Beruflich Dokumente
Kultur Dokumente
Vitamine D and BPPV
Hochgeladen von
yehezkieldwardCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Vitamine D and BPPV
Hochgeladen von
yehezkieldwardCopyright:
Verfügbare Formate
NIH Public Access
Author Manuscript
Med Hypotheses. Author manuscript; available in PMC 2014 October 14.
NIH-PA Author Manuscript
Published in final edited form as:
Med Hypotheses. 2013 February ; 80(2): 201204. doi:10.1016/j.mehy.2012.11.029.
Vitamin D deficiency and benign paroxysmal positioning vertigo
Bela Bki*, Michael Ecker**, Heinz Jnger*, and Yunxia Wang Lundberg
*Department
**Department
of Otolaryngology, County Hospital Krems, Austria
of Laboratory Medicine, County Hospital Krems, Austria
Vestibular
Neurogenetics Laboratory, Boys Town National Research Hospital, Omaha,
Nebraska, USA
Abstract
NIH-PA Author Manuscript
Benign paroxysmal positional vertigo is a common cause of disabling vertigo with a high rate of
recurrence. Although connections between vitamin D deficiency and osteoporosis, as well as
between osteoporosis and benign paroxysmal positional vertigo have been suggested respectively
in the literature, we are not aware of any publication linking vitamin D and benign paroxysmal
positional vertigo. As a hypothesis, we suggest that there is a relation between insufficient vitamin
D level and benign paroxysmal positional vertigo. In order to test this hypothesis, in a small
retrospective pilot study, 25-hydroxyvitamin D levels in serum of patients with benign paroxysmal
positional vertigo and frequency of recurrence after correction of serum level were assessed
retrospectively. Patients with idiopathic positional vertigo had a low average serum level of 25hydroxyvitamin D (23 ng/mL) similar to that of the general Austrian population, which has a high
prevalence of hypovitaminosis D. In 4 cases with chronically recurrent severe vertigo episodes,
average levels of serum 25-hydroxyvitamin D were even significantly lower than in the other
vertigo patients, who had their first episode. Vertigo attacks did not recur after supplementation
with vitamin D.
NIH-PA Author Manuscript
We raise the possibility that patients with benign paroxysmal positional vertigo who have low
vitamin D levels may benefit from supplementation and suggest further epidemiological
investigations to determine the effect of correcting vitamin D deficiency on the recurrence of
vertigo. Given the many known benefits of vitamin D, the authors recommend the measurement of
vitamin D in patients with benign paroxysmal positional vertigo and supplementation if necessary.
Keywords
Vitamin D; Deficiency; paroxysmal positional vertigo
2012 Elsevier Ltd. All rights reserved.
Corresponding author: Bela Bki, HNO-Sekretariat, Landesklinikum Krems, Mitterweg 10, A-3500 Krems, Phone: +43
27328042242, Fax: +43 27328045243, bukibela@hotmail.com.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our
customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of
the resulting proof before it is published in its final citable form. Please note that during the production process errors may be
discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declaration of interest: The authors report no declarations of interest
Bki et al.
Page 2
Introduction
NIH-PA Author Manuscript
BPPV is a common disorder
Benign paroxysmal positional vertigo (BPPV) is the most common neuro-otological
disorder [1]. Today it is accepted, that it is caused by dislodged otoconia, which fall from the
utricular macula and float into the semicricular canals thereby making them sensitive to
gravity [2]. Otoconia crystals have distinct central cores and peripheral zones (for review see
[3]). The core is predominantly organic with a lower level of Ca2+, and the periphery is
largely inorganic with a higher level of Ca2+ [4]. The core, periphery and external surface of
the crystals all have inter-connecting fibrous material with varied diameters and
organization. The main inorganic mineral component is almost exclusively a polymorph of
calcium carbonate (CaCO3). The organic component is usually a predominant glycoprotein.
Otoconia crystals are partially embedded in a membranous/fibrous matrix and are tethered
by proteinaceous filaments to the kinocilium of the underlying hair cells. The formation of
otoconia surrounded by low-calcium endolymph is a tigthly controlled active process [3].
