Beruflich Dokumente
Kultur Dokumente
RWJF Regional Health Collaboratives PDF
Hochgeladen von
iggybauOriginalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
RWJF Regional Health Collaboratives PDF
Hochgeladen von
iggybauCopyright:
Verfügbare Formate
Quality Field Notes
NUMBER 6
JANUARY 2015
Regional Health Improvement Collaboratives
Issue Brief
What Were Learning:
Regional Collaboratives Can Improve the Value of
Local Health Care
The Challenge
Increasing the value of health care is a national issue, but health care is delivered locally, and
improving its quality and making it more affordable requires local action. Moreover, no single
person, group, or profession can go it alone.
Aligning Forces for Quality
AF4Q is the Robert Wood
Johnson Foundations
signature effort to lift the
overall quality of health
care in 16 targeted communities across America.
These briefs distill some
of the key lessons learned
by these regional alliances
of providers, patients,
and payers as they work
to transform their local
health care and provide
models for national
reform.
Aligning Forces for Quality (AF4Q) is comprised of 16 regional health improvement collaboratives
(RHICs) that bring together people who get, give, and pay for care to improve the value of health
care in their community. These multistakeholder groups include organizations that might not
otherwise collaborateincluding purchasers, patients, providers, and payers.
As an independent forum, a collaborative can serve roles no one else can, such as:
Measuring the performance of the regions providers in order to identify opportunities to
improve care and monitor progress
Facilitating payment and delivery system reforms to reward providers that deliver higherquality care, while encouraging patients to use higher-quality providers
Providing training and assistance to health care professionals so they can learn new ways to
analyze problems in care delivery and implement solutions
Educating and engaging patients in their care
Helping to plan and coordinate many different health improvement activities1
40+
Number of regional health care collaboratives in
the U.S. as of 2010.2
12.5
Percentage of the U.S. population that is covered
by Aligning Forces for Quality communities.3
Whats Working
Health care is local and improving it requires those in the community to be the
driving force for improvement. Every community is differentin its distribution of illness,
demographics, and culture. The same is true for the structure of local health care systems and the
types of cost and quality problems that patients, providers, and employers face.
RHICs are well suited to tackle local issues because they understand their markets, and can
organize and energize stakeholders. In addition, since they serve diverse geographies, no
two are alike.
The true benefit of
the multistakeholder
approach is that the
alliances create value
for all stakeholders in
the community. Instead
of each group advancing
strategies that can
conflict or compete,
they have a place where
they can come together
and reach a consensus
on how to improve care
collectively.
KATHERINE BROWNE,
CHIEF OPERATING OFFICER,
ALIGNING FORCES FOR
QUALITY NATIONAL PROGRAM
OFFICE
For example, Maine Quality Counts and Aligning Forces Humboldt serve geographically dispersed
populations where providers are stretched thin, while the Greater Detroit Area Health Council
and the Common Table Health Alliance in Memphis serve largely urban populations with a
higher density of health care systems. Collaboratives also are created based on local conditions,
and their approaches to finding solutions reflect their roots and local needs. The Maine Health
Management Coalition, organized by employers, created public reports about the quality and, later,
the cost of health care to help employers steer employees toward high-value health care providers.
These reports also enable providers to see where they can improve quality. Providers created the
Wisconsin Collaborative for Healthcare Quality, which focuses on using performance measurement
data to let its members benchmark their performance against one another and share quality
improvement techniques.
Health care collaboratives offer an independent forum for convening
stakeholders, some of whom are competitors, filling a role no one else in the
community can. All stakeholdersincluding patients, clinicians, hospitals, health plans,
businesses, and the governmentare affected by the local health care system and any changes in
it. This means that all groups need to be involved in planning and implementing change. Bringing
these unlikely partners together can be a challenging task, since they are from different industries
that have diverse and sometimes conflicting goals.4
Since RHICs do not directly deliver or pay for health care services, they provide a common table
at which stakeholders can share knowledge, skills, and resources. This gives the community a place
to plan, facilitate, and coordinate programs that can change the health care system and strengthen
community relationships.
