Beruflich Dokumente
Kultur Dokumente
NIH Public Access: Suicidal Thoughts and Behavior With Antidepressant Treatment
Hochgeladen von
tugba1234Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
NIH Public Access: Suicidal Thoughts and Behavior With Antidepressant Treatment
Hochgeladen von
tugba1234Copyright:
Verfügbare Formate
NIH Public Access
Author Manuscript
Arch Gen Psychiatry. Author manuscript; available in PMC 2012 September 06.
NIH-PA Author Manuscript
Published in final edited form as:
Arch Gen Psychiatry. 2012 June ; 69(6): 580587. doi:10.1001/archgenpsychiatry.2011.2048.
Suicidal Thoughts and Behavior With Antidepressant Treatment:
Reanalysis of the Randomized Placebo-Controlled Studies of Fluoxetine and Venlafaxine
Dr Robert D. Gibbons, PhD, Dr C. Hendricks Brown, PhD, Dr Kwan Hur, PhD, Dr John M.
Davis, MD, and Dr J. John Mann, MD
Departments of Medicine, Health Studies, and Psychiatry (Dr Gibbons) and Center for Health
Statistics (Drs Gibbons, Brown, and Hur), University of Chicago, and Department of Psychiatry,
University of Illinois at Chicago (Dr Davis), Chicago, and Center for Medication Safety, Pharmacy
Benefit Management Services, Hines Veterans Affairs Hospital, Hines (Dr Hur); Prevention
Science and Methodology Group, Center for Family Studies, Department of Epidemiology and
Public Health, University of Miami, Miami, Florida (Dr Brown); and Department of Molecular
Imaging and Neuropathology, New York State Psychiatric Institute and Department of Psychiatry,
Columbia University College of Physicians and Surgeons, New York (Dr Mann)
NIH-PA Author Manuscript
Abstract
ContextThe US Food and Drug Administration issued a black box warning for antidepressants
and suicidal thoughts and behavior in children and young adults.
ObjectiveTo determine the short-term safety of anti-depressants by standard assessments of
suicidal thoughts and behavior in youth, adult, and geriatric populations and the mediating effect
of changes in depressive symptoms.
Data SourcesAll intent-to-treat person-level longitudinal data of major depressive disorder
from 12 adult, 4 geriatric, and 4 youth randomized controlled trials of fluoxetine hydrochloride
and 21 adult trials of venlafaxine hydrochloride.
Study SelectionAll sponsor-conducted randomized controlled trials of fluoxetine and
venlafaxine.
NIH-PA Author Manuscript
Data ExtractionThe suicide items from the Childrens Depression Rating ScaleRevised and
the Hamilton Depression Rating Scale as well as adverse event reports of suicide attempts and
suicide during active treatment were analyzed in 9185 patients (fluoxetine: 2635 adults, 960
geriatric patients, 708 youths; venlafaxine: 2421 adults with immediate-release venlafaxine and
2461 adults with extended-release venlafaxine) for a total of 53 260 person-week observations.
Data SynthesisSuicidal thoughts and behavior decreased over time for adult and geriatric
patients randomized to fluoxetine or venlafaxine compared with placebo, but no differences were
found for youths. In adults, reduction in suicide ideation and attempts occurred through a
2012 American Medical Association. All rights reserved.
Correspondence: Robert D. Gibbons, PhD, Center for Health Statistics and Departments of Medicine, Health Studies, and Psychiatry,
University of Chicago, 5841 S Maryland Ave, MC 2007, Office W260, Chicago, IL 60637 (rdg@uchicago.edu).
Author Contributions: Dr Gibbons had full access to all of the data in the study and takes responsibility for the integrity of the data
and the accuracy of the data analysis.
Additional Contributions: Data were supplied by the National Institute of Mental Health (Treatment for Adolescents With
Depression Study), Wyeth, and Eli Lilly and Co.
Financial Disclosure: Dr Gibbons has served as an expert witness for the US Department of Justice, Wyeth, and Pfizer
Pharmaceuticals in cases related to antidepressants and anticonvulsants and suicide. Dr Brown directed a suicide prevention program
at the University of South Florida that received funding from JDS Pharmaceuticals. Dr Mann has received research support from
GlaxoSmithKline and Novartis.
Gibbons et al.
Page 2
reduction in depressive symptoms. In all age groups, severity of depression improved with
medication and was significantly related to suicide ideation or behavior.
NIH-PA Author Manuscript
ConclusionsFluoxetine and venlafaxine decreased suicidal thoughts and behavior for adult
and geriatric patients. This protective effect is mediated by decreases in depressive symptoms with
treatment. For youths, no significant effects of treatment on suicidal thoughts and behavior were
found, although depression responded to treatment. No evidence of increased suicide risk was
observed in youths receiving active medication. To our knowledge, this is the first research
synthesis of suicidal thoughts and behavior in depressed patients treated with antidepressants that
examined the mediating role of depressive symptoms using complete longitudinal person-level
data from a large set of published and unpublished studies.
NIH-PA Author Manuscript
In 2004, the US Food and Drug Administration (FDA) issued a black box warning for
antidepressants and risk of suicide in children and adolescents. No actual suicides occurred
in these trials with either antidepressant or placebo, so this concern was based primarily on
suicide ideation and attempts.1 In 2006, the FDA extended the warning to young adults aged
18 to 25 years.2 The original warning was based on a meta-analysis of adverse event reports
(AERs) of suicidal thoughts and behavior from 25 clinical randomized controlled trials
(RCTs) conducted by the pharmaceutical companies in pursuit of approval of antidepressant
medications. These trials were typically short term and limited to the newer antidepressant
classes of selective serotonin reuptake inhibitors and serotoninnorepinephrine reuptake
inhibitors. Results of the analysis revealed an overall odds ratio (OR) of 1.78 (95% CI, 1.14
2.77), indicating that the rate of suicidal thoughts and behavior from AERs was significantly
higher in children randomized to active antidepressant treatment relative to placebo. The
extension of the warning to young adults was based on a second meta-analysis of AERs in
372 RCTs in 99 839 adult patients. The FDA found a result that approached significance for
young adults aged 18 to 24 years (OR=1.62; 95% CI, 0.972.71) and, in contrast, a
significantly decreased risk in adults aged 25 to 64 years (OR=0.79; 95% CI, 0.640.98) and
geriatric patients aged 65 years and older (OR=0.37; 95% CI, 0.180.76).
A similar analysis conducted by the FDA on prospectively measured suicidal thoughts and
behavior in the youth studies failed to detect any evidence of increased risk of antidepressant
treatment in these same studies.1 Their analysis focused on study end point and did not make
use of the full longitudinal data that were available in these studies. No analysis of the
prospective rating scale data was presented by the FDA for studies of adults.
NIH-PA Author Manuscript
To help determine what impact antidepressants have on the course of depression and
suicidal thoughts and behavior in different age groups, we obtained complete longitudinal
data for RCTs of fluoxetine hydrochloride conducted by Eli Lilly and Co, the Treatment for
Adolescents With Depression Study of fluoxetine in children by the National Institute of
Mental Health,3 and adult studies for venlafaxine hydrochloride conducted by Wyeth. These
patient-level data allow us to do the following: (1) estimate rates of change in suicidal
thoughts and behavior during the course of treatment; (2) study the relationship between
depression severity and suicidal thoughts and behavior; and (3) determine the extent to
which changes in depressive symptoms mediate the relationship between antidepressant
treatment and suicidal thoughts and behavior. These analyses substantially expand the
original analyses conducted by the FDA in children by including the complete longitudinal
record for each patient and provide similar analyses for adult and geriatric populations,
which were not previously reported by the FDA. This approach seeks to provide the
clinician with a more accurate risk-benefit estimation for using antidepressants for major
depressive disorder at all ages.
Arch Gen Psychiatry. Author manuscript; available in PMC 2012 September 06.
Gibbons et al.
Page 3
METHODS
STUDY DATA
NIH-PA Author Manuscript
A detailed description of the study data is available on request from the authors and will be
available in a related publication.4
Our measures of suicide ideation and behavior were item 3 of the Hamilton Depression
Rating Scale (HAM-D; used in adult and geriatric patients) and item 13 of the Childhood
Depression Rating ScaleRevised (CDRS-R; used in children and adolescents). These
measures were obtained on a weekly basis. The original response categories are provided in
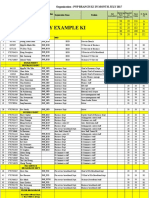
Table 1.
NIH-PA Author Manuscript
Our primary analyses used these as ordinal scales after collapsing the first 2 categories for
the HAM-D and for the CDRS-R. These categories (feels life is not worth living [HAM-D]
or sharp denial of suicidal thoughts [CDRS-R]) do not meet the threshold for suicide
ideation (ie, passive thoughts about wanting to be dead or active thoughts about killing
oneself)5 and have not been found to be predictive of later suicide in psychiatric out-patient
clinic patients6 or nonfatal suicide attempts in RCTs.7 Descriptive analyses of suicide
ideation and behavior were also provided. Suicide ideation and behavior were operationally
defined as a HAM-D item 3 score greater than 2 (a score of 3 indicates suicide ideas or
gestures) or a CDRS-R item 13 score greater than 2 (a score of 3 indicates that the patient
has thoughts about suicide, usually when angry), based on the definitions in the article by
Posner et al.5 For completeness, we augmented these measures with AERs of suicide
attempts and suicide, which were available for the studies by Eli Lilly and Co and the
Treatment for Adolescents With Depression Study. These AERs were coded as 7 for
children and 4 for adults; timing was coded by date at onset. These collapsed ordinal scales
are referred to later as suicide risk measures. For an overall measure of depressive
symptoms, we summed all remaining HAM-D or CDRS-R items, excluding the item related
to suicide to avoid bias in estimating the relationship between depression severity and
suicide risk. This overall measure of depressive symptoms was used to assess the mediating
effect of an antidepressant on suicide risk reduction.
