Beruflich Dokumente
Kultur Dokumente
Cardiovascular Effects
Hochgeladen von
suri_2113Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Cardiovascular Effects
Hochgeladen von
suri_2113Copyright:
Verfügbare Formate
Clin. Cardiol.
11, 253-260 (1988)
Cardiovascular Effects of Berberine in Patients with Severe Congestive Heart
Failure
J . A. MARIN-NETO,M.D.,D.Sci., B.
c. MACIEL,M.D.,A. L. SECCHES, M.D., L. GALLOJr., M.D.
Cardiaccatheterization Laboratory, SeCb de Hemodinlmicae FunCiio Pulmonar, Hospital das Clinicasda Faculdadede Medicina de Ribeifio Preto, University of S b Paulo
Summary: Berberine, an alkaloid of the protoberberine
family, has been shown to have strong positive inotropic
and peripheral resistance-lowering effects in dogs with and
without heart failure. To determine the acute cardiovascular effects of berberine in humans, 12 patients with
refractory congestive heart failure were studied before and
during berberine intravenous infusion at rates of 0.02 and
0.2 mg/kg per min for 30 minutes. The lower infusion
dose produced no significant circulatory changes, apart
from a reduction in heart rate (14%). The 0.2 mg/kg per
min dose elicited several significantchanges: (a) Decreases
in systemic (48%, p<O.Ol) and pulmonary vascular
resistance (41%, p<O.Ol), and in right atrium (2896,
p <0.05) and left ventricularenddiastolic pressures (32% ,
p<O.Ol). (b) Increases in cardiac index (45%, p<O.Ol),
stroke index (45%, p<O.Ol), and LV ejection fraction
measured by contrast angiography (56%, p<O.Ol). (c)
Increases in hemodynamic and echocardiographic indices
of LV performance: peak measured velocity of shorten:
ing (45%, p <0.01), peak shortening velocity at zero load
(41 %, p <0.01), rate of development of pressure at developed isovolumic pressure of 40 mmHg (20%,
p<O.Ol), percent fractional shortening (50%, p<O.Ol),
and the mean velocity of circumferential fiber shortening
(5496, p<O.Ol). (d) Decrease of arteriovenous oxygen
difference (28% , p <0.05) with no changes in total body
oxygen uptake, arterial oxygen tension, or hemoglobin dis-
*Supported by Grant med. 83/2162-0 from the FundacSo de Amparo h Pesquisa do Estado de S b Paulo (FAPESP), Brazil.
Address for reprints:
Jose A. Marin Neto, M.D.,D.Sci.
Cardiac Catheterization Laboratory
Faculdade de Medicina de Ribeirfio Preto
14048 - Ribeirrio Preto, SP, Brad
Received: July 28, 1987
Accepted: September 14, 1987
sociation properties. These salutary acute effects show that
berberine markedly improved cardiac performance in patients with heart failure refractory to conventional medical therapy with digitalis and diuretics. The improvement
is probably subsequent to peripheral vasodilatation and to
inotropic stimulation. Significant untoward effects appear
to be the development of ventricular tachycardia with torsades de pointes morphology, detected in 4 patients 120 h after the infusion of berberine. This possible association requires further elucidation before the administration of bekrine may be extended to other patients in heart
failure.
Key words: berberine, vasodilatation, inotropism, heart
failure, torsades de pointes, anhythmogenicity of antiarrhythmic agents
Introduction
Many pharmacological classes of vasodilators have been
examined extensively over the current and the last decades.
Numerous investigations have demonstrated that such
agents primarily reduce ventricular loading conditions,
thus inducing correspondent increases in stroke volume
and cardiac output. Also,a variety of new positive inotrop
ic agents are being investigated, as a therapeutic measure
directed to correct the intrinsic decrease of cardiac contractility seen in many patients with congestive heart
failure.
It may be proposed that a drug that can directly increase
contractility and, at the same time, reduce peripheral
resistance will be of obvious therapeutic advantage for the
treatment of heart failure. Berberine (BBR) (Fig. 1) is one
of a series of protoberberine alkaloids devoid of digitalislike or adrenergicproperties, that has been shown to lower
peripheral vascular resistance and ~ t i m u l a t ecardiac
~ - ~ inotropism in dogs with and without heart failure. In addition, it has also been shown to antagonize experimentally
induced cardiac dysrhythmias in animal models such as
254
Clin. Cardiol. Vol. 11, April 1988
FIG.1 Chemical structure of berberine, one of the protoberberine
alkaloids.
aconitine and digitalis intoxication in dog^,^.^ or coronary
occlusion in rats. Because of its ability to reduce ventricular afterload and augment myocardial contractility,
BBR appears to be potentially useful in congestive heart
failure. We examined the acute hemodynamic responses
to intravenous BBR infusions in subjects with refractory
chronic congestive heart failure, being subjected to diagnostic cardiac catheterization procedures.
