Beruflich Dokumente
Kultur Dokumente
Jurnal Risperidone PDF
Hochgeladen von
Chairizal Meiristica YanhaOriginalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Jurnal Risperidone PDF
Hochgeladen von
Chairizal Meiristica YanhaCopyright:
Verfügbare Formate
The
n e w e ng l a n d j o u r na l
of
m e dic i n e
original article
Long-Acting Risperidone and Oral
Antipsychotics in Unstable Schizophrenia
Robert A. Rosenheck, M.D., John H. Krystal, M.D., Robert Lew, Ph.D.,
Paul G. Barnett, Ph.D., Louis Fiore, M.D., M.P.H., Danielle Valley, M.P.H.,
Soe Soe Thwin, Ph.D., Julia E. Vertrees, Pharm.D.,
and Matthew H. Liang, M.D., M.P.H., for the CSP555 Research Group*
A bs t r ac t
Background
From the Veterans Affairs (VA) New England Mental Illness, Research Education
and Clinical Center, VA Connecticut
Healthcare System, West Haven, and the
Yale School of Medicine, New Haven, CT
(R.A.R., J.H.K.); the Massachusetts Veterans Epidemiology and Research Information Center VA Cooperative Studies Program Coordinating Center, Boston (R.L.,
L.F., D.V., S.S.T., M.H.L.); the VA Health
Economics Resource Center, Menlo Park,
CA (P.G.B.); and the VA Cooperative
Studies Program Clinical Research Pharmacy Coordinating Center, Albuquerque,
NM (J.E.V.). Address reprint requests to
Dr. Rosenheck at the VA New England
Mental Illness, Research Education and
Clinical Center, VA Connecticut Healthcare System/151D, 950 Campbell Ave.,
West Haven, CT 06516, or at robert
.rosenheck@va.gov.
* The Cooperative Studies Program (CSP)
555 Research Group investigators are
listed in the Supplementary Appendix,
available at NEJM.org.
This article (10.1056/NEJMoa1005987)
was updated on March 7, 2011, at NEJM
.org.
N Engl J Med 2011;364:842-51.
Copyright 2011 Massachusetts Medical Society.
Long-acting injectable risperidone, a second-generation antipsychotic agent, may
improve adherence to treatment and outcomes in schizophrenia, but it has not been
tested in a long-term randomized trial involving patients with unstable disease.
Methods
We randomly assigned patients in the Veterans Affairs (VA) system who had schizophrenia or schizoaffective disorder and who had been hospitalized within the previous 2 years or were at imminent risk for hospitalization to 25 to 50 mg of longacting injectable risperidone every two weeks or to a psychiatrists choice of an oral
antipsychotic. All patients were followed for up to 2 years. The primary end point
was hospitalization in a VA or non-VA psychiatric hospital. Symptoms, quality of life,
and functioning were assessed in blinded videoconference interviews.
Results
Of 369 participants, 40% were hospitalized at randomization, 55% were hospitalized within the previous 2 years, and 5% were at risk for hospitalization. The rate of
hospitalization after randomization was not significantly lower among patients who
received long-acting injectable risperidone than among those who received oral antipsychotics (39% after 10.8 months vs. 45% after 11.3 months; hazard ratio, 0.87;
95% confidence interval, 0.63 to 1.20). Psychiatric symptoms, quality of life, scores
on the Personal and Social Performance scale of global functioning, and neurologic side effects were not significantly improved with long-acting injectable risperidone as compared with control treatments. Patients who received long-acting
injectable risperidone reported more adverse events at the injection site and more
extrapyramidal symptoms.
Conclusions
Long-acting injectable risperidone was not superior to a psychiatrists choice of oral
treatment in patients with schizophrenia and schizoaffective disorder who were
hospitalized or at high risk for hospitalization, and it was associated with more local
injection-site and extrapyramidal adverse effects. (Supported by the VA Cooperative
Studies Program and Ortho-McNeil Janssen Scientific Affairs; ClinicalTrials.gov
number, NCT00132314.)
842
n engl j med 364;9 nejm.org march 3, 2011
The New England Journal of Medicine
Downloaded from nejm.org on September 9, 2015. For personal use only. No other uses without permission.
Copyright 2011 Massachusetts Medical Society. All rights reserved.
Long-Acting Risperidone in schizophrenia
he most common and potentially
remediable cause of treatment failure in
patients with schizophrenia is lack of adherence to prescribed oral medications.1,2 By ensuring sustained levels of drug in the blood,
long-acting injectable delivery may improve adherence and symptom control and reduce the rate of
relapse and hospitalization.2-5
In the United States, the first second-generation
antipsychotic agent to be made available in a longacting injectable delivery system was risperidone
(Risperdal Consta, Ortho-McNeil Janssen). Longacting injectable risperidone may cause fewer
extrapyramidal symptoms than the long-acting
injectable first-generation antipsychotic agents.6
A randomized trial showed the efficacy of
long-acting injectable risperidone over placebo
in patients with schizophrenia,7 and before-andafter studies have shown tolerability in switching
from oral to long-acting injectable risperidone,
with improved symptoms and reduced hospital
use.8-11 These studies involved clinically stable
patients and lacked randomized control groups.
Three randomized trials that also involved patients with stable disease showed no advantage
of long-acting injectable risperidone therapy over
oral treatment.12-14
In this trial involving patients with unstable
disease, we hypothesized that long-acting injectable risperidone would be superior in reducing
the risk of hospitalization for up to 2 years as
compared with a psychiatrists choice of an oral
antipsychotic.
Me thods
Participants
Patients were eligible to participate in the study
if they were 18 years of age or older, had a diagnosis of schizophrenia or schizoaffective disorder as assessed with the use of the Structured
Clinical Interview based on the fourth edition of
the Diagnostic and Statistical Manual of Mental Disorders,15 and were at risk for psychiatric hospitalization as evidenced by current psychiatric hospitalization, hospitalization in the previous 2 years,
or increased use of mental health services to prevent relapse as adjudicated by the study chairpersons (the first two authors). The original entry
criteria required hospitalization in the previous
year but were extended to enhance recruitment
(see the study protocol, available with the full text
of this article at NEJM.org).
Randomization began in September 2006, and
data collection continued for 3 years, with 209
of 369 patients (56.6%) randomly assigned in the
first year, 140 patients (37.9%) assigned in the
second year, and 20 patients (5.4%) assigned
during the first 3 months of the third year.
Follow-up continued for up to 2 years.
Exclusion criteria were the following: detoxification in the previous month; reported past
intolerance to risperidone or intramuscular injections; current treatment with long-acting injectable antipsychotics, oral clozapine, warfarin, or
a combination of these agents; serious medical
conditions; unstable living arrangements; and a
history of assault or suicidal behavior requiring
urgent intervention.
The patients decisional capacity was assessed
with the use of the MacArthur Competence Assessment Tool.16 Guardian consent was allowed.
Subjects received payment for their travel expenses and time: $25 for monthly and injectiononly visits and $45 for extended quarterly assessment visits. The injectable-risperidone group thus
had more planned paid visits than the oral-antipsychotic group. After written informed consent
had been obtained from the patient or guardian,
testing for allergic reactions was performed with
an oral test dose of 1 mg of risperidone. Longacting injectable risperidone was provided free
of charge by Ortho-McNeil Janssen Scientific Affairs, which had no role in the study.
The study and consent forms were approved
by the institutional review boards of the 19 collaborating centers. The analyses were conducted
at the Veterans Affairs (VA) Cooperative Studies
Program Coordinating Center, Boston, and the VA
Health Economics Resource Center, Menlo Park,
California. All authors designed the trial, interpreted the findings, agreed to publication of the
manuscript, and reviewed and approved the manuscript. The first author wrote the first draft of
the manuscript. All authors vouch for the completeness and accuracy of the data, the data
analyses, and the fidelity of this report to the
study protocol.