This independence helps position RHICs as a trusted source of information. The New Mexico
Coalition for Healthcare Quality was created as a result of a need in the community for a neutral
body to bring stakeholders together to help the community move toward a more transparent health
care system. Within a year and a half of its creation, the organization published its first public
report on provider performance.
Governing structures differ among collaboratives. Some ensure that organizations of different
stripes are equally represented. Others are governed solely by representatives of one sector, such
as health care providers, but they collaborate with payers, health plans, and consumer advocates in
their external work.
Leadership is a critical factor in the success of a RHIC. Elizabeth Mitchell, CEO of the Network
for Regional Healthcare Improvement, says successful RHICs have leadership teams that excel
at building and managing relationships. Katherine Browne, chief operating officer of the AF4Q
National Program Office, says it is harder to create a value proposition that multiple stakeholders
can realize in the near term than it is if you are trying to serve only one group, such as employers,
but that is what RHICs must do.
Top Five Must Reads on Regional Health Improvement Collaboratives
1.
2.
3.
4.
1.
Regional Health Improvement Collaboratives: Essential
Elements for Successful Healthcare Reform
2.
Regional Health Improvement Collaboratives Needed Now
More Than Ever: Program Directors Perspectives
3.
Improving Health Care Quality Through Community
Collaboratives
4.
The Future of Collaboration: The Power of Collective Impact
5.
Regional Coalitions for Healthcare Improvement: Definitions,
Lessons, and Prospects
Regional Health Improvement Collaboratives: Essential Elements for Successful Healthcare Reform.
Regional Health Improvement Collaboratives: Essential Elements for Successful Healthcare Reform.
Robert Wood Johnson Foundation. 2014. Aligning Forces for Quality. Accessed September 18. http://www.rwjf.org/en/grants/grantees/aligning-forces-for-quality.html
Regional Health Improvement Collaboratives: Essential Elements for Successful Healthcare Reform.
Das könnte Ihnen auch gefallen
- Bostock v. Clayton County, Georgia DecisionDokument119 SeitenBostock v. Clayton County, Georgia DecisionNational Content DeskNoch keine Bewertungen
- A Bill: in The House of RepresentativesDokument2 SeitenA Bill: in The House of RepresentativesiggybauNoch keine Bewertungen
- AAFP Letter To Domestic Policy Council 6-10-2020Dokument3 SeitenAAFP Letter To Domestic Policy Council 6-10-2020iggybauNoch keine Bewertungen
- Boston Mayor Executive Order 6-12-2020Dokument3 SeitenBoston Mayor Executive Order 6-12-2020iggybauNoch keine Bewertungen
- HR 6437 Coronavirus Immigrant Families Protection AcfDokument16 SeitenHR 6437 Coronavirus Immigrant Families Protection AcfiggybauNoch keine Bewertungen
- S 3721 COVID-19 Racial and Ethnic Disparities Task ForceDokument11 SeitenS 3721 COVID-19 Racial and Ethnic Disparities Task ForceiggybauNoch keine Bewertungen
- HR 4004 Social Determinants Accelerator ActDokument18 SeitenHR 4004 Social Determinants Accelerator ActiggybauNoch keine Bewertungen
- S 3609 Coronavirus Immigrant Families Protection ActDokument17 SeitenS 3609 Coronavirus Immigrant Families Protection ActiggybauNoch keine Bewertungen
- Milwaukee Board of Supervisors Ordinance 20-174Dokument9 SeitenMilwaukee Board of Supervisors Ordinance 20-174iggybauNoch keine Bewertungen
