Beruflich Dokumente
Kultur Dokumente
Pseudohyponatremia Nejm Cps
Hochgeladen von
honeyworksCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Pseudohyponatremia Nejm Cps
Hochgeladen von
honeyworksCopyright:
Verfügbare Formate
The
new england journal
of
medicine
clinical problem-solving
Mind the Gap
Alexander Turchin, M.D., Julian L. Seifter, M.D., and Ellen W. Seely, M.D.
In this Journal feature, information about a real patient is presented in stages (boldface type)
to an expert clinician, who responds to the information, sharing his or her reasoning with
the reader (regular type). The authors commentary follows.
A 62-year-old woman was admitted to the hospital because of abnormal liver-function
tests. She had a history of acute myelogenous leukemia and had undergone transplantation of T-celldepleted allogeneic bone marrow two years earlier. The patient had
had mildly increased aminotransferase levels since the transplantation. Four months
before admission, the levels of alkaline phosphatase and bilirubin became elevated,
presumably because of chronic graft-versus-host disease. Findings on computed tomography (CT) and ultrasonography of the abdomen were negative for disease in the
hepatic parenchyma or biliary tree.
On the day of admission, during a routine appointment, the patients total bilirubin
level was found to have increased from 4.9 mg per deciliter (83.8 mol per liter) the
previous day to 9.0 mg per deciliter (153.9 mol per liter). The serum sodium level was
124 mmol per liter.
From the Division of Endocrinology, Diabetes and Hypertension (A.T., E.W.S.), and
the Division of Nephrology (J.L.S.), Department of Medicine, Brigham and Womens
Hospital, Boston. Address reprint requests
to Dr. Turchin at the Division of Endocrinology, Diabetes and Hypertension, Brigham
and Womens Hospital, 221 Longwood
Ave., Boston, MA 02115, or at aturchin@
partners.org.
N Engl J Med 2003;349:1465-9.
Copyright 2003 Massachusetts Medical Society.
This patient presents with immediate problems of abnormal liver function and hyponatremia. I would initially approach the problem of hyponatremia and then attempt to
find connections to her relevant medical history.
Hyponatremia may occur with a high, low, or normal serum osmolality. High osmolality indicates the presence of excessive extracellular osmoles leading to the entry of
intracellular water into the extracellular fluid and the dilution of the sodium in the extracellular fluid. High glucose levels are a typical cause of this condition, and the patient
may be at particular risk for hyperglycemia if she is taking glucocorticoids. Unlike
glucose, solutes that enter cells, such as urea or ethanol, do not cause intracellular-toextracellular water shift and thus do not cause hyponatremia.
Hyponatremia with low serum osmolality may be observed in patients with hypovolemia, states involving low cardiac output, liver disease, the nephrotic syndrome,
or the syndrome of inappropriate secretion of antidiuretic hormone. Hypoadrenalism
or thyroid deficiency must also be considered. Psychogenic polydipsia can also result
in hypo-osmolal hyponatremia and can be distinguished from the above causes by low
urine osmolality and often on the basis of the history.
When the serum osmolality is normal, the first consideration should be pseudohyponatremia, an artifact of measurement that is most commonly caused by severe degrees
of hypertriglyceridemia or chylomicronemia or by severe paraproteinemia. Hyponatremia with normal osmolality can also occur when more than one disorder is present.
For example, hypothyroid-induced hypo-osmolality could be offset by hyperglycemia.
To begin with, I would like to know whether the review of the patients systems and
the physical examination suggest extracellular volume depletion or fluid overload
and whether she has any stigmata of chronic liver disease. Levels of blood glucose, urea,
and osmolality, as well as urine osmolality and urine sodium, should be measured.
n engl j med 349;15
www.nejm.org
october 9, 2003
Downloaded from www.nejm.org at ALLAN BLAIR CANCER CTR on May 30, 2006 .
Copyright 2003 Massachusetts Medical Society. All rights reserved.
1465
The
new england journal
The patient reported a number of symptoms consistent with the presence of hypothyroidism, including decreased energy, weight gain, constipation,
dry skin, and new-onset hoarseness. Her medications included tacrolimus, prednisone (40 mg per
day), mycophenolate mofetil, ursodiol, atovaquone,
acyclovir, and clarithromycin. She was afebrile. Her
blood pressure was 130/75 mm Hg, and her heart
rate 80 beats per minute. The patient appeared to
be clinically euvolemic. She spoke slowly, with a
coarse voice. The thyroid was not palpable. The
skin was dry and cool, and the nails were brittle.
The reflexes had a slowed relaxation phase. The
patient had scleral icterus and moon facies. There
was no ascites.
The serum osmolality was 294 mOsm per kilogram, the urine osmolality 434 mOsm per kilogram, and the urinary sodium level 62 mmol per liter. The thyrotropin level was 72 U per milliliter,
the serum total thyroxine level 0.6 g per deciliter
(7.7 nmol per liter), the blood urea nitrogen level
43 mg per deciliter (15.4 mmol per liter), the serum
creatinine level 1.4 mg per deciliter (123.8 mol per
liter), and the serum glucose level 85 mg per deciliter (4.7 mmol per liter). Levothyroxine treatment
was begun.
of
medicine
lipemia was observed. A lipid profile obtained two
years earlier showed a total cholesterol level of
181 mg per deciliter (4.68 mmol per liter) and a triglyceride level of 136 mg per deciliter (1.54 mmol
per liter).