Randomization
Randomization was conducted centrally and stratified according to site because of potential practice differences. Randomization was conducted
with the use of randomly permuted blocks of
variable size to ensure an approximate balance
over time.
n engl j med 364;9 nejm.org march 3, 2011
The New England Journal of Medicine
Downloaded from nejm.org on September 9, 2015. For personal use only. No other uses without permission.
Copyright 2011 Massachusetts Medical Society. All rights reserved.
843
The
n e w e ng l a n d j o u r na l
Treatment Groups
m e dic i n e
Patients randomly assigned to long-acting injectable risperidone were seen clinically by a study
nurse every 2 weeks for the first month and then
monthly. All patients were seen monthly by their
psychiatrist and by the nurse. On the basis of
consensus guidelines,17 long-acting injectable risperidone was administered intramuscularly at an
initial dose of 25 mg every 2 weeks. Dosage increments of 12.5 mg were permitted every 4 weeks
at the discretion of the treating psychiatrist, up
to the maximum approved dose of 50 mg.
Steady-state drug levels are reached 6 to 8 weeks
after initiation of treatment with long-acting
injectable risperidone,17 and efforts to reduce
the use of oral antipsychotics subsequently were
encouraged in the injectable-risperidone group.
Previous oral antipsychotics were to be continued
for at least 3 weeks. Treatment interruptions
among patients randomly assigned to long-acting
injectable risperidone were addressed by restarting the intramuscular medication and providing
oral medication for 3 weeks if the interruption
occurred before the steady state was reached, or
if the interruption was longer than 6 weeks.
Concomitant psychotropic medications (i.e.,
antianxiety agents, antidepressants, and oral antipsychotics and mood stabilizers) and anticholinergic medications were allowed.
Control-group participants continued to receive oral antipsychotic therapy as prescribed by
their treating physician. Treating psychiatrists
were given a summary of optimal dosage ranges
for oral antipsychotic and anticholinergic agents,
based on published recommendations.18
baseline (on a scale of 1 to 7, with higher scores
indicating poorer functioning or less improvement). Satisfaction with medication was measured
with the use of the Drug Attitude Inventory (on
a scale of 1 to 20, with higher scores indicating
greater satisfaction).21
Retention on the assigned drug was measured
according to the number of days until discontinuation of the assigned treatment or, among participants assigned to the oral medication, days to
crossover to any new oral or long-acting injectable treatment. The use of long-acting injectable
risperidone was documented according to study
prescribing records, and the use of oral medication was documented according to patient interviews. Efforts were made to ensure that patients
continued to receive the medications selected by
their doctor if they discontinued the study drug.
Symptoms of schizophrenia were measured
according to the total score on the Positive and
Negative Syndrome Scale (PANSS, which ranges
from 30 to 210, with higher scores indicating
more symptoms), and its positive, negative, and
general subscales.22 PANSS ratings were obtained
from standardized videoconferences conducted
by trained raters from MedAvante who were unaware of the patients study-drug assignments.
Psychiatric assessments by video conference are
reliable in patients with schizophrenia and are
well received.23
Subjective psychological distress was measured
with the use of the depression and anxiety subscales of the Brief Symptom Index (on a scale of
0 to 4, with higher scores indicating greater
distress).24
Concomitant Psychosocial Treatment
Quality of Life and Social Functioning
To ensure that no patient was randomly assigned
to less than standard best practice an ethical
imperative a short checklist of potentially useful ancillary psychosocial services available at the
participating centers was provided to all participants during follow-up visits.19
Quality of life was measured with the use of the
HeinrichsCarpenter Quality of Life Scale (ranging from 0 to 120, with higher scores indicating
better quality of life)25 and the Personal and Social Performance scale (ranging from 1 to 100,
with higher scores reflecting better functioning),26 the latter providing a global assessment of
social functioning. Both were administered by
videoconference assessors who were unaware of
the study-drug assignments.
Health-related quality of life was assessed
with the use of the Quality of Well-Being scale
(ranging from 0 to 1, with higher scores indicating greater well-being),27 which has been validated for use in schizophrenia.28
Measures
Blinded videoconference assessments were completed every 3 months on measures of symptoms,
quality of life, and functioning.
At a monthly unblinded meeting with the
study nurse, the Clinical Global Impressions
(CGI) scale20 was used to assess the patients
global mental health status and the change from
844
of
n engl j med 364;9 nejm.org march 3, 2011
The New England Journal of Medicine
Downloaded from nejm.org on September 9, 2015. For personal use only. No other uses without permission.
Copyright 2011 Massachusetts Medical Society. All rights reserved.
Long-Acting Risperidone in schizophrenia
Substance Use
At screening, physicians and patients were asked
whether substance abuse was a problem. Alcohol
and drug use in the previous 30 days was assessed with the use of the alcohol and drug composite indexes from the Addiction Severity Index
(on a scale of 0 to 1, with higher scores indicating more severe problems).29
Side Effects
Neurologic side effects were measured with the
use of three scales.30-32 Sexual dysfunction was
measured with items from the Novel Antipsychotic Medication Experience Scale (ranging from
0 to 4, with higher scores indicating worse side
effects) (Ames D: personal communication).
Hospitalization and Use of Other Medical Services
Administrative data on service use, including hospitalizations, were available for all VA health services. Psychiatric inpatient admissions were identified through the VAs Patient Treatment File.
Non-VA admissions were identified according to
discharge summaries validated as psychiatric by
a physician who was unaware of the patients
study-drug assignments.
The primary outcome measure was the time
from randomization to psychiatric hospitalization (in both VA and non-VA hospitals) or, in the
case of patients who were hospitalized at randomization, the time from the date of discharge
from the initial stay to subsequent hospitalization. The key secondary outcome measure was the
change in the PANSS total score at 12 months.
Secondary analyses compared outcomes at all
time points up to 18 months, rather than the
difference between follow-up scores and baseline scores at one specific time point.
Statistical Analysis
The planned sample size of 450 patients (the
original sample size of 600 was resized because
of recruitment difficulties) provided 90% power
for analyses of our primary outcome and secondary outcome, each with a two-sided test and a
type I error of 2.5% (i.e., 1.25% in each tail). First,
a time-to-event analysis, with the use of the logrank test, compared the hazard ratios associated
with the time to the first psychiatric hospitalization. With a null hypothesis that the hazard ratio
would equal 1, the alternative hypothesis was that
for long-acting injectable risperidone versus oral
agents, the hazard ratio was greater than or equal
to 1.65 or less than or equal to 0.60. This hypothesis was derived from an assumption based on
three studies in which baseline rates of relapse
were approximately 41% in the oral-antipsychotic
group and approximately 25% in the intramuscular-medication group (i.e., a rate ratio of 1.64
[4125] corresponding to a difference of 16 percentage points [41%25%] in the annual rate of
a first psychiatric hospitalization).2,33,34 The follow-up period for this outcome was up to 2 years,
terminating with hospitalization or discontinuation of the assigned study medication.
Confirmatory Cox proportional-hazards analyses controlled for potential confounding factors.
These factors included prior use of risperidone,
history of substance abuse, and hospitalization
at the time of enrollment.
A repeated-measures mixed-effects model was
used to compare the mean change from baseline
to 12 months in the PANSS score for injectable
and oral treatments. With a null hypothesis of
no difference, the alternative hypothesis was
that the difference was greater than or equal to
5 units or less than or equal to 5 units. The
model had fixed effects for treatment group and
time (a categorical variable); the interaction of
treatment with time, site, and individual patients
were treated as random effects. A first-order
autocorrelation structure was used. The baseline
PANSS score was added to the model to assess
its effect on changes from baseline. Confirmatory mixed models were run with the PANSS
score.
