Beruflich Dokumente
Kultur Dokumente
Paper Inflammatory Pathways and Insulin Action: GS Hotamisligil
Hochgeladen von
dewi maspufahOriginalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Paper Inflammatory Pathways and Insulin Action: GS Hotamisligil
Hochgeladen von
dewi maspufahCopyright:
Verfügbare Formate
International Journal of Obesity (2003) 27, S53S55
& 2003 Nature Publishing Group All rights reserved 0307-0565/03 $25.00
www.nature.com/ijo
PAPER
Inflammatory pathways and insulin action
GS Hotamisligil1*
1
Department of Genetics and Complex Diseases, Harvard School of Public Health, Boston, MA, USA
Obesity and type 2 diabetes are associated with a state of abnormal inflammatory response. While this correlation has also been
recognized in the clinical setting, its molecular basis and physiological significance are not yet fully understood. Studies in recent
years have provided important insights into this curious phenomenon. The state of chronic inflammation typical of obesity and
type 2 diabetes occurs at metabolically relevant sites, such as the liver, muscle, and most interestingly, adipose tissues. The
biological relevance of the activation of inflammatory pathways became evident upon the demonstration that interference with
these pathways improve or alleviate insulin resistance. The abnormal production of tumor necrosis factor alpha (TNF-a) in
obesity is a paradigm for the metabolic significance of this inflammatory response. When TNF-a activity is blocked in obesity,
either biochemically or genetically, the result is improved insulin sensitivity. Studies have since focused on the identification of
additional inflammatory mediators critical in metabolic control and on understanding the molecular mechanisms by which
inflammatory pathways are coupled to metabolic control. Recent years have seen a critical progress in this respect by the
identification of several downstream mediators and signaling pathways, which provide the crosstalk between inflammatory and
metabolic signaling. These include the discovery of c-Jun N-terminal kinase (JNK) and Ikappabkinase (IkK) as critical regulators of
insulin action activated by TNF-a and other inflammatory and stress signals, and the identification of potential targets. Here, the
role of the JNK pathway in insulin receptor signaling, the impact of blocking this pathway in obesity and the mechanisms
underlying JNK-induced insulin resistance will be discussed.
International Journal of Obesity (2003) 27, S53S55. doi:10.1038/sj.ijo.0802502
Keywords: JNK; TNF-a; IRS-1; signaling pathways; metabolism; diabetes; inflammation
Obesity is associated with a state of chronic inflammation
characterized by abnormal production of proinflammatory
cytokines and acute phase reactants.1 Several cell types, such
as adipocytes and macrophages, are involved in this
abnormal cytokine production. This seemingly surprising
ability of fat cells to mount an immune response is likely to
be a function of its common features with macrophages2 and
critical in systemic insulin action.3
Insulin signaling is a very complex process that involves
multiple pathways and cascades of phosphorylation events.
For the purposes of this short review, these pathways will not
be described; however, readers could refer to excellent recent
reviews on these pathways.4,5 Over the past decade, it is well
established that insulin receptor signaling is defective at
multiple levels in type 2 diabetes both in experimental
models and humans and this defective signaling is central to
pathogenesis of type 2 diabetes. One such pathway that
involves phosphorylation and signaling via the members of
the insulin-receptor substrate (IRS) family of proteins will be
*Correspondence: Dr GS Hotamisligil, Department of Genetics and
Complex Diseases, Harvard School of Public Health, 665 Huntington
Av., Boston, MA 02115, USA.
E-mail: ghotamis@hsph.harvard.edu
the focus of the present discussion, since it is particularly
relevant to insulin-mediated glucose metabolism and crosstalk with inflammatory pathways.4
Phosphorylation of tyrosine (tyr) residues of IRS-1 upon
activation of the insulin receptor constitutes a critical step in
the transmission of the insulin signal to downstream
effectors and biological outcomes. Several laboratories have
demonstrated that insulin-stimulated tyr phosphorylation of
IRS-1 as well as other proximal substrates of the insulin
receptor is reduced in obesity, and such reduction is believed
to be at the core of the development of insulin resistance.5
We and others have shown that the proinflammatory
cytokine tumor necrosis factor alpha (TNF-a), which promotes insulin resistance in several insulin-responding cells
and tissues, inhibits tyr phosphorylation of IRS-1 resulting in
a state reminiscent of type 2 diabetes and obesity.6 Interestingly, the same phenomenon is observed in the presence of
an increase in intracellular fatty acids,7 which also promote
insulin resistance, showing that both cytokines and fatty
acids may act via common pathways to block insulin action.
