Beruflich Dokumente
Kultur Dokumente
a732b273a10a012b40c8154c371e732b
Hochgeladen von
Agus Wijata0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
5 Ansichten1 Seitenn,n v,nsvanla
Copyright
© © All Rights Reserved
Verfügbare Formate
PDF, TXT oder online auf Scribd lesen
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldennn,n v,nsvanla
Copyright:
© All Rights Reserved
Verfügbare Formate
Als PDF, TXT herunterladen oder online auf Scribd lesen
0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
5 Ansichten1 Seitea732b273a10a012b40c8154c371e732b
Hochgeladen von
Agus Wijatann,n v,nsvanla
Copyright:
© All Rights Reserved
Verfügbare Formate
Als PDF, TXT herunterladen oder online auf Scribd lesen
Sie sind auf Seite 1von 1
AB10 Abstracts
SATURDAY
31
The Differential Relationship Between Regulatory T-Cells and
Age in Children with Food Allergy
Benjamin T. Prince, MD1, Kristin A. Erickson1, Christine
Szychlinski, MS, APN, CPNP2, Robert P. Schleimer, PhD, FAAAAI3,
Paul Bryce, PhD3, Anne Marie Singh, MD1,2; 1Division of Allergy-Immunology, Department of Pediatrics, Northwestern University Feinberg
School of Medicine, Chicago, IL, 2Division of Allergy-Immunology,
Department of Pediatrics, Ann & Robert H. Lurie Childrens Hospital
of Chicago, Chicago, IL, 3Division of Allergy-Immunology, Department
of Medicine, Northwestern University Feinberg School of Medicine, Chicago, IL.
RATIONALE: Regulatory T (Treg) cells are well known to play an
important role in the maintenance of self-tolerance, and patients who lack
these cells, such as in IPEX syndrome, have an increased incidence of
allergic disease. Although studies have highlighted differences in peripheral blood Treg populations of atopic adults, only a few conflicting studies
have examined differences in Tregs among children with allergic diseases.
METHODS: Peripheral blood mononuclear cells were isolated from 47
patients (0-18yrs) and analyzed using flow cytometry for CD3, CD4,
CD25, CD127, CCR6, and Foxp3. Populations of Tregs, defined as
CD4+CD25hiCD127loFoxp3+, were compared in food allergic children
and healthy controls using a 2-tailed Students t-test and linear regression
modeling.
_6yrs had significantly lower percentRESULTS: Food allergic children <
ages (p<0.05) of Tregs compared to healthy controls of similar age. This
difference was not observed in older children. There was a significant
decrease in both Treg cell percentages (p50.018, R50.584) and Treg
expression of Foxp3 (p50.012, R50.613) with age in healthy controls but
not in children with food allergy. Finally, food allergic children >6yrs had
significantly less Tregs expressing CCR6 (p<0.05), a gut-homing marker,
and this cell population significantly increased with age (p50.013,
R50.626) in healthy controls but not food allergic children.
CONCLUSIONS: Younger, food allergic children had significantly lower
percentages of Tregs compared to healthy controls, and this difference did
not persist with older children. This supports the hypothesis that early
childhood is likely a critical time in the development of normal immune
regulation and that Tregs are important in this process.
32
Glutathione S-Transferase Mu 1 (GSTM1) Gene Associated with
Allergic Rhinitis in a Food Allergy Cohort
Sheva K. Chervinskiy, DO1, Lisa Smeester2, Michael D. Kulis, Jr, PhD3,
David B. Peden, MD, MS, FAAAAI4, Brian P. Vickery, MD5, Rebecca C.
Fry, PhD6; 1Department of Pediatrics, University of North Carolina,
Chapel Hill, NC, 2Gillings School of Public Health, University of North
Carolina, Chapel Hill, NC, 3University of North Carolina School of Medicine, Chapel Hill, NC, 4Office #544, Campus Box 7310, University of
North Carolina at Chapel Hill School Medicine, NC, 5Department of Pediatrics, University of North Carolina, Chapel Hill, North Carolina, USA,
6
Gillings School of Public Health, University of North Carolina, Chapel
Hill NC.
RATIONALE: GSTM1 genes have been implicated in atopic inflammatory diseases. In this study, we explored whether GSTM1 genotype was
associated with food allergy phenotypes.
METHODS: Biospecimens from 100 randomly sampled food allergy
research subjects were collected for gene analysis. GSTM1 gene analysis
was carried out as previously described. We conducted a retrospective
chart review to collect phenotypic information, including past medical
history, number of allergic foods, serum specific IgE and food allergy
treatment response. Mann-Whitney and Chi-square analysis was
performed.