NIH-PA Author Manuscript
It has been shown that elderly people may suffer from unrecognized, chronic BPPV. In 2000
a widely cited cross-sectional study was published, which determined the prevalence of
unrecognized benign paroxysmal positional vertigo (BPPV) in an inner-city geriatric
population [5]. Dizziness was found in 61% of patients. Nine percent were found to have
unrecognized BPPV. Patients with unrecognized BPPV were more likely to have reduced
activities of daily living scores, to have sustained a fall in the previous 3 months, and to have
depression. These data indicated that unrecognized BPPV is common within the elderly
population and has associated morbidity. Apart from classical BPPV with nystagmus
chronic subjective BPPV without nystagmus may also be common, recently a mechanism
for that has been suggested [6].
Osteoporosis and BPPV
NIH-PA Author Manuscript
Back in 2003 Vibert et al suggested a connection between BPPV, osteoporosis and
osteopenia [7]. Since then another independent group also showed that bone metabolism has
a connection to BPPV [8]. Recent studies in Dr. Lundbergs laboratory show common
features between bone and otoconia biomineralization. For example, the organization of the
matrix is similar between the two tissues, and most of the protein constituents are present in
both tissues. Similar to that in bone and teeth, biomineralization in otoconia involves tight
regulation of the formation of an organic matrix at specific sites and the deposition of
mineral crystallites in an ordered manner [911, Lundberg, unpublished data]. In animal
experiments it has been shown that this process is dysfunctional in osteoporosis [12]. Even a
beneficial therapeutic effect could be observed between BPPV and osteoporosis when
treated with bisphosphonates in women [13].
Osteoporosis and Vitamin D
The effect of vitamin D on osteoporosis has been established in the literature (for review see
[14]). Calcium and vitamin D play important roles in improving bone mineral density and
reducing the risk of fracture [15]. It is also known that vitamin D supplementation reduces
Med Hypotheses. Author manuscript; available in PMC 2014 October 14.
Bki et al.
Page 3
the risks of falls and fractures in elderly people [16]. According to these authors this may be
due to the effect of vitamin D by improving neuromuscular function.
NIH-PA Author Manuscript
The hypothesis Vitamin D and BPPV
Although connections between vitamin D and improved osteoporosis, as well as between
osteoporosis and BPPV have been suggested respectively in the literature, we are not aware
of any publication linking vitamin D and BPPV. As a hypothesis we suggest, that there is a
relation between vitamin D and BPPV. Therefore, we recommend to measure 25(OH)D in
BPPV patients and to supplement it, if there is a deficiency.
If there is a connection between BPPV and vitamind D, it may also be possible that the
beneficial effect of Vitamin D on reduction of falls in BPPV is perhaps aided by decreasing
recurrence of chronic BPPV.
Pilot study
NIH-PA Author Manuscript
To establish, if in our records any evidence for such a connection can be gathered, we
retrospectively analysed laboratory records to decide if patients with BPPV had low 25hydroxyvitamin D (25(OH)D levels and if so, correcting serum levels showed a beneficial
effect in patients with BPPV.
Patients, methods
We analysed the records of 18 consecutive patients suffering from BPPV who were
examined at the vertigo/dizziness ambulance at Krems General Hospital, Austria between
01st May and 1st August 2011. Inclusion criteria were: 1. Diagnosis of canalolithiasis or
cupulolithiasis either of vertical canals or of the horizontal canal established by typical
positional nystagmus [2]; 2. Availability of the results of follow up examination; 3.
Availability of actual 25(OH)D value in the serum at the first visit or at the follow up
examination; 4. Negative radiological results (MRI of cerebrum); 5. Negative neurological
status; 6. Successful repositioning maneuver at the first visit; 7. Symmetric hearing
thresholds
NIH-PA Author Manuscript
The group of patients included 11 females and 7 males (average age = 67 years (min: 45;
max: 85 years). After documenting history of complaints the routine neurootological
examination was carried out including positional testing as described elsewhere [6].
25(OH)D was measured by Elecsys Vitamin D3 (cobas), an electrochemiluminescence
immunoassay on a combined chemistry and immunoassay platform standardised against the
liquid chromatography-tandem mass spectrometry reference method.