Under these conditions, cytokines and fatty acids stimulate
phosphorylation of IRS-1 on its serine (ser) residues.810 In
contrast to tyr phosphorylation, which results in the
transmission of the insulin signal, ser phosphorylation
Inflammation and insulin action
GS Hotamisligil
S54
blunts insulin signaling.810 In experimental systems, when
ser phosphorylation is prevented, the deleterious action of
TNF-a and possibly fatty acids on insulin signaling might be
prevented as well, further indicating the critical importance
of this modification in insulin-resistant states.
We and others have been investigating the molecular basis
and functional consequences of IRS-1 ser phosphorylation
and the responsible kinase(s). The inhibition of insulin
signaling by TNF-a and fatty acids in adipocytes and
hepatocytes involves activation of a kinase utilizing IRS-1
as a substrate.8,9 Once serine is phosphorylated, IRS-1
becomes a poor substrate for the insulin receptor, and
preventing such serine phosphorylation restores IRS-1mediated insulin receptor signaling in vitro. Of physiological
significance is the fact that in obesity and type 2 diabetes,
such an inhibitory phosphorylation of IRS-1 exists, in the
adipocyte and also in other metabolically important tissues.6
However, the identification of this kinase(s) and of its site(s)
of action on IRS-1 has been difficult due to the presence of
multiple phosphorylation sites on IRS-1, the existence in
cells of multiple distinct kinases that can act on IRS in vitro,4
and by the fact that TNF-a-mediated phosphorylation of IRS1 is a relatively weak phenomenon and therefore uneasy to
quantify.8,9,11 Despite such constraints, recent work has shed
light on IRS-1 phosphorylation sites as well as kinases
relevant to insulin resistance. Among others, biochemical
analysis has led to the identification of several serine
phosphorylation sites on IRS-1, of which ser-307 appears to
be of major importance and targeted by c-Jun N-terminal
kinase (JNK) in vitro.10 In cell-based systems and whole
animals, JNK serves as a sensing juncture for cellular stress
and the inflammatory status.12 JNK also phosphorylates IRS1 at the ser-307 site robustly. It is likely that other sites are
also targeted by this kinase, some simultaneously with serine
307, some depending on the stimulus and context. Phosphorylation of IRS-1 at ser-307 inhibits tyrosine phosphorylation, thereby inactivating further transmission of the
insulin signal. Serine phosphorylation can also be involved
in the targeting of IRS-1 for proteasome-mediated acute
degradation under certain but not all conditions. Of
relevance is the fact that JNK activity is elevated in the
tissues of several obesity models, including obesity resulting
from high-fat feeding and the genetic deficiency of leptin.12
In these mice, there is also elevation of ser-307 phosphorylation of IRS-1 and decreased tyrosine phosphorylation upon
insulin stimulation.
These observations indicated that JNK might be a key
molecule leading to insulin resistance and type 2 diabetes.
This was tested and validated in models where obesity is
generated in genetic deficiency of JNK isoforms, JNK1 and
JNK2.12 The JNK1 and JNK2 isoforms are expressed in most
tissues at different levels and ratios, whereas JNK3 is
primarily present in the central nervous system.13 In
experiments with complete deficiency of JNK1 or JNK2,
most of the obesity-related increase in JNK activity and
the metabolic consequences are attributable to the JNK1
International Journal of Obesity
isoform.12 JNK1 knockout mice gain less weight when fed
either a regular low-fat diet or a high-fat diet. Compared to
wild-type mice, adipose tissue of the JNK1 / mice is
morphologically normal, with smaller adipocytes, and the
liver contains dramatically less fat. Overall, there is a 10%
reduction in total body adipose mass in JNK1 / compared
to wild-type controls with no alterations in the lean body
mass.12 Other tissues do not appear to be affected by lack of
JNK1. Interestingly, the volumes of subcutaneous and
visceral but not gonadal fat depots are reduced in JNK1 /
mice. Plasma levels of adiponectin are increased while those
of resistin are reduced in JNK1-deficient mice on a high-fat
diet.12 JNK1 deficiency also dramatically enhances insulin
sensitivity and confers protection against diet-induced
insulin resistance as well as insulin resistance associated
with the ob/ob model of genetic obesity,12 although to a
lesser extent in the latter. It may seem counterintuitive at
first glance that the improvement in insulin sensitivity,
which should increase the anabolic action of insulin, leads
instead to reduced fat accretion. The reasons for such an
effect remain elusive at this time but suggest that the impact
of the JNK pathway on insulin action is not dependent on its
potentially distinct effects on whole-body adiposity. The
physiological relevance of the JNK1 isoform is further
illustrated by the fact that it is specifically increasedFin
liver, adipose tissue and skeletal muscleFin obesity resulting
in increased total JNK activity and increased IRS-1 serine
phosphorylation at these sites.12 In JNK1-deficient mice,
obesity-related ser-307 phosphorylation of IRS-1 is substantially reduced demonstrating that JNK1 is the predominant
ser kinase activity in obesity acting on IRS-1.12 Both TNF-a
and fatty acids increase JNK1 activity as well as ser
phosphorylation of IRS-1, and ser-307 phosphorylation is
reduced in JNK1 knockout mice. It must be mentioned that
JNK1 is not likely to be the sole serine kinase involved in the
development of insulin resistance. Several studies have
indeed underlined the importance of other kinases such as
protein kinase c (PKC) and IkK.14,15 The interactions
between these various kinases is complex and understanding
of these networks and mechanisms remain incomplete.16
The above discussion has focused on findings in cultured
cells and murine models, but there is evidence that JNK
might be highly relevant to human health. Indeed, human
mutations in the gene coding for JNK-binding protein, a
natural inhibitor of JNK activity, causes type 2 diabetes.17 It
is therefore not unreasonable to suggest that increased JNK
activity more generally plays a role in the development
of insulin resistance and type 2 diabetes in humans. If
JNK inhibitors turn out to be effective in improving
insulin sensitivity as much as gene targeting in experimental
models, they may offer attractive possibilities of developing effective means for the treatment of human insulin
resistance.
