Beruflich Dokumente
Kultur Dokumente
Autoimmunity Reviews: Elena Gianchecchi, Alessandra Fierabracci
Hochgeladen von
LalaTaOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Autoimmunity Reviews: Elena Gianchecchi, Alessandra Fierabracci
Hochgeladen von
LalaTaCopyright:
Verfügbare Formate
Autoimmunity Reviews 14 (2015) 971983
Contents lists available at ScienceDirect
Autoimmunity Reviews
journal homepage: www.elsevier.com/locate/autrev
Review
Gene/environment interactions in the pathogenesis of autoimmunity:
New insights on the role of Toll-like receptors
Elena Gianchecchi a,b, Alessandra Fierabracci a,
a
b
Immunology and Pharmacotherapy Area, Bambino Ges Children's Hospital, IRCCS, Rome, Italy
Vismederi Srl, Siena, Italy
a r t i c l e
i n f o
Article history:
Received 1 July 2015
Accepted 8 July 2015
Available online 13 July 2015
Keywords:
Autoimmunity
Etiopathogenesis
Toll-like receptors
TLR signaling pathway
Candidate autoimmune genes
Preventiontreatment
a b s t r a c t
Autoimmune disorders are increasing worldwide. Although their pathogenesis has not been elucidated yet, a
complex interaction of genetic and environmental factors is involved in their onset.
Toll-like receptors (TLRs) represent a family of pattern recognition receptors involved in the recognition and in
the defense of the host from invading microorganisms. They sense a wide range of pathogen associated molecular
patterns (PAMPs) deriving from metabolic pathways selective of bacterial, viral, fungal and protozoan microorganisms. TLR activation plays a critical role in the activation of the downstream signaling pathway by interacting
and recruiting several adaptor molecules. Although TLRs are involved in the protection of the host, several studies
suggest that, in certain conditions, they play a critical role in the pathogenesis of autoimmune diseases. We
review the most recent advances showing a correlation between some single nucleotide polymorphisms or
copy number variations in TLR genes or in adaptor molecules involved in TLR signaling and the onset of several
autoimmune conditions, such as Type I diabetes, autoimmune polyendocrinopathy candidiasis-ectodermal
dystrophy, rheumatoid arthritis, systemic lupus erythematosus and systemic sclerosis. In light of the foregoing
we nally propose that molecules involved in TLR pathway may represent the targets for novel therapeutic
treatments in order to stop autoimmune processes.
2015 Elsevier B.V. All rights reserved.
Contents
1.
2.
3.
4.
5.
6.
7.
8.
Toll-like receptors . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
TLR signaling mediated through the MyD88-dependent pathway . . . . . . . . . . . .
MyD88-independent signaling pathway induced by TLR3 and TLR4 . . . . . . . . . . .
The TLR-independent cytosolic pattern-recognition receptors (PRRs) for nucleic acids . .
TLR ligands: bacterial, viral, fungal and protozoan PAMPs . . . . . . . . . . . . . . .
The negative regulation of TLR signaling pathway . . . . . . . . . . . . . . . . . . .
The possible involvement of nucleic acid PAMPs and endogenous ligands in autoimmunity
The involvement of TLRs in autoimmune disease onset . . . . . . . . . . . . . . . .
8.1.
Type I diabetes . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
8.2.
Autoimmune polyendocrinopathy candidiasis ectodermal dystrophy . . . . . . .
8.3.
Rheumatoid arthritis . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
8.4.
Systemic lupus erythematosus . . . . . . . . . . . . . . . . . . . . . . . .
8.5.
Systemic sclerosis . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
8.6.
Behcet's disease . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
8.7.
Crohn's disease and ulcerative colitis . . . . . . . . . . . . . . . . . . . . .
8.8.
Multiple sclerosis . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
8.9.
Vitiligo . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
8.10.
Myasthenia gravis . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
972
972
972
973
973
974
974
975
975
976
976
977
978
978
979
979
979
979
Corresponding author at: Immunology and Pharmacotherapy Area, Bambino Ges Children's Hospital, IRCCS, Viale S. Paolo 15, 00146 Rome, Italy. Tel.: +39 06 6859 2656; fax +39 06
6859 2904.
E-mail address: alessandra.erabracci@opbg.net (A. Fierabracci).
http://dx.doi.org/10.1016/j.autrev.2015.07.006
1568-9972/ 2015 Elsevier B.V. All rights reserved.
972
E. Gianchecchi, A. Fierabracci / Autoimmunity Reviews 14 (2015) 971983
9.
Conclusive remarks . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
Acknowledgments . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
References . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
1. Toll-like receptors
TLRs represent a family of pattern recognition receptors [1] which
are type I integral trans-membrane glycoproteins [2,3]. They show a
trimodular structure [3], with an extracellular N-terminal domain and
an intracellular C-terminal region. The rst is constituted by about
1628 leucine rich repeats (LRRs) and has the function to recognize
PAMPs [3], whereas the second, also called Toll/IL-1 receptor (TIR)
domain, is similar to the cytoplasmic region of the interleukin-1 receptor
(IL-1R) [47]. TIR domain has a critical role for TLR function (vide infra)
[3].
Toll was the rst receptor identied in Drosophila, where it was involved in the dorsal ventral patterning in developing embryos [8].
Since the observation performed by the group of Hoffmann [9] that
ies mutant for Toll were characterized by an increased susceptibility
to fungal infections, several homologues of Toll receptor were identied
in mammals and called TLRs [10].
In total 13 and 11 TLRs were identied in mice and in humans, respectively [2]. They are evolutionary conserved [1], playing an essential
role in the recognition of PAMPs [2] from viruses, fungi, protozoan
parasites and bacteria (vide infra) [2]. Different PAMPs are recognized
by specic TLRs [5].
Several immune cells, including B lymphocytes, selective populations of T cells, dendritic cells (DCs) and macrophages [5,11] as well as
non-immune cells such as epithelial cells and broblasts express TLRs
[5]. TLR expression can quickly change in the presence of cytokines,
pathogens and environmental factors [5].
It is possible to distinguish TLRs on the basis of their intracellular
localization. TLR1, TLR2, TLR4, TLR5 and TLR6 can be observed at the cell
membrane, while TLR3, TLR7, TLR8 and TLR9 into cell compartments,
like endosomes. TLRs characterized by an intracellular localization recognize principally bacterial and viral nucleic acids, which are released and
enter in contact with TLRs after being endocytosed and degraded in late
endosomes or lysosomes [5]. It has been hypothesized that TLR intracellular presence plays an essential role for the discrimination between
self-DNA and viral DNA, thus avoiding the development of autoimmune
conditions (vide infra) [12].
After the recognition of PAMPs by TLRs, type I interferon (type I IFN),
chemokines, inammatory cytokines and co-stimulatory molecules are
released by the immune system of the host [47]. More in detail, TIR domain plays a critical role in the activation of the downstream signaling
pathway [3]. The function of TIR domain was identied in C3H/HeJ
mouse strain, characterized by a point mutation which caused an
amino acid change to histidine at position 712 of the cytoplasmic proline residue [13,14]. This amino acid substitution induced a dominant
negative effect on the signaling mediated by TLRs [14,15]. TIR domain
activates the downstream signaling pathway through the interaction
and recruitment of several adaptor molecules [3] such as myeloid
differentiation primary-response protein 88 (MyD88), TIR domaincontaining adapter protein (TIRAP) (also dened as MyD88 adaptorlike (MAL)), TIR domain-containing adapter protein inducing IFN-
(TRIF) (also known as TICAM1) and TRIF-related adapter molecule
(TRAM) (also dened as TICAM2). This recruitment occurs through
TIRTIR interactions [16]. Depending on which molecular adaptor is
recruited, a different signaling pathway is activated; in fact whereas
some pathways are similar among TLRs, others are specically activated
by only one TLR (vide infra) [17]. More in detail the recruitment of
MyD88 occurs for all TLRs, except for TLR3. Both TLR3 and TLR4 promote
the recruitment of TRIF adaptor; however while the rst can initiate
only the TRIF-dependent pathway, TLR4 can activate also a MyD88-
980
980
980
dependent signaling [3]. The adaptor TIRAP is recruited in the signaling
promoted by TLR1, TLR2, TLR4 and TLR6 allowing, through its TIR
domain, the recruitment of MyD88 [3]. The fundamental role played
by TIRAP in the interaction with MyD88 has been demonstrated in
TIRAP-decient mice which showed TLR2- and TLR4-defective signaling
pathways similar to those observed in mice decient for MyD88.
Accordingly MyD88/TIRAP-decient mice did not show any additional
defect as compared with mice showing a single deciency affecting
these adaptors [17]. The TLR7/9 pathway is MyD88-dependent and
does not require TIRAP [17].
2. TLR signaling mediated through the MyD88-dependent pathway
The MyD88-dependent pathway characterizes the signaling induced
by all TLRs, whereas only TLR3 and TLR4 show a pathway independent
from MyD88 (vide infra) (Fig. 1) [10,12].
MyD88 adaptor shows the presence of a death domain in the
N-terminal region, whereas a TIR domain is localized in the C-terminal.
MyD88 interacts with TLRs in their TIR domain and plays a critical function for the induction of inammation by TLR signaling [10,17]. As regard
it has been demonstrated that MyD88 knockout mice did not show
any response when stimulated with imidazoquinoline (a TLR7 ligand)
or cytosine-guanine dinucleotides (CpG) DNA (a TLR9 ligand) [1820],
and interleukin-6 (IL-6) production after stimulation with bacterial agellin (a TLR5 ligand) [21]. Furthermore MyD88-decient mice did not show
any inammatory molecule production, the proliferation of B lymphocytes or endotoxin shock upon lipopolysaccharide (LPS) stimulation [10].
After TLR activation, MyD88 allows the recruitment of IL-1 receptorassociated kinase (IRAK) molecule to TLRs by interacting with the death
domains of the two molecules [10]. Four members belonging to IRAK
family have been identied (IRAK-1, IRAK-2, IRAK-4 and IRAK-M)
[22]. Among these, IRAK-4 plays the most important role in the signaling pathway mediated by MyD88 (Fig. 1) [12,17]. The phosphorylation
of IRAK causes its dissociation from MyD88 and the subsequent association with TRAF6, which constitutes an E3 ligase and is a member of the
TRAF family [12]. TRAF6 is involved in the activation of TGF--activated
kinase 1 (TAK1) [23] and the canonical IB kinases (IKKs) constituted by
IKK and IKK. IKKs cause the phosphorylation of IB protein and
its follow-up degradation by a proteasome-dependent pathway
permitting nuclear factor B (NF-B) translocation into the nucleus
and activation (reviewed (rev.) in [17]).
MyD88 can also promote the activation of the mitogen-activated
protein kinases (MAPKs) p38, extracellular signal-regulated kinase 1/2
(ERK1/2) and c-Jun N-terminal kinases (JNKs) [12,17].
As results of the activation of these TLR signaling pathways, several
inammatory cytokine genes are expressed [17]. The critical role played
by MyD88 in the activation of inammation has been demonstrated
both in mice decient for MyD88 (vide supra) and in the presence of a
variant form of MyD88 known as MyD88s [10]. MyD88s represents a
spliced variant which is characterized by the loss of the intermediate
domain and thus could induce a negative regulation of the inammatory process upon LPS stimulation [24,25].
3. MyD88-independent signaling pathway induced by TLR3 and TLR4
The stimulation of TLR3 and TLR4 can induce the activation of a
MyD88-independent signaling pathway designed as TRIF-dependent
pathway [12], through the association of TLR with TRIF molecule
which occurs differently depending on which TLR is activated. In fact
whereas TLR3 directly associates with TRIF, TLR4 needs the involvement
E. Gianchecchi, A. Fierabracci / Autoimmunity Reviews 14 (2015) 971983
973
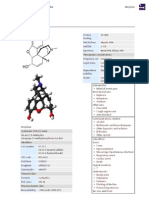
Fig. 1. TLR signaling cascade. The signaling pathway downstream of TLR1, TLR2, TLR3, TLR4, TLR6, TLR7 and TLR9 are represented as examples. The activation of TLR2/1, TLR2/6 and TLR4 on
the cell membrane induces MyD88 and TIRAP recruitment through TIR-TIR interactions. MyD88 leads to the recruitment of IRAK molecules. IRAK-4 has the most important role in MyD88dependent signaling pathway. IRAK-4 is phosphorylated causing its dissociation from MyD88. Then IRAK-4 associates with TRAF6. The latter can activate IRF5 or TAK1. TAK1 can induce
MAPK or IKKb activation. IKKb is involved in the nuclear translocation and activation of NF-kB. A MyD88-independent signaling cascade, called TRIF-dependent signaling pathway, is
activated by TLR3 (localized in endosomes) and TLR4. TLR3 binds directly TRIF, whereas TLR4 requires the involvement of the further adaptor TRAM to interact with TRIF. TLR7/9,
whose localization has been described in endosomes, activate the signaling pathway through the recruitment of MyD88. The black arrows represent TLR signaling pathway, whereas
the red arrows indicate the effects of TLR signaling activation on DNA transcription. The black thicker lines represent the negative regulation of TLR signaling pathway. Figure is adapted
from Ref. [12] and [17].
of TRAM adaptor (Fig. 1) [26]. TRIF can promote three different signaling
pathways [17].
More in detail it can lead, through the involvement of IB kinases
IKK and TANK-binding kinase 1 (TBK1), to IFN regulatory factor 3
(IRF-3) phophorylation [17] at the C-terminal region [12] and IRF-7
activation [3,17]. IRF-3 and IRF-7 translocate into the nucleus, promoting
the expression of genes, such as type I IFN, and especially of IFN- [17].
Moreover TRIF can induce NF-B and MAPK activation through the
direct interaction with TRAF6 [17] or, through the presence of a RIP
homotypic interaction motif, can activate NF-B by recruiting receptorinteracting protein 1 (RIP-1) [3,27].
In human cell lines it has been identied a further adaptor which is
characterized by the presence of the TIR domain and is called sterile
and armadillo motifs (SARM). SARM is able to inhibit the signaling
pathway induced by TRIF [9], but its role has not been yet identied in
mammals [17,28]. In nematodes its homolog TIR-1 is fundamental for
TLR-independent innate immunity [29].
Upon TLR4 stimulation, the deciency of TRIF or MyD88 is responsible for a defective NF-B activation; while TRIF deciency causes an
impaired late activation, deciency of MyD88 induces a defective early
activation [30].
4. The TLR-independent cytosolic pattern-recognition receptors
(PRRs) for nucleic acids
In addition to the TLR signaling pathways previously described, recent studies have demonstrated a non-TLR system for the recognition
of nucleic acids [31], known as the TLR-independent cytosolic patternrecognition receptors (PRRs). This was identied for the rst time for
the recognition of double-stranded RNA (dsRNA) [32]. In fact in addition
to TLR3, dsRNA is recognized by two cytosolic molecules, the retinoic
acid-inducible gene I (RIG-I) and the melanoma differentiationassociated protein 5 (Mda-5) (Fig. 1) [17], recently implicated in the
pathogenesis of T1D [33]. Unknown cytosolic molecules (represented
as X in Fig. 1) are involved in the recognition of dsDNA [17,34]. In
both cases the activation of IFN- stimulator 1 (IPS-1)-dependent
cytosolic signaling pathway occurs, leading to the synthesis of type I
IFNs and inammatory cytokines [17].