Since the serum is not lipemic, extreme hypertriglyceridemia is unlikely. Severe hypercholesterolemia
could cause pseudohyponatremia without lipemic
serum; cholesterol, like triglycerides, is insoluble
and would artifactually lower sodium levels by increasing the solid fraction of plasma. I would like
to know the patients current cholesterol and triglyceride levels.
The lipid profile revealed a total cholesterol level
of 1836 mg per deciliter (47.48 mmol per liter), a
high-density lipoprotein (HDL) cholesterol level
of 68 mg per deciliter (1.76 mmol per liter), a verylow-density lipoprotein (VLDL) cholesterol level
of 42 mg per deciliter (1.09 mmol per liter), a triglyceride level of 208 mg per deciliter (2.35 mmol
per liter), and a calculated low-density lipoprotein
(LDL) cholesterol level of 1726 mg per deciliter
(44.63 mmol per liter). The serum sodium level, as
measured on a blood-gas machine with the use of
direct-ion potentiometry, was 145 mmol per liter.
It is notable that although the patients serum osmolality as measured by the freezing-point depression
was 294 mOsm per kilogram, her calculated osmolality (determined as [2the urine sodium level] +
[the blood urea nitrogen level2.8]+[the serum
glucose level18]) was 268 mOsm per kilogram. In
the absence of hyperglycemia or azotemia that could
account for the osmolal gap (the difference between
the measured osmolality and the calculated osmolality) of 26 mOsm per kilogram, we must consider another explanation for the patients apparent
pseudohyponatremia. I would like to know whether
the blood sample was lipemic; a further laboratory
workup should include the measurement of total
serum protein and a lipid profile in order to rule
out hyperproteinemia and hypertriglyceridemia.
Although hypothyroidism can cause hyponatremia, in this case it is at most a minor contributor,
since the patient does not have low serum osmolality. I would not expect levothyroxine replacement
to improve her serum sodium levels.
These findings are diagnostic of pseudohyponatremia caused by severe hypercholesterolemia. Whereas the instruments for routine chemical analysis
typically use indirect potentiometry (involving the
dilution of samples) to measure sodium levels, in
this case, the equipment for measuring arterial
blood gases, which relies on direct potentiometry,
was used. This latter method confirmed that there
was a normal serum sodium concentration.
It is important to emphasize that the treatment
of hypo-osmolal hyponatremia is very different from
the treatment of pseudohyponatremia, and going
down the wrong management path may harm the
patient. Fluid restriction, which is typically used to
correct hypo-osmolal hyponatremia, could, in a patient like this one, increase the already elevated serum osmolality. This effect could, in turn, worsen a
state of hyperviscosity, if one were present, or impair the blood flow in the microcirculation and aggravate any underlying hypercoagulability.
To treat this patient successfully, it is important
The serum sodium level remained low. The to- to determine the source of the unusually high chotal serum protein level was 5.1 g per deciliter. No lesterol levels. Hypothyroidism or tacrolimus can
1466
n engl j med 349;15
www.nejm.org
october 9 , 2003
Downloaded from www.nejm.org at ALLAN BLAIR CANCER CTR on May 30, 2006 .
Copyright 2003 Massachusetts Medical Society. All rights reserved.
clinical problem-solving
raise the cholesterol level, but not to this degree. Although the laboratory reported that most of the
cholesterol was in the form of LDL cholesterol,
the LDL cholesterol levels were not measured directly, but were calculated. The formula for the calculation of the LDL cholesterol level (total cholesterol levelHDL cholesterol levelVLDL cholesterol
level [the VLDL cholesterol level is usually calculated by dividing the fasting triglyceride level by 5])
assumes that the cholesterol consists solely of HDL,
LDL, and VLDL fractions. In a patient with liver disease, however, another form of cholesterol could be
present: lipoprotein X, which has been described
in patients with severe cholestasis, such as those
with primary biliary cirrhosis or, as in this case, with
chronic graft-versus-host disease. Lipoprotein X is
formed when there is reflux of unesterified cholesterol and phospholipids into the circulation from
the cholestatic biliary ducts; the particles of this
form of cholesterol are not soluble in plasma water
and thus increase the solid fraction of plasma.
A lipoprotein analysis should be performed. Because high levels of lipoprotein X could result in a
hyperviscosity syndrome, the patient should be examined carefully for signs of hyperviscosity, such as
dilated, segmented, and tortuous retinal veins, resulting in a sausage-link appearance. The serum
viscosity should be measured, and if it is found to
be high (>3 centipoise), prophylactic lipid apheresis should be considered.
I agree with the decision to initiate colestipol therapy (particularly given that liver dysfunction is a contraindication to the use of most other lipid-lowering agents); in the absence of higher serum viscosity,
the decision to withhold apheresis was reasonable.
Since cholestasis induced by graft-versus-host disease is the primary cause of the patients extreme
hypercholesterolemia, successful management of
graft-versus-host disease will be crucial in correcting the dyslipidemia.