I should like to conclude this review with some thoughts
regarding the evolutionary reasons and advantages of the
remarkable overlap and correlations between the metabolic
Inflammation and insulin action
GS Hotamisligil
S55
and inflammatory signaling pathways. To this end, I will
allude to the fruit fly Drosophila melanogaster. This lowly and
distant cousin of ours bears a rather unique organ, called the
fat body, which functions at once as liver and hematopoietic/immune system.18 This site also appears as the mammalian homologue of adipose tissue.19 Remarkably, the GATA
family of transcription factors, which influences adipocyte
differentiation in mammals, is involved in the development
of the fat body of Drosophila.19 In the course of evolution,
the individualization of the hepatic, adipose and hematopoietic/immune organs occurred, while the function of a
common network of functional and molecular pathways
were retained in all. This might explain why there are so
many overlapping pathways in the hepatocyte, adipocyte,
macrophage and lymphocyte. The same molecules assume
both metabolic and inflammatory roles. Depending on the
cell type, the action of these overlapping pathways will
produce end points, such as insulin resistance (adipocyte),
atherosclerosis (macrophage) or hyperlipidemia (hepatocyte).
What could be the selective advantage of such a strong
overlap between metabolic and inflammatory signaling
pathways? One such advantage is that a strong immune
response confers higher odds of surviving infection, and
would therefore have been favored by natural selection. At
the same time however, in absence of starvation, a strong
immune response primes the system for an equally strong
metabolic response (eg insulin resistance) to stimuli such as a
high-energy and -fat intake. A survival advantage in hard
times hence becomes deleterious in times of plenty.
Acknowledgements
I thank Julie Gound and Gurol Tuncman for help in preparing this manuscript. Gokhan S Hotamisligil is supported
by grants from the National Institutes of Health and
American Diabetes Association.
References
1 Sethi JK, Hotamisligil GS. Semin Cell Dev Biol 1999; 10: 1929.
2 Charriere G, Cousin B, Arnaud E, Andre M, Bacou F, Penicaud L,
Casteilla L. J Biol Chem 2003; 278: 98509855.
3 Uysal KT, Wiesbrock SM, Marino MW, Hotamisligil GS. Nature
1997; 389: 610614.
4 White MF. Am J Physiol Endocrinol Metab 2002; 283: E413E422.
5 Saltiel AR, Kahn CR. Nature 2001; 414: 799806.
6 Hotamisligil GS In: LeRoith D, Taylor SI, Olefsky JM (eds).
Diabetes Mellitus, A Fundamental and Clinical Text. LippincottRaven: Philadelphia (in press).
7 Shulman GI. J Clin Invest 2000; 106: 171176.
8 Hotamisligil GH, Peraldi P, Budavari A, Ellis R, White MF,
Spiegelman BM. Science 1996; 271: 665668.
9 Kanety H, Hemi R, Papa MZ, Karasik A. J Biol Chem 1996; 271:
98959897.
10 Aguirre V, Uchida T, Yenush L, Davis R, White MF. J Biol Chem
2000; 275: 90479054.
11 Aguirre V, Werner ED, Giraud J, Lee YH, Shoelson SE, White MF. J
Biol Chem 2002; 277: 15311537.
12 Hirosumi J, Tuncman G, Chang L, Gorgun CZ, Uysal KT, Maeda
K, Karin M, Hotamisligil GS. Nature 2002; 420: 333336.
