Beruflich Dokumente
Kultur Dokumente
Orthopaedics: Differential Diagnoses of Joint/Bone Pain
Hochgeladen von
Sok-Moi ChokCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Orthopaedics: Differential Diagnoses of Joint/Bone Pain
Hochgeladen von
Sok-Moi ChokCopyright:
Verfügbare Formate
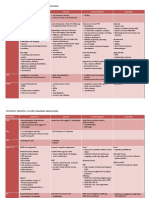
ORTHOPAEDICS: DDx JOINT PAIN | S.M.
CHOK (Manchester Medical School)
INTRINSIC SHOULDER PAIN
Rotator Cuff Disorder
rotator cuff tendinopathy
Hx:
aged 35-60
after heavy lifting, repetitive movements
often in the non-dominant arm
Examinations:
muscle wasting
pain on movements, pain on abduction with thumb down
worse against resistance
restriction of active movements, full but painful passive movements
painful arc (45-160 of active abduction)
impingement (70-140)
most common: supraspinatous in subacromial space
Mx:
active movement with physio and analgesia
subacromial bursa injection of steroids
arthroscopic acromioplasty
subacromial bursitis (rare)
Hx: infections, injury
Examinations:
pinching pain, pain with motion
swelling
tenderness
+ve impingement test
Ix:
X-ray (recurrent shows calcification) / MRI
aspiration
Mx:
rest, ice, analgesia
NSAIDS
steroids (non-infected)
physio
iv abx (septic bursitis)
rotator cuff tear
Hx: trauma in young patients; degeneration of cuff/ attrition from bony spurs of
acromion in elderly patients
Ex: drop arm test to detect large or complete tear
biceps tendonitis
Hx:
anterior shoulder pain, aching
exagerated by heavy lifting, relieved by rest
acute (if chronic --> degeneration)
caused by overuse (no Hx of injury, if yes --> tendon rupture)
Examinations:
Speed's test
Hawkin-Kennedy's test for rotator cuff pathology
Ix: USS
Mx:
rest, ice, analgesia
NSAIDS
steroids
risk of biceps tendon rupture in long-term steroid injection use and in
patients >40yo
discomfort when lifting/pulling (smthg has gone)
ball appears in muscle on elbow flexion
repair is rarely indicated as fx intact
physio: TENS and gentle stretching exercise
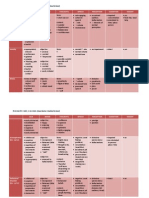
ORTHOPAEDICS: DDx JOINT PAIN | S.M.CHOK (Manchester Medical School)
Glenohumeral Disorders
Acromioclavicular Disorders
adhesive capsulitis (frozen shoulder)
AC joint disruption (caused by trauma)
Hx:
aged 40-65, F>M
sudden onset, spontaneous
inability to sleep on affected side (pain worse at night)
restriction of activities of daily living
PMHx: diabetes, prolonged immobilisation, thyroid disease
Examinations:
generalised deep shoulder joint pain
associated with stiffness
tender to palpation
restriction of active and passive movements (especially external rotation)
Investigations:
diagnosis is clinical
X-ray is commonly normal, performed only if presentation is atypical
Management
1st line: analgesia (paracetamol)
2nd line: NSAIDS
TENS may also be helpful
physio: encourage early activity
surgery: arthroscopic capsular release of adhesion (if conservative Tx fails)
osteoarthritis
aged >60
not as common as hip or knee OA
Hx:
generalised deep shoulder joint pain
restriction of activities, active and passive movements
Mx: joint replacement (good success rate)
Hx:
aged 20s, M>F
collision in high-impact contact sports: fall on to the tip of shoulder with arm in
adduction / direct blow to acromion with humerus adducted
Rockwood Classification (Type I-Type VI)
Examinations:
tender AC joint
visible/palpable 'step' (clavicular separation)
check brachial/radial pulses (axillary/subclavian vessels), brachial plexus,
muscular avulsion (deltoid and trapzius), possible pneumothorax
Ix: X-rays
Mx:
Type I, II, III: conservative (ice, analgesia, sling, NSAIDS, physio)
Type IV, V, VI: open reduction and internalfixation
osteoarthritis and distal clavicular osteolysis
