Beruflich Dokumente
Kultur Dokumente
This
Hochgeladen von
vicenteturasCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
This
Hochgeladen von
vicenteturasCopyright:
Verfügbare Formate
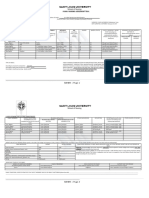
POST OP NURSING
INTERVENTIONS
DIAGNOSTIC
DESCRIPTION
PRE OP NURSING INTERVENTIONS
REFERENC
ES
Laboratory tests
Fecal occult blood
test.
Stool culture
A fecal occult blood test checks for hidden
(occult) blood in the stool. It involves placing
a very small amount of stool on a special
card, which is then tested in the doctor's
office or sent to a laboratory.
Nursing Interventions Instruct the patient
to keep the stool specimen free of urine
or toilet paper, since either can alter the
test results. The nurse or patient should
don gloves and use tongue blades to
transfer the stool to the proper
receptacle. The patient should keep the
diet free of organ meat for 24 to 48 hours
before a guaiac tes
A stool culture checks for the presence of
abnormal bacteria in the digestive tract that
may cause diarrhea and other problems. A
small sample of stool is collected and sent to
a laboratory by your doctor's office. In two or
three days, the test will show whether
abnormal bacteria are present.
Nursing Interventions If an enema must
be administered to collect specimens,
use only normal saline or tap water.
Soapsuds or any other substance could
affect the viability of the organisms
collected. Stool samples for O&P are
obtained before barium examinations.
Instruct the patient not to mix urine with
feces. Don gloves to collect the
specimen, and ensure the specimen is
taken to the laboratory within 30 minutes
of collection in specifi ed container.
During the postoperative
period, reestablishing the
patients physiologic balance,
pain management and
prevention of complications
should be the focus of the
nursing care. To do these it is
crucial that the nurse perform
careful assessment and
immediate intervention in
assisting the patient to optimal
function quickly, safely and
comfortably as possible.
1. Maintaining
adequate body
system functions.
2. Restoring body
homeostasis.
3. Pain and
discomfort
alleviation.
4. Preventing
postoperative
complications.
5. Promoting
adequate
discharge planning
and health
teaching.
Lauritsen
Christensen,
B. (n.d.).
Care of the
Patient with
a
Gastrointesti
nal Disorder.
Retrieved
from
AdultHealth
6e_ch5.pdf
Beauchamp,
Daniel R.,
M.D., Mark
B. Evers,
M.D.,
Kenneth L.
Mattox,
M.D.,
Courtney M.
Townsend,
and David
C. Sabiston,
eds. Sabisto
n Textbook
of Surgery:
The
Biological
Basis of
Modern
Surgical
Imaging tests
Barium
beefsteak meal.
Colorectal
transit study.
Computed
tomography
scan (CT or CAT
scan).
During this test, the patient eats a meal
containing barium (a metallic, chalky liquid
used to coat the inside of organs so that they
will show up on an X-ray), allowing the
radiologist to watch the stomach as it digests
the meal. The amount of time it takes for the
barium meal to be digested and leave the
stomach gives the doctor an idea of how well
the stomach is working and helps to detect
emptying problems that may not show up on
the liquid barium X-ray.
This test shows how well food moves
through the colon. The patient swallows
capsules containing small markers which are
visible on X-ray. The patient follows a highfiber diet during the course of the test, and
the movement of the markers through the
colon is monitored with abdominal X-rays
taken several times three to seven days after
the capsule is swallowed.
This diagnostic imaging procedure uses a
combination of X-rays and computer
technology to produce horizontal, or
axial, images (often called slices) of the
body. A CT scan shows detailed images of
any part of the body, including the bones,
muscles, fat, and organs. CT scans are more
detailed than general X-rays.