STATISTICAL ANALYSIS
NIH-PA Author Manuscript
We first examined the observed distribution of suicide ideation or behavior as a function of
time, treatment, and age group (Table 2). After 8 weeks the data were sparse and were
therefore combined into a single category (9 weeks). The maximum length of follow-up
was 130 days. The observed proportions were based on numbers of patients at risk in each
condition. Unlike our companion study4 where we restricted analysis to the first 6 weeks of
treatment so that all studies included all time points (ie, study and time are unconfounded),
in this study we used all available data during active treatment so that we did not miss any
adverse events. Second, we examined how antidepressant treatment affected suicide risk
over time, using a 3-level mixed-effects ordinal logistic regression model in SuperMix.8 As
in the companion article,4 we conducted an overall analysis of both drugs in adult and
geriatric patients (ie, all trials using the HAM-D) followed by separate analyses for adult,
geriatric, and youth trials of fluoxetine and adult trials of immediate-release and extendedrelease venlafaxine. These analyses accounted for exact days of assessment and controlled
for individual-level covariates of age and sex. Random effects were included at both the
patient and trial levels to account for the correlation of repeated measurements within
patients and the correlation of patients within studies. Incomplete data were treated as
missing at random in these analyses.9 To test the hypothesis that suicide risk is mediated by
changes in depression severity, a second mixed-effects ordinal logistic regression model was
used in which depression severity (HAM-D or CDRS-R total scores eliminating the suicide
Arch Gen Psychiatry. Author manuscript; available in PMC 2012 September 06.
Gibbons et al.
Page 4
NIH-PA Author Manuscript
item) and the treatmentdepression severity interactions were added to the model as timevarying covariates predicting suicide risk status. The interaction term allows the relationship
between depression severity and suicide risk to be different for treated and control
patients.10 We then conducted a mediational analysis to determine the extent to which
reduction in the time-dependent depressive symptom score accounted for the effect of
treatment on concurrent suicide risk. In addition, we fit a 3-level mixed-effects linear
regression model to evaluate the effect of treatment on depression severity (HAM-D or
CDRS-R scores independent of the suicide items) using all available data. The following are
key requirements for a variable to be a mediator: (1) the putative mediator is affected by
treatment; (2) the mediator is related to the outcome, either as a main effect or in interaction
with treatment10; and (3) the mediator contribution reduces the effect of the treatment on
suicide risk status. In the companion article,4 we have demonstrated that treatment is
significantly related to the mediator (change in depression severity) for both drugs and all 3
age groups through 6 weeks; for these mediational analyses, we report effects on depression
severity through 12 weeks. In this article, we test the hypothesis that the mediator
(depression severity) is related to the outcome (suicide risk) and accounts for a significant
proportion of the observed reduction in suicide ideation or behavior. The difference in rates
of change (ie, slopes) in suicide risk between treated and control patients is measured by the
treatmenttime interaction. Comparison of models with and without the mediator effects
allows us to determine the extent to which the effect of treatment on suicide risk is mediated
by the effect of treatment on depression severity. Because these models are on a logit scale,
a calibration of variances for these coefficients is necessary to compare them directly.11 The
proportion of the mediation was then computed as 1 minus the ratio of the treatmenttime
interactions for the model with the mediator to the model without the mediator.11
NIH-PA Author Manuscript
Results are reported as marginal maximum likelihood estimates (MMLEs), standard errors,
and probability values (P values) of the treatmenttime interaction, main effect of
depression severity, and treatmentseverity interaction. Estimates of marginal (populationaveraged) ORs9 were then used to describe the percentage reduction in the probability of
suicide risk following 8 weeks for treated vs control patients. We evaluated models with
nonlinear time trends; however, the linear models provided the best overall fit.
NIH-PA Author Manuscript
There were relatively few suicide attempts and suicides (a total of 20 attempts and 2 suicides
in 21 patients among 9185 patients across all age cohorts and drugs), allowing limited power
to detect potential differences. Overall, a total of 16 suicide attempts were identified through
the standardized CDRS-R or HAM-D measures. An additional 6 suicidal events were
identified from AERs, 4 attempts and 2 suicides. These additional 6 AERs were coded using
the Columbia Classification Algorithm of Suicide Assessment.5 Of the 2 suicides, one was
by an adult receiving fluoxetine and the other was a geriatric patient receiving placebo. Of
the 22 suicidal events, 9 were recorded at baseline (prior to initiation of treatment), 3 in
week 1, 3 in week 2, 5 in week 3, 1 in week 4, and 1 in week 5.
RESULTS
The reported rates of suicide risk at baseline were 5% for adults, 3% for geriatric patients,
and 20% for youths. In general, rates of suicide risk were reduced by 50% or more for both
treated and control groups over time. Table 2 illustrates how suicide risk varies from
baseline, where randomization produced virtually identical rates. For all ages and both
drugs, rates of suicide risk among patients were not markedly different from those of control
patients but were generally lower in treated patients than in control patients over time
(starting from the second week). We note, however, that the simple observed proportions in
Table 2 may be biased because they are restricted to patients with data at each week, and
these patients may not be representative of all randomized patients, especially at later times.
Arch Gen Psychiatry. Author manuscript; available in PMC 2012 September 06.
Gibbons et al.
Page 5
NIH-PA Author Manuscript
The mixed-effects model results described later (summarized in Table 3) make use of all
available data for each subject in constructing the average time trends and therefore are
unbiased in this respect.
OVERALL ANALYSIS OF ADULT AND GERIATRIC PATIENTS
We found a statistically significant difference in the reduction in suicide risk over time
between treated patients and those receiving placebo (MMLE=0.2091; SE=0.0289; P<.
001) (Figure 1). Thus, treated patients had a greater reduction in suicide risk over time
relative to control patients receiving placebo. The rate of change was 58% faster in treated
patients relative to control patients, which results in an estimated 78.9% decrease in the
probability of suicidal risk for control patients after 8 weeks of study participation and a
90.5% decrease for treated patients. Figure 1 displays the estimated probabilities for each of
the 3 ordinal response categories in treated and control patients and reveals that most
suicidal events (19% at baseline) were of low severity (thoughts of death), followed by
ideation with a baseline rate of 3% and suicide attempts or completion at 0.1% at baseline.
The beneficial effect of treatment on the probability of suicide risk is apparent
approximately 2 weeks following treatment initiation.
NIH-PA Author Manuscript
The mediation model of all adult and geriatric patients revealed the following. First, there
was a significant overall faster reduction in depressive symptoms (excluding suicidal
thoughts and behavior) over time for treated patients vs control patients (treatment
difference at 12 weeks: MMLE=4.0337; SE=0.2730; P<.001), as we found in the
companion study.4 This estimate indicates an average estimated difference in depression
severity of 4.03 HAM-D units between treated and control patients at 12 weeks. Second, we
found a statistically significant main effect of depression severity on contemporaneous
suicide risk (MMLE=0.3070; SE=0.0094; P<.001), indicating that depression severity is
positively associated with suicide risk. The treatmentdepression severity interaction was
not statistically significant, indicating that the relationship between depression severity and
suicide risk was similar for treated and control patients (MMLE=0.0159; SE=0.0127; P=.
21). Following adjustment for depression severity (Figure 2), the treatmenttime interaction
was still statistically significant (MMLE=0.0620; SE=0.0314; P=.048); however, it was
dramatically reduced from the model that did not adjust for depression severity. The
percentage of the overall treatment effect attributable to mediation was 77%. This finding
reveals that most of the beneficial effect of antidepressant treatment on suicide risk is
mediated through the effect of antidepressant treatment on depression severity.
NIH-PA Author Manuscript
To interpret these findings in terms of population-averaged effects, we transformed these
individual-level effect parameters for models into population rates of suicide ideation or
attempts over time, adjusted for the mediator. Figure 2 illustrates this mediational effect by
plotting the marginal probability of suicide risk for each threshold in treated and control
patients, adjusting for depression severity. In terms of depression severity, we have selected
a hypothetical patient who begins the trial severely depressed (HAM-D total score=30) and
improves at a rapid rate of 0.35 HAM-D units per day through 12 weeks. In contrast to the
clear intervention differences in Figure 1, Figure 2 reveals that there is essentially no
difference in suicide risk attributable to treatment once the effect of depression severity is
controlled, illustrating the previous mediational analysis result.
ADULT FLUOXETINE STUDIES
A statistically significant treatmenttime interaction was found in adult fluoxetine studies
(MMLE=0.1689; SE=0.0644; P=.009), indicating that treated patients had a significantly
greater reduction in suicide risk over time relative to control patients receiving placebo. The
rate of change was 57% faster in treated patients relative to control patients, resulting in an
Arch Gen Psychiatry. Author manuscript; available in PMC 2012 September 06.