Hx:
after injury, repetitive overuse, idiopathic, intensive sports
PMHx: RA, hyperparathyroidism, myeloma, SLE, infections
Examinations:
diffuse lateral shoulder pain/ localised AC joint pain/ ache in deltoid
worse at night, active and passive movements
cross-adduction worsens pain
ROM is rare
Mx:
activity modification, physio, NSAIDS, analgesia
intra-articular steroids injections
distal clavicular resection if severe cases (open/arthroscopically)
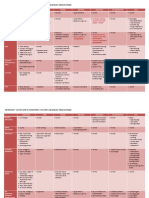
ORTHOPAEDICS: DDx JOINT PAIN | S.M.CHOK (Manchester Medical School)
Shoulder Instability (Dislocation)
usually anterior (caused by fall)
young pt: abduction, extension, posteriorly directed force
elderly pt: outstretched hand
PC: pt holds arm at side of body in external rotation
Ex: anterior bulge, humeral head is palpable
complications:
brachial plexus (axillary/radial nerve etc) damage
damage to rotator cuff muscle
axillary artery damage
associated fracture (humeral head, greater tuberosity, clavicle)
recurrent shoulder dislocation
posterior (epileptic fit)
arm adducted and internally rotated, inability to supine
posterior bulge, humeral head palpable below acromion
nerve and vascular injury not common
Ix: X-rays (AP view and axillary/transscapular 'Y' view)
anterior dislocation:
AP view - head under coracoid process, lateral view - head anterior to glenoid,
transscapular view - head anterior to 'Y'
posterior dislocation:
AP view - normal head of humerus, lateral view - head posterior to glenoid,
transscapular view - head posterior to junction 'Y'
Mx:
first aid:
shoulder and arm splinted in abducted position, elbow flexed 90
reduction methods
surgical repair
stabilisation procedures for recurrent dislocation
EXTRINSIC SHOULDER PAIN
malignancy: apical lung cancer, metastases
referred pain: neck pain, MI, diaphragmatic pain (phrenic nerve)
gallbladder disease / subphrenic abscess
polymyalgia rheumatica (PMR)
Hx:
>50yo, onset >2/52
bilateral shoulder pain, morning stiffness >45min
systemic symptoms
Examinations:
pain on active and passive movement
oedema of hands, wrists, ankles, feet
carpal tunnel syndrome
Ix:
CRP, ESR
USS shows characteristic pathology
Mx:
consider GCA in all PMR pts
glucocorticoids
physio
Red Flag Symptoms/Signs
Hx of malignancy, weight loss, deformity, mass/swelling, abdo discomfort
overlying skin erythema (tumour/infection)
associated systemic illness (polymyalgia rheumatica/GCA)
Hx trauma/convulsion/electric shock (unreduced dislocation)
change in shoulder contour with loss of rotation (dislocation)
presence of significant sensory or motor deficit (neurological lesion)
+ve drop arm test (acute rotator cuff tear)
ORTHOPAEDICS: DDx JOINT PAIN | S.M.CHOK (Manchester Medical School)
ELBOW FRACTURES
Mechanism of Injury in Elbow Fractures
Radial Head and Neck
Fall on to an outstretched hand
Olecranon
Elderly: indirect trauma by pull of triceps and
brachioradialis
Children: direct blow to elbow
Coronoid Process
Fall on to an extended elbow as for elbow dislocation
Distal Humerus
Fall on to an extended outstretched hand
Intercondylar
Direct or indirect blow to elbow
Condylar
Direct blow to a flexed elbow
Capitellum
Fall on to an outstretched hand, direct trauma
Elbow Dislocation
Fall on to an extended elbow
Common in sport in young people
ELBOW PAIN
Tennis Elbow (Lateral Epicondylitis)
inflammation of extensor forearm muscle origin caused by repetitive stress
unilateral lateral apicondyle humerus and upper forearm pain, gradual onset
worse on active and resisted movements of extensor muscles
- wrist and finger flexion with hand pronated
- pain elicited when wrist extended to resist extension of middle finger
1st line: rest, ice, analgesia (NSAIDS), physiotherapy
