Beruflich Dokumente
Kultur Dokumente
Abdominal Pain in Pregnancy
Hochgeladen von
brolieCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Abdominal Pain in Pregnancy
Hochgeladen von
brolieCopyright:
Verfügbare Formate
AJR Integrative Imaging
LIFELONG LEARNING
FOR RADIOLOGY
Abdominal Pain in Pregnancy: Diagnoses and Imaging
Unique to PregnancyReview
Downloaded from www.ajronline.org by 36.80.132.111 on 10/19/15 from IP address 36.80.132.111. Copyright ARRS. For personal use only; all rights reserved
Courtney A. Woodfield1, Elizabeth Lazarus1, Karen C. Chen1,2, William W. Mayo-Smith1
Objective
Abdominal pain during pregnancy can be caused by a wide
variety of diseases including disorders of the obstetric, gynecologic, gastrointestinal, hepatobiliary, genitourinary, and
vascular systems. Some causes are unique to pregnancy, are
exacerbated by pregnancy, or require an altered imaging algorithm for diagnosis during pregnancy. The educational objectives of this review article are for the participant to exercise, self-assess, and improve his or her understanding of the
imaging evaluation of abdominal pain during pregnancy.
Conclusion
This article reviews the causes of abdominal pain that
are unique to pregnancy as well as some of the more common and severe causes of abdominal pain in which the imaging workup differs in the pregnant population. The relative advantages of using ultrasound, CT, and MRI to help
establish the cause of the pain are also reviewed.
Introduction
A wide variety of diseases, including disorders of the obstetric, gynecologic, gastrointestinal, hepatobiliary, genitourinary, and vascular systems, can present as abdominal
pain during pregnancy [13] (Table 1). The clinical diagnosis of an intraabdominal disease in pregnant women is often
obscured by concurrent maternal physiologic and anatomic
changes [3, 4]. Guarding in the setting of peritonitis may
not occur because of the loss of elasticity in the abdominal
wall musculature [2]. Leukocytosis in pregnancy is less useful in clinical evaluation because WBC count is typically
elevated in pregnancy, ranging from 6,00016,000 cells/L
during the first and second trimesters to 2030,000 cells/L
at the end of the third trimester [3]. Ureteral compression
and displacement of intraabdominal organs, including the
appendix, by the gravid uterus may also confound the clinical presentation [2].
A delay in the diagnosis of many of the causes of abdominal pain can be threatening to both the mother and
the fetus [3, 5]. Imaging can clarify a confusing clinical pic-
ture and expedite diagnosis. Ultrasound is widely used as
the initial diagnostic imaging technique during pregnancy
because of its availability, portability, and lack of ionizing
radiation. Ultrasound often can elucidate the cause of abdominal pain, particularly if pain is due to an obstetric and
gynecologic abnormality. However, evaluation of the bowel,
pancreas, ureters, and mesenteric vasculature may be limited on ultrasound because of patient body habitus, a small
field of view, and the presence of overlying structures. Air
within the bowel can particularly limit evaluation of the
mesenteric vessels, pancreas, and bowel.
MRI is also a useful technique for imaging pregnant patients
given the lack of ionizing radiation. Several recent studies have
shown that MRI is valuable in evaluating abdominal pain during pregnancy, especially in the diagnosis of appendicitis,
which is the most common cause of an acute abdomen in pregnancy [68]. To date, no deleterious effects to the developing
fetus exposed to MRI have been reported. Therefore, no specific consideration for MRI during the first, second, or third
trimester has been recommended [9]. The use of MRI for the
evaluation of abdominal pain during pregnancy may be dependent on institutional availability and radiologist experience.
A recent guidance document for safe MR practices from the
American College of Radiology (ACR) does not recommend
the routine use of gadolinium during pregnancy [9]. Gadolinium-based MR contrast agents are known to pass through the
placenta to the fetal circulation. The contrast material is then
excreted by the fetal kidneys into the amniotic fluid where the
agent can remain for an indeterminate amount of time. To
date, no large, well-controlled studies have been performed to
document the presence or absence of adverse fetal effects resulting from maternal gadolinium administration. Therefore,
the potential risks to the fetus remain unknown [9].
Examinations using ionizing radiationin particular,
CTcan also accurately diagnose many causes of abdominal pain during pregnancy. A riskbenefit analysis is particularly warranted before performing an examination involving ionizing radiation on a pregnant or potentially
pregnant patient. However, most diagnostic imaging stud-
Keywords: abdominal pain, CT, MRI, ultrasound, womens imaging
DOI:10.2214/AJR.07.7139
Received November 14, 2008; accepted after revision November 4, 2009.
Department of Diagnostic Imaging, The Warren Alpert Medical School of Brown University, Women and Infants Hospital, Rhode Island Hospital, 593 Eddy St., Providence, RI 02903.
Address correspondence to C. A. Woodfield (courtneywoodfield@yahoo.com).
1
Present address: Department of Radiology, University of California at San Diego, San Diego, CA.
WEB
This is a Web exclusive article.
AJR 2010;194:WS14WS30 0361803X/10/1946WS14 American Roentgen Ray Society
WS14
AJR:194, June 2010
Abdominal Pain in Pregnancy
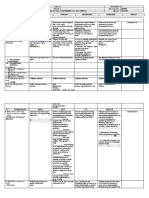
TABLE 1: Causes of Abdominal Pain in Pregnant
Women by Organ System
Organ System
Obstetric
Cause
Abortion
Downloaded from www.ajronline.org by 36.80.132.111 on 10/19/15 from IP address 36.80.132.111. Copyright ARRS. For personal use only; all rights reserved
Ectopic pregnancy
Preterm labor
Placental abruption
Uterine rupture
Gynecologic
Adnexal mass or ovarian cyst
Adnexal torsion
Uterine leiomyoma
Endometriosis
Pelvic inflammatory disease
Gastrointestinal
Appendicitis
Inflammatory bowel disease
Intestinal obstruction
Gastroesophageal reflux
Peptic ulcer disease
Hepatobiliary
HELLP syndrome
Acute fatty liver of pregnancy
Cholelithiasis or choledocholithiasis
Acute cholecystitis
Acute pancreatitis
Hepatitis
Genitourinary
Hydronephrosis of pregnancy
Urolithiasis
Pyelonephritis
Cystitis
Vascular
Gonadal vein thrombosis
Mesenteric vein thrombosis
Gonadal vein syndrome
Aneurysm rupture
Vasculitis
NoteHELLP = hemolysis, elevated liver enzymes, low platelet count.
ies utilizing ionizing radiation do not expose the fetus to a
radiation dose high enough to result in developmental or
neurologic deficits. Therefore, ionizing radiation examinations can still be offered to pregnant women when the study
is in the best health interest of the mother and the patient
understands the minimal and unknown risks to the fetus
[10]. For example, CT remains the most reliable technique
for depicting obstructing urinary tract calculi in pregnant
women [11]. Based on our experience with a low-dose renal
calculus protocol (160 mA and 140 kVp on a 16-MDCT
scanner), the mean radiation dose delivered to the female
pelvis is 16 mGy and to the fetus, 47.2 mGy and 8.511.7
mGy at 0 and 3 months of gestation, respectively [12]. This
dose is below the recommended 50-mGy (5-rad) maternal
AJR:194, June 2010
dose limit for avoiding deterministic radiation effects (i.e.,
effects that have a radiation threshold below which they
should not occur) such as fetal teratogenesis [13]. There is
no known maternal radiation limit for fetal stochastic effects (i.e., effects that can occur regardless of radiation
dose) such as carcinogenesis; therefore, radiation levels
should be kept as low as reasonably achievable (ALARA)
for all ionizing radiation studies [13].
Similar to gadolinium-based MR contrast agents, iodinated IV contrast agents have been shown to cross the placenta
to the fetal circulation and ultimately to be excreted into the
amniotic fluid. No teratogenic fetal effects from a single in
utero exposure to iodinated contrast material at diagnostic
doses have been reported. However, there have also been no
published large, well-controlled studies investigating potential teratogenic effects from iodinated contrast agents. In
early reports, investigators described transient congenital
hypothyroidism after amniofetography using iodinated contrast material [14]. However, more recent small studies of
pregnant patients receiving iodinated contrast material as
part of a CT protocol did not show any effect on thyroid
function [15]. Similar to its recommendations with regard to
gadolinium-based contrast agents, the ACR recommends IV
iodinated contrast administration during pregnancy only
when it is deemed necessary for prompt and accurate evaluation of the pregnant patients medical condition [16].
This review focuses on the causes of abdominal pain that
are unique to pregnancy as well as some of the more common and severe causes of abdominal pain in which the imaging workup differs in the pregnant population compared
with the nonpregnant population. This article also explores
the relative advantages of using different imaging techniques including ultrasound, CT, and MRI to help establish
the cause of the pain.
Obstetric Causes
During the first trimester of pregnancy, common causes
of abdominal and pelvic pain include early pregnancy failure and ectopic pregnancy. During the second and third trimesters, causes of pain include preterm labor and the less
common, but more severe, complications of placental
abruption and uterine rupture.
Early Pregnancy Failure
Spontaneous abortion occurs in approximately 1012%
of known first trimester pregnancies. Although the patient
may be asymptomatic, spontaneous abortion commonly results in pain and vaginal bleeding [17].
Ultrasound is the initial diagnostic test of choice for a
first trimester patient with pain and bleeding. Ultrasound
can confirm early pregnancy failure with high specificity if
no fetal cardiac activity is detected by the time the embryo
measures 5 mm in length or if the pregnancy is known to be
6.5 weeks without an embryo with a heartbeat [18].
WS15
Downloaded from www.ajronline.org by 36.80.132.111 on 10/19/15 from IP address 36.80.132.111. Copyright ARRS. For personal use only; all rights reserved
Woodfield et al.