Ten days later, the patient was readmitted to the
hospital because of new-onset shortness of breath
and dyspnea on exertion. CT of the chest showed
numerous lung nodules, and a sputum culture
grew Aspergillus niger, Nocardia asteroides, and mucor. The serum sodium level was 126 mmol per liter
as measured by indirect potentiometry on admission. Therapy with voriconazole, imipenemcilastatin, amikacin, and liposomal amphotericin B was
begun; treatment with mycophenolate mofetil,
colestipol, tacrolimus, atovaquone, ursodiol, prednisone (40 mg daily), and levothyroxine was continued. A week later, the patients clinical condition
deteriorated; she became progressively more dyspneic, and her oxygen saturation decreased from
98 percent while she was breathing room air on
admission to 92 percent while she was receiving
6 liters of oxygen per minute by nasal cannula; at
the same time, her serum sodium level decreased
to 115 mmol per liter. On repeated measurement,
During the rest of her hospitalization, the patients the total cholesterol level was 1114 mg per deciliserum sodium levels remained stable, around ter (28.8 mmol per liter). The thyroxine level was
125 mmol per liter when measured by indirect po- 2.2 g per deciliter (28.3 nmol per liter).
tentiometry but 135 to 136 mmol per liter when
measured directly. A liver biopsy was performed Although the measurement of the sodium concenand revealed bile-duct degeneration and loss con- tration by indirect potentiometry is not valid, the
sistent with graft-versus-host disease. Lipoprotein worsening of the hyponatremia despite improveelectrophoresis demonstrated that cholesterol was ment in the serum cholesterol level is a cause of conpredominantly carried by lipoprotein X, a finding cern. The measurement of serum osmolality or a
that was attributed to the cholestasis associated direct measure of serum sodium would establish
with graft-versus-host disease. The patient had no whether there is now hypo-osmolal hyponatremia
symptoms suggestive of hyperviscosity, including present that is complicating the underlying pseuvisual changes, vertigo, ataxia, and changes in men- dohyponatremia. Hypo-osmolality could be relattal status. A funduscopic examination was unre- ed to increased water retention associated with hymarkable. The serum viscosity was 1.9 centipoise poxia, with the pulmonary process itself causing
(normal range, 1.4 to 1.8). Lipid apheresis was con- the syndrome of inappropriate secretion of antidiusidered but, given the absence of symptoms and the retic hormone, or to diminished cardiac or renal
mild elevation of the serum viscosity, was deferred function. It is unlikely that there is adrenal insuffiuntil a trial of medical therapy had been completed. ciency, since the patient is taking glucocorticoids. I
Colestipol therapy was initiated, and the patient was would measure the serum and urine osmolality
discharged from the hospital.
and the serum creatinine level. The sodium con-
n engl j med 349;15
www.nejm.org
october 9, 2003
Downloaded from www.nejm.org at ALLAN BLAIR CANCER CTR on May 30, 2006 .
Copyright 2003 Massachusetts Medical Society. All rights reserved.
1467
The
new england journal
of
medicine
centration should be remeasured by direct poten- failure, or end-stage liver failure unlikely. These findtiometry.
ings are, however, consistent with the syndrome of
inappropriate secretion of antidiuretic hormone.
Given the acute worsening of hyponatremia while The pulmonary disease is the most likely cause, althe cholesterol levels were improving, a second though stress, nausea, or pain (if these are present)
workup was performed. As measured by direct po- could also play a part.
tentiometry, the serum sodium level was 128 mmol
per liter. The serum osmolality was 269 mOsm per The syndrome of inappropriate secretion of antikilogram, the serum glucose level was 104 mg per diuretic hormone, presumably caused by the lung
deciliter (5.8 mmol per liter), the blood urea nitro- infections, was diagnosed, and fluid intake was
gen level was 29 mg per deciliter (10.4 mmol per li- restricted to 1500 ml daily. The serum sodium level
ter), the serum creatinine level was 1.5 mg per deci- (as determined by direct potentiometry) and the
liter (132.6 mol per liter), the urine osmolality was serum osmolality normalized within several days.
335 mOsm per kilogram, and the urinary sodium
level was 44 mmol per liter. Oxygenation progrescommentary
sively decreased.
Hyponatremia remains a common problem in hosAlthough there is still an osmolal gap (now de- pitalized patients, with a prevalence of up to 12 percreased to 23 mOsm per kilogram), there is now also cent.1 As the discussant notes, appropriate managetrue hypo-osmolality. Combined with the inappro- ment depends on distinguishing between two main
priately high osmolality of the urine, this points to categories of processes leading to a low laboratory
high levels of vasopressin. The absence of clinical sodium value: hypo-osmolar (or true) hyponatresigns of dehydration and the presence of a relative- mia versus iso-osmolar or hyperosmolar hyponatrely high urinary sodium level (particularly if there is mia, or pseudohyponatremia.
no oliguria) and inappropriately high urinary osmoHypo-osmolar hyponatremia is a serious delality make intravascular depletion, congestive heart rangement of homeostasis and can lead to lifethreatening complications, such as seizures or alterations in mental status; it requires careful correction.
In contrast, pseudohyponatremia is not, in itself,
Normal Fraction
Increased Fraction
dangerous, and the primary treatment is for the unof Solid-Phase Particles
of Solid-Phase Particles
derlying cause (in this case, hypercholesterolemia).
There may be more than one cause, as in the case
described above.
Pseudohyponatremia secondary to hyperlipidemia was originally described in the 1950s,2 when
electrolytes were measured by flame photometry.
Water phase
With this technique, the serum sample is diluted beSolid phase
fore the actual measurement is obtained. Therefore,
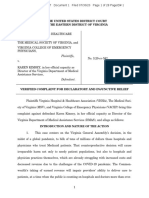
if more than the normal fraction of serum (7 percent
Standard volume
by volume) consists of proteins or lipids, the degree
of diluent added
of dilution is underestimated, resulting in artificially low sodium levels (Fig. 1).