13 Davis RJ. Cell 2000; 103: 239252.
14 Griffin ME, Marcucci MJ, Cline GW, Bell K, Barucci N, Lee D,
Goodyear LJ, Kraegen EW, White MF, Shulman GI. Diabetes 1999;
48: 12701274.
15 Yuan M, Konstantopoulos N, Lee J, Hansen L, Li ZW, Karin M,
Shoelson SE. Science 2001; 293: 16731677.
16 Jiang G, Dallas-Yang Q, Liu F, Moller DE, Zhang BB. J Biol Chem
2003; 278: 180186.
17 Waeber G, Delplanque J, Bonny C, Mooser V, Steinmann M,
Widmann C, Maillard A, Miklossy J, Dina C, Hani EH, Vionnet N,
Nicod P, Boutin P, Froguel P. Nat Genet 2000; 24: 291295.
18 Rehorn KP, Thelen H, Michelson AM, Reuter R. Development 1996;
122: 40234031.
19 Tong Q, Dalgin G, Xu H, Ting CN, Leiden JM, Hotamisligil GS.
Science 2000; 290: 134138.
International Journal of Obesity
Das könnte Ihnen auch gefallen
- Diabetes in Pregnancy: The Complete Guide to ManagementVon EverandDiabetes in Pregnancy: The Complete Guide to ManagementLisa E. MooreNoch keine Bewertungen
- Obesity and Insulin Resistance: Barbara B. Kahn and Jeffrey S. FlierDokument9 SeitenObesity and Insulin Resistance: Barbara B. Kahn and Jeffrey S. Fliersapphire_asaphNoch keine Bewertungen
- 1340 FullDokument9 Seiten1340 FullAkma RahaNoch keine Bewertungen
- Obesity and Insulin Resistance: Barbara B. Kahn and Jeffrey S. FlierDokument9 SeitenObesity and Insulin Resistance: Barbara B. Kahn and Jeffrey S. FlierernaataNoch keine Bewertungen
- Insulin Resistance: Definition and Consequences: H.E. LebovitzDokument14 SeitenInsulin Resistance: Definition and Consequences: H.E. LebovitzCarlos Andre Hernández EléspuruNoch keine Bewertungen
- Insulin InsightDokument8 SeitenInsulin Insighttestreader1984Noch keine Bewertungen
- Deluca 2006Dokument2 SeitenDeluca 2006edh labNoch keine Bewertungen
- Sex Steroids and Insulin Resistance: Callum LIVINGSTONE and Mary COLLISONDokument16 SeitenSex Steroids and Insulin Resistance: Callum LIVINGSTONE and Mary COLLISONputrefactio6669Noch keine Bewertungen
- 1.full DiabetDokument11 Seiten1.full DiabetRichard ChayadiNoch keine Bewertungen
- Case 2Dokument23 SeitenCase 2EJ CorpusNoch keine Bewertungen
- Ajtr0002 0316Dokument16 SeitenAjtr0002 0316bagas umam alwiNoch keine Bewertungen
- Skeletal Muscle Insulin Resistance in Normoglycemic SubjectDokument7 SeitenSkeletal Muscle Insulin Resistance in Normoglycemic SubjectMuhammad Yusuf HanifNoch keine Bewertungen
- The Role of TNF: A in Adipocyte MetabolismDokument11 SeitenThe Role of TNF: A in Adipocyte MetabolismLatona Adeola ZainabNoch keine Bewertungen
- 2090 FullDokument9 Seiten2090 FullChloe WongNoch keine Bewertungen
- Downsi 6 PDFDokument11 SeitenDownsi 6 PDFmutimutimutiNoch keine Bewertungen
- J. Biol. Chem.-2014-Zhao-29112-22Dokument12 SeitenJ. Biol. Chem.-2014-Zhao-29112-22fatimakh462Noch keine Bewertungen
- Grupo 3 Obesity InflammationDokument9 SeitenGrupo 3 Obesity InflammationJeisonAlejandroÁlvarezVergaraNoch keine Bewertungen
- Liaqat 2017Dokument8 SeitenLiaqat 2017Hamza AldiriNoch keine Bewertungen
- GlicoseDokument5 SeitenGlicoseMayra PereiraNoch keine Bewertungen
- Trends in Insulin Resistance Insights Into Mechanisms andDokument25 SeitenTrends in Insulin Resistance Insights Into Mechanisms andgiorgiocrucittiNoch keine Bewertungen
- Pathophysiology of Insulin ResistanceDokument8 SeitenPathophysiology of Insulin ResistanceCamilo VidalNoch keine Bewertungen
- Zhou 2019Dokument11 SeitenZhou 2019Andreea Claudia NegrilaNoch keine Bewertungen
- Evidence For Increased Serine/Threonine Phosphorylation in Pregnancy and GDMDokument8 SeitenEvidence For Increased Serine/Threonine Phosphorylation in Pregnancy and GDMNagalakshmi SettyNoch keine Bewertungen
