Beruflich Dokumente
Kultur Dokumente
Manejo de Traumatismo Mayor en Pediatria
Hochgeladen von
sucy asto fabianCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Manejo de Traumatismo Mayor en Pediatria
Hochgeladen von
sucy asto fabianCopyright:
Verfügbare Formate
EMM255.
fm Page 418 Monday, November 19, 2001 3:13 PM
Emergency Medicine (2001) 13, 418425
Blackwell Science, Ltd
Paediatric Emergency Medicine
Current trends in the management of
major paediatric trauma
Gary J Browne, Amanda J Cocks and Mary E McCaskill
Department of Emergency Medicine, The Childrens Hospital at Westmead, Sydney,
New South Wales, Australia
Epidemiology
Trauma systems for children
Trauma is the leading cause of death in children
aged 114 years in the developed world. Traumatic
injury is a major cause of disability. It has been said
that inadequate evaluation (and, thus, inappropriate
treatment) contributes to approximately 30% of early
deaths in children with severe trauma.1 Prompt and
accurate assessment of injury severity and early
initiation of critical care is important to prevent such
deaths.
The most common causes of injury in children are
falls, motor vehicle accidents, pedestrian accidents,
bicycle accidents and child abuse. In children under
12 months of age, non-accidental injury is especially
important. Head injury is the most common cause
of morbidity and mortality in paediatric trauma due
to the relatively large head size, less neck control
and plasticity of brain tissues. The presence of a
significant extracranial injury doubles the morbidity
and mortality of children with head trauma. In the
child with severe traumatic injury, multisystem trauma
is typical. This is because of the small body mass, to
which energy is imparted, resulting in a greater force
applied per unit body area. This intense energy leads
to more multisystem injuries.
The trauma system for children in New South Wales
(NSW) uses designated major paediatric trauma
hospitals, together with regional trauma hospitals,
to optimize the trauma care provided for children.
This is supported by a statewide paediatric medical
retrieval service, which ensures provision of expedient
transfer of trauma patients to a major paediatric
trauma hospital.2
Prehospital services have a key role in paediatric
trauma care, as in adult trauma care. In NSW, the
prehospital services are centrally coordinated, but
are regionalized for metropolitan and rural areas.
This allows for assessment at the scene by ambulance personnel and communication via radio to the
receiving emergency department (ED). Airway obstruction and hypovolaemia remain the two most common
prehospital reasons for preventable death in children.
Management of paediatric trauma requires the use
of well-defined criteria to mobilize a trauma team
based on historical and physiological data. Activation
of a trauma team ensures a high level of expertise is
rapidly available. In rural centres, the trauma team
should be composed of locally available expertise for
rapid stabilization and prompt transfer to a major
Key words:
children, differences, outcomes, priorities, trauma.
See Commentary, page 405.
Correspondence:
Dr Gary Browne, Director of Emergency Services, Royal Alexandra Hospital for Children, The Childrens Hospital
at Westmead, Sydney, NSW 2145, Australia. Email: GaryB@chw.edu.au
Gary J Browne, MB BS, FACEM, FRACP( Paed), Director of Emergency Services; Amanda J Cocks, MB BS, FACEM, FRACP(Paed),
Staff Specialist; Mary E McCaskill, MB BS, FACEM, DipPaed, Staff Specialist.
EMM255.fm Page 419 Monday, November 19, 2001 3:13 PM
Paediatric emergency medicine
trauma centre, with advice sought from the major
centre as early as possible.
The family should be involved quickly. Parents are
encouraged to attend the resuscitation, but must be
escorted at all times by a trauma social worker or a
designated senior nurse. This is a key step in managing the child and parents.
Approach to major trauma
Staff need to be mindful of the many differences
between children and adults in anatomy, physiology
and psychology. This makes the assessment of the
injured child and their injuries particularly unique
(Table 1). The child with major trauma can be
haemodynamically unpredictable. Injuries can cross
the usual anatomical boundaries and, commonly, there
is more than one injury. Knowledge of potential
pathophysiology allows for better prediction of outcome. For example, head injury is characterized by
age-related differences in pathobiology and pathophysiology, with the brain in children being less
buoyant and plastic. Therefore, children with diffuse
head injury are more prone to cerebral oedema,
punctate haemorrhage and intracranial hypertension,
problems often associated with transient seizures that
can produce unexpected apnoea. Despite these features, and often a very low Glasgow Coma Scale (GCS)
score on presentation, they often have a good outcome.3
Table 1.
The primary survey and resuscitation
The outcome of children with severe traumatic injury
is related to both the mechanism and extent of injury,
as well as to the success of initial resuscitation.4
Good prognosis following initial resuscitation is suggested by: (i) slowing of the heart rate (< 130 b.p.m.,
with improvement in other physiological signs);
(ii) increased pulse pressure (> 20 mmHg); (iii) return
of normal skin colour; (iv) increased warmth of the
extremities; (v) clearing of sensorium; (vi) increased
systolic blood pressure (> 80 mmHg); and (vii) urinary
output of 12 mL/kg per h.
The purpose of the primary survey in children, as
in adults, is to diagnose and treat life-threatening
conditions and to detect and correct abnormal
physiology, hence avoiding a secondary insult. The
priorities of the primary survey are shown in Table 2.