5. TLR ligands: bacterial, viral, fungal and protozoan PAMPs
PAMPs are products of metabolic pathways selective of a group of
microorganisms [17]; being necessary for their survival, PAMPs are
highly conserved among pathogens, in contrast to the heterogeneity
of viral proteins, whose structure is rapidly modied to escape recognition by the host immune system in mammals [10,17].
Several elements of the bacterial cell wall are recognized by TLRs.
More in detail TLR4 and TLR2 sense LPS, constituting the wall of
Gram-negative bacteria, and peptidoglycan (PG), forming a thick layer
in the cell wall of Gram-positive bacteria, respectively. Furthermore
TLR2 recognizes lipoarabinomannan (LAM) of mycobacteria, and both
TLR2/6 or TLR2/1 sense diacyl or triacyl lipopeptides of mycoplasma,
mycobacteria and bacteria [3].
Bacterial proteins, such as agellin, represents PAMPs. Flagellin is
the principal constituent of bacterial agella; the constant domain D1,
relatively conserved among different species [5], is recognized by
TLR5. Furthermore unmethylated CpG DNA of bacteria constitutes an
immunostimulant sensed by TLR9 which resides in endosomes [3].
974
E. Gianchecchi, A. Fierabracci / Autoimmunity Reviews 14 (2015) 971983
Since TLR9 is present in this intracellular compartment, the recognition
by TLR9 occurs after the transport of bacterial DNA into endosome. Here
dsDNA is degraded into single stranded regions containing CpG motifs
through reducing and acidic conditions. In humans TLR9 expression is
limited to B cells and plasmacytoid dendritic cells (pDCs) [5]. Selective
components, not yet identied, from uropathogenic bacteria are
recognized by murine TLR11 [35].
In agreement with the important role played by TLR2 in recognizing
PAMPs, it has been demonstrated that TLR2-decient mice (TLR2/)
were more susceptible to Streptococcus pneumoniae and Staphylococcus
aureus infections [36,37]. After the recognition of bacterial PAMPs by
TLRs, the release of inammatory cytokines, and in particular conditions
of type I IFNs, is induced [3].
Among viral PAMPs recognized by TLRs, there are envelope proteins
like those of respiratory syncytial virus (RSV) and the hemagglutinin
protein characterizing Measles virus recognized by TLR4 and TLR2, respectively. Also nucleic acids of viruses constitute PAMPs which are
identied by TLR3, TLR7, TLR8 and TLR9. Their DNA, such as the bacterial
DNA, presents DNA motifs characterized by unmethylated CpG DNA.
This last contains oligonucleotides that are able to strongly induce
TNF-I from pDCs [3]. TLR7 and TLR8, whose genes are characterized by
elevated homology, reside within the endosomal membrane. In mice
TLR8 seems to be nonfunctional [5]. More in detail mouse TLR7 and
human TLR8 recognize both viral and self guanosine and/or uridinerich single-stranded RNA (ssRNA) [2,38] and synthetic antiviral molecules [38], like Imiquimod and R848 [3], whereas dsRNA produced by
viruses during replication constitutes the ligand of TLR3 [3,17]. Accordingly TLR3 is able to sense polyinosine-deoxycytidylic acid (poly I:C)
which is a synthetic analog of dsRNA and constitutes also a vaccine adjuvant (vide infra) [3]. In pDCs or in natural interferon- producing cells
(NIPCs), characterized by the release of high levels of IFN- during viral
infections [39], viral PAMPs are recognized mainly by TLR7 [40]. Also
DCs and broblasts secreted type I IFN in response to ssRNA viruses, but
this occurred in a signaling pathway independent from TLR7 [41]. Upon
herpes simplex virus 1 and 2 (HSV-1 and HSV-2) infections IFN- release
induced by TLR9 activation is mediated principally by pDCs [42].
Many fungal PAMPs activate TLRs [5], such as glucuronoxylomannans
which is sensed by TLR4 and cluster of differentiation 14 (CD14),
-glucans and phospholipomannans recognized by TLR2. Accordingly
with the critical role played by MyD88 in TLR signaling pathway,
MyD88-deciency caused a higher susceptibility to develop fungal
infections in mice [3].
Regarding protozoan components recognized by TLRs, TLR2 sense
lipophosphoglycan (LPG) of Leishmania species and unsaturated
alkylacylglycerol of Trypanosoma species, whereas both TLR2 and
TLR4 sense glycosylphosphatidylinositol anchors (GPI-anchors) and
glycoinositolphospholipids (GIPLs) of Plasmodium (P.) falciparum,
Toxoplasma (T.) gondii and Trypanosoma. Furthermore TLR9 recognizes
Trypanosoma species' genomic DNA [3,43]. The human TLR11 is characterized by the presence of a stop codon in the gene which renders it
nonfunctional, whereas the murine TLR11 recognizes a prolin-like
molecule from T. gondii. It has been hypothesized that more than one
TLR could sense PAMPs from different protozoan parasites, since mice
decient for only one TLR did not show defective responses to live
protozoan parasites, whereas MyD88 deciency caused a more general
defect in TLR signaling [5]. In fact the deciency of MyD88 inuenced
protozoa infections in mice, inducing a defective synthesis of proinammatory cytokines associated with an increased parasitemia and
mortality [5,44].
6. The negative regulation of TLR signaling pathway
A strict negative regulation aimed to limit the immune process and
inammation characterizes TLR signaling pathway through several
molecules with different activities (Fig. 1). Some molecules downregulate the expression of TLRs, such as TLR4 and TLR9 whose degradation is
induced by the E3 ubiquitin ligase Triad3A through a proteasomedependent pathway (rev. in [17]). Other molecules, like TRAF4, IRF4
and STL2, represent negative regulators of TLR signaling by sequestrating molecules involved in this pathway [12,45]. TRAF4 prevents TRAF6
recruitment to the adapter complex, although other independent
mechanisms, including -arrestins [46] and the intracellular ubiquitinediting protein A20 [12,47], are able to negatively regulate TRAF6.
IRF4 and STL2 have the role to bind MyD88 [12]. IRF4 expression is
increased after TLR activation [12] and associated with MyD88 [48].
This binding occurs in the same region of IRF5 and prevents IRF5 recruitment reducing the IRF5-dependent inammatory process. ST2L is a
member of IL-1 receptor family and, through its binding to MyD88
and TIRAP, does not allow their recruitment to TLR4 [12]. Accordingly,
IRF4- or ST2L-decient mice were both characterized by a higher
production of inammatory cytokines, associated with hyper-activation
of MAPKs and NF-kB (rev. in [12]), and with an altered induction of LPS
tolerance in case of ST2L deciency [49].
Some molecules can degrade target proteins [12], such as IRF3
whose phosphorylation at Ser339 promotes its ubiquitination and
degradation by proteasome in order to limit IFN responses [50], or the
caspase 8-dependent cleavage of TRAF1 induced by TRIF. This mechanism causes the release of a fragment of TRAF1 with the ability to inhibit
the TRIF-dependent activation of NF-kB and IRF3 [51]. After TLR2 and
TLR4 activation, the downstream signaling pathway is negatively regulated through the ubiquitination and degradation of TIRAP promoted by
the E3 ligase suppressor of cytokine signaling-1 (SOCS1) [52].
At last some molecules inhibit the transcription of gene targets [12],
like IL-6 and IL-12. The access to the promoter region of these genes is
limited for NF-kB and transcription factor activator protein 1 (AP-1)
through the activity of histone deacetylases, recruited by activating
transcription factor 3 (ATF3), which alters chromatine structure [53].
7. The possible involvement of nucleic acid PAMPs and endogenous
ligands in autoimmunity
The involvement of microbial PAMPs and endogenous ligands in autoimmunity has been hypothesized through the activation of TLR and/or
their increased expression acting in synergy with the formation of
autoantigen-autoantibody immune complexes (rev. in [2]). Necrotic
cells can induce danger signal and promote inammation by activating
TLR4. This activation could be responsible for autoimmune responses
[54]. Furthermore TLR4 can bind other endogenous ligands released
from damaged cells, including several extracellular matrix components
(ECM), such as hyaluronic acid oligosaccharides and bronectin extra
domain A, and brinogen which is able to promote the synthesis of
chemokines by macrophages. Mammals present unmethylated DNA at
a very lower level in respect to viruses or bacteria and this may prevent
autoimmune responses to self-antigens [54].
Also the abnormal internalization and transport of dsDNA fragments
from necrotic cells into endosomes could induce autoimmune responses
after their binding to TLR3 [54].
Furthermore a correlation between TLRs and endogenous dangerassociated molecular patterns, like advanced glycation end products
has been hypothesized. These can be sensed by PPRs that show the
same ligands of TLRs and activate the same intracellular pathway [55].
TLR agonists, such as poly I:C, constitute also vaccine adjuvants
whose aim is the induction of a stronger immune response towards
the antigen contained in the vaccine and thus they confer a higher protection. Although vaccine adjuvants have been supposed to be implied
in the onset of autoimmune disorders, through the activation of several
endosomal or surface TLRs, no convincing data support the presence of a
correlation between vaccine adjuvants and autoimmunity [56].
However the host has some mechanisms that permit to avoid
autoimmunity; among these, different cell compartments in which
TLRs recognize PAMPs and diverse levels of TLR expression in the various intracellular structures. In fact the recognition of proteins and lipids
E. Gianchecchi, A. Fierabracci / Autoimmunity Reviews 14 (2015) 971983
occurs on the cell membrane, whereas nucleic acids are recognized in
endosomes and for this reason the expression of TLR7 is very low in
cells having high activity of phagocytosis. The recognition of self nucleic
acids is avoided by the endosomal expression of TLR7 and TLR9 [57], as
demonstrated by the fact that chimeric TLR9 localized to the cell
membrane was able to respond to CpG DNA [5].
Moreover the DNA and RNA of the host have specic characteristics
in order to prevent autoimmunity (rev. in [17]). More in detail, although
also in vertebrates DNA is characterized by the methylation of CpG nucleotides, it shows a reduced frequency; furthermore there are specic
sequences, identied also in the telomere [2], able to inhibit the signaling through TLR9 [2,58]. RNA of vertebrates differs from bacterial RNA
for the presence of many modied nucleotides with a reduced ability
to activate DCs in respect to the RNA of bacteria [59]. Another
mechanism that prevents the autoimmune response is the conned
expression of nucleic acid-recognizing TLRs to specic cell types, such
as pDCs that express TLR7 and TLR9, but not TLR3. The dual activation
of both TCR and B cell receptor (BCR) is essential for B lymphocyte
activation and thus TLR signaling, but under certain conditions, this
could play a critical role in the pathogenesis of autoimmune disorders
[2,17,60], including systemic lupus erythematosus (SLE). This disorder
is characterized by the presence of nuclear debris due to the impaired
clearance of apoptotic cells that can represent self-antigens able to
bind BCRs, induce TLR9 expression and activate both TLR9 and B
lymphocytes with the subsequent production of autoantibodies [61].
8. The involvement of TLRs in autoimmune disease onset
Increasing evidence has demonstrated the correlation between the
presence of altered TLR expression, some single nucleotide polymorphisms (SNPs) or copy number variations (CNV) in TLR genes or in
molecules involved in TLR signaling and the development of several
autoimmune conditions including type I diabetes (T1D) [6264],
autoimmune polyendocrinopathy candidiasis-ectodermal dystrophy
(APECED) [65], rheumatoid arthritis (RA) [6670], SLE [71,72], systemic
sclerosis (SSc) [7376], Behcet's disease (BD) [77,78], Crohn's disease
(CD), ulcerative colitis (UC) [7981], multiple sclerosis (MS) [82,83],
vitiligo [84] and myasthenia gravis (MG) [85,86] (Table 1).
8.1. Type I diabetes
Type I diabetes (T1D) represents an organ specic autoimmune
disorder in which pancreatic cells of the islet of Langherans secerning
insulin are selectively destroyed by T-helper 1 (Th1) lymphocytes
[8789]. These cells begin the inltration of the pancreas and, through
the release of cytokines, support cytotoxic T lymphocytes (Tc)
which are responsible for the progressive destruction of cells [62].
Although the etiology must be yet elucidated, a combination of environmental, genetic and stochastic factors contributes to its pathogenesis
[87,88,90]. The role of TLRs in T1D onset has been analyzed in several
animal models. C57BL/6 mice co-treated with TLR3 agonist and insulin
developed insulitis [91]. Furthermore TLR3 and TLR7 engagement
converted -cell autoreactivity into overt autoimmune disease by upregulating major histocompatibility complex (MHC) class I molecules
on murine pancreatic cells [92]. TLR2 activation in APCs contributed
to T1D onset in non-obese diabetic (NOD) mice by inducing -cell
death [93]. In addition TLR activation induced by Kilham rat virus
(KRV) infection promoted autoimmune diabetes in bio-breeding
diabetes resistant (BBDR) rats [94]. MyD88 represents another critical
factor involved in T1D pathogenesis, as MyD88/ NOD mice shows a
complete prevention from the disease [95,96].
Different expression of several TLRs has been described in T1D
subjects as compared to healthy individuals. The analysis of TLR9
mRNA expression has been performed on 59 long-term (LT) T1 patients,
33 new-onset (NO) T1D patients, 19 subjects at risk (AT) for T1D and 70
controls [97]. TLR9 expression was signicantly reduced in LT T1D
975
patients compared to healthy controls, whereas it was increased in the
AT group than in controls. No differences have been observed in the
NO group [97]. The group of Meyers [98] examined whether altered
TLR signaling was involved in the rst stages of T1D. They found an
increased frequency of IL-1-expressing monocytes and a reduction in
mDCs expressing IL-6 in newly diagnosed T1D patients than nondiabetic subjects. In a following study Alkanani and colleagues [99]
tested TLR-induced IL-6 and IL-1 release by monocytes and mDCs
from genetically susceptible subjects positive for islet autoantibodies
and thus characterized by a higher risk to develop T1D. They reported
a slight increase of mDCs, pDCs and monocytes in seropositive individuals for autoantibodies than seronegative subjects, although this difference was not statistically signicant. They found also a dysregulation of
TLR-induced IL-6 and IL-1 responses in freshly isolated mDCs and
monocytes from seropositive individuals compared with autoantibodynegative subjects. It has been hypothesized that these immunological abnormalities observed in at-risk individuals before T1D onset could be
linked with the early disease mechanisms by affecting the balance between proinammatory and regulatory mechanisms in the peripheral
blood and/or pancreatic islet -cells [99]. This alteration may induce
islet inammation and up-regulation of T cells recognizing pancreatic islets [100]. We have recently observed [101] that T1D subjects harboring
the protein tyrosine phosphatase non-receptor type 22 (PTPN22)
C1858T SNP, which constitutes a genetic variant highly correlated with
the onset of several autoimmune conditions including T1D [90], showed
an enhanced TLR response upon stimulation with CpG that led to altered
B cell phenotype composition. Increasing evidence supports the hypothesis that activation of TLRs, including TLR9, could promote autoimmune
conditions, and infections may play a critical role in triggering disease
onset [101].