local steroid injection can be applied
surgery if pt does not respond to conservative Tx
self-limiting: 6/12-2yrs, most recover within 1yr
Golfer's Elbow (Medial Epicondylitis)
inflammation of flexor forearm muscles, caused by repetitive stress
gradual onset pain and tenderness over medial epicondyle, radiating to forearm
exacerbated by wrist flexion and pronation, grasping objects and shaking hands
- pronate and flex wrist and forearm
- pain on medial aspect of elbow
associated ulnar neuropathy: sensation, tingling 4th/5th fingers
- ulnar nerve runs behind epicondyle
- brachial artery runs anteromedially
conservative Mx, self-limiting condition (steroids may help)
Olecranon Bursitis (Student's Elbow)
focal swelling overlying posterior tip of elbow, may or may not be painful
exacerbated by pressure (leaning on table)
- look out for septic (skin changes) and gouty bursitis (presence of tophi)
Examinations:
- clearly demarcated swelling, may be tender to touch, red, warm
- normal ROM but may be limited at the end of flexion due to pain
- unusual restriction of movements with Hx trauma --> olecranon fracture
- skin inspection: contusion/abrasion --> injury
Ix:
- uric acid level: exclude gout or pseudogout
- ESR, CRP, WBC: infection, septic bursitis
- X-rays to exclude fracture
- aspiration: diagnostic and to relieve symptoms
Mx:
- RICE method: Rest, Ice, Compression, Elevation
- abx if infected (staphy.aureus)
- steroids injection if traumatic bursitis
- surgery: aspiration or bursectomy if indicated
can cause septicaemia and osteomyelitis
ORTHOPAEDICS: DDx JOINT PAIN | S.M.CHOK (Manchester Medical School)
WRIST and HANDS
Carpal Tunnel Syndrome
median nerve damage
caused by increased pressure in carpal tunnel compartment
- superior border: flexor retinaculum ligament (aka transverse carpal ligament)
- inferior border: all the carpal bones
risk factors:
- genetics
- flexion/extension injuries to wrist
- conditions in the compartment: aneurysm, neurofibroma, lipoma, ganglion, gouty
tophi, xanthoma, haemangioma
- PMHx: DM, thyroid myxoedema, menopause, acromegaly, renal dialysis,
amyloidosis, inflammatory arthritides
- other: pregnancy, lactation, lack of aerobic exercise, use of walking aids
Presentations:
- tingling, numbness, pain (median nerve distribution)
- worse at night, causes wakening
- +ve Phalen's test, +ve Tinel's test, +ve carpal tunnel compression test
- associated muscle wasting of thenar eminence, weakness in hand grip
- significant sensory loss and skin changes (dry, scaly, reddened, atrophic)
Ix:
- gold standard: electroneurography (ENG)
- EMG, USS, MRI can be done as confirmatory tests
Mx:
- no Tx needed. symptoms resolve within 6/12
- minimise activities that exacerbate symptoms
- NSAIDS may be beneficial (no evidence)
- local steroid injections (diagnostic and therapeutic purposes)
- surgery: release nerve by cutting flexor retinaculum (transverse carpal)
- physio
WRIST and HANDS
Cubital Tunnel Syndrome (aka Ulnar Neuritis)
ulnar nerve damage
- most damage occurs at elbow where it passes through cubital tunnel (between
medial epicondyle and olecranon and tendinous arch)
- pressure in Guyon's canal (wrist) from feep ganglion, tumour or laceration
- compression of deep motor branch against pisiform and hamate (prolonged
pressure over outer palm)
aetiology:
- bone/joint: constricting fascial bands, cubitus valgus, bony spurs, OA/RA, medial
epicondylitis, tumours, ganglia, elbow fractures, dislocation
- nerve: subluxation of ulnar nerve, direct compression
- repetitive elbow flexion/extension
Presentation (ulnar nerve palsy)
- wasting, weakness of hand muscles
- clawing or abduction of ring and little fingers (hyperextension at MCP joints and