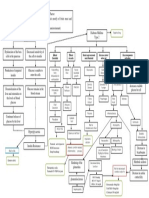
P Preventing and/or relieving
complications
O Optimal respiratory
function
S Support: psychosocial
well-being
T Tissue perfusion and
cardiovascular status
maintenance
O Observing and
maintaining adequate fluid
intake
P Promoting adequate
nutrition and elimination
A Adequate fluid and
electrolyte balance
R Renal function
maintenance
E Encouraging activity and
mobility within limits
T Thorough wound care for
adequate wound healing
I Infection Control
V Vigilant to manifestations
of anxiety and promoting ways
of relieving it
E Eliminating environmental
hazards and promoting client
safety
GI Function and Nutrition
If in place,
maintain
nasogastric tube
and monitor
patency and
drainage.
Practice. 16t
h ed.
London: W.
B. Saunders
Co., 2001.
Read
more: http://
www.surger
yencycloped
ia.com/PaSt/Preoperat
iveCare.html#ix
zz3p8rGcSD
R
Vera, RN,
M. (Ed.).
(2014,
January 23).
Postoperativ
e Phase.
Defecograph
Lower GI
(gastrointestinal)
series (also
called barium
enema).
Defecography is an X-ray of the anorectal
area that evaluates completeness of stool
elimination, identifies anorectal
abnormalities, and evaluates rectal muscle
contractions and relaxation. During the
examination, the patient's rectum is filled with
a soft paste that is the same consistency as
stool. The patient then sits on a toilet
positioned inside an X-ray machine, and
squeezes and relaxes the anus to expel the
solution. The doctor studies the X-rays to
determine if anorectal problems occurred
while the patient was emptying the paste
from the rectum.
A lower GI series is a procedure that
examines the rectum, the large intestine, and
the lower part of the small intestine. Barium
is given into the rectum as an enema. An Xray of the abdomen shows strictures
(narrowed areas), obstructions (blockages),
and other problems.
Magnetic
resonance
imaging (MRI).
MRI is a diagnostic procedure that uses a
combination of large magnets,
radiofrequencies, and a computer to produce
detailed images of organs and structures
within the body. The patient lies on a bed that
moves into the cylindrical MRI machine. The
machine takes a series of pictures of the
inside of the body using a magnetic field and
radio waves. The computer enhances the
pictures produced. The test is painless, and
does not involve exposure to radiation.
Because the MRI machine is like a tunnel,
Provide
symptomatic
therapy, including
antiemetic
medications for
nausea and
vomiting.
Administer
phenothiazine
medications as
prescribed
for severe,
persistent hiccups.
Assist patient to
return to normal
dietary intake
gradually at a
pace set by patient
(liquids rst, then
soft foods, such as
gelatin, junket,
custard, milk, and
creamed soups,
are added
gradually, then
solid food).
Remember that
paralytic ileus and
intestinal
obstruction
are potential
postoperative
complications that
occur more frequently in patients
undergoing
intestinal or
abdominal
surgery.
Arrange for patient
some people are claustrophobic or unable to
hold still during the test, and may be given a
sedative to help them relax. Metal objects
cannot be present in the MRI room, so
people with pacemakers or metal clips or
rods inside the body cannot have this test
done. All jewelry must be removed before the
procedure.
Magnetic
resonance
cholangiopancre
atography
(MRCP).
Oropharyng
eal motility
(swallowing)
study.
Radioisotop
e gastricemptying scan.
Ultrasound.
This test uses magnetic resonance imaging
(MRI) to view the bile ducts. The machine
uses radio waves and magnets to scan
internal tissues and organs.
This is a study in which the patient is given
small amounts of a liquid containing barium
to drink with a bottle, spoon, or cup. A series
of X-rays is taken to evaluate what happens
as the liquid is swallowed.
During this test, the patient eats food
containing a radioisotope, which is a slightly
radioactive substance that will show up on a
scan. The dosage of radiation from the
radioisotope is very small and not harmful,
but allows the radiologist to see the food in
the stomach and how quickly it leaves the
stomach, while the patient lies under a
machine.
to consult with the
dietitian to
plan appealing,
high-protein meals
that provide
sufcient
ber, calories, and
vitamins.
