Beruflich Dokumente
Kultur Dokumente
Postpartum Issues
Hochgeladen von
RosemaryCastroCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Postpartum Issues
Hochgeladen von
RosemaryCastroCopyright:
Verfügbare Formate
Maternal and Child Health Nursing
Postpartum
MATERNAL and CHILD HEALTH NURSING
POSTPARTUM
Lecturer: Mark Fredderick R. Abejo RN, MAN
_____________________________________________________________________________
.
I.
PHYSIOLOGICAL MATERNAL CHANGES
A. LOCHIA discharge from the uterus during the first 3 weeks after delivery.
Increasing Lochia as the day passes by may indicate Heparin Intoxication.
LOCHIAL CHANGES
LOCHIA RUBRA
Dark red discharge occurring in the first 2-3 days.
Contains epithelial cells, erythrocytes and decidua.
Characteristic human odor.
LOCHIA SEROSA
Pinkish to brownish discharge occurring 3-10 days after delivery.
Serosanguineous discharge containing decidua, erythrocytes, leukocytes, cervical mucus and
microorganisms.
Has a strong odor.
LOCHIA ALBA
Almost colorless to creamy yellowish discharge occurring from 10 days to 3 weeks after delivery.
Contains leukocytes, decidua,epithelial cells, fat, cervical mucus, cholesterol crystals, and bacteria.
Has no odor.
B. UTERUS
MCHN
Process of involution takes 4-6 weeks to complete.
Weight decreases from 2 lbs to 2 oz.
Fundus steadily descends into true pelvis; Fundal height decreases about 1 fingerbreadth (1 cm)/day; by
10-14 days postpartum, cannot be palpated abdominally.
Abejo
Maternal and Child Health Nursing
Postpartum
C. Uterine Involution
1. Description
a. The rapid decrease in the size of the uterus as it returns to the nonpregnant state
b. Clients who breastfeed may experience a more rapid involution
2. Assessment
a. Weight of the uterus decreases from 2 pounds
to 2 ounces in 6 week
b. Endometrium regenerates
c. Fundus steadily descends into the pelvis
d. Fundal height decreases about 1 fingerbreadth (1 cm) per day
E. By 10 days postpartum, uterus cannot be palpated abdominally
NOTE: Deviation of the fundus to the right or left and location of the fundus above the umbilical are signs that the
bladder is distended
NOTE: Height of the Umbilicus on the First Postpartum Day
The height is usually SLIGHTLY below the umbilicus about 24 hours after delivery. The top of the umbilicus is
normally MIDWAY between the umbilicus and the symphysis pubis.
D. Breasts
1. Breasts continue to secrete colostrum
2. A decrease in estrogen and progesterone levels after delivery stimulates increased prolactin levels, which
promote breast milk production.
3. Breasts become distended with milk on the third day
4. Engorgement occurs in 48 to 72 hours in non breast feeding mothers.
NOTE:
Bradycardia is a normal physiologic change for 6-10 days postpartum
E. Gastrointestinal tract
1. Women are usually very hungry after delivery
2. Constipation can occur
3. Hemorrhoids are common
II.
POSTPARTUM NURSING INTERVENTIONS
Monitor Vital Signs
NOTE: Maternal temperature during the first 24 hours following delivery may rise to 100. 4` F (38`C) as a
result of dehydration. The nurse can reassure the new mother that these symptoms are normal.
Postpartum Exercise
Supine Position with the knees flexed, and then inhale deeply while allowing the abdomen to expand and
exhale while contracting the abdominal muscles. The purpose of this exercise is to strengthen the
abdominal muscles. Examples are reaching for the knees; push ups and sits ups on the first postpartum
day.
Assess height, consistency, and location of the fundus
Monitor color, amount, and odor of lochia
Assess lochia and color volume
Give RhoGAM to mother if ordered. RhoGAM promotes lysis of fetal Rh (+) RBCs.
Administer RhoGam as prescribed within 72 hours postpartum to the Rh-negative client who has given
birth to an Rh-positive neonate.
Rhogam (D) immune globulin is given by intramuscular injection
Check episiotomy and perineum for signs of infection.
Promote successful feeding.
