Beruflich Dokumente
Kultur Dokumente
Molecules: in Vitro Activity of Plant Extracts and Alkaloids Against Clinical
Hochgeladen von
Julian FelixOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Molecules: in Vitro Activity of Plant Extracts and Alkaloids Against Clinical
Hochgeladen von
Julian FelixCopyright:
Verfügbare Formate
Molecules 2011, 16, 5453-5459; doi:10.
3390/molecules16075453
OPEN ACCESS
molecules
ISSN 1420-3049
www.mdpi.com/journal/molecules
Article
In Vitro Activity of Plant Extracts and Alkaloids against Clinical
Isolates of Extended-Spectrum -Lactamase (ESBL)-Producing
Strains
Guo-Ying Zuo 1,*, Fan-Yan Meng 1,2, Jun Han 3, Xiao-Yan Hao 2,*, Gen-Chun Wang 1,
Yun-Ling Zhang 1 and Qing Zhang 1
1
Research Center for Natural Medicines, Kunming General Hospital, PLA, Kunming 650032, China;
E-Mails: zhangyunling@126.com (Y.-L.Z.); kmz@263.net (Q.Z.)
School of Pharmacy, Guiyang Medical College, Guiyang 550004, China;
E-Mail: mfy_0@163.com (F.-Y.M.)
School of Basic Medicine, Yunnan Traditional Chinese Medical College, Kunming 650500, China;
E-Mail: hanzjn@126.com (J.H.)
* Authors to whom correspondence should be addressed; E-Mails: zuogouiyng@263.net (G.-Y.Z);
haoxiaoyan@vip.163.com (X.-Y.H); Tel.: +86-871-4774941; Fax: +86-871-4774941 (G.-Y.Z).
Received: 23 May 2011; in revised form: 12 June 2011 / Accepted: 13 June 2011 /
Published: 28 June 2011
Abstract: The antibacterial activity of 80% ethanol extracts of 10 medicinal plants
collected in Yunnan (Southwest China), was tested against clinical isolates of extendedspectrum -lactamase (ESBL)-producing strains. Their MIC values ranged between
1.5612.50 mg/mL. The most active plant extract was Chelidonium majus L.
(MIC = 1.56 mg/mL). Two potent isoquinoline alkaloids, 8-hydroxydihydrosanguinarine
and 8-hydroxydihydrochelerythrine, were identified as the major active principles through
bioassay-guided fractionation and identification of the active ethyl acetate fraction from
C. majus, with minimum MIC/MBC values of 15.63/62.50 g/mL.
Keywords: antibacterial plant
8-hydroxydihydrochelerythrine
extracts;
ESBLs;
8-hydroxydihydrosanguinarine;
Molecules 2011, 16
5454
1. Introduction
Extended-spectrum -lactamases (ESBLs) are enzymes produced in some Gram-negative bacilli
that mediate resistance to extended-spectrum antibiotics like cephalosporin and aztreonam. The first
clinical isolates expressing acquired ESBLs were identified in Germany in 1983 [1]. ESBLs have the
ability to hydrolyse and cause resistance to various types of the newer -lactam antibiotics, including
the expanded-spectrum (or third-generation) cephalosporins (e.g., cefotaxime, ceftriaxone, ceftazidime)
and monobactams (e.g., aztreonam), but not the cephamycins (e.g., cefoxitin and cefotetan) and
carbapenems (e.g., imipenem, meropenem, and ertapenem). They are most common in clinical isolates
of Escherichia coli and Klebsiella pneumoniae of the Enterobacteriaceae. The ESBL-producing
multidrug-resistant (MDR) pathogens are the result of the selective pressure of currently used
antibiotics and have been well recognized as a global nosocomial problem in recent years [2]. As
plants can produce antimicrobial compounds to protect themselves from biotic attack, the search for
antibacterial agents with different chemical structure and biological mode of action from plant sources
is an alternative option in the fight against these microbes [3-5].
In the course of screening for active plant products against MDR bacteria, we paid special attention
to the effects of Chinese medicinal plants on clinical isolates of ESBL-producing microorganisms.
Here, we report the activities of ten plant extracts and two potent isoquinoline alkaloids
8-hydroxydihydrosanguinarine (hhS, 1) and 8-hydroxydihydrochelerythrine (hhC, 2), obtained through
bioassay-guided fractionation and identification from one of the active extracts of Chelidonium majus L.
(bai-qu-cai in Chinese, [6]).
2. Results and Discussion
As shown in Table 1, various potencies against MDR and the ATCC control of E. coli were
demonstrated by the tested extracts, with inhibitory zone diameters (IZDs) of 11.021.0 mm and MIC
values of 1.5612.50 mg/mL, respectively. Most of the extracts were active not only against MDR
but also non-MDR strains of E. coli, which suggested the different mechanisms of effect and their
potentials as alternative sources for combating the increasingly troublesome problem of bacterial
infections in hospitals [2].
Bioassay-guided fractionation and isolation of an active extract from C. majus led to the
identification of the 8-hydroxylated benzo[c]phenanthridine alkaloids hhS and hhC as the major active
compounds. They showed potent activity against both clinical MDR isolates and ATCC control strains
of E. coli, with the low MIC of 15.63 g/mL (Figure 1 and Table 2). Other compounds in the active
extracts are under investigation.