- 7th Circuit Affirming Preliminary Injunction Cook County v. WolfDokument82 Seiten7th Circuit Affirming Preliminary Injunction Cook County v. WolfiggybauNoch keine Bewertungen
- HR 6585 Equitable Data Collection COVID-19Dokument18 SeitenHR 6585 Equitable Data Collection COVID-19iggybauNoch keine Bewertungen
- HR 6763 COVID-19 Racial and Ethnic Disparities Task ForceDokument11 SeitenHR 6763 COVID-19 Racial and Ethnic Disparities Task ForceiggybauNoch keine Bewertungen
- Cook County v. Wolf Denial Motion To Dismiss Equal ProtectionDokument30 SeitenCook County v. Wolf Denial Motion To Dismiss Equal ProtectioniggybauNoch keine Bewertungen
- NCAPIP Recommendations For Culturally and Linguistically Appropriate Contact Tracing May 2020Dokument23 SeitenNCAPIP Recommendations For Culturally and Linguistically Appropriate Contact Tracing May 2020iggybauNoch keine Bewertungen
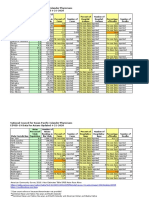
- COVID-19 Data For Native Hawaiians and Pacific Islanders UPDATED 4-21-2020 PDFDokument2 SeitenCOVID-19 Data For Native Hawaiians and Pacific Islanders UPDATED 4-21-2020 PDFiggybauNoch keine Bewertungen
- Covid-19 Data For Asians Updated 4-21-2020Dokument2 SeitenCovid-19 Data For Asians Updated 4-21-2020iggybauNoch keine Bewertungen
- SF StayHome MultiLang Poster 8.5x11 032620Dokument1 SeiteSF StayHome MultiLang Poster 8.5x11 032620iggybauNoch keine Bewertungen
- Doe v. Trump 9th Circuit Denial of Stay of Preliminary InjunctionDokument97 SeitenDoe v. Trump 9th Circuit Denial of Stay of Preliminary InjunctioniggybauNoch keine Bewertungen
- COVID 19 FaceCovering 1080x1080 4 SPDokument1 SeiteCOVID 19 FaceCovering 1080x1080 4 SPiggybauNoch keine Bewertungen
- Doe v. Trump Denial of All Writs Injunction Against April 2020 Presidential ProclamationDokument9 SeitenDoe v. Trump Denial of All Writs Injunction Against April 2020 Presidential ProclamationiggybauNoch keine Bewertungen
- Tri-Caucus Letter To CDC and HHS On Racial and Ethnic DataDokument3 SeitenTri-Caucus Letter To CDC and HHS On Racial and Ethnic DataiggybauNoch keine Bewertungen
- Doe v. Trump Preliminary Injunction Against Proclamation Requiring Private Health InsuranceDokument48 SeitenDoe v. Trump Preliminary Injunction Against Proclamation Requiring Private Health InsuranceiggybauNoch keine Bewertungen
- WA v. DHS Order On Motion To CompelDokument21 SeitenWA v. DHS Order On Motion To CompeliggybauNoch keine Bewertungen
- CDC Covid-19 Report FormDokument2 SeitenCDC Covid-19 Report FormiggybauNoch keine Bewertungen
- MMMR Covid-19 4-8-2020Dokument7 SeitenMMMR Covid-19 4-8-2020iggybauNoch keine Bewertungen
- ND California Order On Motion To CompelDokument31 SeitenND California Order On Motion To CompeliggybauNoch keine Bewertungen
- Booker-Harris-Warren Letter To HHS Re Racial Disparities in COVID ResponseDokument4 SeitenBooker-Harris-Warren Letter To HHS Re Racial Disparities in COVID ResponseStephen LoiaconiNoch keine Bewertungen
- Physician Association Letter To HHS On Race Ethnicity Language Data and COVID-19Dokument2 SeitenPhysician Association Letter To HHS On Race Ethnicity Language Data and COVID-19iggybauNoch keine Bewertungen
- Democratic Presidential Candidate Positions On ImmigrationDokument10 SeitenDemocratic Presidential Candidate Positions On ImmigrationiggybauNoch keine Bewertungen
- Pete Buttigieg Douglass PlanDokument18 SeitenPete Buttigieg Douglass PlaniggybauNoch keine Bewertungen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Answer Chapter 7Dokument4 SeitenAnswer Chapter 7Bùi Thanh Ngọc BíchNoch keine Bewertungen