Further studies have described the presence of an altered TLR expression not only in T1D subjects, but also in their rst-degree relatives. The
whole-genome expression prole of peripheral blood mononuclear cells
(PBMCs) isolated from 9 T1D patients, their 10 rst-degree relatives and
10 healthy controls has been analyzed by using the human high-density
expression microarray chip [62]. T1D subjects showed a signicant
different expression of 9 genes with respect to controls. First-degree relatives of T1D patients, independently by the presence or not of autoantibodies, showed up-regulation of TLR2, TLR6 and TIRAP in respect with
healthy controls. This observation supports the idea that autoantibodynegative healthy relatives showed however a different regulation of
several immune-related signaling pathways [62], accordingly with the
presence of proinammatory islet-selective T cell responses observed
in these subjects by the group of de Marquesini [102].
Devaraj and colleagues [103] described a signicant increase of TLR2
and TLR4 ligands in T1D patients, supporting the role played by the
proinammatory environment in T1D onset. Regarding the association
between T1D and the presence of SNPs in molecules involved in TLR signaling, the study conducted by the group of Castiblanco [104] on T1D
subjects from a Colombian population reported no association
between the TIRAP (MAL) functional polymorphism S180L and T1D.
T1D was associated with TLR2 SNP (rs3804100) in the Norwegian
and Korean populations, but this correlation was not observed in the
Spanish population (rev. in [64]). The group of Assmann investigated
whether TLR3 (rs11721827, rs13126816, rs5743313, rs7668666 and
rs3775291) SNPs were involved in T1D onset [105]. 449 T1D patients
and in 507 nondiabetic subjects were analyzed. TLR3 (rs3775291) and
(rs13126816) SNPs were associated with risk for T1D. Furthermore an
association between an early age at diagnosis and poor glycemic control
and (rs5743313) and (rs117221827) SNPs was described [105]. Recently 28 SNPs in TLR1, TLR2, TLR3, TLR4, TLR5, TLR6, TLR8 and TLR9, many of
those even not included in previous genome wide association studies
(GWAS), were genotyped in 429 Chinese Han T1D patients and 300
healthy controls [64]. The analysis demonstrated for the rst time the
association of T1D with TLR1 ((rs5743612, -626) and (rs4833095, 1017)) and TLR6 (rs3775073, -1329) SNPs. Conversely, in the Caucasian
976
E. Gianchecchi, A. Fierabracci / Autoimmunity Reviews 14 (2015) 971983
T1D population TLR1-626 SNP was not analyzed in GWAS, whereas
TLR1-1017 and TLR6-1329 SNPs did not show any correlation with the
pathology [64]. It has been hypothesized that this discrepancy between
the two studies could be due to different ethnicity. Further investigations on other populations could elucidate the putative association between TLR SNPs and T1D onset [64].
Since in children at risk for T1D IFN-I expression has been reported
before the onset of islet autoimmunity and moreover recent studies
have strongly associated T1D with RNA virus infection (rev. in [33]),
Lincez and colleagues [33] have evaluated the role of MDA5, encoded
by T1D risk gene interferon induced with helicase C domain 1 (IH1).
This gene selectively recognizes dsRNA virus intermediates. They demonstrated that a reduced expression of IH1 protected NOD mice from
spontaneous and virus-mediated T1D. Mice heterozygous for the Ih1
gene showed a lower MDA5 protein expression, promoting the
expansion of regulatory T cells (Tregs) with a concomitant reduction
of effector CD4+ T cells in the pancreas [33].
cells; its loss caused both an altered negative selection of self-directed
T cells in the thymus [65] and the presence of autoantibodies in the peripheral blood. Moreover several tissues were inltrated by autoreactive
T lymphocytes [65,108]. Zhu and colleagues [65] observed an overexpression of mRNA and protein induced by the interaction of AIRE
with the promoter regions of TLR1, TLR3 and TLR8 genes in a mouse
macrophage-like cell line (RAW264.7) stably expressing AIRE. In addition mRNA levels of target gene products, such as TNF- and IFN-,
were enhanced upon stimulation with TLR1 and TLR3 ligands.
Conversely, the group of Hong [109] did not report any alteration in
the expression of pattern recognition receptors in APECED patients, affected or not by Candida infection with respect to healthy controls.
The contrasting results among the two studies could be due to the
different cell type or species of origins. However the observations reported by Hong et al. [109] regarding the absence of altered TLR2, TLR4
and TLR6 expression [109] could not explain the increased susceptibility
of APECED patients to Candida infection [65].
8.2. Autoimmune polyendocrinopathy candidiasis ectodermal dystrophy
8.3. Rheumatoid arthritis
APECED (OMIM#240300), also called autoimmune polyendocrine
syndrome type I (APS-1) [106], is a rare condition characterized by endocrine gland destruction and mucocutaneous candidiasis [65]. It represents an autosomal recessive pathology due to mutations in the
autoimmune regulator (AIRE) gene [107]. AIRE expression has been
mostly described in the thymus and also in peripheral tissues, such as
fetal liver, testis, ovary, peripheral lymphoid organs and in the peripheral blood, including CD14+, DCs, granulocytes, macrophages and B cells
(rev. in [65]). AIRE regulates the negative selection of organ-specic T
RA is a chronic inammatory disease in which joint structure of the
affected subject is destroyed by activated immune cells that inltrate
and accumulate into the synovial joints. Several different cell populations, such as macrophages, which are the principal responsible for synovitis, contribute to the release of pro-inammatory cytokines and
other mediators leading to RA onset [110]. Several animal models
were used to investigate the role of TLR3 and TLR7 in RA pathogenesis.
A signicant TLR3 up-regulation has been observed in splenocytes in
the rat pristane-induced arthritis (PIA) model upon pristane treatment
Table 1
TLRs and molecules of the TLR signaling pathway affected by altered gene expression, CNV and SNPs in human autoimmune disorders. nr = not reported.
Gene
Altered expression
CNV
SNP
TLR1
TLR2
MG [85]
T1D [62];
BD [78];
ocular BD [181];
MS [197];
MG [85]
SSc [76];
RA [123125];
ocular BD [181];
MG [85]
SSc [76];
BD [77,78]; IBD [81];
RA [125];
ocular BD [181];
MS [197];
MG [85,86]
MG [85]
T1D [62];
MG [85]
RA [124]
nr
nr
T1D (rs5743612, -626 and rs4833095, -1017 in Chinese Han [64]).
T1D (rs3804100 in Norwegian and Korean populations [64]);
SSc (rs5743704, Pro631His in Europeans [74]);
vitiligo (rs5743708, Arg753Glu in Turkish population [84]);
ocular BD (rs2289318 and rs3804099 in Chinese Han population [186]).
nr
MS (rs3775290, c.1377 in Han people from South China [82]);
T1D (rs3775291 and rs13126816 [105]);
Early age at T1D diagnosis and poor glycemic control (rs5743313 and rs117221827) [105];
RA and with sero-negative RA and disease activity (rs3775291 in a Danish population [132]).
RA (rs1927911 in Caucasians [70]);
vitiligo (rs4986790, Asp299Gly in Turkish population [84]);
IBD (rs4986790, Asp299Gly in Caucasians [7981,189192]; rs4986791, Thr399Ile in
Caucasians [7981,189192]);
SLE (D299G in South Indians [152]);
CD (rs4986790, Asp299Gly [190]).
UC (R392X and N592S in North Indian population [195].
T1D (rs3775073, -1329 in Chinese Han population [64]).
TLR3
TLR4
TLR5
TLR6
TLR7
TLR8
Ocular BD [181];
MG [85]
TLR9
T1D [97];
RA [126];
SLE [141];
MG [85]
MG [85]
T1D [62]
nr
nr
TLR10
TIRAP (MAL)
TICAM1
IRF5
nr
nr
nr
Childhood SLE onset in Mexican population [71]; SLE (rs3853839 in Taiwanese females [154] and in Danish patients [155]).
SLE in Yucatan Mayan [72];
BD in Chinese Han population [187]
nr
Association with rheumatoid factor autoantibody positivity (rs5741883, in European
population [68]);
SLE [156], SLE (rs3764880 in Taiwanese females [154]; rs3764879 in Danish subjects
[155]).
nr
MS (rs352140, 2848 in Han people from South China [82]);
RA (rs187084, -1486T/C in Turkish population [134]);
SLE (rs5743836, -1237 C/T in South Indian Tamils [153]).
nr
nr
nr
nr
CD [193]; CD susceptibility and clinical outcome in a New Zealand population [194].
BD (S180L in UK population [185])
Vitiligo (Caucasians [199])
MS (rs4728142 and rs3807306 in Spanish, Swedish and Finnish [83]);
RA [67]; RA in European Caucasian [135], Korean [136], Tunisian [137] and Japanese populations [138];
SLE in European Americans [157], African Americans [158], Swedish [159], Chinese [160] and
conrmed in four ethnicities (European Americans, Hispanic Americans, African-Americans,
and Asian Americans) [156]; SLE (rs10488631 in an Egyptian cohort [161]).
E. Gianchecchi, A. Fierabracci / Autoimmunity Reviews 14 (2015) 971983
and stimulation of TLR3 with poly-I:C. Accordingly, TLR3 inhibition by
using small interfering RNA (siRNA) ameliorated RA in this animal
model [111]. The treatment with methotrexate (MTX) inhibited RA
symptoms and induced TLR3 over-expression in splenocytes from PIA
and collagen-induced arthritis (CIA) rat models [112]. Contrasting
data emerged from the study conducted by Yarilina and colleagues
[113], where it was demonstrated that TLR3 activation inhibited
arthritis in CIA and K/BxN serum transfer models. These data support
the hypothesis that TLR3 may play a role in the regulation of inammation rather than in the promotion of the inammatory process [113].
Regarding TLR7 role in RA pathogenesis, a brief TLR7 stimulation
with the agonist 1 V136 at low level was not sufcient to induce
cytokine release, but only was able to establish TLR7 tolerance and ameliorated disease in the K/BxN serum transfer model [114]. Although
TLR7/CIA model and WT mice developed RA with a similar frequency,
TLR7/CIA model was characterized by a decrease in paw swelling,
number of paws affected and clinical score than WT mice [115].
Accordingly, an amelioration of RA symptoms was observed after
intra-articular TLR7 knockdown in rat CIA model [116].
TLR8 role in RA must be yet fully elucidated, in fact whereas in
humans TLR8, such as TLR7, is functional allowing the recognition of
ssRNA, in murine models TLR8 did not activate the downstream signaling upon ligation to ssRNA [117]. Furthermore autoimmunity onset was
described in TLR8/ mice and found associated with enhanced TLR7
expression in DCs, whereas autoimmunity did not develop when TLR7
and/or TLR8 were knocked down [118]. Thus TLR7 signaling could be
modulated by TLR8 [118].
TLR9 may play an anti-inammatory role in arthritis through the
induction of tolerance. It has been demonstrated that TLR3, TLR4, TLR7
and TLR9 stimulation requires PTPN22, whose variant was associated
with RA onset, for IFN production [119].
Accordingly arthritis was suppressed after TLR stimulation in
PTPN22 knockout mice [120]. PTPN22 has been widely studied both in
several murine models and in humans since it constitutes one of the
most important genes able to inuence the susceptibility to autoimmune disorders by regulating both innate and adaptive immunity [121].
Moreover it has been reported that TLR9 antagonist diminished
arthritis severity in the rat PIA model suggesting a putative role for
TLR9 in arthritis onset [122].
TLR expression has been evaluated also in RA synovium which
showed the expression of TLR3, TLR7, TLR8 and TLR9. Moreover TLR3,
TLR7 and TLR9 were up-regulated, especially in RA synovial broblasts
(RASFs), macrophages and DCs [123126], as compared with osteoarthritis or healthy subject tissues. TLR3 and TLR8 ligands promoted
cytokine and matrix metalloprotease (MMP) production in RA synovial
cells. Among TLRs, the higher amount of TNF released from RA synovial
cultures was induced by TLR8 [66].
Several studies have investigated the correlation between TLR SNPs
and RA, reporting the presence of several associations in different ethnic
cohorts. TLR4 Asp299Gly was not associated with RA in an English cohort
[127]. Conversely the case-control study conducted in the Netherlands reported that the condition of heterozygosity for Asp299Gly was protective
in early untreated RA [128]. Kuuliala and colleagues [129] observed that
Asp299Gly SNP interfered with a quick response to therapy in RA than
Asp299Asp. Regarding TLR2 SNPs, no association has been found between
TLR2 Arg677Trp (rs number was not reported) and Arg753Gln
(rs5743708) SNPs and RA in Spanish patients [130]. Moreover no correlation was observed between the pathology and TLR1, TLR2, TLR4, TLR6 and
TLR9 SNPs in a cohort of French RA patients [131], whereas a recent study
demonstrated that TLR4 (rs1927911) SNP was associated with disease activity in Caucasian RA patients [70]. Recently it has been demonstrated
the association of TLR3 (rs3775291) SNP with RA in a Danish population
and also with sero-negative RA and disease activity in this subset [132].
TLR9 SNP (rs187084) was modestly associated with RA in a Turkish
population, whereas no correlation has been found in French and Dutch
cohorts [131,133,134]. A correlation between TLR8 SNP (rs5741883)
977
and rheumatoid factor autoantibody positivity has been reported in an
European population [68]. The casecontrol study performed by the
group of Sanchez examined the possible association of TLR4 SNPs
(Asp299Gly rs4986790 and Thr399Ile rs4986791) with RA. 224 Spanish
patients affected by RA and 199 healthy subjects were analyzed but any
signicant difference was not observed in TLR4 SNPs genotype or allele
distribution in RA patients with respect to controls [130].
The meta-analysis conducted by the group of Han [67] demonstrated
an association between IRF5 SNP and RA. IRF5 confers susceptibility to RA
and was able to inuence its erosive phenotype in European Caucasians
[135]. Moreover this correlation was furtherly conrmed in a Korean
[136], Tunisian [137] and Japanese [138] populations. Also MyD88 and
MAL/TIRAP are involved in the inammation and in the process of
destruction in human RA synovial tissue cultures [139].
8.4. Systemic lupus erythematosus
SLE is a systemic autoimmune condition which occurs more
frequently in women. It is characterized by B cell hyperactivity and
the presence of various circulating autoantibodies [72,140], in particular
to dsDNA and RNA-binding proteins [140]. The etiology is multifactorial: genetic, environmental factors, including hormones, UV light, drugs,
infections and immune system alterations are involved in its pathogenesis (rev. in [72]). Although the role of innate immunity in autoimmune
disorders is not yet fully elucidated, it has been hypothesized that altered innate immunity responses may play a critical role in SLE onset
[141], as demonstrated by the presence of several immunological
alterations in individuals affected by SLE. SLE patients showed increased
apoptosis responsible for the release of DNA and RNA that can be sensed
by TLR9 and TLR7, respectively [142,143]. PBMCs obtained from
SLE patients with active disease presented an expansion of TLR9expressing B cells and monocytes in respect to patients with inactive
disease in correlation with the presence of anti-dsDNA antibodies [61].