Further descriptive analysis of outcome and
side-effect measures used mixed models of all
outcome data up to 18 months because of extensive sample attrition after that time. Because of
the skewed distribution of service use, the significance of differences was tested with the
Wilcoxon rank-sum test.
R e sult s
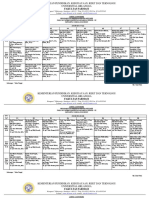
Study Participants
Altogether, 1045 patients were screened at 19 VA
medical centers between 2006 and 2009, yielding
a final analytic sample of 369 patients (Fig. 1).
Five sites discontinued the study because of insufficient recruitment. Participants were hospitalized at the time of randomization (40%), had
been hospitalized within the previous 2 years
n engl j med 364;9 nejm.org march 3, 2011
The New England Journal of Medicine
Downloaded from nejm.org on September 9, 2015. For personal use only. No other uses without permission.
Copyright 2011 Massachusetts Medical Society. All rights reserved.
845
The
n e w e ng l a n d j o u r na l
of
m e dic i n e
1045 Patients were assessed for eligibility
514 Were ineligible
110 Patients or physicians declined participation
39 Patients or physicians never called back
382 Underwent randomization
192 Were assigned to receive
oral treatment
190 Were assigned to receive
injectable risperidone
7 Declined participation
2 Declined participation
185 Received oral treatment
120 Completed study
65 Were lost to follow-up or discontinued intervention
188 Received injectable risperidone
117 Completed study
71 Were lost to follow-up or discontinued intervention
3 Were excluded because
patient did not have a
Social Security number or
did not have baseline data
1 Was excluded because
of lack of baseline data
182 Were included in analysis
187 Were included in analysis
Figure 1. Enrollment, Randomization, and Follow-up of the Study Patients.
(55%), or had recent increased service use indicating a risk of hospitalization (5%). At screening,
problems with medication adherence were reported for 64% of the patients; 43% of the patients
reported problems by themselves and in 60% of
the cases, problems were reported by physicians.
Active problems with alcohol or drug use were
reported for 37% of the patients; 25% were reported by the participants and 36% were reported by their physicians. There were no significant
differences between groups at baseline in this
sample of older male veterans (Table 1 in the
Supplementary Appendix, available at NEJM.org).
Treatment and Follow-Up Assessments
For patients assigned to and receiving long-acting
injectable risperidone, at 6 weeks, 86% of injection doses were 25 mg, 11% were 37.5 mg, and
3% were 50 mg, with an average of 1.8 injections
846
per month. During the remainder of the trial,
17% of doses were 25 mg, 31% were 37.5 mg, and
50% were 50 mg, with an average of 1.5 injections per month (the percentages do not sum to
100 because of rounding). During the first 6 weeks,
40% of patients receiving long-acting injectable
risperidone received concomitant oral antipsychotics. During the remainder of the trial, 32%
of injections were accompanied by prescriptions
for oral antipsychotics during the same month.
The follow-up interview rates in the intentionto-treat analysis were as follows: 60% (223 patients) at 1 year, 46% (170) at 18 months, and
29% (107) at 24 months, with no significant differences between groups at these time points
(P=0.42 to 0.99). The mean (SD) duration of
participation was 474235 days for long-acting
injectable risperidone versus 502226 days for
oral antipsychotics (P=0.22).
n engl j med 364;9 nejm.org march 3, 2011
The New England Journal of Medicine
Downloaded from nejm.org on September 9, 2015. For personal use only. No other uses without permission.
Copyright 2011 Massachusetts Medical Society. All rights reserved.
Long-Acting Risperidone in schizophrenia
Outcomes
1.0
Freedom from Hospitalization
Long-acting injectable treatment was not superior to oral treatment in the duration of adherence
to the randomized treatment (P=0.19) (Fig. 1 in
the Supplementary Appendix). Among participants receiving oral treatment, however, 21 of 182
(12%) switched to long-acting injectable risperidone an average of 153203 days after randomization. There were no significant differences with
respect to the initiation of concomitant psycho
tropic medications (Fig. 2 in the Supplementary
Appendix).
A total of 237 of 369 patients (64%) continued
to receive the study drug throughout their participation in the study. Reasons for medication
discontinuation were not significantly different
between groups (Table 2 in the Supplementary
Appendix).
With a mean follow-up of 11.3 and 10.8
months, respectively, 81 of 182 (45%) patients
receiving oral medication and 72 of 187 (39%)
receiving long-acting injectable risperidone were
hospitalized. Long-acting injectable risperidone
was not superior to oral treatment with respect
to the time to hospitalization (P=0.39 by the
log-rank test; hazard ratio, 0.87, 95% confidence
interval [CI], 0.63 to 1.20) (Fig. 2). An analysis
that excluded the 21 subjects who switched from
an oral antipsychotic to long-acting injectable
risperidone provided similar results (hazard ratio,
1.00; 95% CI, 0.71 to 1.40), as did an analysis
that was adjusted for covariates (hazard ratio,
0.82; 95% CI, 0.59 to 1.13).
The mixed-model analysis of the change from
baseline to 12 months in the PANSS total score
did not show superiority of long-acting injectable risperidone (P=0.72).
Further outcome comparisons across all time
points up to 18 months showed no significant
between-group differences in the PANSS total
score or subscales (Table 1, and Fig. 3 in the
Supplementary Appendix). No significant superiority of long-acting injectable risperidone was
observed on the blindly rated HeinrichsCarpenter
Quality of Life Scale or its subscales, the Personal and Social Performance scale or the selfreported Quality of Well-Being scale, the current
CGI functioning measure, or the Addiction Severity Index composite drug scores (Table 1). The
composite alcohol index of the Addiction Severity Index was higher in the oral-antipsychotic
group (P=0.04) and the Drug Attitude Inventory
P=0.39 by the log-rank test
0.8
Injectable risperidone
0.6
Oral antipsychotic
0.4
0.2
0.0
12
15
18
21
24
49
45
28
37
Months after Randomization
No. at Risk
Oral antipsychotic 182
Injectable
187
risperidone
136
136
116
110
96
92
84
82
71
65
58
53
Figure 2. Time to Hospitalization after Randomization.
In this analysis, data on patients who withdrew from the study were censored at the time of withdrawal from the study.
favored long-acting injectable risperidone (P=0.02).
Although there was no superiority of long-acting
injectable risperidone on the unblinded assessment of illness severity at each time point, the
unblinded CGI improvement score, representing
the rater-perceived change from baseline, favored
long-acting injectable risperidone (P<0.001).
Analysis of adverse events (Table 3 in the Supplementary Appendix) showed that patients who
received long-acting injectable risperidone had
more general disorders and administration site
conditions (injection-related pain or induration)
(P=0.04) and nervous system disorders (headache and extrapyramidal signs and symptoms)
(P<0.001). There were four deaths. In the injectable-risperidone group, one patient died in his
sleep from an unknown cause and another committed suicide. In the oral-antipsychotic group, one
patient died from chronic obstructive pulmonary
disease, and another from accidental drowning.
Use of Services
A larger proportion of patients receiving longacting injectable risperidone were hospitalized at
the time of randomization and they were hospitalized for more days during the period before
randomization (Table 2). After randomization,
there were no significant differences between
groups with respect to VA service use (Table 2) or
non-VA service use (Table 4 in the Supplementary
Appendix), including the number of hospital days.
n engl j med 364;9 nejm.org march 3, 2011
The New England Journal of Medicine
Downloaded from nejm.org on September 9, 2015. For personal use only. No other uses without permission.
