Beruflich Dokumente
Kultur Dokumente
Guy Cohen, CICM Med 2 Year
Hochgeladen von
Guy Hagai CohenOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Guy Cohen, CICM Med 2 Year
Hochgeladen von
Guy Hagai CohenCopyright:
Verfügbare Formate
Guy Cohen 5729640200
How do cancer cells spread to other parts of the body?
The process that cancer cells undertake in order to spread to other parts of the body is called
metastasis. This process leads to an increased risk of mortality due to cancer. There are six basic steps that a
primary cancer cell must undergo in order to metastasise: local invasion, intravasation, circulation, arrest and
extravasation, proliferation, and angiogenesis.
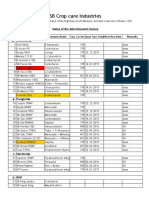
Figure 1: Six basic steps in metastasis (Taken from Integrative Medical Biochemistry, Michael W.
King)
In local invasion, the cancer cells break away and invade the nearby local tissue. In order to do this, it must
be released from the extracellular matrix (ECM) of the primary tumour. There are two main mechanisms that
cancer cells can do this by. One of these mechanisms is a reduction in the production of cell adhesion
molecules; one cell adhesion molecule known as E-cadherins are usually found to be under-expressed in
metastatic cancer. In prostate cancer, malignant cells with reduced E-cadherins are significantly more
virulent than those with normal levels. Because of this correlation, E-cadherins are considered to be tumour
supressors. The other mechanism for local invasion in metastasis is ECM degradation. Matrix
metalloproteinases (MMPs) are one of the important types of enzymes involved with ECM remodeling.
Metastatic cancer cells show a marked increase in MMPs, with high regards to MMP-2 and MMP-9, which
leads to degeneration of the basement membrane and ECM, and allows the cells to intravasate.
Guy Cohen, CICM Med 2nd year
Guy Cohen 5729640200
Intravasation is the invasion of malignant cells into a blood or lymphatic vessel. One of the genes that
promotes intravasation encodes urokinase (uPA), which degrades ECM components and basement
membranes around the primary growth. uPA also activates the aforementioned MMPs. There are two
methods of intravasation: active and passive. In active intravasation, the tumour cells specifically adhere to
the endothelial cells of the capillaries, allowing it to mobilize through the entire body. In passive
intravasation, the tumour cells passively shed, such as when it receives a traumatic force, which increases
the number of tumour cells in the blood stream. Also, tumours growing in restricted spaces can eventually
get squeezed into blood and lymphatic vessels, forcing cells into these vessels and metastasise.
Once the tumour cells have intravasated, they must circulate through the blood stream or lymphatic vessels
to other parts of the body. They are now considered to be circulating tumour cells (CTCs)/ CTCs will be
exposed to various immune cells, such as macrophages, NK cells and T cells. They must be able to survive
exposure to the immune cells. Some of the surveillance cells release chemokines, causing an immune
response to tumor cells. Only 1 in 10000 tumour cells have the capability to colonise successfully. Upon
reaching their target destination, the cells are arrested in the capillaries. One of the simpler ways in which
this happens is by size restriction, as larger clumps of tumour cells can become entrapped within narrow
capillaries. However, another proposed mechanism is that cancerous cells can undergo involves actively
adhering to either endothelial cells.
After cells have been arrested, they can either: extravasate, or proliferate within the vessels. The colonies of
cells that grow within the vessels eventually damage the vessel and release the contents into the surrounding
tissue. In extravasation, the cells invade the cells of the capillaries and move into the tissue that is around
that vessel. Once the cells have extravasated, they must be able to survive and proliferate. They form sites
known as micrometastases, in which they are still too small to be detected clinically. They remain dormant
until they have a sufficient blood supply.
Since cancer cells rapidly utilize glucose by the Warburg effect, they tend to exist in hypoxic state, which
induces angiogenesis. Hypoxia causes elevated levels of HIF-1, which then stimulates VEGF, one major
angiogenetic stimulant. VEGF proteins interact with specific tyrosine kinase receptors on endothelial and
lymphatic cells, resulting in proliferation of endothelial cells around the tumour cells. A blood supply is
needed to obtain the oxygen and nutrients necessary for continued tumor growth.
This is the basic process by which cancer can spread to other parts of the body. Other pathways have been
proposed before, such as perineural pathways, but the method described above is the conventional method
by which primary cancers can metastasise.