Additional sonographic findings such as abnormal gestational sac size or shape and embryonic bradycardia may be
suggestive of a poor outcome but are not definitive for early
pregnancy failure. Large gestational sacs without a yolk sac or
an embryo are worrisome. The most widely accepted discriminatory sizes of the gestational sac using endovaginal
ultrasound are an 8-mm mean sac diameter by which a yolk
sac must be visualized and a 16-mm mean sac diameter by
which an embryo must be visualized for the pregnancy to be
considered normal [19, 20]. However, a range of higher discriminatory values has been reported in the literature, with
mean sac diameter values up to 13 mm for visualization of the
yolk sac and 18 mm for visualization of the embryo proposed
before considering a pregnancy abnormal [1921]. Given this
range of values, use of the discriminatory sac size is limited.
Worrisome findings on ultrasound also include slow embryonic cardiac activity, irregular gestational sac, and low position of the gestational sac [22]. Embryonic heartbeat rates
below 80 beats per minute (bpm) at 6.06.2 weeks or below
100 bpm at 6.37.0 weeks menstrual age are associated with
a very high rate of early pregnancy failure [23].
When the ultrasound examination either shows worrisome features or is inconclusive, such as in cases with an
embryo smaller than 5 mm without a heartbeat, follow-up
ultrasound is indicated. Follow-up ultrasound is typically
performed 57 days later to allow measurable growth. Correlating sonographic findings with maternal serum level of
-HCG can also help indicate whether early pregnancy failure has occurred. A gestational sac is expected to be visible
when the -HCG level is above 2,000 mIU/mL (third inter-
Fig. 1Tubal ectopic pregnancy in woman 8 weeks pregnant who presented
with right-sided pelvic pain. Gray-scale transvaginal ultrasound image reveals
extrauterine gestational sac (arrows) with yolk sac (arrowhead) between right
ovary (O) and uterus (UT).
national reference preparation) and the embryo when the
-HCG level is above 10,800 mIU/mL [24].
Ectopic Pregnancy
Ectopic pregnancy, which remains the most frequent obstetric cause of death in pregnancy, often presents with abdominal or pelvic pain in the first trimester [25]. The incidence of ectopic pregnancy has been increasing steadily
since 1970. This increased incidence correlates with an increase in the prevalence of risk factors for ectopic pregnancy including sexually transmitted diseases and assisted reproductive techniques [26, 27]. Ultrasound plays an
instrumental role in ruling out an ectopic pregnancy if it
Fig. 2Interstitial ectopic pregnancy.
A, Woman 7 weeks pregnant who presented with abdominal pain. Gray-scale transvaginal ultrasound image shows eccentric intrauterine gestational sac (arrows)
containing yolk sac and embryo. Endometrium (arrowheads) extends up to, but does not surround, gestational sac; these findings are consistent with interstitial pregnancy.
B, Woman 8 weeks pregnant who presented with abdominal pain. Coronal T2-weighted single-shot fast spin-echo MR image also shows eccentric intrauterine
gestational sac (arrows) that is not surrounded by endometrium (arrowheads).
WS16
AJR:194, June 2010
Downloaded from www.ajronline.org by 36.80.132.111 on 10/19/15 from IP address 36.80.132.111. Copyright ARRS. For personal use only; all rights reserved
Abdominal Pain in Pregnancy
can confirm an intrauterine pregnancy. Heterotopic pregnancy, a coexistent ectopic and intrauterine pregnancy, is
rare (1 in 7,000) in the general population. However, the
incidence of heterotopic pregnancy is higher after in vitro
fertilization, approaching 1% in some studies [28, 29].
In a small percentage of cases, ultrasound may conclusively diagnose ectopic pregnancy if it shows an extrauterine
gestational sac with a yolk sac or embryo (Fig. 1). More commonly, ultrasound reveals findings that are only suggestive of
an ectopic pregnancynotably, an adnexal mass and pelvic
free fluid. An adnexal mass is the most common sonographic
finding in ectopic pregnancy, occurring in 6584% of cases
[3032]. The adnexal mass can have a variety of appearances, including appearing to be a saclike ring, solid, or complex.
A small amount of pelvic free fluid can be seen in normal
pregnancies, but a moderate to large amount of pelvic fluid,
particularly if in association with an adnexal mass, significantly increases the risk for ectopic pregnancies. The presence of fluid-containing echoes, correlating with hemoperitoneum, carries a 93% positive predictive value for ectopic
pregnancy [33]. Occasionally ultrasound findings may appear normal in the setting of ectopic pregnancy.
MRI can be used as a problem-solving technique for the
less common nontubal forms of ectopic pregnancies when
sonography is indeterminate. With its multiplanar capabilities, MRI can help to confirm a suspected cervical ectopic
pregnancy or cesarean section scar ectopic pregnancy before
treatment. In addition, MRI can help differentiate between
eccentric implantation in the endometrium versus an interstitial ectopic pregnancy (Fig. 2). An interstitial ectopic pregnancy on MRI will appear as a gestational sac centered in the
cornual aspect of the uterine wall and will be separated from
the endometrium by an intact junctional zone [34] (Fig. 2).
Placental Abruption
Symptoms of placental abruption are variable but often
include vaginal bleeding and abdominal or pelvic pain. Placental abruption is defined as in utero separation of the placenta from the myometrium and accounts for 1025% of
prenatal deaths [35]. In most cases, ultrasound does not show
any signs of abruption because the hemorrhage resulting
from placental separation can pass through the cervical os.
Sonographic findings suggestive of placental abruption,
when they are visible, are usually due to hematomas. Visualization of a hematoma is clinically important because these
pregnancies have a worse prognosis [35]. The most common
location of hematomas in this setting is subchorionic (i.e.,
between the uterine wall and chorionic membrane) [36]. Retroplacental (behind the placenta) and preplacental (in front
of the placenta) hematomas are less common. The sonographic appearance of a hematoma varies with its acuity.
Acute hematomas are hyperechoic to isoechoic (Fig. 3). Initially, the only finding of an acute or subacute hematoma on
ultrasound may be an abnormally thickened placenta. In
AJR:194, June 2010
Fig. 3Placental abruption in woman 20 weeks pregnant who presented with
abdominal pain and vaginal bleeding. Gray-scale transabdominal ultrasound
image shows isoechoic collection in retroplacental location (arrows),
representing acute retroplacental hematoma secondary to placental abruption.
Normal placenta (arrowheads) is seen.
these cases, T1-weighted MRI may be used to help distinguish high-signal hematomas from the lower-T1-signal-intensity placenta [37]. Hematomas more than 12 weeks in
age appear progressively more hypoechoic [36].
Preterm Labor
Preterm labor is defined as uterine contractions strong
enough to cause cervical dilatation and effacement between
20 and 37 weeks gestation. The abdominal pain that accompanies these contractions is often clinically distinguishable, so imaging is typically not indicated for diagnosis.
However, ultrasound evaluation of cervical length is the
most sensitive predictor of preterm birth. The shorter the
cervical length measures, the higher the risk of preterm
birth. Also, the earlier a shortened cervical length is found,
the higher the risk of preterm birth. A normal cervical
length is more than 30 mm between 14 and 30 gestational
weeks [3840]. Cervical funneling is also associated with an
increased risk of preterm labor. Funneling occurs when the
internal os is open proximally and gradually narrows, approximating the appearance of a cone. If funneling is present, the cervical length is almost always shortened. However, the presence of funneling in a patient with a normal
cervical length does not increase the risk of preterm birth.
Uterine Rupture
Uterine rupture is a rare, catastrophic event that often
presents with severe abdominal pain. Predisposing factors
include previous uterine surgery, including cesarean deliveries and myomectomy, and congenital uterine malformations. Uterine rupture can occur during labor or before delivery such as in cases of interstitial ectopic pregnancies
that rupture [41]. Only a very short time interval for successful intervention exists once uterine rupture has occurred, so imaging in this setting may consume valuable
WS17
Woodfield et al.
time. If imaging is performed, ultrasound, CT, or MRI may
show herniation of the gestational sac contents (Fig. 4).
The choice of imaging technique will depend on patient stability and technique availability at a given institution.
Downloaded from www.ajronline.org by 36.80.132.111 on 10/19/15 from IP address 36.80.132.111. Copyright ARRS. For personal use only; all rights reserved
Gynecologic Causes
Common gynecologic causes of pain during pregnancy
include complications related to adnexal masses, ovarian
torsion, and leiomyomas. Adnexal masses are often first detected at the time of a routine first trimester dating or second trimester anatomic survey ultrasound examination [2].
Ovarian torsion and leiomyoma degeneration both have a
higher incidence during pregnancy [4244].
Adnexal Masses
Adnexal masses occur in approximately 2% of all pregnancies [3]. Adnexal masses are not a usual cause of pain, with
65% of these masses being asymptomatic and discovered incidentally on physical examination or sonography [2]. The size
of the mass also does not necessarily dictate whether it will
cause pain [2, 3]. However, if an adnexal mass is compressed,
if it compresses an adjacent organ or organs, as is more likely
to occur during pregnancy in association with an enlarging
gravid uterus, or if it becomes complicated by torsion, hemorrhage, or rupture, the adnexal mass may present with pain.
Imaging evaluation of the adnexa should be performed, starting with ultrasound, in all pregnant women presenting with
pain [42, 45]. Ultrasound provides the ability to distinguish
adnexal masses that are small, uncomplicated, and likely to
spontaneously resolve from those that appear larger and more
complex with a higher likelihood of malignancy, torsion, or
persistent pain from mass effect during pregnancy.