Nutritional
supplements, such
as Ensure or
Sustacal, may be
recommended.
Instruct patient to
take multivitamins,
iron, and vitamin
C supplements
postoperatively if
prescribed
Drainage
Presence of
drainage, need to
connect tubes to a
specific drainage
system, presence
and condition of
dressings
Ultrasound is a diagnostic imaging
technique that uses high-frequency sound
waves and a computer to create images of
blood vessels, tissues, and organs.
Ultrasounds are used to view internal organs
as they function, and to assess blood flow
through various vessels. Gel is applied to the
area of the body being studied, such as the
abdomen, and a wand called a transducer is
placed on the skin. The transducer sends
sound waves into the body that bounce off
organs and return to the ultrasound machine,
producing an image on the monitor. A picture
or videotape of the test is also made so it can
be reviewed in the future.
Upper GI
(gastrointestinal)
series (also
called barium
swallow).
Upper GI series is a diagnostic test that
examines the organs of the upper part of the
digestive system: the esophagus, stomach,
and duodenum (the first section of the small
intestine). Barium is swallowed and X-rays
are then taken to evaluate the digestive
organs.
Endoscopic
procedures
Colonoscopy
.
Colonoscopy is a procedure that allows
the doctor to view the entire length of the
large intestine (colon), and can often help
identify abnormal growths, inflamed tissue,
ulcers, and bleeding. It involves inserting a
colonoscope, a long, flexible, lighted tube, in
through the rectum up into the colon. The
colonoscope allows the doctor to see the
lining of the colon, remove tissue for further
examination, and possibly treat some
problems that are discovered.
Endoscopic
retrograde
cholangiopancre
atography
(ERCP).
Esophagogastroduo
denoscopy (also
called EGD or upper
endoscopy).
Sigmoidosco
py
ERCP is a procedure that allows the doctor
to diagnose and treat problems in the liver,
gallbladder, bile ducts, and pancreas. The
procedure combines X-ray and the use of an
endoscope, a long, flexible, lighted tube. The
scope is guided through the patient's mouth
and throat, then through the esophagus,
stomach, and duodenum (the first part of the
small intestine). The doctor can examine the
inside of these organs and detect any
abnormalities. A tube is then passed through
the scope, and a dye is injected that will
allow the internal organs to appear on an Xray.
An EGD (upper endoscopy) is a procedure
that allows the doctor to examine the inside
of the esophagus, stomach, and duodenum
with an endoscope, which is guided into the
mouth and throat, then into the esophagus,
stomach, and duodenum. The endoscope
allows the doctor to view the inside of this
area of the body, as well as to insert
instruments through the scope for the
removal of a sample of tissue for biopsy (if
necessary).
A sigmoidoscopy is a diagnostic procedure
that allows the doctor to examine the inside
of a portion of the large intestine, and is
helpful in identifying the causes of diarrhea,
abdominal pain, constipation, abnormal
growths, and bleeding. A short, flexible,
lighted tube, called a sigmoidoscope, is
inserted into the intestine through the rectum.
The scope blows air into the intestine to
inflate it and make viewing the inside easier.
Other procedures
Anorectal
manometry.
Esophageal
manometry.
Esophageal
pH monitoring
This test helps determine the strength of the
muscles in the rectum and anus. These
muscles normally tighten to hold in a bowel
movement and relax when a bowel
movement is passed. Anorectal manometry
is helpful in evaluating anorectal
malformations and Hirschsprung's disease,
among other problems. A small tube is
placed into the rectum to measure the
pressures exerted by the sphincter muscles
that ring the canal.
This test helps determine the strength of the
muscles in the esophagus. It is useful in
evaluating gastroesophageal reflux and
swallowing abnormalities. A small tube is
guided into the nostril, then passed into the
throat, and finally into the esophagus. The
pressure the esophageal muscles produce at
rest is then measured.