Accordingly, the study performed by the group of Nakano [141] demonstrated an over-expression of TLR9, strictly related to disease activity, on
B lymphocytes in SLE subjects. SLE patients are characterized also by an
abnormal methylation of DNA. This process leads to the production of
CpG, which could be involved in the activation of TLR9. As a consequence of TLR9-CpG interaction, anti-dsDNA antibody and IL-10
production are induced [141]. The latter is a regulatory cytokine able
to promote the production of pathogenic antibodies levels in certain
disorders, especially in SLE [141,144].
TLR7 plays a critical role in SLE pathogenesis through the binding to
self-antigens containing endogenous RNA followed by the induction of
type I IFN expression [145].
Furthermore increasing evidence observed in murine SLE models
demonstrates the role played by TLR7 and TLR9 in autoimmune processes. Reduction of SLE development was observed after treating (NZB
NZW)F1 mice with a TLR7 and TLR9 dual inhibitor [146] and C57BL/6
(B6)-FasIpr mice carrying the Unc93b1 mutation that affects TLR7 and
TLR9 signaling [147].
The study of TLR7-decient MRL-FasIpr and decient TLR9-decient
MRL-FasIpr mice revealed a marked suppression of autoimmune
responses against RNA-related autoantigens [148,149] and the involvement of TLR9 in anti-DNA and anti-chromatin autoantibodies production,
respectively [148,150].
RNA-selective autoantibody production was enhanced both in
FcYRIIB-decient B6 mice over-expressing TLR7 and in mice presenting
the duplication of TLR7 gene [72].
Several studies have analyzed in different populations whether CNV
of TLR7 could represent a risk factor for SLE onset reporting contrasting
results. The study conducted by Kelley and colleagues [151] regarding
the relative copy number of TLR7 in 50 Caucasian and 49 AfricanAmerican SLE patients and 91 healthy controls, reported that CNV was
not a risk factor for SLE onset in these populations and was not associated with the autoantibody prole. Conversely, it has been demonstrated
978
E. Gianchecchi, A. Fierabracci / Autoimmunity Reviews 14 (2015) 971983
that CNV of TLR7 was correlated with childhood SLE onset in the Mexican population [71]. More in detail SLE women showed a signicant increase in CNV of TLR7 in respect to controls; furthermore an increased
association has been described in female as compared with male patients [71]. A recent work performed by the group of Pacheco [72]
highlighted the role of TLR7 CNV in 80 Yucatan Mayan SLE women
and 150 controls, reporting the association between SLE development
and the increased copy number of this gene to 3 copies observed in
10% of SLE patients. However any signicant difference in mRNA TLR7
expression between patients and controls was not described. It has
been hypothesized that the increased copy number of TLR7 could promote autoimmune processes, through the enhanced production of
IFN- [72].
Several investigations have analyzed the possible association between SLE and TLR SNPs. A recent investigation performed by Rupasree
[152] conrmed for the rst time that TLR4 D299G SNP increased the
risk for SLE among South Indians. Moreover TLR4 (D299G, T399I),
TLR9 -1486T N C and TIRAP S180L SNPs contributed towards phenotypic
heterogeneity and they were able to inuence specic autoantibody
production in SLE. Another recent study investigated whether TLR2
(R753Q) and TLR9 (-1237C/T) SNPs were associated with lupus susceptibility, clinical and autoantibody phenotypes. Samples from 300 SLE
South Indian Tamils and 460 ethnicity matched controls were analyzed
by real time PCR [153]; whereas TLR2 gene remained monomorphic in
patients and controls, therefore not conferring susceptibility to SLE,
the T allele of TLR9 gene was more frequent and conferred a signicant
risk to develop SLE. However both SNPs did not inuence the clinical or
autoantibody phenotype of SLE and could exert an additive effect in the
presence of other genetic and environmental risk factors increasing the
susceptibility to SLE in South Indian Tamils. Recent investigations
demonstrated that TLR7 (rs3853839) and TLR8 (rs3764880) increased
risk of SLE in Taiwanese females [154]. The previously association reported between the (rs3853839) SNP of TLR7 and SLE in Asian patients
has also been observed in Danish patients [155]. Furthermore the group
of Armstrong have identied TLR8 as a new SLE-associated gene [156].
TLR8 (rs3764879) SNP correlated with SLE in Danish subjects [155].
A diminished susceptibility to SLE onset has been observed in the
presence of a SNP affecting MAL protein which is involved in TLR4 and
TLR2 signaling pathways (rev. in [45]). The association between IRF5
variants and SLE had been described in several populations, such as
European Americans [157], African Americans [158], in a Swedish
cohort [159], in Chinese [160] and conrmed in four ethnicities
(European Americans, Hispanic Americans, African-Americans, and
Asian Americans) by Armstrong and colleagues [156]. A recent study
provides additional evidence for the association between IRF5
rs10488631 variant and lupus susceptibility in an Egyptian cohort [161].
8.5. Systemic sclerosis
SSc is a complex and dynamic connective tissue pathology of
unknown etiology characterized by initial vascular injuries followed
by exagerated extracellular matrix (ECM) and collagen production due
to broblasts hyperactivation [162,163]. SSc encompasses diffuse cutaneous SSc (dcSSc) and limited cutaneous SSc (lcSSc). In dSSc, brosis
characterized not only the skin but also internal organs causing their
failure, whereas in lcSSc collagen is deposited prevalently in skin and
there are also vascular complications [73]. No treatment is available to
stop the progression of brosis [164]. Several studies performed on animal models and SSc patients have supported the role of TLRs in its pathogenesis by converting a self-limited tissue repair into an uncontrolled
brotic process [73,75,76]. Among endogenous TLR ligands involved in
SSc onset there are cellular stress proteins, matrix-derived molecules,
immune complexes and nucleic acids released from necrotic or
damaged cells [73].
More in detail, C3H/HeJ mice carrying a SNP in TLR4 showed a reduction in skin sclerosis induced by bleomycin [165], although endogenous
TLR4 ligands were present at high concentration [76]. Accordingly
bleomycin-treated TLR4/ mice (rev. in [76]) showed a decrease in
dermal and lung brosis than their wild-type counterparts. The group
of Takahashi [76] conrmed the critical role of TLR4 in another SSc
murine model called TLR4/;TSK/+ mice, characterized by the loss
of TLR4, observing a strong decrease in hypodermal brosis with respect
to control TSK/+ mice.
It has been described that SSc patients had high levels of high mobility group box 1 (HMGB-1) and hyaluronic acid (HA) both in serum and
lesional skin (rev. in [76]). These two molecules stimulate TLR4 and,
through the up-regulation of transforming growth factor (TGF-)
signaling, induced broblast activation [165].
Moreover the deletion of TLR4 inhibited the expression of IL-6, a
pro-brotic cytokine involved in SSc pathogenesis [76], in broblasts,
immune and endothelial cells upon treatment with bleomycin and LPS
in vivo and in vitro, respectively. Conversely, enhanced expression of
both TLR3 and TLR4 were observed in affected skin and lung biopsies
obtained from SSc subjects.
In a recent investigation 14 functional SNPs in TLR2, TLR4, TLR7, TLR8
and TLR9 have been genotyped in a discovery cohort of 452 European
SSc patients and 537 geographically-matched healthy controls. The replication cohort was composed of 1,170 SSc patients and 925 controls.
The rare Pro631His SNP in TLR2 was associated with antitopoisomerase
positivity and with SSc phenotype [74]. Moreover functional study
showed higher levels of inammatory mediators produced by
monocyte-derived DCs carrying the TLR2 variant Pro631His after stimulation with TLR ligands [74].
8.6. Behcet's disease
BD is an inammatory disorder whose complex pathogenesis is
caused by genetic and environmental factors [166168], such as microbial factors in genetically susceptible subjects [166,169,170]. It is characterized by the presence of recurrent oral aphthous and genital ulcers,
uveitis, skin lesions [167,169] and can involve the gastrointestinal
tract (intestinal BD) [167,169,171] and the CNS [166,167]. Immunological defects are present in BD patients, including alterations in the phenotype and functions of lymphocytes, neutrophil hyper-activation and
up-regulation of proinammatory and Th1-type cytokines [172,173].
It has been hypothesized that infectious agents, including Streptococcus
sanguis [174] or HSV [175,176], could play a role in BD pathogenesis.
Furthermore micro-organisms presenting antigens, like heat shock
proteins (HSPs), characterized by molecular mimicry could cause autoimmune responses through the activation of selective TCRs and the innate immune system by stimulating TLRs. These immunological
alterations may induce BD onset [77].
The involvement of TLRs in BD pathogenesis has been demonstrated
[78]. More in detail TLR2 and TLR4 mRNA expression were observed in
ileocaecal ulcer lesions, whereas no TLR expression was reported in unaffected sites of the same sample, allowing to hypothesize the existence
of a correlation between TLR expression and intestinal BD manifestation
[78]. Furthermore the co-presence of HSP60, constituting a nonpathogen-derived ligand of TLRs [78,177,178], TLR2 and IL-12 in the
lesions could indicate the involvement of TLR2 expressing cells in promoting the damaging Th1-type responses [78]. TLR4 mRNA was constitutively increased in PBMCs of BD patients, regardless of disease
activity [77]. TLR4 up-regulation might be responsible for the defective
heme oxygenase (HO-1) expression observed in BD PBMCs, leading to
the enhanced inammatory response that characterized BD [77]. In
fact HO-1 constitutes an inducible heme-degrading enzyme able to suppress inammatory processes and whose deciency was correlated to
severe chronic inammation in both HO-1 knockout mice [179] and
humans [180]. HO-1 expression was suppressed upon stimulation
with LPS (a TLR4 ligand) or HSP60, whereas LPS inhibitory effect was
completely blocked by polymyxin B, a LPS neutrizer [77]. A following
study conrmed the presence of a marked higher expression of both
E. Gianchecchi, A. Fierabracci / Autoimmunity Reviews 14 (2015) 971983
979
mRNA and protein level not only of TLR4, but also of TLR2, TLR3 and
TLR8 in PBMCs from active ocular BD patients as compared with controls, leading to hypothesize that TLR up-regulation may be involved
in the pathogenesis of BD [181]. Many studies have investigated the
possible correlation between TLR SNPs and BD.
It has been demonstrated that TLR9 SNPs were not correlated with
BD susceptibility in Japanese patients [182]. Dhifallah and colleagues
[183] reported no alteration in TLR9 (1237T/C rs5743836) SNP frequency between Tunisian BD patients and healthy controls, whereas differences were observed in the distribution of TLR9 (1486T/C rs187084)
SNP genotype frequencies, but they did not reach statistical signicance.
Furthermore no correlation has been observed between TLR9 SNPs and
the main clinical manifestations. The group of Boiardi [184] investigated
the association of Asp299Gly (rs4986790) and Thr399Ile (rs4986791)
TLR4 SNPs with BD in 189 Italian patients and 210 healthy volunteers,
but no statistical signicant differences were observed in the distribution
of allele and genotype frequencies between BD patients and controls.
TLR2, TLR4 and TIRAP SNPs were analyzed in BD patients from
different geographical areas and only TIRAP S180L was signicantly
associated with the pathology in UK individuals; however this correlation was not observed in Middle Eastern patients [185].
In the two-stage control-association study performed by Fang and
colleagues [186], an association between ocular BD and TLR2 SNPs
(rs2289318 and rs3804099) was observed in a Han Chinese population,
although these two SNPs did not exert any effect on the release of
TNF-, IL-6, IL-10, and IL-1. No association was reported between BD
and TLR2 SNP (rs13150331), TLR4 SNP (rs7037117), TLR8 SNP
(rs3764880) and TLR9 SNPs (rs187084, rs352139, rs352140). A recent
investigation conducted by the same group [187] provided evidence
that a high copy number of TLR7 conferred risk for BD in a Chinese
Han population; however TLR7 CNV did not induce any alteration on
the release of TNF-, IL-6, IL-1, and IFN-.
a signicant correlation between Asp299Gly and CD, but not UC. Further
analysis have to be performed to conrm the association between TLR4
SNPs and UC in Caucasians. An association of TLR10 and susceptibility to
CD has been described in two cohorts of 284 and 224 CD patients [193].
Furthermore genetic variations in TLR10 play a role in interindividual
differences in CD susceptibility and clinical outcome in a New Zealand
population [194].
A recent study investigated whether TLR1-R80T, TLR2-R753Q, TLR3S258G, TLR5-R392X and -N592S and TLR6-S249P SNPs in UC patients
from North Indian [195]. Only TLR5 variants R392X and N592S showed
signicant association with UC. Patients carrying different genotypes of
TLR4 and TLR5 SNPs showed a signicant modulation of cytokine level
[195].
8.7. Crohn's disease and ulcerative colitis
8.9. Vitiligo
CD and UC represent two principal forms of idiopathic inammatory
bowel disease (IBD). This is a complex disorder characterized by the
presence of a chronic inammation affecting the gastrointestinal tract
and frequent extra-intestinal manifestations [188]. More in detail aberrant innate and adaptive immune responses directed towards PAMPs
from microorganisms constituting the intestinal ora, have been
hypothesized to be responsible for IBD onset in genetically susceptible
subjects. This hypothesis is supported by the observation that UC and
CD patients show an impaired epithelial barrier and an enhanced
intestinal permeability [188].
Although its pathogenesis is not fully elucidated, multiple nongenetic and genetic factors could be involved in IBD etiology including
altered TLR expression and TLR SNPs [81]. TLR4 expression was low in
intestinal biopsies from healthy subjects, whereas it was strongly enhanced in intestinal epithelial cells, local macrophages and DCs present
in the inamed mucosa of IBD patients (rev. in [81]).
The possible involvement of TLR2 (Arg677Trp and Arg753Glu), TLR4
(Asp299Gly and Thr399Ile) and TLR9 (1237T/C) SNPs in IBD pathology
has been evaluated by Shen and colleagues in Chinese Han and
Caucasian populations [80]. They described an association between
both TLR4 SNPs and CD and UC only in Caucasians.
A meta-analysis conducted by the same group [81] conrmed the
signicant correlation between TLR4 (Asp299Gly and Thr399Ile) SNPs
and CD and UC in the Caucasian population, whereas no association
was observed between Asp299Gly and CD phenotype, including age at
onset. These data were in agreement with the study conducted by
Franchimont and colleagues [79] in a prevalent Caucasian population
and with other meta-analyses previously performed [189192]. Other
studies have reported contrasting results. In fact whereas some analysis
described only a higher frequency of Asp299Gly allele in patients with
CD and UC (rev. in [81]), the study conducted by De Jager [190] showed
Vitiligo represents a complex disease in which the autoimmune
destruction of melanocytes causes the onset of pigmented skin
maculopatches [198]. Although its etiology remains unknown, genetic
and environmental factors contribute to its onset. A recent study investigated whether TLR2 SNP (Arg753Glu) and TLR4 SNPs (Asp299Gly and
Thr399Ile) were associated with this disorder. A total of 100 Turkish
patients affected by vitiligo and 100 controls have been analyzed.