From the results in Table 2, it is noted that though they were both phenotypic confirmatory
ESBL-producing strains, the activity of hhS and hhC against such strains from E. coli were general
much more active than those from K. pneumoniae. This could be attributed to the different resistance
profiles of the two bacterial species with different genotypes [1,2].
Molecules 2011, 16
5455
Table 1. IZD (mm) and MIC (mg/mL) of the crude extracts and active fractions against selected strains.
KUN201236 Wp
Ec b
IZD
20.0
MIC
1.56
Ec-MDR c
IZD
MIC
15.0
3.12
Anacardiaceae
KUN61317
16.0
3.12
13.0
6.25
Papaveraceae
KUN201093 Ap
21.0
3.12
14.0
3.12
No.
Species
Family
Speciesmen
number
Chelidonium majus L.
Galla Chinensis
(Rhus chinensis)
Macleaya cordata
(Willd.) R. Br.
Medinilla
luchuenensis C. Y.
Wu et C. Chen
Michelia chapaensis
Dandy
Papaveraceae
2
3
4
5
Melastomataceae KUN372
13.0
3.12
11.0
6.25
Magnoliaceae
Rh
15.0
3.12
12.0
6.25
Ap
12.0
6.25
11.0
12.50
16.0
3.12
13.0
3.12
Sagentodoxaceae KUN3514
14.0
3.12
11.0
6.25
Theaceae
YCP85965
Ap
11.0
12.50 NA d
NA d
Carprifoliaceae
KUN287
Ap
NA d
NA d
NA d
NA d
Papaveraceae
Papaveraceae
Papaveraceae
KUN201236 Fr-E
KUN201236 Fr-E1
KUN201236 Fr-E2
19.0
26.0
22.0
1.56
0.39
0.78
17.0
20.0
19.0
3.12
1.56
1.56
Myrsine africana L.
Myrsinaceae
Paeonia lactiflora
Pall.
Sagentodoxa cuneata
(Oliv.) Rehd. et Wils.
Eurya yunnanensis
P.S. Hsu
Viburnum foetidum
Will. Var. foetidum
C. majus
C. majus
C. majus.
Ranunculaceae
8
9
10
11
12
13
Part a
KUN12152
HITBC
032831
KUN
365353
Ap: aerial parts; F: fruits; R: roots; Rh: rhizome; Wp: whole plants; W: wart, Fr-E: ethyl acetate
fraction; Fr-E1 and Fr-E2,: two sub-fractions of Fr-E; b Ec: E. coli (ATCC25922); c Ec-MDR: A
total of five selected isolates of ESBLs-producing strains were tested; d NA: not active at
concentrations up to 50 mg/mL.
Figure 1. Structures of the four alkaloids (1: hhS; 2: hhC; 3: hS; 4: hC).
O
O
N
R2O
CH3
OR1
R3
1
2
3
4
R1
R1
R1
R1
R2 = CH2 , R3 = OH
= R2 = CH3 , R3 = OH
R2 = CH2 , R3 = H
= R2 = CH3 , R3 = H
C. majus has a long history in Chinese and European herbal medicine [6,7] as being useful for the
treatment of many diseases. The present study reveals its in vitro anti-MDR activities against clinical
isolates of ESBL-producing strains for the first time as far as we are aware [7,8]. It was found that
Molecules 2011, 16
5456
among the four tested alkaloids the 8-hydroxylated ones were generally more active than the nonhydroxylated alkaloids. This type of alkaloids has been previously demonstrated to possess activity
against clinical isolates of methicillin-resistant Staphylococcus aureus (MRSA) and resistant clinical
yeast isolates [9,10]. Hence, they show broad-spectrum antimicrobial properties. However, to assess
the efficacy and safety of these extracts and pure compounds, further in vitro and in vivo
pharmacological assays are needed.
Table 2. MICs and MBCs of the alkaloids and control agent for strains of clinical isolates.
Strain and agent
MIC (g/mL )
Range
90%
MBC (g/mL)
Range
50%
50%
90%
15.63250.0
62.50500.0
750.03000.0
1500.03000.0
0.030.50
31.25
125.0
1500 d
3000 d
0.12
125.0
250.0
3000 d
3000 d
0.25
62.50500.0
125.001000.0
NA d
NA d
0.12-2.0
62.50
125.0
NA d
NA d
0.25
250.0
500.0
NA d
NA d
0.50
93.8375.0
187.5750.0
750.03000.0
1500.03000.0
0.061.00
187.5
187.5
1500 d
3000 d
0.25
375.0
375.0
3000 d
3000 d
0.50
375.01500.0
375.01500.0
NA d
NA d
0.122.0
750.0
750.0
NA d
NA d
0.500
1500.0
1500.0
NA d
NA d
1.00
Ec-MDR
hhS
hhC
hS
hC
imipenem
K p-MDR b
hhS
hhC
hS
hC
imipenem
Ec c
hhS
hhC
hS
hC
imipenem
15.63
125.0
375.0
375.0
0.12
31.25
250.0
1500.0
1500.0
0.25
Ec-MDR: 18 isolates of ESBLs-producing strains from E. coli; b K p-MDR: 12 isolates of ESBLsproducing strains from K. pneumonia; c Ec: E. coli (ATCC25922); d NA: not active at concentrations
up to 3000 g/mL.