Methods
Patient Population
Twelve patients (2 female, 10 male) with severe congestive heart failure (CHF), refractory to conventional
medical treatment were studied after institutional approval
and informed consent was obtained. The investigation was
in accordance with the Declaration of Helsinki. The mean
age was 47.8 years (range 27 to 66). Etiologic diagnosis
was chronic Chagas cardiopathy in 6, idiopathic dilated
cardiomyopathy in 4, ischemic heart disease in 1, and
chronic rheumatic aortic regurgitation in the last patient.
Six patients were categorized as functional class III and
the remaining 6 were placed in class IV according to the
New York Heart Association Classification (1964). All
patients studied were receiving a daily digoxin dose of
0.25 mg orally and furosemide (daily oral dose range 40
to 160 mg). In addition, 2 patients were on spironolactone (daily oral dose 100 and 200 mg, respectively). All
patients had previously received vasodilators or a
converting-enzyme inhibitor; these drugs were discontinued at least 48 hours before the study. The digitalis and
diuretics administration was maintained unaltered throughout the period of study, as was antiarrhythmic therapy
based on amiodarone (600 mg daily, in 2 patients) and
disopyramide (200 mg daily, in 2 patients).
Study Design
Patients were hospitalized for at least 3 days before
catheterization, to ensure a stable medical regimen and
diet. All studies were carried out in the afternoon, in a
postprandial condition following a light meal, without
premedication.
After routine diagnostic coronary and left ventricular
cineangiography with Hypaque 75% (30 ml at 10 ml/s),
about 20 minutes supine rest was allowed for return to
the basal state.8Hemodynamic, oxymetric, and echocardiography measurements were then camed out for baseline
condition, followed by a 30-min intravenous infusion period of berberine at the rate of 0.02 mg/kg per min, with
an increment to 0.2 mg/kg per min for an additional period
of 30 minutes. At each period, the hemodynamic measurements were repeated. At the end of the period of the
higher infusion rate, echocardiographic,and oxymetric determinations were performed again, and a second injection of contrast was done for selective left cineangiography (same technique as for the first injection).
Measurements
Right and left-sided cardiac catheterization was performed after cut-down in the right antecubital fossa under local anesthesia. Selective coronary arteriography was
performed, followed by left ventricular cineangiography
through a Sones 8F catheter. This catheter was thereafter
replaced by a #7F Millar tip-micromanometer,which was
positioned across the aortic valve, to measure pressures
in the left ventricle and aorta simultaneously. A triplelumen flow-directed catheter was used for measurement
of pressures in the pulmonary circulation and right heart,
as well as for determinationof cardiac output by thermodilution. Injections of 10 ml cold solution were effected in
triplicate (5 injections if variation exceeded lo%), using
a model DTCCO-07 Electronics for Medicine Honeywell
cardiac output computer. The electrocardiogram,the analogic output of thermodilution curves, pressures, and the
first derivative of left ventricular pressure were displayed
on a Hewlett-Packard 8890-B multichannel recorder,
stored on magnetic tape and processed by computer. Indices of left ventricular contractility, including peak
dP/dt, the peak measured velocity of the contractile element (VPM), the peak shortening velocity at zero load
(Vmax),and the rate of development of pressure at the developed isovolumic pressure of 40 mmHg (dP/dt/DP40)
were derived by on-line computer processing of the pressure signal, according to standard calculation^.^
Systemic vascular resistance (SVR) and pulmonary vascular resistance (PVR) were calculated (dyne-sar)
from the following formulas: SVR= 80 x (mean aortic
pressure -mean right atrial pressure)/cardiac output and
PVR =80 x (mean pulmonary pressure - mean wedge
pressure)/cardiac output.
Expired air was collected in 3 minute periods and passed
through a Beckman metabolic measurement cart, permitting determination of oxygen uptake (VO,) and C 0 2
production. Arterial and mixed venous (pulmonary artery)
samples were drawn for determination of oxygen content
J. A. Marin Net0 et al.: Berbenne in human heart failure
in a Coming 175 Gas Analyser, and calculation of the arteriovenous oxygen difference (AA-V02); in addition, a
Hemo-0-Scan Aminco Analyser was used to draw the
hemoglobin dissociation curve for each patient, allowing
the determinationof the arterial pressure at which the saturation was 50% (P50).
Left ventricular ejection fraction was measured by the
single-plane method of Sandler and Dodge,Io by means
of a Vanguard motion analyzer.
Two-dimensional echocardiography was camed out
with a Hewlett-Packard 77020 A imaging system, permitting the measurement of end-diastolic and end-systolic
left ventricular dimensions, and the calculation of the percent fractional shortening (AD%)and of the mean circumferential fiber shortening velocity (VCF).
Statistical Analysis
The significance of the acute effects of both infusion
rates, as compared to baseline values, was assessed by
a paired Student's t-test. Significance of data was determined at the level of p<O.O5.