Figure 1. Artificially Low Ion Levels as Determined by Dilution-Based Methods.
In the 1980s, flame photometry began to be used
Normally, serum contains 7 percent solids by volume. In order to reduce the
less frequently, as direct potentiometry became more
volume of blood needed for analysis, serum is frequently diluted before the
common.3 In direct potentiometry, undiluted serum
actual measurement is obtained. The same volume of diluent is always used;
samples are used to measure the transmembrane
the degree of dilution is estimated under the assumption that the serum conpotentials resulting from electrolyte gradients, and
tains 7 percent solid-phase particles. When the fraction of solid-phase particles
the measurement is therefore not dependent on the
is increased, the same amount of diluent results in a greater dilution, unbewater content of the sample. Consequently, a numknownst to the laboratory personnel (right side of figure). Consequently, the
calculation of an ion level with the use of a degree of dilution that is based on
ber of major medical textbooks state that pseudothe incorrect fraction of solid-phase particles will lead to an underestimate.
hyponatremia is rarely encountered with the use of
modern instruments.4-6 However, more than two
1468
n engl j med 349;15
www.nejm.org
october 9 , 2003
Downloaded from www.nejm.org at ALLAN BLAIR CANCER CTR on May 30, 2006 .
Copyright 2003 Massachusetts Medical Society. All rights reserved.
clinical problem-solving
thirds of the instruments that are currently in use in
laboratories in the United States use a technique of
indirect ion potentiometry for the measurement of
electrolytes.7 In fact, since a large number of directpotentiometry instruments are used only for the
analysis of blood gases, the proportion of routine
measurements of sodium performed with indirectpotentiometry instruments is likely to be even higher. Like flame photometry, this method involves the
dilution of the sample before the actual measurement is obtained, which minimizes the amount of
blood that is needed but renders the method susceptible to the same error of underestimating the
degree of dilution.
There is also a misconception that only hypertriglyceridemia, and not hypercholesterolemia, causes
pseudohyponatremia.6 Unlike high triglyceride levels, high cholesterol levels do not cause the blood
to be visibly lipemic,8 which would alert laboratory
personnel and permit the removal of excess lipids.
Severe hypercholesterolemia is an important but uncommon cause of pseudohyponatremia, and there
are only a few case reports in the literature,9-11 all of
them involving pseudohyponatremia secondary to
high levels of lipoprotein X. It has been hypothesized that the reflux of bile lipoproteins into the
bloodstream is a mechanism for the formation of
lipoprotein X, and the incubation of bile lipoproteins with serum or albumin in vitro leads to the appearance of lipoprotein-Xlike particles.12 Levels
of lipoprotein X can be as high as several thousand
milligrams per deciliter of cholesterol. Aside from
interfering with laboratory tests and, in extreme
cases, causing the hyperviscosity syndrome,13 high
levels of lipoprotein X are not known to lead to any
pathologic consequences.
A systematic approach to hyponatremia that is
based on the serum osmolality, such as that followed
by the discussant, can enable the clinician to avoid
errors in diagnosis and potentially harmful treatment. Deaths have followed the misdiagnosis of
pseudohyponatremia as true hyponatremia with aggressive attempts to increase the sodium level with
the use of fluid restriction and hypertonic saline resulting in severe dehydration and hypernatremia.14
A careful diagnostic evaluation with attention to basic physiologic principles and to findings that are
inconsistent with the presumed cause is crucial for
the effective management of this common problem.
We are indebted to Mary Paton of the College of American Pathologists for her help in obtaining data on the laboratory instruments used to measure sodium, to Dr. Donald Wiebe for his assistance in measuring lipoprotein X, and to Drs. Frederick Grant,
Robert J. Soiffer, and Elizabeth Rhee for their help in taking care of
the patient.
references
1. Croal BL, Blake AM, Johnston J, Glen
AC, OReilly DS. Absence of relation between
hyponatraemia and hypothyroidism. Lancet
1997;350:1402.
2. Albrink MJ, Hald PM, Man EB, Peters
JP. The displacement of serum water by the
lipids of hyperlipemic serum: a new method
for the rapid determination of serum water.
J Clin Invest 1955;34:1483-8.
3. Weisberg LS. Pseudohyponatremia: a reappraisal. Am J Med 1989;86:315-8.
4. Robinson AG, Verbalis JG. Posterior pituitary gland. In: Larsen PR, Kronenberg
HM, Melmed S, Polonsky KS, eds. Williams
textbook of endocrinology. 10th ed. Philadelphia: W.B. Saunders, 2003:281-329.
5. Lewis JL III. Water, electrolyte, mineral,
and acid-base metabolism. In: Beers MH,
Berkow R, eds. The Merck manual of diagnosis and therapy. Whitehouse Station, N.J.:
Merck Research Laboratories, 1999:12064.
6. Fukagawa M, Kurokawa K, Papadakis
MA. Fluid & electrolyte disorders. In: Tierney
LM Jr, McPhee SJ, Papadakis MA, eds. Current medical diagnosis & treatment 2003.
42nd ed. New York: McGraw-Hill, 2003:83966.
7. Participant summary report: surveys
1982-2002. Northfield, Ill.: College of American Pathologists, 1982-2002.
8. Van Eck WF, Peters JP, Man EB. Significance of lactescence in blood serum. Metabolism 1952;1:383-95.
9. Coakley JC, Vervaart PP, McKay MRG.
Factitious hyponatremia in a patient with
cholestatic jaundice following bone marrow
transplantation. Pathology 1986;18:158-9.