- Proyecto Fondecyt 1160792 Texto Principal BiosegDokument12 SeitenProyecto Fondecyt 1160792 Texto Principal BiosegAndrea Granda ValenciaNoch keine Bewertungen
- 29126.1 20150227101459 CoveredDokument10 Seiten29126.1 20150227101459 CoveredeeeeNoch keine Bewertungen
- Endoplasmic Reticulum Stress Is Reduced in Tissues of Obese Subjects After Weight LossDokument8 SeitenEndoplasmic Reticulum Stress Is Reduced in Tissues of Obese Subjects After Weight LossJulia SCNoch keine Bewertungen
- Drug Discovery: Targeting Inflammation in DiabetesDokument1 SeiteDrug Discovery: Targeting Inflammation in Diabeteschanpreet12Noch keine Bewertungen
- When Metabolism and Epigenetics ConvergeDokument3 SeitenWhen Metabolism and Epigenetics ConvergeMariano PerezNoch keine Bewertungen
- E745 FullDokument7 SeitenE745 FullVelasco EduardoNoch keine Bewertungen
- Inflamacion Estres y DiabetesDokument9 SeitenInflamacion Estres y DiabetesDavid CBNoch keine Bewertungen
- Adipokines, Inflammation, and The Endothelium in Diabetes: Waleed Aldhahi, MD, FRCPC, and Osama Hamdy, MD, PHDDokument6 SeitenAdipokines, Inflammation, and The Endothelium in Diabetes: Waleed Aldhahi, MD, FRCPC, and Osama Hamdy, MD, PHDneysaonlineNoch keine Bewertungen
- Resolving The Paradox of Hepatic Insulin ResistanceDokument10 SeitenResolving The Paradox of Hepatic Insulin ResistanceMauro Rojas ZúñigaNoch keine Bewertungen
- Pathogenesis of Gestasional Diabetes MellitusDokument24 SeitenPathogenesis of Gestasional Diabetes MellitusNadya Meilinar SamsonNoch keine Bewertungen
- Bisphenol-A: A New Diabetogenic Factor?: ReviewDokument9 SeitenBisphenol-A: A New Diabetogenic Factor?: ReviewKaren Mercado RNoch keine Bewertungen
- Targeting The NLRP3 Inflammasome To Reduce Diet-Induced Metabolic Abnormalities in MiceDokument39 SeitenTargeting The NLRP3 Inflammasome To Reduce Diet-Induced Metabolic Abnormalities in Miceanirbanmanna88320Noch keine Bewertungen
- Fang 2005Dokument10 SeitenFang 2005pamela gaitanNoch keine Bewertungen
- The Obese Healthy Paradox: Is Inflammation The Answer?Dokument9 SeitenThe Obese Healthy Paradox: Is Inflammation The Answer?Maria Isabel Queipo OrtuñoNoch keine Bewertungen
- Insulin's Mechanism of ActionDokument14 SeitenInsulin's Mechanism of ActionKishore ChinnaNoch keine Bewertungen
- En V52n2a11 PDFDokument11 SeitenEn V52n2a11 PDFivanhariachandraNoch keine Bewertungen
- Molecular Basis of Type 2 DiabetesDokument22 SeitenMolecular Basis of Type 2 DiabetespimpellerNoch keine Bewertungen
- Prediction of Type 2 Diabetes: A Natural History PerspectiveDokument9 SeitenPrediction of Type 2 Diabetes: A Natural History Perspectiveandree_zz4890Noch keine Bewertungen
- Loss of EGR-I Uncouples Compensatory Responses of Pancreatic Beta CellDokument17 SeitenLoss of EGR-I Uncouples Compensatory Responses of Pancreatic Beta Cellichengmelody0108Noch keine Bewertungen
- Chronic Inflammation in Fat Plays A Crucial Role in The Development of Obesity-Related Insulin ResistanceDokument10 SeitenChronic Inflammation in Fat Plays A Crucial Role in The Development of Obesity-Related Insulin ResistanceRachel Lalaine Marie SialanaNoch keine Bewertungen
- Hypothalamic Inflammation and ObesityDokument16 SeitenHypothalamic Inflammation and ObesitySindy Noreima Nino VegaNoch keine Bewertungen
- GLP 1Dokument19 SeitenGLP 1Larissa Gomes NevesNoch keine Bewertungen
- Non Alcoholic Fatty Liver Disease ThesisDokument5 SeitenNon Alcoholic Fatty Liver Disease ThesisAshley Hernandez100% (2)
- 1 Octeto de DefronzoDokument23 Seiten1 Octeto de DefronzoLesli Rodriguez50% (2)
- Cellular Mechanism of DM FinalDokument70 SeitenCellular Mechanism of DM FinalJamil Muqtadir BhattiNoch keine Bewertungen