flexion of IP joints)
- numbness, tingling along little finger
- weakness of grip and pinch strength, loss of fine dexterity
- pain and tenderness at cubital tunnel
- exclude mass lesions at cubital tunnel region
- +ve Tinel's sign over cubital tunnel, +ve elbow flexion test, +ve Froment's sign
Ix
- USS of cubital tunnel
- MRI for ulnar nerve lesions at elbow
Mx
- physio
- splinting
- NSAIDS
- surgical transposition of nerve and surgical decompression
ORTHOPAEDICS: DDx JOINT PAIN | S.M.CHOK (Manchester Medical School)
HIP FRACTURE
Intracapsular Fractures
young pt: high-energy impact
elderly pt: osteoporosis, osteomalacia, falls
Presentations:
- sudden inability to bear weight
- affected leg: shortened, adducted, externally rotated
- pain over the hip may be particularly aggravated by rotation of leg
Ix:
- X-rays: AP and lateral views (broken Shanton's line)
- Garden's classification
o Garden I: trabeculae angulated, inferior cortex intact, no displacement
o Garden II: trabeculae in line, fracture line is visible from superior to inferior
cortex
o Garden III: obvious complete fracture line, slight displacement, rotation of
femoral head
o Garden IV: gross, often complete, displacement of femoral head
Mx:
- analgesia morphine iv 0.1mg/kg (NSAIDS not recommended) + antiemetic
- surgery ASAP
o undisplaced: internal fixation (dynamic hip screw)
o displaced: total hip replacement (young people and old people who are fit and
mobile); hemiarthroplasty (if not fit and mobile)
Complications
- avascular necrosis
- malunion/ nonunion
- haemorrhage (crystalloid to resuscitate)
- infection
- post-op: early mobilisation
o to prevent DVT, PE, stroke, MI, pressure ulcers
Extracapsular/Intratrochanteric Fractures
treated surgically unless contra-indicated:
- with internal fixation, arthroplasty if internal fixation fails
- extramedullary implants eg dynamic hip screws DHS (aka sliding hip screws)
Femoral Shaft Fracture (including proximal Subtrochanteric Fracture)
affected leg: shortened, externally rotated and abducted at hip
Mx:
- ABC resuscitate
- analgesia, femoral nerve block
- intramedullary nailing
- early mobilisation, regular physio to prevent DVT, PE
Complications: fat embolism, infection, shortening, angulation, nonunion
Supracondylar Fracture
distal 1/3 of femur, result of violent direct injury
often comminuted, intra-articular with associated damage to knee joint
undisplaced: conservative skeletal traction with knee in 30 flexion
displaced: internal fixation
Posterior Hip Dislocation
affected leg: flexed, internally rotated, adduction, shortened
resuscitate, analgesia
Allis' technique for reduction under GA (X-ray to recheck after reduction)
Complications: sciatica nerve injury, vascular injury, possible avascular necrosis
Internal fixation
shorter hospital stays
enables patients to return to function earlier (improve rehab)
reduces the incidence of nonunion (improper healing) and malunion (healing in
improper position) of broken bones.
ORTHOPAEDICS: DDx JOINT PAIN | S.M.CHOK (Manchester Medical School)
KNEE PAIN/LOWER LEG
Patella Dislocation
typically laterally, caused by twisting or direct blow, with knee slightly flexed
knee pain, large effusion, knee held in flexion with lateral displacement of patella,
popping sensation as patella slips sideways out
Entonox reduction, analgesia, immobilise in cylinder cast (3-6/52)
X-ray after reduction (not required prior to reduction)
RECURRENT DISLOCATION
- reduction: plaster backslab and physio for quadriceps
- surgery may be required if conservative fails
Patella Fracture
fall onto flexed knee, or sudden contraction of quadriceps muscle
Types: stable? displaced? comminuted? open?