Results
Control and postberberine hemodynamic, echocardiographic, and oxymetric measurements (mean fSD) are
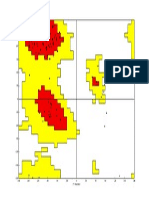
presented in Tables I to III. Figures 2 to 6 also depict individual behavior of several circulatory parameters for
baseline condition and after the infusion rate of 0.2
mg/kg/min of berberine.
Control measurements showed severe left ventricular
dysfunction, with low cardiac output, high arteriovenous
oxygen difference, and increased vascular resistances.
The first infusion rate (0.02mg/kg/min) failed to induce significant circulatory changes, with the exception
of a modest decrease in heart rate, from 89.6f 18.1 to
77.3f19.1 beatdmin (-14%, pc0.05).
The infusionof bekrine at the rate of 0.2mg/kg per min
was associated with profound circulatory alterations. The
heart rate returned to near baseline values (89.9f28.0
beatslmin). As compared to control condition, there was
a significant fall in all cardiovascularpressures measured:
rightatrium, from 13.0f7.6to9.3*7.0mmHg, -28%,
p<0.05; pulmonary wedge, from 21.7f7f7.0 to
16.2f6.0 mmHg, -25%, p<O.Ol; pulmonary artery,
from 30.5f9.6 to 25.1 f9.2 mmHg, - 18%, p cO.01;left
ventricular end-diastolic, from 21.0f10.8 to 14.2f5.4
mmHg, - 32% ,p <0.01;mean aortic, from 98.1f9.9 to
85.4f9.7mmHg, - 13%, pCO.01 (Table I and Fig. 2).
Significant increases were produced in cardiac index (from
2.2f0.9to 3.2f0.9 l/min/m2, +45%, pCO.Ol), stroke
index (from 24.5f11.9 to 35.6f14.6 ml/m2, +45%,
p<O.Ol), and left ventricular stroke work index (from
33.9f16.8 to 39.1f16.0 g.min/m2, +15%, pc0.05)
(Table I and Fig. 3). A significant decrease was seen in sys-
zc
Fj
0
'g
2
i2
C
0
0
$8
8
C
._
c)
A
,
G
c1
w
A
;1"
255
256
Clin. Cardiol. Vol. 1 1 , April 1988
TABLEI1 Effects of berberine on isovolumic-phase indices of left ventricular performance
Control
Berberine (0.02 mg/kg/min)
Berberine (0.2 mglkglmin)
Peak (+) dP/dt
VPM
1089 f2 10
1075 f240
1203f289"
1.07f0.42
1.16f0.41
1 S5f0.56
dP/dt/DP 40
X,"
1.26f0.40
1.40f0.47
1.78 f0.56"
18.9f2.7
19.5f2.9
22.6f4.5'
'<0.01.
Abbreviations: Peak (+) dP/dt=maximum positive first time derivative of left ventricular pressure (mmHg/s); VPM =left ventricular peak measured shortening velocity (circ/s); V,, =maximum left ventricular shortening velocity (circk); dP/dt/DP 40=value
of the rate of development of pressure at the developed isovolumic pressure of 40 mmHg (s-I).
TABLEIII Effects of intravenous berberine on echocardiographic variables and oxymetric characteristics
n= 12
LVDd
AD %
LVDs
Control
65.Jf8.8 53.7f8.5
Berberine (0.2 mglkglmin) 65.0f9.4 47.3f9.3'
18.3f4.0
27.5f5.7'
vo2
VCF
PaOz
AA-VO2
0.70f0.17 224563 76.4f 10.3 6.53f2.47
1.08f0.25b 241f61 71.9f9.2 4.73f1.52'
p50
28.7f2.75
27.5f2.28
"p <0.05.
bp<O.Ol*
Abbreviations: LVDd =left ventricularend-diastolicdimension (cm); LVDs =left ventricular end-systolic dimension (cm); AD % =percent
fractional shortening; VCF=mean circumferential fiber shortening velocity (circ/s); VOz=oxygen uptake (mllrnin, STPD);
PaO, =arterial oxygen tension (mmHg); AA-VO2=arterial venous oxygen difference (ml/100 ml); Ps0=arterial oxygen tension for
saturation 50%.
F
LVEDP-(mmHg)
lo0l
40c
4.0
---7t21
2.0
I
80
I SVR (dyne*s*cm-')
15001
4000t
k-AD%
1 PVR (dyne*s*cm-5)
I=%=
1000
FIG.2 Individual changes in mean aortic pressure (AoP), left ventricular end-diastolic pressure (LVEDP), systemic (SVR) and pulmonary vascular resistance (PVR) from control (C) to the end of
the 30-min period of 0.2 mg/kg/min infusion of berberine (B). Bars
indicate mean values, for the group. p<O.OI, for all parameters.
VcF-(circls)
1.4
'i
20
f g m
"
FIG.3 Individual changes in cardiac index (CI), systemic arteriovenous oxygen difference (AA -V02), percent fractional shortening (AD%), and mean velocity of circumferential shortening
(VCF), from control (C) to the end of 30 minute period of 0.2
mglkglmin infusion of berberine (B). Bars indicate mean values for
the group. p<O.OI for all parameters.