Copyright 2011 Massachusetts Medical Society. All rights reserved.
847
The
n e w e ng l a n d j o u r na l
of
m e dic i n e
Table 1. Follow-up Assessment Outcomes Based on Mixed Models with the Use of All Available Data over All Time
Points up to 18 Months.*
Variable
Oral Antipsychotic Injectable Risperidone Mean Difference
P Value
PANSS
Total score
74.690.92
74.100.91
0.591.27
0.65
General symptoms
37.170.46
36.890.45
0.270.64
0.67
Positive symptoms
18.840.38
18.120.38
0.720.48
0.13
Negative symptoms
18.690.35
19.030.35
0.350.37
0.36
HeinrichsCarpenter Quality of Life Scale
Total score
2.860.06
2.780.06
0.080.07
0.28
Interpersonal relations
2.550.08
2.460.08
0.090.10
0.36
Instrumental functioning
2.660.05
2.650.05
0.01 0.06
0.81
Intrapsychic foundations
3.240.06
3.140.06
0.10 0.08
0.18
Personal and Social Performance Scale
53.830.78
53.640.78
0.180.90
0.84
Body-mass index
30.690.50
30.070.51
0.620.72
0.39
Clinical Global Impressions
Severity of illness
4.190.13
4.220.13
0.030.09
0.34
Change in condition
3.520.08
3.220.08
0.300.06
<0.001
0.130.03
0.070.03
0.060.03
0.04
Addiction Severity Index**
Alcohol use
0.0120.003
0.0180.003
0.0060.004
0.13
Brief Symptom Index
Drug use
0.670.62
0.640.62
0.030.06
0.55
Quality of Well-Being scale
0.660.02
0.670.02
0.010.01
0.63
Abnormal Involuntary Movement Scale
0.260.04
0.210.04
0.060.03
0.11
SimpsonAngus Scale
0.230.05
0.220.05
0.010.03
0.60
Barnes Akathisia Scale
0.440.09
0.450.09
0.010.06
0.80
1.060.10
1.010.10
0.050.10
0.61
1.100.11
0.930.11
0.170.11
0.13
7.960.13
8.270.13
0.310.13
0.02
NAMES***
Sexual interest
Sexual activities
Drug Attitude Inventory
*
Plusminus values are means SE. For all outcomes, the treatment comparison was a linear contrast based on a
mixed-effects model with three fixed effects (time, treatment, and timetreatment interaction), with site as a random effect and with autocorrelated repeated measures over time.
Scores on the Positive and Negative Syndrome Scale (PANSS) range from 30 to 210, with higher scores indicating
more symptoms.
Scores on the HeinrichsCarpenter Quality of Life Scale range from 0 to 120, with higher scores indicating better
quality of life.
Scores on the Personal and Social Performance Scale range from 1 to 100, with higher scores reflecting better functioning.
Body-mass index is the weight in kilograms divided by the square of the height in meters.
Scores on the Clinical Global Impressions scale range from 1 to 7, with higher scores indicating poorer functioning
or less improvement.
** Scores on the Addiction Severity Index range from 0 to 1, with higher scores indicating more severe problems.
Scores on the Brief Symptom Index range from 0 to 4, with higher scores indicating greater distress.
Scores on the Quality of Well-Being scale range from 0 to 1, with higher scores indicating better well-being.
Scores on the Abnormal Involuntary Movement Scale range from 0 to 4, with higher scores indicating more severe
tardive dyskinesia.
Scores on the SimpsonAngus Scale range from 0 to 4, with higher scores indicating more severe extrapyramidal
symptoms.
Scores on the Barnes Akathisia Scale range from 0 to 5, with higher scores indicating more severe akathisia.
*** Scores on the Novel Antipsychotic Medication Experience Scale (NAMES) range from 0 to 4, with higher scores indicating worse side effects.
Scores on the Drug Attitude Inventory range from 1 to 20, with higher scores indicating greater satisfaction.
848
n engl j med 364;9 nejm.org march 3, 2011
The New England Journal of Medicine
Downloaded from nejm.org on September 9, 2015. For personal use only. No other uses without permission.
Copyright 2011 Massachusetts Medical Society. All rights reserved.
Long-Acting Risperidone in schizophrenia
Discussion
This randomized, controlled trial showed that in
high-risk patients with schizophrenia or schizo
affective disorder, long-acting injectable risperidone was not superior to oral antipsychotics with
respect to the primary outcome of time to hospitalization, or multiple standard measures of
symptoms, quality of life, side effects, or service
use. Greater numbers of adverse events were reported by the injectable-risperidone group. These
events primarily included injection-site phenom-
ena, headache, and extrapyramidal signs and
symptoms, suggesting that patients receiving oral
medication may flexibly adjust their medication
use to avoid such adverse effects. The duration of
treatment with long-acting injectable risperidone
was not significantly longer than the duration of
treatment with oral antipsychotics.
The findings were not modified by the addition of covariates or the exclusion of crossover
observations (for participants who switched from
oral to long-acting injectable treatment). Differences in the alcohol composite index of the Ad-
Table 2. Use of Health Services Provided by the Veterans Affairs System.*
Type of Use
Oral
Antipsychotic
(N=182)
Injectable
Risperidone
(N=187)
P Value
1.04.1
1.04.0
0.95
15.4
15.0
0.91
20.343.4
19.259.7
0.80
62.1
64.7
0.60
Inpatient care
Acute medical or surgical hospital stays
Days
Patients with any hospitalization (%)
Total acute psychiatric hospital stays after randomization
Total days
Patients with any hospitalization (%)
Hospitalization at time of randomization
Patients hospitalized (%)
Days from hospitalization at randomization to discharge
35.2
45.5
0.04
2.77.4
8.453.0
0.02
42.9
36.4
0.20
17.641.1
10.828.0
0.21
2.62.5
2.21.5
0.60
Hospitalizations subsequent to the original stay
Patients with new hospitalization after randomization (%)*
Days in subsequent stays
No. of subsequent stays among patients with any stays
Residential treatment, nonhospital
Patients with any residential treatment admission (%)
23.6
19.3
0.31
26.486.4
18.171.3
0.49
Individual psychiatry
58.965.8
52.056.2
0.67
Group psychiatry
30.163.5
24.556.6
0.36
Vocational rehabilitation
5.415.4
3.815.3
0.25
Telephone psychiatry
3.66.6
2.44.8
0.05
1.02.9
0.62.0
0.33
15.115.9
16.124.3
0.22
0.77
Days
Outpatient care
Outpatient visits after randomization (no.)
Other psychiatry
Medical and surgical
Other ancillary care
Total outpatient visits
Visits to administer long-acting injectable risperidone (no.)
22.433.3
23.140.5
136.5137.0
122.4130.9
0.26
1.24.9
19.714.7
<0.001
* These data pertain to hospitalizations at Veterans Affairs (VA) hospitals only and thus the percentages are somewhat
smaller than the total proportion of patients who were hospitalized (i.e., at either VA or non-VA hospitals).
n engl j med 364;9 nejm.org march 3, 2011
The New England Journal of Medicine
Downloaded from nejm.org on September 9, 2015. For personal use only. No other uses without permission.
Copyright 2011 Massachusetts Medical Society. All rights reserved.
849
The
n e w e ng l a n d j o u r na l
diction Severity Index and the Drug Attitude Inventory were not significant after adjustment for
multiple comparisons. Although the current CGI
scores assigned by raters who were aware of the
patients study-drug assignments did not differ
between groups, the CGI improvement scores assigned by these raters indicated significantly
greater improvement in the group of patients who
received long-acting injectable risperidone, suggesting an unblinded rater bias favoring longacting injectable risperidone.