Sources:
"Metastasis." Wikipedia. N.p., n.d. Web. https://en.wikipedia.org/wiki/Metastasis
Rodwell, Victor W et al. Harper's Illustrated Biochemistry. Print.
King, Michael W. Integrative Medical Biochemistry Examination And Board Review. Print.
Guy Cohen, CICM Med 2nd year
Das könnte Ihnen auch gefallen
- Metastasis Colonisation of TumorDokument9 SeitenMetastasis Colonisation of TumorRUOITRAUANNoch keine Bewertungen
- Cancer MetastasisDokument29 SeitenCancer Metastasisukhti sarahNoch keine Bewertungen
- Cancer: Cancer Is Defined As An Uncontrolled Proliferation ofDokument12 SeitenCancer: Cancer Is Defined As An Uncontrolled Proliferation ofnikNoch keine Bewertungen
- Angiogenesis & MetastasisDokument11 SeitenAngiogenesis & Metastasisbanwarigupta141Noch keine Bewertungen
- M1.1. Hallmark of Cancer The Capacity For Invasion and MetastasisDokument3 SeitenM1.1. Hallmark of Cancer The Capacity For Invasion and MetastasisClaudia Tocila-MataselNoch keine Bewertungen
- Cellular Invasion & MetastasisDokument19 SeitenCellular Invasion & Metastasisasraf amirullahNoch keine Bewertungen
- Cancer BiologyDokument14 SeitenCancer BiologyADARSH RNoch keine Bewertungen
- Cell Division and Cancer 2 2Dokument25 SeitenCell Division and Cancer 2 2callaxcallaNoch keine Bewertungen
- Neoplasia S. M Jawwad AliDokument25 SeitenNeoplasia S. M Jawwad AliAnt EverafterNoch keine Bewertungen
- Capitol 22 - Cancer PDFDokument24 SeitenCapitol 22 - Cancer PDFsimonaNoch keine Bewertungen
- (Sever R Brugge JS) Signal Transduction in CancerDokument22 Seiten(Sever R Brugge JS) Signal Transduction in CancerJosé Luis García MezaNoch keine Bewertungen
- The CEllular AberrationsDokument17 SeitenThe CEllular AberrationsShara Sampang100% (1)
- Understanding Cancer What Is Cancer and Types of CancerDokument6 SeitenUnderstanding Cancer What Is Cancer and Types of CancerPatrisha KerrNoch keine Bewertungen
- LEO's ASSIGNMENTDokument16 SeitenLEO's ASSIGNMENTTemitope Oluwakemi OlaNoch keine Bewertungen
- JSCR 18 013Dokument7 SeitenJSCR 18 013Mary ChikamaraNoch keine Bewertungen
- Immune Cell Promotion of MetastasisDokument14 SeitenImmune Cell Promotion of MetastasisCristian Gutiérrez VeraNoch keine Bewertungen
- Stem Cells in Solid Tumors Cancer Stem Cell (CSC)Dokument37 SeitenStem Cells in Solid Tumors Cancer Stem Cell (CSC)MuralidharanNoch keine Bewertungen
- Biology For EngineersDokument15 SeitenBiology For Engineerskoushikmondal4507Noch keine Bewertungen
- How Cancer Spreads MetastasisDokument6 SeitenHow Cancer Spreads MetastasisAfia TawiahNoch keine Bewertungen
- What Is Cancer Cellhow Does It DevelopDokument3 SeitenWhat Is Cancer Cellhow Does It DevelopStephanie Nichole Ian CasemNoch keine Bewertungen
- What Is Cancer?Dokument36 SeitenWhat Is Cancer?Minhaj HaiderNoch keine Bewertungen
- Cellular AberrationDokument199 SeitenCellular AberrationCeis Canlas De Castro100% (1)
- Unco Ntrolled Proliferation: Distinguishing Property of Malignant Cells. Without Intervention, Cancerous Tissues Grow inDokument7 SeitenUnco Ntrolled Proliferation: Distinguishing Property of Malignant Cells. Without Intervention, Cancerous Tissues Grow inYukiNoch keine Bewertungen
- Oncolgy UnitDokument12 SeitenOncolgy UnitAtia IftikharNoch keine Bewertungen
- Cancer and Malignant GrowthDokument3 SeitenCancer and Malignant GrowthTapan Kumar PalNoch keine Bewertungen
- NeoplasiaDokument51 SeitenNeoplasiaElstella Eguavoen Ehicheoya100% (1)