They reported a signicant association between TLR2 and TLR4
Asp299Gly SNPs, while no difference has been observed in TLR4
Thr399Ile SNP distribution among vitiligo and healthy subjects [84].
Among genes reported to be associated with vitiligo, TICAM1 represents
a susceptibility loci in Caucasians (rev. in [199]).
8.8. Multiple sclerosis
Multiple sclerosis (MS) is a chronic inammatory disease affecting
the CNS which is characterized by immune mediated demyelination
and damage of axons. MS constitutes a complex disorder and it has
been hypothesized that environmental and genetic factors contribute
to its etiology [196]. It is estimated that it affects more than two million
of people worldwide. The expression of TLR2 and TLR4 were assessed by
ow-cytometry on PBMCs and a signicant high expression of both has
been observed in MS patients than in healthy controls [197]. It has been
hypothesized that elevated expression of these genes could be responsible for innate immune activation in patients affected by MS [197].
TLR3 c.1377 and TLR9 2848 SNPs were related to MS in Han people
from South China, whereas TLR9-1486 did not show any association
with MS [82]. Two IRF5 SNPs (rs4728142 and rs3807306) and a 5 bp
insertion-deletion in the promoter and rst intron of IRF5 gene were associated with MS in Spanish, Swedish and Finnish patients, whereas no
association was reported between IRF5 rs12539741 SNP and MS [83].
8.10. Myasthenia gravis
MG represents a rare T cell-dependent autoimmune syndrome characterized by autoantibodies recognizing several components of the neuromuscular junction (NMJ) and causing muscle weakness and early
fatigability (rev. in [200,201]). Several forms of MG have been identied
on the basis of age of disease onset, associated thymus pathologies and
the presence of pathogenic autoantibodies (rev. in [201]). Although
the pathogenesis remains unclear, genetic and environmental factors,
especially prolonged viral infections, appear to be involved in MG
onset [200,201].
Several evidence support the hypothesis that pathogen infections
could represent triggering factors for MG. This may occur through a
mechanism of molecular mimicry of microbial antigens that could promote the activation of T lymphocytes against self-antigens. In particular
Measles and EpsteinBarr virus (EBV) infections have been demonstrated
to precede this autoimmune condition [200]. Increasing data have
highlighted that thymus, the rst organ in which occurs autosensitization
980
E. Gianchecchi, A. Fierabracci / Autoimmunity Reviews 14 (2015) 971983
and mainteinance of the autoimmune response in AChR-positive MG subjects, presents alterations not only in its morphology but also in its functions in 80% of patients affected by the generalized form of MG [200,
201]. Cavalcante et al. [200] reported the persistence and reactivation of
EBV in the thymus of patients with the early onset MG. EBV infection
may sustain the autoimmune response in the thymus by activating and
immortalizing thymic self-reactive B lymphocytes. Moreover these cells
can leave the organ and continue autoimmune responses also in the periphery. Here autoimmunity may be sustained by the fact that Tregs are
defective and by the formation of skeletal muscle-derived muscle-type
acetylcholine receptor (AChR)/immune complexes in lymph nodes.
Most of the MG cases have autoantibodies towards the AChR (rev. in
[201]). The chronic self-perpetuating inammation may be due to TLRsignaling activation [202]. Few studies have investigated the involvement
of TLRs in MG onset. mRNA expression of several TLRs was found to be
highly altered in PBMCs obtained from MG patients in respect to nonMG patients: TLR2, TLR3, TLR4, TLR5, TLR8 and TLR9 expression was enhanced, whereas TLR1, TLR6 and TLR10 was diminished. Furthermore a
correlation between TLR9 mRNA expression and MG clinical severity
was observed; this envisages the potential involvement of TLR signaling
pathway in MG pathogenesis [85]. Bernasconi et al. [86] found that
TLR4 was over-expressed in hyperplastic thymus from MG patients. A potential association between viral infection and MG has been supported
also by the fact that poly (I:C) injections were able to induce the selective
proliferation of B lymphocytes, the production of serum anti-AChR antibodies and MG-like clinical signs in wild-type mice, but not in mice decient for IFN-I receptor [203].
9. Conclusive remarks
The etiopathogenesis of autoimmune disorders is due to the interaction of environmental [204] and genetic factors. Increasing evidence
support the critical role played by TLR pathway in the activation of
immune-mediated tissue damage that characterizes autoimmune conditions. Increasing results obtained from the analysis of several experimental models of autoimmunity and the discovery of TLR SNPs and
CNV found associated with certain autoimmune conditions in peculiar
ethnic groups, have highlighted the relevance of the TLR signaling
pathway in autoimmunity onset. Molecules involved in TLR pathway
may represent the targets for novel therapeutics in order to stop the
autoimmune process [205]. Pharmacological treatments acting on
different targets, such as MyD88, IRAK1, IRAK4, TLR7 and TLR9, have
been unravelled. Experiments conducted in vitro and in experimental
animal models of autoimmunity as SLE, IBD, MS and RA, demonstrated
the efcacy of TLRs and TLR signaling cascade inhibitions [205,206].
Experimental data however demonstrate that, being TLR pathway
critically involved in the immune defense of the host against infections,
an accurate selection of the target and a strict regulation of its activity
within the signaling cascade is necessary in order to obtain the desired
therapeutic effect [205]. Moreover an important contribution to better
elucidate the involvement of TLRs in the pathogenesis of autoimmunity
could be given by whole exome sequencing (WES), representing a
powerful tool for the detection of protein coding and splicing variants
associated with complex inherited pathologies [207].
Acknowledgments
This work was supported by the Italian Ministry of Health Ricerca
Corrente (201502P0034960).
References
[1] Thwaites R, Chamberlain G, Sacre S. Emerging role of endosomal toll-like receptors
in rheumatoid arthritis. Front Immunol 2014;5:1.
[2] Hurst J, von Landenberg P. Toll-like receptors and autoimmunity. Autoimmun Rev
2008;7:2048.
[3] Kumar H, Kawai T, Akira S. Pathogen recognition in the innate immune response.
Biochem J 2009;420:116.
[4] Janeway Jr CA, Medzhitov R. Innate immune recognition. Annu Rev Immunol 2002;
20:197216.
[5] Akira S, Uematsu S, Takeuchi O. Pathogen recognition and innate immunity. Cell
2006;124:783801.
[6] Medzhitov R. Recognition of microorganisms and activation of the immune response. Nature 2007;449:81926.
[7] Beutler BA. TLRs and innate immunity. Blood 2009;113:1399407.
[8] Hashimoto C, Hudson KL, Anderson KV. The Toll gene of Drosophila, required for
dorsalventral embryonic polarity, appears to encode a transmembrane protein.
Cell 1988;52:26979.
[9] Lemaitre B, Nicolas E, Michaut L, Reichhart J-M, Hoffmann JA. The dorsoventral regulatory gene cassette spatzle/Toll/cactus controls the potent antifungal response in
Drosophila adults. Cell 1996;86:97383.
[10] Takeda K, Akira S. TLR signaling pathways. Semin Immunol 2004;16:39.
[11] Rock FL, Hardiman G, Timans JC, Kastelein RA, Bazan JF. A family of human receptors structurally related to Drosophila Toll. Proc Natl Acad Sci U S A 1998;95:
58893.
[12] Kawai T, Akira S. TLR signaling. Semin Immunol 2007;19:2432.
[13] Poltorak A, He X, Smirnova I, Liu MY, Huffel CV, Du X, et al. Defective LPS signaling
in C3H/HeJ and C57BL/10ScCr mice: mutation in Tlr4 gene. Science 1998;282:
20858.
[14] Hoshino K, Takeuchi O, Kawai T, Sanjo H, Ogawa T, Takeda Y, et al. Cutting edge:
Toll-like receptor 4 (TLR4)-decient mice are hyporesponsive to lipopolysaccharide: evidence for TLR4 as the Lps gene product. J Immunol 1999;162:374952.
[15] Underhill DM, Ozinsky A, Hajjar AM, Stevens A, Wilson CB, Bassetti M, et al. The
Toll-like receptor 2 is recruited to macrophage phagosomes and discriminates between pathogens. Nature 1999;401:8115.
[16] Akira S, Takeda K. Toll-like receptor signalling. Nat Rev Immunol 2004;4:499511.
[17] Kaisho T, Akira S. Toll-like receptor function and signaling. J Allergy Clin Immunol
2006;117:97987.
[18] Hacker H, Vabulas RM, Takeuchi O, Hoshino K, Akira S, Wagner H. Immune cell activation by bacterial CpG-DNA through myeloid differentiation marker 88 and
tumor necrosis factor receptor-associated factor (TRAF)6. J Exp Med 2000;192:
595600.
[19] Schnare M, Holt AC, Takeda K, Akira S, Medzhitov R. Recognition of CpG DNA is mediated by signaling pathways dependent on the adaptor protein MyD88. Curr Biol
2000;10:113942.
[20] Hemmi H, Kaisho T, Takeuchi O, Sato S, Sanjo S, Hoshino K, et al. Small antiviral
compounds activate immune cells via TLR7 MyD88-dependent signalling pathway.
Nat Immunol 2002;3:196200.
[21] Hayashi F, Smith KD, Ozinsky A, Hawn TR, Yi EC, Goodlett DR, et al. The innate immune response to bacterial agellin is mediated by Toll-like receptor-5. Nature
2001;410:1099103.
[22] Suzuki N, Suzuki S, Yeh WC. IRAK-4 as the central TIR signaling mediator in innate
immunity. Trends Immunol 2002;23:5036.
[23] Chen ZJ. Ubiquitin signalling in the NF-kappaB pathway. Nat Cell Biol 2005;7:
75865.
[24] Janssens S, Burns K, Tschopp J, Beyaert R. Regulation of interleukin-1 and
lipopolysaccharide-induced NF-B activation by alternative splicing of MyD88. Curr
Biol 2002;12:46771.
[25] Burns K, Janssens S, Brissoni B, Olivos N, Beyaert R, Tschopp J. Inhibition of IL-1
receptor/Toll-like receptor signaling through the alternatively spliced, short form
of MyD88 is due to its failure to recruit IRAK-4. J Exp Med 2003;197:2638.
[26] Yamamoto M, Sato S, Hemmi H, Uematsu S, Hoshino K, Kaisho T, et al. TRAM is specically involved in the Toll-like receptor 4-mediated MyD88-independent signaling pathway. Nat Immunol 2003;4:114450.
[27] Meylan E, Burns K, Hofmann K, Blancheteau V, Martinon F, Kelliher M, et al. RIP1 is
an essential mediator of Toll-like receptor 3-induced NF-kappa B activation. Nat
Immunol 2004;5:5037.
[28] Carty M, Goodbody R, Schroder M, Stack J, Moynagh PN, Bowie AG. The human
adaptor SARM negatively regulates adaptor protein TRIF-dependent Toll-like receptor signaling. Nat Immunol 2006;7:107481.
[29] Couillault C, Pujol N, Reboul J, Sabatier L, Guichou JF, Kohara Y, et al. TLRindependent control of innate immunity in Caenorhabditis elegans by the TIR domain adaptor protein TIR-1, an ortholog of human SARM. Nat Immunol 2004;5:
48894.
[30] Covert MW, Leung TH, Gaston JE, Baltimore D. Achieving stability of
lipopolysaccharide-induced NF-kappaB activation. Science 2005;309:18547.
[31] Kawai T, Akira S. Innate immune recognition of viral infection. Nat Immunol 2006;7:
1317.
[32] Yoneyama M, Kikuchi M, Natsukawa T, Shinobu N, Imaizumi T, Miyagishi M, et al.
The RNA helicase RIG-I has an essential function in double-stranded RNA-induced
innate antiviral responses. Nat Immunol 2004;5:7307.
[33] Lincez PJ, Shanina I, Horwitz MS. Reduced expression of the MDA5 gene IFIH1 prevents autoimmune diabetes. Diabetes 2015;64:218493.
[34] Ishii KJ, Coban C, Kato H, Takahashi K, Torii Y, Takeshita F, et al. A Toll-like receptorindependent antiviral response induced by double-stranded B-form DNA. Nat
Immunol 2006;7:408.
[35] Zhang D, Zhang G, Hayden MS, Greenblatt MB, Bussey C, Flavell RA, et al. A toll-like
receptor that prevents infection by uropathogenic bacteria. Science 2004;303:
15226.
[36] Takeuchi O, Hoshino K, Akira S. Cutting edge: TLR2-decient and MyD88-decient
mice are highly susceptible to Staphylococcus aureus infection. J Immunol 2000;
165:53926.
E. Gianchecchi, A. Fierabracci / Autoimmunity Reviews 14 (2015) 971983
[37] Echchannaoui H, Frei K, Schnell C, Leib SL, Zimmerli W, Landmann R. Toll-like receptor 2-decient mice are highly susceptible to Streptococcus pneumoniae meningitis because of reduced bacterial clearing and enhanced inammation. J Infect Dis
2002;186:798806.
[38] Wagner H. The immunobiology of the TLR9 subfamily. Trends Immunol 2004;25:
3816.
[39] Siegal FP, Kadowaki N, Shodell M, Fitzgerald-Bocarsly PA, Shah K, Ho S, et al. The nature of the principal type 1 interferon-producing cells in human blood. Science 1999;
284:18357.
[40] Kato H, Takeuchi O, Sato S, Yoneyama M, Yamamoto M, Matsui K, et al. Differential
roles of MDA5 and RIG-I helicases in the recognition of RNA viruses. Nature 2006;
441:1015.
[41] Kato H, Sato S, Yoneyama M, Yamamoto M, Uematsu S, Matsui K, et al. Cell typespecic involvement of RIG-I in antiviral response. Immunity 2005;23:1928.
[42] Krug A, French AR, Barchet W, Fischer JA, Dzionek A, Pingel JT, et al. TLR9dependent recognition of MCMV by IPC and DC generates coordinated cytokine responses that activate antiviral NK cell function. Immunity 2004;21:10719.
[43] Kawai T, Akira S. The roles of TLRs, RLRs and NLRs in pathogen recognition. Int
Immunol 2009;21:31737.
[44] Adachi K, Tsutsui H, Kashiwamura S, Seki E, Nakano H, Takeuchi O, et al. Plasmodium berghei infection in mice induces liver injury by an IL-12- and toll-like receptor/
myeloid differentiation factor 88-dependent mechanism. J Immunol 2001;167:
592834.
[45] Lee S, Kang D, Ra EA, Lee TA, Ploegh HL, Park B. Negative regulation of TLR9 signaling by its N-terminal proteolytic cleavage product. J Immunol 2014;193:372635.
[46] Wang Y, Tang Y, Teng L, Wu Y, Zhao X, Pei G. Association of beta-arrestin and
TRAF6 negatively regulates Toll-like receptor-interleukin 1 receptor signaling.
Nat Immunol 2006;7:13947.
[47] Boone DL, Turer EE, Lee EG, Ahmad RC, Wheeler MT, Tsui C, et al. The ubiquitinmodifying enzyme A20 is required for termination of Toll-like receptor responses.