10. Ko GTC, Yeung VTF, Chow CC, Mak TW,
Cockram CS. Pseudohyponatraemia second-
n engl j med 349;15
www.nejm.org
ary to hypercholesterolaemia. Ann Clin Biochem 1997;34:324-5.
11. Hickman PE, Dwyer KP, Masarei JRL.
Pseudohyponatremia, hypercholesterolemia, and primary biliary cirrhosis. J Clin
Pathol 1989;42:167-71.
12. Manzato E, Fellin R, Baggio G, Walch S,
Neubeck W, Seidel D. Formation of lipoprotein-X: its relationship to bile compounds.
J Clin Invest 1976;57:1248-60.
13. Rosenson RS, Baker AL, Chow MJ, Hay
RV. Hyperviscosity syndrome in a hypercholesterolemic patient with primary biliary cirrhosis. Gastroenterology 1990;98:1351-7.
14. Frier BM, Steer CR, Baird JD, Bloomfield S. Misleading plasma electrolytes in diabetic children with severe hyperlipidaemia.
Arch Dis Child 1980;55:771-5.
Copyright 2003 Massachusetts Medical Society.
october 9, 2003
Downloaded from www.nejm.org at ALLAN BLAIR CANCER CTR on May 30, 2006 .
Copyright 2003 Massachusetts Medical Society. All rights reserved.
1469
New England Journal of Medicine
CORRECTION
Mind the Gap
Mind the Gap . On page 1466, in the formula that begins on line 4
of the third paragraph in the left-hand column, the first amount should
have read ``2 the serum sodium level, rather than ``2 the urine
sodium level, as printed.
N Engl J Med 2003;349:1880-a
Downloaded from www.nejm.org at ALLAN BLAIR CANCER CTR on May 30, 2006 .
Copyright 2003 Massachusetts Medical Society. All rights reserved.
New England Journal of Medicine
CORRECTION
Mind the Gap
Mind the Gap . On page 1466, lines 6 through 8 of the third paragraph
in the left-hand column, the sentence beginning, ``In the absence of
hyperglycemia or azotemia that could account for the osmolal gap
warrants correction. Neither hyperglycemia nor azotemia could contribute to the osmolal gap. On page 1469, lines 3 through 6 of the
partial paragraph in the right-hand column should have read, ``Levels
of lipoprotein X can be as high as several thousand milligrams per
deciliter of serum, rather than ``Levels of lipoprotein X can be as
high as several thousand milligrams per deciliter of cholesterol, as
printed.
N Engl J Med 2004;350:629
Downloaded from www.nejm.org at ALLAN BLAIR CANCER CTR on May 30, 2006 .
Copyright 2003 Massachusetts Medical Society. All rights reserved.
Das könnte Ihnen auch gefallen
- Exocrine Pancreatic Insufficiency in AdultsDokument18 SeitenExocrine Pancreatic Insufficiency in Adultshoneyworks100% (1)
- Acute Renal Failure Case StudyDokument18 SeitenAcute Renal Failure Case Studymanjeet3680% (5)
- Biosimilars: Pros and Cons in Current Practice: MBBS, MRCP (Uk), FRCP (Edin), FamsDokument51 SeitenBiosimilars: Pros and Cons in Current Practice: MBBS, MRCP (Uk), FRCP (Edin), FamshoneyworksNoch keine Bewertungen
- Lymph Nodes.120182800Dokument43 SeitenLymph Nodes.120182800honeyworks100% (1)
- Ash Sap 2016Dokument672 SeitenAsh Sap 2016honeyworksNoch keine Bewertungen
- Repertory of Miasms H 36011Dokument32 SeitenRepertory of Miasms H 36011Fazal Akhtar100% (3)
- Harrison MCQ NephrologyDokument7 SeitenHarrison MCQ Nephrologydrtpk80% (15)
- Diabetic KetoacidosisDokument12 SeitenDiabetic KetoacidosisSarah GatuzNoch keine Bewertungen
- Nephrology TestDokument112 SeitenNephrology TestRapid Medicine50% (2)
- FwprogrammeDokument38 SeitenFwprogrammeSujatha J Jayabal87% (15)
- Complementary and Alternative Medical Lab Testing Part 6: Liver and GallbladderVon EverandComplementary and Alternative Medical Lab Testing Part 6: Liver and GallbladderNoch keine Bewertungen
- Fast Facts: Hyperlipidemia: Bringing clarity to lipid managementVon EverandFast Facts: Hyperlipidemia: Bringing clarity to lipid managementNoch keine Bewertungen
- Test 3 July 2018Dokument8 SeitenTest 3 July 2018Mobin Ur Rehman KhanNoch keine Bewertungen
- Indigo Boarding Pass SampleDokument1 SeiteIndigo Boarding Pass Samplehoneyworks75% (4)
- Immunisation History Statement 3Dokument2 SeitenImmunisation History Statement 3Fordham JessNoch keine Bewertungen
- Endocrinology 101 150Dokument29 SeitenEndocrinology 101 150Ahmed El AlfyNoch keine Bewertungen
- NCP Deficit Fluid VolumeDokument4 SeitenNCP Deficit Fluid VolumeKingJayson Pacman06Noch keine Bewertungen
- DR List IshwarDokument18 SeitenDR List IshwarIshwar Rajput100% (1)