Gibbons et al.
Page 6
NIH-PA Author Manuscript
83.0% decrease in the probability of suicide risk for control patients after 8 weeks of study
participation and a 91.6% decrease for treated patients. Fluoxetine produced a faster decline
in depressive symptoms over time compared with placebo (treatment difference at 12 weeks:
MMLE = 4.2882; SE=0.5645; P<.001). The mediation model revealed a statistically
significant main effect of depression severity (MMLE=0.3091; SE=0.0206; P<.001),
indicating that depression severity is positively associated with suicide risk. The
treatmentdepression severity interaction was not statistically significant, indicating that the
relationship between depression severity and suicide risk was the same for treated and
control patients (MMLE=0.0342; SE=0.0283; P=.23). Following adjustment for depression
severity, the difference in rates of change in suicide risk between treated and control patients
was not statistically significant (MMLE=0.0192; SE=0.0674; P=.78). The percentage of the
overall treatment effect attributable to mediation was 82%. This finding reveals that the
beneficial effect of fluoxetine treatment on suicide risk in adults is mediated through the
effect of antidepressant treatment on depression severity.
ADULT IMMEDIATE-RELEASE VENLAFAXINE STUDIES
NIH-PA Author Manuscript
A statistically significant treatmenttime interaction was found in adult immediate-release
venlafaxine studies (MMLE=0.3777; SE=0.0650; P<.001), indicating that treated patients
had a significantly greater reduction in suicide risk over time relative to control patients
receiving placebo. The rate of change was 82% faster in treated patients relative to control
patients, resulting in an 81.0% decrease in the probability of suicidal thoughts or behavior
for control patients after 8 weeks of study participation and a 93.5% decrease for treated
patients. Immediate-release venlafaxine produced a faster decline in depressive symptoms
over time than did placebo (treatment difference at 12 weeks: MMLE=5.0358; SE=0.5032;
P<.001). The mediation model revealed a statistically significant main effect of depression
severity (MMLE=0.3219; SE=0.0168; P<.001), indicating that depression severity is
positively associated with suicide risk. The treatmentdepression severity interaction was
not statistically significant, indicating that the relationship between depression severity and
suicide risk was the same for treated and control patients (MMLE=0.0056; SE=0.0221; P=.
80). Following adjustment for depression severity, the treatmenttime interaction remained
statistically significant (MMLE=0.1672; SE=0.0631; P=.008); however, the magnitude was
substantially reduced. The percentage of the overall treatment effect attributable to
mediation was 81%. This finding reveals that most of the beneficial effect of immediaterelease venlafaxine treatment on suicide risk in adults is mediated through the effect of
antidepressant treatment on depression severity.
ADULT EXTENDED-RELEASE VENLAFAXINE STUDIES
NIH-PA Author Manuscript
A statistically significant treatmenttime interaction was found in adult extended-release
venlafaxine studies (MMLE=0.1501; SE=0.0565; P=.008), indicating that treated patients
had a significantly greater reduction in suicide risk over time relative to control patients
receiving placebo. The rate of change was 37% faster in treated patients relative to control
patients, resulting in a 77.1% decrease in the probability of suicide risk for control patients
after 8 weeks of study participation and an 88.7% decrease for treated patients. Patients
receiving extended-release venlafaxine experienced a faster decline in depressive symptoms
(treatment difference at 12 weeks: MMLE=3.5658; SE=0.4402; P<.001) relative to control
patients. The mediation model revealed a statistically significant main effect of depression
severity (MMLE=0.2923; SE=0.0156; P<.001), indicating that depression severity is
positively associated with suicide risk. The treatmentdepression severity interaction was
not statistically significant, indicating that the relationship between depression severity and
suicide risk was the same for treated and control patients (MMLE=0.0106; SE=0.0211; P=.
62). Following adjustment for depression severity, the treatmenttime interaction was no
longer statistically significant (MMLE=0.0088; SE=0.0515; P=.86). The percentage of the
Arch Gen Psychiatry. Author manuscript; available in PMC 2012 September 06.
Gibbons et al.
Page 7
NIH-PA Author Manuscript
overall treatment effect attributable to mediation was 83%. This finding reveals that the
beneficial effect of extended-release venlafaxine treatment on suicide risk in adults is
mediated through the effect of antidepressant treatment on depression severity.
GERIATRIC FLUOXETINE STUDIES
NIH-PA Author Manuscript
A statistically significant treatmenttime interaction was found in geriatric fluoxetine
studies (MMLE=0.1479; SE=0.0688; P=.03), indicating that treated patients had a
significantly greater reduction in suicide risk over time relative to control patients receiving
placebo. The rate of change was 66% faster in treated patients relative to control patients,
resulting in a 69.0% decrease in the probability of suicide risk for control patients after 8
weeks of study participation and an 84.0% decrease for treated patients. Geriatric patients
receiving fluoxetine decreased their depressive symptoms more quickly than did patients
receiving placebo (treatment difference at 12 weeks: MMLE=2.7224; SE=0.8308; P=.001).
The mediation model revealed a statistically significant main effect of depression severity
(MMLE=0.2963; SE=0.0289; P<.001), indicating that depression severity is positively
associated with suicide risk. The treatmentdepression severity interaction was not
statistically significant, indicating that the relationship between depression severity and
suicide risk was the same for treated and control patients (MMLE=0.0417; SE=0.0417; P=.
32). Following adjustment for depression severity, the treatmenttime interaction was no
longer statistically significant (MMLE=0.1501; SE=0.0788; P=.06). The percentage of the
overall treatment effect attributable to mediation was 57%. This finding reveals that slightly
more than half of the beneficial effect of fluoxetine treatment relative to placebo on suicide
risk in geriatric patients is mediated through the effect of antidepressant treatment on
depression severity (ie, partial mediation).
YOUTH FLUOXETINE STUDIES
NIH-PA Author Manuscript
The treatmenttime interaction was not statistically significant in youth fluoxetine studies
(MMLE=0.0809; SE=0.0595; P=.17), indicating that we could find no difference between
treated and control patients in terms of suicide risk. The marginal ORs indicated a 61.3%
decrease in the probability of suicidal thoughts or behavior for control patients after 8 weeks
of study participation and a 50.3% decrease for treated patients. Youth patients receiving
fluoxetine decreased their depressive symptoms more quickly than patients receiving
placebo (treatment difference at 12 weeks: MMLE=3.8976; SE=1.5238; P=.01). A
statistically significant main effect of depression severity (MMLE=0.1261; SE=0.0116; P<.
001) on suicide risk was found, indicating that depression severity is positively associated
with suicide risk. The treatmentdepression severity interaction was not statistically
significant, indicating that the relationship between depression severity and suicide risk was
the same for treated and control patients (MMLE = 0.0046; SE=0.0141; P=.74). Despite a
strong association between depression severity and suicide risk in youths, treatment with
fluoxetine was not found to be related to suicide risk when compared with placebo.
COMMENT
Results of the first analysis of all longitudinal suicidal event data across published and
unpublished placebo-controlled RCTs of fluoxetine (adult, youth, and geriatric patients) and
venlafaxine (adults) revealed that there was no evidence of increased suicide risk with
treatment. Except for youths, the level of suicide risk for most subjects in these trials was
low, and for all groups there was a major reduction in risk over time. Most events were
suicidal ideation. We found that for adults treated with fluoxetine, extended-release
venlafaxine, or immediate-release venlafaxine and geriatric patients treated with fluoxetine,
treatment resulted in significant decreases relative to placebo in suicide risk measures over
time. No statistically significant differences were found for fluoxetine in youths. Suicide risk
Arch Gen Psychiatry. Author manuscript; available in PMC 2012 September 06.
Gibbons et al.
Page 8
NIH-PA Author Manuscript
was strongly related to severity of depression, and changes over time in suicide risk closely
mirrored those of depression severity changes over this same period in both youths and
adults. Other studies have reported that the rate of suicidal behavior in major depressive
disorder is much higher during episodes than between episodes.12 For all adult trials,
depression severity mediated the effect of antidepressant medication on suicide risk.
Mediation accounted for approximately 80% of the overall treatment effect in adults, but
less (57%) for geriatric patients. For youths, depression severity was strongly related to
suicide risk and depression responded to treatment, but no effect of treatment on suicide risk
was found.
NIH-PA Author Manuscript
These results clarify the relationship between suicidal thoughts and behavior and
antidepressant treatment, particularly in adult and geriatric patients, because they suggest
that adult and geriatric patients whose symptoms do not diminish remain at higher suicide
risk. Variation in response to antidepressant treatment is substantial; in one trial, it was
estimated that more than half of adults were nonresponsive to placebo and 30% were
nonresponsive to a selective serotonin reuptake inhibitor.13 The STAR*D results indicate
that a sizable proportion of those who are nonresponsive to a first antidepressant can
improve under an alternative medication.14 Our findings emphasize the need to successfully
treat episodes of major depressive disorder to lower the suicide risk. Our results for adult
and geriatric patients, which show statistically significant beneficial effects of antidepressant
treatment on suicide risk, largely agree with the FDA findings and further demonstrate the
mediating role of depressive symptom change. With respect to youths, we did not replicate
the FDAs finding of increased risk with antidepressant treatment. However, the FDA found
that fluoxetine was the only antidepressant that was effective for depression. Our results
apply to fluoxetine and it remains to be determined whether the findings generalize to other
antidepressants. Newer, improved prospective measures of suicidal ideation and behavior
now exist,5 are now mandated by the FDA, and should be analyzed as done here.