257
J. A. Marin Net0 et al.: Beherine in human heart failure
1400p3
0.5
80 -
I000
0.3Im&
60 -
40 -
04-
c
r
--
600b
20
FIG.4 Individual changes in left ventricular ejection fraction (EF),
the maximum rate of rise of left ventricular pressure (peak + dP/dt),
the peak shortening velocity at zero load (V,,,), and the rate of
development of pressure at the developed isovolumic pressure of
40 mmHg (dP/dt/DP 40),from control to the end of the 30-min
of 0.2 mg/kg min infusion of berberine (B). Bars indicate mean
values for the group. p<O.O1 for all parameters.
20
30
~~
50
LVEDP (rnmHg)
FIG.5 Relationship between left ventricular end-diastolic pressure
(LVEDP) and stroke index (SVI). Dots are control values and arrowheads are values at the end of the 3 0 4 1 1 period of 0.2
mg/kg/min infusion of berberine.
10
40
temic vascular resistance (from 2667 f 1064 to 1384f459
dyneeu~crn-~,
-48%, p < 0.01) and pulmonary vascular
resistance (from 745 f293 to 441 f250 dyne-scm-s,
-41%, p<O.Ol) (Table I and Fig. 2). Left ventricular
ejection fraction was elevated from: 0.27f0.07 to
0.42fO.11, +56%,p<0.01 (TableIandFig.4).Atypical case is illustrated in Figure 6, showing end-diastolicand
end-systolicframes before and after behrine . The left ventricular indices of contractility were also significantly increased after the infusion of 0.2 mg/kg per min of berberine (Table I1 and Fig. 4): Peak+dP/dt from 1089f210 to
1203f289 mmHg/s, + l o % , pc0.01; VPM, from
FIG.6 Left ventriculographic response to 0.2 mg/kg/min infusion of berberine for 30 min. A representative case of Chagas cardiac failure
is shown. Panels at left represent end-diastolic frames, before (upper) and during berberine (lower). Right panels correspond the end-systolic
frames respectively. Ejection fraction was 0.25 in control, and 0.43 during berberine condition.
258
Clin. Cardiol. Vol. 11, April 1988
1.07f0.42 to 1.55f0.56circ/s, f45%, p<O.Ol; V,
from 1.26f0.40 to 1.78f0.56 circ/s, +41%, p<O.Ol;
dP/dt/DP 40, from 18.952.7 to 22.6f4.5 .s-I, +20%,
p<O.Ol. Improvement in left ventricular performance is
also shown by increases in echocardiographic measurements of AD% (from 18.3k4.0 to 27.5f5.7, +50%,
p <0.01) and VCF (from 0.7 fO. 17 to 1.08f0.25 circ/s,
+54%, p<O.Ol) (Table I11 and Fig. 2) as well as by the
shift to the left and upward in the relationshipbetween left
ventricular filling pressure and stroke volume index (Fig.
5). Table I11 also shows that the V02,the PaOzand the Pso
were not significantly affected by berberine, while an important reduction was noticed in AA - V 0 2 (from
6.53f2.47 to4.73fl.53 ml/dl, -28%, p<0.05) (Fig.
3).
Side Effects
Facial flushing was seen in 2 cases. In two others, transient nausea was experienced within one hour after the
end of infusion of berberine. In 4 patients, repetitive episodes of sustained ventricular tachycardia of the type torsades de pointes occurred between 1 and 20 hours after
the end of the infusion. No predisposing factor to this complication was detected in these 4 patients regarding age,
etiology ( 2 with idiopathic dilated cardiomyopathy, 1
ischemic, and 1 chronic Chagas heart disease), and severity of cardiac failure (3 in class 111), electrolyte status,
digoxin levels, or previous use of antiarrhythmic drugs
(in only 2 cases: amiodarone in one and disopyramide in
the other). On the other hand, the QT interval corrected
for heart rate (QT,) was consistently increased following
berberine administration in all patients. In the group
without arrhythmic side effects, the QT, increased from
0.42 (0.34-0.50) in baseline condition to 0.48 (0.40-0.59)
after berberine. In the 4 patients who developed VT, the
QT, increased from 0.38, 0.52, 0.46, and 0.43 in baseline, to, respectively, 0.50, 0.59, 0.55, and 0.58 during
the hemodynamic determinations after berberine infusion
at the rate of 0.2 mg/kg per min. In 4 patients of the group
without VT in whom the QT, was evaluated 12 h after
the berberine infusion, its value was: 0.46, 0.56, 0.56,
and 0.50. In the patients who had VT, the QT, was still
excessively prolonged 12 h after the cessation of berberine infusion: 0.60, 0.70, 0.66, 0.64.No other ECG
changes were seen in either group.