The most common adnexal masses during pregnancy are
corpus luteum or other functional ovarian cysts. The differential diagnosis for a complex-appearing adnexal mass
includes hemorrhagic corpus luteum cyst, ovarian cystadenoma, and ovarian teratoma. However, approximately
18% of adnexal masses found during pregnancy are malignant [42]. Therefore, when the sonographic appearance
of an adnexal mass is not specific, MRI can be used for further characterization to help determine patient management during pregnancy [45, 46] (Fig. 5). Complex adnexal
masses, particularly if they are already a source of pain,
may warrant surgical removal during pregnancy because of
an increased risk of torsion, rupture, and malignancy [47].
Ovarian Torsion
The incidence of ovarian torsion is increased during pregnancy, complicating 1 in 800 pregnancies. This increased incidence is most likely related to an increased incidence of
adnexal masses. Up to 7% of adnexal masses reportedly result in ovarian torsion during pregnancy [42, 43]. However,
torsion can also occur in an otherwise normal ovary, usually
the right ovary [2, 3]. During pregnancy, ovarian torsion
most commonly occurs between 6 and 14 weeks gestation
when uterine enlargement is most rapid [3, 45]. However, in
at least one study, up to 45% of cases of ovarian torsion presented during the second and third trimesters [48].
Sonography is the preferred imaging technique for the diagnosis of ovarian torsion, with the diagnosis made by a combination of gray-scale and color Doppler findings. The most consistent finding is an enlarged ovary [43, 49]. Additional findings
include a twisted vascular pedicle, pelvic free fluid, and a coexistent ovarian mass. The color Doppler findings are often variable. The most frequent finding on Doppler evaluation of the
ovary is either reduced or absent arterial flow. However, ovarian arterial waveforms may be detectible in the setting of torsion. This is theorized to be either due to venous thrombosis
alone eliciting symptoms or due to the dual blood supply of
the ovary [49, 50]. If the ultrasound findings are indetermi-
Fig. 4Uterine rupture in woman 15 weeks pregnant who presented with severe abdominal pain.
A and B, Gray-scale sagittal ultrasound images show fetus (arrow, A) superior to uterine fundus (arrowheads, A) and distension of endometrium with heterogeneous
hypoechoic material (arrowheads, B) due to hemorrhage after uterine rupture. Abdominal pregnancy resulting from rupture of interstitial ectopic pregnancy was
diagnosed at surgery and pathology.
WS18
AJR:194, June 2010
Downloaded from www.ajronline.org by 36.80.132.111 on 10/19/15 from IP address 36.80.132.111. Copyright ARRS. For personal use only; all rights reserved
Abdominal Pain in Pregnancy
Fig. 5Ovarian torsion in woman 11 weeks pregnant who presented with 2 days of lower abdominal and pelvic pain.
A, Transverse gray-scale transabdominal ultrasound image through pelvis shows cystic and solid midline mass (arrows). Separate normal right ovary was seen
transvaginally (not shown). Separate left ovary was not seen on transabdominal or transvaginal ultrasound. MRI was performed for further evaluation 1 hour later.
B, Coronal T2-weighted fast spin-echo MR shows enlarged, partially necrotic left ovary (black arrows) and cystic mass arising from left ovary (white arrow) with few
septations in inferior aspect of mass (arrowhead). Left ovary and mass were surgically removed later that day. Pathology results were torsed, necrotic left ovary with
mucinous cystadenocarcinoma of left ovary serving as lead point mass.
nate for torsion, MRI may better show ovarian edema resulting from early or intermittent ovarian torsion [45] (Fig. 6).
Leiomyomas
Uterine leiomyomas are commonly encountered during
pregnancy, with 1 in 500 pregnant women hospitalized for a
leiomyoma-related complication [44]. Approximately half of
all leiomyomas grow during pregnancy, mainly in the first
trimester because of rising estrogen levels [51]. Abdominal
pain and uterine contractions can result from necrosis and
degeneration of leiomyomas secondary to rapid growth.
Red degeneration is the most common type of degeneration during pregnancy and occurs when a leiomyoma outgrows its blood supply with resulting hemorrhage. Such leiomyomas can appear on ultrasound as circumscribed masses
with cystic spaces or heterogeneous echogenicity [51, 52]
Fig. 6Degenerated fibroid in woman 17 weeks pregnant who presented with right-sided abdominal pain.
A and B, Transverse (A) and sagittal (B) transabdominal ultrasound images show exophytic fibroid (straight arrows) extending from right lateral aspect of uterus. Inner
hypoechoic region with low-level echoes (arrowheads) represents cystic degeneration secondary to necrosis. Intrauterine fetal head (curved arrow, A) is seen.
AJR:194, June 2010
WS19
Downloaded from www.ajronline.org by 36.80.132.111 on 10/19/15 from IP address 36.80.132.111. Copyright ARRS. For personal use only; all rights reserved
Woodfield et al.
Fig. 7Ovarian edema in woman 13 weeks pregnant who presented with right lower quadrant pain.
A, Transvaginal ultrasound image with spectral Doppler shows mildly enlarged right ovary (volume = 16.1 cm 3) with arterial flow.
B, Axial T2-weighted single-shot fast spin-echo image from MR examination performed same day as ultrasound (A) shows increased signal intensity of central ovarian
stroma (black arrow) and peripheral displacement of subcentimeter physiologic ovarian follicles (white arrows); these findings are consistent with ovarian edema.
Surgery confirmed right ovarian edema due to compression of right adnexal vessels between enlarging uterus and anterior pelvic wall.
(Fig. 7). Ultrasound can further confirm a degenerating leiomyoma as the source of pain if the patient experiences pain
when the probe is directly placed over the leiomyoma [44].
On MRI, red degeneration of a leiomyoma manifests as peripheral or diffuse high signal intensity on T1-weighted images and corresponding variable signal intensity with or
without a low-signal-intensity rim on T2-weighted images
[48]. Leiomyomas are also the most common solid adnexal
masses in pregnancy [45]. Exophytic leiomyomas have the
potential to torse during pregnancy, causing pain due to loss
of blood supply and rapid necrosis.
mately 1 in 1,500 deliveries [53]. Early diagnosis is important
because a 66% increased incidence of appendiceal perforation during pregnancywith a resulting increased rate of
fetal loss and maternal mortalityhas been reported with
surgical delays greater than 24 hours from the time of symptom onset [53]. Clinically diagnosing appendicitis during
Gastrointestinal Causes
Gastrointestinal causes of pain during pregnancy include
appendicitis and other inflammatory, infectious, and obstructive processes of the bowel. These diseases are neither unique
to nor more common in pregnancy but can be more difficult
to diagnose during pregnancy. The approach to imaging the
bowel of a pregnant patient also differs from that of a nonpregnant patient because ultrasound and MRI are typically
preferred over techniques that impart ionizing radiation such
as radiography and CT.
Appendicitis
Appendicitis is the most common nonobstetric reason for
emergency surgery during pregnancy, occurring in approxi-
WS20
Fig. 8Acute appendicitis in 25-year-old pregnant woman who presented with
right lower quadrant pain. Sagittal gray-scale ultrasound image shows blindending, dilated, tubular structure (arrows) in right lower quadrant containing
ovoid echogenic structure (arrowhead) with posterior acoustic shadowing. Acute
appendicitis with appendicolith was diagnosed at surgery.
AJR:194, June 2010
Downloaded from www.ajronline.org by 36.80.132.111 on 10/19/15 from IP address 36.80.132.111. Copyright ARRS. For personal use only; all rights reserved
Abdominal Pain in Pregnancy
pregnancy is difficult because of multiple factors including,
first, the variable appendiceal position (the appendix is gradually displaced upward during pregnancy); second, limited
physical examination of the gravid abdomen; and, third, the
nonspecificity of symptoms such as nausea, vomiting, guarding, and leukocytosis during pregnancy [2, 3, 54].
The primary options for imaging pregnant patients with
suspected appendicitis are ultrasound, MRI, and CT. Ultrasound is usually the first imaging technique of choice because
of its availability, lack of ionizing radiation, and lack of need
for IV contrast material. The sonographic criteria for diagnosing appendicitis in pregnant patients are the same as in
nonpregnant patients: visualization of a dilated (> 67 mm
in diameter), aperistaltic, noncompressible, and blind-ending
tubular structure arising from the cecum. The outer diameters of both a normal appendix and an inflamed appendix
are known to vary on ultrasound, with reported normal appendix diameters ranging from 2 to 13 mm and inflamed appendix diameters from 6 to 30 mm [55]. Therefore, an appendix with a diameter of between 6 and 7 mm without
additional features of acute inflammation may be considered
indeterminate for appendicitis [56]. Associated findings, such
as appendiceal wall thickening (> 2 mm), appendicoliths, and
surrounding hyperechoic inflamed fat, or hypoechoic fluid
may also be seen sonographically (Fig. 8). However, ultrasound of the appendix is a highly operator-dependent examination that can be further limited by the pregnant body
habitus. Sensitivities ranging from 50% to 100%, specificities ranging from 33% to 92%, accuracies ranging from 73%
to 93%, and negative predictive values ranging from 64% to
88% have been reported for the sonographic diagnosis of appendicitis in the general adult population [5762]. In addition, an elevated or retrocecal appendix may be difficult to
find sonographically and a ruptured appendix may have nonspecific findings on ultrasound. Therefore, a negative ultrasound examination does not exclude the possibility of appendicitis and if there remains high clinical suspicion for
appendicitis (persistent right lower quadrant pain of uncertain cause), additional imaging should be considered [63].
When available, MRI is the next preferred examination
for evaluating the appendix in pregnancy also because of its
lack of ionizing radiation. Recent studies have shown that
MRI can reliably diagnose acute appendicitis during pregnancy with 100% sensitivity and 94% specificity [7, 64].