- 1diet-Induced Obesity Increases NF-JB Signaling in Reporter MiceDokument8 Seiten1diet-Induced Obesity Increases NF-JB Signaling in Reporter MicepopopioNoch keine Bewertungen
- J. Nutr.-2004-Wang-1032-8Dokument7 SeitenJ. Nutr.-2004-Wang-1032-8Daniel Lee Eisenberg JacobsNoch keine Bewertungen
- Perspectives: G Protein-Coupled Receptors As Targets For Anti-Diabetic TherapeuticsDokument13 SeitenPerspectives: G Protein-Coupled Receptors As Targets For Anti-Diabetic TherapeuticsAlicia Cerpa LunaNoch keine Bewertungen
- Modulation of Glucose Transporter Protein by Dietary Flavonoids in Type 2 Diabetes MellitusDokument17 SeitenModulation of Glucose Transporter Protein by Dietary Flavonoids in Type 2 Diabetes MellitusAinun Jariah FahayNoch keine Bewertungen
- Obesity Is Associated With Macrophage Accumulation in Adipose TissueDokument13 SeitenObesity Is Associated With Macrophage Accumulation in Adipose TissueRachel Lalaine Marie SialanaNoch keine Bewertungen
- Literature Review On Insulin ResistanceDokument8 SeitenLiterature Review On Insulin Resistanceyjdzpccnd100% (1)
- Resistensi Insulin Terkait ObesitasDokument7 SeitenResistensi Insulin Terkait ObesitasEster HutabaratNoch keine Bewertungen
- NIH Public Access: Mechanisms of Insulin Resistance in ObesityDokument17 SeitenNIH Public Access: Mechanisms of Insulin Resistance in ObesityPutri Wulan SukmawatiNoch keine Bewertungen
- Moderate Weight Loss Attenuates Chronic Endoplasmic Reticulum Stress and Mitochondrial Dysfunction in Human ObesityDokument10 SeitenModerate Weight Loss Attenuates Chronic Endoplasmic Reticulum Stress and Mitochondrial Dysfunction in Human ObesityJulia SCNoch keine Bewertungen
- Diabetes Mellitus Type 2 Research PaperDokument6 SeitenDiabetes Mellitus Type 2 Research Paperntjjkmrhf100% (1)
- The Impact of Strategic Human Resource Management On PerformnceDokument11 SeitenThe Impact of Strategic Human Resource Management On PerformnceMahmud AbdullahNoch keine Bewertungen
- Perhitungan BEPDokument1 SeitePerhitungan BEPdewi maspufahNoch keine Bewertungen
- Fitomedika April 2011Dokument7 SeitenFitomedika April 2011dewi maspufahNoch keine Bewertungen
- Angular MotionDokument22 SeitenAngular Motiondewi maspufahNoch keine Bewertungen
- SPT BatangDokument6 SeitenSPT Batangdewi maspufahNoch keine Bewertungen
- Lesson Plan On Nursing Care of A Patient With Acute Renal FailureDokument17 SeitenLesson Plan On Nursing Care of A Patient With Acute Renal FailurePriyanka NilewarNoch keine Bewertungen
- Emergency Viva (Full)Dokument48 SeitenEmergency Viva (Full)ashokarathnasingheNoch keine Bewertungen
- Ebook John Murtaghs General Practice Companion Handbook PDF Full Chapter PDFDokument67 SeitenEbook John Murtaghs General Practice Companion Handbook PDF Full Chapter PDFroberto.duncan209100% (27)
- Child Guidance ClinicDokument22 SeitenChild Guidance ClinicBinal Joshi67% (3)
- اسئلة امتحان الفصل الاول حشوات الجذورDokument7 Seitenاسئلة امتحان الفصل الاول حشوات الجذورJowan EmadNoch keine Bewertungen
- Vandana Raut Tata Memorial Centre 31yrsDokument2 SeitenVandana Raut Tata Memorial Centre 31yrsvandanaNoch keine Bewertungen
- Oct Symp AbhiDokument54 SeitenOct Symp AbhiMonisha ArulalanNoch keine Bewertungen
- Diplopia: Diagnosis and Management: Author: Saurabh JainDokument3 SeitenDiplopia: Diagnosis and Management: Author: Saurabh Jainlia indria watiNoch keine Bewertungen
- 23-5-2022 Presentation JentadeutoDokument52 Seiten23-5-2022 Presentation JentadeutofsvtqsNoch keine Bewertungen
- First Aid For The Usmle Step 1 2022-Mcgraw-Hill Education 2022Dokument1 SeiteFirst Aid For The Usmle Step 1 2022-Mcgraw-Hill Education 2022Beto RendonNoch keine Bewertungen