This study avoided the problem of publications being biased in favor of positive clinical
trials by examining all industry trials of fluoxetine and venlafaxine but nevertheless did not
have enough statistical power to analyze suicidal ideation and actual suicidal behavior
separately. Suicidal ideation rates and the ratios to suicides and suicide attempts are higher
in youths compared with adults, making ideation a potentially weaker indicator of risk of
behavior in youths.15
NIH-PA Author Manuscript
The mediation analyses show the importance of antidepressant response in mediating the
benefit of antidepressants for suicide risk in adult and geriatric patients. It is important to
note that these analyses could be done only by combining individual patient-level data in the
same analysis. The methods we have used here, nonlinear mixed-effects regression models
and mediation analysis, are applied to answer complex hypotheses with individual-level data
that are synthesized across multiple trials. These methods of person-level meta-analysis or
integrative data analysis16 are superior to standard meta-analysis,17 which cannot adjust
adequately for different time frames, different ways of handling missing data, and different
analytical choices for mediation analysis. A second critically important aspect of these
studies is that they all have random assignment and blinded assessment. In all trials, these
procedures balanced suicidal thought and behavior incidence at baseline between treated and
control patients and assured equivalent assessment procedures. Randomization brings about
balance in both observable and unobservable potential confounders, whereas no such
guarantee is available for observational data.
A limitation of these studies is that they rely on a single ordinal clinician rating of suicidal
thoughts and behavior, supplemented by AERs of suicide attempts or suicides. For youths,
the FDA analyses that relied on suicide-related AERs in the clinical records alone found
Arch Gen Psychiatry. Author manuscript; available in PMC 2012 September 06.
Gibbons et al.
Page 9
NIH-PA Author Manuscript
statistically significant increased risk of suicidal thoughts and behavior for those treated with
antidepressants compared with placebo, whereas we did not find this effect in our analysis of
the systematically collected CDRS-R suicide item that was augmented with the AERs of
suicidal behavior. There is debate in the literature on how best to examine mediation in
nonlinear longitudinal models. In particular, the proportion of reduction in effect due to
mediation, which we used in this article, is known to be unstable when the treatment effect
is small.11 For adults, the large treatment effects and depressive symptom effects on suicide
risk mitigate this concern, but the percentage reduction for geriatric patients has more
uncertainty.
NIH-PA Author Manuscript
Unanswered questions remain. While the findings of mediation are clear for adults in 3 sets
of trials and geriatric patients in 1 set of trials, we did not find a statistically significant
effect of treatment on suicide in youths, despite a large overall reduction in depressive
symptoms. We do not yet know why some youths whose depressive symptoms are reduced
continue to have suicidal ideation and behavior. Perhaps other psychopathology plays a
more important role in suicidal behavior and ideation such as aggressive impulsive traits in
youths.18 Thus, even if antidepressants reduce depressive symptoms overall in youths, it is
possible that a subset may retain some level of risk for suicidal ideation or attempts. The
overall rate, however, was not significantly greater than that found for youths randomized to
placebo. It was the finding of an increased rate of ideation and attempts using AERs that
formed the entire basis for the FDA black box warning, and notably, we do not find such a
signal using data that draw on both AERs and prospective systematic ratings of suicidal
ideation and behavior.
A limitation of RCTs for studying suicide risk is that suicidal patients are often excluded
from such studies. While this may be true, we note that the rate of suicidal thoughts and
behavior were highest at baseline, and 9 of the 20 suicide attempts occurred prior to
treatment initiation (ie, were rated as being present at baseline).
In summary, we found that treatment with fluoxetine and venlafaxine decreased suicide risk
in adult and geriatric patients and that the effect of treatment on depression severity appears
to be the mechanism whereby antidepressants lower suicide risk in adult and geriatric
patients. We found no evidence that fluoxetine increased risk of suicidal thoughts or
behavior in youths.
Acknowledgments
NIH-PA Author Manuscript
Funding/Support: This work was supported by grants MH062185 (Dr Mann), R56 MH078580 (Drs Gibbons and
Brown), MH8012201 (Drs Gibbons and Brown), and MH040859 (Dr Brown) from the National Institute of Mental
Health and grant 1U18HS016973 from the Agency for Healthcare Research and Quality (Dr Gibbons).
References
1. Hammad, TA. [Accessed December 15, 2010] Review and evaluation of clinical data.
http://www.fda.gov/ohrms/dockets/ac/04/briefing/2004-4065b1-10-TAB08-Hammads-Review.pdf
2. US Food and Drug Administration. [Accessed December 15, 2010] Clinical review: relationship
between antidepressant drugs and suicidality in adults.
http://www.fda.gov/ohrms/dockets/ac/06/briefing/2006-4272b1-01-FDA.pdf
3. March J, Silva S, Petrycki S, Curry J, Wells K, Fairbank J, Burns B, Domino M, McNulty S,
Vitiello B, Severe J. Treatment for Adolescents With Depression Study (TADS) Team. Fluoxetine,
cognitive-behavioral therapy, and their combination for adolescents with depression: Treatment for
Adolescents With Depression Study (TADS) randomized controlled trial. JAMA. 2004; 292(7):
807820. [PubMed: 15315995]
Arch Gen Psychiatry. Author manuscript; available in PMC 2012 September 06.
Gibbons et al.
Page 10
NIH-PA Author Manuscript
NIH-PA Author Manuscript
NIH-PA Author Manuscript
4. Gibbons RD, Hur K, Brown CH, Davis JM, Mann JJ. Who benefits from antidepressants? synthesis
of 6-week patient-level outcomes from double-blind placebo controlled randomized trials of
fluoxetine and venlafaxine. Arch Gen Psychiatry. In press.
5. Posner K, Oquendo MA, Gould M, Stanley B, Davies M. Columbia Classification Algorithm of
Suicide Assessment (C-CASA): classification of suicidal events in the FDAs pediatric suicidal risk
analysis of antidepressants. Am J Psychiatry. 2007; 164(7):10351043. [PubMed: 17606655]
6. Brown GK, Steer RA, Henriques GR, Beck AT. The internal struggle between the wish to die and
the wish to live: a risk factor for suicide. Am J Psychiatry. 2005; 162(10):19771979. [PubMed:
16199851]
7. Posner K, Brown GK, Stanley B, Brent DA, Yershova KV, Oquendo MA, Currier GW, Melvin GA,
Greenhill L, Shen S, Mann JJ. The ColumbiaSuicide Severity Rating Scale: initial validity and
internal consistency findings from three multisite studies with adolescents and adults. Am J
Psychiatry. 2011; 168:12661277.10.1176/appi.ajp.2011.10111704 [PubMed: 22193671]
8. Hedeker, D.; Gibbons, RD.; Du Toit, SHC.; Patterson, D. SuperMix: A Program for Mixed-Effects
Regression Models. Chicago, IL: Scientific Software International; 2008.
9. Siddique J, Brown CH, Hedeker D, Duan N, Gibbons RD, Miranda J, Lavori PW. Missing data in
longitudinal trials, part B: analytic issues. Psychiatr Ann. 2008; 38(12):793801. [PubMed:
19668352]
10. Kraemer HC, Gibbons RD. Why does the randomized clinical trial methodology so often mislead
clinical decision making? focus on moderators and mediators of treatment. Psychiatr Ann. 2009;
39(7):736745.10.3928/00485713-20090625-06
11. MacKinnon DP, Lockwood CM, Brown CH, Wang W, Hoffman JM. The intermediate endpoint
effect in logistic and probit regression. Clin Trials. 2007; 4(5):499513. [PubMed: 17942466]
12. Oquendo MA, Galfalvy H, Russo S, Ellis SP, Grunebaum MF, Burke A, Mann JJ. Prospective
study of clinical predictors of suicidal acts after a major depressive episode in patients with major
depressive disorder or bipolar disorder. Am J Psychiatry. 2004; 161(8):14331441. [PubMed:
15285970]
13. Muthn B, Brown HC. Estimating drug effects in the presence of placebo response: causal
inference using growth mixture modeling. Stat Med. 2009; 28(27):33633385. [PubMed:
19731223]
14. Rush AJ. STAR*D: what have we learned? Am J Psychiatry. 2007; 164(2):201204. [PubMed:
17267779]
15. Mann JJ, Emslie G, Baldessarini RJ, Beardslee W, Fawcett JA, Goodwin FK, Leon AC, Meltzer
HY, Ryan ND, Shaffer D, Wagner KD. ACNP Task Force report on SSRIs and suicidal behavior
in youth. Neuropsychopharmacology. 2006; 31 (3):473492. [PubMed: 16319919]
16. Curran PJ, Hussong AM. Integrative data analysis: the simultaneous analysis of multiple data sets.
Psychol Methods. 2009; 14(2):81100. [PubMed: 19485623]
17. Brown CH, Sloboda Z, Faggiano F, Teasdale B, Keller F, Burkhart G, Vigna-Taglianti F, Howe G,
Masyn K, Wang W, Muthn B, Stephens P, Grey S, Perrino T. Prevention Science and
Methodology Group. Methods for synthesizing findings on moderation effects across multiple
randomized trials [published online March 1, 2011]. Prev Sci. 10.1007/s11121-011-0207-8
18. Brent DA, Oquendo M, Birmaher B, Greenhill L, Kolko D, Stanley B, Zelazny J, Brodsky B,
Bridge J, Ellis S, Salazar JO, Mann JJ. Familial pathways to early-onset suicide attempt: risk for
suicidal behavior in offspring of mood-disordered suicide attempters. Arch Gen Psychiatry. 2002;
59(9):801807. [PubMed: 12215079]
Arch Gen Psychiatry. Author manuscript; available in PMC 2012 September 06.