Presentations: pain, swelling, crepitus, difficulty extending knee
Managements:
- vertical: analgesia, immobilise in non-weight-bearing cylinder cast, crutches
- transverse: analgeisa, immobolise, likely to require internal fixation
Knee Ligament Injuries
(typical injury triad: ACL + MCL + medial meniscus)
anterior cruciate
- twisting injury when lands on the leg (flexed foot)
- conservative: analgesia, PRICE method to control effusion, maintain ROM
- sugical: graft to replace ACL
posterior cruciate
- hyperreflexion is the most common mechanism
- often asymptomatic in first 2-3/52, posterior drawer +ve after 2-3/52
- conservative: analgesia, effusion, maintain ROM, PRICE method, physio
- surgery: ligament reconstruction/autograft (young pt or with knee instability)
medial collateral
- injured by blow to lateral aspect of knee whilst foot is fixed
- conservative Mx, PRICE methods, non-weight-bearing crutches
- surgery is rarely needed
lateral collateral
- injured by blow to medial aspect of knee whilst foot fixed
- mainly surgical: Achilles allograt reconstruction
- conservative Mx with crutches and hinged bracing are helpful
- watch out for common peroneal nerve injury
meniscal tears
- twisting to a flexed knee (medial); adduction+internal rotation (lateral)
- acute: popping, catching, locking or buckling along with joint line pain
- Mx: conservative if possible, PRICE method
- arthroscopy is needed for locked knee, cysts, or persisting symptoms
o options include repair or partial menisectomy
Prepatellar Bursitis (aka Housemaid's Knee)
causes: acute trauma, recurrent minor injury, infection (staphy aureus), co-existing
inflammatory diseases, crystal-depositing condition
presentations: pain, swelling, redness, warmth, ROM eg difficulty kneeling/walking,
systemic unwell (indicate septic bursitis)
aspiration: WBC, protein, lactate, glucose; culture gram -ve bacteria (septic),
monosodium urate crystal (gout), calcium pyrophosphate crystals (pseudogout)
imaging not usually required
Non-septic bursitis:
- conservative: PRICE for non septic bursitis, physio referral
- medical: corticosteroids (exclude infection prior to injection), NSAIDS
- surgical: arthroscopic bursectomy or open bursectomy
Septic bursitis
- aspiration
- iv abx (cephalosporins, augmentin, flucloxicillin etc whilst awaiting culture
- incision and drainage within 36-48hrs of abx Tx
ORTHOPAEDICS: DDx JOINT PAIN | S.M.CHOK (Manchester Medical School)
PROBS IN THE FOOT
Deformities
Hallux Vagus
big toe deviate laterally (risk of 2 arthritis)
Pes Planus
flat feet, loss of medial longitudinal arch
associated with dysfx of posterior tibialis tendon
Pes Cavus
accentuated longitudinal foot arch.
associated with polio, spina bifida, cerebral palsy, CharcotMarie-Tooth dis, syringomyelia, Friedreich's ataxia, spinal
tumour, muscular dystrophy
Hammer Toes
hyperflexed PIP joint and extended DIP joint
2nd toe most commonly affected
Claw Toes
extended MTP joint, flexed DIP and PIP joints
Mallet Toes
flexed DIP joint in isolation
Achilles Tendon Rupture
Risk factors:
- athletes, injury (forced dorsiflexion of foot), deep laceration over tendon
- aging, recurrent/chronic Achilles tendonitis, long-termsteroids use, systemic
conditions (RA, gout, SLE), quinolone abx use
Presentations:
- acute onset, sharp pain --> dull ache, inability to stand tiptoe, altered gait,
