and 5, the
infants in the treatment group also had a slightly higher
frequency, albeit this was not statistically significant.
Analyzed by ANOVA, the frequency of stools was
difference between the two groups. (F Value = 6.301, P =
0.016).
Transcutaneous bilirubin levels
As shown in Table 4, the measured value of transcutaneous jaundice (measured on the chest in the morning) on
the first day postnatally (when study of the given infant
began) of the control group is 4.4 1.4 mg/dl, whilst that of
the treatment group is 4.2 1.1 mg/dl, showing no significant difference. Whereas the values measured on the second, third, fourth and fifth day after birth of the control
group were 8.2 1.7, 10.6 1.8, 11.7 1.4 and 1.6 2.2
mg/dl respectively. In contrast, those of the baby massage
treatment group were 7.2 1.3, 9.1 1.9, 9.9 2.9 and 9.5
3.1 mg/dl, respectively, showing a significant decrease for
over each day (p < 0.05). The same results were found in
other measurement areas and times (data not shown) and
analyzed by ANOVA, the value of transcutaneous jaundice
was difference between the two groups. (F Value = 7.49,
P = 0.009).
Serum bilirubin values
Total bilirubin levels of 4th day are shown in Table 5.
The treatment infants had significantly lower levels of total
bilirubin (11.7 2.8 mg/dl) compared to the control infants
(13.7 1.7 mg/dl) (p < 0.01). Unbound bilirubin levels
showed no significant difference between the two groups
(control 0.4 0.1 g/dl vs. treatment 0.4 0.2 g/dl; p =
0.77).
101
Baby Massage Ameliorates Neonatal Jaundice
Table 4. Comparison of Daily Measurements by Transcutaneous Jaundice Meter (mg/dl).
Control (N = 22)
Treatment (N = 20)
T Value
P Value
Day 1
4.4 1.4
4.2 1.1
0.52
0.60
Day 2
Day 3
Day 4
Day 5
8.2 1.7
10.6 1.8
11.7 1.4
11.6 2.2
7.2 1.3
9.1 1.9
9.9 2.9
9.5 3.1
2.11
2.61
2.66
2.48
0.04*
0.01*
0.01*
0.02*
All values are means standard error of the mean (s.d.). *p < 0.05. Analyzed by ANOVA,
the value of transcutaneous jaundice was difference between the two groups (F Value = 7.49, P =
0.009).
Table 5. Serum bilirubin level on day 4.
Total Bilirubin (mg/dl)
Unbound Bilirubin (g/dl)
Control (N = 22)
Treatment (N = 20)
T Value
P Value
13.7 1.7
0.4 0.1
11.7 2.8
0.4 0.2
2.84
0.30
0.007
0.77
Discussion
This is the first report of a clinical controlled trial demonstrating a difference in neonatal jaundice for term infants
that are exposed to baby massage when compared to normal
care alone. Preliminary data indicates that baby massage
could reduce neonatal jaundice and provide a useful tool to
newborn jaundice and control bilirubinemia to within the
normal range.
The significant reduction of neonatal jaundice in the
treatment group can be explained by the treatment infants
higher frequency of stooling on the first and the second day
compared to control infants. It is thought the massage may
stimulate the infants to pass meconium. Newborn infants
usually have their first stool within 24 hours after birth.
This meconium, which consists of amniotic fluid components swallowed during the prenatal period, gastrointestinal
secretion, bile etc., is excreted within 3 days after birth. In
this study, stooling frequency was shown to be higher in the
massage treatment group compared to the control group,
especially in the first 2 days. Furthermore, increased stool
frequency on days 1 and 2 may be the cause for the low
values of serum total bilirubin on day 4 and transcutaneous
bilirubin on days 2-5 for the treatment infants. This is consistent with other studies. Gourley et al. (1992) demonstrated a negative relationship between stool production and
bilirubin levels in healthy term infants during the first 3
weeks of life. Semmekrot et al. (2004) reported that
frequent bowel movements diminished the enterohepatic
circulation of bilirubin in a newborn infant, thereby increas
ing bilirubin excretion.