An esophageal pH monitor measures the
acidity inside of the esophagus. It is helpful in
evaluating gastroesophageal reflux disease
(GERD). A thin, plastic tube is placed into a
nostril, guided down the throat, and then into
the esophagus. The tube stops just above
the lower esophageal sphincter, which is at
the connection between the esophagus and
the stomach. At the end of the tube inside the
esophagus is a sensor that measures pH, or
acidity. The other end of the tube outside the
body is connected to a monitor that records
the pH levels for a 24- to 48-hour period.
Normal activity is encouraged during the
study, and a diary is kept of symptoms
experienced, or activity that might be
suspicious for reflux, such as gagging or
coughing, and any food intake by the patient.
It is also recommended to keep a record of
the time, type, and amount of food eaten.
The pH readings are evaluated and
compared to the patient's activity for that
time period.
Capsule
endoscopy.
A capsule endoscopy helps doctors examine
the small intestine, because traditional
procedures, such as an upper endoscopy or
colonoscopy, cannot reach this part of the
bowel. This procedure is helpful in identifying
causes of bleeding, detecting polyps,
inflammatory bowel disease, ulcers, and
tumors of the small intestine. A sensor device
is placed on a patient's abdomen and a
PillCam is swallowed. The PillCam passes
naturally through the digestive tract while
transmitting video images to a data recorder.
The data recorder is secured to a patient's
waist by a belt for eight hours. Images of the
small bowel are downloaded onto a
computer from the data recorder. The images
are reviewed by a doctor on a computer
screen. Normally, the PillCam passes
through the colon and is eliminated in the
stool within 24 hours.
Gastric
manometry
Magnetic
resonance
cholangiopancre
atography
(MRCP).
This test measures electrical and muscular
activity in the stomach. The doctor passes a
thin tube down the patient's throat into the
stomach. This tube contains a wire that takes
measurements of the electrical and muscular
activity of the stomach as it digests foods
and liquids. This helps show how the
stomach is working, and if there is any delay
in digestion.
This test uses magnetic resonance imaging
(MRI) to obtain pictures of the bile ducts. The
machine uses radio waves and magnets to
scan internal organs and tissues.
Das könnte Ihnen auch gefallen
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (120)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- Autism Reversal Toolbox + Full + PDF + Free + Jerry KantorDokument215 SeitenAutism Reversal Toolbox + Full + PDF + Free + Jerry Kantorrodolfo_soberón100% (25)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- Gastrointestinal DisordersDokument118 SeitenGastrointestinal DisordersAhmad MakhloufNoch keine Bewertungen
- Digestive System: Submitted By: Caimoso, Tricia Ann D. Quiambao, Aliyah Lourdes D. Bs Psychology 3-3Dokument9 SeitenDigestive System: Submitted By: Caimoso, Tricia Ann D. Quiambao, Aliyah Lourdes D. Bs Psychology 3-3Tricia Ann CaimosoNoch keine Bewertungen
- PhoenixDokument3 SeitenPhoenixvicenteturas100% (1)