Gibbons et al.
Page 11
NIH-PA Author Manuscript
NIH-PA Author Manuscript
Figure 1.
Probabilities of suicide risk in adult and geriatric fluoxetine hydrochloride and venlafaxine
hydrochloride studies. Solid lines indicate estimated probabilities for control patients
receiving placebo; dashed lines, estimated probabilities for treated patients; thoughts of
death curves, wishes he or she were dead or any thoughts of possible death to self or
worse; ideation curves, suicide ideas or gestures or worse; and attempts or completion
curves, suicide attempts or suicides.
NIH-PA Author Manuscript
Arch Gen Psychiatry. Author manuscript; available in PMC 2012 September 06.
Gibbons et al.
Page 12
NIH-PA Author Manuscript
NIH-PA Author Manuscript
Figure 2.
Probabilities of suicide risk adjusting for depression severity in adult and geriatric fluoxetine
hydrochloride and venlafaxine hydrochloride studies. Solid lines indicate estimated
probabilities for control patients; dashed lines, estimated probabilities for treated patients;
thoughts of death curves, wishes he or she were dead or any thoughts of possible death to
self or worse; ideation curves, suicide ideas or gestures or worse; and attempts or
completion curves, suicide attempts or suicides.
NIH-PA Author Manuscript
Arch Gen Psychiatry. Author manuscript; available in PMC 2012 September 06.
Gibbons et al.
Page 13
Table 1
Suicide Risk Response Categories
NIH-PA Author Manuscript
Score
Description
HAM-D item 3
0
Absent
Feels life is not worth living
Wishes he or she were dead or any thoughts of possible death to self
Suicide ideas or gestures
Attempts at suicide, any serious attempt
CDRS-R item 13
NIH-PA Author Manuscript
Understands the word suicide but does not apply term to self
Sharp denial of suicidal thoughts
Has thoughts about suicide, usually when angry
Between 3 and 5
Has recurrent thoughts of suicide
Between 5 and 7
Has made suicide attempt within the last month or is actively suicidal
Abbreviations: HAM-D, Hamilton Depression Rating Scale; CDRS-R, Childhood Depression Rating ScaleRevised.
NIH-PA Author Manuscript
Arch Gen Psychiatry. Author manuscript; available in PMC 2012 September 06.
NIH-PA Author Manuscript
96 (14.6)
68 (8.8)
114 (13.2)
189 (14.8)
148 (8.8)
105 (14.3)
90 (15.6)
167 (8.4)
78 (9.0)
50 (4.0)
81 (13.6)
396 (0)
297 (0.7)
335 (1.5)
529 (1.7)
609 (1.3)
683 (2.2)
731 (2.2)
904 (4.5)
883 (3.6)
1008 (5.4)
Placebo
288 (0)
259 (1.2)
491 (0.4)
910 (1.2)
1006 (0.7)
1151 (1.1)
1261 (1.7)
1382 (2.1)
1364 (2.4)
1627 (4.7)
Treatment
Abbreviations: ER, extended release; IR, immediate release.
105 (4.8)
183 (10.9)
96 (11.5)
139 (5.8)
205 (8.8)
253 (9.5)
139 (14.4)
393 (18.8)
315 (20.6)
Treatment
Placebo
Adult
108 (3.7)
53 (1.9)
160 (1.3)
309 (1.6)
313 (1.6)
364 (1.9)
360 (2.2)
393 (1.8)
354 (2.5)
470 (3.2)
Placebo
Fluoxetine Hydrochloride, No. (%)
Week
Youth
118 (0)
66 (1.5)
144 (2.8)
310 (0.6)
339 (2.1)
360 (1.4)
370 (0.5)
409 (1.7)
368 (1.6)
490 (2.7)
Treatment
Geriatric
NIH-PA Author Manuscript
Observed Suicidal Thoughts and Behavior Over Time
57 (1.8)
117 (0)
196 (1.0)
397 (1.3)
196 (1.5)
641 (1.7)
662 (1.7)
719 (2.8)
716 (4.9)
919 (6.3)
Placebo
116 (0)
177 (0.6)
357 (1.1)
619 (1.0)
321 (0.9)
965 (0.4)
1034 (1.2)
1096 (1.3)
1061 (2.5)
1502 (5.5)
Treatment
IR
300 (0.7)
448 (0.2)
169 (1.2)
614 (0.7)
199 (0.5)
807 (0.7)
819 (1.1)
903 (1.0)
871 (1.0)
994 (1.6)
Placebo
690 (0.6)
725 (0.6)
276 (0.7)
900 (0.6)
278 (1.8)
1182 (0.3)
1145 (0.5)
1264 (0.6)
1276 (0.9)
1467 (1.7)
Treatment
ER
Venlafaxine Hydrochloride, No. (%)
NIH-PA Author Manuscript
Table 2
Gibbons et al.
Page 14
Arch Gen Psychiatry. Author manuscript; available in PMC 2012 September 06.
NIH-PA Author Manuscript
NIH-PA Author Manuscript
<.001
4.0337
0.2730
<.001
0.3070
0.0094
<.001
P value
MMLE
SE
P value
MMLE
SE
P value
0.0127
SE
.03
0.0688
0.1479
<.001
0.0650
0.3777
<.001
0.5645
4.2882
.001
0.8308
2.7224
<.001
0.5032
5.0358
<.001
0.0116
0.1261
<.001
0.0206
0.3091
<.001
0.0289
0.2963
<.001
0.0168
0.3219
Depressive Symptoms on Suicide Risk
.01
1.5238
3.8976
Treatment on Depressive Symptoms at 12 wk
.009
0.0644
0.1689
IR
.74
0.0141
0.0046
.23
0.0283
0.0342
.32
0.0417
0.0417
.80
0.0221
0.0056
Arch Gen Psychiatry. Author manuscript; available in PMC 2012 September 06.
0.0314
.048
SE
P value
.05
0.0662
0.1293
.78
0.0674
0.0192
.06
0.0788
0.1501
.008
0.0631
0.1672
.86
0.0515
0.0088
Abbreviations: ER, extended release; IR, immediate release; MMLE, marginal maximum likelihood estimate.
0.0620
MMLE
.62
0.0211
0.0106
<.001
0.0156
0.2923
<.001
0.4402
3.5658
.008
0.0565
0.1501
ER
Venlafaxine Hydrochloride
Treatment on Suicide Risk Adjusted for Depressive Symptoms
.21
0.0159
MMLE
P value
0.0595
0.0809
.17
Geriatric
Treatment on Suicide Risk
Adult
Fluoxetine Hydrochloride
Youth
TreatmentDepressive Symptoms Interaction on Suicide Risk
0.0289
0.2091
MMLE
SE
Overall
Statistic
Marginal Maximum Likelihood Estimates, Standard Errors, and P Values for Each Cohort and Effect
NIH-PA Author Manuscript
Table 3
Gibbons et al.