The mechanism of delayed passage of meconium
resulting in hyperbilirubinemia is thought to be caused by
enhanced enterohepatic circulation. If the enterohepatic
circulation continues as in the prenatal period, bilirubin levels in the blood will rise (Nishida 1994). Intestinal activi-
ties are not sufficient immediately after birth because ingestion is not yet established. Therefore, direct (conjugated)
bilirubin that is excreted into the intestines is easily reabsorbed, associating with increased bilirubin production.
Also, there was a report indicated that infants with significantly delayed meconium passage due to megacolon and
anal atresia, etc. have a higher tendency to develop hyperbilirubinemia (Yoshitake and Baba 1984). There were no
such infants in our study. By hastening meconium passage
on the first and the second days, the enterohepatic circulation was possibly controlled to its physiological range, preventing the level of bilirubin from rising to a pathological
level.
Through massage, stimuli can be directly sent to the
exteroceptorthe skins sensory terminal. The flow of
blood, lymph and tissue fluid in the subcutaneous tissues,
are induced by massage stimuli to the skin. As a result, all
elements essential to the body are adjusted, and waste products are collected and excreted. In addition, massage treatment given to various parts of the body stimulates the vagus
nerve and heightens the production of food-absorbing hormone, which subsequently increases the secretion of gastric
and pancreatic fluid. This increases the amount of milk the
infant suckles, and enhances food digestion (Field et al.
1986; Field and Diego 2008). Kerstin states that sedation
of physiological stimuli like touch and heat results in muscle relaxation, a decrease in cortisol levels, a reduction in
cardiovascular activities, and activation of enterokinesis
which helps digestion (Uvnas-Moberg 1998).
Although we found some limitations in our study, our
results are still very impressive. The sample size is not big
enough and this may mask otherwise significant results.
Because we had to select and treat the infant immediately
after they born and cant wait for collected to a certain
number, so we use a semi-random method (by day selec
tion) to allocate the samples. If baby massage activated the
102
J. Chen et al.
vagus nerve and enhanced the production of the foodabsorbing hormone, it was necessary to compare the
amount of milk the infant suckled. In this study, although
all newborn infants were breast-fed, it was impossible to
measure the amount of milk suckled, and therefore this
indicator was not included in the analysis of our results.
Despite the complexities of neonatal jaundice, this study
has shown that baby massage is an effective treatment for
its control in healthy term infants. Further research is
required to find out if changes in massage frequency, duration, timing, massage areas and methods have additional
effects on neonatal jaundice.
Conclusions
This study has addressed the practice of giving baby
massage at an early stage after birth effectively lowers neonatal bilirubin levels. The neonate massage treatment group
showed a significant decrease in bilirubin levels over each
day, when compared to the control group. The mean stool
frequency of the treatment group on day 1 and day 2 was
significantly higher, as massage stimulation will encourage
the neonate to pass more meconium which contains
bilirubin. It is therefore suggested that baby massage may
contribute towards the prevention of newborn jaundice and
control bilirubinemia to within normal ranges.
Acknowledgments
We would like to thank the mothers and infants and also the
staff at Sekizuka Hospital for participating in this study.
Conflicts of Interest
The authors declare no conflict of interest.
References
American Academy of Pediatrics, Provisional Committee for
Quality Improvement and Subcommittee on Hyperbilirubinemia (1994) Practice parameter: management of hyperbiliru-
binemia in the healthy term newborn. Pediatrics, 94, 558-565.
Dennery, P.A. & Lorch, S. (2007) Neonatal blue-light phototherapy could increase the risk of dysplastic uevus development. Pediatrics, 120, 247-248.
Field, T. (2002) Massage therapy. Med. Clin. North Am., 86, 163171.
Field, T. & Diego, M. (2008) Vagal activity, early growth and
emotional development. Infant Behav. Dev., 31, 361-373.
Field, T., Diego, M. & Hernandez-Reif, M. (2010) Preterm infant
massage therapy research: a review. Infant Behav. Dev., 33,
115-124.