MR examinations for appendicitis in pregnancy at our institution include an oral contrast preparation (300 mL of
barium sulfate [Readi-CAT 2, E-Z-EM] and 300 mL of ferumoxsil [GastroMARK, AMAG Pharmaceuticals]) started
2 hours before the examination. These agents are used because they are the oral contrast preparations already available in our department for other CT (barium sulfate) and
MR (ferumoxsil) examinations, and this specific negative
oral contrast preparation has been previously described in
the literature as a means of limiting bowel susceptibility
artifact and confirming appendiceal patency [7].
The MR examination then consists of the following sequences: axial, sagittal, and coronal T2-weighted single-shot
fast spin echo (SSFSE), axial T1-weighted dual gradient-echo,
Fig. 9Acute appendicitis in 30-year-old pregnant woman who presented with right lower quadrant pain. Ultrasound findings were normal.
A and B, Axial (A) and sagittal (B) T2-weighted single-shot fast spin-echo MR images reveal dilated (1.2 cm) appendix with high-T2-signal-intensity luminal contents
(straight arrows) due to fluid and adjacent periappendiceal fat stranding and fluid (arrowheads); these findings are indicative of periappendiceal inflammation. Lowsignal-intensity oral contrast material fills cecum (curved arrow, B). Acute appendicitis without perforation was diagnosed at surgery.
AJR:194, June 2010
WS21
Downloaded from www.ajronline.org by 36.80.132.111 on 10/19/15 from IP address 36.80.132.111. Copyright ARRS. For personal use only; all rights reserved
Woodfield et al.
Fig. 10Small-bowel obstruction in 31-year-old pregnant woman who presented with abdominal pain and distention. Patient has history of gastric bypass surgery.
A, Transverse gray-scale ultrasound image of left abdomen shows dilated loop of bowel (arrows).
B, Subsequent axial enhanced CT image through abdomen reveals multiple dilated loops of small bowel with airfluid levels (arrows) and superior mesenteric vein
thrombus (arrowhead). Small-bowel obstruction due to internal hernia was diagnosed at surgery. Hypercoagulability due to pregnancy was implicated as cause of
superior mesenteric vein thrombus.
axial true fast imaging with steady-state precession (FISP),
and axial STIR. The multiplanar T2-weighted SSFSE images
allow imaging of the bowel in a relatively motionless state and
help to confirm the location of the appendix in more than one
plane. The axial T1-weighted gradient-echo images are obtained to help confirm appendiceal patency by showing blooming artifact from air or oral contrast material in the appendix
lumen from out-of-phase to in-phase imaging. The axial true
FISP images also help differentiate high-signal-intensity ad
nexal vessels from the lower signal intensity of a normal appendix, and the axial STIR sequence is used to highlight any
periappendiceal edema or fluid associated with appendicitis.
The largest study to date of MRI for appendicitis in pregnant patients has described the following criteria for diagnosing acute appendicitis in this population: an appendix
diameter of > 7 mm with high-T2-signal-intensity luminal
contents, appendiceal wall thickening (> 2 mm), or periappendiceal fat stranding and fluid [7] (Fig. 9). An appendix
with high-T2-signal-intensity luminal contents and a diameter of between 6 and 7 mm on MRI without associated
wall thickening or periappendiceal inflammatory changes
may be considered indeterminate for appendicitis and warrants close clinical follow-up [7, 65].
Appendicitis can also be readily diagnosed on CT using the
same criteria in pregnant patients as in nonpregnant patients
[12]. CT is generally performed if MRI is unavailable or if
the patient has contraindications to MRI to prevent a delay
in the diagnosis and treatment of a possible appendicitis.
Sensitivities ranging from 72% to 100%, specificities ranging
from 83% to 99%, accuracies ranging from 78% to 98%, and
WS22
negative predictive values ranging from 64% to 99% have
been reported for the CT diagnosis of appendicitis in the general adult population [58, 59, 61, 62, 66].
Infectious Diseases and Inflammatory Bowel Disease
Infection and inflammation of the bowel are additional potential causes of acute abdominal pain during pregnancy. Inflammatory bowel disease has a peak incidence in women of
Fig. 11Hepatic rupture in 28-year-old recently postpartum woman with HELLP
(hemolysis, elevated liver enzymes, low platelet count) syndrome and abdominal
pain. Axial enhanced CT image reveals high-attenuation (52-HU) perihepatic
material (arrows) diagnostic of hemoperitoneum, which was secondary to
hepatic rupture. Note lower-attenuation (8-HU) small bilateral pleural effusions
(arrowheads).
AJR:194, June 2010
Downloaded from www.ajronline.org by 36.80.132.111 on 10/19/15 from IP address 36.80.132.111. Copyright ARRS. For personal use only; all rights reserved
Abdominal Pain in Pregnancy
B
Fig. 12Gallstone pancreatitis in 27-year-old pregnant woman who presented
with right upper quadrant and epigastric pain. Patient had undergone
laparoscopic cholecystectomy 2 years earlier.
A, Coronal thick-slab MR cholangiopancreatography image illustrates mild
dilatation of intrahepatic bile ducts (arrowheads) and moderate dilation of
common bile duct (arrow).
B and C, Axial T2-weighted single-shot fast spin-echo MR images through level
of distal common bile duct (B) and pancreas (C) reveal dependent filling defect
in distal common bile duct (arrowhead, B) and small amount of retroperitoneal
and peripancreatic fluid (arrows, C). This fluid was believed to be secondary to
gallstone-related pancreatitis because patient had elevated serum amylase (1,321
U/L) and lipase (1,015 U/L) levels. Subsequent ERCP with stone extraction resulted
in resolution of patients abdominal pain and normalization of serum amylase
and lipase levels. Common duct stone is not visible on coronal thick-slab MR
cholangiopancreatography image because of volume averaging with high-signalintensity bile.
reproductive age. Disease activity is largely independent of
pregnancy; however, activity during pregnancy is associated
with increased fetal loss rate and fetal growth retardation [3].
Ultrasound is often the first imaging study chosen for evaluating localized or generalized abdominal pain during pregnancy
and may reveal a thick-walled segment of bowel in the setting
of active infection or inflammation [67]. However, cross-sectional imaging is commonly required to evaluate the entire
extent of disease as well as any associated complications such
as bowel obstruction, fistulas, or abscess formation.
Both MRI and CT can show the presence, extent, and
complications of infectious and inflammatory bowel diseases.
MR examinations without or with an oral preparation (MR
enterography) using T2-weighted SSFSE images can readily
depict thick-walled segments of small and large bowel and
associated complications in pregnant patients and nonpregnant patients [65, 68]. Similar to CT, findings of Crohns disease on MRI include segmental bowel wall thickening and
small-bowel involvement. Additional findings such as bowel
stenosis with prestenotic dilatation, fibrofatty proliferation,
increased vascularity of the vasa recta, and mesenteric adenopathy may also be readily depicted on both CT and MRI
AJR:194, June 2010
[69]. The role of MRI in evaluating ulcerative colitis is less
established, but MRI can reportedly show the continuous colonic wall thickening and loss of haustral folds characteristic
of ulcerative colitis [70].
Bowel Obstruction
Bowel obstruction is a third gastrointestinal emergency
that can arise during pregnancy with an incidence of 1 in
2,500 deliveries. Maternal mortality associated with bowel
obstruction is as high as 6% and is most commonly secondary to adhesions [71]. Pregnant patients more commonly
present with bowel obstruction in the third trimester perhaps
because of increased mass effect of the enlarging gravid uterus on the large and small bowel with resulting bowel displacement [72]. Clinically diagnosing bowel obstruction in a pregnant patient can be difficult because the gravid uterus limits
physical examination and because some of the symptoms of
bowel obstruction (abdominal pain, nausea, vomiting) are
also common symptoms of pregnancy. However, the onset of
such symptoms after the first trimester should raise the possibility of other gastrointestinal abnormalities or diseases
such as intestinal obstruction [2].
WS23
Downloaded from www.ajronline.org by 36.80.132.111 on 10/19/15 from IP address 36.80.132.111. Copyright ARRS. For personal use only; all rights reserved
Woodfield et al.
Ultrasound is again often the first imaging study of
choice for evaluating generalized abdominal pain in pregnancy and may show dilated loops of bowel with fluid levels
and aperistalsis with long-standing or high-grade obstruction, but ultrasound does not reliably depict the point or
cause of bowel obstruction. Therefore, cross-sectional imaging with MRI or CT is again often required for further
characterization (Fig. 10). Similar to imaging bowel inflammation or infection, MR studies for bowel obstruction can
be performed with the use of multiplanar T2-weighted
SSFSE imaging and may be performed with or without oral
contrast preparation [73]. If MRI cannot be performed expeditiously or expertise in MR interpretation is not readily
available, CT may be performed because the risk of delayed
diagnosis and treatment of a potential bowel obstruction
may pose a greater risk to the fetus than radiation exposure
from a diagnostic examination.
Hepatobiliary Causes
Two hepatic complications unique to pregnancy that can
present with acute abdominal pain are HELLP (hemolysis,
elevated liver enzymes, low platelet count) syndrome and
acute fatty liver of pregnancy (AFLP). Although pancreatitis is not unique to pregnancy, the approach to imaging
pregnant patients with pancreatitis differs from that of the
nonpregnant patient.