Non-nursing woman- tight bra for 72 hours, ice packs, minimizes breast stimulation.
Nursing woman- success depends on infant sucking and maternal production of milk.
Postpartum Blues (3-7 days) Normal occurrence of roller coaster emotions
MCHN
Abejo
Maternal and Child Health Nursing
Postpartum
Sexual activities- abstain from intercourse until episiotomy is healed and lochia ceased
around 3-4 weeks. Remind that Assess height, consistency, and location of the fundus
breastfeeding
does not give adequate protection.
Assess breasts for engorgement
Monitor episiotomy for healing ( assess dehiscence & evisceration)
Assess incisions or dressings of cesarean birth client ( prone to infection)
Monitor bowel status ( prone to constipation)
Monitor I &0
Encourage frequent voiding (prevent urinary retention which will predispose the mother to uterus
displacement & infection)
Encourage ambulation ( to prevent thromboplebitis & paralytic ileus
Assess bonding with the newborn infant ( to prevent failure to thrive)
NOTE:
A positive bonding experience is indicated when the mother turns her face toward the baby to initiate eye-to-eye
contact. Observation of new mothers has shown that a fairly regular pattern of maternal behaviors is exhibited at
first contact with the newborn. The mother follows a progression of touching activities from fingertip exploration
toward palmar contact to enfolding the infant with the whole hand and arm. The mother also increase the time
spent in the en face position. The mother arranges herself or the newborn so that her face and eyes are in the same
plane as in her infant.
III.
POSTPARTUM DISCOMFORTS
A. Perineal discomfort
Apply ice packs to the perineum during the first 24 hours to reduce swelling after the first 24 hours, apply
warmth by sitz baths
B. Episiotomy
1. Instruct the client to administer perineal care after each voiding
2. Encourage the use of an analgesic spray as prescribed
3. Administer analgesics as prescribed if comfort measures are unsuccessful
C. Breast discomfort
PREVENTION:
The BEST PREVENTION TECHNIQUE IS TO EMPTY THE BREST REGULARLY AND FREQUENTLY
WITH FEEDINGS. The 2nd is EXPRESSING A LITTLE MILK BEFORE NURSING, MASSAGING THE BREASTS
GENTLY OR TAKING A WARM SHOWER BEFORE FEEDING MAY HELP TO IMPROVE MILK FLOW. Placing
as much of the areola as possible into the neonates mouth is one method. Other methods include changing position
with each nursing so that different areas of the nipples receive the greatest stress from nursing and avoiding breast
engorgement, which make I difficult for the neonate to grasp. In addition, nursing more frequently, so that a
ravenous neonate is not sucking vigorously at the beginning of the feedings, AND FEEDING ON DEMAND to
prevent over hunger is helpful. AIRDRYING THE NIPPLES AND EXPOSING THEM TO THE LIGHT HAVE ALSO
BEEN RECOMMENDED. Warm Tea bags, which contain tannic acid also, will sooth soreness. WEARING A
SUPPORTIVE BRASSIERE DOES NOT PREVENT BREAST ENGORGEMENT. APPLYING ICE and LANOLIN
DOES NOT RELIEVE BREAST ENGORGEMENT.
MCHN
Abejo
Maternal and Child Health Nursing
Postpartum
INTERVENTION:
Measures that help relieve nipple soreness in a breast-feeding client include lubricating the nipples with a
few drops of expressed milk before feedings, applying ice compresses just before feedings, letting the nipples air dry
after feedings, and avoiding the use of soap on the nipples.
NOTE: Specific nursing care for breast Engorgement
1. Breastfeed frequently
2. Apply warm packs before feeding
3. Apply ice packs between feedings
NOTE: Specific Nursing Care for Cracked nipples
1. Expose nipples to air for 10 to 20 minutes after feeding
2. Rotate the position of the baby for each feeding
3. Be sure that the baby is latched on to the areola, not just the nipple
NOTE: Do not use soap on the breasts, as it tends to remove natural oils, which increases the chance of cracked
nipples
IV.
A.
POST PARTUM COMPLICATIONS
HEMORRHAGE
CAUSES
The #1 cause of POSTPARTUM
HEMORRHAGE IS RETAINED
PLACENTAL FRAGMENTS.