The nuances of the primary survey as it relates to
paediatrics are discussed below.
Airway with cervical spine control
The anatomy of the airway in children is different to
that of adults. In children, the airway is smaller and
floppier and, in the young child, the disproportion
between the cranium and mid-face makes it more
likely that the airway will obstruct when the child
is lying flat. Children also have a much higher
Differences in paediatric anatomy and physiology
Anatomical/physiological characteristic
Clinical relevance
Small body size
Injuring forces dissipate over a small body mass,
resulting in a high frequency of multiple organ injuries
Places child at risk of hypothermia and dehydration
Places child at particular risk of head injury
and high cervical spine injury
Injuries to internal organs are commonly seen
without external signs of trauma or fracture
(e.g. pulmonary contusions without rib fractures)
Tongue easily obstructs airway
May obscure glottis during intubation
Risk is oesophageal intubation
Uncuffed ETT are used in children < 8 years of
age to avoid pressure necrosis
Risk is intubation of right main bronchus
Large body surface area:mass ratio
Relatively large size of head
Compliant, elastic paediatric skeleton
Airway characteristics
Large tongue, small mouth
Epiglottis less stiff
Larynx more cephalad and anterior
Cricoid cartilage at the narrowest part of airway
Trachea is short
Blood volume is 80 mL/kg
Guides intravenous resuscitation
ETT, endotracheal tube.
419
EMM255.fm Page 420 Monday, November 19, 2001 3:13 PM
GJ Browne et al.
Table 2.
Trauma resuscitation guidelines
Immediate life-threatening injuries
Life-saving procedures
Airway
Obstructed airway
Laryngeal/tracheal trauma
Faciomaxillary trauma
Breathing
Tension pneumothorax
Flail chest
Haemothorax
Sucking chest wound (open pneumothorax)
Central depression of respiration
Haemorrhage
Internal
External
Oxygen; simple airway positioning manoeuvres
Oropharyngeal airway
Endotracheal intubation
Cricothyroidotomy
Tracheostomy
Intercostal cannula
Intercostal tube
Endotracheal intubation
Cover sucking chest wound on three sides
Circulation
Disability
Exposure
Cardiac tamponade/rupture
Neurological dysfunction
Hypothermia
Hypoglycaemia
Pressure over bleeding sites
Two large-bore i.v. cannulas
Intra-osseous infusion
Pericardiocentesis
Emergency thoracotomy (penetrating trauma only)
Avoid secondary brain insult by optimizing ABC
Warming of patient
Warming of all fluids
Substrate as 10% glucose
ABC, airway, breathing and circulation.
respiratory rate and oxygen consumption, and smaller
residual volume, and this may lead to earlier hypoxia.
Establishment of an open airway should be initially
attempted by using standard simple airway manoeuvres. In the setting of trauma and possible cervical
spine injury, this should involve a jaw thrust with
cervical spine immobilization and suction. The oropharyngeal airway may assist in maintaining this
open airway. The oropharyngeal airway in children is
inserted using a tongue depressor and placing it
directly, rather than inserting the airway upside down
and rotating 180, as is performed in adults.
Intubation is not immediately necessary if a patent
airway and adequate ventilation are achieved. However,
in major paediatric trauma, rapid sequence intubation
is often required. The size of the endotracheal tube
( ETT) required can be estimated by looking at the size
of the childs little finger or it can be calculated using
the formula:
ETT internal diameter = age /4 + 4 ( > 1 year)
The level at which the ETT should be taped at the lips
can be estimated by watching the ETT pass between
the vocal cords and advancing it approximately 3 cm.
Alternatively, this can be calculated using the formula:
420
Level at lips + age/2 + 12 ( > 1 year)
The choice of drugs for rapid sequence intubation
will be a muscle relaxant and sedative and, in children under 2 years of age, we recommend the use of
atropine to prevent the severe bradycardia that can
occur on intubation. A detailed discussion of tracheal intubation is beyond the scope of the present
paper.
Airway obstruction in children is rarely complete,
the exception being facial burns, facial trauma and
laryngeal injury. Children who are partially obstructed
but are making good respiratory effort and are well
saturated should be allowed to adopt a position of
comfort while expert help is summoned in order to
provide definitive treatment. In the obtunded patient,
the insertion of a laryngeal mask airway (LMA) can
provide an adequate airway, avoiding the need for
cricothyrotomy. If airway obstruction is complete and
LMA insertion is not possible, a needle cricothyrotomy should be considered. This is performed using
a 1418 gauge cannula connected to a three-way tap
and oxygen at 15 L/min. Needle cricothyrotomy is a
temporizing measure only and a definitive surgical
tracheostomy should be completed within 2 h. Surgical
cricothyrotomy is contraindicated in children under
EMM255.fm Page 421 Monday, November 19, 2001 3:13 PM
Paediatric emergency medicine
11 years of age because it is fraught with difficulty and
rarely gives a satisfactory result.