Nat Immunol 2004;5:105260.
[48] Negishi H, Ohba Y, Yanai H, Takaoka A, Honma K, Yui K, et al. Negative regulation of
Toll-like-receptor signaling by IRF-4. Proc Natl Acad Sci U S A 2005;102:1598994.
[49] Brint EK, Xu D, Liu H, Dunne A, McKenzie AN, O'Neill LA, et al. ST2 is an inhibitor of
interleukin 1 receptor and Toll-like receptor 4 signaling and maintains endotoxin
tolerance. Nat Immunol 2004;5:3739.
[50] Saitoh T, Tun-Kyi A, Ryo A, Yamamoto M, Finn G, Fujita T, et al. Negative regulation
of interferon-regulatory factor 3-dependent innate antiviral response by the prolyl
isomerase Pin1. Nat Immunol 2006;7:598605.
[51] Su X, Li S, Meng M, Qian W, Xie W, Chen D, et al. TNF receptor-associated factor-1
(TRAF1) negatively regulates Toll/IL-1 receptor domain-containing adaptor inducing IFN-beta (TRIF)-mediated signaling. Eur J Immunol 2006;36:199206.
[52] Mansell A, Smith R, Doyle SL, Gray P, Fenner JE, Crack PJ, et al. Suppressor of cytokine signaling 1 negatively regulates Toll-like receptor signaling by mediating Mal
degradation. Nat Immunol 2006;7:14855.
[53] Gilchrist M, Thorsson V, Li B, Rust AG, Korb M, Kennedy K, et al. Systems biology
approaches identify ATF3 as a negative regulator of Toll-like receptor 4. Nature
2006;441:1738.
[54] Richez C, Blanco P, Rifkin I, Moreau JF, Schaeverbeke T. Role for toll-like receptors in
autoimmune disease: the example of systemic lupus erythematosus. Joint Bone
Spine 2011;78:12430.
[55] Bot A. In this issue: autoimmunity and innate immunity. Int Rev Immunol 2014;33:
12.
[56] van der Laan JW, Gould S, Tanir JY, Vaccines ILSIHESI, Committee Adjuvants Safety
Project. Safety of vaccine adjuvants: focus on autoimmunity. Vaccine 2015;33:
150714.
[57] Edwards AD, Diebold SS, Slack EM, Tomizawa H, Hemmi H, Kaisho T, et al. Toll-like
receptor expression in murine DC subsets: lack of TLR7 expression by
CD8alpha + DC correlates with unresponsiveness to imidazoquinolines. Eur J
Immunol 2003;33:82733.
[58] Gursel I, Gursel M, Yamada H, Ishii KJ, Takeshita F, Klinman DM. Elements in mammalian telomeres suppress bacterial DNA-induced immune activation. J Immunol
2003;171:1393400.
[59] Kariko K, Buckstein M, Ni H, Weissman D. Suppression of RNA recognition by Tolllike receptors: the impact of nucleoside modication and the evolutionary origin of
RNA. Immunity 2005;23:16575.
[60] Rifkin IR, Leadbetter EA, Busconi L, Viglianti G, Marshak-Rothstein A. Toll-like receptors, endogenous ligands, and systemic autoimmune disease. Immunol Rev
2005;204:2742.
[61] Papadimitraki ED, Choulaki C, Koutala E, Bertsias G, Tsatsanis C, Gergianaki I, et al.
Expansion of toll-like receptor 9-expressing B cells in active systemic lupus erythematosus: implications for the induction and maintenance of the autoimmune process. Arthritis Rheum 2006;54:360111.
[62] Stechova K, Kolar M, Blatny R, Halbhuber Z, Vcelakova J, Hubackova M, et al.
Healthy rst degree relatives of patients with type 1 diabetes exhibit signicant
differences in basal gene expression pattern of immunocompetent cells compared
to controls: expression pattern as predeterminant of autoimmune diabetes. Scand J
Immunol 2011;75:2109.
[63] Lee MS. Treatment of autoimmune diabetes by inhibiting the initial event. Immune
Netw 2013;13:1948.
[64] Sun C, Zhi D, Shen S, Luo F, Sanjeevi CB. SNPs in the exons of Toll-like receptors are
associated with susceptibility to type 1 diabetes in Chinese population. Hum
Immunol 2014;75:10848.
[65] Zhu W, Yang W, He Z, Liao X, Wu J, Sun J, et al. Overexpressing autoimmune regulator regulates the expression of toll-like receptors by interacting with their promoters in RAW264.7 cells. Cell Immunol 2011;270:15663.
981
[66] Sacre SM, Lo A, Gregory B, Simmonds RE, Williams L, Feldmann M, et al. Inhibitors
of TLR8 reduce TNF production from human rheumatoid synovial membrane cultures. J Immunol 2008;181:80029.
[67] Han SW, Lee WK, Kwon KT, Lee BK, Nam EJ, Kim GW. Association of polymorphisms in interferon regulatory factor 5 gene with rheumatoid arthritis: a
metaanalysis. J Rheumatol 2009;36:6937.
[68] Enevold C, Radstake TR, Coenen MJ, Fransen J, Toonen EJ, Bendtzen K, et al. Multiplex screening of 22 single-nucleotide polymorphisms in 7 Toll-like receptors: an
association study in rheumatoid arthritis. J Rheumatol 2010;37:90510.
[69] Lin YT, Verma A, Hodgkinson CP. Toll-like receptors and human disease: lessons
from single nucleotide polymorphisms. Curr Genomics 2012;13:63345.
[70] Davis ML, LeVan TD, Yu F, Sayles H, Sokolove J, Robinson W, et al. Associations of
toll-like receptor (TLR)-4 single nucleotide polymorphisms and rheumatoid arthritis disease progression: an observational cohort study. Int Immunopharmacol
2015;24:34652.
[71] Garca-Ortiz H, Velzquez-Cruz R, Espinosa-Rosales F, Jimnez-Morales S, Baca V,
Orozco L. Association of TLR7 copy number variation with susceptibility to
childhood-onset systemic lupus erythematosus in Mexican population. Ann
Rheum Dis 2010;69:18615.
[72] Pacheco GV, Cruz DC, Gonzlez Herrera LJ, Prez Mendoza GJ, Adrin Amaro GI,
Nakazawa Ueji YE, et al. Copy number variation of TLR-7 gene and its association
with the development of systemic lupus erythematosus in female patients from
Yucatan Mexico. Genet Epigenet 2014;6:316.
[73] Wei J, Bhattacharyya S, Tourtellotte WG, Varga J. Fibrosis in systemic sclerosis:
emerging concepts and implications for targeted therapy. Autoimmun Rev 2011;
10:26775.
[74] Broen JC, Bossini-Castillo L, van Bon L, Vonk MC, Knaapen H, Beretta L, et al. A rare
polymorphism in the gene for Toll-like receptor 2 is associated with systemic sclerosis phenotype and increases the production of inammatory mediators. Arthritis
Rheum 2012;64:26471.
[75] Bhattacharyya S, Kelley K, Melichian DS, Tamaki Z, Fang F, Su Y, et al. Toll-like receptor 4 signaling augments transforming growth factor- responses: a novel
mechanism for maintaining and amplifying brosis in scleroderma. Am J Pathol
2013;182:192205.
[76] Takahashi T, Asano Y, Ichimura Y, Toyama T, Taniguchi T, Noda S, et al. Amelioration of tissue brosis by toll-like receptor 4 knockout in murine models of systemic
sclerosis. Arthritis Rheum 2015;67:25465.
[77] Kirino Y, Takeno M, Watanabe R, Murakami S, Kobayashi M, Ideguchi H, et al. Association of reduced heme oxygenase-1 with excessive Toll-like receptor 4 expression in peripheral blood mononuclear cells in Behet's disease. Arthritis Res Ther
2008;10:R16.
[78] Nara K, Kurokawa MS, Chiba S, Yoshikawa H, Tsukikawa S, Matsuda T, et al. Involvement of innate immunity in the pathogenesis of intestinal Behet's disease.
Clin Exp Immunol 2008;152:24551.
[79] Franchimont D, Vermeire S, El Housni H, Pierik M, Van Steen K, Gustot T, et al. Decient host-bacteria interactions in inammatory bowel disease? The toll-like receptor (TLR)-4 Asp299gly polymorphism is associated with Crohn's disease and
ulcerative colitis. Gut 2004;53:98792.
[80] Shen XY, Shi RH, Wang Y, Zhang HJ, Zhou XQ, Shen FC, et al. Toll-like receptor
gene polymorphisms and susceptibility to inammatory bowel disease in Chinese Han and Caucasian populations. Zhonghua Yi Xue Za Zhi 2010;90:
141620.
[81] Shen X, Shi R, Zhang H, Li K, Zhao Y, Zhang R. The Toll-like receptor 4 D299G and
T399I polymorphisms are associated with Crohn's disease and ulcerative colitis: a
meta-analysis. Digestion 2010;81:6977.
[82] Ji X, Wang Y, Huang G, Zhou W. TLR3c.1377, TLR9-1486, and TLR9 2848 gene polymorphisms and multiple sclerosis. Zhong Nan Da Xue Xue Bao Yi Xue Ban 2010;35:
11622.
[83] Kristjansdottir G, Sandling JK, Bonetti A, Roos IM, Milani L, Wang C, et al. Interferon
regulatory factor 5 (IRF5) gene variants are associated with multiple sclerosis in
three distinct populations. J Med Genet 2008;45:3629.
[84] Karaca N, Ozturk G, Gerceker BT, Turkmen M, Berdeli A. TLR2 and TLR4 gene polymorphisms in Turkish vitiligo patients. J Eur Acad Dermatol Venereol 2013;27:
e8590.
[85] Wang YZ, Yan M, Tian FF, Zhang JM, Liu Q, Yang H, et al. Possible involvement of
Toll-like receptors in the pathogenesis of myasthenia gravis. Inammation 2013;
36:12130.
[86] Bernasconi P, Barberis M, Baggi F, Passerini L, Cannone M, Arnoldi E, et al. Increased
toll-like receptor 4 expression in thymus of myasthenic patients with thymitis and
thymic involution. Am J Pathol 2005;167:12939.
[87] Silveira PA, Grey ST. B cells in the spotlight: innocent bystanders or major
players in the pathogenesis of type 1 diabetes. Trends Endocrinol Metab
2006;17:12835.
[88] Bluestone JA, Herold K, Eisenbarth G. Genetics, pathogenesis and clinical interventions in type 1 diabetes. Nature 2010;464:1293300.
[89] Fierabracci A. The potential of multimer technologies in type 1 diabetes prediction
strategies. Diabetes Metab Res Rev 2011;27:21629.
[90] Gianchecchi E, Palombi M, Fierabracci A. The putative role of the C1858T polymorphism of protein tyrosine phosphatase PTPN22 gene in autoimmunity. Autoimmun
Rev 2013;12:71725.
[91] Wen L, Peng J, Li Z, Wong FS. The effect of innate immunity on autoimmune diabetes and the expression of Toll-like receptors on pancreatic islets. J Immunol 2004;
172:317380.
[92] Lang KS, Recher M, Junt T, Navarini AA, Harris NL, Freigang S, et al. Toll-like receptor
engagement converts T-cell autoreactivity into overt autoimmune disease. Nat
Med 2005;11:13845.
982
E. Gianchecchi, A. Fierabracci / Autoimmunity Reviews 14 (2015) 971983
[93] Kim HS, Han MS, Chung KW, Kim S, Kim E, Kim MJ, et al. Toll-like receptor 2 senses
beta-cell death and contributes to the initiation of autoimmune diabetes. Immunity
2007;27:32133.
[94] Zipris D, Lien E, Xie JX, Greiner DL, Mordes JP, Rossini AA. TLR activation synergizes
with Kilham rat virus infection to induce diabetes in BBDR rats. J Immunol 2005;
174:13142.
[95] Wen L, Ley RE, Volchkov PY, Stranges PB, Avanesyan L, et al. Innate immunity and
intestinal microbiota in the development of Type 1 diabetes. Nature 2008;455:
1109-3.
[96] Aumeunier A, Grela F, Ramadan A, Pham Van L, Bardel E, Gomez Alcala A, et al. Systemic Toll-like receptor stimulation suppresses experimental allergic asthma and
autoimmune diabetes in NOD mice. PLoS One 2010;5 e11484.
[97] Han D, Cai X, Wen J, Matheson D, Skyler JS, Kenyon NS, et al. Innate and adaptive
immune gene expression proles as biomarkers in human type 1 diabetes. Clin
Exp Immunol 2012;170:1318.
[98] Meyers A, Shah R, Gottlieb P, Zipris D. Altered toll-like receptor signaling pathways
in human type 1 diabetes. J Mol Med 2010;88:122131.
[99] Alkanani AK, Rewers M, Dong F, Waugh K, Gottlieb PA, Zipris D. Dysregulated Tolllike receptor-induced interleukin-1 and interleukin-6 responses in subjects at risk
for the development of type 1 diabetes. Diabetes 2012;61:252533.
[100] Kristiansen OP, Mandrup-Poulsen T. Interleukin-6 and diabetes: the good, the bad,
or the indifferent? Diabetes 2005;54:S11424.
[101] Gianchecchi E, Crin A, Giorda E, Luciano R, Perri V, Russo AL, et al. Altered B cell
homeostasis and toll-like receptor 9-driven response in type 1 diabetes carriers
of the C1858T PTPN22 allelic variant: implications in the disease pathogenesis.
PLoS One 2014;9 e110755.
[102] Petrich de Marquesini LG, Fu J, Connor KJ, Bishop AJ, McLintock NE, Pope C, et al.
IFN-gamma and IL-10 islet-antigen-specic T cell responses in autoantibodynegative rst-degree relatives of patients with type 1 diabetes. Diabetologia
2010;53:145160.
[103] Devaraj S, Dasu MR, Park SH, Jialal I. Increased levels of ligands of Toll-like receptors
2 and 4 in type 1 diabetes. Diabetologia 2009;52:16658.
[104] Castiblanco J, Varela DC, Castao-Rodrguez N, Rojas-Villarraga A, Hincapi ME,
Anaya JM. TIRAP (MAL) S180L polymorphism is a common protective factor
against developing tuberculosis and systemic lupus erythematosus. Infect Genet
Evol 2008;8:5414.
[105] Assmann TS, Brondani Lde A, Bauer AC, Canani LH, Crispim D. Polymorphisms in
the TLR3 gene are associated with risk for type 1 diabetes mellitus. Eur J Endocrinol
2014;170:51927.
[106] Proust-Lemoine E, Saugier-Veber P, Wmeau JL. Polyglandular autoimmune syndrome type I. Presse Med 2012;41:e65162.
[107] Fierabracci A. Recent insights into the role and molecular mechanisms of the autoimmune regulator (AIRE) gene in autoimmunity. Autoimmun Rev 2011;10:
13743.
[108] Sediv A, Cihkov D, Lebl J. Immunological ndings in patients with autoimmune
polyendocrinopathy-candidiasis-ectodermal dystrophy (APECED) and their family
members: are heterozygotes subclinically affected? J Pediatr Endocrinol Metab
2002;15:14916.