Taken together, these findings are consistent
with three efficacy trials that also showed no
superiority of long-acting injectable risperidone
over oral regimens in patients with stable schizophrenia.12-14 Two studies have suggested that
unintended intramuscular injections into fat tissue may decrease pharmacologic effectiveness,
but this was not assessed in our study.35,36
Our study had several limitations. First, 12%
of control patients received long-acting injectable
risperidone treatment an average of 5 months
into the trial. This may have biased the results
in favor of oral treatment in the intention-totreat analysis. Replication of the analyses of hospitalization risk and blinded outcomes excluding
observations after these crossovers or discontinuation of long-acting injectable risperidone yielded no significant findings favoring long-acting
injectable treatment.
Second, the dose of long-acting injectable risperidone may have been inadequate in some paReferences
1. Thieda P, Beard S, Richter A, Kane J.
An economic review of compliance with
medication in the treatment of schizophrenia. Psychiatr Serv 2003;54:508-16.
2. Weiden PJ, Olfson M. Cost of relapse
in schizophrenia. Schizophr Bull 1995;21:
419-29.
3. Davis JM, Matalon L, Watanabe MD,
Blake L, Matalon L. Depot antipsychotic
drugs: place in therapy. Drugs 1994;47:74173.
4. Adams CE, Fenton MK, Quraishi S,
David AS. Systematic meta-review of depot antipsychotics for people with schizophrenia. Br J Psychiatry 2001;179:290-9.
5. Hogarty GE, Schooler NR, Ulrich R,
Mussare F, Ferro P, Herron E. Fluphena
zine and social therapy in the aftercare of
schizophrenic patients: relapse analyses
of a two-year controlled study of fluphenazine decanoate and fluphenazine hydrochloride. Arch Gen Psychiatry 1979;36:
1283-94.
850
of
m e dic i n e
tients, and some injections were missed, but this
reflects the real-world practice that was the focus
of this effectiveness study.
Third, decisions regarding hospitalization
were unblinded, and the direction of any bias is
unknown. If physicians thought there was less
need to hospitalize patients, knowing that they
were receiving ample medication, the bias could
favor long-acting injectable risperidone. On the
other hand, if admitting physicians knew that
patients receiving long-acting risperidone were
symptomatic in spite of being adequately medicated, the bias could favor oral treatment.
Fourth, this sample involved older, primarily
male veterans, and results may not be generalizable to other populations.
Finally, although our revised target sample
was 450 subjects, we enrolled only 382 subjects,
and data were available for only 369 because of
early dropouts. Dropout patterns and sample
sizes were similar to those of previous schizophrenia trials.36,37 Our study did not show the
superiority of long-acting injectable risperidone,
but the confidence intervals for the time to hospitalization were fairly wide (hazard ratio, 0.87;
95% CI, 0.63 to 1.20), and the study was not
large enough to exclude modest differences
between the groups.
Supported by the Veterans Affairs Cooperative Studies Program and an unrestricted grant from Ortho-McNeil Janssen
Scientific Affairs.
Disclosure forms provided by the authors are available with
the full text of this article at NEJM.org.
6. Miyamoto S, Duncan GE, Goff DC,
Lieberman JA. Therapeutics of schizophrenia. In: Davis KL, Charney D, Coyle
JT, Nemeroff C, eds. Neuropsychopharmacology: the fifth generation of progress. Philadelphia: Lippincott Williams
& Wilkins, 2002:775-807.
7. Kane JM, Eerdekens M, Lindenmayer
JP, Keith SJ, Lesem M, Karcher K. Longacting injectable risperidone: efficacy and
safety of the first long-acting atypical
antipsychotic. Am J Psychiatry 2003;160:
1125-32.
8. Mller HJ, Llorca PM, Sacchetti E,
Martin SD, Medori R, Parellada E. Efficacy
and safety of direct transition to risperidone
long-acting injectable in patients treated
with various antipsychotic therapies. Int
Clin Psychopharmacol 2005;20:121-30.
9. Fleischhacker WW, Eerdekens M,
Karcher K, et al. Treatment of schizophrenia with long-acting injectable risperidone: a 12-month open-label trial of the
first long-acting second-generation antipsychotic. J Clin Psychiatry 2003;64:12507.
10. Lindenmayer J-P, Eerdekens E, Berry
SA, Eerdekens M. Safety and efficacy of
long-acting risperidone in schizophrenia:
a 12-week, multicenter, open-label study
in stable patients switched from typical
and atypical oral antipsychotics. J Clin
Psychiatry 2004;65:1084-9.
11. Fleischhacker WW. Second-generation
antipsychotic long-acting injections: systematic review. Br J Psychiatry Suppl 2009;
52:S29-S36.
12. Chue P, Eerdekens M, Augustyns I,
et al. Comparative efficacy and safety of
long-acting risperidone and risperidone
oral tablets. Eur Neuropsychopharmacol
2005;15:111-7.
13. Bai YM, Ting Chen T, Chen JY, et al.
Equivalent switching dose from oral risperidone to risperidone long-acting injection: a 48-week randomized, prospective,
n engl j med 364;9 nejm.org march 3, 2011
The New England Journal of Medicine
Downloaded from nejm.org on September 9, 2015. For personal use only. No other uses without permission.
Copyright 2011 Massachusetts Medical Society. All rights reserved.
Long-Acting Risperidone in schizophrenia
single-blind pharmacokinetic study. J Clin
Psychiatry 2007;68:1218-25.
14. Keks NA, Ingham M, Khan A, Karcher
K. Long-acting injectable risperidone v.
olanzapine tablets for schizophrenia or
schizoaffective disorder: randomised, controlled, open-label study. Br J Psychiatry
2007;191:131-9.
15. First MB, Spitzer RL, Gibbon MB,
Williams JB. Structured Clinical Interview
for Axes I and II DSM IV Disorders Patient Edition (SCID-I/P). New York: Biometrics Research Institute, New York State
Psychiatric Institute, 1996.
16. Grisso T, Appelbaum PS. MacArthur
Competence Assessment Tool Treatment. Worcester: University of Massachusetts Medical Center, 1995.
17. Keith SJ, Pani L, Nick B, et al. Practical application of pharmacotherapy with
long-acting risperidone for patients with
schizophrenia. Psychiatr Serv 2004;55:
997-1005.
18. Lehman AF, Kreyenbuhl J, Buchanan
RW, et al. The Schizophrenia Patient Outcomes Research Team (PORT): updated
treatment recommendations 2003. Schizo
phr Bull 2004;30:193-217.
19. Rosenheck R, Tekall J, Peters J, et al.
Does participation in psychosocial treatment augment the benefit of clozapine?
Arch Gen Psychiatry 1998;55:618-25.
20. Guy W. Clinical Global Impressions
(CGI). In: ECDEU assessment manual for
psychopharmacology. Rockville, MD: National Institute of Mental Health, 1976:
534-7.
21. Hogan TP, Awad AG, Eastwood R.
A self-report scale predictive of drug com-
pliance in schizophrenics: reliability and
discriminative validity. Psychol Med 1983;
13:177-83.
22. Kay SR, Fiszbein A, Opler LA. The
Positive and Negative Syndrome Scale
(PANSS) for schizophrenia. Schizophr Bull
1987;13:261-76.
23. Ruskin PE, Reed S, Kumar R, et al.
Reliability and acceptability of psychiatric
diagnosis via telecommunication and audiovisual technology. Psychiatr Serv 1998;
49:1086-8.
24. Derogatis LR, Spencer N. The Brief
Symptom Index: administration, scoring
and procedure manual. Baltimore: Johns
Hopkins University Press, 1982.
25. Heinrichs DW, Hanlon ET, Carpenter
WT Jr. The Quality of Life Scale: an instrument for rating the schizophrenic deficit
syndrome. Schizophr Bull 1984;10:388-98.