Cervical spine
Children with possible cervical spine injury should be
immobilized appropriately using in-line axial bimanual
immobilization or a hard cervical collar of appropriate
size, sandbags and adhesive tape strap-ping the head
and trunk to a spinal board. In young infants, a rolledup towel under the shoulder can overcome spinal
malalignment due the protrusion of the occiput.5
X-Rays of the cervical spine in the awake child
under 5 years of age consist of two static cervical spine
X-rays (anteroposterior and lateral) and, if necessary,
a fine-cut axial computed tomography (CT) scan. The
open-mouth odontoid (OMO) view in young children is
frequently of poor quality and is unsatisfactory for
reporting. It is performed to exclude a fracture of the
dens, which almost exclusively occurs through the
synchondosis in children under 5 years of age and
is easily seen on a good lateral film.6,7 Obtaining
adequate flexionextension films in children under
5 years of age is difficult; false-negative reporting is
common and should not be relied on to clear the
cervical spine.8 A more detailed assessment of cervical
spine injury in children is given in (Fig. 1).8,9
Breathing
The administration of high-flow supplemental oxygen
(12 L/min) via a reservoir oxygen facemask is given
to all children with significant injury. Assisted ventilation with a bagvalve mask device is required if
spontaneous ventilation is inadequate.
Tension pneumothorax may be well tolerated in
small children due to increased tissue elasticity. Once
clinical signs develop, this suggests that the airway
pressure has increased to levels that will result in
imminent cardiovascular collapse. Tension pneumothorax is relieved by inserting a 1418 gauge overthe-needle catheter into the affected side. In children,
use the second intercostal space, mid-clavicular line,
while in the small infant use the fourth intercostal
space, anterior axillary line, thus avoiding complications due to limited space during resuscitation due
to small body size. The pneumothorax must then be
definitively treated by inserting a chest tube. Traumatic
asphyxia is a syndrome of cervicofacial cyanosis, sub-
conjunctival haemorrhages, venous engorgement and
petechiae of the head and neck. Although it is rare,
traumatic asphyxia is commonly associated with other
injuries, such as blunt pulmonary injury, and may
result in unexpected clinical deterioration if not diagnosed early in the primary survey.10
Circulation
Shock is a syndrome that results from tissue perfusion that is inadequate to meet metabolic needs. In
children, it may exist with normal blood pressure.
Although cardiac output falls in children in an almost
linear fashion as blood volume is depleted, blood
pressure is unchanged because of increased vascular
resistance and tachycardia, which maintain cardiac
output. When cardiac reserve is depleted, hypotension
occurs. A bradycardia indicates a grave situation.
Hypotension is, therefore, a late and often sudden sign
of cardiovascular decompensation. After life-threatening
conditions, such as cardiac tamponade, are excluded,
a persistent tachycardia may be the only indication
that there is occult blood loss with persistent shock.
The childs initial vasoconstrictive response to
hypovolaemia is why intravenous access can be
difficult. If no intravascular access is established after
6090 s, or three attempts in an unstable child, try the
intra-osseous route. Insert the intra-osseous needle in
the proximal tibia or distal femur, directing the needle
away from the epiphyseal plate. Fluids and drugs can
be given with the assistance of a pressure-infusion
device. Avoid the intra-osseous route in the presence
of a tibial or femoral fracture, inferior vena cava
disruption or a vascular injury in the affected leg.
All intravenous (i.v.) fluids should be administered
warmed to 37C to reduce the occurrence of hypothermia. If a patient fails to improve after two fluid
boluses of 20 mL/kg each, then blood (whole blood
20 mL/kg or packed cells 10 mL/kg) is required. If
packed cells are used, the volume is made up using
saline, plasma or 5% albumin. If the child is stable
and blood is available within 1015 min, wait for fully
cross-matched blood. If the child is unstable, typespecific blood may have to be used. If a delay of even a
few minutes is critical, group O-negative blood is given.
Children have small blood volumes and cannot
afford to loose large amounts of blood if haemodynamic instability is to be avoided. Occult blood
loss from the head and neck region, in particular
from scalp lacerations, can result in haemodynamic
421
EMM255.fm Page 422 Monday, November 19, 2001 3:13 PM
GJ Browne et al.
Figure 1. Paediatric cervical spine assessment. C-spine, cervical spine; CT, computed tomography; ED, emergency department; MRI,
magnetic resonance imaging.
422
EMM255.fm Page 423 Monday, November 19, 2001 3:13 PM
Paediatric emergency medicine
instability. Aggressive control of haemorrhage (direct
pressure to external bleeding sites) is indicated. In
children with multisystem trauma, stabilizing fractures of the femur may be crucial for pain relief and
control of bleeding. Thomas splints are not available in appropriate sizes for smaller children. Where
haemodynamic instability is of concern, a medical
antishock trousers (MAST) suit of appropriate size
should be used.
A haemodynamically unstable child should never
be sent to CT scan to define the site of bleeding. The
only option is surgical intervention.
Choice of fluid for resuscitation
Much remains to be learnt about fluid resuscitation
in children. The choice of colloid over crystalloid has
been reported to increase mortality, although evidence is weak and remains unproven in critically ill
children.11 In children, blunt trauma is the rule and
the liberal use of fluids is the current accepted practice, titrating this to the clinical response of the child.