HELLP Syndrome
HELLP syndrome is a rare but serious condition that
most commonly presents in the late third trimester or early
postpartum period in association with severe preeclampsia
or eclampsia. It is estimated that up to 1028% of pre
eclampsia pregnancies are associated with some degree of
HELLP syndrome [3]. Patients with HELLP syndrome
variably present with hemolytic anemia, thrombocytopenia (< 100,000/mm3), and liver function test abnormalities
(elevated lactate dehydrogenase level, > 600 U/L; elevated
bilirubin level, > 1.2 mg/dL; or elevated aspartate amino
transferase level, > 70 U/L) [2]. The deposition of intravascular fibrin deposits in the liver with HELLP syndrome results in various hepatic manifestations ranging from
hepatic congestion and edema to hepatic necrosis, hemorrhage, and rupture, which can require emergent cesarean
delivery, exploratory laparotomy, or hepatic embolization
[74]. The clinical presentation of HELLP syndrome is variable and nonspecific. Patients most commonly present with
abdominal pain and nausea. Patients with severe complications of hepatic rupture and hemorrhage may present with
abdominal pain that radiates to the right upper quadrant
or right shoulder and with hypovolemic shock [3].
The main role of imaging in patients with clinically diagnosed HELLP syndrome is to identify the hepatic complications. Ultrasound, CT, or MRI can be used to assess the
presence and extent of hepatic injury. The selected imaging
WS24
technique will depend on availability, patient stability, and
whether the patient is postpartum. Ultrasound can show
intra- and extrahepatic hematomas and fluid collections.
CT and MR examinations can further reveal the extent of
hepatic damage and can help distinguish among hepatic
edema, necrosis, and hemorrhage [74] (Fig. 11).
Acute Fatty Liver of Pregnancy
AFLP is also a rare but serious hepatic complication unique
to pregnancy that can be fatal. It is characterized by microvascular fatty infiltration of the liver and can result in both
hepatic and renal failure. Patients also typically present in the
late third trimester or early postpartum period with symptoms of abdominal pain, vomiting, and jaundice. Similar to
HELLP syndrome, management of AFLP centers on prompt
delivery and supportive care [3]. AFLP can be difficult to differentiate from HELLP syndrome and preeclampsia or eclampsia clinically. However, histologically HELLP syndrome
and AFLP can be readily differentiated because HELLP syndrome is characterized by periportal hemorrhage, sinusoidal
fibrin deposition, and occasional periportal necrosis, whereas
AFLP is characterized by microvesicular fatty infiltration
with occasional necrosis and inflammation [2].
Imaging with ultrasound, CT, or MRI may also help distinguish between HELLP syndrome and AFLP as well as depict
the extent of hepatic complications. However, in the early
stages of AFLP the liver may appear normal [75]. The imaging of patients with suspected AFLP will depend on technique
availability, patient stability, and pregnancy status. Ultrasound is often the first technique of choice for pregnant and
unstable patients and can reveal diffuse increased heterogeneity and echogenicity of the hepatic echotexture. If the patient
is postpartum, CT is often the first imaging study of choice
and may reveal diffuse decreased hepatic attenuation. The
role of MRI for diagnosing AFLP has not been determined,
but MR examinations performed with T1-weighted dual gradient-echo in-phase and out-of-phase sequences can readily
depict hepatic steatosis by showing loss of hepatic signal intensity from in-phase to out-of-phase images.
Pancreatitis
Pancreatitis is a rare cause of abdominal pain during pregnancy, occurring in 0.11% of pregnancies and occurring most
commonly in the third trimester [3]. In pregnancy, gallstones
are the most common cause of pancreatitis because pregnancy
promotes the formation of sludge and stones within the gallbladder due to increased cholesterol synthesis, bile stasis, and
decreased gallbladder contraction. In addition, higher levels of
maternal estrogen in the third trimester can increase triglyceride synthesis and, in some cases, can induce pancreatitis secondary to hypertriglyceridemia. Increased intraabdominal
pressure on the bile ducts in the third trimester has also been
proposed as a potential reason for the reported increased incidence of pancreatitis in the third trimester [4, 76].
AJR:194, June 2010
Downloaded from www.ajronline.org by 36.80.132.111 on 10/19/15 from IP address 36.80.132.111. Copyright ARRS. For personal use only; all rights reserved
Abdominal Pain in Pregnancy
B
Fig. 13Obstructive hydronephrosis in 23-year-old pregnant woman who
presented with left flank pain.
A, Sagittal gray-scale ultrasound image of left kidney shows mild hydronephrosis
(arrow).
B, Transverse color Doppler ultrasound image through bladder shows right
ureteral jet (arrow) but absence of left ureteral jet. Neither left ureteral calculus
nor dilatation of left ureter was seen sonographically.
C, Subsequent unenhanced CT image reveals 2-mm calculus (arrow) at left
ureterovesical junction.
In the nonpregnant population, contrast-enhanced CT is
usually the study of choice for evaluating complications of
pancreatitis. However, during pregnancy ultrasound can
first be used to search for the cause and complications of
pancreatitis including choledocholithiasis and pseudocyst
formation. If ultrasound is normal or indeterminate, MRI
with multiplanar T2-weighted SSFSE and axial T1-weighted sequences and MR cholangiopancreatography (MRCP)
with heavily T2-weighted sequences can be performed to
confirm the diagnosis of pancreatitis and to search for
causes and complications of pancreatitis (Fig. 12). Screen-
AJR:194, June 2010
ing the biliary tree for possible stones with MRCP can also
help avoid or guide a more invasive ERCP procedure, thus
minimizing maternal and fetal risk and exposure to ionizing
radiation [13].
Genitourinary Causes
Urinary tract causes of pain during pregnancy include
physiologic and obstructive hydronephrosis and infectious
causes such as cystitis and pyelonephritis, which do not usually
require imaging for diagnosis and treatment. The incidence of
urolithiasis is not increased during pregnancy. However, the
WS25
Downloaded from www.ajronline.org by 36.80.132.111 on 10/19/15 from IP address 36.80.132.111. Copyright ARRS. For personal use only; all rights reserved
Woodfield et al.
Fig. 14Obstructive hydronephrosis in 31-year-old pregnant woman who
presented with right flank pain.
A, Sagittal gray-scale ultrasound image of right kidney shows mild hydronephrosis
(arrow). No right-sided perinephric fluid, calculus, ureteral dilatation, or ureteral
jet is seen. Subsequent MR examination of abdomen and pelvis was performed
1 day later to further differentiate between obstructive versus physiologic right
hydronephrosis.
B and C, Coronal T2-weighted single-shot fast spin-echo MR images through
abdomen illustrate moderate right perinephric fluid (arrows, B) and mild right
hydroureteronephrosis (arrows, C) with abrupt termination of dilated right
ureter at level of pelvic rim (arrowhead, C); these findings are suggestive of
obstructive right hydroureteronephrosis. Ureteral calculus was not visible on MR
examination. Patient subsequently passed 3-mm calculus.
approach to imaging urolithiasis and the need to differentiate
between physiologic and obstructive hydronephrosis differs
between pregnant and nonpregnant patients.
Hydronephrosis
Obstructive hydronephrosis typically presents in the second or third trimester and is most commonly caused by urinary tract calculi [13]. Urolithiasis is reportedly detected in
1 in 90 to 1 in 3,800 pregnancies and occurs more commonly
in multipara pregnancies with equal involvement of the
right and left sides [2]. Hospitalization for pain management is often required for pregnant patients with symptomatic urolithiasis, although 7080% of all obstructive calculi
will spontaneously pass with conservative management [2].
WS26
Potential complications of urolithiasis include pyelonephritis and premature labor induced by renal colic with or without concomitant infection.
Physiologic dilatation of the collecting system, which occurs in up to 90% of pregnant patients, can mimic obstructive
hydronephrosis clinically and can delay accurate diagnosis
[2]. Physiologic hydronephrosis is usually asymptomatic, but
it can present with abdominal pain and functional ureteral
obstruction [77]. Physiologic dilatation of the renal pelvis
and ureter, the major pitfall in the assessment of urolithiasis
in pregnant patients, is due to the combination of hormonerelated relaxation of the ureters during pregnancy and extrinsic compression of the ureters by the growing uterus and
engorged ovarian veins against the iliopsoas muscle [2]. It is
AJR:194, June 2010
Downloaded from www.ajronline.org by 36.80.132.111 on 10/19/15 from IP address 36.80.132.111. Copyright ARRS. For personal use only; all rights reserved
Abdominal Pain in Pregnancy
more commonly seen on the right ureter because of relative
protection of the left ureter by the sigmoid colon.
Ultrasound is usually the first imaging technique of
choice for evaluating hydronephrosis and urolithiasis during pregnancy with reported sensitivities for renal and ureteral calculi ranging between 34% and 95% [78, 79]. Ultrasound may directly show calculi or reveal secondary findings
of acute obstruction such as hydronephrosis with perinephric fluid or an absent ureteral jet. The absence of the
ureteral jet on the suspected side of obstruction is reported
to have a sensitivity of 100% and a specificity of 91% for
the diagnosis of obstructive hydronephrosis and indicates
complete obstruction [80] (Fig. 13). However, an absent
ureteral jet has also been reported in approximately 15% of
asymptomatic pregnant women [81]. To decrease false-positive results of absent ureteral jets, patients can be imaged
in the contralateral decubitus position (i.e., left posterior
oblique to visualize the right ureteral jet) to decrease gravid
uterus mass effect on the bladder and ureter. Transvaginal
ultrasound and transverse images through the bladder can
also facilitate detection of distal ureteral calculi.
Using Doppler ultrasound, the intrarenal resistive index
(RI) can be calculated. This value may aid in differentiating
between physiologic hydronephrosis and pathologic hydronephrosis because normal pregnancy does not usually affect
the intrarenal RI; an elevated RI (> 0.70) should be considered abnormal. The elevation in the RI usually occurs within
6 hours after acute obstruction of the collecting system. The
RI as a test for diagnosing obstructive hydronephrosis in
pregnancy has a reported sensitivity, specificity, and accuracy of 45%, 91%, and 87%, respectively. However, a difference of 0.40 or greater between the RIs of the normal kidney
and the abnormal kidney (RI) is reportedly a better indication of obstruction in the kidney with the higher RI [82].