Uterine atony and vaginal &
cervical tears are associated with
early postpartum hemorrhage
The #2 cause is OVERDISTENTION OF THE UTERUS
from more than (10) pounds,
OTHERS ARE: 4000 gms,
neonate, excessive oxytocin use,
Polyhydramnios and Placental
Disorders.
You should assess for uterine
atony after a c-section delivery.
This is more common after a csection than after a vaginal
delivery.
SIGNS OF HEMORRHAGE
Boggy uterus (does not
respond to massage)
A boggy uterus would be
palpable above the umbilicus and
would be soft and poorly
contracted.
Abnormal
clots
unusual
pelvic discomfort or headache
Excessive
or
bright-red
bleeding
Signs of shock
Early Hemorrhage starts on the
first 24 hours, or more than 500
ml of blood on the first 24 hrs in
a Normal spontaneous delivery..
MANAGEMENT
Fluid replacement
Emergency lay
Oxygen
Vital signs
Perineal pad count
Psychological support
Massaging the lower abdomen
after delivery is done to maintain
a firm uterus, which will aid in
the clumping down of blood
vessels in the uterus, thereby
preventing any further bleeding.
BOGGY UTERUS
Uterine atony means that the
uterus is not firm or it is not
contracting. The nurse should
gently massage the uterus which
will contract the uterus and make
it firm. Clients who are
predisposed are usually
MULTIPLE GESTATION,
POLYHYDRAMNIOS,
PROLONGED LABOR and LGA
(LARGE GESTATIONAL AGE
fetus.
B. THROMBOPLEBITIS
Inflammation of the vein caused by a clot
The positive Homans sign indicate is possibility of thrombophlebitis or a deep venous thrombosis that is
present in the lower extremities.
When assessing for Homans sign ask the patient to stretch her kegs out with the knee slightly flexed while
dorsiflex the foot. A positive sign is present when pain is felt at the back of the knee or calf. It is normal for a
patient on magnesium sulfate to feel tired because it acts as a central nervous depressant and often makes the
patient drowsy.
MCHN
Abejo
Maternal and Child Health Nursing
Postpartum
MANIFESTATION
Edematous extremities
Fever with chills
Pain and redness in affected
area
Positive Homans sign
MANAGEMENT
Preventive
CURATIVE
Immobilize extremity
Analgesics
Anticoagulant
Thrombolytics
MANIFESTATION
Fever
Chills
Poor appetite
General body malaise
Abdominal pain
Foul-smelling lochia
MANAGEMENT
Antibiotics
Oxytocin
Analgesics
Maintain hygiene
Semi-fowlers positions
Vital signs
Early ambulations
Assess lochia
C. INFECTION
PREDISPOSING FACTORS
Rupture of membranes over
24 hours before delivery
Retained placental
fragments
Internal fetal monitoring
Vaginal infection
Puerperial infection is an
infection of the genital tract.
Bright red blood is a normal
Early signs and symptoms of
puerperial infection include
chills, fever, and flu-like
symptoms. It can occur up to one
month after delivery.
lochial finding in the first 24
hours after delivery. Lochia
should never contain large clots,
tissue fragments, or membranes.
A foul odor may signal infection,
as may absence of lochia.
D. MASTITIS
MCHN
Abejo
Maternal and Child Health Nursing
Postpartum
ASSESSMENT
Elevated temperature, chills,
general aching, malaise and
localized pain
Engorgement, hardness and
reddening of the breasts
Nipple soreness and fissures
Inflammation of the breast as a
result of infection
Primarily seen in breastfeeding
mothers 2 to 3 weeks after
delivery but may occur at any
time during lactation
MANAGEMENT
Instruct the mother in good hand washing and breast
hygiene techniques
Apply heat or cold to site as prescribed
Maintain lactation in breastfeeding mothers
Encourage manual expression of breast milk or use
of breast pump every 4 hours
Encourage mother to support, breasts by wearing a
supportive bra
Administer analgesics & antibiotics as prescribed
E. Postpartum Mood Disorders
MOOD DISORDERS
Postpartum Blues
Postpartum Depression
Normal processes during
postpartum include the withdrawal
of progesterone and estrogen and
lead to the psychological response
known as "the blues."