Mortality in injured children is associated with
an Injury Severity Scale 25, a GCS score 7 or a
Paediatric Trauma Scale 4. The amount of emergency blood transfusion required is singularly the
most important independent predictive factor of
outcome in children because blood transfused in
amounts 20 mL/kg significantly increases the risk
of coagulopathy and multisystem organ failure. There
is a need for better end-points of resuscitation in
children if adverse outcomes from fluid mismanagement are to be avoided. Traditionally, normal pulse
rate and systolic blood pressure for age and urine
output > 1 mL/kg per h usually signify adequate fluid
resuscitation. Metabolic end-points, such as base
excess and lactate, can augment traditional signs of
successful resuscitation12 and may be useful measures
in the injured child (Table 3). Physicians must be
aware that the excessive use of chloride-containing
fluids can cause hyperchloraemic acidosis, resulting
in persistently abnormal base excess. This can cause
fluid overload if not recognized.
There are some special situations in which care
should be taken with fluid resuscitation. We have
perceived an increase in penetrating trauma in
children, which has raised the issue of delayed
resuscitation in this group. The aim is to promote clot
stabilization in a more physiological environment and
allow surgical intervention to occur in a controlled
Table 3.
Metabolic end-points useful initially in resuscitation 12
Base excess
Lactate (mmol/L)
Mild
Moderate
Severe
2 to 5
<2
6 to 14
24
< 15
>4
way.13 Delayed resuscitation in paediatric penetrating
trauma should only be considered if surgical intervention is imminent. However, it remains to be shown
whether this approach improves patient outcome.
Fluid therapy must also be carefully considered
in the management of traumatic brain injury (TBI) in
children. The aim is to prevent secondary insult from
systemic hypotension, hypoxia and intracranial hypertension. Optimization of cerebral perfusion pressure
(CPP; the difference between mean arterial pressure
(MAP) and intracranial pressure (ICP)) is a therapeutic
aim in the management of brain-injured patients. It is
believed that neurological outcome improves if CPP is
maintained at levels of 6070 mmH 2O. Hypotension
is the single most important correctable cause of
secondary brain injury with a direct affect on CPP.
Appropriate use of fluids and the early introduction
of inotropes in maintaining MAP of at least 70 mmHg,
to avoid fluid overload, is recommended.14
Disability or attention to central
nervous system disorder
To quickly assess paediatric disability in the primary
survey use the AVPU mnemonic: the child will either
be Alert, responsive to Verbal stimuli, responsive to
Painful stimuli or Unresponsive. A score of P or U
suggests a GCS score < 8 and requires urgent attention and further assessment. Note pupillary size and
reaction to light.
Exposure and things not to forget
1. Undress the child fully to examine the entire body.
2. Children are prone to hypothermia. Monitor core
temperature via a rectal probe. Expose the child
only as long as it takes to complete the physical
examination. Maintain normothermia by using
warmed i.v. fluids, blood warmers, warm blankets
and overhead heating lamps.
3. Agitation and/or pain needs aggressive management. Adequate analgesia must be provided early
423
EMM255.fm Page 424 Monday, November 19, 2001 3:13 PM
GJ Browne et al.
and is most appropriately provided through the
use of intravenous opiates. Intravenous morphine
should be titrated carefully to relieve severe pain,
commencing with a dose of 0.10.2 mg/kg. The
treatment of pain allows for better clinical assessment and helps prevent secondary insult due to
agitation caused by pain.
4. Ensure adequate monitoring of children: respiratory
rate, blood pressure, oxygen saturation, heart rate
and peripheral perfusion.
5. Check all hardware on children who have been
transported to hospital.
6. Psychological support must be provided early to
family and child by an appropriate member of the
trauma team, assisted by the team social worker.
Secondary survey: Paediatric priorities
The important aspects of the secondary survey with
respect to paediatric trauma are:
1. Continuing resuscitation and monitoring. Any
deterioration mandates immediate return to the
airway, breathing and circulation (ABC). Remember,
blunt abdominal injury is the second-most frequent
cause of preventable death in paediatric trauma
after airway problems.
2. History. An AMPLE history should be obtained
from the child (if possible), family, ambulance personnel, friends and bystanders using the mnemonic:
A: Allergies
M: Medication
P: Past history
L: Last ate; Last tetanus
E: Event
3. Head-to-toe examination. Perform a systematic
head-to-toe, front-and-back examination to detect
any injuries not noted in the primary survey. A
formal assessment of the childs neurological state
should now be performed, including documentation of the paediatric coma score (Table 4). The
need to perform a digital rectal examination on a
paediatric trauma patient should be assessed on an
individual basis by the attending surgical trauma
team member.
4. Investigations. Blood specimens should already
have been collected during the resuscitation phase.
Hypoglycaemia may be present and a bedside blood
sugar level should be performed at this time. In
terms of radiological investigations, a standard
trauma series is required (i.e. chest X-ray, lateral
424
Table 4.
Paediatric Glasgow Coma Scale scores.
Response
Eye opening (all ages)
Spontaneously
Response to voice
Response to pain
No reponse
Best motor response
> 1 year
Obeys commands
Localizes pain
Flexion withdrawal
Decorticate posturing
Decerebrate posturing
No response
< 1 year
Spontaneously
Localizes pain
Flexion withdrawal
Decorticate posturing
Decerebrate posturing
No response
Best verbal response
> 5 years
Oriented and appropriate
Disoriented conversation
Inappropriate words
Incomprehensible sounds
No response
25 years
Appropriate words
Inappropriate words
Cries and/or screams
Grunts
No response
023 months
Smiles, coos
Cries but consolable
Persistant cries and/or screams
Grunts
No response
Score
4
3
2
1
6
5
4
3
2
1
6
5
4
3
2
1
5
4
3
2
1
5
4
3
2
1
5
4
3
2
1
Entries given for eye opening, best motor response in children
> 1 year of age and best verbal response for children > 5 years of age
are the traditional Glasgow Coma Scale.
cervical spine X-ray and pelvic X-ray). Further
radiological investigation will be determined by
clinical assessment. An electrocardiogram should
be performed in cases of chest trauma with suspected myocardial contusion.