Page 15
Das könnte Ihnen auch gefallen
- Gibbons 2012Dokument8 SeitenGibbons 2012Doc HadiNoch keine Bewertungen
- Antidepressants Versus Interpersonal Psychotherapy in Treating Depression in HIV-positive PatientsDokument6 SeitenAntidepressants Versus Interpersonal Psychotherapy in Treating Depression in HIV-positive PatientsMittaningtyasNoch keine Bewertungen
- Psy Mock Exam NoteDokument8 SeitenPsy Mock Exam NoteIssac LiNoch keine Bewertungen
- Animal Models of Suicide-Trait-Related BehaviorsDokument9 SeitenAnimal Models of Suicide-Trait-Related BehaviorsDoina AlbescuNoch keine Bewertungen
- Treatment of Anxiety Disorders by Psychiatrists From The American Psychiatric Practice Research NetworkDokument6 SeitenTreatment of Anxiety Disorders by Psychiatrists From The American Psychiatric Practice Research NetworkStephNoch keine Bewertungen
- Jurnal JiwaDokument4 SeitenJurnal JiwaNaomiFettyNoch keine Bewertungen
- Garlow 2013Dokument5 SeitenGarlow 2013Doc HadiNoch keine Bewertungen
- MetaanalisisDokument8 SeitenMetaanalisisreant79Noch keine Bewertungen
- JCPDokument11 SeitenJCPChangNoch keine Bewertungen
- Jurnal SkizoafektifDokument7 SeitenJurnal SkizoafektifkhairinanurulNoch keine Bewertungen
- Prevalence, Persistence, and Sociodemographic Correlates of DSM-IV Disorders in The National Comorbidity Survey Replication Adolescent SupplementDokument18 SeitenPrevalence, Persistence, and Sociodemographic Correlates of DSM-IV Disorders in The National Comorbidity Survey Replication Adolescent SupplementGaluh SabikhaNoch keine Bewertungen
- Efficacy of Antidepressants and Benzodiazepines in Minor Depression Systematic Review and MetaanalysisDokument6 SeitenEfficacy of Antidepressants and Benzodiazepines in Minor Depression Systematic Review and MetaanalysisChica MirandaNoch keine Bewertungen
- St. John's Wort Equals Paroxetine in New Study: Visits, Calls May Help Elderly DepressionDokument1 SeiteSt. John's Wort Equals Paroxetine in New Study: Visits, Calls May Help Elderly DepressionkurumeuNoch keine Bewertungen
- NIH Public Access: Author ManuscriptDokument10 SeitenNIH Public Access: Author ManuscriptIrma Sari MuliadiNoch keine Bewertungen
- Atypical Antipsychotics Assessed at ACNPDokument15 SeitenAtypical Antipsychotics Assessed at ACNPargatuNoch keine Bewertungen
- HHS Public Access: Antidepressant Use and Cognitive Decline: The Health and Retirement StudyDokument16 SeitenHHS Public Access: Antidepressant Use and Cognitive Decline: The Health and Retirement StudyRavennaNoch keine Bewertungen
- Literature Review of Risk Factors and Interventions On Postpartum DepressionDokument7 SeitenLiterature Review of Risk Factors and Interventions On Postpartum DepressionafmzhpeloejtzjNoch keine Bewertungen
- Psilocybin May Help Treat Depression, A Small Study FindsDokument3 SeitenPsilocybin May Help Treat Depression, A Small Study FindsAnnisaNoch keine Bewertungen
- A Randomized, Placebo-Controlled Trial of Citalopram For The Treatment of Major Depression in Children and AdolescentsDokument5 SeitenA Randomized, Placebo-Controlled Trial of Citalopram For The Treatment of Major Depression in Children and AdolescentsSharon AdeleNoch keine Bewertungen
- NIH Public Access: Author ManuscriptDokument7 SeitenNIH Public Access: Author ManuscriptSapto SutardiNoch keine Bewertungen
- Psychiatric Treatment in Primary Care Patients With Anxiety Disorders: A Comparison of Care Received From Primary Care Providers and PsychiatristsDokument7 SeitenPsychiatric Treatment in Primary Care Patients With Anxiety Disorders: A Comparison of Care Received From Primary Care Providers and PsychiatristsBillGhoes'toNoch keine Bewertungen
- Herrmann WM, Stephan K. Int Psychogeriatr. 1992 4 (1) :25-44.Dokument20 SeitenHerrmann WM, Stephan K. Int Psychogeriatr. 1992 4 (1) :25-44.Ангелина СкоморохинаNoch keine Bewertungen
- Duloxetine Treatment For GADDokument8 SeitenDuloxetine Treatment For GADWhitney FarrarNoch keine Bewertungen
- 2015 ExccDokument16 Seiten2015 ExccD.MNoch keine Bewertungen
- Sexual Dysfunction - PsychosisDokument7 SeitenSexual Dysfunction - PsychosisListiana Masyita DewiNoch keine Bewertungen
- Herbel StudyDokument13 SeitenHerbel StudyspamoseNoch keine Bewertungen
- Discuss Assessing The Effectiveness of One TreatmentDokument2 SeitenDiscuss Assessing The Effectiveness of One TreatmentEmilia PiotrakNoch keine Bewertungen
- Behavior TherapyDokument29 SeitenBehavior TherapyKrisztina MkNoch keine Bewertungen
- Suicidio CBT PDFDokument17 SeitenSuicidio CBT PDFMauricio HarkerNoch keine Bewertungen
- Linehan 1991Dokument5 SeitenLinehan 1991Ekatterina DavilaNoch keine Bewertungen
- Antidepressan DepresiDokument10 SeitenAntidepressan DepresiSeptiaPutriNidyatamaNoch keine Bewertungen
- Cognitive Behavioral TherapyDokument14 SeitenCognitive Behavioral TherapyLunaFiaNoch keine Bewertungen
- Prevalen of DDokument8 SeitenPrevalen of DĐỗ Văn ĐứcNoch keine Bewertungen
- Relapse and Impairment in Bipolar DisorderDokument4 SeitenRelapse and Impairment in Bipolar DisorderRakasiwi GalihNoch keine Bewertungen
- 25 Depression Alliance Abstracts, June 09Dokument7 Seiten25 Depression Alliance Abstracts, June 09sunkissedchiffonNoch keine Bewertungen
- Epilepsy & Behavior: Shanna M. Guilfoyle, Sally Monahan, Cindy Wesolowski, Avani C. ModiDokument6 SeitenEpilepsy & Behavior: Shanna M. Guilfoyle, Sally Monahan, Cindy Wesolowski, Avani C. ModiJhonny BatongNoch keine Bewertungen
- Prediction of Psychosis in Youth at High Clinical RiskDokument20 SeitenPrediction of Psychosis in Youth at High Clinical Risksaurav.das2030Noch keine Bewertungen
- Britishjournalofpsychiatry BRITISHJOURNALOFPSYCHIATRY (2001), 179,514 518 (2 0 0 1), 1 7 9, 5 1 4 5 1 8Dokument6 SeitenBritishjournalofpsychiatry BRITISHJOURNALOFPSYCHIATRY (2001), 179,514 518 (2 0 0 1), 1 7 9, 5 1 4 5 1 8Imam FirdausNoch keine Bewertungen
- Affective Instability and Suicidal Ideat20160629 23040 WFCGFH With Cover Page v2Dokument16 SeitenAffective Instability and Suicidal Ideat20160629 23040 WFCGFH With Cover Page v2Clarice Almeida da SilvaNoch keine Bewertungen
- Nursing ResearchDokument9 SeitenNursing Researchapi-546707775Noch keine Bewertungen
- Evaluation of Depression and Suicidal Patients in The Emergency RoomDokument15 SeitenEvaluation of Depression and Suicidal Patients in The Emergency RoomjuanpbagurNoch keine Bewertungen
- Characterisation of Depression in Patients With SchizophreniaDokument7 SeitenCharacterisation of Depression in Patients With SchizophreniaJulián Bravo NaranjoNoch keine Bewertungen
- Lithium Treatment of Conduct Disorders in AdolescentsDokument2 SeitenLithium Treatment of Conduct Disorders in Adolescentsmonicamor74Noch keine Bewertungen
- Cognitive-Behavioral Therapy For Suicide Prevention (CBT-SP) : Treatment Model, Feasibility, and AcceptabilityDokument9 SeitenCognitive-Behavioral Therapy For Suicide Prevention (CBT-SP) : Treatment Model, Feasibility, and AcceptabilityStefan BasilNoch keine Bewertungen
- Comparison of Nefazodone, The Cog Behav Sys of Psychotherapy TX DepressionDokument9 SeitenComparison of Nefazodone, The Cog Behav Sys of Psychotherapy TX DepressionCarolina BerríosNoch keine Bewertungen
- The Long-Term Effects of Antipsychotic Medication on 精神病病程Dokument9 SeitenThe Long-Term Effects of Antipsychotic Medication on 精神病病程wen zhangNoch keine Bewertungen
- We Therell 2009Dokument10 SeitenWe Therell 2009Oslo SaputraNoch keine Bewertungen
- ContentServer 3Dokument8 SeitenContentServer 3Riris KurnialatriNoch keine Bewertungen
- Dropout From Outpatient Mental Health Care in The United StatesDokument10 SeitenDropout From Outpatient Mental Health Care in The United Statescalamr309Noch keine Bewertungen
- Suicidal Intension Among Depresssion pts.-1Dokument18 SeitenSuicidal Intension Among Depresssion pts.-1Firdouse ShajiNoch keine Bewertungen
- 1 s2.0 S0213616321000458 MainDokument10 Seiten1 s2.0 S0213616321000458 MainU of T MedicineNoch keine Bewertungen