- Part2MICRO (COMPILED)Dokument9 SeitenPart2MICRO (COMPILED)Thea GonzalesNoch keine Bewertungen
- Trauma: H. Scott Bjerke, Felix Lui, Areti Tillou, and Frederick A. LuchetteDokument38 SeitenTrauma: H. Scott Bjerke, Felix Lui, Areti Tillou, and Frederick A. LuchettecharoiteNoch keine Bewertungen
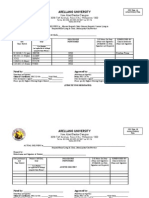
- Arellano University: Jose Abad Santos CampusDokument7 SeitenArellano University: Jose Abad Santos CampusLloyd VargasNoch keine Bewertungen
- Angiographic ProjectionsDokument16 SeitenAngiographic ProjectionsKarren_M888Noch keine Bewertungen
- CBCT-Scan in DentistryDokument24 SeitenCBCT-Scan in DentistryBilly Sam80% (5)
- Pressure Ulcer Assessment Chart & Body MapDokument2 SeitenPressure Ulcer Assessment Chart & Body MapWidfdsafdsaNoch keine Bewertungen
- Case Report Large Uterine Fibroids in Pregnancy With Successful Caesarean MyomectomyDokument4 SeitenCase Report Large Uterine Fibroids in Pregnancy With Successful Caesarean MyomectomyChidimma VictoryNoch keine Bewertungen
- 683 2Dokument15 Seiten683 2M Noaman AkbarNoch keine Bewertungen
- The European Guideline On Management of Major Bleeding and Coagulopathy Following Trauma Sixth Edition (2023) PDFDokument1 SeiteThe European Guideline On Management of Major Bleeding and Coagulopathy Following Trauma Sixth Edition (2023) PDFMatheus LiraNoch keine Bewertungen
- Immuno Oncology Therapies White Paper PPDDokument12 SeitenImmuno Oncology Therapies White Paper PPDkevalNoch keine Bewertungen
- Otitis MediaDokument7 SeitenOtitis MediaNader Smadi67% (3)
- A Rare Case of Puerperal Uterine Inversion and Literature ReviewDokument3 SeitenA Rare Case of Puerperal Uterine Inversion and Literature ReviewIJAR JOURNALNoch keine Bewertungen
- Chapter - 2 Microorganisms (Continuation)Dokument2 SeitenChapter - 2 Microorganisms (Continuation)ARSHAD JAMILNoch keine Bewertungen
- The Effects of Laparoscopic Nissen FundoplicationDokument2 SeitenThe Effects of Laparoscopic Nissen FundoplicationGabriel CassNoch keine Bewertungen
- Comen SCD600 Training V2.1 PresentationDokument21 SeitenComen SCD600 Training V2.1 PresentationDeclan WangNoch keine Bewertungen
- Liver BiopsyDokument3 SeitenLiver BiopsyBiway RegalaNoch keine Bewertungen
- Fitzpatricks Dermatology in General Medicine 8ed 1Dokument10 SeitenFitzpatricks Dermatology in General Medicine 8ed 1ANTINNoch keine Bewertungen
- 5 4 3 2 1 Grounding Techniqueqspae PDFDokument2 Seiten5 4 3 2 1 Grounding Techniqueqspae PDFsheetcherry57Noch keine Bewertungen
- Pacemakers - Fact SheetDokument7 SeitenPacemakers - Fact Sheettalha.k.rajpootNoch keine Bewertungen
- BernottiDokument44 SeitenBernottiAlexandra Alexandra100% (2)
- Return of the God Hypothesis: Three Scientific Discoveries That Reveal the Mind Behind the UniverseVon EverandReturn of the God Hypothesis: Three Scientific Discoveries That Reveal the Mind Behind the UniverseBewertung: 4.5 von 5 Sternen4.5/5 (52)
- The Rise and Fall of the Dinosaurs: A New History of a Lost WorldVon EverandThe Rise and Fall of the Dinosaurs: A New History of a Lost WorldBewertung: 4 von 5 Sternen4/5 (597)
- Why We Die: The New Science of Aging and the Quest for ImmortalityVon EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityBewertung: 4 von 5 Sternen4/5 (5)
- A Brief History of Intelligence: Evolution, AI, and the Five Breakthroughs That Made Our BrainsVon EverandA Brief History of Intelligence: Evolution, AI, and the Five Breakthroughs That Made Our BrainsBewertung: 4.5 von 5 Sternen4.5/5 (6)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisVon EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisBewertung: 3.5 von 5 Sternen3.5/5 (2)