EMM255.fm Page 425 Monday, November 19, 2001 3:13 PM
Paediatric emergency medicine
Observation and re-evaluation
Abdominal trauma is the leading cause of initially
unrecognized fatal injury in children. Unique anatomical features predispose children to a variety of
abdominal injuries. Particular injury mechanisms lead
to specific injuries that can be difficult to identify (e.g.
lap belt injury).15 Abdominal signs of injury may be
absent. If abdominal trauma is considered likely in a
stable child, consider observation and serial evaluations. This should be done only if the child is
haemodynamically stable. The focus should be on
increasing tenderness and distension during serial
abdominal examinations. Gastric tube decompression
may aid examination. Aspiration of blood suggests
significant injury. Serial testing of urine for blood
may detect occult renal injury.16 Diagnostic peritoneal
lavage has no role in paediatric trauma.
Definitive care and disposition
After completion of the secondary survey, reassess the
childs response to resuscitation and prioritize injuries
according to immediate threats to life and then those
with potential morbidity. Urgent laparotomy in the
child with an abdominal injury should be considered if:
1. The child remains hypotensive despite 40 mL/kg
i.v. fluid resuscitation over a 6 h period (i.e. half the
blood volume).
2. A hollow viscus injury is suspected (e.g. free air on
chest or abdominal X-ray).
3. Diaphragmatic rupture is detected on chest X-ray
or abdominal CT scan.
4. Significant gastrointestinal haemorrhage is detected
by nasogastric tube or rectal examination.
Analgesia continues to be an important consideration throughout the childs stay in the ED. Regional
nerve block of the femoral nerve is of value for fractured femur. Nitrous oxide may be useful, especially
in orthopaedic injuries, but should be avoid in TBI,
pneumothorax or eye injuries. Methoxyfluorane is
proving valuable in managing pain in children with
orthopaedic and eye injuries (G Browne, pers. obs.).
The management of major paediatric trauma
requires a multidisciplinary approach so that medical
care is tailored to meet the specific needs of the injured
child and, in addition, attends to the needs of their
family. An understanding of the different patho-
biology, pathophysiology and the unique way in which
children can present with major trauma will allow this
multidisciplinary team to achieve the best possible
patient outcome.
References
1.
Furnival RA, Woodward GA, Schunk JE. Delayed diagnosis of
injury in pediatric trauma. Pediatrics 1996; 98: 56 62.
2.
Hulka F, Mullins RJ, Mann NC et al. Influence of a state-wide
trauma system in pediatric hospitalization and outcome. J.
Trauma 1997; 42: 514 19.
3.
Lieh-Lai MW, Theodorou AA, Sarnaik AP et al. Limitations of
the Glasgow Coma Scale in predicting outcome in children with
traumatic brain injury. J. Pediatr. 1992; 120: 195 9.
4.
Orliaguet GA, Meter PG, Blanot S et al. Predictive factors of
outcome in severely traumatised children. Anesthesia Analgesia
1998; 87: 537 42.
5.
Nypaver M, Treloar D. Neutral cervical spine positioning in
children. Ann. Emerg Med. 1994; 23: 208 11.
6.
Swischuk LE, John SD, Hendrick EP. Is the open-mouth
odontoid view necessary in children under 5 years? Pediatr.
Radiol. 2000; 30: 186 9.
7.
Gohn D, Armstrong D, Beck L et al. Cervical spine injuries in
children. J. Trauma 1990; 30: 463 9.
8.
Dwek JR, Chung CB. Radiography of cervical spine injury in
children: Are flexion extension radiographs useful for acute
trauma? Am. J. Radiol. 2000; 174: 161719.
9.
Hoffman JR, Mower WR, Wolfson AB et al. Validity of a set of
clinical criteria to rule out injury to the cervical spine in
patients with blunt trauma. N. Engl. J. Med. 2000; 343: 94 9.
10. Black TL, Snyder CL, Miller JP et al. Significance of chest
trauma in children. South. Med. J. 1996; 89: 494 6.
11. Cochrane Injuries Group Albumin Reviewers. Human albumin
administration in critically ill patients. Systemic review of
randomised controlled trials. BMJ 1998; 317: 235 42.
12. Davis JW, Parks SN, Kaups KL et al. Admission base deficit
predicts transfusion requirements and risk of complications.
J. Trauma 1996; 41: 769 74.
13. Bickell WH, Wall MJ, Pepe PE et al. Immediate versus delayed
fluid resuscitation for hypotensive patients with penetrating
torso injuries. N. Engl. J. Med. 1994; 331: 1105 9.
14. Barlow KM, Minns RA. The relation between intracranial
pressure and outcome in non-accidental head injury. Dev. Med.
Child. Neurol. 1999; 41: 220 5.