[109] Hong M, Ryan KR, Arkwright PD, Gennery AR, Costigan C, Dominguez M, et al. Pattern recognition receptor expression is not impaired in patients with chronic
mucocutanous candidiasis with or without autoimmune polyendocrinopathy candidiasis ectodermal dystrophy. Clin Exp Immunol 2009;156:4051.
[110] Boissier MC, Semerano L, Challal S, Saidenberg-Kermanac'h N, Falgarone G. Rheumatoid arthritis: from autoimmunity to synovitis and joint destruction. J
Autoimmun 2012;39:2228.
[111] Meng L, Zhu W, Jiang C, He X, Hou W, Zheng F, et al. Toll-like receptor 3 upregulation in macrophages participates in the initiation and maintenance of pristaneinduced arthritis in rats. Arthritis Res Ther 2010;12:R103.
[112] Zhu W, Meng L, Jiang C, Xu J, Wang B, Han Y, et al. Overexpression of toll-like receptor 3 in spleen is associated with experimental arthritis in rats. Scand J Immunol
2012;76:26370.
[113] Yarilina A, DiCarlo E, Ivashkiv LB. Suppression of the effector phase of inammatory
arthritis by double-stranded RNA is mediated by type I IFNs. J Immunol 2007;178:
220411.
[114] Hayashi T, Gray CS, Chan M, Tawatao RI, Ronacher L, McGargill MA, et al. Prevention of autoimmune disease by induction of tolerance to Toll-like receptor 7. Proc
Natl Acad Sci U S A 2009;106:27649.
[115] Alzabin S, Kong P, Medghalchi M, Palfreeman A, Williams R, Sacre S. Investigation
of the role of endosomal Toll-like receptors in murine collagen-induced arthritis reveals a potential role for TLR7 in disease maintenance. Arthritis Res Ther 2012;14:
R142.
[116] Chen SY, Shiau AL, Li YT, Lin YS, Lee CH, Wu CL, et al. Suppression of collageninduced arthritis by intra-articular lentiviral vector-mediated delivery of Toll-like
receptor 7 short hairpin RNA gene. Gene Ther 2012;19:75260.
[117] Heil F, Hemmi H, Hochrein H, Ampenberger F, Kirschning C, Akira S, et al. Speciesspecic recognition of single-stranded RNA via toll-like receptor 7 and 8. Science
2004;303:15269.
[118] Demaria O, Pagni PP, Traub S, de Gassart A, Branzk N, Murphy AJ, et al. TLR8 deciency leads to autoimmunity in mice. J Clin Invest 2010;120:365162.
[119] Begovich AB, Carlton VE, Honigberg LA, Schrodi SJ, Chokkalingam AP, Alexander
HC, et al. A missense single-nucleotide polymorphism in a gene encoding a protein
tyrosine phosphatase (PTPN22) is associated with rheumatoid arthritis. Am J Hum
Genet 2004;75:3307.
[120] Wang Y, Stanford S, Zhou W, Auger Jennifer L, Cheng G, Campbell A, et al. Rheumatoid arthritis-associated PTPN22 modulates toll-like receptor-mediated, type 1
interferon-dependent innate immunoregulation. Arthritis Rheum 2012;64:2452.
[121] Zheng J, Petersen F, Yu X. The role of PTPN22 in autoimmunity: learning from mice.
Autoimmun Rev 2014;13:26671.
[122] Herman S, Fischer A, Pfatschbacher J, Hoffmann M, Steiner G. A TLR 9 antagonist diminishes arthritis severity in a rat model of rheumatoid arthritis. Ann Rheum Dis
2011;70:A39.
[123] Brentano F, Schorr O, Gay RE, Gay S, Kyburz D. RNA released from necrotic synovial
uid cells activates rheumatoid arthritis synovial broblasts via Toll-like receptor 3.
Arthritis Rheum 2005;52:265665.
[124] Roelofs MF, Joosten LA, Abdollahi-Roodsaz S, van Lieshout AW, Sprong T, van den
Hoogen FH, et al. The expression of toll-like receptors 3 and 7 in rheumatoid arthritis synovium is increased and costimulation of toll-like receptors 3, 4, and 7/8 results in synergistic cytokine production by dendritic cells. Arthritis Rheum 2005;
52:231322.
[125] Ospelt C, Brentano F, Rengel Y, Stanczyk J, Kolling C, Tak PP, et al. Overexpression of
toll-like receptors 3 and 4 in synovial tissue from patients with early rheumatoid
arthritis: toll-like receptor expression in early and longstanding arthritis. Arthritis
Rheum 2008;58:368492.
[126] Tamaki Y, Takakubo Y, Hirayama T, Konttinen YT, Goodman SB, Yamakawa M, et al.
Expression of Toll-like receptors and their signaling pathways in rheumatoid synovitis. J Rheumatol 2011;38:81020.
[127] Kilding R, Akil M, Till S, Amos R, Wineld J, Iles MM, et al. A biologically
important single nucleotide polymorphism within the toll-like receptor-4
gene is not associated with rheumatoid arthritis. Clin Exp Rheumatol 2003;
21:3402.
[128] Radstake TR, Franke B, Hanssen S, Netea MG, Welsing P, Barrera P, et al. The Tolllike receptor 4 Asp299Gly functional variant is associated with decreased rheumatoid arthritis disease susceptibility but does not inuence disease severity and/or
outcome. Arthritis Rheum 2004;50:9991001.
[129] Kuuliala K, Orpana A, Leirisalo-Repo M, Kautiainen H, Hurme M, Hannonen P, et al.
Polymorphism at position +896 of the Toll-like receptor 4 gene interferes with
rapid response to therapy in rheumatoid arthritis. Ann Rheum Dis 2006;65:
12413.
[130] Sanchez E, Orozco G, Lopez-Nevot MA, Jimenez-Alonso J, Martin J. Polymorphisms
of toll-like receptor 2 and 4 genes in rheumatoid arthritis and systemic lupus erythematosus. Tissue Antigens 2004;63:547.
[131] Jaen O, Petit-Teixeira E, Kirsten H, Ahnert P, Semerano L, Pierlot C, et al. No evidence of major effects in several Toll-like receptor gene polymorphisms in rheumatoid arthritis. Falgarone G; European Consortium on Rheumatoid Arthritis
Families. Arthritis Res Ther 2009;11:R5.
[132] Laska MJ, Hansen B, Troldborg A, Lorenzen T, Stengaard-Pedersen K, Junker P, et al.
A non-synonymous single-nucleotide polymorphism in the gene encoding Toll-like
Receptor 3 (TLR3) is associated with sero-negative rheumatoid arthritis (RA) in a
Danish population. BMC Res Notes 2014;7:716.
[133] Coenen MJ, Enevold C, Barrera P, Schijvenaars MM, Toonen EJ, Scheffer H, et al. Genetic variants in toll-like receptors are not associated with rheumatoid arthritis
susceptibility or anti-tumour necrosis factor treatment outcome. PLoS One 2010;
5 e14326.
[134] Etem EO, Elyas H, Ozgocmen S, Yldrm A, Godekmerdan A. The investigation of
toll-like receptor 3, 9 and 10 gene polymorphisms in Turkish rheumatoid arthritis
patients. Rheumatol Int 2011;31:136974.
[135] Dawidowicz K, Allanore Y, Guedj M, Pierlot C, Bombardieri S, Balsa A, et al. The interferon regulatory factor 5 gene confers susceptibility to rheumatoid arthritis and
inuences its erosive phenotype. Ann Rheum Dis 2011;70:11721.
[136] Kim YJ, Park JH, Kim I, Kim JO, Bae JS, Shin HD, et al. Putative role of functional interferon regulatory factor 5 (IRF5) polymorphism in rheumatoid arthritis in a Korean population. J Rheumatol 2008;35:210618.
[137] Maalej A, Hamad MB, Reba A, Teixeira VH, Bahloul Z, Marzouk S, et al. Association
of IRF5 gene polymorphisms with rheumatoid arthritis in a Tunisian population.
Scand J Rheumatol 2008;37:4148.
[138] Shimane K, Kochi Y, Yamada R, Okada Y, Suzuki A, Miyatake A, et al. A single nucleotide polymorphism in the IRF5 promoter region is associated with susceptibility
to rheumatoid arthritis in the Japanese population. Ann Rheum Dis 2009;68:
37783.
[139] Sacre SM, Andreakos E, Kiriakidis S, Amjadi P, Lundberg A, Giddins G, et al. The Tolllike receptor adaptor proteins MyD88 and Mal/TIRAP contribute to the inammatory and destructive processes in a human model of rheumatoid arthritis. Am J
Pathol 2007;170:51825.
[140] Kotzin BL. Systemic lupus erythematosus. Cell 1996;85:3036.
[141] Nakano S, Morimoto S, Suzuki J, Nozawa K, Amano H, Tokano Y, et al. Role of pathogenic auto-antibody production by Toll-like receptor 9 of B cells in active systemic
lupus erythematosus. Rheumatology (Oxford) 2008;47:1459.
[142] Rahman A, Isenberg D. Systemic lupus erythematosus. N Engl J Med 2008;358:
92939.
[143] Rnnblom L, Pascual V. The innate immune system in SLE: type I interferons and
dendritic cells. Lupus 2008;17:3949.
[144] Robinson ES, Werth VP. The role of cytokines in the pathogenesis of cutaneous
lupus erythematosus. Cytokine 2014;73:32634.
[145] Eichler E, Nickerson D, Altshuler D, Bowcock A, et al. Completing the map of human
genetics variation. Nature 2007;447:1615.
[146] Barrat FJ, Meeker T, Chan JH, Guiducci C, Coffman RL. Treatment of lupus-prone
mice with a dual inhibitor of TLR7 and TLR9 leads to reduction of autoantibody
production and amelioration of disease symptoms. Eur J Immunol 2007;37:
35826.
[147] Tabeta K, Hoebe K, Janssen EM, Du X, Georgel P, Crozat K, et al. The Unc93b1 mutation 3d disrupts exogenous antigen presentation and signaling via Toll-like receptors 3, 7 and 9. Nat Immunol 2006;7:15664.
E. Gianchecchi, A. Fierabracci / Autoimmunity Reviews 14 (2015) 971983
[148] Christensen SR, Shupe J, Nickerson K, Kashgarian M, Flavell RA, Shlomchik MJ. Tolllike receptor 7 and TLR9 dictate autoantibody specicity and have opposing inammatory and regulatory roles in a murine model of lupus. Immunol 2006;25:
41728.
[149] Santiago-Raber ML, Kikuchi S, Borel P, Uematsu S, Akira S, Kotzin BL, et al. Evidence
for genes in addition to Tlr7 in the Yaa translocation linked with acceleration of
systemic lupus erythematosus. J Immunol 2008;181:155662.
[150] Christensen SR, Kashgarian M, Alexopoulou L, Flavell RA, Akira S, Shlomchik MJ.
Toll-like receptor 9 controls anti-DNA autoantibody production in murine lupus. J
Exp Med 2005;202:32131.
[151] Kelley J, Johnson M, Alarcn G, Kimberly R, Edberg J. Variation in the relative copy
number of the TLR-7 gene in patients with systemic lupus erythematosus and
healthy control subjects. Arthritis Rheum 2007;56:33758.
[152] Rupasree Y, Naushad SM, Rajasekhar L, Uma A, Kutala VK. Association of TLR4
(D299G, T399I), TLR91486T N C, TIRAP S180L and TNF- promoter (-1031,
-863, -857) polymorphisms with risk for systemic lupus erythematosus among
South Indians. Lupus 2015;24:507.
[153] Devaraju P, Gulati R, Antony PT, Mithun CB, Negi VS. Susceptibility to SLE in South
Indian Tamils may be inuenced by genetic selection pressure on TLR2 and TLR9
genes. Mol Immunol 2015;64:1236.
[154] Wang CM, Chang SW, Wu YJ, Lin JC, Ho HH, Chou TC, et al. Genetic variations in
Toll-like receptors (TLRs 3/7/8) are associated with systemic lupus erythematosus
in a Taiwanese population. Sci Rep 2014;4:3792.
[155] Enevold C, Nielsen CH, Jacobsen RS, Hermansen ML, Molbo D, Avlund K, et al. Single
nucleotide polymorphisms in genes encoding toll-like receptors 7, 8 and 9 in Danish patients with systemic lupus erythematosus. Mol Biol Rep 2014;41:575563.
[156] Armstrong DL, Reiff A, Myones BL, Quismorio FP, Klein-Gitelman M, McCurdy D,
et al. Identication of new SLE-associated genes with a two-step Bayesian study
design. Genes Immun 2009;10:44656.
[157] Graham RR, Kozyrev SV, Baechler EC, Reddy MV, Plenge RM, Bauer JW, et al. A common haplotype of interferon regulatory factor 5 (IRF5) regulates splicing and expression and is associated with increased risk of systemic lupus erythematosus.
Nat Genet 2006;38:5505.
[158] Kelly JA, Kelley JM, Kaufman KM, Kilpatrick J, Bruner GR, Merrill JT, et al. Interferon
regulatory factor-5 is genetically associated with systemic lupus erythematosus in
African Americans. Genes Immun 2008;9:18794.
[159] Sigurdsson S, Gring HH, Kristjansdottir G, Milani L, Nordmark G, Sandling JK, et al.
Comprehensive evaluation of the genetic variants of interferon regulatory factor 5
(IRF5) reveals a novel 5 bp length polymorphism as strong risk factor for systemic
lupus erythematosus. Hum Mol Genet 2008;17:87281.
[160] Siu HO, Yang W, Lau CS, Chan TM, Wong RW, Wong WH, et al. Association of a haplotype of IRF5 gene with systemic lupus erythematosus in Chinese. J Rheumatol
2008;35:3602.
[161] Elghzaly AA, Metwally SS, El-Chennawi FA, Elgayaar MA, Mosaad YM, El-Toraby EE,
et al. IRF5, PTPN22, CD28, IL2RA, KIF5A, BLK and TNFAIP3 genes polymorphisms
and lupus susceptibility in a cohort from the Egypt Delta; relation to other ethnic
groups. Hum Immunol 2015 Jun 17. http://dx.doi.org/10.1016/j.humimm.2015.
06.001.
[162] Gabrielli A, Avvedimento EV, Krieg T. Scleroderma. N Engl J Med 2009;360:
19892003.
[163] Asano Y. Future treatments in systemic sclerosis. J Dermatol 2010;37:5470.
[164] Varga J, Abraham D. Systemic sclerosis: a prototypic multisystem brotic disorder. J
Clin Invest 2007;117:55767.
[165] Yamamoto T, Takagawa S, Katayama I, Yamazaki K, Hamazaki Y, Shinkai H, et al.
Animal model of sclerotic skin. I: Local injections of bleomycin induce sclerotic
skin mimicking scleroderma. J Invest Dermatol 1999;112:45662.
[166] Lehner T. Immunopathogenesis of Behet's disease. Ann Med Interne 1999;150:
4837.
[167] Yurdakul S, Hamuryudan V, Yazici H. Behet syndrome. Curr Opin Rheumatol
2004;16:3842.