Field, T.M., Schanberg, S.M., Scafidi, F., Bauer, C.R., Vega-Lahr,
N., Garcia, R., Nystrom, J. & Kuhn, C.M. (1986) Tactile/
kinesthetic stimulation effects on preterm neonates. Pediatrics, 77, 654-658.
Gourley, G.R., Kreamer, B. & Arend, R. (1992) The effect of diet
on feces and jaundice during the first 3 weeks of life. Gastroenterology, 103, 660-667.
Hernandez-Reif, M., Diego, M. & Field, T. (2007) Preterm infants
show reduced stress behaviors and activity after 5 days of
massage herapy. Infant Behav. Dev., 30, 557-561.
Matichard, E., Le Hnanff, A., Sanders, A., Leguyadec, J., Crickx,
B. & Descamps, V. (2006) Effect of neonatal phototherapy on
melanocytic nevus count in children. Arch. Dermatol., 142,
1599-1604.
Newman, T.B. & Maisels, M.J. (2007) Evidence insufficient to
Recommend melanoma surveillance following phototherapy
for jaundice. Arch. Dermatol, 143, 1216-1217.
Nishida, H. (1994) Introduction of neonatology. 2nd ed., Medical
academy of classical learning. Tokyo, 639 (in Japanese).
Semmekrot, B.A., de Vries, M.C., Gerrits, G.P. & van Wieringen,
P.M. (2004) Optimal breastfeeding to prevent hyperbilirubinaemia in healthy, term newborns. Ned. Tijdschr. Geneeskd.,
148, 2016-2019.
Underdown, A., Barlow, J., Chung, V. & Stewart-Brown, S. (2006)
Massage intervention for promoting mental and physical
health in infants aged under six months. Cochrane Database
Syst. Rev., 18, CD005038.
Uvnas-Moberg, K. (1998) Oxytocin may mediate the benefits of
positive social interaction and emotions. Psychoneuroendocrinology, 23, 819-835.
Yoshitake, K. & Baba, K. (1984) Nursing care of neonates and
premature neonates. Kango MOOK No11. Kanehara & Co.,
LTD, Tokyo (in Japanese).
Das könnte Ihnen auch gefallen
- Prescription WritingDokument7 SeitenPrescription WritingSam DemonteverdeNoch keine Bewertungen
- Job Description: Iii. Key Performance IndicatorsDokument2 SeitenJob Description: Iii. Key Performance IndicatorsBidisha BasuNoch keine Bewertungen
- Myocardial Infarction With CABG Concept MapDokument1 SeiteMyocardial Infarction With CABG Concept MapMaria Therese100% (1)
- 9 1 EndosDokument6 Seiten9 1 EndosmghNoch keine Bewertungen
- Sample of MRCOG Assessment 2021 - Saeed HasanDokument28 SeitenSample of MRCOG Assessment 2021 - Saeed HasanIslam AwniNoch keine Bewertungen
- Oil Masssage ResearchDokument58 SeitenOil Masssage ResearchSanket TelangNoch keine Bewertungen
- Operating Manual and Sop For Private Medical ClinicsDokument31 SeitenOperating Manual and Sop For Private Medical ClinicsKlinik Rakyat LangkapNoch keine Bewertungen
- EbolaDokument15 SeitenEbolaIbama MirillaNoch keine Bewertungen
- Pijat Bayi Untuk Ikterik NeonatusDokument6 SeitenPijat Bayi Untuk Ikterik NeonatusIlham Barry Amrulloh JokamNoch keine Bewertungen
- Terapi Pijat English PDFDokument6 SeitenTerapi Pijat English PDFari dwiNoch keine Bewertungen
- Hiperalgesia PDFDokument6 SeitenHiperalgesia PDFannagm97Noch keine Bewertungen
- Ijrm 11 583 PDFDokument6 SeitenIjrm 11 583 PDFAnsoriNoch keine Bewertungen
- Massage Intervention For Preterm Infants by Their Mothers: A Randomized Controlled TrialDokument7 SeitenMassage Intervention For Preterm Infants by Their Mothers: A Randomized Controlled TrialopanocayNoch keine Bewertungen