- GitDokument23 SeitenGitHannah Meriel Del MundoNoch keine Bewertungen
- Case Study-Ectopic PNDokument55 SeitenCase Study-Ectopic PNArbie Jacinto100% (2)
- Gerd, Peptic Ulcer, Ulcerative Colitis, Crohn's DiseaseDokument11 SeitenGerd, Peptic Ulcer, Ulcerative Colitis, Crohn's DiseasekamipimaNoch keine Bewertungen
- Prep 2023Dokument909 SeitenPrep 2023Imran A. Isaac100% (6)
- Med Surg QuizDokument91 SeitenMed Surg QuizCharles Gerard B. Beluan0% (1)
- Management of Patients With Oral and Esophageal Disorders PDFDokument85 SeitenManagement of Patients With Oral and Esophageal Disorders PDFNixi Mbuthia100% (1)
- 3rd Yr TURASDokument1 Seite3rd Yr TURASvicenteturasNoch keine Bewertungen
- Release Crash Info PrevDokument1 SeiteRelease Crash Info PrevwwwdotaugieunderscoremercadoNoch keine Bewertungen
- 3rd Yr TURASDokument1 Seite3rd Yr TURASvicenteturasNoch keine Bewertungen
- 3rd Yr TURASDokument1 Seite3rd Yr TURASvicenteturasNoch keine Bewertungen
- 3rd Yr TURASDokument1 Seite3rd Yr TURASvicenteturasNoch keine Bewertungen
- Saint Louis University: School of NursingDokument1 SeiteSaint Louis University: School of NursingvicenteturasNoch keine Bewertungen
- Vii. Nursing Care PlanDokument4 SeitenVii. Nursing Care PlanvicenteturasNoch keine Bewertungen
- PRIOR To ComDokument2 SeitenPRIOR To ComvicenteturasNoch keine Bewertungen
- 3rd Yr TURASDokument1 Seite3rd Yr TURASvicenteturasNoch keine Bewertungen
- Saint Louis University: School of Nursing Family Nursing Assessment ToolDokument2 SeitenSaint Louis University: School of Nursing Family Nursing Assessment ToolvicenteturasNoch keine Bewertungen
- Saint Louis University: School of NursingDokument5 SeitenSaint Louis University: School of NursingvicenteturasNoch keine Bewertungen
- 3d. Family Nursing Assessment Tool Pp3 7 B 1Dokument5 Seiten3d. Family Nursing Assessment Tool Pp3 7 B 1vicenteturasNoch keine Bewertungen
- IzationDokument9 SeitenIzationvicenteturasNoch keine Bewertungen
- Lack of Insulin Decreases Available Glucose For CellDokument1 SeiteLack of Insulin Decreases Available Glucose For CellvicenteturasNoch keine Bewertungen
- Portfolio Reflective WritingDokument8 SeitenPortfolio Reflective WritingvicenteturasNoch keine Bewertungen
- DiabetesDokument4 SeitenDiabetesvicenteturasNoch keine Bewertungen
- DiabetesDokument4 SeitenDiabetesvicenteturasNoch keine Bewertungen
- PricingDokument3 SeitenPricingvicenteturasNoch keine Bewertungen
- Risk Factors of Cough and Cold 1Dokument1 SeiteRisk Factors of Cough and Cold 1vicenteturasNoch keine Bewertungen
- Risk Factors of Cough and Cold 1Dokument1 SeiteRisk Factors of Cough and Cold 1vicenteturasNoch keine Bewertungen
- Risk Factors of Cough and Cold BrochureDokument2 SeitenRisk Factors of Cough and Cold BrochurevicenteturasNoch keine Bewertungen
- 1Dokument2 Seiten1vicenteturasNoch keine Bewertungen
- JVJV NCP Risk For Fluid Volume DeficitDokument2 SeitenJVJV NCP Risk For Fluid Volume DeficitvicenteturasNoch keine Bewertungen
- Worksheet ABCDokument8 SeitenWorksheet ABCvicenteturasNoch keine Bewertungen
- 3d. Family Nursing Assessment Tool Pp1 2 BDokument2 Seiten3d. Family Nursing Assessment Tool Pp1 2 BvicenteturasNoch keine Bewertungen