[168] Karasneh J, Gl A, Ollier WE, Silman AJ, Worthington J. Whole-genome screening
for susceptibility genes in multicase families with Behet's disease. Arthritis
Rheum 2005;52:183642.
[169] Sakane T, Takeno M, Suzuki N, Inaba G. Behet's disease. N Engl J Med 1999;341:
128491.
[170] Melikoglu M, Uysal S, Krueger JG, Kaplan G, Gogus F, Yazici H, et al. Characterization
of the divergent wound-healing responses occurring in the pathergy reaction and
normal healthy volunteers. J Immunol 2006;177:641521.
[171] Takada Y, Fujita Y, Igarashi M, Katsumata T, Okabe H, Saigenji K, et al. Intestinal
Behet's disease-pathognomonic changes in intramucosal lymphoid tissues and effect of a rest cure on intestinal lesions. J Gastroenterol 1997;32:598604.
[172] Gl A. Behet's disease: an update on the pathogenesis. Clin Exp Rheumatol 2001;
19:S6S12.
[173] Zierhut M, Mizuki N, Ohno S, Inoko H, Gl A, Ono K, et al. Immunology and functional genomics of Behet's disease. Cell Mol Life Sci 2003;60:190322.
[174] Skin Anonymous, hypersensitivity to streptococcal antigens and the induction of
systemic symptoms by the antigens in Behcet's disease: a multicenter study,. The
Behcet's Disease Research Committee of Japan. J Rheumatol 1989;16:50611.
[175] Sezer FN. The isolation of a virus as the cause of Behcet's diseases. Am J Ophthalmol
1953;36:30115.
[176] Lee S, Bang D, Cho YH, Lee ES, Sohn S. Polymerase chain reaction reveals herpes
simplex virus DNA in saliva of patients with Behcet's disease. Arch Dermatol Res
1996;288:17983.
[177] Ohashi K, Burkart V, Floh S, Kolb H. Cutting edge: heat shock protein 60 is a putative endogenous ligand of the toll-like receptor-4 complex. J Immunol 2000;164:
55861.
983
[178] Vabulas RM, Ahmad-Nejad P, da Costa C, Miethke T, Kirschning CJ, Hcker H, et al.
Endocytosed HSP60s use toll-like receptor 2 (TLR2) and TLR4 to activate the toll/
interleukin-1 receptor signaling pathway in innate immune cells. J Biol Chem
2001;276:313329.
[179] Poss KD, Tonegawa S. Reduced stress defense in heme oxygenase 1-decient cells.
Proc Natl Acad Sci U S A 1997;94:1092530.
[180] Yachie A, Niida Y, Wada T, Igarashi N, Kaneda H, Toma T, et al. Oxidative stress
causes enhanced endothelial cell injury in human heme oxygenase-1 deciency.
J Clin Invest 1999;103:12935.
[181] Liu X, Wang C, Ye Z, Kijlstra A, Yang P. Higher expression of Toll-like receptors 2, 3,
4, and 8 in ocular Behcet's disease. Invest Ophthalmol Vis Sci 2013;54:60127.
[182] Ito A, Ota M, Katsuyama Y, Inoko H, Ohno S, Mizuki N. Lack of association of Tolllike receptor 9 gene polymorphism with Behet's disease in Japanese patients. Tissue Antigens 2007;70:4236.
[183] Ben Dhifallah I, Lachheb J, Houman H, Hamzaoui K. Toll-like-receptor gene polymorphisms in a Tunisian population with Behet's disease. Clin Exp Rheumatol
2009;27:S5862.
[184] Boiardi L, Atzeni F, Casali B, Farnetti E, Nicoli D, Pipitone N, et al. Toll-like receptor 4
(TLR4) gene polymorphisms in Italian patients with Behet's disease. Clin Exp
Rheumatol 2009;27:S437.
[185] Durrani O, Banahan K, Sheedy FJ, McBride L, Ben-Chetrit E, Greiner K, et al. TIRAP
Ser180Leu polymorphism is associated with Behcet's disease. Rheumatology (Oxford) 2011;50:17605.
[186] Fang J, Hu R, Hou S, Xiang Q, Qi J, Zhou Y, et al. Association of TLR2 gene polymorphisms with ocular Behcet's disease in a Chinese Han population. Invest
Ophthalmol Vis Sci 2013;54:838492.
[187] Fang J, Chen L, Tang J, Hou S, Liao D, Ye Z, et al. Association between copy number
variations of TLR7 and ocular Behet's disease in a Chinese Han population. Invest
Ophthalmol Vis Sci 2015;56:151723.
[188] Geremia A, Biancheri P, Allan P, Corazza GR, Di Sabatino A. Innate and adaptive immunity in inammatory bowel disease. Autoimmun Rev 2014;13:310.
[189] Browning BL, Huebner C, Petermann I, Gearry RB, Barclay ML, Shelling AN, et al. Has
toll-like receptor 4 been prematurely dismissed as an inammatory bowel disease
gene? Association study combined with meta-analysis shows strong evidence for
association. Am J Gastroenterol 2007;102:250412.
[190] De Jager PL, Franchimont D, Waliszewska A, Bitton A, Cohen A, Langelier D. The role
of the Toll receptor pathway in susceptibility to inammatory bowel diseases.
Genes Immun 2007;8:38797.
[191] Hong J, Leung E, Fraser AG, Merriman TR, Vishnu P, Krissansen GW. TLR2, TLR4 and
TLR9 polymorphisms and Crohn's disease in a New Zealand Caucasian cohort. J
Gastroenterol Hepatol 2007;22:17606.
[192] Hume GE, Fowler EV, Doecke J, Simms LA, Huang N, Palmieri O, et al. Novel NOD2
haplotype strengthens the association between TLR4 Asp299Gly and Crohn's disease in an Australian population. Inamm Bowel Dis 2008;14:58590.
[193] Abad C, Gonzlez-Escribano MF, Diaz-Gallo LM, Lucena-Soto JM, Mrquez JL, Leo E,
et al. Association of Toll-like receptor 10 and susceptibility to Crohn's disease independent of NOD2. Genes Immun 2011;12:63542.
[194] Morgan AR, Lam WJ, Han DY, Fraser AG, Ferguson LR. Genetic variation within TLR10
is associated with Crohn's disease in a New Zealand population. Hum Immunol 2012;
7:41620.
[195] Meena NK, Ahuja V, Meena K, Paul J. Association of TLR5 gene polymorphisms in
ulcerative colitis patients of north India and their role in cytokine homeostasis.
PLoS One 2015;10:e0120697.
[196] Trapp BD, Nave KA. Multiple sclerosis: an immune or neurodegenerative disorder?
Annu Rev Neurosci 2008;31:24769.
[197] Hasheminia SJ, Zarkesh-Esfahani SH, Tolouei S, Shaygannejad V, Shirzad H,
Hashemzadeh Chaleshtory M. Toll like receptor 2 and 4 expression in peripheral
blood mononuclear cells of multiple sclerosis patients. Iran J Immunol 2014;11:
7483.
[198] Kovacs SO. Vitiligo. J Am Acad Dermatol 1998;38:64766.
[199] Spritz RA. Modern vitiligo genetics sheds new light on an ancient disease. J
Dermatol 2013;40:3108.
[200] Cavalcante P, Cu P, Mantegazza R, Berrih-Aknin S, Bernasconi P, Le Panse R. Etiology of myasthenia gravis: innate immunity signature in pathological thymus.
Autoimmun Rev 2013;12:86374.
[201] Marx A, Pster F, Schalke B, Saruhan-Direskeneli G, Melms A, Strbel P. The different roles of the thymus in the pathogenesis of the various myasthenia gravis subtypes. Autoimmun Rev 2013;12:87584.
[202] Ning S. Innate immune modulation in EBV infection. Herpesviridae 2011;2:1.
[203] Cu P, Dragin N, Weiss JM, Martinez-Martinez P, Roussin R, Berrih Aknin S, et al.
Implication of dsRNA signaling in the etiology of autoimmune myasthenia gravis.
Ann Neurol 2013;73:28193.
[204] Temajo NO, Howard N. The mosaic of environment involvement in autoimmunity:
the abrogation of viral latency by stress, a non-infectious environmental agent, is
an intrinsic prerequisite prelude before viruses can rank as infectious environmental agents that trigger autoimmune diseases. Autoimmun Rev 2014;13:63540.
[205] Zhu J, Mohan C. Toll-like receptor signaling pathways-therapeutic opportunities.
Mediators Inamm 2010;2010:781235.
[206] Horton CG, Pan ZJ, Farris AD. Targeting Toll-like receptors for treatment of SLE. Mediators Inamm 2010;2010.
[207] Johar AS, Anaya JM, Andrews D, Patel HR, Field M, Goodnow C, et al. Candidate gene
discovery in autoimmunity by using extreme phenotypes, next generation sequencing and whole exome capture. Autoimmun Rev 2015;14:2049.
Das könnte Ihnen auch gefallen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5795)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1091)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- USMLE Road Map ImmunologyDokument242 SeitenUSMLE Road Map ImmunologyFernanda Granillo100% (9)
- In Ammation in Heart Failure: JACC State-of-the-Art ReviewDokument17 SeitenIn Ammation in Heart Failure: JACC State-of-the-Art ReviewAhmad FauzanNoch keine Bewertungen
- Toll Like Receptors and Their LigandsDokument21 SeitenToll Like Receptors and Their Ligandsakash_81087Noch keine Bewertungen
- Damps, Pamps, and Lamps in Immunity and Sterile InflammationDokument26 SeitenDamps, Pamps, and Lamps in Immunity and Sterile InflammationCony G100% (1)
- Sleep Health Reciprocal Regulation of Sleep and Innate ImmunityDokument27 SeitenSleep Health Reciprocal Regulation of Sleep and Innate ImmunityPolly MollyNoch keine Bewertungen
- Novel Aspects of Pharmacological Therapies For Acute Renal FailureDokument16 SeitenNovel Aspects of Pharmacological Therapies For Acute Renal FailureproluvieslacusNoch keine Bewertungen
- Role of Progesterone in Tlr4-Myd88-Dependent Signaling Pathway in Pre-EclampsiaDokument5 SeitenRole of Progesterone in Tlr4-Myd88-Dependent Signaling Pathway in Pre-EclampsiaCarl Enrique PSNoch keine Bewertungen
- Asst - Prof. Meroj A. Jasem Ph.D. Student Molecular Immunology CourseDokument26 SeitenAsst - Prof. Meroj A. Jasem Ph.D. Student Molecular Immunology CourseahmadNoch keine Bewertungen
- The Immunological Basis of The Hygiene HypothesisDokument19 SeitenThe Immunological Basis of The Hygiene HypothesisRoxana Alarcón VásquezNoch keine Bewertungen
- Once The Barrier Is Breached How Are Pathogens Detected and Dealt With?Dokument64 SeitenOnce The Barrier Is Breached How Are Pathogens Detected and Dealt With?Seyeon Clare LeeNoch keine Bewertungen
- 18225-Article Text-81558-1-10-20170301 PDFDokument274 Seiten18225-Article Text-81558-1-10-20170301 PDFMuhammad Tariq RazaNoch keine Bewertungen
- Structure and Function of Joints PDFDokument53 SeitenStructure and Function of Joints PDFABHAY KUMARNoch keine Bewertungen
- Autoimmunity Reviews: Maximiliano Javier Jiménez-Dalmaroni, M. Eric Gerswhin, Iannis E. AdamopoulosDokument8 SeitenAutoimmunity Reviews: Maximiliano Javier Jiménez-Dalmaroni, M. Eric Gerswhin, Iannis E. AdamopoulosTeodor CabelNoch keine Bewertungen
- Shinjita Das M.D., Rachel Reynolds M.D. (Auth.), Joshua Zeichner (Eds.) - Acneiform Eruptions in Dermatology - A Differential Diagnosis-Springer-Verlag New York (2014) PDFDokument405 SeitenShinjita Das M.D., Rachel Reynolds M.D. (Auth.), Joshua Zeichner (Eds.) - Acneiform Eruptions in Dermatology - A Differential Diagnosis-Springer-Verlag New York (2014) PDFMaryNoch keine Bewertungen
- Pgs 145-59, Neonatal Immunity by Constantin Bona (Humana Press) 2004 - $145.00Dokument401 SeitenPgs 145-59, Neonatal Immunity by Constantin Bona (Humana Press) 2004 - $145.00Riki TobingNoch keine Bewertungen
- MorphineDokument13 SeitenMorphineAli Sayed100% (2)
- Antiphospholipid Syndrome - From Pathogenesis To Novel Immunomodulatory TherapiesDokument6 SeitenAntiphospholipid Syndrome - From Pathogenesis To Novel Immunomodulatory TherapiesardirshajiNoch keine Bewertungen
- Presepsin 6Dokument189 SeitenPresepsin 6donkeyendutNoch keine Bewertungen
- From Pathogenesis of Acne Vulgaris To Anti-Acne AgentsDokument13 SeitenFrom Pathogenesis of Acne Vulgaris To Anti-Acne AgentsNazihan Safitri AlkatiriNoch keine Bewertungen
- Yang 2017Dokument10 SeitenYang 2017wendyNoch keine Bewertungen
- IL1 AntagonistaDokument13 SeitenIL1 AntagonistaZitlal-lin VictoriaNoch keine Bewertungen
- Acellular CarbsDokument15 SeitenAcellular CarbsstarmittNoch keine Bewertungen
- First French-Argentine Immunology Congress, 2010 Abstracts Held On Buenos Aires, Argentina, 2nd-5th November, 2010Dokument105 SeitenFirst French-Argentine Immunology Congress, 2010 Abstracts Held On Buenos Aires, Argentina, 2nd-5th November, 2010International Medical PublisherNoch keine Bewertungen
- Vaccinium Meridionale y AspirinaDokument58 SeitenVaccinium Meridionale y AspirinaMaria Elena MaldonadoNoch keine Bewertungen
- Shao 2019Dokument8 SeitenShao 2019Muhamad Akbar NamusyNoch keine Bewertungen
- Pathogenicity and Innate Response To Avibacterium Paragallinarum in ChickensDokument9 SeitenPathogenicity and Innate Response To Avibacterium Paragallinarum in ChickensJosXe CalderonNoch keine Bewertungen
- Nutraceuticos Na H PiloryDokument16 SeitenNutraceuticos Na H PiloryflaviaNoch keine Bewertungen
- Russel J. Reiter Pedro Abreu-Gonzalez Alberto Dominguez-RodriguezDokument80 SeitenRussel J. Reiter Pedro Abreu-Gonzalez Alberto Dominguez-RodriguezFilipos ConstantinNoch keine Bewertungen
- Immunity To Fungi: Tobias M Hohl, Amariliz Rivera and Eric G PamerDokument8 SeitenImmunity To Fungi: Tobias M Hohl, Amariliz Rivera and Eric G PamerPieralessandro LasalviaNoch keine Bewertungen
- Toll Like ReceptorsDokument15 SeitenToll Like ReceptorsAdyas AdrianaNoch keine Bewertungen