15. Myers LG, Dent DL, Stewart RM et al. Blunt splenic injuries.
Dedicated surgeons can achieve a high rate of non-operative
success in patients of all ages. J. Trauma 2000; 48: 801 8.
16. Rothrock SG, Green SM, Morgan R. Abdominal trauma in
infants and children: Prompt identification and early management of serious and life-threatening injuries. Pediatr. Emerg.
Care 2000; 16: 106 15.
425
Das könnte Ihnen auch gefallen
- Initial Assessment and Management of Pediatric Trauma PatientsDokument8 SeitenInitial Assessment and Management of Pediatric Trauma PatientsannisaNoch keine Bewertungen
- Research Paper On Shaken Baby SyndromeDokument8 SeitenResearch Paper On Shaken Baby Syndromefys4gjmk100% (1)
- Help Pedsurgeryafrica30Dokument10 SeitenHelp Pedsurgeryafrica30Andi Firman MubarakNoch keine Bewertungen
- Management of Pediatric Mandible Fractures PDFDokument16 SeitenManagement of Pediatric Mandible Fractures PDFarfahNoch keine Bewertungen
- The Kids Are Alright Pediatric Trauma PearlsDokument21 SeitenThe Kids Are Alright Pediatric Trauma PearlsDaniel Torres CutivaNoch keine Bewertungen
- Initial Assessment and Management OF Pediatric Trauma PatientsDokument11 SeitenInitial Assessment and Management OF Pediatric Trauma PatientsCarlos TellezNoch keine Bewertungen
- Thoracic TraumaDokument39 SeitenThoracic TraumaYaniNoch keine Bewertungen
- Conference Paper: Rapid Physical Assessment of The Injured ChildDokument4 SeitenConference Paper: Rapid Physical Assessment of The Injured ChildMaiush JbNoch keine Bewertungen
- Perioperative Management of The Pediatric Patient With Traumatic Brain InjuryDokument14 SeitenPerioperative Management of The Pediatric Patient With Traumatic Brain InjuryBaha MirzaeifarNoch keine Bewertungen
- Thesis On Birth AsphyxiaDokument4 SeitenThesis On Birth Asphyxiaimmkhuwhd100% (3)
- Glasgow Coma ScaleDokument13 SeitenGlasgow Coma ScaleDanna Christine Gumboc PaguntalanNoch keine Bewertungen
- Tec 2012Dokument16 SeitenTec 2012claugg123Noch keine Bewertungen
- Open Fractures in ChildrenDokument16 SeitenOpen Fractures in ChildrenCristina Rivas DuarteNoch keine Bewertungen
- Biomedical Journal: SciencedirectDokument11 SeitenBiomedical Journal: SciencedirectTahir AlyasNoch keine Bewertungen
- Trauma in Children: Initial Assessment and ManagementDokument39 SeitenTrauma in Children: Initial Assessment and ManagementDrTushar GoswamiNoch keine Bewertungen
- Rapid Physical Assessment of The Injured Child: Robert Steelman, MD, DMDDokument4 SeitenRapid Physical Assessment of The Injured Child: Robert Steelman, MD, DMDkrantiNoch keine Bewertungen
- Birth TraumaDokument18 SeitenBirth TraumaJemmy SieNoch keine Bewertungen
- Chapter 157 Trauma in ChildrenDokument4 SeitenChapter 157 Trauma in ChildrenDezarae LetoNoch keine Bewertungen
- Pediatric Trauma: Presented By: Erwin MaulanaDokument39 SeitenPediatric Trauma: Presented By: Erwin Maulanaadliah zahiraNoch keine Bewertungen
- Pediatric Head Injury 2013Dokument16 SeitenPediatric Head Injury 2013Salim Issa KhamashtaNoch keine Bewertungen
- Management of Facial AsymmetryDokument28 SeitenManagement of Facial AsymmetrykrazeedoctorNoch keine Bewertungen
- Trauma in ChildrenDokument11 SeitenTrauma in ChildrenEdwardRazvanNoch keine Bewertungen
- Pediatrics 2005 Trotter 771 83Dokument16 SeitenPediatrics 2005 Trotter 771 83Ligia RiosNoch keine Bewertungen
- Paediatric Trauma: Pauline M Cullen MBCHB FrcaDokument5 SeitenPaediatric Trauma: Pauline M Cullen MBCHB FrcadamonenNoch keine Bewertungen
- Cervical Spine Injury: Julie C. LeonardDokument15 SeitenCervical Spine Injury: Julie C. LeonardCamilla CristinaNoch keine Bewertungen
- Seminars in Pediatric Surgery: Progress in Anesthesia and Management of The Newborn Surgical PatientDokument5 SeitenSeminars in Pediatric Surgery: Progress in Anesthesia and Management of The Newborn Surgical PatientAsif KhanNoch keine Bewertungen
- JMedSci345238-453531 123553Dokument3 SeitenJMedSci345238-453531 123553Rachmad SanjayaNoch keine Bewertungen
- BB Sacudido PDFDokument62 SeitenBB Sacudido PDFEvelynMenesesNoch keine Bewertungen
- Pediatric Voice Disorder Diagnosis and Treatment Options Beyond NodulesDokument8 SeitenPediatric Voice Disorder Diagnosis and Treatment Options Beyond NodulesDaniel Celestino DiazNoch keine Bewertungen