3. Experimental
3.1. Plant Material
Ten authenticated plant materials (Table 1) were collected in the mountainous Dali and Honghe
districts of Yunnan Province, China, at attitudes of 6002,500 m in September of 2007. They were
identified by Shui Yuming of t he Kunming Institute of Botany, the Chinese Academy of Science
(CAS, China) where voucher specimens were deposited.
3.2. Bacterial Strains and Culture Media
ESBL-producing MDR strains (18 from E. coli and 12 from K. pneumoniae isolates, respectively)
were obtained from the infectious samples of critically ill patients at Kunming General Hospital
Molecules 2011, 16
5457
(KGH). Pathogen purification and identification were conducted in the clinical microbiology
laboratory of KGH following the standard procedures and the criteria of the Clinical and Laboratory
Standards Institute (CLSI) [11-13]. Briefly, the isolates were initially screened using disks of
ceftazidime (30 g) and aztreonam (30 g), and confirmed by using both ceftazidime and cefotaxime
(30 g), alone and in combination with clavulanic acid (10 g). An isolate of a 5-mm increase in a
zone diameter for either antimicrobial agent tested in combination with clavulanic acid compared with
its zone when tested alone [e.g., ceftazidime zone = 16 mm; ceftazidime-clavulanic acid (30/10 g)
zone = 21 mm] was identified as an ESBL-producing isolate. The control strain ATCC 25922 (E. coli)
was obtained from the National Institute for the Control of Pharmaceutical and Biological Products
(NICPBP, China). Standard Mueller-Hinton agar and broth (MHA and MHB, Tianhe Microbial Agents
Co., Hangzhou, China) were used as culture media. Imipenem (Merck & Co., Inc.) was used as the
positive control agent.
3.3. Extract Preparation and Isolation of the Active Compounds from C. majus Extracts
The air-dried and ground plant material (30 g) was macerated with 80% ethanol (500 mL) for 5 days,
filtered and the mare was further macerated twice with the same solvent overnight and filtered after
being sonicated for 30 min. The filtrates were combined and the solvent was evaporated at 40 C under
vacuum. Ten extracts were prepared as a whole (Table 1).
A larger sample (300 g) of active extract from C. majus (3 kg) was suspended in 600 mL of
sterilized and deionated water and the suspension was successively fractionated between water and
petroleum ether and AcOEt, of which the AcOEt fraction (Fr-E) showed the most activity in a
bioassay-guided fractionation procedure. The fraction (25 g) was subjected to vacuum liquid
chromatography over silica gel-H (500 mesh, Qingdao Haiyang Chemical Co., Ltd. Qingdao, China)
and eluted with gradients of CHCl3MeOH to afford two active fractions (Fr-E1 and Fr-E2), which
were further purified by reverse-phase HPLC column chromatography to yield the two alkaloids 1
(15.4 mg) and 2 (8.5 mg), respectively. Two other alkaloids, dihydrosanguinarine (hS, 3, 200 mg) and
dihydrochelerythrine (hC, 4, 80 mg), were also obtained. All the spectral data were in agreement with
the literature [14,15]. Their structures are shown in Figure 1. The MIC and MBC of the four alkaloids
were determined accordingly at concentrations ranged from 0.0033.0 mg/mL (Table 2).
3.4. Susceptibility Test
The ten extracts were first subjected to a susceptibility test of their IZD (mm) following the previous
agar well diffusion method with a slight modification [16]. The inoculums were 1.5 108 CFU/mL
suspensions and 70 L aliquots of the extracts (50 mg/mL in 50% aqueous DMSO) were placed in
6 mm (diam.) agar wells, incubated at 35 C for 24 h. The MIC of the extracts (concentrations ranged
from 0.550 mg/mL in 50% DMSO) for each organism were determined by the two-fold serial broth
macro dilution method with MHB in tubes [12,16,17], with a slight modification as incubated at 35 C
for 24 h and each tube contained inoculums of 5 105 CFU/mL. All experiments were carried out in
triplicate with 50% aqueous DMSO as the solvent control. The results are shown in Table 1.
Molecules 2011, 16
5458
4. Conclusions
Ten Chinese medicinal plant extracts demonstrated varying levels of activity against clinical
isolates of extended-spectrum -lactamase (ESBL)-producing strains. Four alkaloids were identified
from C. majus extracts, with 8-hydroxydihydrosanguinarine and 8-hydroxydihydrochelerythrine being
the most active compounds. Their clinical utility against infections of ESBLs producers warrant further
pharmacological investigations.
Acknowledgments
This work was supported by a grant from the National Natural Science Foundation of China (NSFC
81073126) and the supporting fund of Yunnan Province of China (2008PY001). We are also grateful
to the Kunming Institute of Botany (CAS) for spectral analysis.