Postpartum depression is a
psychiatric problem that occurs
later in postpartum and is
characterized by more severe
symptoms of inadequacy.
Because the client's behavior is
normal, notifying her physician and
conducting a home assessment
aren't necessary.
Postpartum Psychosis
ASSESSMENT
Onset: 1-10 days postpartum lasting 2 weeks or less
Fatigue
Weeping anxiety
Mood instability
Onset: 3-5 days lasting more than 2 weeks
Confusion
Fatigue
Agitation
Feeling of hopelessness and shame let down feeling
Alterations in mood roller coaster emotions
Appetite and sleep disturbance
According to Rubin, dependence and passivity are typical during the takingin period, which may last up to 3 days after delivery. A client experiencing
postpartum depression demonstrates anxiety, confusion, or other signs and
symptoms consistently. Maternal role attainment occurs over 3 to 10 months.
Attachment also is an ongoing process that occurs gradually.
Onset: 3-5 days postpartum
Symptoms of depression plus delusions
Auditory hallucinations
Hyperactivity
POSTPARTUM WARNING S/S TO REPORT TO THE PHYSICIAN
Increased bleeding, clots or passage of tissue.
Bright red vaginal bleeding anytime after birth.
Pain greater than expected.
Temperature elevation to 100.4 F.
Feeling of full bladder accompanied by inability to void.
Enlarging hematoma.
Feeling restless accompanied by pallor; cool, clammy skin; rapid HR; dizziness; and visual disturbance.
Pain, redness, and warmth accompanied by a firm area in the calf.
Difficulty breathing, rapid heart rate, chest pain, cough, feeling of apprehension, pale, cold, or blue skin
color
MCHN
Abejo
Maternal and Child Health Nursing
Postpartum
V.
Psychological Adaptation
Psychological Adaptation
Taking-in Phase
Taking-hold Phase
Letting-Go
Postpartum blues: overwhelming sadness
Postpartum depression
Postpartum Psychoses
Rubin's Postpartum Phases of Regeneration (POSTPARTUM PSYCHOSOCIAL ADAPTATION)
TAKING IN PHASE (DEPENDENT) First 3 Days
During this time, food and sleep are a major focus for the client. In addition, she works through the birth
experience to sort out reality from fantasy and to clarify any misunderstandings. This phase lasts 1 to 3 days after
birth. The primary concern is to meet her own needs.
Takes place 1-2 days postpartum
Mother is passive and dependent; concerned with own needs.
Verbalizes about the delivery experience.
Sleep/food important.
Mother focuses on her own primary needs, such as sleep and food
Important for the nurse to listen and to help the mother interpret the events of delivery to make them more
meaningful
Not an optimum time to teach the mother about baby care
TAKING HOLD PHASE (DEPENDENT/INDEPENDENT)
The client is concerned regarding her need to resume control of all facets of her life in a competent manner. At this
time, she is ready to learn self-care and infant care skills.
3-10 days postpartum
Mother strives for independence and begins to reassert herself.
Mood swings occur. May cry for no reason.
Maximal stage of learning readiness.
Mother requires reassurance that she can perform tasks of motherhood.
Begins to assume the tasks of mothering
An optimum time to teach the mother about baby care.
LETTING GO PHASE (INTERDEPENCE)
MCHN
10 to 6 weeks postpartum
Realistic regarding role transition.
Shows pattern of life-style that includes the new baby but still focuses on entire family as a unit.
Accepts baby as separate person.