- A Framework For The Management of The Pediatric AirwayDokument23 SeitenA Framework For The Management of The Pediatric AirwayDaniel GallegoNoch keine Bewertungen
- Pediatric Trauma PrioritiesDokument60 SeitenPediatric Trauma PrioritiesThan WynnNoch keine Bewertungen
- To Be ConDokument53 SeitenTo Be ConLiza AingelicaNoch keine Bewertungen
- Birth IjryDokument13 SeitenBirth IjryNaresh JeengarNoch keine Bewertungen
- Positional Plagiocephaly From Structure To Function Clinic - 2020 - Early HumanDokument6 SeitenPositional Plagiocephaly From Structure To Function Clinic - 2020 - Early HumanmireliNoch keine Bewertungen
- Nurs 641 Case Study PresentationDokument12 SeitenNurs 641 Case Study Presentationapi-251235373Noch keine Bewertungen
- Smile Restoration After Facial PalsyDokument6 SeitenSmile Restoration After Facial PalsyJimmie CooperNoch keine Bewertungen
- Choanal AtresiaDokument8 SeitenChoanal AtresiaCharmila Sari0% (1)
- Birth InjuriesDokument7 SeitenBirth InjuriesWendy NyamweyaNoch keine Bewertungen
- Children With Achondroplasia Guidance For Parents and Health Care ProfessionalsDokument22 SeitenChildren With Achondroplasia Guidance For Parents and Health Care Professionalshorace35Noch keine Bewertungen
- The Pediatric Physical Examination - HEENT - UpToDateDokument87 SeitenThe Pediatric Physical Examination - HEENT - UpToDateEmily LinharesNoch keine Bewertungen
- Imaging Abusive Head Trauma: Why Use Both Computed Tomography and Magnetic Resonance Imaging?Dokument15 SeitenImaging Abusive Head Trauma: Why Use Both Computed Tomography and Magnetic Resonance Imaging?ariqNoch keine Bewertungen
- Anotia/Microtia: Minnesota Department of Health Fact Sheet November 2005Dokument3 SeitenAnotia/Microtia: Minnesota Department of Health Fact Sheet November 2005Carlos Santiago VivenzaNoch keine Bewertungen
- Otogenic Brain Abscess Treatment ExperienceDokument5 SeitenOtogenic Brain Abscess Treatment ExperienceNeysaAzaliaEfrimaisaNoch keine Bewertungen
- CP Neon EncepthDokument9 SeitenCP Neon EncepthJuan Carlos HuanacheaNoch keine Bewertungen
- Test Bank For Essentials of Pediatric Nursing 1st Edition Theresa KyleDokument13 SeitenTest Bank For Essentials of Pediatric Nursing 1st Edition Theresa KyleAnthonyRiveraqion100% (32)
- Lesiones Centinelas en Abuso FiěsicoDokument13 SeitenLesiones Centinelas en Abuso FiěsicoagraslfNoch keine Bewertungen
- Neral ConsiderationsDokument13 SeitenNeral ConsiderationsNga NguyễnNoch keine Bewertungen
- Dental Management of Cerebral PalsyDokument17 SeitenDental Management of Cerebral PalsyIJAR JOURNALNoch keine Bewertungen
- RCH DEM Head Injury GuidelinesDokument4 SeitenRCH DEM Head Injury GuidelinesJerry LeeNoch keine Bewertungen
- Pediatricfacialtrauma: Tom W. Andrew,, Roshan Morbia,, H. Peter LorenzDokument9 SeitenPediatricfacialtrauma: Tom W. Andrew,, Roshan Morbia,, H. Peter LorenzFivi KurniawatiNoch keine Bewertungen
- Pediatric Trauma Care EssentialsDokument39 SeitenPediatric Trauma Care Essentialspuja argaNoch keine Bewertungen
- An Update On The Perioperative Management of Children With Upper Respiratory InfectionsDokument18 SeitenAn Update On The Perioperative Management of Children With Upper Respiratory InfectionsAditya ManjunathNoch keine Bewertungen
- Tepas 1987Dokument12 SeitenTepas 1987IipAlqadrieNoch keine Bewertungen
- CACAS Activity5 Case Study On A NewbornDokument5 SeitenCACAS Activity5 Case Study On A Newbornxianell dinglasanNoch keine Bewertungen
- Managing Minor Head Injuries in ChildrenDokument9 SeitenManaging Minor Head Injuries in ChildrenHesti Nurmala RizqiNoch keine Bewertungen
- Taylor - Pediatric TraumaDokument5 SeitenTaylor - Pediatric TraumaRicardo GrilloNoch keine Bewertungen
- 0 The Child With Hearing LossDokument2 Seiten0 The Child With Hearing LossGirish SubashNoch keine Bewertungen
- Techniques in Pediatric MRI - Tips For Imaging Children: How-I-do-itDokument11 SeitenTechniques in Pediatric MRI - Tips For Imaging Children: How-I-do-itBOUSSAID KARIMNoch keine Bewertungen
- Primary Management of PolytraumaVon EverandPrimary Management of PolytraumaSuk-Kyung HongNoch keine Bewertungen