- The Anatomy and The Ultimate Cure of CancerVon EverandThe Anatomy and The Ultimate Cure of CancerBewertung: 5 von 5 Sternen5/5 (2)
- Cancers and Abnormal GrowthsDokument37 SeitenCancers and Abnormal GrowthsNABAKOOZA ELIZABETHNoch keine Bewertungen
- Metastasis and InvasionDokument18 SeitenMetastasis and InvasionYona Yohana SNoch keine Bewertungen
- PathologyDokument15 SeitenPathologySaba SaqerNoch keine Bewertungen
- Rishika Vijayvargiya Class XII ADokument21 SeitenRishika Vijayvargiya Class XII ARajat PorwalNoch keine Bewertungen
- CancerDokument231 SeitenCancerJoshua EsparteroNoch keine Bewertungen
- Ecancermedicalscience 2016 Article 701.esDokument35 SeitenEcancermedicalscience 2016 Article 701.esgoya7941Noch keine Bewertungen
- Articles Bu Ke 1Dokument3 SeitenArticles Bu Ke 1dina aribahNoch keine Bewertungen
- Cancer BiologyDokument31 SeitenCancer BiologyGEETA MOHAN100% (1)
- L11, Pathophysiology ManualDokument11 SeitenL11, Pathophysiology Manualph.mt.pharmaNoch keine Bewertungen
- Module 2 Proliferative Growth Patterns Etiology Role of The Immune SystemDokument69 SeitenModule 2 Proliferative Growth Patterns Etiology Role of The Immune SystemAlessandra MercadoNoch keine Bewertungen
- CancerDokument18 SeitenCancerIftikhar AhmedNoch keine Bewertungen
- Hallmarks PresentationDokument10 SeitenHallmarks PresentationmanasNoch keine Bewertungen
- Cellular Aberration 1Dokument9 SeitenCellular Aberration 1pauchanmnlNoch keine Bewertungen
- It Is Characterized by Four Key Features (Latin Terms in Brackets)Dokument11 SeitenIt Is Characterized by Four Key Features (Latin Terms in Brackets)نيوار سنديNoch keine Bewertungen
- It Is Characterized by Four Key Features (Latin Terms in Brackets)Dokument11 SeitenIt Is Characterized by Four Key Features (Latin Terms in Brackets)نيوار سنديNoch keine Bewertungen
- Neoplasia 2015Dokument174 SeitenNeoplasia 2015sukainaNoch keine Bewertungen
- Cancer Karp 16Dokument5 SeitenCancer Karp 16Claudia Perez MestreNoch keine Bewertungen
- Notes On Cancer (Class XII)Dokument2 SeitenNotes On Cancer (Class XII)Aryan JaiswalNoch keine Bewertungen
- Anaphy (Lab Activity)Dokument3 SeitenAnaphy (Lab Activity)Mvl KakashiNoch keine Bewertungen
- GatauDokument3 SeitenGatauameliaNoch keine Bewertungen
- Is Module 8Dokument26 SeitenIs Module 8gladyskheyagamNoch keine Bewertungen
- Molecular Cell BiologyDokument36 SeitenMolecular Cell BiologyEda BasarirNoch keine Bewertungen
- Frontiers in Bioscience E4, 2502-2514, June 1, 2012Dokument13 SeitenFrontiers in Bioscience E4, 2502-2514, June 1, 2012ginocolaciccoNoch keine Bewertungen
- WALEEDDokument3 SeitenWALEEDHashim OmarNoch keine Bewertungen
- Chapter 6 NeoplasiaDokument24 SeitenChapter 6 Neoplasiahenna patelNoch keine Bewertungen
- CancerDokument19 SeitenCancerparabharshita2709Noch keine Bewertungen
- What Is Cancer - National Cancer Institute PDFDokument7 SeitenWhat Is Cancer - National Cancer Institute PDFAlexis CastilloNoch keine Bewertungen
- Oncology NursingDokument7 SeitenOncology NursingDiana Laura Lei100% (1)
- Jurnal NeoplasmaDokument10 SeitenJurnal NeoplasmaFadhilah Asyifa DewantiNoch keine Bewertungen
- Cell Renewal and Cell DeathDokument7 SeitenCell Renewal and Cell Deathmem734094Noch keine Bewertungen
- Blood Vessels Vasculogenesis Endothelial Mesoderm Embryo: Angiogenesis Is The Physiological Process Through Which NewDokument23 SeitenBlood Vessels Vasculogenesis Endothelial Mesoderm Embryo: Angiogenesis Is The Physiological Process Through Which NewDaniel SutantoNoch keine Bewertungen