localised swelling, weak/absent plantar flexion
Ix: clinical. USS or MRI if diagnosis is unclear
Mx:
- open surgical Tx for people with high physical activity level
- conservative Tx for people less physically active
- rehab: non-weight bearing, use of brace (orthosis)
Complications: re-rupture and immobility
Other CONDITIONS
Osteomyelitis
infection of bone (staphy aureus, pseudomonas, E.coli, streptococci)
risk factors: trauma, iatrogenic (ortho surgery/device), DM, PAD, chronic joint disease,
alcohol, iv drug use, chronic steroid use, immunosuppression, TB, HIV, sickle cell
presentations:
- long bones: painful, immobile limb, swelling, extreme tenderness associated with
redness and warmth
- vertebral: acute septicaemia, localised oedema, erythema, tenderness, chronic
back pain worse at rest and night, unremitting in nature
Pott's Disease vertebral osteomyelitis resulting fom haematogenous spread of TB
- DM foot ulcers: pain masked by neuropathy
- chronic: previous acute infection, localised bone pain, erythema, swelling, nonhealing ulcers, draining sinus tracts, ROM, chronic fatigue, malaise
Ix: bloods (inflammatory markers), cultures, aspiration, MRI (acute), X-ray (chronic)
Mx:
- abx: fluclox for 6/52 (+fusidic acid +rifampicin for first 2/52) | 12/52 if chronic
- clindamycin (penicillin alergic); vancomycin (MRSA suspected)
- analgesia, surgery to debride bone and close any defects
Osteomalacia
presentations: (gradual onset)
- widespread bone pain and tenderness (esp low back pain and hip pain)
- proximal muscle weakness and lethargy, waddling gait
- other signs: costochondral swelling, spinal curvature, hypocalcaemia, multiple
fractures (often bilateral, symmetrical), dental deformities, hyporeflexia
Vit D deficiency
- LFTS (cirrhosis), kidney fx: (defective 1,25-dihydroxyvitamin D synthesis), anaemia
(GI malabsorption), PTH hormone level
- DHx: anticonvulsants, rifampicin, HAART etc
Das könnte Ihnen auch gefallen
- Renal: AKI+CKDDokument6 SeitenRenal: AKI+CKDSok-Moi ChokNoch keine Bewertungen
- Dermatology: Skin LesionsDokument2 SeitenDermatology: Skin LesionsSok-Moi ChokNoch keine Bewertungen
- Neurology: Seizure and AntiepilepticDokument4 SeitenNeurology: Seizure and AntiepilepticSok-Moi ChokNoch keine Bewertungen
- O&G: Sexually Transmitted InfectionsDokument3 SeitenO&G: Sexually Transmitted InfectionsSok-Moi ChokNoch keine Bewertungen
- Psychiatry: AntidepressantsDokument2 SeitenPsychiatry: AntidepressantsSok-Moi Chok100% (1)
- Psychiatry: DementiaDokument3 SeitenPsychiatry: DementiaSok-Moi Chok100% (2)
- Psychiatry: Mental State ExaminationDokument3 SeitenPsychiatry: Mental State ExaminationSok-Moi Chok100% (3)
- Rheumatology: Differential Diagnoses of ArthritisDokument3 SeitenRheumatology: Differential Diagnoses of ArthritisSok-Moi Chok100% (1)
- Examination: Neuro Lower LimbDokument3 SeitenExamination: Neuro Lower LimbSok-Moi ChokNoch keine Bewertungen
- Examination: Neuro Upper LimbDokument2 SeitenExamination: Neuro Upper LimbSok-Moi ChokNoch keine Bewertungen
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Anti-Inflammatory Nutraceuticals and Chronic Diseases: Subash Chandra Gupta Sahdeo Prasad Bharat B. Aggarwal EditorsDokument479 SeitenAnti-Inflammatory Nutraceuticals and Chronic Diseases: Subash Chandra Gupta Sahdeo Prasad Bharat B. Aggarwal EditorsRora11100% (1)
- Pharmacology McqNEW 2Dokument7 SeitenPharmacology McqNEW 2Ayman Ragab100% (2)