RESULTS: Of the 100 samples obtained, 81 subjects were successfully
genotyped, and 48/81 (x %) had a null GSTM1 genotype. Of the genotyped
subjects, 68 were successfully phenotyped via chart review. GSTM1 status
had no significant association with specific IgE, number of food allergies,
or response to food allergy treatment, as measured by food challenge
outcomes. There was no statistically significant association between
J ALLERGY CLIN IMMUNOL
FEBRUARY 2015
GSTM1 genotype with reported history of asthma or atopic dermatitis.
We found that patients with a GSTM1 genotype had a statistically
significant association with the incidence of allergic rhinitis in in this
cohort (p5 0.03).
CONCLUSIONS: In this cohort of food allergy patients, allergic rhinitis
was significantly associated with the GSTM1 genotype. This supports
previous studies revealing the association of this gene with allergic airway
disease. GSTM1 did not impact food allergy phenotype nor treatment
response to food allergy desensitization.
33
Disseminated Atypical Mycobacterial Infection in Three
Patients with Complete Digeorge Anomaly
Noah O. Agada, MD1, Suellen M. Yin, MD2, Jonathan S. Tam, MD2,
Matthew S. Kelly, MD1, M. Louise Markert, MD, PhD, FAAAAI1;
1
Duke University Medical Center, Durham, NC, 2Childrens Hospital
Los Angeles, Los Angeles, CA.
RATIONALE: Complete DiGeorge anomaly is a primary immunodeficiency characterized by athymia with fewer than 50 nave T cells/mm3
associated with either a cardiac defect or hypoparathyroidism.
Disseminated mycobacterial infection has not been described in these
patients. We present three cases of disseminated atypical mycobacterial
infection that developed among children with complete DiGeorge
anomaly.
METHODS: Clinical, laboratory, immunologic and radiologic data of
patients with complete DiGeorge anomaly referred to Duke University for
transplant were reviewed.
RESULTS: In patient 1 (P1), the diagnosis of disseminated mycobacterium avium complex (MAC) was made by lung biopsy 4 months after
thymus transplantation after a mass was noted on chest CT obtained to
evaluate for a source of fevers. P2 was diagnosed with MAC 2.4 months
after thymus transplantation from a mycobacterial blood culture obtained
for persistent fever. P2 was given steroids for possible immune reconstitution inflammatory syndrome when fevers recurred 18 days after starting
anti-mycobacterial therapy. In P3, a chest CT obtained to evaluate fevers
revealed lymphadenopathy and mycobacterial culture of a thoracic lymph
node biopsy grew Mycobacterium kansasii. P1 is on enteral medications
for MAC at 22 months post-transplantation and has normal T cell numbers.
P2 died 5 months after transplantation with finding of disseminated MAC
on autopsy. Flow cytometry revealed nave T cell development; the autopsy
showed thymopoiesis. P3 is 3 months post-transplantation, remains on
anti-mycobacterial treatment, and has not yet developed nave T cells.
CONCLUSIONS: Azithromycin or clarithromycin prophylaxis should be
considered for patients with complete DiGeorge anomaly. Aggressive antimycobacterial therapy without steroids is recommended.
Das könnte Ihnen auch gefallen
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (119)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (587)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2219)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (894)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- JHA Installation of Solar PanelDokument4 SeitenJHA Installation of Solar Panelperquino oasan100% (3)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- 7 Day Free Guide PDFDokument14 Seiten7 Day Free Guide PDFGuille RodriguezNoch keine Bewertungen
- HairDokument4 SeitenHairRena Carissa100% (1)
- About Critical Care NursingDokument7 SeitenAbout Critical Care NursingaivynNoch keine Bewertungen
- DR, OR, WardDokument14 SeitenDR, OR, WardjanNoch keine Bewertungen