- State-by-State Laws Report 2015Dokument238 SeitenState-by-State Laws Report 2015MPP100% (5)
- Laporan Faal Respi 2021 - Kenni KenedyDokument25 SeitenLaporan Faal Respi 2021 - Kenni Kenedykenni kenedyNoch keine Bewertungen
- KAT - Official GuideDokument11 SeitenKAT - Official GuideMatheus MendonçaNoch keine Bewertungen
- 1.2 Dangerous Area of The ScalpDokument8 Seiten1.2 Dangerous Area of The Scalpvague_darklord50% (2)
- Improving vision through cataract procedures and YAG capsulotomyDokument9 SeitenImproving vision through cataract procedures and YAG capsulotomyBplo CaloocanNoch keine Bewertungen
- 10.1007-S00210-008-027serotonin Pharmacology in The Gastrointestinal Tract: A ReviewDokument23 Seiten10.1007-S00210-008-027serotonin Pharmacology in The Gastrointestinal Tract: A ReviewanataeusNoch keine Bewertungen
- OBDokument9 SeitenOBDennis ArevaloNoch keine Bewertungen
- Nclex Exam Maternal and Child Health Nursing 2 30 Items PDF FreeDokument8 SeitenNclex Exam Maternal and Child Health Nursing 2 30 Items PDF FreeLianne BuensucesoNoch keine Bewertungen
- Diabetic Ketoacidosis - Anand Singh BrarDokument5 SeitenDiabetic Ketoacidosis - Anand Singh BrarAnand Singh BrarNoch keine Bewertungen
- A3 24pt 9BN0 - 01 Question Paper PDFDokument69 SeitenA3 24pt 9BN0 - 01 Question Paper PDFAhmed SadhanNoch keine Bewertungen
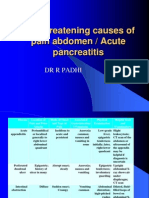
- Life Threatening Causes of Pain Abdomen / Acute PancreatitisDokument27 SeitenLife Threatening Causes of Pain Abdomen / Acute PancreatitisDr. Rajesh Padhi100% (1)
- CDLQIDokument1 SeiteCDLQIYossy VesriNoch keine Bewertungen
- The Functional Value of Electrical Muscle Stimulation For The Rehabilitation of The Hand In..Dokument2 SeitenThe Functional Value of Electrical Muscle Stimulation For The Rehabilitation of The Hand In..Marco PastoreNoch keine Bewertungen
- FNCPDokument3 SeitenFNCPNyj QuiñoNoch keine Bewertungen
- Eye - Blur Vision Part IIDokument56 SeitenEye - Blur Vision Part IIStaporn Kasemsripitak100% (2)
- CV Disease Drug StudyDokument11 SeitenCV Disease Drug StudyMaria Francheska OsiNoch keine Bewertungen
- Warfarin INR Antibx InteractionDokument3 SeitenWarfarin INR Antibx InteractionSheila UlinaNoch keine Bewertungen
- Dermatologic PharmacologyDokument88 SeitenDermatologic PharmacologyAlunaficha Melody KiraniaNoch keine Bewertungen
- English Role Play Script for Nursing StudentsDokument4 SeitenEnglish Role Play Script for Nursing StudentsIefana Fihtreey TaezZkeyaNoch keine Bewertungen
- Stepladder Plating Following Lower Subapical and Geniop - 2022 - Advances in OraDokument2 SeitenStepladder Plating Following Lower Subapical and Geniop - 2022 - Advances in OraГне ДзжNoch keine Bewertungen
- Psych Lab Finals (NCM 117)Dokument12 SeitenPsych Lab Finals (NCM 117)Harvey T. Dato-onNoch keine Bewertungen
- Drug Study Ready TramadolDokument1 SeiteDrug Study Ready TramadolCezanne CruzNoch keine Bewertungen
- SPPDDokument1 SeiteSPPDBahul MunirNoch keine Bewertungen
- Lecture - 3 Properties of Cardiac MuscleDokument35 SeitenLecture - 3 Properties of Cardiac MuscleMRM7MDNoch keine Bewertungen
- MMC 1Dokument48 SeitenMMC 1Tianliang GuoNoch keine Bewertungen
- General Parasitology L2Dokument27 SeitenGeneral Parasitology L2kayse abtidoonNoch keine Bewertungen
- Gpat SylabusDokument2 SeitenGpat Sylabusdeepanshushilpi786Noch keine Bewertungen
- Expression of Vascular Endothelial Growth Factor (VEGF) and New Blood Vessels Formation On Wound Incision Post Ropivacaine Administration in Animal ModelDokument8 SeitenExpression of Vascular Endothelial Growth Factor (VEGF) and New Blood Vessels Formation On Wound Incision Post Ropivacaine Administration in Animal ModelInternational Journal of Innovative Science and Research TechnologyNoch keine Bewertungen
- Nursing Responsibilities Adverse Effect Indication / Contraindication Mechanism of Action Drug Name IndicationDokument1 SeiteNursing Responsibilities Adverse Effect Indication / Contraindication Mechanism of Action Drug Name IndicationOmar IzzoNoch keine Bewertungen
- Saint Peter's Physician Associates - Our Doctors in Your NeighborhoodDokument2 SeitenSaint Peter's Physician Associates - Our Doctors in Your NeighborhoodSaint Peter's Healthcare SystemNoch keine Bewertungen