Beruflich Dokumente
Kultur Dokumente
Efikasi Azitromisin
Hochgeladen von
Nadia DesiOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Efikasi Azitromisin
Hochgeladen von
Nadia DesiCopyright:
Verfügbare Formate
RESEARCH BRIEF
Efficacy and Safety of Azithromycin for Uncomplicated
Typhoid Fever: An Open Label Non-comparative Study
ANJU AGGARWAL, #APURBA GHOSH, SUNIL GOMBER, ##MONJORI MITRA AND $AO PARIKH
From the Department of Pediatrics, University College of Medical Sciences and Guru Tegh Bahadur Hospital, New
Delhi; #Institute of Child Health, 11, Dr Biresh Guha Street, Kolkata; ##Medclin Research Pvt Ltd, Kolkata; and
$Alembic Limited; India.
Correspondence to:
Dr Monjori Mitra,
Research Director,
Medclin Research Pvt Ltd, 195/2
ChakrobortyPara
Kolkata 700 107, West Bengal,
India. monjorim@vsnl.net
Received: May 6, 2010;
Initial review: June 28, 2010;
Accepted: November 26, 2010.
An open-labelled, non-comparative study was conducted in 117 children aged 212 years to evaluate the efficacy and safety of azithromycin (20mg/ kg/day for 6
days) for the treatment of uncomplicated typhoid fever. Of the patients enrolled
based on a clinical definition of typhoid fever, 109 (93.1%) completed the study.
Mean (SD) of duration of fever at presentation was 9.1(4.5) days. Clinical cure was
seen in 102 (93.5%) subjects, while 7 were withdrawn from the study because of
clinical deterioration. Mean day of response was 3.451.97. BACTEC blood
culture was positive for Salmonella typhi in 17/109 (15.5%) and all achieved
bacteriological cure. No serious adverse event was observed. Global well being
assessed by the investigator and subjects was good in 95% cases which was done
at the end of the treatment. Azithromycin was found to be safe and efficacious for
the management of uncomplicated typhoid fever.
Key words: Azithromycin, Children, Management Typhoid fever.
Published Online: 2011 February, 28. PII: S09747559INPE1000377-2
idespread emergence of multidrugresistant S. typhi has necessitated
the search for other therapeutic
options
for
typhoid
fever.
Fluoroquinolones have proven effective, but to date
they are not recommended for use in children, and
quinolone-resistant strains of S. typhi have been
reported [1]. Azalides, are another class of antibiotics which have shown promise in the treatment of
typhoid fever. Azithromycin, the first drug of this
class and studies comparing the efficacy of
azithromycin with cefixime in adults and children
with typhoid fever have reported it to be safe and
efficacious [2-4]. Few studies are exclusively
reported in children [5,6]. We planned this openlabeled, study to assess the safety and efficacy of
single daily dose of azithromycin for uncomplicated
typhoid fever in children.
INDIAN PEDIATRICS
METHODS
This multicentre study was conducted with prior
approval of the study protocol from the Institutional
Ethics Committee of both participating institutions.
We planned to enroll 120 children from outpatient
department of the two centres. Children aged 2-12
years with fever (axillary/oral temperature 38.5C)
for at least 4 days with clinical features suggestive of
uncomplicated typhoid fever (abdominal pain and
tenderness, diarrhea or constipation, and hepatosplenomegaly) were enrolled. Only those children
whose guardians were able to record body
temperature and note down all information in the
case diary for assessment during study visits and
were telephonically available, were included.
Written informed parental consent was taken from
all subjects prior to enrolment.
553
VOLUME 48__JULY 17, 2011
AGGARWAL, et al.
AZITHROMYCIN FOR TYPHOID FEVER
was categorized compliant if >80% of study medication consumed according to prescribed regimen.
Children with complicated typhoid fever (those
with gastro-intestinal bleeding, suspected intestinal
perforation, pneumonia, stupor, coma) or those taking antibiotics other than amoxicillin, ampicillin,
cotrimaxazole or chloramphenicol in the last 4 days
were excluded. Children with history of documented S. typhi and/or paratyphi infection within last
12 weeks or history of hypersensitivity reactions to
azithromycin were also excluded.
Children who were BACTEC blood culture
positive were evaluated on day 10 also for repeat
blood culture. A window period of 2days was
admissible for each visit. If the temperature
increased or the clinical condition of the patient
worsened or there was a serious drug reaction,
patient was taken off from the study and treated with
ofloxacin (15mg/kg/day oral) or intravenous ceftriaxone (100mg/kg/day). All follow ups were carried
out in the out-patient department of the hospital.
On day of recruitment a complete medical,
treatment and vaccination history was recorded.
Complete physical examination was carried out and
blood collected for complete blood count, malarial
parasite, BACTEC blood culture. BACTEC blood
culture was carried out as per standard procedure.
Isolates were identified by standard microbiological
methods and disc susceptibility testing was performed by the modified Kirby Bauer method. Study
medication was dispensed and monitoring instruction provided to the patient. The subjects received
azithromycin dispersible tablet/suspension at a dose
of 20mg/kg/body weight in a single daily dose for 6
days. Paracetamol 15mg/kg body weight orally was
used as antipyretic. No antibiotics other than the
study medications were dispensed.
Primary efficacy end-point was clinical cure rate
at day 10 and bacteriological cure rate in children
who were initially bacteriological positive. Clinical
cure was defined as defervescence/fever clearance
and subsidence of clinical symptoms. Fever
clearance/defervescence was considered as sustained period of 72 hours with axillary temperature
less than 37C (98.6F). Secondary efficacy end
points were (i) clinical improvement rates at second
follow up visit i.e. day 7 in percentage of subjects
who do not achieve fever clearance but who show
signs and symptoms of improvement (ii) tolerability/
global assessment of well being assessed by the
clinician at second follow up visit (day 7) to be
measured on a 4 point Likert Scale (excellent=3,
good=2, fair=1, poor=0) as assessed by the investigator and as reported by the patient or his guardian.