- Jurnal 4Dokument7 SeitenJurnal 4Siska YunitaNoch keine Bewertungen
- Jurnal Kenaikan Berat Badan WhinikeDokument10 SeitenJurnal Kenaikan Berat Badan WhinikeWhinike CintyaNoch keine Bewertungen
- Navodaya College of Nursing: Proforma For Registration of Subjects ForDokument18 SeitenNavodaya College of Nursing: Proforma For Registration of Subjects ForStephy SojanNoch keine Bewertungen
- A Clinical Study of Programmed Labour and Its Maternal and Foetal OutcomeDokument4 SeitenA Clinical Study of Programmed Labour and Its Maternal and Foetal OutcomeInternational Organization of Scientific Research (IOSR)Noch keine Bewertungen
- Jurnal Masage TX Vs KMCDokument10 SeitenJurnal Masage TX Vs KMCjtriasdiNoch keine Bewertungen
- Wa0008. PDFDokument12 SeitenWa0008. PDFLal NandaniNoch keine Bewertungen
- Rahmawati 2019 IOP Conf. Ser. Earth Environ. Sci. 255 012001Dokument6 SeitenRahmawati 2019 IOP Conf. Ser. Earth Environ. Sci. 255 012001Ayu DiantariNoch keine Bewertungen
- A Follow-Up KAISA 2013Dokument6 SeitenA Follow-Up KAISA 2013Daniela LucenaNoch keine Bewertungen
- 56 1-Gunay Original 10 2Dokument9 Seiten56 1-Gunay Original 10 2Mbah AbuNoch keine Bewertungen
- Complementary Therapies in Medicine: SciencedirectDokument6 SeitenComplementary Therapies in Medicine: SciencedirectSurya Puji KusumaNoch keine Bewertungen
- Synopsis: ST John'S College of NursingDokument19 SeitenSynopsis: ST John'S College of NursingsyarifaNoch keine Bewertungen
- Research PresentationDokument35 SeitenResearch PresentationKaku ManiNoch keine Bewertungen
- Jurnal 3Dokument8 SeitenJurnal 3Siska YunitaNoch keine Bewertungen
- Massage AnakDokument8 SeitenMassage AnakNofinta AnggrainiNoch keine Bewertungen
- The Observation of The Curative Effects of Nursing Intervention On The Premature Infant With JaundiceDokument3 SeitenThe Observation of The Curative Effects of Nursing Intervention On The Premature Infant With JaundiceSasha Hidayat FullNoch keine Bewertungen
- Role of Massage Therapy On Reduction of Neonatal Hyperbilirubinemia in Term and Preterm Neonates: A Review of Clinical TrialsDokument10 SeitenRole of Massage Therapy On Reduction of Neonatal Hyperbilirubinemia in Term and Preterm Neonates: A Review of Clinical TrialsEni RahmawatiNoch keine Bewertungen
- Critical AppraisalDokument7 SeitenCritical AppraisalGum GulNoch keine Bewertungen
- Neonatal Pain Management DissertationDokument8 SeitenNeonatal Pain Management DissertationWillSomeoneWriteMyPaperForMeNorman100% (1)
- Nesting DN O2Dokument9 SeitenNesting DN O2septiana dwi lestariNoch keine Bewertungen
- Early Skin-To-skin Contact in NeonatesDokument9 SeitenEarly Skin-To-skin Contact in NeonatesMegan WierzbowskiNoch keine Bewertungen
- CHN1 Lec Session #19 SASDokument9 SeitenCHN1 Lec Session #19 SASMark Raymunstine TamposNoch keine Bewertungen
- Pubmed Preocedimiento Invasivos NeonatalesDokument2 SeitenPubmed Preocedimiento Invasivos NeonataleseddcitoNoch keine Bewertungen
- Neonatal Procedural Pain Exposure and Pain Management in Ventilated Preterm Infants During The First 14 Days of LifeDokument7 SeitenNeonatal Procedural Pain Exposure and Pain Management in Ventilated Preterm Infants During The First 14 Days of LifePaula Andrea Beltran RamirezNoch keine Bewertungen