- Distribution ManagementDokument13 SeitenDistribution Managementanureetcheema100% (1)
- Factors Influencing Customer Satisfaction at Kenya Airways Cargo ServiceDokument70 SeitenFactors Influencing Customer Satisfaction at Kenya Airways Cargo ServiceHACHALU FAYENoch keine Bewertungen
- Certificate of Moral Fitness ANITA MC KIGENDokument9 SeitenCertificate of Moral Fitness ANITA MC KIGENWalter Ochieng100% (4)
- 2012 UspsDokument8 Seiten2012 Uspsapi-167783914Noch keine Bewertungen
- ArrestDokument7 SeitenArrestBar TopnocherNoch keine Bewertungen
- Whole Brain Literacy Self - Mastery: Capability Building ProgramDokument2 SeitenWhole Brain Literacy Self - Mastery: Capability Building ProgramRhea Loida Bernabe-AngelNoch keine Bewertungen
- AIDA Model For NetflixDokument4 SeitenAIDA Model For NetflixLakshmi ShuklaNoch keine Bewertungen
- Rifts d20 Conversion Manual v34Dokument192 SeitenRifts d20 Conversion Manual v34bossloki67% (3)
- Listening Strategies.: Top Down and The Bottom UpDokument2 SeitenListening Strategies.: Top Down and The Bottom Upmartin100% (1)
- How To Get Rich - Jared DiamondDokument11 SeitenHow To Get Rich - Jared DiamondRommel Acosta100% (1)
- Business PolicyDokument40 SeitenBusiness PolicyTage Nobin100% (2)
- 5 Families - Teaching StrategiesDokument1 Seite5 Families - Teaching StrategiesZiyan SheriffNoch keine Bewertungen
- "Entrepreneurship": Overview ofDokument20 Seiten"Entrepreneurship": Overview ofKathy Cameros Dela PazNoch keine Bewertungen
- Information and Data Security: Dr. B. Chandra MohanDokument16 SeitenInformation and Data Security: Dr. B. Chandra MohanADITYA SINGHNoch keine Bewertungen
- Activity Completion Report: A Lampshade Making ProjectDokument7 SeitenActivity Completion Report: A Lampshade Making ProjectciriloNoch keine Bewertungen
- SAP HR Interview Questions and Answers - SAP Training TutorialsDokument3 SeitenSAP HR Interview Questions and Answers - SAP Training TutorialsPradeep KumarNoch keine Bewertungen
- Formality in Writing: Aspect of Professional and Academic LanguageDokument62 SeitenFormality in Writing: Aspect of Professional and Academic LanguageTimNoch keine Bewertungen
- Obtl Understanding Culture, Society and Politics JeffDokument7 SeitenObtl Understanding Culture, Society and Politics JeffJeffrey MasicapNoch keine Bewertungen
- Myp4 Common Formative Assessment Unit 3Dokument4 SeitenMyp4 Common Formative Assessment Unit 3Sherif RamadanNoch keine Bewertungen
- Reading PlanDokument3 SeitenReading PlanMark Andrew FernandezNoch keine Bewertungen
- GAIN - Flight Safety HandbookDokument180 SeitenGAIN - Flight Safety HandbookDennis Groves100% (4)
- Visual Support Using Smarty SymbolsDokument15 SeitenVisual Support Using Smarty SymbolsSmarty SymbolsNoch keine Bewertungen
- MMHRM MCQDokument12 SeitenMMHRM MCQYusuf SiyaNoch keine Bewertungen
- Software Architecture For Developers, Volu - Simon BrownDokument200 SeitenSoftware Architecture For Developers, Volu - Simon BrownFlorgle FloopNoch keine Bewertungen
- Abakada VS PurisimaDokument3 SeitenAbakada VS PurisimaLuna BaciNoch keine Bewertungen
- HSM 386 2 Level 2 Strip Cut Professional Paper Shredder ManualDokument4 SeitenHSM 386 2 Level 2 Strip Cut Professional Paper Shredder Manualbob bobNoch keine Bewertungen
- D.N.R. College of Engineering &technologyDokument1 SeiteD.N.R. College of Engineering &technologyeshwari369Noch keine Bewertungen
- ADR Nov 20Dokument4 SeitenADR Nov 20Lara De los SantosNoch keine Bewertungen
- Payment of Bonus Act 1965Dokument14 SeitenPayment of Bonus Act 1965Achin SharmaNoch keine Bewertungen