Conflict of Interest
The authors declare no conflict of interest.
References
Gniadkowski, M. Evolution and epidemiology of extended-spectrum -lactamases (ESBLs) and
ESBL-producing microorganisms. Clin. Microbiol. Infect. 2001, 7, 597608.
2. Pitout, J.D.D.; Laupland, K.B. Extended-spectrum -lactamase-producing enterobacteriaceae, an
emerging public health concern. Lancet Infect. Dis. 2007, 8, 159166.
3. Ahmad, I.; Aqil, F. In vitro efficacy of bioactive extracts of 15 medicinal plants against
ESL-producing multidrug-resistant enteric bacteria. Microbiol. Res. 2007, 162, 264275.
4. Lai, P.K.; Roy, J. Antimicrobial and chemopreventive properties of herbs and spices. Curr. Med.
Chem. 2004, 11, 14511460.
5. Stavri, M.; Piddock, L.J.; Gibbons, S. Bacterial efflux pump inhibitors from natural sources.
J. Antimicrob. Chemother. 2007, 59, 12471260.
6. Jiangsu New Medical College. Bai-qu-cai Chelidonium majus L. In Dictionary of Chinese
Materia Medica; Shanghai Scientific Technical Press: Shanghai, China, 1977; Volume 1,
pp. 726727.
7. Colombo, M.L.; Bosisio, E. Pharmacological activities of Chelidonium majus L. (Papaveraceae).
Pharmacol. Res. 1996, 33, 127134.
8. Gibbons, S. Anti-staphylococcal plant natural products. Nat. Prod. Rep. 2004, 21, 263277.
9. Zuo, G.Y.; Meng, F.Y.; Hao, X.Y.; Zhang, Y.L.; Wang, G.C.; Xu, G.L. Antibacterial Alkaloids
from Chelidonium majus Linn (Papaveraceae) against clinical isolates of methicillin-resistant
Staphylococcus aureus. J. Pharm. Pharmaceut. Sci. 2008, 11, 9094.
10. Meng, F.Y.; Zuo, G.Y.; Hao, X.Y.; Wang, G.C.; Xiao, H.T.; Zhang, J.Q.; Xu, G.L. Antifungal
activity of the benzo[c]phenanthridine alkaloids from Chelidonium majus Linn against resistant
clinical yeast isolates. J. Ethnopharmacol. 2009, 125, 494496.
11. Clinical and Laboratory Standards Institute. Performance Standards for Antimicrobial Disk
Susceptibility Tests. Approved Standard; CLSI: Wayne, PA, USA, 2006; M2A9.
1.
Molecules 2011, 16
5459
12. Clinical and Laboratory Standards Institute. Performance Standards for Antimicrobial
Susceptibility Testing17th Informational Supplement. Approved Standard; CLSI: Wayne, PA,
USA, 2007; M100S17.
13. Farmer, J.J., III. Enterobacteriaceae, Introduction, Identification. In Manual of Clinical
Microbiology, 7th Ed.; Murray, P.R., Baron, E.J., Pfaller, M.A., Tenover, F.C., Yolken, R.H.,
Eds.; American Society of Microbiology: Washington, DC, USA, 1999; pp. 442458.
14. Cho, K.M.; Yoo, I.D.; Kim, W.G. 8-Hydroxydihydrochelerythrine, 8-hydroxydihydroSanguinarine
with a potent acetylcholinesterase inhibitory activity from Chelidonium majus L. Biol. Pharm.
Bull. 2006, 29, 23172320.
15. Navarro, V.; Delgado, G. Two antimicrobial alkaloids from Bocconia arborea. J. Ethnopharmacol.
1999, 66, 223226.
16. Okoli, A.S.; Okeke, M.I.; Iroegbu, C.U.; Ebo, P.U. Antibacterial activity of Harungana
madagascariensis leaf extracts. Phytother. Res. 2002, 16, 174179.
17. Clinical and Laboratory Standards Institute. Methods for Dilution Antimicrobial Susceptibility
Tests for Bacteria that Grow Aerobically, 7th Edition; Approved Standard; CLSI: Wayne, PA,
USA, 2006; M7A7.
Sample Availability: Samples of the compounds 14 are available from the authors.
2011 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article
distributed under the terms and conditions of the Creative Commons Attribution license
(http://creativecommons.org/licenses/by/3.0/).