Mother may feel deep loss over separation of the baby from part of the body and may grieve over the loss
Mother may be caught in a dependent/independent role, wanting to feel safe and secure yet wanting to
make decisions
Teenage mothers need special consideration because of the conflict taking place within them as part of
adolescence
Abejo
Das könnte Ihnen auch gefallen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Manual For Documenting Diagnosis in Per-Pd 301 - 2013 PDFDokument33 SeitenManual For Documenting Diagnosis in Per-Pd 301 - 2013 PDFNeeta AnandaNoch keine Bewertungen
- Healthcare Stats - Assignment #2Dokument6 SeitenHealthcare Stats - Assignment #2erickgregs0% (1)
- EliteSchedule16 17mar172017 PDFDokument1 SeiteEliteSchedule16 17mar172017 PDFRosemaryCastroNoch keine Bewertungen
- Hormonal Physiology of Childbearing PDFDokument248 SeitenHormonal Physiology of Childbearing PDFRosemaryCastro100% (1)
- FREESchool Supply LabelsDokument1 SeiteFREESchool Supply LabelsRosemaryCastroNoch keine Bewertungen
- OB ReviewDokument257 SeitenOB ReviewRosemaryCastro100% (1)
- Hormonal Physiology of Childbearing PDFDokument248 SeitenHormonal Physiology of Childbearing PDFRosemaryCastro100% (1)
- ABG ROME FlowchartDokument1 SeiteABG ROME FlowchartRosemaryCastro100% (1)
- IV Solutions CheatsheetDokument1 SeiteIV Solutions CheatsheetRosemaryCastroNoch keine Bewertungen
- PHN SAMPLE AppDokument3 SeitenPHN SAMPLE AppRosemaryCastroNoch keine Bewertungen
- NRP GeneralDokument1 SeiteNRP GeneralRosemaryCastroNoch keine Bewertungen
- SIM Lab Sign UpsDokument3 SeitenSIM Lab Sign UpsRosemaryCastroNoch keine Bewertungen
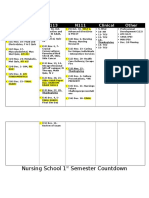
- And The School Bell Rings For Spring 16: Welcome To Second Semester!Dokument4 SeitenAnd The School Bell Rings For Spring 16: Welcome To Second Semester!RosemaryCastroNoch keine Bewertungen
- Monthly Shot January 2016Dokument7 SeitenMonthly Shot January 2016RosemaryCastroNoch keine Bewertungen
- Where Have I Been While in NURSING SCHOOL?: Résumé Worksheet Belonging To - Save MeDokument2 SeitenWhere Have I Been While in NURSING SCHOOL?: Résumé Worksheet Belonging To - Save MeRosemaryCastroNoch keine Bewertungen
- National Travel Fund Application1Dokument2 SeitenNational Travel Fund Application1RosemaryCastroNoch keine Bewertungen
- Club Agreement FormDokument4 SeitenClub Agreement FormRosemaryCastroNoch keine Bewertungen
- Chlamydia: California Department of Public HealthDokument12 SeitenChlamydia: California Department of Public HealthRosemaryCastroNoch keine Bewertungen
- N144 Peer Evaluation Rosemary CastroDokument2 SeitenN144 Peer Evaluation Rosemary CastroRosemaryCastroNoch keine Bewertungen
- Team #: 2 Names of Health Education Project Group Members Who Worked On This In-Class Activity: Rosemary Castro, Lachelle Manalo ObjectivesDokument2 SeitenTeam #: 2 Names of Health Education Project Group Members Who Worked On This In-Class Activity: Rosemary Castro, Lachelle Manalo ObjectivesRosemaryCastroNoch keine Bewertungen
- Nursing School Weeks 9-16Dokument2 SeitenNursing School Weeks 9-16RosemaryCastroNoch keine Bewertungen
- Smith - Et - Al-2020-Cochrane - Database - of - Systematic - Reviews - ARTIGO 4 JACKDokument118 SeitenSmith - Et - Al-2020-Cochrane - Database - of - Systematic - Reviews - ARTIGO 4 JACKJackelineNoch keine Bewertungen
- Vacuum Extraction Is An Artificial LaborDokument6 SeitenVacuum Extraction Is An Artificial LaborYuriko_L7Noch keine Bewertungen
- Pain Management Plan MCN 314Dokument3 SeitenPain Management Plan MCN 314claudette1882Noch keine Bewertungen