- YanyanDokument7 SeitenYanyansigitdwimulyoNoch keine Bewertungen
- Synopsis Phototherapy in JaunicDokument5 SeitenSynopsis Phototherapy in JaunicEngr Saeed Ur RehmanNoch keine Bewertungen
- Difference of The Pain During The DPTDokument5 SeitenDifference of The Pain During The DPTKhoirul FikriNoch keine Bewertungen
- Birth Room ResearchDokument15 SeitenBirth Room ResearchCalin BabNoch keine Bewertungen
- Massage Improves Growth Quality by Decreasing Body Fat Deposition in Male Preterm InfantsDokument6 SeitenMassage Improves Growth Quality by Decreasing Body Fat Deposition in Male Preterm InfantsAna LyaNoch keine Bewertungen
- The Effect of The Facilitated Tucking Position in Reducing Vaccination-Induced Pain in NewbornsDokument7 SeitenThe Effect of The Facilitated Tucking Position in Reducing Vaccination-Induced Pain in NewbornsCassanovaNovaNoch keine Bewertungen
- Acta Paediatrica Volume 100 Issue 12 2011 (Doi 10.1111/j.1651-2227.2011.02372.x) Shuko Nagai Naohiro Yonemoto Norotiana Rabesandratana Diavola - Long-Term Effects of Earlier Initiated ContinuousDokument7 SeitenActa Paediatrica Volume 100 Issue 12 2011 (Doi 10.1111/j.1651-2227.2011.02372.x) Shuko Nagai Naohiro Yonemoto Norotiana Rabesandratana Diavola - Long-Term Effects of Earlier Initiated ContinuousNovaNoch keine Bewertungen
- The Effect of Phototherapy (24 Hours) Towards Jaundice Degrees of The Newborn in Hospital Nicu West Nusa Tenggara ProvinceDokument9 SeitenThe Effect of Phototherapy (24 Hours) Towards Jaundice Degrees of The Newborn in Hospital Nicu West Nusa Tenggara ProvinceAnonymous nGCyG4nqhNoch keine Bewertungen
- A Comparative Study On Effect of Ambulation and Birthing Ball On Maternal and Newborn Outcome Among Primigravida Mothers in Selected Hospitals in MangalorDokument4 SeitenA Comparative Study On Effect of Ambulation and Birthing Ball On Maternal and Newborn Outcome Among Primigravida Mothers in Selected Hospitals in MangalorHella WarnierNoch keine Bewertungen
- Effect of Therapeutic Massage On Relieving Pregnancy DiscomfortsDokument8 SeitenEffect of Therapeutic Massage On Relieving Pregnancy DiscomfortsDerison MarsinovaNoch keine Bewertungen
- Weight Gain in Preterm Low Birth Weight Infants With Multisensory InterventionDokument5 SeitenWeight Gain in Preterm Low Birth Weight Infants With Multisensory Interventionagung setiawanNoch keine Bewertungen
- The Effect of Preoperative Fasting To Postoperative NauseaDokument7 SeitenThe Effect of Preoperative Fasting To Postoperative NauseasantiNoch keine Bewertungen
- J. Pediatr. Psychol. 2003 Dieter 403 11Dokument10 SeitenJ. Pediatr. Psychol. 2003 Dieter 403 11knikmahNoch keine Bewertungen
- Artikel 1 Pandita 2018Dokument5 SeitenArtikel 1 Pandita 2018Eline DebaereNoch keine Bewertungen
- Anderson 2019Dokument27 SeitenAnderson 2019Muhammad SawalNoch keine Bewertungen
- Kangaroo Care in Pre-Term or Low Birth Weight Babies in A Postnatal WardDokument8 SeitenKangaroo Care in Pre-Term or Low Birth Weight Babies in A Postnatal Wardanon_922417777Noch keine Bewertungen
- Breastfeeding Is Analgesic in Healthy Newborns: ContextDokument6 SeitenBreastfeeding Is Analgesic in Healthy Newborns: ContextSigit AndriantoNoch keine Bewertungen