26. Morosini PL, Magliano L, Brambilla L,
Ugolini S, Pioli R. Development, reliability
and acceptability of a new version of the
DSM-IV Social and Occupational Functioning Assessment Scale (SOFAS) to assess routine social functioning. Acta Psychiatr Scand 2000;101:323-9.
27. Kaplan RM, Anderson JP. The general
health policy model: an integrated approach. In: Spilker B, ed. Quality of life
and pharmacoeconomics in clinical trials.
2nd ed. Philadelphia: Lippincott-Raven,
1996:309-22.
28. Pyne JM, Sullivan G, Kaplan R, Williams DK. Comparing the sensitivity of
generic effectiveness measures with symptom improvement in persons with schizophrenia. Med Care 2003;41:208-17.
29. McLellan AT, Luborsky L, Woody GE,
OBrien CP. An improved diagnostic evaluation instrument for substance abuse patients: the Addiction Severity Index. J Nerv
Ment Dis 1980;168:26-33.
30. Barnes TR. A rating scale for drug induced akathisia. Br J Psychiatry 1989;154:
672-6.
31. Guy W. Abnormal Involuntary Movement Scale (AIMS). In: ECDEU assessment
manual for psychopharmacology. Rockville, MD: National Institute of Mental
Health, 1976:534-7.
32. Simpson GM, Angus JW. A rating
scale for extrapyramidal side effects. Acta
Psychiatr Scand Suppl 1970;212:11-9.
33. Herz MI, Glazer WM, Mostert MA,
et al. Intermittent vs maintenance medication in schizophrenia: two-year results.
Arch Gen Psychiatry 1991;48:333-9.
34. Young JL, Zonana HV, Shepler L. Medication noncompliance in schizophrenia:
codification and update. Bull Am Acad
Psychiatry Law 1986;14:105-22.
35. Nesvg R, Tanum L. Therapeutic drug
monitoring of patients on risperidone depot. Nord J Psychiatry 2005;59:51-5.
36. Marder SR, Meibach RC. Risperidone
in the treatment of schizophrenia. Am J
Psychiatry 1994;151:825-35.
37. Csernansky JG, Mahmoud R, Brenner
R. A comparison of risperidone and haloperidol for the prevention of relapse in
patients with schizophrenia N Engl J Med
2002;346:16-22. [Erratum, N Engl J Med
2002;346:1424.]
Copyright 2011 Massachusetts Medical Society.
new nejm application for iphone
The NEJM Image Challenge app brings a popular online feature to the smartphone.
Optimized for viewing on the iPhone and iPod Touch, the Image Challenge app lets
you test your diagnostic skills anytime, anywhere. The Image Challenge app
randomly selects from 300 challenging clinical photos published in NEJM,
with a new image added each week. View an image, choose your answer,
get immediate feedback, and see how others answered.
The Image Challenge app is available at the iTunes App Store.
n engl j med 364;9 nejm.org march 3, 2011
The New England Journal of Medicine
Downloaded from nejm.org on September 9, 2015. For personal use only. No other uses without permission.
Copyright 2011 Massachusetts Medical Society. All rights reserved.
851
Das könnte Ihnen auch gefallen
- Setiawan 2015Dokument8 SeitenSetiawan 2015ShibaNoch keine Bewertungen
- Assignment 4Dokument5 SeitenAssignment 4NIKITA0% (1)
- Adoc - Pub Harborne J B Metode Fitokimia Penuntun Cara ModernDokument5 SeitenAdoc - Pub Harborne J B Metode Fitokimia Penuntun Cara ModernFirdaNoch keine Bewertungen
- Uji Stabilitas Formulasi Krim Tabir Surya Serbuk RUMPUT LAUT (Eucheuma Cottonii. Doty)Dokument4 SeitenUji Stabilitas Formulasi Krim Tabir Surya Serbuk RUMPUT LAUT (Eucheuma Cottonii. Doty)miftahulnazifahNoch keine Bewertungen
- Jurnal Maserasi Hal 5Dokument8 SeitenJurnal Maserasi Hal 5ElsiiNoch keine Bewertungen
- Identifikasi Hidrokuinon Pada Krim Pemutih Racikan Yang Beredar Di Pasar Tengah Bandar Lampung Secara Kromatografi Lapis Tipis (KLT)Dokument8 SeitenIdentifikasi Hidrokuinon Pada Krim Pemutih Racikan Yang Beredar Di Pasar Tengah Bandar Lampung Secara Kromatografi Lapis Tipis (KLT)Chandra YuniantoNoch keine Bewertungen
- Dipiro PneumoniaDokument8 SeitenDipiro Pneumoniameri dayaniNoch keine Bewertungen
- SPO High AlerTDokument19 SeitenSPO High AlerTHendraTriSaputroNoch keine Bewertungen
- Daftar Pustaka: Drug Substances and ProductsDokument2 SeitenDaftar Pustaka: Drug Substances and ProductsFaizah Min FadhlillahNoch keine Bewertungen
- 1099-1105 Ijpr1301179Dokument7 Seiten1099-1105 Ijpr1301179Indah Indryani UNoch keine Bewertungen
- FarmakokinetikaDokument142 SeitenFarmakokinetikaAstrid Bernadette Ulina PurbaNoch keine Bewertungen
- Analisis Deskriptif Efek Samping Penggunaan Obat Anti Tuberculosis Pada Pasien TBC Di Rsud Dr. Pirngadi MedanDokument7 SeitenAnalisis Deskriptif Efek Samping Penggunaan Obat Anti Tuberculosis Pada Pasien TBC Di Rsud Dr. Pirngadi MedanEva MelisaNoch keine Bewertungen
- Pharmacy Intravena Admixture Services (Pivas) : IV - Admixture Handling CytotoxicDokument32 SeitenPharmacy Intravena Admixture Services (Pivas) : IV - Admixture Handling CytotoxicintanNoch keine Bewertungen
- Indonesian FDA Regulations On Indonesian Traditional Nutraceuticals (Herbs) ContributorsDokument16 SeitenIndonesian FDA Regulations On Indonesian Traditional Nutraceuticals (Herbs) ContributorsDyva VanillaNoch keine Bewertungen
- Pert 3. Sediaan Radiofarmasi Dan RadiolabelingDokument19 SeitenPert 3. Sediaan Radiofarmasi Dan Radiolabelingwida safitrNoch keine Bewertungen
- Farmakologi FarmakodinamikDokument26 SeitenFarmakologi FarmakodinamikMuhammad Nikko AomadaniNoch keine Bewertungen
- Kuliah Colon DDS Reguler-Ganjil 2010 INDDokument125 SeitenKuliah Colon DDS Reguler-Ganjil 2010 INDYartiSulistiaNingratNoch keine Bewertungen
- Bromhexin Method of Analysis PDFDokument8 SeitenBromhexin Method of Analysis PDFJitendra YadavNoch keine Bewertungen
- Jurnal Rumus Kadar AbuDokument5 SeitenJurnal Rumus Kadar AbualyanuraNoch keine Bewertungen
- Biopharmaceutics Classification System-The Scientific Basis PDFDokument5 SeitenBiopharmaceutics Classification System-The Scientific Basis PDFtrianawidiacandra100% (1)
- Floor Stock AlamandaDokument2 SeitenFloor Stock AlamandayuliNoch keine Bewertungen
- Coek - Info - The Pharmaceutical Codex Principles and Practice oDokument1 SeiteCoek - Info - The Pharmaceutical Codex Principles and Practice oNomiNoch keine Bewertungen
- Ikatan Apoteker Indonesia (Iai) Cabang Kota BekasiDokument2 SeitenIkatan Apoteker Indonesia (Iai) Cabang Kota BekasichevyluvianaNoch keine Bewertungen
- JurnalDokument4 SeitenJurnallailaNoch keine Bewertungen
- Farmasi Industri: Stabilitas ObatDokument113 SeitenFarmasi Industri: Stabilitas ObatMelani JunaediNoch keine Bewertungen