- Unassisted Childbirth: From Primitive To Its RiseDokument4 SeitenUnassisted Childbirth: From Primitive To Its RiseLorenz Sagayaga ListaNoch keine Bewertungen
- Anti Hospital Detention Bill BGHMC PresentationDokument9 SeitenAnti Hospital Detention Bill BGHMC PresentationVenus PangilinanNoch keine Bewertungen
- Salima Ikram, Jessica Kaiser, Roxie Walker - Egyptian Bioarchaeology - Humans, Animals, and The Environment-Sidestone Press (2015) PDFDokument252 SeitenSalima Ikram, Jessica Kaiser, Roxie Walker - Egyptian Bioarchaeology - Humans, Animals, and The Environment-Sidestone Press (2015) PDFArkava DasNoch keine Bewertungen
- Prevalence of Maternal Mortality Rate in (CHC) Safana WardDokument44 SeitenPrevalence of Maternal Mortality Rate in (CHC) Safana WardUsman Ahmad TijjaniNoch keine Bewertungen
- Prevalence and Factors Associated With Hypertension in Pregnancy Among Pregnant Women Attending Fort Portal Regional Referral Hospital in UgandaDokument10 SeitenPrevalence and Factors Associated With Hypertension in Pregnancy Among Pregnant Women Attending Fort Portal Regional Referral Hospital in UgandaKIU PUBLICATION AND EXTENSIONNoch keine Bewertungen
- Obstetric HDU and ICU: Guidelines ForDokument52 SeitenObstetric HDU and ICU: Guidelines ForsidharthNoch keine Bewertungen
- Determinan Keteraturan Kunjungan Masa Nifas Di Puskesmas Topore Kabupaten MamujuDokument5 SeitenDeterminan Keteraturan Kunjungan Masa Nifas Di Puskesmas Topore Kabupaten MamujuEka NursafitriNoch keine Bewertungen
- Republic Act No. 8187Dokument4 SeitenRepublic Act No. 8187mitsune21100% (1)
- Uterine MalformationsDokument14 SeitenUterine Malformationsmercy100% (2)
- Ilocano Folk BeliefsDokument7 SeitenIlocano Folk BeliefsMark Anthony InocencioNoch keine Bewertungen
- Nursing Bullets (Obstetrics & Gynaecology)Dokument17 SeitenNursing Bullets (Obstetrics & Gynaecology)RF RFNoch keine Bewertungen
- Imma Rswp-Final WebDokument94 SeitenImma Rswp-Final WebvivekpattniNoch keine Bewertungen
- LOVEYOURCONTENTSTDPregnancyStudentWorkbook PDFDokument24 SeitenLOVEYOURCONTENTSTDPregnancyStudentWorkbook PDFChlodette Eizl M. Laurente100% (1)
- 002 POS Format 1Dokument9 Seiten002 POS Format 1Roland Philip GoNoch keine Bewertungen
- Qulity Management of Health Facility: Project ProposalDokument12 SeitenQulity Management of Health Facility: Project ProposalRaksa RaNoch keine Bewertungen
- Pharmacologic Class: Ergot Alkaloid Therapeutic Class: Oxytocic Pregnancy Risk Category CDokument6 SeitenPharmacologic Class: Ergot Alkaloid Therapeutic Class: Oxytocic Pregnancy Risk Category CayotanNoch keine Bewertungen
- ANC RVUC 2nd Draft CommentedDokument20 SeitenANC RVUC 2nd Draft CommentedFantaNoch keine Bewertungen
- Minggu 1 (Terminology in Clinical Setting)Dokument13 SeitenMinggu 1 (Terminology in Clinical Setting)Rizka Karina ZahraNoch keine Bewertungen
- Methergine Drug StudyDokument3 SeitenMethergine Drug StudyjoshNoch keine Bewertungen
- Complications of The Third Stage of LabourDokument6 SeitenComplications of The Third Stage of LabourSong QianNoch keine Bewertungen
- Syllabus For Paper I & Ii For M.B.B.S Course Subject - AnatomyDokument10 SeitenSyllabus For Paper I & Ii For M.B.B.S Course Subject - AnatomyPreetam PaulNoch keine Bewertungen
- Burnaby Hospital ReportDokument141 SeitenBurnaby Hospital ReportThe Vancouver SunNoch keine Bewertungen
- ObstetricsDokument8 SeitenObstetricsrevathidadam55555100% (1)
- Partograph NotessssDokument17 SeitenPartograph NotessssSunil KumarNoch keine Bewertungen
- Anemia in PregnancyDokument33 SeitenAnemia in PregnancyKomal Dhulap100% (1)