- As en 556.1-2002 Sterilization of Medical Devices - Requirements For Medical Devices To Be Designated STERILEDokument8 SeitenAs en 556.1-2002 Sterilization of Medical Devices - Requirements For Medical Devices To Be Designated STERILESAI Global - APACNoch keine Bewertungen
- Olympus EndosDokument9 SeitenOlympus EndoshoneyworksNoch keine Bewertungen
- Knowledge, Attitude and Practices of School Children On Prevention and Control of Superficial Fungal in Western KenyaDokument7 SeitenKnowledge, Attitude and Practices of School Children On Prevention and Control of Superficial Fungal in Western KenyaPremier PublishersNoch keine Bewertungen
- Hyperthermia (Thurs)Dokument1 SeiteHyperthermia (Thurs)Christine Esguerra OrozcoNoch keine Bewertungen
- Case History 33Dokument4 SeitenCase History 33Hida KurticNoch keine Bewertungen
- Jaundice As A Presentation of Thyrotoxic CrisisDokument3 SeitenJaundice As A Presentation of Thyrotoxic CrisisRizki AmeliaNoch keine Bewertungen
- A Physiologic-Based Approach To The Treatment of A Patient With HypokalemiaDokument6 SeitenA Physiologic-Based Approach To The Treatment of A Patient With HypokalemiaPablo IgnacioNoch keine Bewertungen
- sTUDI KASUS LIPIDDokument3 SeitensTUDI KASUS LIPIDAccung BuccuNoch keine Bewertungen
- HyperkalemiaDokument23 SeitenHyperkalemiaarungNoch keine Bewertungen
- Case Study 2Dokument2 SeitenCase Study 2api-547174770100% (1)
- HYPERALDOSTERONISMDokument7 SeitenHYPERALDOSTERONISMMarnee Justine ColladoNoch keine Bewertungen
- Lectura Recomendada HiperkalemiaDokument7 SeitenLectura Recomendada HiperkalemianeomaosNoch keine Bewertungen
- Glucocorticoid-Induced Central Diabetes Insipidus in A Case of Malignant LymphomaDokument10 SeitenGlucocorticoid-Induced Central Diabetes Insipidus in A Case of Malignant LymphomaoliviaNoch keine Bewertungen
- Journal Presentation: The New England Journal of Medicine Case Records of The Massachusetts General HospitalDokument49 SeitenJournal Presentation: The New England Journal of Medicine Case Records of The Massachusetts General HospitalSomnath SenguptaNoch keine Bewertungen
- Endoc, Pancreas, ThyroidDokument9 SeitenEndoc, Pancreas, ThyroidKatrina Vianca DecapiaNoch keine Bewertungen
- Medical Surgical Nursing - NeuroDokument19 SeitenMedical Surgical Nursing - NeuroChristian EstevesNoch keine Bewertungen
- Case Challenge: Diagnosing and Managing CKD Comorbidities: Literature ReviewDokument8 SeitenCase Challenge: Diagnosing and Managing CKD Comorbidities: Literature ReviewPratik TripathiNoch keine Bewertungen
- Hipernatremia en SX HiperosmolarDokument3 SeitenHipernatremia en SX HiperosmolarKrloss MartinezNoch keine Bewertungen
- Acute Pancreatitis With Normal Serum Lipase: A Case SeriesDokument4 SeitenAcute Pancreatitis With Normal Serum Lipase: A Case SeriesSilvina VernaNoch keine Bewertungen
- Disorders of Carbohydrate Metabolism.: Abdelmoniem Saeed Mohammed Er SpecialistDokument49 SeitenDisorders of Carbohydrate Metabolism.: Abdelmoniem Saeed Mohammed Er SpecialistYousef Al-AmeenNoch keine Bewertungen
- HiponatremiaDokument10 SeitenHiponatremiaHakim Arul100% (1)
- HypokalemiaDokument10 SeitenHypokalemiaAgronaSlaughterNoch keine Bewertungen
- CometDokument9 SeitenCometSohail AhmedNoch keine Bewertungen
- Reduction of Plasma Triglycerides by Diet in Subjects With Chronic Renal FailureDokument15 SeitenReduction of Plasma Triglycerides by Diet in Subjects With Chronic Renal FailureDina sayunaNoch keine Bewertungen
- Streptozotocin Diabetes MellitusDokument11 SeitenStreptozotocin Diabetes MellitusNurfadilaYahyaNoch keine Bewertungen
- Hyperkalemia Revisited: ReviewDokument8 SeitenHyperkalemia Revisited: ReviewFisiologiaUFCGNoch keine Bewertungen
- Progressive Muscle Weakness: More There Than Meets The Eye: Im Board ReviewDokument7 SeitenProgressive Muscle Weakness: More There Than Meets The Eye: Im Board Reviewbdalcin5512Noch keine Bewertungen
- Hyperosmolar Diabetic Non-Ketotic Coma, Hyperkalaemia and An Unusual Near Death ExperienceDokument7 SeitenHyperosmolar Diabetic Non-Ketotic Coma, Hyperkalaemia and An Unusual Near Death ExperienceAnonymous nEQNlgbYQCNoch keine Bewertungen
- DD Metabolic SyndromeDokument5 SeitenDD Metabolic SyndromeEluNoch keine Bewertungen