- Gut: the new and revised Sunday Times bestsellerVon EverandGut: the new and revised Sunday Times bestsellerBewertung: 4 von 5 Sternen4/5 (393)
- Buddha's Brain: The Practical Neuroscience of Happiness, Love & WisdomVon EverandBuddha's Brain: The Practical Neuroscience of Happiness, Love & WisdomBewertung: 4 von 5 Sternen4/5 (216)
- 10% Human: How Your Body's Microbes Hold the Key to Health and HappinessVon Everand10% Human: How Your Body's Microbes Hold the Key to Health and HappinessBewertung: 4 von 5 Sternen4/5 (33)
- The Molecule of More: How a Single Chemical in Your Brain Drives Love, Sex, and Creativity--and Will Determine the Fate of the Human RaceVon EverandThe Molecule of More: How a Single Chemical in Your Brain Drives Love, Sex, and Creativity--and Will Determine the Fate of the Human RaceBewertung: 4.5 von 5 Sternen4.5/5 (517)
- Masterminds: Genius, DNA, and the Quest to Rewrite LifeVon EverandMasterminds: Genius, DNA, and the Quest to Rewrite LifeNoch keine Bewertungen
- Gut: The Inside Story of Our Body's Most Underrated Organ (Revised Edition)Von EverandGut: The Inside Story of Our Body's Most Underrated Organ (Revised Edition)Bewertung: 4 von 5 Sternen4/5 (411)
- Tales from Both Sides of the Brain: A Life in NeuroscienceVon EverandTales from Both Sides of the Brain: A Life in NeuroscienceBewertung: 3 von 5 Sternen3/5 (18)
- All That Remains: A Renowned Forensic Scientist on Death, Mortality, and Solving CrimesVon EverandAll That Remains: A Renowned Forensic Scientist on Death, Mortality, and Solving CrimesBewertung: 4.5 von 5 Sternen4.5/5 (397)
- Undeniable: How Biology Confirms Our Intuition That Life Is DesignedVon EverandUndeniable: How Biology Confirms Our Intuition That Life Is DesignedBewertung: 4 von 5 Sternen4/5 (11)
- Seven and a Half Lessons About the BrainVon EverandSeven and a Half Lessons About the BrainBewertung: 4 von 5 Sternen4/5 (110)
- The Ancestor's Tale: A Pilgrimage to the Dawn of EvolutionVon EverandThe Ancestor's Tale: A Pilgrimage to the Dawn of EvolutionBewertung: 4 von 5 Sternen4/5 (812)
- Who's in Charge?: Free Will and the Science of the BrainVon EverandWho's in Charge?: Free Will and the Science of the BrainBewertung: 4 von 5 Sternen4/5 (65)
- The Other Side of Normal: How Biology Is Providing the Clues to Unlock the Secrets of Normal and Abnormal BehaviorVon EverandThe Other Side of Normal: How Biology Is Providing the Clues to Unlock the Secrets of Normal and Abnormal BehaviorNoch keine Bewertungen
- Lymph & Longevity: The Untapped Secret to HealthVon EverandLymph & Longevity: The Untapped Secret to HealthBewertung: 4.5 von 5 Sternen4.5/5 (13)
- The Lives of Bees: The Untold Story of the Honey Bee in the WildVon EverandThe Lives of Bees: The Untold Story of the Honey Bee in the WildBewertung: 4.5 von 5 Sternen4.5/5 (44)
- The Consciousness Instinct: Unraveling the Mystery of How the Brain Makes the MindVon EverandThe Consciousness Instinct: Unraveling the Mystery of How the Brain Makes the MindBewertung: 4.5 von 5 Sternen4.5/5 (93)
- Moral Tribes: Emotion, Reason, and the Gap Between Us and ThemVon EverandMoral Tribes: Emotion, Reason, and the Gap Between Us and ThemBewertung: 4.5 von 5 Sternen4.5/5 (115)
- Why We Sleep: Unlocking the Power of Sleep and DreamsVon EverandWhy We Sleep: Unlocking the Power of Sleep and DreamsBewertung: 4.5 von 5 Sternen4.5/5 (2083)
- Good Without God: What a Billion Nonreligious People Do BelieveVon EverandGood Without God: What a Billion Nonreligious People Do BelieveBewertung: 4 von 5 Sternen4/5 (66)