- Antenatal & Postnatal Care: 1. General InformationDokument7 SeitenAntenatal & Postnatal Care: 1. General InformationanishnithaNoch keine Bewertungen
- Efficacy of Transpalatal Arch As An Anchorage Rein PDFDokument7 SeitenEfficacy of Transpalatal Arch As An Anchorage Rein PDFOana CostanNoch keine Bewertungen
- Drug Doses 2017Dokument127 SeitenDrug Doses 2017Yuliawati HarunaNoch keine Bewertungen
- Link Zoom KONIKA 18-19 OctDokument6 SeitenLink Zoom KONIKA 18-19 OctAgus WijataNoch keine Bewertungen
- 7869 40826 3 PB PDFDokument8 Seiten7869 40826 3 PB PDFHendra AjaNoch keine Bewertungen
- Pediatric Infectious Diseases Conference Focuses on COVID ManagementDokument2 SeitenPediatric Infectious Diseases Conference Focuses on COVID ManagementAgus WijataNoch keine Bewertungen
- Pone 0026881Dokument5 SeitenPone 0026881Agus WijataNoch keine Bewertungen
- 7869 40826 3 PB PDFDokument8 Seiten7869 40826 3 PB PDFHendra AjaNoch keine Bewertungen
- Mile-Stones of Develovment of ChildrenDokument9 SeitenMile-Stones of Develovment of ChildrenAgus WijataNoch keine Bewertungen
- Pediatric Infectious Diseases Conference Focuses on COVID ManagementDokument2 SeitenPediatric Infectious Diseases Conference Focuses on COVID ManagementAgus WijataNoch keine Bewertungen
- Faktor-Faktor Yang Berhubungan Dengan Kejadian Berat Badan Lahir Rendah (BBLR) Di Kabupaten KudusDokument10 SeitenFaktor-Faktor Yang Berhubungan Dengan Kejadian Berat Badan Lahir Rendah (BBLR) Di Kabupaten KudusDellaNoch keine Bewertungen
- Pediatric Infectious Diseases Conference Focuses on COVID ManagementDokument2 SeitenPediatric Infectious Diseases Conference Focuses on COVID ManagementAgus WijataNoch keine Bewertungen
- Wed SongDokument1 SeiteWed SongAgus WijataNoch keine Bewertungen
- Kids Games Powerpoint TemplateDokument26 SeitenKids Games Powerpoint TemplateAgus WijataNoch keine Bewertungen
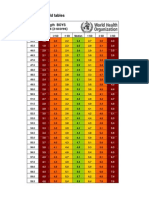
- Boys weight-length z-scores birth to 2 yearsDokument5 SeitenBoys weight-length z-scores birth to 2 yearsAgus WijataNoch keine Bewertungen
- Nna en November09Dokument3 SeitenNna en November09Agus WijataNoch keine Bewertungen
- Early Biochemical Indicators of Hypoxic-Ischemic Encephalopathy After Birth AsphyxiaDokument5 SeitenEarly Biochemical Indicators of Hypoxic-Ischemic Encephalopathy After Birth AsphyxiaAgus WijataNoch keine Bewertungen
- Espr Abstracts: Background: Hypoxic-Ischemic Brain Injury (HIE) Is The Most Common Perinatal Cerebral Insult AssociatedDokument1 SeiteEspr Abstracts: Background: Hypoxic-Ischemic Brain Injury (HIE) Is The Most Common Perinatal Cerebral Insult AssociatedAgus WijataNoch keine Bewertungen
- Biochemical Marker As Predictor of Outcome in Perinatal AsphyxiaDokument4 SeitenBiochemical Marker As Predictor of Outcome in Perinatal AsphyxiaAgus WijataNoch keine Bewertungen
- Status of Serum Bilirubin, Serum Proteins and Prothrombin Time in Babies With Perinatal AsphyxiaDokument4 SeitenStatus of Serum Bilirubin, Serum Proteins and Prothrombin Time in Babies With Perinatal AsphyxiaAgus WijataNoch keine Bewertungen
- 0 C 96053 C 581 B 042832000000Dokument1 Seite0 C 96053 C 581 B 042832000000Agus WijataNoch keine Bewertungen
- Edwin Kim, MD A. Wesley Burks, MD Michael Pistiner, MD, MMSCDokument1 SeiteEdwin Kim, MD A. Wesley Burks, MD Michael Pistiner, MD, MMSCAgus WijataNoch keine Bewertungen
- SDQ Score Sheet and Instructions For Self ReoprtDokument2 SeitenSDQ Score Sheet and Instructions For Self ReoprtAgus WijataNoch keine Bewertungen
- CC 100Dokument4 SeitenCC 100Agus WijataNoch keine Bewertungen
- Neuron-Specific Enolase As A Marker of The Severity and Outcome of Hypoxic Ischemic EncephalopathyDokument5 SeitenNeuron-Specific Enolase As A Marker of The Severity and Outcome of Hypoxic Ischemic EncephalopathyAgus WijataNoch keine Bewertungen
- Test Definition: NSE: Reporting Title: Neuron Specific Enolase, SDokument1 SeiteTest Definition: NSE: Reporting Title: Neuron Specific Enolase, SAgus WijataNoch keine Bewertungen