Das könnte Ihnen auch gefallen
- Metabolic Inhibitors V1: A Comprehensive TreatiseVon EverandMetabolic Inhibitors V1: A Comprehensive TreatiseR HochsterNoch keine Bewertungen
- Antibacterial Alkaloids From Chelidonium Majus Linn (Papaveraceae) Against Clinical Isolates of Methicillin-Resistant Staphylococcus AureusDokument5 SeitenAntibacterial Alkaloids From Chelidonium Majus Linn (Papaveraceae) Against Clinical Isolates of Methicillin-Resistant Staphylococcus AureusFitrianidilaNoch keine Bewertungen
- Jefa (Rv2459), A Drug Efflux Gene in Mycobacterium TuberculosisDokument3 SeitenJefa (Rv2459), A Drug Efflux Gene in Mycobacterium TuberculosisaristyabudiarsoNoch keine Bewertungen
- Rhizoma Extracts On Methicillin-Resistant Staphylococcus AureusDokument5 SeitenRhizoma Extracts On Methicillin-Resistant Staphylococcus AureusJuan Favela HernandezNoch keine Bewertungen
- Asian Journal of Pharmaceutical and Clinical ResearchDokument6 SeitenAsian Journal of Pharmaceutical and Clinical ResearchLeandro DouglasNoch keine Bewertungen
- Antibiotic Impregnated Tablets For Screening Esbl and Ampc Beta LactamasesDokument4 SeitenAntibiotic Impregnated Tablets For Screening Esbl and Ampc Beta LactamasesIOSR Journal of PharmacyNoch keine Bewertungen
- Metallo-Beta-Lactamase Producing Gram-Negative Bacterial IsolatesDokument6 SeitenMetallo-Beta-Lactamase Producing Gram-Negative Bacterial IsolatesShyam MishraNoch keine Bewertungen
- Antimicrobial Activities of Flavonoid Glycosides From Graptophyllum Antibacterial ActionDokument12 SeitenAntimicrobial Activities of Flavonoid Glycosides From Graptophyllum Antibacterial ActionAzrinurafifarsyaddilaNoch keine Bewertungen
- Staphylococcus Aureus, The Most Virulent Staphylococcus Species, Is Also The Prevalent Pathogen IsolatedDokument6 SeitenStaphylococcus Aureus, The Most Virulent Staphylococcus Species, Is Also The Prevalent Pathogen IsolatedVivi RocheNoch keine Bewertungen
- Synergistic Antibacterial Activity of Salvia Officinalis and Cichorium Intybus Extracts and AntibioticsDokument7 SeitenSynergistic Antibacterial Activity of Salvia Officinalis and Cichorium Intybus Extracts and AntibioticsSAHID IQBALNoch keine Bewertungen
- Isolation and Characterization of Actinomycetes From Soil and Evaluation of Antibacterial Activities of Actinomycetes Against PathogensDokument9 SeitenIsolation and Characterization of Actinomycetes From Soil and Evaluation of Antibacterial Activities of Actinomycetes Against PathogensTrương Tấn SangNoch keine Bewertungen
- Anti-Mycobacterial Activity of Piper Longum L. Fruit Extracts Against Multi Drug Resistant Mycobacterium SPPDokument9 SeitenAnti-Mycobacterial Activity of Piper Longum L. Fruit Extracts Against Multi Drug Resistant Mycobacterium SPPBilici EcaterinaNoch keine Bewertungen
- Bpswinter2011 0218Dokument3 SeitenBpswinter2011 0218Fahru DinNoch keine Bewertungen
- Me NTH ADokument4 SeitenMe NTH ASoumitra NathNoch keine Bewertungen
- Antimicrobial Activities of PlantsDokument190 SeitenAntimicrobial Activities of Plantsjitenmech0% (1)
- Pharmaceuticals 14 01229Dokument30 SeitenPharmaceuticals 14 01229Popusoi AnaNoch keine Bewertungen
- Phytochemical, Antimicrobial, Antioxidant, and in Vitro Cytotoxicity Evaluation of Echinops Erinaceus Kit TanDokument18 SeitenPhytochemical, Antimicrobial, Antioxidant, and in Vitro Cytotoxicity Evaluation of Echinops Erinaceus Kit Tanshrooq sweilamNoch keine Bewertungen
- HJNHNNDokument9 SeitenHJNHNNProbioticsAnywhereNoch keine Bewertungen
- Medical Microbiology & DiagnosisDokument4 SeitenMedical Microbiology & DiagnosisdianaNoch keine Bewertungen
- Phytochemical Study and Antibacterial Activity of Ethanolic and Aqueous Extracts of Barks of Myrianthus Holstii Engl. (Cecropiaceae)Dokument8 SeitenPhytochemical Study and Antibacterial Activity of Ethanolic and Aqueous Extracts of Barks of Myrianthus Holstii Engl. (Cecropiaceae)IJAR JOURNALNoch keine Bewertungen
- Efflux Pump Inhibitore of Clinically Relevant Drug Resistant BacteriaDokument45 SeitenEfflux Pump Inhibitore of Clinically Relevant Drug Resistant BacteriaJob TekakwoNoch keine Bewertungen
- Bero 2009 2 PDFDokument33 SeitenBero 2009 2 PDFRatan Deep ChauhanNoch keine Bewertungen