- Case Study About Hypertension With Electrolyte Imbalance Part 1Dokument21 SeitenCase Study About Hypertension With Electrolyte Imbalance Part 1THE NURSING CORNERS0% (1)
- Casos Clínicos K+ Core Curriculum AJKDDokument3 SeitenCasos Clínicos K+ Core Curriculum AJKDFabiola AlonsoNoch keine Bewertungen
- Case Report Glycogenic Hepatopathy in Type 1 Diabetes MellitusDokument4 SeitenCase Report Glycogenic Hepatopathy in Type 1 Diabetes MellitusCarlos Alberto Rodriguez ValbuenaNoch keine Bewertungen
- Relation Between Hyperuricemia and Metabolic Syndrome Among Obese WomenDokument8 SeitenRelation Between Hyperuricemia and Metabolic Syndrome Among Obese WomenKara Citra KalandraNoch keine Bewertungen
- Normal Protein Diet and L-Ornithine-L-Aspartate For Hepatic EncephalopathyDokument4 SeitenNormal Protein Diet and L-Ornithine-L-Aspartate For Hepatic EncephalopathyElisa SalakayNoch keine Bewertungen
- Clinical History and Initial Laboratory DataDokument10 SeitenClinical History and Initial Laboratory DataputrisyifaaNoch keine Bewertungen
- Module 3-Specimen Collection and ProcessingDokument10 SeitenModule 3-Specimen Collection and ProcessingAllyah Ross DuqueNoch keine Bewertungen
- Cholesterol, Triglycerides, and Associated Lipoproteins - Clinical Methods - NCBI BookshelfDokument30 SeitenCholesterol, Triglycerides, and Associated Lipoproteins - Clinical Methods - NCBI BookshelfNeha MasarkarNoch keine Bewertungen
- CSP FEB2020 BROCHURE 150120 8pp v1-1Dokument8 SeitenCSP FEB2020 BROCHURE 150120 8pp v1-1hajir hassanNoch keine Bewertungen
- Cardiac Enzyme Analysis: Anika Dahal Lecturer MmihsDokument40 SeitenCardiac Enzyme Analysis: Anika Dahal Lecturer Mmihsanika dahalNoch keine Bewertungen
- Abordaje de PX Con Enf RenalDokument12 SeitenAbordaje de PX Con Enf Renalcleooatra mairenaNoch keine Bewertungen
- Hyperglycemic Crises in Patients With Diabetes Mellitus: Position StatementDokument9 SeitenHyperglycemic Crises in Patients With Diabetes Mellitus: Position StatementChristian SalimNoch keine Bewertungen
- Jama Hta ResistenteDokument9 SeitenJama Hta ResistenteMayra Alejandra Prada SerranoNoch keine Bewertungen
- 6 Hypertension Nursing Care - Arif Setyo UpoyoDokument40 Seiten6 Hypertension Nursing Care - Arif Setyo UpoyoRizka Nur AgustinNoch keine Bewertungen
- Clinical Biochemistry: MSD Manual Veterinary ManualDokument5 SeitenClinical Biochemistry: MSD Manual Veterinary ManualDursa MiressaNoch keine Bewertungen
- HELLP SyndromeDokument8 SeitenHELLP SyndromeFred OseiNoch keine Bewertungen
- 7decaf9c Cb18 4623 Bced Ecef2197e451Dokument25 Seiten7decaf9c Cb18 4623 Bced Ecef2197e451PrabhuNoch keine Bewertungen
- CaseDokument7 SeitenCaseDenny EmiliusNoch keine Bewertungen
- Perez Pozo2009Dokument8 SeitenPerez Pozo2009Anonymous 0mtGtB6u3Noch keine Bewertungen
- Primary Hyperaldosteronism - StatPearls - NCBI BookshelfDokument7 SeitenPrimary Hyperaldosteronism - StatPearls - NCBI BookshelfCecil-An DalanonNoch keine Bewertungen
- Polygenic HypercholesterolemiaDokument6 SeitenPolygenic HypercholesterolemiaSamhitha Ayurvedic ChennaiNoch keine Bewertungen
- Endocrin 5Dokument6 SeitenEndocrin 5Loyla RoseNoch keine Bewertungen
- Hypercalcemic Crisis: Reinhard ZieglerDokument7 SeitenHypercalcemic Crisis: Reinhard ZieglerRo KohnNoch keine Bewertungen
- Gestosis MergedDokument141 SeitenGestosis MergedRamNoch keine Bewertungen
- Electrolyte & Acid Base Disturbances in Diabetes MellitusDokument12 SeitenElectrolyte & Acid Base Disturbances in Diabetes MellitusAla SoroceanuNoch keine Bewertungen
- Anemia CasesDokument35 SeitenAnemia CasesBogdan UrichianuNoch keine Bewertungen
- Hypoglycemia in Diabetes: Pathophysiology, Prevalence, and PreventionVon EverandHypoglycemia in Diabetes: Pathophysiology, Prevalence, and PreventionNoch keine Bewertungen
- NH Protocol For Covid Management FinalDokument7 SeitenNH Protocol For Covid Management FinalhoneyworksNoch keine Bewertungen
- Sarfaraz Jalil Baig, Deepraj Bhandarkar, Pallawi Priya - Newer Concepts and Procedures in Hernia Surgery - An Atlas-Springer (2023)Dokument258 SeitenSarfaraz Jalil Baig, Deepraj Bhandarkar, Pallawi Priya - Newer Concepts and Procedures in Hernia Surgery - An Atlas-Springer (2023)honeyworksNoch keine Bewertungen
- Basic Ercp InterpretationDokument19 SeitenBasic Ercp Interpretationhoneyworks100% (2)