The sensitivity, specificity, and accuracy of RI for diagnosing acute unilateral ureteral obstruction in pregnant women
are reported to be 95%, 100%, and 99%, respectively [82].
Ultrasound has the advantages of being portable and
noninvasive and not exposing the pregnant patient to ionizing radiation or IV contrast material. However, maternal
body wall acoustics, the gravid uterus, and overlying bowel
gas often limit visualization of the ureter. Therefore, a normal or indeterminate renal ultrasound examination may
require additional imaging if there is strong clinical suspicion for urolithiasis.
Further imaging options may depend on the stage of gestation. To limit radiation exposure to the developing fetus,
some authors have suggested a limited IV urography examination consisting of a scout film, 10-minute film, and
minimal number of additional films if the patient is less
than 24 weeks gestation and a low-dose CT examination
using a low-dose renal calculus protocol if the patient is
greater than 24 weeks gestation [83]. The high sensitivity
(> 95%) and specificity (> 98%) of CT for detecting urinary
AJR:194, June 2010
tract calculi as small as 12 mm make CT typically the first
imaging technique of choice in nonpregnant patients and
the second imaging technique of choice in pregnant patients for diagnosing urolithiasis [13].
MR urography (MRU) with T2-weighted imaging has also
been reported to have a high sensitivity for the detection of
urinary tract dilatation and for the identification of the site
of obstruction. MRU can also help differentiate between
physiologic hydronephrosis and obstructive hydronephrosis
[84]. Features of obstructive hydronephrosis with MRI include renal enlargement, perinephric fluid, and an abrupt
change in the caliber of the ureter above or below the uterus
(Fig. 14). In contrast, physiologic hydronephrosis on MRU is
characterized by gradual, smooth tapering of the mid ureter
due to extrinsic compression between the gravid uterus and
iliopsoas muscle [84] (Fig. 15). MRI is also particularly helpful in revealing complications of pyelonephritis. However, it
remains a useful second-line examination largely because of
its limited ability in detecting small calculi and characterizing the exact size and shape of calculi.
Vascular Causes
Vascular causes of abdominal pain that have a higher incidence in pregnancy include venous thromboembolic disease,
gonadal vein dilatation, and splenic artery aneurysm rupture.
Venous Thromboembolic Disease
Both venous stasis and hypercoagulability place pregnant patients at increased risk for venous thrombosis. Venous stasis begins in the first trimester and peaks around 36
weeks of gestation and is likely due to a combination of
progesterone-induced venodilation, pelvic venous compression by the gravid uterus, and pulsatile compression of the
left iliac vein by the right iliac artery [85]. The hypercoagulable state of pregnancy results from the fact that the hemostatic system is progressively activated to prepare the
patient for the hemostatic challenge of delivery.
Most venous thromboembolic events occur in the lower
extremities. However, pregnant patients are also at increased risk for pelvic, hepatic (Budd-Chiari syndrome),
mesenteric, and gonadal venous thrombi. Mesenteric venous thrombosis is particularly ominous because it can result in bowel infarction and because it is difficult to diagnose given that patients typically present with insidious
onset of poorly localized abdominal pain and nonspecific
findings on physical examination [3]. Color Doppler ultrasound can diagnose hepatic thrombosis or occlusion, but
the role of ultrasound for the diagnosis of pelvic, mesenteric, and gonadal venous thrombosis is limited. MRI or
contrast-enhanced CT can diagnose abdominal and pelvic
venous thrombosis (Fig. 10B). In the pregnant patient, depending on institution experience and MR availability, MR
venography (MRV) may be the preferred imaging test because MRV avoids the use of radiation and can be per-
WS27
Downloaded from www.ajronline.org by 36.80.132.111 on 10/19/15 from IP address 36.80.132.111. Copyright ARRS. For personal use only; all rights reserved
Woodfield et al.
Fig. 15Physiologic hydronephrosis in 22-year-old pregnant woman who
presented with persistent right flank pain radiating inferiorly. Sagittal T2weighted single-shot fast spin-echo MR image through abdomen and pelvis
shows mild dilatation of right ureter with gradual, smooth tapering of distal ureter
(arrow) between posterior gravid uterus and iliopsoas muscle. These findings
are consistent with physiologic hydronephrosis, which is normal finding of
pregnancy that can cause abdominal pain and can be confused with obstructive
hydronephrosis.
Fig. 16Gonadal vein syndrome in 27-year-old pregnant woman who presented
with right-sided abdominal pain. Axial time-of-flight MR image shows patent but
dilated gonadal veins, with dilatation of right (long arrow) being greater than left
(short arrow) vein. Given that no other reason for abdominal pain was evident
on MR examination or clinically, patients pain was attributed to dilatation of
right gonadal vein. Also note patency but compression of inferior vena cava
(arrowhead) by gravid uterus.
formed without the use of IV contrast material. Both timeof-flight and true FISP MR sequences can detect flow and
depict thrombus in abdominal and pelvic vessels. However,
unenhanced sequences can be limited by flow signal artifacts [86]. Treatment of thromboembolic disease during
pregnancy requires systemic anticoagulation therapy.
Splenic Artery Aneurysm
Pregnancy is a major risk factor for the rupture of a splenic
artery aneurysm, particularly in the third trimester or during
labor. It has been theorized that hormonal changes during
pregnancy alter the elastic properties of the arterial wall [88].
Splenic artery aneurysms are usually asymptomatic but can
occasionally present as vague epigastric or left upper quadrant
pain. If a splenic artery aneurysm ruptures, it can be a catastrophic event associated with both maternal and fetal mortality. Therefore, if a splenic artery aneurysm is detected incidentally in a woman of child-bearing age, elective treatment
with splenectomy, artery resection, aneurysm exclusion, or
aneurysm embolization is recommended even if the patient is
asymptomatic [3, 89]. Splenic artery aneurysms can be detected on abdominal ultrasound, CT, or MRI.
Gonadal Vein Syndrome
Enlargement of the right gonadal vein in the late second
and third trimesters of pregnancy has also been reported as
a potential cause of abdominal pain [65]. Dilatation of the
gonadal vein itself or the resulting extrinsic compression of
the ureter by the enlarged gonadal vein has been referred to
as right ovarian vein syndrome [65]. Rarely, subsequent
rupture of the dilated right ovarian vein during pregnancy
has been described [87]. Right ovarian vein dilatation is likely a diagnosis of exclusion when it is the only finding on ultrasound, MRI, or CT to account for a pregnant patients
right-sided pain (Fig. 16).
WS28
References
1. Firstenberg MS, Malangoni MA. Gastrointestinal surgery during pregnancy.
Gastroenterol Clin North Am 1998; 27:7388
2. Mayer IE, Hussain H. Abdominal pain in pregnancy. Gastroenterol Clin North
AJR:194, June 2010
Downloaded from www.ajronline.org by 36.80.132.111 on 10/19/15 from IP address 36.80.132.111. Copyright ARRS. For personal use only; all rights reserved
Abdominal Pain in Pregnancy
Am 1998; 27:136
3. Cappell MS, Friedel D. Abdominal pain during pregnancy. Gastroenterol Clin
North Am 2003; 32:158
4. Sharp HT. The acute abdomen during pregnancy. Clin Obstet Gynecol 2002;
45:405413
5. Melnick DM, Wahl WL, Dalton VK. Management of general surgical problems in the pregnant patient. Am J Surg 2004; 187:170180
6. Oto A, Ernst RD, Shah R, et al. Right lower quadrant pain and suspected appendicitis in pregnant women: evaluation with MR imaging: initial experience.
Radiology 2005; 234:445451
7. Pedrosa I, Levine D, Eyvazzadeh AD, Siewert B, Ngo L, Rofsky NM. MR
imaging of acute appendicitis in pregnancy. Radiology 2006; 238:891899
8. Birchard KR, Brown MA, Hyslop WB, Firat Z, Semelka RC. MRI of acute
abdominal and pelvic pain in pregnant patients. AJR 2005; 184:452458
9. Kanal E, Barkovich AJ, Bell C, et al.; ACR Blue Ribbon Panel on MR Safety. ACR
guidance document for safe MR practices: 2007. AJR 2007; 188:14471474
10. American College of Radiology Website. ACR practice guideline for imaging
pregnant or potentially pregnant adolescents and women with ionizing radiation. www.acr.org/SecondaryMainMenuCategories/quality_safety/guidelines/
dx/Pregnancy.aspx. Published 2008. Accessed on February 21, 2010
11. Sudah M, Vanninen RL, Partanen K, et al. Patients with acute flank pain: comparison of MR urography with unenhanced helical CT. Radiology 2002;
223:98105
12. Lazarus E, Mayo-Smith WW, Mainiero MB, Spencer PK. CT in the evaluation of
nontraumatic abdominal pain in pregnant women. Radiology 2007; 244:784790
13. Patel SJ, Reede DL, Katz DS, Subramaniam R, Amorosa JK. Imaging the pregnant patient for nonobstetric conditions: algorithms and radiation dose considerations. RadioGraphics 2007; 27:17051722
14. Rodesch F, Camus M, Ermans AM, Dodion J, Delange F. Adverse effect of
amniofetography on fetal thyroid function. Am J Obstet Gynecol 1976;
126:723726
15. Atwell TD, Lteif AN, Brown DL, et al. Neonatal thyroid function after administration of IV iodinated contrast agent to 21 pregnant patients. AJR 2008;
191:268271
16. American College of Radiology Website. Manual on contrast media. www.acr.
org/SecondaryMainMenuCategories/qualitysafety/contrast_manual.aspx. Published 2008. Accessed February 22, 2010
17. Wilcox AJ, Weinberg CR, OConner JF, et al. Incidence of early loss of pregnancy. N Engl J Med 1988; 319:189194
18. Laing FC, Frates MC, Benson CB. Ultrasound evaluation during the first trimester of pregnancy. In: Callen PW, ed. Ultrasonography in obstetrics and
gynecology, 5th ed. Philadelphia, PA: Saunders, 2008:181224
19. Rowling SE, Langer JE, Coleman BG, et al. Sonography during early pregnancy: dependence of threshold and discriminatory values on transvaginal