Clinical control of the ventricular tachycardia was
achieved in all cases by cardioversion and isoproterenol
administration. A remarkable hemodynamic stability was
observed during the VT episodes, even though these patients had striking curtailment of cardiovascular reserve
in baseline condition. The QT, interval was gradually
reduced, returning to baseline values around 24 h after
the infusion of barberine.
All patients studied had otherwise uneventful discharge
from the hospital a few days after the cardiac catheterization date.
Discussion
The goal of this investigation was to examine the acute
hemodynamic effects of intravenous BBR administration
in patients with refractory chronic congestive heart failure.
Our results indicate that BBR evoked significant
hemodynamic effects in these patients, at the infusion rate
of 0.2 mg/kg per min. A marked reduction in systemic
and pulmonary vascular resistance, coupled with increased
cardiac output, resulted in significant decreases in both
systemic and pulmonary arterial pressures. The filling
pressures of both ventricles were lowered, and such reduction was associated with increased stroke index, showing
a shift in the Frank-Starling curve upward and to the left.
Further evidence of improvement in cardiovascular function is shown by favorable BBR effects on several
hemodynamic and echocardiographic indices of left ventricular performance. Correspondent with the increase in
cardiac output elicited by BBR, an important reduction
was detected in the systemic arteriovenous difference of
oxygen content.
The hemodynamic improvement in these patients during BBR administration is probably due to an effective
unloading of both ventricles combined with stimulation
of the inotropic state of the myocardium. Arteriolar
vasodilatation was certainly responsible for the drop in
systemic pressure and resistance during BBR. Although
no significant changes in ventricular diastolic volumes
could be detected by angiographic or echocardiographic
methods, a major salutary decreasing effect on ventricular afterload was surely induced by BBR, due to
diminished vascular resistance, and ventricular pressurevolume values during systole. That this, in fact, was the
case is shown by a decrease in left ventricular systolic
dimension and by the increase in left ventricular ejection
fraction. On the other hand, a possible direct venodilator
effect of BBR cannot be ascertained from this study, because no attempt was made to measure capacitance in
venous beds. Nevertheless, a beneficial effect of BBR on
preload conditions was evoked, at least in terms of the
marked decreases in ventricular filling pressures that were
correspondent to significantly reduced systemic and pulmonary venous pressures. Finally, the changes in the indices of inotropism, as measured during both the isovolumic and the ejection phases of contraction, suggest a
modificationof the contmctile state of the myocardium during BBR administration. It is known that such indices can
be influenced by concomitant changes in heart rate,
preload, and afterload11-14
conditions. However, it should
be noted that no change in heart rate was seen, and that a
reduction in ventricular filling pressure, as measured during BBR, should tend to decrease, instead of increase the
isovolumic phase indices of performance. Furthermore, the
hypothesis of a positive inotropic effect during BBR is corroborated by the fact that some isovolumic phase indices
(e.g., the rate of developmentof pressure at the developed
isovolumic pressure of 40 mmHg) are quite insensitive to
J. A. Marin Net0 et al. : Berberine in human heart failure
afterload changes. Whether the change in inotropic state
is due to direct effects of BBR (as suggested by the evidence
from animal experiment~~-~)
or reflex stimulation elicited
by the drop in arterial pressure, cannot be ascertained in
the conditions of the present study. On the other hand, in
vitro studies with isolated vascular smooth muscle would
need to be performed to assess direct vasodilating properties of berberine. Also, the relative vasodilator versus inotropic effects should be further elucidated by comparison,
in the same patients, of changes induced in vascular
resistance and in the indices of contractility by pure inotropes such as dob~tamine~
or pure vasodilators such as
nitroprusside.
Apart from defects of alveolar ventilation, perfusion, and
diffusion, many patients in heart failure have the potential
for venous admixture disturbances.I 6 . l 7 Moreover, the potent vasodilators often used in this context may produce
deleterious effects because of further increase in the net
physiologic right-to-left shunt, thus leading to reduced sysIn our patients, BBR augtemic arterial
mented the oxygen transport, because no changes were detected in arterial oxygen tension (PaO,) or in the
hemoglobin-oxygenbinding characteristics(Pso), but cardiac output was increased. However, it may be concluded
that BBR does not cause increased ventilation-perfusion
matching abnormalities, nor does it induce overriding of
local hypoxic vasoconstriction in the lungs, at least in resting conditions. Whether this would hold true during exercise remains to be elucidated in subsequent studies.