- Mi2018 2845352 PDFDokument5 SeitenMi2018 2845352 PDFDewi LarasatiNoch keine Bewertungen
- The Effectiveness of Sucrose As A Pain Reducing Substance During Procedures in NICUDokument11 SeitenThe Effectiveness of Sucrose As A Pain Reducing Substance During Procedures in NICUInternational Journal of Innovative Science and Research TechnologyNoch keine Bewertungen
- Admin,+5 +anes+layoutDokument3 SeitenAdmin,+5 +anes+layoutwewewwe memeNoch keine Bewertungen
- The Effectiveness of Kegel Exercise For The Acceleration of Perineum Wound Healing On Postpartum WomenDokument3 SeitenThe Effectiveness of Kegel Exercise For The Acceleration of Perineum Wound Healing On Postpartum WomenKasmin M. AminNoch keine Bewertungen
- Early Skin-To-Skin Contact For Mothers and Their Healthy Newborn InfantsDokument8 SeitenEarly Skin-To-Skin Contact For Mothers and Their Healthy Newborn InfantsNeelu SharmaNoch keine Bewertungen
- Skin To SkinDokument9 SeitenSkin To SkinAsiatiNoch keine Bewertungen
- PainDokument9 SeitenPainRinda KurniawatiNoch keine Bewertungen
- Infra Red vs. Sitz BathDokument7 SeitenInfra Red vs. Sitz BathMikeNoch keine Bewertungen
- O Gfshds Jjjp4Dokument12 SeitenO Gfshds Jjjp4BentaigaNoch keine Bewertungen
- European Journal of Obstetrics & Gynecology and Reproductive BiologyDokument8 SeitenEuropean Journal of Obstetrics & Gynecology and Reproductive Biologyana pintoNoch keine Bewertungen
- HipotermihipotermiaDokument6 SeitenHipotermihipotermiaRiana Pasca RoshianNoch keine Bewertungen
- 65 128 2 PB Touch TerapiDokument6 Seiten65 128 2 PB Touch Terapilaila muslikhahNoch keine Bewertungen
- Endoscopy in Pediatric Inflammatory Bowel DiseaseVon EverandEndoscopy in Pediatric Inflammatory Bowel DiseaseLuigi Dall'OglioNoch keine Bewertungen
- Treatment Strategy for Unexplained Infertility and Recurrent MiscarriageVon EverandTreatment Strategy for Unexplained Infertility and Recurrent MiscarriageKeiji KurodaNoch keine Bewertungen
- A Cross-Sectional Study On Person-Centred Communication in The Care of Older People: The COMHOME Study ProtocolDokument9 SeitenA Cross-Sectional Study On Person-Centred Communication in The Care of Older People: The COMHOME Study Protocolgladeva yugi antariNoch keine Bewertungen
- List of Irregular VerbsDokument2 SeitenList of Irregular Verbsapi-32189462367% (3)
- Continuity of CareDokument7 SeitenContinuity of Caregladeva yugi antariNoch keine Bewertungen
- Jurnal Mastitis 11 Atau CekDokument14 SeitenJurnal Mastitis 11 Atau Cekgladeva yugi antariNoch keine Bewertungen
- Jurnal Barat 6Dokument6 SeitenJurnal Barat 6gladeva yugi antariNoch keine Bewertungen
- IL-6 in Inflammation, Immunity, and DiseaseDokument3 SeitenIL-6 in Inflammation, Immunity, and Diseasegladeva yugi antariNoch keine Bewertungen
- Jurnal KPDDokument6 SeitenJurnal KPDErka Wahyu KinandaNoch keine Bewertungen
- Maternal Serum Interlukin-6 Level in Preterm Labor: Interleukina 6 W Surowicy Krwi Matki A Poród PrzedwczesnyDokument5 SeitenMaternal Serum Interlukin-6 Level in Preterm Labor: Interleukina 6 W Surowicy Krwi Matki A Poród Przedwczesnygladeva yugi antariNoch keine Bewertungen