transducer frequency. AJR 1999; 172:983988
20. Levi CS, Lyons EA, Lindsay DJ. Early diagnosis of nonviable pregnancy with
endovaginal US. Radiology 1988; 167:383385
21. Rowling SE, Coleman BG, Langer JE, et al. First-trimester US parameters of
failed pregnancy. Radiology 1997; 203:211217
22. Nyberg DA, Laing FC, Filly RA. Threatened abortion: sonographic distinction
of normal and abnormal gestation sacs. Radiology 1986; 158:397400
23. Doubilet PM, Benson CB. Embryonic heart rate in the early first trimester:
what rate is normal? J Ultrasound Med 1995; 14:431434
24. Bree RL, Edwards M, Bhm-Velz M, Beyler S, Roberts J, Mendelson EB.
Transvaginal sonography in the evaluation of normal early pregnancy: correlation with HCG level. AJR 1989; 153:75
25. Centers for Disease Control and Prevention (CDC). Current Trends Ectopic
Pregnancy: United States, 19901992. MMWR 1995; 44:4648
26. Maymon R, Shulman A. Controversies and problems in the current management of tubal pregnancy. Hum Reprod Update 1996; 2:541551
27. Clayton HB, Schieve LA, Peterson HB, et al. Ectopic pregnancy risk with assisted reproductive technology procedures. Obstet Gynecol 2006; 107:595
604
28. Fernandez H, Gervaise A. Ectopic pregnancies after infertility treatment: modern diagnosis and therapeutic strategy. Hum Reprod Update 2004; 10:503513
AJR:194, June 2010
29. Goldman GA, Fisch B, Ovadia J, Tadir Y. Heterotopic pregnancy after assisted
reproductive technologies. Obstet Gynecol Surv 1992; 47:217221
30. Brown DL, Doubilet PM. Transvaginal sonography for diagnosing ectopic
pregnancy: positivity criteria and performance characteristics. J Ultrasound
Med 1994; 13:259266
31. Nyberg DA, Mack LA, Jeffrey RB Jr, Laing FC. Endovaginal sonographic evaluation of ectopic pregnancy: a prospective study. AJR 1987; 149:11811186
32. Cacciatore B. Can the status of tubal pregnancy be predicted with transvaginal
sonography? A prospective comparison of sonographic, surgical, and serum
hCG findings. Radiology 1990; 177:481484
33. Nyberg DA, Hughes MP, Mack LA, Wang KY. Extrauterine findings of ectopic
pregnancy at transvaginal US: importance of echogenic fluid. Radiology 1991;
178:823826
34. Jung SE, Byun JY, Lee JM, et al. MR imaging of maternal diseases in pregnancy. AJR 2001; 177:12931300
35. Nyberg DA, Mach LA, Benedetti TJ, Cyr DR, Schuman WP. Placental abruption and placental hemorrhage: correlation of sonographic findings with fetal
outcome. Radiology 1987; 164:357361
36. Nyberg DA, Cyr DR, Mack LA, Wilson DA, Shuman WP. Sonographic spectrum of placental abruption. AJR 1987; 148:161164
37. Trop I, Levine D. Hemorrhage during pregnancy: sonography and MR imaging. AJR 2001; 176:607615
38. Iams JD, Goldenberg RL, Meis PJ, et al. The length of the cervix and the risk
of spontaneous premature delivery: National Institute of Child Health and Human Development Maternal Fetal Medicine Unit Network. N Engl J Med 1996;
334:567572
39. Hibbard JU, Tart M, Moawad AH. Cervical length at 1622 weeks gestation
and risk for preterm delivery. Obstet Gynecol 2000; 96:972978
40. Murakawa H, Utumi T, Hasegawa I, Tanaka K, Fuzimori R. Evaluation of
threatened preterm delivery by transvaginal ultrasonographic measurement of
cervical length. Obstet Gynecol 1993; 82:829832
41. Rooholamini SA, Au AH, Hansen GC, et al. Imaging of pregnancy-related
complications. RadioGraphics 1993; 13:753770
42. Schmeler KM, Mayo-Smith WW, Peipert JF, et al. Adnexal masses in pregnancy:
surgery compared with observation. Obstet Gynecol 2005; 105:10981103
43. Chang HC, Bhatt S, Dogra VS. Pearls and pitfalls in diagnosis of ovarian torsion. RadioGraphics 2008; 28:13551368
44. Eyvazzadeh AD, Levine D. Imaging of pelvic pain in the first trimester of pregnancy. Radiol Clin North Am 2006; 44:863877
45. Chiang G, Levine D. Imaging of adnexal masses in pregnancy. J Ultrasound
Med 2004; 23:805819
46. Bromley B, Benaccerraf B. Adnexal masses during pregnancy: accuracy of
sonographic diagnosis and outcome. J Ultrasound Med 1997; 16:447452
47. Ribic-Pucelj M, Kobal B, Peternelj-Marinsek S. Surgical treatment of adnexal
masses in pregnancy: indications, surgical approach and pregnancy outcome. J
Reprod Med 2007; 52:273279
48. Smorgick N, Pansky M, Feingold M, et al. The clinical characteristics and
sonographic findings of maternal ovarian torsion in pregnancy. Fertil Steril
2009; 92:19831987; Epub Nov. 5, 2008
49. Stark JE, Siegel MJ. Ovarian torsion in prepubertal and pubertal girls: sonographic findings. AJR 1994; 163:14791482
50. Rosado WM Jr, Trambert MA, Gosink BB, Pretorius DH. Adnexal torsion:
diagnosis by using Doppler sonography. AJR 1992; 159:12511253
51. Lev-Toaff AS, Coleman BG, Arger PH, et al. Leiomyomas in pregnancy: sonographic study. Radiology 1987; 164:375380
52. Kawakami S, Togashi K, Konishi I, et al. Red degeneration of uterine leiomyoma: MR appearance. J Comput Assist Tomogr 1994; 18:925928
53. Tamir IL, Bongard FS, Klein SR. Acute appendicitis in the pregnant patient.
Am J Surg 1990; 160:571576
54. Oto A, Srinivasan PN, Ernst RD, et al. Revisiting MRI for appendix location
during pregnancy. AJR 2006; 186:883887
55. Rettenbacher T, Hollerweger A, Macheiner P, et al. Outer diameter of the vermiform appendix as a sign of acute appendicitis: evaluation at US. Radiology
2001; 218:757762
56. Jeffrey RB, Jain KA, Nghiem HV. Sonographic diagnosis of acute appendicitis:
WS29
Downloaded from www.ajronline.org by 36.80.132.111 on 10/19/15 from IP address 36.80.132.111. Copyright ARRS. For personal use only; all rights reserved
Woodfield et al.
interpretive pitfalls. AJR 1994; 162:5559
57. Lim HK, Bae SH, Seo GS. Diagnosis of acute appendicitis in pregnant women:
value of sonography. AJR 1992; 159:539542
58. Wise SW, Labuski MR, Kasales CJ, et al. Comparative assessment of CT and
sonographic techniques for appendiceal imaging. AJR 2001; 176:933941
59. Johansson EP, Rydh A, Riklund KA. Ultrasound, computed tomography, and laboratory findings in the diagnosis of appendicitis. Acta Radiol 2007; 48:267273
60. Israel GM, Malguria N, McCarthy S, Copel J, Weinreb J. MRI vs ultrasound
for suspected appendicitis during pregnancy. J Magn Reson Imaging 2008;
28:428433
61. Poortman P, Lohle PN, Schoemaker CM, et al. Comparison of CT and sonography in the diagnosis of acute appendicitis: a blinded prospective study. AJR
2003; 181:13551359
62. Gaitini D, Beck-Razi N, Mor-Yosef D, et al. Diagnosing acute appendicitis in
adults: accuracy of color Doppler sonography and MDCT compared with surgery and clinical follow-up. AJR 2008; 190:13001306
63. Mourad J, Elliott JP, Erickson L, Lisboa L. Appendicitis in pregnancy: new
information that contradicts long-held clinical beliefs. Am J Obstet Gynecol
2000; 182:10271029
64. Cobben LP, Groot I, Haans L, Blickman JG, Puylaert J. MRI for clinically
suspected appendicitis during pregnancy. AJR 2004; 183:671675
65. Pedrosa I, Zeikus EA, Levine D, et al. MR imaging of acute right lower quadrant pain in pregnant patients and nonpregnant patients. RadioGraphics 2007;
27:721753
66. Raman SS, Lu DS, Kadell BM, Vodopich DJ, Sayre J, Cryer H. Accuracy of
nonfocused helical CT for the diagnosis of acute appendicitis: a 5-year review.