During a follow up examination the neurootological examination was repeated and in cases
with low serum level of 25(OH)D and no history of nephrolithiasis, supplementation started.
If the level of 25(OH)D was under 20 ng/mL, then the supplementation consisted of daily
8000 IU cholecalciferol for two weeks, and daily 4000 IU cholecalciferol for the next two
weeks, then a weekly dose of 8000 IU was given as recommended in [17]. Shortest follow
up was 8 month. After this time the patients were contacted on the phone and, in an
interview, their eventual complaints were assessed.
Med Hypotheses. Author manuscript; available in PMC 2014 October 14.
Bki et al.
Page 4
Statistics
NIH-PA Author Manuscript
We carried out a nonparametric (no normal distribution) two-tailed Mann Whitney test, to
test significant difference between the two groups.
Results
At the first examination in all cases posterior canalolithiasis could be demonstrated (11 on
the right, 7 on the left side). It was possible to carry out a successful repositioning (Epleymaneuver [18] in every case.
History of complaints
In one case the patient had had vestibular neuritis 3 weeks before the BPPV episode on the
same side as the BPPV (in this case the 25(OH)D level was normal). In 14 cases (Group A)
the patients had their first episode of BPPV, in average since 12 days (min: 4 days, max: 60
days). In four cases (Group B) the patients had been having multiple episodes over several
years. The data of these patients are shown in Table 1.
NIH-PA Author Manuscript
Average 25(OH)D level in all patients (Group A+ Group B) was 23 ng/mL (minimum:11,
25% percentile: 15; median 17; 75% percentile 33; maximum 51). In 10 cases the 25(OH)D
level was under 20 ng/mL (an insufficient 25(OH)D level [19] and clearly under the
recommendation of [17]).
After having examined all BPPV patients we divided the group of all patients into two
groups. Group A: first manifestation, Group 2: recurrent BPPV. In Group A average serum
25(OH)D level was 27 ng/mL (minimum:13, 25% percentile: 16; median 24; 75% percentile
37; maximum 51). In Group B average serum 25(OH)D level was 14 ng/mL (minimum:11,
25% percentile: 12; median 14; 75% percentile 15; maximum 15). The difference between
the two groups was significant (Mann Whitney test; p< 0.02). We show the data distribution
in Fig. 2.
Follow up evaluation
NIH-PA Author Manuscript
At the time of the first follow up examination nystagmus due to BPPV could not be
demonstrated in any cases. Until the time of the telephone interview there was no recurrence
of the BPPV complaints in any of the groups.
Consequences of the hypothesis and discussion
We found that our patients with idiopathic BPPV had low average vitamin D serum levels
(23 ng/mL). This is similar to that of the general Austrian population (in average 20.9
mg/mL [20]), which has a high prevalence of vitamin D hypovitaminosis. We identified 4
patients, who had been having recurrent episodes of BPPV for a longer time before the
examination with a frequency of 46 relapses/year for several years. These patients as a
subgroup had significantly lower average serum level of 25(OH)D than patients in the
subgroup in which with a first episode. After having been supplemented with vitamin D,
BPPV patients have not encountered relapses in the follow up period of at least 8 month.
Med Hypotheses. Author manuscript; available in PMC 2014 October 14.
Bki et al.
Page 5
NIH-PA Author Manuscript
Although some BPPV cases are benign, most cases recur. In a recent study the recurrence
rate of BPPV was 27%, and relapse largely occurred in the first 6 months ([21]). At present,
the generally accepted recurrence rate of BPPV after successful treatment is 40 to 50% at 5
years of average follow up. A subset of individuals appears prone to multiple recurrences
[21, 22]. In our study in 4 cases with chronically recurrent severe BPPV episodes low levels
of serum 25(OH)D could be measured, and, BPPV did not recur after supplementation with
Vitamin D.
These preliminary results show that a hypothesis linking vitamin D and BPPV may be valid.
Although we cannot rule out coincidence at the present, given the multiple benefits of
vitamin D, we recommend supplementation in BPPV cases.