Future experimental and clinical studies need also to define whether the occurrence of ventricular tachycardia of
torsades de pointes type in 4 of our patients was due to
electrophysiologicaleffects of berberine. In normal dogs,
anesthetized with morphine-pentobarbital, no significant
effects were noticed in depolarization or conduction properties of atrial, junctional, and ventriculartissues, in a study
being carried out in our laboratory. In addition, we did not
perform Holter monitoring of patients before and after BBR
administration, to check if sustained ventricular arrhythmias were already present in baseline condition. However,
BBR does appear to have antiarrhythmic effects,2.6.7 in
animal models. Thus, it may be reasoned that BBR could
possess the potential for aggravationor provocation of ventricular arrhythmias, as shown by evidence from studies
with other antiarrhythmicdrugs.Z0-22
This important point
should be scrutinized carefully before the use of BBR can
be recommended for patients in heart failure for its promising effects on ventricular performance and peripheral
resistance. Further studies are now in progress in our
laboratory, exploring possible electrophysiologicalactions
of BBR on the repolarization properties of the canine myocardium. It should be stressed that the mechanisms possibly responsible for the actions of berberine upon the contractile state and vasoregulation are still unknown. In a recent study of isolated guinea pig atrial tissue, it has been
suggested that berberine enhancement of the force-velocity
relationship and of the duration of the active state may be
259
due to alteration in transsarcolemmal flux of calcium and
inhibition of intracellularcalcium sequestration system.23
On the other hand, inhibition of rat acetylcholinesterasehas
been postulated as a contributory factor to the hypotensive
action of berberine.24
Acknowledgments
We are grateful to Professor SCrgio H. Ferreira (Pharmacology Department, Medical School of Ribeifio Preto), and to Dr. Peter R. Moroko, for the stimulus and expert research assistance during this study.
We also acknowledge the excellent work of Mrs.EdnCia
F. Verceze in typing this manuscript.
References
1. Maroko PR, Zalewski A, Krol R, Cheung WM: Protoberberine alkaloids - a new family of inotropic agents (abstr). Circulation 66 (suppl 11), 137 (1982)
2. Krol R, Zalewski A, Cheung WM, Maroko PR: Additive effects of berberine and ouabain on myocardial contractility
(abstr). Clin Res 30 (3), 673-A (1982)
3. Vik-Mo H, Faria DB, Cheung WH, Maroko PR: Beneficial
effects of berberine on left ventricular function in dogs with
heart failure (abstr). Clin Res 3 I , 224-A (1 983)
4. Zalewski A, Krol R, Maroko PR: Berberine, a new inotropic
agent - distinction between its cardiac and peripheral responses
(abstr). Clin Res 31 (2), 227-A (1983)
5. Krol R, Zalewski A, Maroko PR: Beneficial effects of berberine, a new positive inotropic agent, on digitalis-induced ventricular arrhythmias (abstr). Circulation 66 (suppl. II), 56 (1982)
6. Ksiezycka E, Cheung WM, Maroko PR: Antiarrhythmic effects of berberine on aconitine-induced ventricular and supraventricular arrhythmias (abstr). Clin Res 312, 197-A (1983)
7. Ribeiro LGT, Bowker BL, Maroko PR: Beneficial effects of
berberine on early mortality after experimental coronary artery
occlusion in rats (abstr). Circulation 66 (suppl II), 56 (1982)
8. Kurnik PB, Tiefenbmnn AJ, Ludbrook PA: Peripheral
hemodynamic effects of intraventricular and intracoronaty contrast media in man. Invest Radiol 20, 203 (1985)
9. Yang SS, Bentivoglio LG, MaranhHo V, Goldberg H: Assessment of ventricular function. In From Cardiac Catheterization
Data to Hemodynamic Parameters. F. A. Davis Co., Philadelphia (1978) 233
10. Sandler H, Dodge HT: The use of single-plane angiocardiograms for the calculation of left ventricular volume in man.
Am Heart J 75, 325 (1968)
11. HirshleiferJ, Crawford M, ORourke RA, Kadiner JS: Influence
of acute alterations in heart rate and systemic arterial pressure
on echocardiographic measures of left ventricular performance
in normal human subjects. Circulation 52, 835 (1975)
12. Mason DT, Braunwald E, Covell JW, Sonnenblick EH, Ross
J Jr: Assessment of cardiac contractility. The relation between
the rate of pressure rise and ventricular pressure during isovolumic systole. Circulation 44,47 (1971)
13. Quinones MA, Gaasch WH, Alexander JK: Influence of acute
changes in preload, afterload, contractile state and heart on ejection and isovolumic indices of myocardial contractility in man.
Circulation 53, 293 (1976)
260
Clin. Cardiol. Vol. 11, April 1988
14. Rankin LS, Moos S , Grossman W: Alterations in preload and
15.
16.
17.