AJR 2002; 178:13191325
67. Worlicek H, Lutz H, Heyder N, Matek W. Ultrasound findings in Crohns disease
and ulcerative colitis: a prospective study. J Clin Ultrasound 1987; 15:153163
68. Haggett PJ, Moore NR, Shearman JD, Travis SP, Jewell DP, Mortensen NJ.
Pelvic and perineal complications of Crohns disease: assessment using magnetic resonance imaging. Gut 1995; 36:407410
69. Furukawa A, Saotome T, Yamasaki M, et al. Cross-sectional imaging in Crohn
disease. RadioGraphics 2004; 24:689702
70. Maccioni F, Colaiacomo MC, Parlanti S. Ulcerative colitis: value of MR imaging. Abdom Imaging 2005; 30:584592
71. Perdue PW, Johnson HW Jr, Stafford PW. Intestinal obstruction complicating
pregnancy. Am J Surg 1992; 164:384388
72. Davis MR, Bohon CJ. Intestinal obstruction in pregnancy. Clin Obstet Gynecol
1983; 26:832842
73. Regan F, Beall DP, Bohlman ME, Khazan R, Sufi A, Schaefer DC. Fast MR imaging and the detection of small-bowel obstruction. AJR 1998; 170:14651469
74. Nunes JO, Turner MA, Fulcher AS. Abdominal imaging features of HELLP
syndrome: a 10-year retrospective review. AJR 2005; 185:12051210
75. Castro MA, Ouzounian JG, Colletti PM, Shaw KJ, Stein SM, Goodwin TM.
Radiologic studies in acute fatty liver of pregnancy: a review of the literature
and 19 new cases. J Reprod Med 1996; 41:839843
76. Bzowej NH. Gastrointestinal complications of pregnancy. In: Grendell JH,
Friedman SL, McQuaid KR, eds. Current diagnosis & treatment in gastroenterology. New York, NY: McGraw-Hill, 2003:183185
77. Puskar D, Balagovic I, Filipovic A, et al. Symptomatic physiologic hydronephrosis in
pregnancy: incidence, complications and treatment. Eur Urol 2001; 39:260263
78. Parulkar BG, Hopkins TB, Wollin MR, Howard PJ, Lal A. Renal colic during
pregnancy: a case for conservative treatment. J Urol 1998; 159:365368
79. Stothers L, Lee LM. Renal colic in pregnancy. J Urol 1992; 148:13831387
80. Deyoe LA, Cronan JJ, Breslaw BH, Ridlen MS. New techniques of ultrasound
and color Doppler in the prospective evaluation of acute renal obstruction: do
they replace the intravenous urogram? Abdom Imaging 1995; 20:5863
81. Wachsberg RH. Unilateral absence of ureteral jets in the third trimester of pregnancy: pitfall in color Doppler US diagnosis of urinary obstruction. Radiology
1998; 209:279281
82. Shokeir AA, Mahran MR, Abdulmaaboud M. Renal colic in pregnant women:
role of renal resistive index. Urology 2000; 55:344347
83. Fielding JR, Washburn D. Imaging the pregnant patient: a uniform approach. J
Womens Imaging 2005; 7:1621
84. Spencer JA, Chahal R, Kelly A, Taylor K, Eardley I, Lloyd SN. Evaluation of
painful hydronephrosis in pregnancy: magnetic resonance urographic patterns in
physiologic dilatation versus calculus obstruction. J Urol 2004; 171:256260
85. Greer IA. Thrombosis in pregnancy: maternal and fetal issues. Lancet 1999;
353:12581265
86. Nagayama M, Watanabe Y, Okumura A, Amoh Y, Nakashita S, Dodo Y. Fast
MR imaging in obstetrics. RadioGraphics 2002; 22:563580
87. Renuka T, Dhaliwal LK, Gupta I. Hemorrhage from ruptured utero-ovarian
veins during pregnancy. Int J Gynaecol Obstet 1998; 60:167168
88. Stanley JC, Fry WJ. Pathogenesis and clinical significance of splenic artery
aneurysms. Surgery 1974; 76:898909
89. Parangi S, Levine D, Henry A, Isakovich N, Pories S. Surgical gastrointestinal
disorders during pregnancy. Am J Surg 2007; 193:223232
F O R YO U R I N F O R M AT I O N
The readers attention is directed to the Self-Assessment-Module for this article,
which appears on page S42.
WS30
AJR:194, June 2010
Das könnte Ihnen auch gefallen
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5795)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Indivior PLC Presents at Morgan Stanley 19th Annual Global Healthcare Conference, Sep-13-2021 09 - 30 AMDokument12 SeitenIndivior PLC Presents at Morgan Stanley 19th Annual Global Healthcare Conference, Sep-13-2021 09 - 30 AMKing KingssonNoch keine Bewertungen
- Post Partum Ischemic Stroke About A CaseDokument2 SeitenPost Partum Ischemic Stroke About A CaseInternational Journal of Innovative Science and Research TechnologyNoch keine Bewertungen
- English 3 w5Dokument6 SeitenEnglish 3 w5Almie Adarayan BrosotoNoch keine Bewertungen
- MAPEH 8 QUESTI0NNAIRE 2nd QuarterDokument2 SeitenMAPEH 8 QUESTI0NNAIRE 2nd QuarterRhea Mae Onyot JumaritoNoch keine Bewertungen
- Injection Moulding TechniqueDokument14 SeitenInjection Moulding Techniquedrpooja.kaloniyaNoch keine Bewertungen
- LETTERSDokument4 SeitenLETTERSTisha RobbinsNoch keine Bewertungen
- Samms Vaughan2017Dokument9 SeitenSamms Vaughan2017Jose Alonso Aguilar ValeraNoch keine Bewertungen
- MHP 1Dokument3 SeitenMHP 1Asna anwerNoch keine Bewertungen
- Same-Day Sequential Cataract Surgery: Steve A. Arshinoff and Silvia OdorcicDokument10 SeitenSame-Day Sequential Cataract Surgery: Steve A. Arshinoff and Silvia OdorcicBenjamin NgNoch keine Bewertungen
- Urinary Tract InfectionDokument50 SeitenUrinary Tract InfectionJanuaryNoch keine Bewertungen
- EAPP Quarter 1 Week 3 ModuleDokument14 SeitenEAPP Quarter 1 Week 3 ModuleChool Cydrick B. BascosNoch keine Bewertungen
- DLL Mapeh g4 q2 w3Dokument6 SeitenDLL Mapeh g4 q2 w3Daniel MingoyNoch keine Bewertungen
- Roiger Bullock AP2e PPT Chapter01Dokument83 SeitenRoiger Bullock AP2e PPT Chapter01Jemuel Harel M. FloridaNoch keine Bewertungen
- Laminates AND Veneers: Dr. Sakshi Rawal Department of Prosthodontics MDS II YearDokument76 SeitenLaminates AND Veneers: Dr. Sakshi Rawal Department of Prosthodontics MDS II Yearsapna100% (2)
- Acute PainDokument4 SeitenAcute PainCuttie Anne GalangNoch keine Bewertungen
- Chronic Interstitial Nephritis in Agricultural.20Dokument8 SeitenChronic Interstitial Nephritis in Agricultural.20corazones.232.mgNoch keine Bewertungen
- Lucid Dreaming - Lucid Dreams - A Beginner's Guide On How To Control Your Dreams With Different Techniques PDFDokument127 SeitenLucid Dreaming - Lucid Dreams - A Beginner's Guide On How To Control Your Dreams With Different Techniques PDFMargarita Petrova50% (2)
- 11 Ways Women's Heart Attacks Are Different From Men'sDokument25 Seiten11 Ways Women's Heart Attacks Are Different From Men'sSri KondabattulaNoch keine Bewertungen
- Pengelolaan Penyakit Diabetes Mellitus Pada Saat Pandemi Covid-19Dokument10 SeitenPengelolaan Penyakit Diabetes Mellitus Pada Saat Pandemi Covid-19Musdari RiantoNoch keine Bewertungen
- Chole CystitisDokument1 SeiteChole CystitisEirah Nicole JumawanNoch keine Bewertungen
- Fish and Shell Fish Immunology: Full Length ArticleDokument9 SeitenFish and Shell Fish Immunology: Full Length ArticleKirana Rahmada SafitriNoch keine Bewertungen
- Ebook PDF Core Curriculum For Oncology Nursing 5th Edition PDFDokument41 SeitenEbook PDF Core Curriculum For Oncology Nursing 5th Edition PDFcarla.shurtliff473100% (40)
- 19BMS134 - Divyajeet Singh'Dokument63 Seiten19BMS134 - Divyajeet Singh'Divyajeet SinghNoch keine Bewertungen
- 13 - Isolate An Individual Species From A Mixed Culture of Bacteria Using Streak PlatingDokument1 Seite13 - Isolate An Individual Species From A Mixed Culture of Bacteria Using Streak PlatingImogenNoch keine Bewertungen
- TPS 2020 Bahasa InggrisDokument9 SeitenTPS 2020 Bahasa InggrisYopi Panca YudhaNoch keine Bewertungen
- Tahun Nomor NamaDokument18 SeitenTahun Nomor NamaALDO STEFANUZ (STIK)Noch keine Bewertungen
- Chapter 2Dokument2 SeitenChapter 2Castro RicNoch keine Bewertungen
- Tersano and Deposon PathogenSummarySheetDokument2 SeitenTersano and Deposon PathogenSummarySheetNikhil C me18s303Noch keine Bewertungen
- A Collaborative Retrospective Study On The Efficacy and Safety of Intravitreal Dexamethasone Implant (Ozurdex) in Patients With Diabetic Macular EdemaDokument17 SeitenA Collaborative Retrospective Study On The Efficacy and Safety of Intravitreal Dexamethasone Implant (Ozurdex) in Patients With Diabetic Macular EdemaJosé Díaz OficialNoch keine Bewertungen
- Anemia: Clinical Approach and Management: Dairion Gatot, Savita Handayani, Heny Syahrini, Andri MardiaDokument22 SeitenAnemia: Clinical Approach and Management: Dairion Gatot, Savita Handayani, Heny Syahrini, Andri MardiarubyniNoch keine Bewertungen