The so-called classical effects of vitamin D are that on bone density, bone quality and
muscle performance. In this context, it is listed among the classical effects that falling of
elderly people was significantly reduced in vitamin D supplemented individuals compared to
those receiving calcium and placebo [23, 24].
NIH-PA Author Manuscript
Theoretically it may even be possible that supplementation with vitamin D brings about a
decrease of falls through decreasing the frequency of unrecognized BPPV. Even if this not
the case, it is easy to see that perhaps a synergistic relationship may be influenced by
correcting abnormally low vitamin D levels. In the literature the possibility of numerous
other, so-called non-classical effects also have been described (cardiovascular, diabetes
mellitus, cancer, multiple sclerosis, allergy, asthma (see Review[19]). These authors also
classified vitamin D status according to measured 25(OH)D concentration: less than 10
ng/mL: deficient; between 1120: insufficient; higher than 20 ng/ml: optimal. Recently an
international panel reached agreement about the need for vitamin D supplementation in
specific groups of patients in these clinical areas and the need for assessing their 25hydroxyvitamin D (25(OH)D) serum levels for optimal clinical care. A target range of at
least 30 to 40 ng/mL was recommended ([17]). The mechanism of the beneficial effect of
vitamin D may involve improvement of pathologic biomineralization of otoconia similar to
that of bone and teeth.
We decided to publish our hypothesis because of the following reasons:
NIH-PA Author Manuscript
According to theoretical considerations the existence of a link between otolithic
disturbances and vitamin D deficiency is highly probable
Given the prevalence of vitamin D deficiency and the simplicity of the
procedure (measurement of vitamin D levels and supplementation if necessary)
the recommended correction should be done anyway
BPPV is so common, that even if the supplementation of vitamin D inhibits
recurrence only in a small percentage of cases, this means a large number of
cases with improvement
We suggest further statistical epidemiological investigations to determine average serum
levels of 25(OH)D in patients with BPPV and the effect of correcting vitamin D deficiency
on the recurrence of BPPV. Even until these results are available, given the other known
Med Hypotheses. Author manuscript; available in PMC 2014 October 14.
Bki et al.
Page 6
benefits of vitamin D, we recommend measurement of 25(OH)D and supplementation if
necessary.
NIH-PA Author Manuscript
Acknowledgments
Source of support
YWL is supported by a grant from the National Institute on Deafness and Other Communication Disorders (R01
DC008603)
References
NIH-PA Author Manuscript
NIH-PA Author Manuscript
1. von Brevern M, Radtke A, Lezius F, et al. Epidemiology of benign paroxysmal positional vertigo: a
population based study. J Neurol Neurosurg Psychiatry. 2007; 78:710715. [PubMed: 17135456]
2. Parnes LS, Agrawal SK, Atlas J. Diagnosis and management of benign paroxysmal positional
vertigo (BPPV). CMAJ. 2003; 169:681693. [PubMed: 14517129]
3. Lundberg YW, Zhao X, Yamoah EN. Assembly of the otoconia complex to the macular sensory
epithelium of the vestibule. Brain Res. 2006; 1091:4757. [PubMed: 16600187]
4. Lins U, Farina M, Kurc M, et al. The otoconia of the guinea pig utricle: internal structure, surface
exposure, and interactions with the filament matrix. J Struct Biol. 2000; 131:6778. [PubMed:
10945971]
5. Oghalai JS, Manolidis S, Barth JL, Stewart MG, Jenkins HA. Unrecognized benign paroxysmal