- Review Jurnal Interaksi Obat Antihipertensi - Radhwa Fauztina (20190350050)Dokument13 SeitenReview Jurnal Interaksi Obat Antihipertensi - Radhwa Fauztina (20190350050)Radhwa FauztinaNoch keine Bewertungen
- Materi IAI Palangka Raya - Rev PDFDokument55 SeitenMateri IAI Palangka Raya - Rev PDFNopernas CahayaNoch keine Bewertungen
- 02-Pharmaceutical Care ProcessDokument42 Seiten02-Pharmaceutical Care ProcessBalsam Zahi Al-Hasan100% (1)
- Review On Prefilled Syringe As A Modern Technique For Packaging and Delivery of ParenteralDokument6 SeitenReview On Prefilled Syringe As A Modern Technique For Packaging and Delivery of ParenteralShivraj JadhavNoch keine Bewertungen
- Daftar Obat Aman Dan Berbahaya Untuk Ibu Hamil Dan MenyusuiDokument28 SeitenDaftar Obat Aman Dan Berbahaya Untuk Ibu Hamil Dan MenyusuiDwiPrasetyaningRahmawatiNoch keine Bewertungen
- A Review On Water Used in Pharma Industry: European Journal of Pharmaceutical and Medical ResearchDokument11 SeitenA Review On Water Used in Pharma Industry: European Journal of Pharmaceutical and Medical ResearchDinesh babuNoch keine Bewertungen
- Parameter FarmakokinetikDokument12 SeitenParameter FarmakokinetikNnay AnggraeniNoch keine Bewertungen
- Jurnal Review MegaDokument6 SeitenJurnal Review MegaLa OgaNoch keine Bewertungen
- PPDokument6 SeitenPPElvina iskandarNoch keine Bewertungen
- Dipiro Edisi 9 KolestrolDokument10 SeitenDipiro Edisi 9 KolestrolFriska tampuboLonNoch keine Bewertungen
- Artikel 1 PDFDokument9 SeitenArtikel 1 PDFsintiaNoch keine Bewertungen
- Prosedur Asli IodoformDokument3 SeitenProsedur Asli IodoformtartilaNoch keine Bewertungen
- Uji Aktivitas Antibakteri Kombinasi Minyak Atsiri Daun Gelam Putih (Melaleuca Leucadendra) Dan Rimpang Jahe (Zingiber Officinale) Terhadap Bakteri Staphylococcus Aureus Dan Escherichia Coli Secara inDokument74 SeitenUji Aktivitas Antibakteri Kombinasi Minyak Atsiri Daun Gelam Putih (Melaleuca Leucadendra) Dan Rimpang Jahe (Zingiber Officinale) Terhadap Bakteri Staphylococcus Aureus Dan Escherichia Coli Secara inberliana faradisaNoch keine Bewertungen
- Bio Evailabilitas Dan Bioekivalensi Aciclovir BABEDokument13 SeitenBio Evailabilitas Dan Bioekivalensi Aciclovir BABERian Nurdiana100% (1)
- Computational Methods For Prediction of Drug LikenessDokument10 SeitenComputational Methods For Prediction of Drug LikenesssciencystuffNoch keine Bewertungen
- Development and Validation of A Liquid Chromatography Method For The Analysis of Paromomycin Sulfate and Its Impurities 2155 9872.1000102Dokument4 SeitenDevelopment and Validation of A Liquid Chromatography Method For The Analysis of Paromomycin Sulfate and Its Impurities 2155 9872.1000102rbmoureNoch keine Bewertungen
- Expired DateDokument38 SeitenExpired DateAnggie Restyana100% (1)
- Monitoring Efek Samping ObatDokument8 SeitenMonitoring Efek Samping ObatWilujeng SulistyoriniNoch keine Bewertungen
- Daun LeilemDokument8 SeitenDaun Leilemniken retnoNoch keine Bewertungen
- Analisis Simetikon PDFDokument9 SeitenAnalisis Simetikon PDFArini Musfiroh50% (2)
- Pendekatan SOAP Farmasi KlinikDokument40 SeitenPendekatan SOAP Farmasi KlinikmadeNoch keine Bewertungen
- Kelompok 10 - Metode Optimasi Senyawa PenuntunDokument36 SeitenKelompok 10 - Metode Optimasi Senyawa Penuntunapr_aprililianti100% (1)
- KARAKTERISTIK TUGAS DAN TANGGUNG JAWAB APOTEKER MUSLIM - NewDokument30 SeitenKARAKTERISTIK TUGAS DAN TANGGUNG JAWAB APOTEKER MUSLIM - NewBantuinAku KakNoch keine Bewertungen
- Preformulasi AsetosalDokument2 SeitenPreformulasi AsetosalTazyinul Qoriah AlfauziahNoch keine Bewertungen
- Bab V Analisis Farmakoterapi - DRP 5.1 Lembar Pemakaian Obat Di IGDDokument16 SeitenBab V Analisis Farmakoterapi - DRP 5.1 Lembar Pemakaian Obat Di IGDCosmas ZebuaNoch keine Bewertungen
- CTM Direct CompressionDokument8 SeitenCTM Direct CompressionrizkamarNoch keine Bewertungen
- OPTIMASI ZAT WARNA BUNGA TELANG (Clitoria Ternatea) Sebagai Pewarna Alami Pada Sirup ParasetamolDokument9 SeitenOPTIMASI ZAT WARNA BUNGA TELANG (Clitoria Ternatea) Sebagai Pewarna Alami Pada Sirup ParasetamolReza Fadillah AchmadNoch keine Bewertungen
- Glimepiride TabletDokument48 SeitenGlimepiride Tabletrabd samNoch keine Bewertungen
- AHFS Drug InformationDokument10 SeitenAHFS Drug InformationMika FebryatiNoch keine Bewertungen
- 11 Farmakokinetika Klinik Antibiotika Aminoglikosida PDFDokument19 Seiten11 Farmakokinetika Klinik Antibiotika Aminoglikosida PDFIrfanSektionoNoch keine Bewertungen
- Jadwal Ujian Sidang Periode 112 TGL 26-27 Juni 2021 (Rev)Dokument9 SeitenJadwal Ujian Sidang Periode 112 TGL 26-27 Juni 2021 (Rev)Yohan Nafisa NetNoch keine Bewertungen
- Coump & Disp (B - Latifah)Dokument101 SeitenCoump & Disp (B - Latifah)Muhammad Nurhadi Bin AbdulghaffarNoch keine Bewertungen
- Long-Acting Risperidone and Oral Antipsychotics in Unstable SchizophreniaDokument29 SeitenLong-Acting Risperidone and Oral Antipsychotics in Unstable SchizophreniahermanfirdausNoch keine Bewertungen
- Long-Acting Risperidone (1) .En - IdDokument10 SeitenLong-Acting Risperidone (1) .En - IdZidnil UlaNoch keine Bewertungen
- The Great Replacement The Violent Consequences of Mainstreamed Extremism by ISDDokument36 SeitenThe Great Replacement The Violent Consequences of Mainstreamed Extremism by ISDTom Lacovara-Stewart RTR TruthMediaNoch keine Bewertungen
- Summary of Evidence: Chicago Police Torture TrialDokument118 SeitenSummary of Evidence: Chicago Police Torture TrialAndres100% (1)
- NSTP (LTS) Activity 1 Ma. Nicole Pateño: 1. Give Your Own Perspective About The VMGO of BISU?Dokument3 SeitenNSTP (LTS) Activity 1 Ma. Nicole Pateño: 1. Give Your Own Perspective About The VMGO of BISU?MA. NICOLE PATENONoch keine Bewertungen
- State - CIF - Parent - Handbook - I - Understanding - Transfer - Elgibility - August - 2021-11 (Dragged) PDFDokument1 SeiteState - CIF - Parent - Handbook - I - Understanding - Transfer - Elgibility - August - 2021-11 (Dragged) PDFDaved BenefieldNoch keine Bewertungen
- Philosophy and National DevelopmentDokument8 SeitenPhilosophy and National DevelopmentIzo SeremNoch keine Bewertungen
- Tom Sawyer Vocabulary.1681608284879Dokument22 SeitenTom Sawyer Vocabulary.1681608284879Vhone NeyraNoch keine Bewertungen
- Social - Security - Net - TAMIL NADUDokument4 SeitenSocial - Security - Net - TAMIL NADUTamika LeeNoch keine Bewertungen
- SuccessionDokument47 SeitenSuccessionHyuga NejiNoch keine Bewertungen
- Manual Complex Engineering Problem: COMSATS University Islamabad Abbottabad CampusDokument35 SeitenManual Complex Engineering Problem: COMSATS University Islamabad Abbottabad CampusHajra SwatiNoch keine Bewertungen