18.
ejection phase indices of left ventricular performance. Circularion 51, 910 (1975)
Colucci WS, Wright RF, Jaski BE, Fifer MA, Braunwald E:
Milrinone and dobutamine in severe heart failure: Differing
hernodynamic effects and individual patient responsiveness. Circulation 73, 111, 175 (1986)
Colley PS, Cheney FW: Sodium nitmprusside increases qs/qt
in dogs with regional atelectasis. Anesthesiology 47,338 (1977)
Mookhejee S , Fuleihan D, Warner RA, Vardan S,Obeid AI:
Effects of sublingual nitroglycerin on resting pulmonary gas
exchange and hemodynamics in man. Circulation 57, 106
(1978)
Mookhejee S , Keighley JFH, Warner RA, Bowser MA, Obeid
AI: Hemodynamic, ventilatory and blood gas changes during
infusion of sodium nitmfenicyanide (nitroprusside). Chest 72,
273 (1977)
19. Hales CA, Westphal D: Hypoxemia following administration
of sublingual nitroglycerin. Am J Cardiol 65, 91 1 (1978)
20. Poser RF, Podrid PJ, Lombardi F, Lown B: Aggravation of
arrhythmia induced with antiarrhythmic drugs during electrophysiologic testing. Am Heart J 110, 9 (1985)
2 1. T o m s V, Flowers D, Somberg JC: The arrhythmogenicity of
antiarrhythmic agents. Am Hearr J 109, 1090 (1985)
22. Velebit V, Podrid P, Lown B, Cohen BH, Graboys TB: Aggravation and provocation of ventricular arrhythmias by antiarrhythmic drugs. Circulation 65, 886 (1982)
23. Shaffer JE: Inotropic and chronotmpic activity of berberine on
isolated guinea pigs atria. J Cardiovasc Pharmacol 7, 307
(1985)
24. Chun YT, Yip TT, Lav KL, Kong YC: A biochemical study
of the hypotensive effect of berberine in rats. Cen Pharmacol
10, 177 (1979)
Das könnte Ihnen auch gefallen
- Blood Film Preparation and Staining Procedures: Erend OuwenDokument7 SeitenBlood Film Preparation and Staining Procedures: Erend OuwenSuresh Kumar RamanathanNoch keine Bewertungen
- Claire Tdp12 MembersonlyDokument78 SeitenClaire Tdp12 Membersonlysuri_2113Noch keine Bewertungen
- MaheswaramDokument1 SeiteMaheswaramsuri_2113Noch keine Bewertungen
- Berberine CollagenDokument1 SeiteBerberine Collagensuri_2113Noch keine Bewertungen
- Oecd GL423Dokument14 SeitenOecd GL423Sheldon Jay SilvaNoch keine Bewertungen
- Blood Film Preparation and Staining Procedures: Erend OuwenDokument7 SeitenBlood Film Preparation and Staining Procedures: Erend OuwenSuresh Kumar RamanathanNoch keine Bewertungen
- ZXCVBDokument4 SeitenZXCVBsuri_2113Noch keine Bewertungen
- New Aspects of Saccharomyces Cerevisiae As ADokument8 SeitenNew Aspects of Saccharomyces Cerevisiae As Asuri_2113Noch keine Bewertungen
- Oecd Guideline For The Testing of ChemicalsDokument29 SeitenOecd Guideline For The Testing of Chemicalssuri_2113Noch keine Bewertungen
- Blood Film Preparation and Staining Procedures: Erend OuwenDokument7 SeitenBlood Film Preparation and Staining Procedures: Erend OuwenSuresh Kumar RamanathanNoch keine Bewertungen
- Reqest For Proposal (RFP) and Schedules PDFDokument37 SeitenReqest For Proposal (RFP) and Schedules PDFsuri_2113Noch keine Bewertungen
- Type I Collagen Extracted From Rat-Tail and BovineDokument12 SeitenType I Collagen Extracted From Rat-Tail and Bovinesuri_2113Noch keine Bewertungen
- ZXCVBDokument4 SeitenZXCVBsuri_2113Noch keine Bewertungen
- A Collagen Peptide-Based Physical Hydrogel ForDokument6 SeitenA Collagen Peptide-Based Physical Hydrogel Forsuri_2113Noch keine Bewertungen
- Emulsifying Fibers Effect of PH, ProteinDokument9 SeitenEmulsifying Fibers Effect of PH, Proteinsuri_2113Noch keine Bewertungen
- A Collagen Peptide-Based Physical Hydrogel ForDokument6 SeitenA Collagen Peptide-Based Physical Hydrogel Forsuri_2113Noch keine Bewertungen
- Net JRFDokument10 SeitenNet JRFB. Rajeev Kungur100% (2)
- PHD Brochure 2012Dokument17 SeitenPHD Brochure 2012suri_2113Noch keine Bewertungen
- Shilajit An Ancient PanaceaDokument10 SeitenShilajit An Ancient PanaceaRahul SrivastavNoch keine Bewertungen
- Revision HistoryDokument9 SeitenRevision HistoryVictOr VFNoch keine Bewertungen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Long Test 2 - Science 6: Match The Excretory Organs in COLUMN B With Its Description in COLUMN ADokument3 SeitenLong Test 2 - Science 6: Match The Excretory Organs in COLUMN B With Its Description in COLUMN Akatherine corveraNoch keine Bewertungen