positional vertigo in elderly patients. Otolaryngol Head Neck Surg. 2000; 122:630634. [PubMed:
10793337]
6. Buki B, Simon L, Garab S, Lundberg YW, Jnger H, Straumann D. Sitting-up vertigo and trunk
retropulsion in patients with benign positional vertigo but without positional nystagmus. J Neurol
Neurosurg Psychiatry. 2011; 82:98104. [PubMed: 20660923]
7. Vibert D, Kompis M, Hausler R. Benign paroxysmal positional vertigo in older women may be
related to osteoporosis and osteopenia. Ann Otol Rhinol Laryngol. 2003; 112:885889. [PubMed:
14587980]
8. Jeong SH, Choi SH, Kim JY, Koo JW, Kim HJ, Kim JS. Osteopenia and osteoporosis in idiopathic
benign positional vertigo. Neurology. 2009; 72:10691076. [PubMed: 19307540]
9. Zhao X, Yang H, Yamoah EN, Lundberg YW. Gene targeting reveals the role of Oc90 as the
essential organizer of the otoconial organic matrix. Dev Biol. 2007; 304:508524. [PubMed:
17300776]
10. Xu Y, Zhang H, Yang H, Zhao X, Lovas S, Lundberg YW. Expression, functional, and structural
analysis of proteins critical for otoconia development. Dev Dyn. 2010; 239:26592673. [PubMed:
20803598]
11. Yang H, Zhao X, Xu Y, Wang L, He Q, Lundberg YW. Matrix recruitment and calcium
sequestration for spatial specific otoconia development. PLoS One. 2011; 6:e20498. [PubMed:
21655225]
12. Vibert D, Sans A, Kompis M, et al. Ultrastructural changes in otoconia of osteoporotic rats. Audiol
Neurootol. 2008; 13:293301. [PubMed: 18391565]
13. Mikulec AA, Kowalczyk KA, Pfitzinger ME, Harris DA, Jackson LE. Negative association
between treated osteoporosis and benign paroxysmal positional vertigo in women. J Laryngol
Otol. 2010; 124:374376. [PubMed: 19930786]
14. Lips P, van Schoor NM. The effect of vitamin D on bone and osteoporosis. Best Pract Res Clin
Endocrinol Metab. 2011; 25:585591. [PubMed: 21872800]
15. Ahmadieh H, Arabi A. Vitamins and bone health: beyond calcium and vitamin D. Nutr Rev. 2011;
69:584598. [PubMed: 21967159]
16. Dhesi JK, Jackson SH, Bearne LM, et al. Vitamin D supplementation improves neuromuscular
function in older people who fall. Age Ageing. 2004; 33:589595. [PubMed: 15501836]
Med Hypotheses. Author manuscript; available in PMC 2014 October 14.
Bki et al.
Page 7
NIH-PA Author Manuscript
17. Souberbielle JC, Body JJ, Lappe JM, et al. Vitamin D and musculoskeletal health, cardiovascular
disease, autoimmunity and cancer: Recommendations for clinical practice. Autoimmun Rev. 2010;
9:709715. [PubMed: 20601202]
18. Epley JM. Canalith repositioning maneuver. Otolaryngol Head Neck Surg. 1994; 111:688690.
[PubMed: 7970818]
19. Thacher TD, Clarke BL. Vitamin D insufficiency. Mayo Clin Proc. 2011; 86:5060. [PubMed:
21193656]
20. Kudlacek S, Schneider B, Peterlik M, et al. Assessment of vitamin D and calcium status in healthy
adult Austrians. Eur J Clin Invest. 2003; 33:323331. [PubMed: 12662163]
21. Perez P, Franco V, Cuesta P, Aldama P, Alvarez MJ, Mndez JC. Recurrence of benign
paroxysmal positional vertigo. Otol Neurotol. 2012; 33:437443. [PubMed: 22388730]
22. Fife TD. Benign paroxysmal positional vertigo. Semin Neurol. 2009; 29:500508. [PubMed:
19834861]
23. Bischoff-Ferrari HA, Dawson-Hughes B, Staehelin HB, et al. Fall prevention with supplemental
and active forms of vitamin D: a meta-analysis of randomised controlled trials. BMJ. 2009;
339:b3692. [PubMed: 19797342]
24. Annweiler C, Montero-Odasso M, Schott AM, Berrut G, Fantino B, Beauchet O. Fall prevention
and vitamin D in the elderly: an overview of the key role of the non-bone effects. J Neuroeng
Rehabil. 2010; 7:5063. [PubMed: 20937091]
NIH-PA Author Manuscript
NIH-PA Author Manuscript
Med Hypotheses. Author manuscript; available in PMC 2014 October 14.
Bki et al.