- 3d. Family Nursing Assessment Tool pp1 2 BDokument2 Seiten3d. Family Nursing Assessment Tool pp1 2 BvicenteturasNoch keine Bewertungen
- CopdDokument5 SeitenCopdvicenteturasNoch keine Bewertungen
- Mso Example Setup File ADokument1 SeiteMso Example Setup File ASueño InalcanzableNoch keine Bewertungen
- Directory (Contacts)Dokument1 SeiteDirectory (Contacts)vicenteturasNoch keine Bewertungen
- Dapus LPDokument5 SeitenDapus LPintan nurhalizaNoch keine Bewertungen
- What Is Reflux EsophagitisDokument2 SeitenWhat Is Reflux EsophagitisDzul Hilmi Mohd JaniNoch keine Bewertungen
- Lecture 1-EsophagusDokument66 SeitenLecture 1-Esophagusmashe1Noch keine Bewertungen
- ACG Clinical Guideline For The Diagnosis And.154Dokument30 SeitenACG Clinical Guideline For The Diagnosis And.154PNoch keine Bewertungen
- Nisi Dominus FrustraDokument11 SeitenNisi Dominus FrustraJonathan GonzalesNoch keine Bewertungen
- Laryngomalaci 2016 Ajoshua Bedwell, MD, GeorgeZalzal, MDNDokument4 SeitenLaryngomalaci 2016 Ajoshua Bedwell, MD, GeorgeZalzal, MDNwawa chenNoch keine Bewertungen
- Q&a 1Dokument19 SeitenQ&a 1api-3818438Noch keine Bewertungen
- Daftar PustakaDokument3 SeitenDaftar PustakaIndah Pratiwii IriandyNoch keine Bewertungen
- IN-VITRO ANALYSIS OF Moringa Oleifera Lam. LEAVES AND: Curcuma Longa Linn. Extract As A ManducableDokument92 SeitenIN-VITRO ANALYSIS OF Moringa Oleifera Lam. LEAVES AND: Curcuma Longa Linn. Extract As A ManducableJerico CenizaNoch keine Bewertungen
- Dysphagia DiseaseDokument212 SeitenDysphagia DiseaseAprita NurkarimaNoch keine Bewertungen
- Why Excess Stomach Acid Mimics HungerDokument13 SeitenWhy Excess Stomach Acid Mimics Hungershane charltonNoch keine Bewertungen
- Group 6 Presentation Heartburn ObstetricDokument21 SeitenGroup 6 Presentation Heartburn ObstetricSyafiqAziziNoch keine Bewertungen
- 欧洲呼吸学会成人及儿童慢性咳嗽诊治指南Dokument31 Seiten欧洲呼吸学会成人及儿童慢性咳嗽诊治指南GaryNoch keine Bewertungen
- Ranitidine NeomedDokument5 SeitenRanitidine NeomedMarsyaNoch keine Bewertungen
- Usmle 01 1415 Manual DGDokument55 SeitenUsmle 01 1415 Manual DGMiguel Marcio Ortuño MejiaNoch keine Bewertungen
- Summary of The 2018 NASPGHAN-ESPGHAN Pediatric Gastroesophageal Reflux Clinical Practice GuidelineDokument4 SeitenSummary of The 2018 NASPGHAN-ESPGHAN Pediatric Gastroesophageal Reflux Clinical Practice GuidelineAyu KendranNoch keine Bewertungen
- LPRDokument29 SeitenLPRrizky8Noch keine Bewertungen
- Diseases of The Digestive SystemDokument5 SeitenDiseases of The Digestive SystemmeiuuNoch keine Bewertungen
- Gastric Versus Jejunal Feeding: Evidence or Emotion?: Nutrition Issues in Gastroenterology, Series #42Dokument11 SeitenGastric Versus Jejunal Feeding: Evidence or Emotion?: Nutrition Issues in Gastroenterology, Series #42Giselle Pezoa WattsonNoch keine Bewertungen
- YOGA AND DIGESTION and ELIMINATION1Dokument25 SeitenYOGA AND DIGESTION and ELIMINATION1Toby SmallNoch keine Bewertungen
- Gejala Dan Penatalaksanaan Penyakit Refluks Gastroesofageal (GERD)Dokument17 SeitenGejala Dan Penatalaksanaan Penyakit Refluks Gastroesofageal (GERD)irmsNoch keine Bewertungen