- Prevalence and Treatment Outcomes of Persistent Negative Mood Among Children With Attention-Deficit/ Hyperactivity Disorder and Aggressive BehaviorDokument10 SeitenPrevalence and Treatment Outcomes of Persistent Negative Mood Among Children With Attention-Deficit/ Hyperactivity Disorder and Aggressive BehaviorRafael MartinsNoch keine Bewertungen
- Prevalence of Apathy Following Head Injury: R.Kant, J.D.Duffy and A.PivovarnikDokument6 SeitenPrevalence of Apathy Following Head Injury: R.Kant, J.D.Duffy and A.PivovarnikSara GRNoch keine Bewertungen
- Reduced Risk of AnxietyDokument7 SeitenReduced Risk of AnxietySyaika Amelia ZahraNoch keine Bewertungen
- Metaanalisis CBT Vs TauDokument14 SeitenMetaanalisis CBT Vs TauIndrawaty SuhuyanliNoch keine Bewertungen
- Anxiety in Major Depression: Relationship To Suicide AttemptsDokument5 SeitenAnxiety in Major Depression: Relationship To Suicide AttemptsRen DNoch keine Bewertungen
- Are Subjects in Pharmacological Treatment Trials of Depression Representative of Patients in Routine Clinical Practice?Dokument6 SeitenAre Subjects in Pharmacological Treatment Trials of Depression Representative of Patients in Routine Clinical Practice?Sharon AdeleNoch keine Bewertungen
- Depresia CazDokument19 SeitenDepresia CazBetu SasuNoch keine Bewertungen
- Bereavement Challenges and Their Relationship To Physical and Psychological Adjustment To LossDokument10 SeitenBereavement Challenges and Their Relationship To Physical and Psychological Adjustment To LossJeselle CaputolanNoch keine Bewertungen
- Mindfulness: Implications For Substance Abuse and AddictionDokument7 SeitenMindfulness: Implications For Substance Abuse and Addictiontugba1234Noch keine Bewertungen
- Lai 2015Dokument13 SeitenLai 2015tugba1234Noch keine Bewertungen
- Dual Diagnosis and Quality of Life in Patients in Treatment For Opioid DependenceDokument12 SeitenDual Diagnosis and Quality of Life in Patients in Treatment For Opioid Dependencetugba1234Noch keine Bewertungen
- Ijbs 09 216Dokument5 SeitenIjbs 09 216tugba1234Noch keine Bewertungen
- Maybe 2 PDFDokument18 SeitenMaybe 2 PDFSheryl ElitaNoch keine Bewertungen
- Accepted Manuscript: Drug and Alcohol DependenceDokument33 SeitenAccepted Manuscript: Drug and Alcohol Dependencetugba1234Noch keine Bewertungen
- Dr. Hendro-Parallel Symposium 8 PDFDokument15 SeitenDr. Hendro-Parallel Symposium 8 PDFtugba1234Noch keine Bewertungen
- Phenomenology of SchizophreniaDokument7 SeitenPhenomenology of Schizophreniatugba1234Noch keine Bewertungen
- Obtaining International Excellence Through Cross-Border Research Initiatives: A Consortium-Sponsored JournalDokument1 SeiteObtaining International Excellence Through Cross-Border Research Initiatives: A Consortium-Sponsored Journaltugba1234Noch keine Bewertungen
- Hamilton Anxiety Rating Scale (HAM-A)Dokument2 SeitenHamilton Anxiety Rating Scale (HAM-A)Elsa Ameliana ManurungNoch keine Bewertungen
- Phenomenology of SchizophreniaDokument7 SeitenPhenomenology of Schizophreniatugba1234Noch keine Bewertungen
- Classification of Psychiatric Disorders: Ug Class Dept. of PsychiatryDokument26 SeitenClassification of Psychiatric Disorders: Ug Class Dept. of Psychiatrytugba1234Noch keine Bewertungen
- The Hypothalamic-pituitary-Adrenal Axis in Anxiety and PanicDokument6 SeitenThe Hypothalamic-pituitary-Adrenal Axis in Anxiety and Paniccitra dewiNoch keine Bewertungen
- Video Stres OksidatifDokument7 SeitenVideo Stres Oksidatiftugba1234Noch keine Bewertungen
- Tech Titan Usb Anti-Virus User Manual The Ultimate USB Anti-Virus Featured in This Product Is Powered by Kaspersky LabDokument24 SeitenTech Titan Usb Anti-Virus User Manual The Ultimate USB Anti-Virus Featured in This Product Is Powered by Kaspersky Labtugba1234Noch keine Bewertungen
- ARRDokument2 SeitenARRtugba1234Noch keine Bewertungen
- GWL InaDokument25 SeitenGWL Inatugba1234Noch keine Bewertungen
- What Is DepressionDokument5 SeitenWhat Is Depressiontugba1234Noch keine Bewertungen
- Depression Among ODHA JamaicaDokument5 SeitenDepression Among ODHA Jamaicatugba1234Noch keine Bewertungen
- Psikolog Distress PD TBCDokument9 SeitenPsikolog Distress PD TBCtugba1234Noch keine Bewertungen
- Prognosis Apprisal Sheet PDFDokument2 SeitenPrognosis Apprisal Sheet PDFAkhmad AfriantoNoch keine Bewertungen
- Prevalence of Depression in People Living With HIV/AIDS Undergoing ART and Factors Associated With ItDokument9 SeitenPrevalence of Depression in People Living With HIV/AIDS Undergoing ART and Factors Associated With Ittugba1234Noch keine Bewertungen
- Behavioural Weight Loss Intervention With Serious Mentall IllnessDokument9 SeitenBehavioural Weight Loss Intervention With Serious Mentall Illnesstugba1234Noch keine Bewertungen
- 11 Anti Anxiety DrugsDokument17 Seiten11 Anti Anxiety Drugstugba1234Noch keine Bewertungen
- Geriatric Psychiatry, 14: 858-865.: Daftar PustakaDokument5 SeitenGeriatric Psychiatry, 14: 858-865.: Daftar Pustakatugba1234Noch keine Bewertungen
- Simpson Angus ScaleDokument6 SeitenSimpson Angus ScaleManish KumarNoch keine Bewertungen
- Psikotropika Obat Acuan PenggolonganDokument6 SeitenPsikotropika Obat Acuan Penggolongantugba1234Noch keine Bewertungen
- Treatment and PerceptionsDokument24 SeitenTreatment and Perceptionstugba1234Noch keine Bewertungen
- Amnesia and Crime: Dominique Bourget, MD, and Laurie Whitehurst, PHDDokument12 SeitenAmnesia and Crime: Dominique Bourget, MD, and Laurie Whitehurst, PHDtugba1234Noch keine Bewertungen
- Ethical Conflicts in Psychology PDF DownloadDokument2 SeitenEthical Conflicts in Psychology PDF DownloadAvory0% (2)
- DNA Vs RNA - Introduction and Differences Between DNA and RNADokument10 SeitenDNA Vs RNA - Introduction and Differences Between DNA and RNAKienlevyNoch keine Bewertungen
- Brosur YSIO X.preeDokument20 SeitenBrosur YSIO X.preeRadiologi RSUD KilisuciNoch keine Bewertungen
- Music 9 Q3 Mod4 Musical Elements of Given Romantic Period PiecesDokument19 SeitenMusic 9 Q3 Mod4 Musical Elements of Given Romantic Period PiecesFinn Daniel Omayao100% (1)
- Transparency and Digitalization in The Public Administration of RomaniaDokument8 SeitenTransparency and Digitalization in The Public Administration of RomaniaMădălina MarincaşNoch keine Bewertungen
- [18476228 - Organization, Technology and Management in Construction_ an International Journal] Adaptive Reuse_ an Innovative Approach for Generating Sustainable Values for Historic Buildings in Developing CountriesDokument15 Seiten[18476228 - Organization, Technology and Management in Construction_ an International Journal] Adaptive Reuse_ an Innovative Approach for Generating Sustainable Values for Historic Buildings in Developing Countrieslohithsarath bethalaNoch keine Bewertungen
- PetrifiedDokument13 SeitenPetrifiedMarta GortNoch keine Bewertungen
- Paper 1 AnalysisDokument2 SeitenPaper 1 AnalysisNamanNoch keine Bewertungen
- Lab Manual Switchgear and Protection SapDokument46 SeitenLab Manual Switchgear and Protection SapYash MaheshwariNoch keine Bewertungen
- Taoist Master Zhang 张天师Dokument9 SeitenTaoist Master Zhang 张天师QiLeGeGe 麒樂格格100% (2)
- Flow of FoodDokument2 SeitenFlow of FoodGenevaNoch keine Bewertungen
- PNP Ki in July-2017 AdminDokument21 SeitenPNP Ki in July-2017 AdminSina NeouNoch keine Bewertungen
- Classification of Books Using Python and FlaskDokument5 SeitenClassification of Books Using Python and FlaskIJRASETPublicationsNoch keine Bewertungen
- Arts 6 Week 6Dokument9 SeitenArts 6 Week 6JENNEFER ESCALANoch keine Bewertungen
- Web-Based Attendance Management System Using Bimodal Authentication TechniquesDokument61 SeitenWeb-Based Attendance Management System Using Bimodal Authentication TechniquesajextopeNoch keine Bewertungen
- CAREDokument11 SeitenCARELuis SementeNoch keine Bewertungen
- Daewoo 710B PDFDokument59 SeitenDaewoo 710B PDFbgmentNoch keine Bewertungen
- Openvpn ReadmeDokument7 SeitenOpenvpn Readmefzfzfz2014Noch keine Bewertungen
- Clint Freeman ResumeDokument2 SeitenClint Freeman ResumeClint Tiberius FreemanNoch keine Bewertungen