- Wallflexbiliary Productinfo Brochure PDFDokument6 SeitenWallflexbiliary Productinfo Brochure PDFhoneyworksNoch keine Bewertungen
- Benign Liver Tumours EASL CPGDokument34 SeitenBenign Liver Tumours EASL CPGhoneyworksNoch keine Bewertungen
- Anal Carcinoma: NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines)Dokument54 SeitenAnal Carcinoma: NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines)honeyworksNoch keine Bewertungen
- Dose EscalationDokument14 SeitenDose EscalationhoneyworksNoch keine Bewertungen
- DM GastroenterologyDokument27 SeitenDM GastroenterologyhoneyworksNoch keine Bewertungen
- Pi Is 1542356513007076Dokument7 SeitenPi Is 1542356513007076honeyworksNoch keine Bewertungen
- ShowPdf PDFDokument1 SeiteShowPdf PDFhoneyworksNoch keine Bewertungen
- ACG Abnormal Liver Chemistries Guideline 2017Dokument18 SeitenACG Abnormal Liver Chemistries Guideline 2017honeyworksNoch keine Bewertungen
- Fellowship Entrance Test (FET) 2017-Admission Session PDFDokument80 SeitenFellowship Entrance Test (FET) 2017-Admission Session PDFhoneyworksNoch keine Bewertungen
- Notice For Reporting at The Allotted Medical College Against Seat Allotted in Mop-Up RoundDokument1 SeiteNotice For Reporting at The Allotted Medical College Against Seat Allotted in Mop-Up RoundhoneyworksNoch keine Bewertungen
- Pavan CVDokument1 SeitePavan CVhoneyworksNoch keine Bewertungen
- Treatment of Hyponatremia - Syndrome of Inappropriate Antidiuretic Hormone Secretion (SIADH) and Reset OsmostatDokument15 SeitenTreatment of Hyponatremia - Syndrome of Inappropriate Antidiuretic Hormone Secretion (SIADH) and Reset Osmostathoneyworks100% (1)
- Drug StudyDokument2 SeitenDrug StudyJi Vista MamigoNoch keine Bewertungen
- OBM752 HM Unit-IV NotesDokument34 SeitenOBM752 HM Unit-IV NotesRajanNoch keine Bewertungen
- Howtousea Nebulizer in Pediatric ClientsDokument11 SeitenHowtousea Nebulizer in Pediatric ClientsAngelina Nicole G. TungolNoch keine Bewertungen
- Dka in PedsDokument11 SeitenDka in PedsMohamed YasserNoch keine Bewertungen
- Europian Medicin Agency For EyleaDokument83 SeitenEuropian Medicin Agency For EyleabangunNoch keine Bewertungen
- ComplaintDokument28 SeitenComplaintLia TabackmanNoch keine Bewertungen
- PSM MCQsDokument9 SeitenPSM MCQsRitesh SinghaNoch keine Bewertungen
- Daftar PustakaDokument3 SeitenDaftar PustakaNahrijah JahrinaNoch keine Bewertungen
- ConjuntivitisDokument21 SeitenConjuntivitisjoal510Noch keine Bewertungen
- Bhandari MagneticDokument12 SeitenBhandari MagneticrajanrathodNoch keine Bewertungen
- Neuromyelitis Optica (Nmo) and Nmo Spectrum DisorderDokument9 SeitenNeuromyelitis Optica (Nmo) and Nmo Spectrum DisorderVonny MaharaniNoch keine Bewertungen
- NevroblastomprotokollDokument217 SeitenNevroblastomprotokollsfghhhNoch keine Bewertungen
- DR Adedayo OSHOLOWU - Clinical Director - Special Olympics - NIGERIADokument3 SeitenDR Adedayo OSHOLOWU - Clinical Director - Special Olympics - NIGERIAAdedayo OsholowuNoch keine Bewertungen
- Complications of MalariaDokument12 SeitenComplications of MalariaAneesh MyneniNoch keine Bewertungen
- Tolbert Medical Clinic Anniston, Alabama: Planning Assessment, Space Program & Site Test Fit AnalysisDokument15 SeitenTolbert Medical Clinic Anniston, Alabama: Planning Assessment, Space Program & Site Test Fit Analysisalassadi09Noch keine Bewertungen
- Neonatal Anaesthesia 2 Anaesthesia For Neonates With Abdominal Wall DefectsDokument10 SeitenNeonatal Anaesthesia 2 Anaesthesia For Neonates With Abdominal Wall DefectsDr. Anish GolchhaNoch keine Bewertungen
- PDF To WordDokument284 SeitenPDF To WordVictoria UrsachiNoch keine Bewertungen
- The Andrew Wakefield CaseDokument3 SeitenThe Andrew Wakefield Caseapi-202268486Noch keine Bewertungen
- Efficacy of Ethanol Against Viruses in Hand DisinfectionDokument9 SeitenEfficacy of Ethanol Against Viruses in Hand DisinfectionImaec LimitedNoch keine Bewertungen
- Planning Design and Analysis of G+1 Hospital Building For Iiit Srikakulam CampusDokument1 SeitePlanning Design and Analysis of G+1 Hospital Building For Iiit Srikakulam CampusSaritha TejavathNoch keine Bewertungen
- Cardiopulmonary Assessment 2020721956580Dokument36 SeitenCardiopulmonary Assessment 2020721956580Kavya MittalNoch keine Bewertungen