- Angio GenesisDokument12 SeitenAngio GenesisVasu Reddy ChallaNoch keine Bewertungen
- NCP - DMDokument4 SeitenNCP - DMMonica Garcia88% (8)
- Sidomuncul20190313064235169 1 PDFDokument298 SeitenSidomuncul20190313064235169 1 PDFDian AnnisaNoch keine Bewertungen
- Coc 1 ExamDokument7 SeitenCoc 1 ExamJelo BioNoch keine Bewertungen
- Java Edition Data Values - Official Minecraft WikiDokument140 SeitenJava Edition Data Values - Official Minecraft WikiCristian Rene SuárezNoch keine Bewertungen
- Technology 6 B Matrixed Approach ToDokument12 SeitenTechnology 6 B Matrixed Approach ToNevin SunnyNoch keine Bewertungen
- (QII-L2) Decorate and Present Pastry ProductsDokument30 Seiten(QII-L2) Decorate and Present Pastry ProductsLD 07100% (1)
- Purposive Communication Preliminary DiscussionDokument2 SeitenPurposive Communication Preliminary DiscussionJohn Mark100% (1)
- Net Pert: Cable QualifierDokument4 SeitenNet Pert: Cable QualifierAndrés Felipe Fandiño MNoch keine Bewertungen
- AWS Compete CustomerDokument33 SeitenAWS Compete CustomerSergeyNoch keine Bewertungen
- Review and Basic Principles of PreservationDokument43 SeitenReview and Basic Principles of PreservationKarl Marlou Bantaculo100% (1)
- Technical DescriptionDokument2 SeitenTechnical Descriptioncocis_alexandru04995Noch keine Bewertungen
- Lugam Annex Elementary School Second Quarter Second Periodical Test in EPP 6 H.EDokument4 SeitenLugam Annex Elementary School Second Quarter Second Periodical Test in EPP 6 H.Ejess amielNoch keine Bewertungen
- Matrices and Vectors. - . in A Nutshell: AT Patera, M Yano October 9, 2014Dokument19 SeitenMatrices and Vectors. - . in A Nutshell: AT Patera, M Yano October 9, 2014navigareeNoch keine Bewertungen
- Jordan CVDokument2 SeitenJordan CVJordan Ryan SomnerNoch keine Bewertungen
- Reviewer in EntrepreneurshipDokument6 SeitenReviewer in EntrepreneurshipRachelle Anne SaldeNoch keine Bewertungen
- Sweat Equity SharesDokument8 SeitenSweat Equity SharesPratik RankaNoch keine Bewertungen
- Assesment Test in English 9Dokument3 SeitenAssesment Test in English 9Chazz SatoNoch keine Bewertungen
- Ep Docx Sca SMSC - V2Dokument45 SeitenEp Docx Sca SMSC - V290007Noch keine Bewertungen
- Introduction of ProtozoaDokument31 SeitenIntroduction of ProtozoaEINSTEIN2D100% (2)
- IFSSO Newsletter Jul-Sep 2010Dokument2 SeitenIFSSO Newsletter Jul-Sep 2010rjotaduranNoch keine Bewertungen
- Phenomenology of The SelfDokument5 SeitenPhenomenology of The SelfGuilherme CastelucciNoch keine Bewertungen
- MMB & DFT 2012 Workshop ProceedingsDokument44 SeitenMMB & DFT 2012 Workshop ProceedingsFelipe ToroNoch keine Bewertungen
- Measures For FloodsDokument4 SeitenMeasures For FloodsMutsitsikoNoch keine Bewertungen
- HC+ Shoring System ScaffoldDokument31 SeitenHC+ Shoring System ScaffoldShafiqNoch keine Bewertungen
- Limestone Standards PDFDokument2 SeitenLimestone Standards PDFJacqueline BerueteNoch keine Bewertungen
- Products ListDokument11 SeitenProducts ListPorag AhmedNoch keine Bewertungen
- PC Engines APU2 Series System BoardDokument11 SeitenPC Engines APU2 Series System Boardpdy2Noch keine Bewertungen
- ISSA2013Ed CabinStores v100 Часть10Dokument2 SeitenISSA2013Ed CabinStores v100 Часть10AlexanderNoch keine Bewertungen
- Adsorption ExperimentDokument5 SeitenAdsorption ExperimentNauman KhalidNoch keine Bewertungen
- Schermer 1984Dokument25 SeitenSchermer 1984Pedro VeraNoch keine Bewertungen