- Antimicrobial Efficacy of N - (3 - Chloro - (Substituted Aryl) - 4-Oxoazetidin - 1-Yl) Pyridine-4 - Carboxamides Against Resistant Bacterial Strains Obtained From Clinical IsolatesDokument8 SeitenAntimicrobial Efficacy of N - (3 - Chloro - (Substituted Aryl) - 4-Oxoazetidin - 1-Yl) Pyridine-4 - Carboxamides Against Resistant Bacterial Strains Obtained From Clinical IsolatesInternational Medical PublisherNoch keine Bewertungen
- Sambiloto 4Dokument8 SeitenSambiloto 4Radiksa AzryNoch keine Bewertungen
- High-Level Gentamicin Resistance Mediated by Aac (6 ) - Ie-Aph (2") - Ia Gene inDokument12 SeitenHigh-Level Gentamicin Resistance Mediated by Aac (6 ) - Ie-Aph (2") - Ia Gene inMouna KhazriNoch keine Bewertungen
- Article1401275147 - Shah Et AlDokument6 SeitenArticle1401275147 - Shah Et AlGustavo Gutiérrez GómezNoch keine Bewertungen
- A. Crassicauda, M. Eupeus and H. Lepturus Scorpion Venoms Initiate A Strong in Vivo Anticancer Immune Response in CT26-tumor Mice ModelDokument8 SeitenA. Crassicauda, M. Eupeus and H. Lepturus Scorpion Venoms Initiate A Strong in Vivo Anticancer Immune Response in CT26-tumor Mice ModelJuan Nicolas Perez GarzonNoch keine Bewertungen
- tmp3C58 TMPDokument9 Seitentmp3C58 TMPFrontiersNoch keine Bewertungen
- Antibacterial Effect of Cassia Fistula Extract On Pathogenic Bacteria of Veterinary ImportanceDokument5 SeitenAntibacterial Effect of Cassia Fistula Extract On Pathogenic Bacteria of Veterinary ImportanceAsif MajeedNoch keine Bewertungen
- Antifungal Drug Discovery: Something Old and Something New: PearlsDokument3 SeitenAntifungal Drug Discovery: Something Old and Something New: PearlsGilang Kasynamidt Al'hafidhNoch keine Bewertungen
- Antimicrobial Activities of Flavonoid Glycosides From Graptophyllum Grandulosum and Their Mechanism of Antibacterial ActionDokument11 SeitenAntimicrobial Activities of Flavonoid Glycosides From Graptophyllum Grandulosum and Their Mechanism of Antibacterial ActionRaquel Filgueira de Souza FerreiraNoch keine Bewertungen
- Translate Uts MikrobioDokument9 SeitenTranslate Uts MikrobioReni ArpNoch keine Bewertungen
- 1 Zarfel2013Dokument8 Seiten1 Zarfel2013luismitlvNoch keine Bewertungen
- Pathogens 11 00151 v2Dokument14 SeitenPathogens 11 00151 v2Mayang WulanNoch keine Bewertungen
- Novel Chalcones and 1,3,5 Triphenyl 2 PyrazolineDokument6 SeitenNovel Chalcones and 1,3,5 Triphenyl 2 PyrazolineMaria PappovaNoch keine Bewertungen
- He Use of Hericium Erinaceus and Trametes Versicolor Extracts in Supportive Treatment in OncologyDokument16 SeitenHe Use of Hericium Erinaceus and Trametes Versicolor Extracts in Supportive Treatment in Oncologymalvina.sekolonik911Noch keine Bewertungen
- Chebulae Fructus 1Dokument10 SeitenChebulae Fructus 1nacha nurhasanahNoch keine Bewertungen
- Contributions To The Complex Study On Antitumor Activity of Usnea BarbataDokument6 SeitenContributions To The Complex Study On Antitumor Activity of Usnea BarbataNordsci ConferenceNoch keine Bewertungen
- Immunocytotoxic Effect of Aqueous Leaf Extract of Cassia Occidentalis On Human Peripheral Blood Mononuclear Cells and NeutrophilsDokument7 SeitenImmunocytotoxic Effect of Aqueous Leaf Extract of Cassia Occidentalis On Human Peripheral Blood Mononuclear Cells and NeutrophilsUMYU Journal of Microbiology Research (UJMR)Noch keine Bewertungen
- Inhibitory and Killing Activities of Medicinal Plants Against Multiple Antibiotic-Resistant Helicobacter PyloriDokument8 SeitenInhibitory and Killing Activities of Medicinal Plants Against Multiple Antibiotic-Resistant Helicobacter PyloriNyayu_FitrianiNoch keine Bewertungen
- Anticancer Effects of Chinese Herbal Medicine, Science or Myth?Dokument9 SeitenAnticancer Effects of Chinese Herbal Medicine, Science or Myth?marcussiNoch keine Bewertungen
- Synthesis of Benzimidazolyl 134 Oxadiazo20160813 6377 1s2hcfo With Cover Page v2Dokument12 SeitenSynthesis of Benzimidazolyl 134 Oxadiazo20160813 6377 1s2hcfo With Cover Page v2Praveen T MNoch keine Bewertungen
- 060 JimenezDokument6 Seiten060 JimenezAri Puji AstutiNoch keine Bewertungen