- Exposing and Retracting InstrumentsDokument8 SeitenExposing and Retracting Instrumentsyamie sulongNoch keine Bewertungen
- Pharmacoepidemiology: Origin & EvolutionDokument5 SeitenPharmacoepidemiology: Origin & EvolutiongowthamNoch keine Bewertungen
- Physiology of LactationDokument3 SeitenPhysiology of LactationAswathy Chandran100% (1)
- General Physiology: APEC Exam Study NotesDokument9 SeitenGeneral Physiology: APEC Exam Study NotesKC PalattaoNoch keine Bewertungen
- Exosome-Based Immunotherapy: A Promising Approach For Cancer TreatmentDokument16 SeitenExosome-Based Immunotherapy: A Promising Approach For Cancer Treatment1810 15Marvin LionelNoch keine Bewertungen
- Catheter Ablation For AFDokument12 SeitenCatheter Ablation For AFPeny Ruth Jessica DamanikNoch keine Bewertungen
- Methods of Nutrient DeliveryDokument3 SeitenMethods of Nutrient DeliveryFarmisa MannanNoch keine Bewertungen
- IGCSE Excretion (Updated)Dokument23 SeitenIGCSE Excretion (Updated)buhNoch keine Bewertungen
- Muscular DystrophyDokument64 SeitenMuscular DystrophysridharNoch keine Bewertungen
- Water Birth PPDokument5 SeitenWater Birth PPAzi SamiNoch keine Bewertungen
- PBL 4 - Acyanotic Heart DiseaseDokument27 SeitenPBL 4 - Acyanotic Heart DiseaseNadiah Abdul HalimNoch keine Bewertungen
- Neonatology Thesis TopicsDokument7 SeitenNeonatology Thesis Topicspwqlnolkd100% (1)
- PBLDokument6 SeitenPBLzuhaldarwisNoch keine Bewertungen
- 4HB0 01 Que 20180110 PDFDokument28 Seiten4HB0 01 Que 20180110 PDFCrustNoch keine Bewertungen
- Qso-20-14-Nh - Revised 3-13-2020 PDFDokument6 SeitenQso-20-14-Nh - Revised 3-13-2020 PDFAdrian RuxandaNoch keine Bewertungen
- Effectiveness of Psychotherapy On Suicidal Risk - A Systematic Review of Observational Studies (MENDEZ, Et Al, 2019)Dokument10 SeitenEffectiveness of Psychotherapy On Suicidal Risk - A Systematic Review of Observational Studies (MENDEZ, Et Al, 2019)JAVIERA CONSTANZA MUÑOZ VERGARANoch keine Bewertungen
- Hayya Moph QLMDokument4 SeitenHayya Moph QLMrrthamadNoch keine Bewertungen
- Cystitis & UrethritisDokument13 SeitenCystitis & UrethritisfemmyNoch keine Bewertungen
- GC-#1580121-V1-Naphcare #70624-23 Inmate Health Care Services AgreementDokument110 SeitenGC-#1580121-V1-Naphcare #70624-23 Inmate Health Care Services AgreementActionNewsJaxNoch keine Bewertungen
- PWAT (Panographic Wound Assesment Tool) RevisedDokument4 SeitenPWAT (Panographic Wound Assesment Tool) RevisedYunie ArmyatiNoch keine Bewertungen
- TS Nicaragua Health System RPTDokument74 SeitenTS Nicaragua Health System RPTAlcajNoch keine Bewertungen
- Trelegy and Device InformationDokument40 SeitenTrelegy and Device Informationtechang1Noch keine Bewertungen
- Congenital Anomaly 15-09-2015Dokument116 SeitenCongenital Anomaly 15-09-2015gibranNoch keine Bewertungen
- ImciDokument3 SeitenImciJohn Benzon0% (1)
- Viral ConjunctivitisDokument15 SeitenViral ConjunctivitisMary Cathlane TeroNoch keine Bewertungen
- Occupational Industrial and Environmental Toxicology, 2nd EditionDokument3 SeitenOccupational Industrial and Environmental Toxicology, 2nd EditionTalha AfzalNoch keine Bewertungen
- Dense Breast Tissue and RisksDokument2 SeitenDense Breast Tissue and RisksJulia AndersonNoch keine Bewertungen
- Complete Ophtho VM555 CoursepackDokument189 SeitenComplete Ophtho VM555 Coursepacknandhus2227Noch keine Bewertungen