Page 8
NIH-PA Author Manuscript
NIH-PA Author Manuscript
Figure 1.
Our hypothesis establishes connection between vitamin D and BPPV. The arrows show the
connections established in the literature so far, the question mark designates the hypothetical
connection
NIH-PA Author Manuscript
Med Hypotheses. Author manuscript; available in PMC 2014 October 14.
Bki et al.
Page 9
NIH-PA Author Manuscript
NIH-PA Author Manuscript
Figure 2.
Column statistics of 25(OH)D serum levels in Group A and B (individual values and mean
95% confidence interval are shown)
NIH-PA Author Manuscript
Med Hypotheses. Author manuscript; available in PMC 2014 October 14.
Bki et al.
Page 10
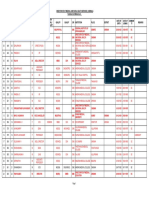
Table 1
NIH-PA Author Manuscript
Data and 25(OH)D levels of four patients with severe recurrent BPPV
Patient
number
Sex
Age
25(OH)D
(ng/mL)
History of complaints (since when)
14
64
11
recurrent episodes since 2 years; sum of episodes 8; each episode for weeks
15
45
16
recurrent episodes since 4 years, sum of episodes : 10; each episode for weeks
16
72
13
episodes 10 years ago, then 5 years ago, since 2 years approx. every second month; sum of episodes 13;
each episode for days
18
53
15
since 2 years every third months; sum of episodes: 5; each episode for weeks
NIH-PA Author Manuscript
NIH-PA Author Manuscript
Med Hypotheses. Author manuscript; available in PMC 2014 October 14.
Das könnte Ihnen auch gefallen
- Otolaryngology - Head and Neck Surgery-2015 - Rhinitis AllergicDokument43 SeitenOtolaryngology - Head and Neck Surgery-2015 - Rhinitis AllergicAlpascaFirdausNoch keine Bewertungen
- Treatment of Allergic Rhinitis: DENISE K. SUR, MD, and STEPHANIE SCANDALE, MD, David Geffen School of MedicineDokument7 SeitenTreatment of Allergic Rhinitis: DENISE K. SUR, MD, and STEPHANIE SCANDALE, MD, David Geffen School of MedicineM Isyhaduul IslamNoch keine Bewertungen
- Acute Otitis Exteena (Clinical Guideline 2014)Dokument25 SeitenAcute Otitis Exteena (Clinical Guideline 2014)friscahalimNoch keine Bewertungen
- CTG HaDokument15 SeitenCTG HaNabila SaribanunNoch keine Bewertungen
- How To Read A CTGDokument12 SeitenHow To Read A CTGyehezkieldward100% (1)
- CKD Treatment AlgorithmDokument1 SeiteCKD Treatment AlgorithmyehezkieldwardNoch keine Bewertungen
- BNP & Nt-Pro BNPDokument7 SeitenBNP & Nt-Pro BNPyehezkieldwardNoch keine Bewertungen
- Research Article: Age-Related Changes in Bone Remodelling and Structure in Men: Histomorphometric StudiesDokument4 SeitenResearch Article: Age-Related Changes in Bone Remodelling and Structure in Men: Histomorphometric StudiesyehezkieldwardNoch keine Bewertungen
- Anemia and Chronic Kidney Disease: What You Need To Know AboutDokument8 SeitenAnemia and Chronic Kidney Disease: What You Need To Know AboutyehezkieldwardNoch keine Bewertungen
- Noel Vs NoaelDokument4 SeitenNoel Vs NoaelyehezkieldwardNoch keine Bewertungen
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- What Is Subinvolution?Dokument5 SeitenWhat Is Subinvolution?Xierl BarreraNoch keine Bewertungen
- MScHandbook Imperial Chemical EnggDokument87 SeitenMScHandbook Imperial Chemical EnggMurugeshNoch keine Bewertungen
- Final ThesisDokument58 SeitenFinal Thesisgnanasegaram vithursanNoch keine Bewertungen
- Citation WorksheetDokument5 SeitenCitation WorksheetZafar Ibn Kader 2013819030Noch keine Bewertungen