- New Developments in The Medicinal Chemistry Targeting Drug-Resistant Infection - Part-IDokument2 SeitenNew Developments in The Medicinal Chemistry Targeting Drug-Resistant Infection - Part-IFernando CarvalhoNoch keine Bewertungen
- Research Article Piper Betle L. AgainstDokument8 SeitenResearch Article Piper Betle L. AgainstAjay BhoyeNoch keine Bewertungen
- Preliminary Screening of Bioactive Metabolites From Three Fungal Species ofDokument10 SeitenPreliminary Screening of Bioactive Metabolites From Three Fungal Species ofdhyantiNoch keine Bewertungen
- Journal of Chemical and Pharmaceutical ResearchDokument13 SeitenJournal of Chemical and Pharmaceutical ResearchSandeep GoudNoch keine Bewertungen
- PHAR Article 71695Dokument9 SeitenPHAR Article 71695Mariam DiaNoch keine Bewertungen
- Di 2017Dokument10 SeitenDi 2017V LjNoch keine Bewertungen
- Bacteriological Profile of Blood Stream Infections at A Rural Tertiary Care Teaching Hospital of Western Uttar PradeshDokument9 SeitenBacteriological Profile of Blood Stream Infections at A Rural Tertiary Care Teaching Hospital of Western Uttar PradeshHArdik NegiNoch keine Bewertungen
- Synthesis, Antitubercular Activity and Docking Study of Novel Cyclic Azole Substituted Diphenyl Ether DerivativesDokument9 SeitenSynthesis, Antitubercular Activity and Docking Study of Novel Cyclic Azole Substituted Diphenyl Ether DerivativesJafar HerizNoch keine Bewertungen
- AntileishmanialsDokument11 SeitenAntileishmanialsRICHARD MACIENTE SILVINO DA SILVANoch keine Bewertungen
- Phytochemical Screening and Antibacterial Activity of Four Cnidoscolus Species (Euphorbiaceae) Against Standard Strains and Clinical IsolatesDokument8 SeitenPhytochemical Screening and Antibacterial Activity of Four Cnidoscolus Species (Euphorbiaceae) Against Standard Strains and Clinical IsolatesÓscar AguirreNoch keine Bewertungen
- Antimicrobial Resistance Profile of Helicobacter Pylori Clinical Isolates in Duhok City, Kurdistan Region/IraqDokument4 SeitenAntimicrobial Resistance Profile of Helicobacter Pylori Clinical Isolates in Duhok City, Kurdistan Region/IraqInternational Organization of Scientific Research (IOSR)Noch keine Bewertungen
- Evaluation of A Diagnostic Flow Chart For Detection and Confirmation of Extended Spectrum B-Lactamases (ESBL) in EnterobacteriaceaeDokument11 SeitenEvaluation of A Diagnostic Flow Chart For Detection and Confirmation of Extended Spectrum B-Lactamases (ESBL) in EnterobacteriaceaeRaffaharianggaraNoch keine Bewertungen
- Life 11 00257Dokument15 SeitenLife 11 00257AzzahraNoch keine Bewertungen
- Antimicrobial Activity of Medicinal Plants Full ThesisDokument8 SeitenAntimicrobial Activity of Medicinal Plants Full Thesismaritzatysonconnecticut100% (2)
- Artigo 3 - Identification of A Diverse Synthetic Abietane Diterpenoid Library andDokument5 SeitenArtigo 3 - Identification of A Diverse Synthetic Abietane Diterpenoid Library andLaura CristóvãoNoch keine Bewertungen
- 2019-Ardisia sieboldii-ZNCDokument9 Seiten2019-Ardisia sieboldii-ZNCSuprio KamalNoch keine Bewertungen
- Ahmed 2013Dokument5 SeitenAhmed 2013sii nuriantiNoch keine Bewertungen
- JADWAL PRAKTIKUM COMPOUNDING NewDokument4 SeitenJADWAL PRAKTIKUM COMPOUNDING NewJulian FelixNoch keine Bewertungen
- Brookfield Digital Viscometer: Operating Instructions Manual NoDokument31 SeitenBrookfield Digital Viscometer: Operating Instructions Manual NoJulian FelixNoch keine Bewertungen
- SalbutamolDokument7 SeitenSalbutamolJulian FelixNoch keine Bewertungen
- Studi KasusDokument3 SeitenStudi KasusJulian FelixNoch keine Bewertungen
- Extraction, Isolation and Identification of Avonoid From Euphorbia Neriifolia LeavesDokument6 SeitenExtraction, Isolation and Identification of Avonoid From Euphorbia Neriifolia LeavesAbdurrazaqNoch keine Bewertungen
- Keep Your Pharmacy Spirit On FireDokument2 SeitenKeep Your Pharmacy Spirit On FireJulian FelixNoch keine Bewertungen
- Irv 12045Dokument13 SeitenIrv 12045Julian FelixNoch keine Bewertungen
- Molecules: New Flavonoid Glycosides FromDokument7 SeitenMolecules: New Flavonoid Glycosides FromJulian FelixNoch keine Bewertungen
- Nutrients 06 04881Dokument14 SeitenNutrients 06 04881Julian FelixNoch keine Bewertungen