- Maternal Serum Interleukin 6 and 8 and C-Reactive Protein in Predicting The Tocolytic Therapy in Preterm LaborDokument5 SeitenMaternal Serum Interleukin 6 and 8 and C-Reactive Protein in Predicting The Tocolytic Therapy in Preterm Laborgladeva yugi antariNoch keine Bewertungen
- The Egyptian Heart Journal: Ahmed Elshazly, Hazem Khorshid, Hany Hanna, Ammar AliDokument3 SeitenThe Egyptian Heart Journal: Ahmed Elshazly, Hazem Khorshid, Hany Hanna, Ammar AliImran TarmiziNoch keine Bewertungen
- Module 4 PPT FinalDokument29 SeitenModule 4 PPT FinalEl LahNoch keine Bewertungen
- Blood Pressure ProjectDokument3 SeitenBlood Pressure ProjectjademvdfNoch keine Bewertungen
- BREASTFEEDINGDokument2 SeitenBREASTFEEDINGFianisa RizkaNoch keine Bewertungen
- Functions and Duties of Psychiatric Social Work by Sanjay VermaDokument10 SeitenFunctions and Duties of Psychiatric Social Work by Sanjay VermaSanjay VermaNoch keine Bewertungen
- SepsisDokument43 SeitenSepsisHamza Shaikh100% (1)
- Sineflex Solutions: Sineflex Dr. Mahesh Iyer (Co Founder)Dokument10 SeitenSineflex Solutions: Sineflex Dr. Mahesh Iyer (Co Founder)Atreyee SarkarNoch keine Bewertungen
- Palliative CareDokument12 SeitenPalliative CareSonya VanceNoch keine Bewertungen
- Public Health CareDokument11 SeitenPublic Health CareFemale calmNoch keine Bewertungen
- CC Lab ActDokument3 SeitenCC Lab ActTrisha IbarraNoch keine Bewertungen
- Telemedicine - Meaning, Challenges and OpportunitiesDokument7 SeitenTelemedicine - Meaning, Challenges and OpportunitiesAim PrimaNoch keine Bewertungen
- Cleansing and Moist Greg Goodman 2009Dokument1 SeiteCleansing and Moist Greg Goodman 2009Prajnamita Manindhya El FarahNoch keine Bewertungen
- Case Presentation 2Dokument11 SeitenCase Presentation 2Angel Jonele ManongsongNoch keine Bewertungen
- Worksheet On Exercise No. 7 Case Study On Diabetes Mellitus 222Dokument7 SeitenWorksheet On Exercise No. 7 Case Study On Diabetes Mellitus 222jameela sapiandanteNoch keine Bewertungen
- Occupational Health and Safety - 2Dokument4 SeitenOccupational Health and Safety - 2Kero KeropiNoch keine Bewertungen
- 7 Steps To The Perfect PICO Search White PaperDokument9 Seiten7 Steps To The Perfect PICO Search White PaperNurkhasanah 71Noch keine Bewertungen
- 2015 Contrast MediaDokument129 Seiten2015 Contrast Medialander55Noch keine Bewertungen
- Research Concept Note For Addmission Into The Doctor of MedicineDokument2 SeitenResearch Concept Note For Addmission Into The Doctor of Medicineumar farukNoch keine Bewertungen
- Depression and Heart Disease - Johns Hopkins Women's Cardiovascular Health CenterDokument3 SeitenDepression and Heart Disease - Johns Hopkins Women's Cardiovascular Health CenterSanjay KumarNoch keine Bewertungen
- CURS - ENGLEZA - Boli Infectioase PDFDokument246 SeitenCURS - ENGLEZA - Boli Infectioase PDFLesan IulianaNoch keine Bewertungen
- Incident vs. Prevalent Cases and Measures of OccurrenceDokument3 SeitenIncident vs. Prevalent Cases and Measures of OccurrenceRenzo FernandezNoch keine Bewertungen
- Albert R JonsenDokument3 SeitenAlbert R JonsenJonathan HigginsNoch keine Bewertungen
- Radiation Therapy of Benign DiseasesDokument355 SeitenRadiation Therapy of Benign Diseasesyves2022sahaNoch keine Bewertungen