- Antimicrob. Agents Chemother. 2015 Ramachandran 1162 7Dokument6 SeitenAntimicrob. Agents Chemother. 2015 Ramachandran 1162 7Agus WijataNoch keine Bewertungen
- 0 C 96053 C 581 B 042832000000Dokument1 Seite0 C 96053 C 581 B 042832000000Agus WijataNoch keine Bewertungen
- 5211Dokument7 Seiten5211Agus WijataNoch keine Bewertungen
- SDQ Score Sheet and Instructions For Self ReoprtDokument2 SeitenSDQ Score Sheet and Instructions For Self ReoprtAgus WijataNoch keine Bewertungen
- Apnea NewbornDokument2 SeitenApnea NewbornAgus WijataNoch keine Bewertungen
- To Compare Rosuvastatin With Atorvastatin in Terms of Mean Change in LDL C in Patient With Diabetes PDFDokument7 SeitenTo Compare Rosuvastatin With Atorvastatin in Terms of Mean Change in LDL C in Patient With Diabetes PDFJez RarangNoch keine Bewertungen
- Gems of Homoepathic Materia Medica J D Patil.01602 - 2belladonnaDokument7 SeitenGems of Homoepathic Materia Medica J D Patil.01602 - 2belladonnaPooja TarbundiyaNoch keine Bewertungen
- Garfinkel Case at The University of MinnesotaDokument9 SeitenGarfinkel Case at The University of MinnesotaMarkingsonCaseNoch keine Bewertungen
- ns3360 Lesson Plans Spring2014Dokument11 Seitenns3360 Lesson Plans Spring2014api-232466940Noch keine Bewertungen
- Audit Program Ppi (Mariani, SKM, Mha)Dokument23 SeitenAudit Program Ppi (Mariani, SKM, Mha)Dedy HartantyoNoch keine Bewertungen
- TEMPLATE-B-Master-list-of-Learners-for-the-Pilot-Implementation-of-F2F-Classes-for-S.Y.-2021-2022Dokument7 SeitenTEMPLATE-B-Master-list-of-Learners-for-the-Pilot-Implementation-of-F2F-Classes-for-S.Y.-2021-2022Resa Consigna MagusaraNoch keine Bewertungen
- Bradford Assay To Detect Melamine ConcentrationsDokument3 SeitenBradford Assay To Detect Melamine ConcentrationsVibhav SinghNoch keine Bewertungen
- Jobs Safety Analysis for Radiography WorkDokument4 SeitenJobs Safety Analysis for Radiography WorkGan KusumaNoch keine Bewertungen
- Resume 101: Write A Resume That Gets You NoticedDokument16 SeitenResume 101: Write A Resume That Gets You Noticedgqu3Noch keine Bewertungen
- Organsymbol KartenDokument24 SeitenOrgansymbol KartenMacaio100% (2)
- Rosemont Health Center Rev01Dokument7 SeitenRosemont Health Center Rev01Amit VishwakarmaNoch keine Bewertungen
- The Ethics of Medical Marijuana Government Restrictions vs. Medical Necessity - An UpdateDokument12 SeitenThe Ethics of Medical Marijuana Government Restrictions vs. Medical Necessity - An UpdateAle PicadoNoch keine Bewertungen
- CAE-UOE Part1Dokument4 SeitenCAE-UOE Part1nikitsaNoch keine Bewertungen
- Life 2E Pre-Intermediate Unit 1 WB PDFDokument8 SeitenLife 2E Pre-Intermediate Unit 1 WB PDFTrần Quý Dương100% (2)
- Biochemistry For Anesthesiologists and IntensivistsDokument11 SeitenBiochemistry For Anesthesiologists and IntensivistsAndi tenri sanda datuNoch keine Bewertungen
- ConclusionDokument1 SeiteConclusionSamNoch keine Bewertungen
- ICU HandoverDokument2 SeitenICU HandoverMark 'Mark Douglas' DouglasNoch keine Bewertungen
- Femoral Fractures in Children: Surgical Treatment. Miguel Marí Beltrán, Manuel Gutierres, Nelson Amorim, Sérgio Silva, JorgeCoutinho, Gilberto CostaDokument5 SeitenFemoral Fractures in Children: Surgical Treatment. Miguel Marí Beltrán, Manuel Gutierres, Nelson Amorim, Sérgio Silva, JorgeCoutinho, Gilberto CostaNuno Craveiro LopesNoch keine Bewertungen
- Material Safety Data Sheet: Tert-Amyl Alcohol MSDSDokument6 SeitenMaterial Safety Data Sheet: Tert-Amyl Alcohol MSDSmicaziv4786Noch keine Bewertungen
- Science Chapter on ReproductionDokument4 SeitenScience Chapter on ReproductionAnita GargNoch keine Bewertungen
- Drug Study HydrocodoneDokument1 SeiteDrug Study HydrocodoneYlrenne DyNoch keine Bewertungen
- Surat Izin Masuk: FM.01-AOP - ROM/Rev.4.0/29.01.2020Dokument4 SeitenSurat Izin Masuk: FM.01-AOP - ROM/Rev.4.0/29.01.2020Donking ThotosikNoch keine Bewertungen
- Renal Regulation of Extracellular Fluid Potassium ConcentrationDokument32 SeitenRenal Regulation of Extracellular Fluid Potassium ConcentrationDaniel AdamsNoch keine Bewertungen