- Molecules: New Flavonoid Glycosides FromDokument7 SeitenMolecules: New Flavonoid Glycosides FromJulian FelixNoch keine Bewertungen
- Biology 03 00536Dokument15 SeitenBiology 03 00536Julian FelixNoch keine Bewertungen
- Contoh Soal EAP TestDokument21 SeitenContoh Soal EAP TestEndang Frida Siahaan81% (16)
- Bioactive Constituents From The Leaves of Melastoma Malabathricum. L.Dokument8 SeitenBioactive Constituents From The Leaves of Melastoma Malabathricum. L.Julian FelixNoch keine Bewertungen
- EapDokument2 SeitenEapJulian FelixNoch keine Bewertungen
- Cover + No KatalogDokument2 SeitenCover + No KatalogMifti SyawaliNoch keine Bewertungen
- Guideline On Preparation of Site Master FilesDokument8 SeitenGuideline On Preparation of Site Master FilesIshara VithanaNoch keine Bewertungen
- 5 Vol3 Issue3 MS 15175Dokument8 Seiten5 Vol3 Issue3 MS 15175kanna_dhasan25581Noch keine Bewertungen
- Seminar On Coarse Dispersion SDokument17 SeitenSeminar On Coarse Dispersion SSaimanideepak Vallamsetti0% (1)
- Biological Properties of Lemongrass An OverviewDokument1 SeiteBiological Properties of Lemongrass An OverviewLilia RotariNoch keine Bewertungen
- Philip Marmina CVDokument3 SeitenPhilip Marmina CVPhilipMarminaNoch keine Bewertungen
- 7a. Antibacterial AgentsDokument32 Seiten7a. Antibacterial AgentsNiala AlmarioNoch keine Bewertungen
- Tutorial 7: QuestionsDokument3 SeitenTutorial 7: QuestionsKouser SultanaNoch keine Bewertungen
- Determination and Validation of Uv Spectrophotometric Method For Estimation of Bicalutamide TabletDokument5 SeitenDetermination and Validation of Uv Spectrophotometric Method For Estimation of Bicalutamide TabletGembong Van BeethovenNoch keine Bewertungen
- Irrational Use of Drugs - 2Dokument17 SeitenIrrational Use of Drugs - 2Umair MazharNoch keine Bewertungen
- RMO Handbook AussieDokument48 SeitenRMO Handbook Aussienvrtm43Noch keine Bewertungen
- CP Diare Persisten Feb 2017Dokument4 SeitenCP Diare Persisten Feb 2017Prisscy TilisNoch keine Bewertungen
- Klasifikasi ADRDokument3 SeitenKlasifikasi ADRAstari PuspaningdyahNoch keine Bewertungen
- Microencapsulation SummaryDokument48 SeitenMicroencapsulation SummaryDullah Zungu100% (2)
- BethanecholDokument3 SeitenBethanecholI.m. DanielNoch keine Bewertungen
- Internship Report MAHADDokument13 SeitenInternship Report MAHADMahad aslam QureshiNoch keine Bewertungen
- Review Rasa SindhuraDokument9 SeitenReview Rasa SindhuraNCSASTRONoch keine Bewertungen
- LMWH QML 06Dokument7 SeitenLMWH QML 06pd7qmlNoch keine Bewertungen
- Daftar Nama DistributorDokument12 SeitenDaftar Nama DistributorAny Moneta SariNoch keine Bewertungen
- Catapres (Clonidine)Dokument2 SeitenCatapres (Clonidine)Adrianne BazoNoch keine Bewertungen
- 4-Farmakologi Obat Penyakit MataDokument30 Seiten4-Farmakologi Obat Penyakit MataDensy Nurtita FitrianiNoch keine Bewertungen
- M/s. Lupin Limited vs. Competition Commission of India, OthersDokument3 SeitenM/s. Lupin Limited vs. Competition Commission of India, OthersVijay KandpalNoch keine Bewertungen
- Effective Treatment With Hormeel S Dosage RecommendationsDokument2 SeitenEffective Treatment With Hormeel S Dosage Recommendationssurfer_Noch keine Bewertungen
- MDS3 Ch45 HospitalPharmacyMgmt Nov2011Dokument17 SeitenMDS3 Ch45 HospitalPharmacyMgmt Nov2011Andre SamsungNoch keine Bewertungen
- Secundum Artem: Compounding For Otic DisordersDokument0 SeitenSecundum Artem: Compounding For Otic Disordersdebieyolanda_7180456Noch keine Bewertungen
- Drug Calculations WorkbookDokument32 SeitenDrug Calculations Workbookvhon100% (1)
- Presentation GMP and CGMP ConsiderationsDokument42 SeitenPresentation GMP and CGMP ConsiderationsMimi SlifiNoch keine Bewertungen
- MBA Projaet-Concept Pharmaceuticals LimitedDokument93 SeitenMBA Projaet-Concept Pharmaceuticals LimitedMechanical PrasadNoch keine Bewertungen
- Daftar ObatDokument11 SeitenDaftar Obataudyta maharani putriNoch keine Bewertungen
- Pharma Executive SummaryDokument35 SeitenPharma Executive SummaryUzair Ul GhaniNoch keine Bewertungen
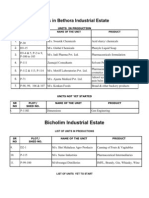
- Goa Industrial Estates 1Dokument11 SeitenGoa Industrial Estates 1Vishal SalveNoch keine Bewertungen