- Tmi Lumbar Fusion Rehabilitation ProtocolDokument2 SeitenTmi Lumbar Fusion Rehabilitation ProtocolJackyNoch keine Bewertungen
- Education For AllDokument4 SeitenEducation For AllNamrata SaxenaNoch keine Bewertungen
- Treatment Aspects in Perioperative NursingDokument51 SeitenTreatment Aspects in Perioperative NursingShibin Jacob100% (2)
- Mitchell H. Katz-Evaluating Clinical and Public Health Interventions - A Practical Guide To Study Design and Statistics (2010)Dokument176 SeitenMitchell H. Katz-Evaluating Clinical and Public Health Interventions - A Practical Guide To Study Design and Statistics (2010)Lakshmi SethNoch keine Bewertungen
- Systemic Response To InjuryDokument15 SeitenSystemic Response To InjuryJohnVincentPagaddu100% (1)
- Detection of NoncomplianceDokument12 SeitenDetection of Noncompliancesomayya waliNoch keine Bewertungen
- Effectiveness of Ergonomic Intervention inDokument10 SeitenEffectiveness of Ergonomic Intervention inTania SánchezNoch keine Bewertungen
- Confined Space Entry FaqDokument4 SeitenConfined Space Entry FaqSyed Rameez MohiuddinNoch keine Bewertungen
- Technology Process Fortification Ruchika SachdevaDokument23 SeitenTechnology Process Fortification Ruchika SachdevaHimex EquipmentsNoch keine Bewertungen
- Issues in CPPD Nomenclature and ClassificationDokument8 SeitenIssues in CPPD Nomenclature and ClassificationMonika Diaz KristyanindaNoch keine Bewertungen
- Part-IDokument507 SeitenPart-INaan SivananthamNoch keine Bewertungen
- Phobias - See What Makes Some People AfraidDokument2 SeitenPhobias - See What Makes Some People Afraidbeep777Noch keine Bewertungen
- Bacterial Vaginosis Treatment - UpToDateDokument12 SeitenBacterial Vaginosis Treatment - UpToDateAlex Esteban Espinoza CevallosNoch keine Bewertungen
- Format Nutritional StatusDokument43 SeitenFormat Nutritional StatusDirkie Meteoro Rufin83% (6)
- The Factories Act 1948Dokument96 SeitenThe Factories Act 1948NIKITHAA ASHWINNoch keine Bewertungen
- Cossh Risk Assessment: Carried Out By: Department: Date: Substance Name: CRA NumberDokument2 SeitenCossh Risk Assessment: Carried Out By: Department: Date: Substance Name: CRA NumberNiraNoch keine Bewertungen
- Wendy J. Dahl - Health Benefits of Pulses-Springer International Publishing (2019) PDFDokument160 SeitenWendy J. Dahl - Health Benefits of Pulses-Springer International Publishing (2019) PDFSolomon AssefaNoch keine Bewertungen
- Diabetic Ketoacidosis Case StudyDokument5 SeitenDiabetic Ketoacidosis Case Studyjc_albano29100% (7)
- Q2 Lesson 7Dokument25 SeitenQ2 Lesson 7mint hvryNoch keine Bewertungen
- Beneficence and NonDokument4 SeitenBeneficence and NonRoselle Farolan LopezNoch keine Bewertungen
- Power of Plants 1Dokument14 SeitenPower of Plants 1api-399048965Noch keine Bewertungen
- Student Copy Conti - Intrapartal Week8Dokument25 SeitenStudent Copy Conti - Intrapartal Week8Toyour EternityNoch keine Bewertungen
- AssignmentDokument2 SeitenAssignmentYahya TariqNoch keine Bewertungen
- NegOr Q4 MAPEH7 Module4a v2Dokument12 SeitenNegOr Q4 MAPEH7 Module4a v2fauralaurenceNoch keine Bewertungen
- Interview Paper SW 3010Dokument7 SeitenInterview Paper SW 3010api-319252753Noch keine Bewertungen
- Scheme of Work - Form 4: Week (1 - 3)Dokument7 SeitenScheme of Work - Form 4: Week (1 - 3)honeym694576Noch keine Bewertungen