- MurmursDokument10 SeitenMurmursAlina KievskyNoch keine Bewertungen
- Ebook - Artes Marciais - DR Jwing-Ming Yang - Tai Chi - Qigong - The Secret of YouthDokument33 SeitenEbook - Artes Marciais - DR Jwing-Ming Yang - Tai Chi - Qigong - The Secret of YouthsabaraceifadorNoch keine Bewertungen
- Dr. Az Rifki, Span - Kic Departemen Anestesiologi Dan Reanimasi Rsi Siti Rahmah/Fk-Fkg Universitas Baiturrahmah PadangDokument62 SeitenDr. Az Rifki, Span - Kic Departemen Anestesiologi Dan Reanimasi Rsi Siti Rahmah/Fk-Fkg Universitas Baiturrahmah PadangKamelia MarcshendaNoch keine Bewertungen
- Cardiac Catheterization ProcedureDokument10 SeitenCardiac Catheterization ProcedureDimpal Choudhary100% (4)
- Basic Coronary Angiography - All Slides PDFDokument55 SeitenBasic Coronary Angiography - All Slides PDFCarlos Arroyo0% (1)
- Prof 1, Sem 1 L 45 - CLASSIFICATION OF AKHLAT (HUMOURSDokument14 SeitenProf 1, Sem 1 L 45 - CLASSIFICATION OF AKHLAT (HUMOURSMI Manuha100% (1)
- Atlas Histology of HeartDokument2 SeitenAtlas Histology of HeartYasir HadyNoch keine Bewertungen
- Massage and The Lymphatic SystemDokument9 SeitenMassage and The Lymphatic Systemarmanious64Noch keine Bewertungen
- Anaesthesia FOR Closed Heart ProcedureDokument45 SeitenAnaesthesia FOR Closed Heart ProcedureVaibhav JainNoch keine Bewertungen
- ESC Arterial Hypertension 2018Dokument98 SeitenESC Arterial Hypertension 2018ddantoniusgmailNoch keine Bewertungen
- What Keeps The Blood Moving!Dokument25 SeitenWhat Keeps The Blood Moving!mikeeNoch keine Bewertungen
- Cardiovascular Summary Saunders Comprehensive Review For The Nclex RN ExaminationDokument40 SeitenCardiovascular Summary Saunders Comprehensive Review For The Nclex RN ExaminationdanicaNoch keine Bewertungen
- Equine Veterinary - Circulatory System - Horse First AiDokument1 SeiteEquine Veterinary - Circulatory System - Horse First AiRenan RodriguesNoch keine Bewertungen
- Shkagld STD 7 Science Revision Worksheet 2019 2020Dokument3 SeitenShkagld STD 7 Science Revision Worksheet 2019 2020YashaswiNoch keine Bewertungen
- Functions of The Circulatory SystemDokument4 SeitenFunctions of The Circulatory SystemMaria Charma AnlapNoch keine Bewertungen
- Chapter 12Dokument28 SeitenChapter 12Muhammad AmirNoch keine Bewertungen
- AAUA Post UTME Past Questions and Answers EduNgr PDFDokument121 SeitenAAUA Post UTME Past Questions and Answers EduNgr PDFbbllngNoch keine Bewertungen
- Summarizing and ParaphrasingDokument14 SeitenSummarizing and ParaphrasingRia NirwanaNoch keine Bewertungen
- Pig Heart and Lung Dissection ProcedureDokument2 SeitenPig Heart and Lung Dissection ProcedurelchamblessNoch keine Bewertungen
- Comprehensive Surgical Management of Congenital Heart DiseaseDokument561 SeitenComprehensive Surgical Management of Congenital Heart DiseaseMardari Claudiu100% (4)
- Lesson Plan No 5Dokument6 SeitenLesson Plan No 5hafeez ahmedNoch keine Bewertungen
- Pitting and Non-Pitting Oedema: Clinical SkillsDokument3 SeitenPitting and Non-Pitting Oedema: Clinical SkillsDinnar Ulya FauziahNoch keine Bewertungen
- Mutia Sukma Dewi 2010.04.0.0142 (Jurnal) PDFDokument12 SeitenMutia Sukma Dewi 2010.04.0.0142 (Jurnal) PDFmutiaNoch keine Bewertungen
- NCP For Acute Coronary SyndromeDokument3 SeitenNCP For Acute Coronary Syndromesarahtot75% (4)
- Cardiac Tamponad E: Pathophysiology and ManagementDokument105 SeitenCardiac Tamponad E: Pathophysiology and ManagementBimaNoch keine Bewertungen
- Activity 12 Lymphatic and Immune System PDFDokument3 SeitenActivity 12 Lymphatic and Immune System PDFmicaela bernaldezNoch keine Bewertungen
- Cal EcgDokument7 SeitenCal EcgNur Amirah FarhanahNoch keine Bewertungen
- ACC/AHA Heart Failure Classification: Nyha Class SymptomsDokument2 SeitenACC/AHA Heart Failure Classification: Nyha Class SymptomsZoher PainterNoch keine Bewertungen
- The Bainbridge and The Reverse Bainbridge.8Dokument13 SeitenThe Bainbridge and The Reverse Bainbridge.8Archisha KapoorNoch keine Bewertungen