- 56408e8ca7356 Allhoff 2003Dokument8 Seiten56408e8ca7356 Allhoff 2003yiğit tirkeşNoch keine Bewertungen
- A Poem For Cotton PickersDokument4 SeitenA Poem For Cotton Pickersapi-447987846Noch keine Bewertungen
- FLW Cronon Inconstant Unity Passion PDFDokument25 SeitenFLW Cronon Inconstant Unity Passion PDFAlexandraBarbieruNoch keine Bewertungen
- Internship Report NgoDokument14 SeitenInternship Report Ngosamarth chauhanNoch keine Bewertungen
- 6-Re - Petition For Radio and T.V. Coverage A.M. No. 10-11-5-SC, A.M. No. 10-11-6-SC and A.M. No. 10-11-7-SCDokument6 Seiten6-Re - Petition For Radio and T.V. Coverage A.M. No. 10-11-5-SC, A.M. No. 10-11-6-SC and A.M. No. 10-11-7-SCFelicity HuffmanNoch keine Bewertungen
- Melody Gardot Your Heart Is As Black As NightDokument8 SeitenMelody Gardot Your Heart Is As Black As NightmiruNoch keine Bewertungen
- Brij Pal Vs StateDokument7 SeitenBrij Pal Vs StateSatyendra ChauhanNoch keine Bewertungen
- Position PaperDokument9 SeitenPosition PaperJamellen De Leon BenguetNoch keine Bewertungen
- Jurnal Filsafat Hukum (Tri & Yusuf)Dokument5 SeitenJurnal Filsafat Hukum (Tri & Yusuf)vacefa2507Noch keine Bewertungen
- Assurance Principles, Professional Ethics and Good Governance SyllabusDokument15 SeitenAssurance Principles, Professional Ethics and Good Governance SyllabusGerlie0% (1)
- Session 5 - Marketing ManagementDokument6 SeitenSession 5 - Marketing ManagementJames MillsNoch keine Bewertungen
- Abs CBN vs. Ombudsman 2010Dokument11 SeitenAbs CBN vs. Ombudsman 2010Mara VinluanNoch keine Bewertungen
- Employment Contract: Prepared By: Atty. Daniel L. DiazDokument8 SeitenEmployment Contract: Prepared By: Atty. Daniel L. DiazKuya KimNoch keine Bewertungen
- Rakowski Complaint1 Amy MorrisDokument4 SeitenRakowski Complaint1 Amy Morrisapi-286623412Noch keine Bewertungen
- The Cincinnati Time Store As An Historical Precedent For Societal ChangeDokument11 SeitenThe Cincinnati Time Store As An Historical Precedent For Societal ChangeSteve Kemple100% (1)
- Deed of Assignment SM DavaoDokument2 SeitenDeed of Assignment SM DavaoFrancisqueteNoch keine Bewertungen
- Almirez Vs Infinite Loop TechnologyDokument2 SeitenAlmirez Vs Infinite Loop TechnologyJulian DubaNoch keine Bewertungen
- Business Communication 1Dokument13 SeitenBusiness Communication 1Kishan SrivastavaNoch keine Bewertungen
- Online Training of Trainers' (Tot) /walkthrough of Modules ScheduleDokument5 SeitenOnline Training of Trainers' (Tot) /walkthrough of Modules ScheduleJames Domini Lopez LabianoNoch keine Bewertungen
- b00105047 Posthuman Essay 2010Dokument14 Seitenb00105047 Posthuman Essay 2010Scott Brazil0% (1)
- NOSTALGIA - Grandma's Fridge Is Cool - Hemetsberger Kittiner e MullerDokument24 SeitenNOSTALGIA - Grandma's Fridge Is Cool - Hemetsberger Kittiner e MullerJúlia HernandezNoch keine Bewertungen
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Von EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Bewertung: 3 von 5 Sternen3/5 (1)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedVon EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedBewertung: 4.5 von 5 Sternen4.5/5 (82)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDVon EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDBewertung: 5 von 5 Sternen5/5 (3)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionVon EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionBewertung: 4 von 5 Sternen4/5 (404)
- The Age of Magical Overthinking: Notes on Modern IrrationalityVon EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityBewertung: 4 von 5 Sternen4/5 (32)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeVon EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeBewertung: 2 von 5 Sternen2/5 (1)
- Manipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesVon EverandManipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesBewertung: 4.5 von 5 Sternen4.5/5 (1412)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsVon EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNoch keine Bewertungen
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsVon EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsBewertung: 4 von 5 Sternen4/5 (4)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsVon EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsBewertung: 5 von 5 Sternen5/5 (1)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisVon EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisBewertung: 4.5 von 5 Sternen4.5/5 (42)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaVon EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- The Comfort of Crows: A Backyard YearVon EverandThe Comfort of Crows: A Backyard YearBewertung: 4.5 von 5 Sternen4.5/5 (23)
- The Obesity Code: Unlocking the Secrets of Weight LossVon EverandThe Obesity Code: Unlocking the Secrets of Weight LossBewertung: 4 von 5 Sternen4/5 (6)
- Why We Die: The New Science of Aging and the Quest for ImmortalityVon EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityBewertung: 4.5 von 5 Sternen4.5/5 (6)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisVon EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisBewertung: 3.5 von 5 Sternen3.5/5 (2)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeVon EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeBewertung: 4.5 von 5 Sternen4.5/5 (254)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Von EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Bewertung: 4.5 von 5 Sternen4.5/5 (110)
- To Explain the World: The Discovery of Modern ScienceVon EverandTo Explain the World: The Discovery of Modern ScienceBewertung: 3.5 von 5 Sternen3.5/5 (51)
- Critical Thinking: How to Effectively Reason, Understand Irrationality, and Make Better DecisionsVon EverandCritical Thinking: How to Effectively Reason, Understand Irrationality, and Make Better DecisionsBewertung: 4.5 von 5 Sternen4.5/5 (39)
- The Marshmallow Test: Mastering Self-ControlVon EverandThe Marshmallow Test: Mastering Self-ControlBewertung: 4.5 von 5 Sternen4.5/5 (60)
- Dark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingVon EverandDark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingBewertung: 4 von 5 Sternen4/5 (1138)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessVon EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessBewertung: 4.5 von 5 Sternen4.5/5 (328)