- Jpedal ManualDokument20 SeitenJpedal ManualDamián DávilaNoch keine Bewertungen
- Introduction To Password Cracking Part 1Dokument8 SeitenIntroduction To Password Cracking Part 1Tibyan MuhammedNoch keine Bewertungen
- A 138Dokument1 SeiteA 138pooja g pNoch keine Bewertungen
- ACCA F2 2012 NotesDokument18 SeitenACCA F2 2012 NotesThe ExP GroupNoch keine Bewertungen
- June 2017 (IAL) MS - Unit 1 Edexcel Physics A-LevelDokument16 SeitenJune 2017 (IAL) MS - Unit 1 Edexcel Physics A-LevelNyraStardollNoch keine Bewertungen
- Xtype Power Train DTC SummariesDokument53 SeitenXtype Power Train DTC Summariescardude45750Noch keine Bewertungen
- Toshiba MotorsDokument16 SeitenToshiba MotorsSergio Cabrera100% (1)
- Lesson 1 Q3 Figure Life DrawingDokument10 SeitenLesson 1 Q3 Figure Life DrawingCAHAPNoch keine Bewertungen
- Electrical Engineering Lab Vica AnDokument6 SeitenElectrical Engineering Lab Vica Anabdulnaveed50% (2)
- ST3 ManualDokument48 SeitenST3 ManualRon FosterNoch keine Bewertungen
- Healthymagination at Ge Healthcare SystemsDokument5 SeitenHealthymagination at Ge Healthcare SystemsPrashant Pratap Singh100% (1)
- An Autobiography of Trauma: A Healing JourneyVon EverandAn Autobiography of Trauma: A Healing JourneyBewertung: 5 von 5 Sternen5/5 (2)
- Summary: The Myth of Normal: Trauma, Illness, and Healing in a Toxic Culture By Gabor Maté MD & Daniel Maté: Key Takeaways, Summary & AnalysisVon EverandSummary: The Myth of Normal: Trauma, Illness, and Healing in a Toxic Culture By Gabor Maté MD & Daniel Maté: Key Takeaways, Summary & AnalysisBewertung: 4 von 5 Sternen4/5 (9)
- The Complex PTSD Workbook: A Mind-Body Approach to Regaining Emotional Control & Becoming WholeVon EverandThe Complex PTSD Workbook: A Mind-Body Approach to Regaining Emotional Control & Becoming WholeBewertung: 4.5 von 5 Sternen4.5/5 (49)
- My Grandmother's Hands: Racialized Trauma and the Pathway to Mending Our Hearts and BodiesVon EverandMy Grandmother's Hands: Racialized Trauma and the Pathway to Mending Our Hearts and BodiesBewertung: 5 von 5 Sternen5/5 (70)
- Rewire Your Anxious Brain: How to Use the Neuroscience of Fear to End Anxiety, Panic, and WorryVon EverandRewire Your Anxious Brain: How to Use the Neuroscience of Fear to End Anxiety, Panic, and WorryBewertung: 4.5 von 5 Sternen4.5/5 (157)
- The Upward Spiral: Using Neuroscience to Reverse the Course of Depression, One Small Change at a TimeVon EverandThe Upward Spiral: Using Neuroscience to Reverse the Course of Depression, One Small Change at a TimeBewertung: 4.5 von 5 Sternen4.5/5 (140)
- Summary of The Body Keeps the Score: Brain, Mind, and Body in the Healing of Trauma by Bessel van der Kolk MDVon EverandSummary of The Body Keeps the Score: Brain, Mind, and Body in the Healing of Trauma by Bessel van der Kolk MDBewertung: 4.5 von 5 Sternen4.5/5 (167)
- Vagus Nerve: A Complete Self Help Guide to Stimulate and Activate Vagal Tone — A Self Healing Exercises to Reduce Chronic Illness, PTSD, Anxiety, Inflammation, Depression, Trauma, and AngerVon EverandVagus Nerve: A Complete Self Help Guide to Stimulate and Activate Vagal Tone — A Self Healing Exercises to Reduce Chronic Illness, PTSD, Anxiety, Inflammation, Depression, Trauma, and AngerBewertung: 4.5 von 5 Sternen4.5/5 (16)
- Rapid Weight Loss Hypnosis: How to Lose Weight with Self-Hypnosis, Positive Affirmations, Guided Meditations, and Hypnotherapy to Stop Emotional Eating, Food Addiction, Binge Eating and MoreVon EverandRapid Weight Loss Hypnosis: How to Lose Weight with Self-Hypnosis, Positive Affirmations, Guided Meditations, and Hypnotherapy to Stop Emotional Eating, Food Addiction, Binge Eating and MoreBewertung: 5 von 5 Sternen5/5 (17)
- The Worry Trick: How Your Brain Tricks You into Expecting the Worst and What You Can Do About ItVon EverandThe Worry Trick: How Your Brain Tricks You into Expecting the Worst and What You Can Do About ItBewertung: 4.5 von 5 Sternen4.5/5 (107)
- Somatic Therapy Workbook: A Step-by-Step Guide to Experiencing Greater Mind-Body ConnectionVon EverandSomatic Therapy Workbook: A Step-by-Step Guide to Experiencing Greater Mind-Body ConnectionNoch keine Bewertungen
- Don't Panic: Taking Control of Anxiety AttacksVon EverandDon't Panic: Taking Control of Anxiety AttacksBewertung: 4 von 5 Sternen4/5 (12)
- BORDERLINE PERSONALITY DISORDER: Help Yourself and Help Others. Articulate Guide to BPD. Tools and Techniques to Control Emotions, Anger, and Mood Swings. Save All Your Relationships and Yourself. NEW VERSIONVon EverandBORDERLINE PERSONALITY DISORDER: Help Yourself and Help Others. Articulate Guide to BPD. Tools and Techniques to Control Emotions, Anger, and Mood Swings. Save All Your Relationships and Yourself. NEW VERSIONBewertung: 4.5 von 5 Sternen4.5/5 (24)
- Brain Inflamed: Uncovering the Hidden Causes of Anxiety, Depression, and Other Mood Disorders in Adolescents and TeensVon EverandBrain Inflamed: Uncovering the Hidden Causes of Anxiety, Depression, and Other Mood Disorders in Adolescents and TeensBewertung: 5 von 5 Sternen5/5 (2)
- Summary: No Bad Parts: Healing Trauma and Restoring Wholeness with the Internal Family Systems Model by Richard C. Schwartz PhD & Alanis Morissette: Key Takeaways, Summary & AnalysisVon EverandSummary: No Bad Parts: Healing Trauma and Restoring Wholeness with the Internal Family Systems Model by Richard C. Schwartz PhD & Alanis Morissette: Key Takeaways, Summary & AnalysisBewertung: 5 von 5 Sternen5/5 (5)
- Binaural Beats: Activation of pineal gland – Stress reduction – Meditation – Brainwave entrainment – Deep relaxationVon EverandBinaural Beats: Activation of pineal gland – Stress reduction – Meditation – Brainwave entrainment – Deep relaxationBewertung: 5 von 5 Sternen5/5 (9)
- A Profession Without Reason: The Crisis of Contemporary Psychiatry—Untangled and Solved by Spinoza, Freethinking, and Radical EnlightenmentVon EverandA Profession Without Reason: The Crisis of Contemporary Psychiatry—Untangled and Solved by Spinoza, Freethinking, and Radical EnlightenmentNoch keine Bewertungen
- Critical Thinking: How to Effectively Reason, Understand Irrationality, and Make Better DecisionsVon EverandCritical Thinking: How to Effectively Reason, Understand Irrationality, and Make Better DecisionsBewertung: 4.5 von 5 Sternen4.5/5 (39)
- Heal the Body, Heal the Mind: A Somatic Approach to Moving Beyond TraumaVon EverandHeal the Body, Heal the Mind: A Somatic Approach to Moving Beyond TraumaBewertung: 4.5 von 5 Sternen4.5/5 (56)
- Winning the War in Your Mind: Change Your Thinking, Change Your LifeVon EverandWinning the War in Your Mind: Change Your Thinking, Change Your LifeBewertung: 5 von 5 Sternen5/5 (558)
- Redefining Anxiety: What It Is, What It Isn't, and How to Get Your Life BackVon EverandRedefining Anxiety: What It Is, What It Isn't, and How to Get Your Life BackBewertung: 4.5 von 5 Sternen4.5/5 (152)
- When Religion Hurts You: Healing from Religious Trauma and the Impact of High-Control ReligionVon EverandWhen Religion Hurts You: Healing from Religious Trauma and the Impact of High-Control ReligionBewertung: 4 von 5 Sternen4/5 (11)
- I Don't Want to Talk About It: Overcoming the Secret Legacy of Male DepressionVon EverandI Don't Want to Talk About It: Overcoming the Secret Legacy of Male DepressionBewertung: 4.5 von 5 Sternen4.5/5 (106)
- Feel the Fear… and Do It Anyway: Dynamic Techniques for Turning Fear, Indecision, and Anger into Power, Action, and LoveVon EverandFeel the Fear… and Do It Anyway: Dynamic Techniques for Turning Fear, Indecision, and Anger into Power, Action, and LoveBewertung: 4 von 5 Sternen4/5 (250)





























































































![[18476228 - Organization, Technology and Management in Construction_ an International Journal] Adaptive Reuse_ an Innovative Approach for Generating Sustainable Values for Historic Buildings in Developing Countries](https://imgv2-2-f.scribdassets.com/img/document/422064728/149x198/344a5742a7/1565947342?v=1)