Children were treated at their home and reassessed in the out-patient department on day 4, day
7 and day 10 after the start of the treatment. On day 4
and day 7 temperature chart and symptom diary was
evaluated with a complete physical examination.
Drug compliance was assessed by history collecting
the empty wrappers/bottles. The overall compliance
RESULTS
A total of 117 children were enrolled, but 8 were lost
TABLE I CLINICAL CHARACTERISTICS OF STUDY CHILDREN AT BASELINE AND FOLLOW UP
Clinical findings
Visit 1 (Day 0)
Visit 2 (Day 4)
Visit 3 (Day 7)
Visit 4 (Day 10)
Fever >38.4C
109
100
29
26.6
12
11
6.4
Headache
74
67.8
17
15.5
1.8
0.0
Constipation/diarrhea
61
55.9
7.3
0.0
0.0
Poor appetite
39
35.7
32
29.3
5.5
2.7
Abdominal pain
69
63.3
15
13.7
1.8
0.0
Splenomegaly
27
24.7
22
20.1
16
14.6
6.4
Hepatomegaly
73
66.9
56
51.3
35
32.1
15
13.7
INDIAN PEDIATRICS
554
VOLUME 48__JULY 17, 2011
AGGARWAL, et al.
AZITHROMYCIN FOR TYPHOID FEVER
WHAT THIS STUDY ADDS?
Azithromycin as a single daily dose therapy for 6 days was safe and efficacious for clinically diagnosed
uncomplicated typhoid fever.
to follow up and 109 (93.5%) 68 males completed
the study. Mean (SD) age was 7.5 (2.81) years. Only
22 subjects had prior history of typhoid vaccination
(duration from receiving vaccine was less than 3
years in 9). Mean (SD) of duration of fever at
presentation was 9.1 (4.5) days, of which 51 (46.7)
presented within 7 days, 35 (32.1%) within 8-10
days and 23 ( 21.1%) of more than 11 days duration.
DISCUSSION
Azithromycin appears to be an effective drug for
treating uncomplicated typhoid fever in children
with efficacy rate of more than 90%. Treatment
failure rates of 9.3% have been observed in earlier
studies on azithromycin [4]. Two other studies have
reported a clinical cure rate of 82% and 92% [5,7].
Sensitivity pattern seen in our study is also similar to
other Indian study demonstrating a nalidixic acid
resistance of 88% [8], hence the importance of
azithromycin.
Only 23 (21.1%) children had received
antibiotics (amoxicillin) before presentation. Table 1
shows the baseline clinical characteristics and that
on follow up. Treatment failure was noticed in 7
(6.4%) patients by day 10. These were withdrawn
from the study. Three of them received intravenous
ceftriaxone and 4 received oral ofloxacin as an addon therapy and all improved by day 7-15 of
enrollment. All the patients had more than 80%
compliance. Mean day of response to fever was 3.4
(1.9) days.
This study was not a randomized controlled trial
or a comparative trial which is one of the limitations
of the study. Of the subjects studied, 21.1% received
amoxicillin before enrollement, this could have
influenced the BACTEC blood culture results,
though culture positivity was similar in those
received antibiotics and those who did not.
Acknowledgments: Prof M Pal and Dr P Bharati of Indian
Statistical Institute, Kolkata for statistical analysis of the study.
Contributors: All authors contributed to design and conduct of
the study and drafting the paper.
Funding: Alembic Limited.
Competing interests: AOP is Associate Vice President of
Alembic Ltd, which manufactures azithromycin.
BACTEC blood culture was positive in 17
(15.5%) patients, of which one patient did not
complete the study. Hence, 16/109 were BACTEC
blood culture positive (Table II). All of these
patients achieved bacteriological cure at 10th day.
Five of these subjects required add on antibiotics.
We did not have any case of multidrug resistant
typhoid. Resistance to quinolones including
ciprofloxacin was significantly high. Clinical
characteristics and response rates were similar in
BACTEC blood culture positive and BACTEC
blood culture negative cases. No serious adverse
effects were observed except worsening of diarrhea
in two subjects.
TABLE II IN VITRO SUSCEPTIBILITY OF S.TYPHI ISOLATES
FROM BACTEC CULTURE POSITIVE SUBJECTS
(N=17)
Drug
Clinical improvement on day 7 was seen in 92
(84.4%) subjects. Global well being assessed by the
investigator on day 10 was excellent in 54.6%, good
in 37.9%, fair in 4.62% and poor in 0.92%. Global
well-being as assessed by the subjects was excellent
44.2%, good in 47.2%, fair in 3.7% and poor in
1.8%.
INDIAN PEDIATRICS
555
Susceptible (%)
Amoxicillin
100
Cefixime
100
Ceftriaxone
100
Chloramphenicol
100
Cotrimoxazole
94.4
Ofloxacin
83.3
Ciprofloxacin
77.7
Azithromycin
77.7
Nalidixic Acid
16.6
VOLUME 48__JULY 17, 2011
AGGARWAL, et al.
AZITHROMYCIN FOR TYPHOID FEVER
REFERENCES
1. Yanagi D, de Vries GC, Rahardjo D, Alimsardjono L,
Wasito EB, De I, et al. Emergence of fluoroquinoloneresistant strains of Salmonella enterica in Surabaya,
Indonesia. Diagn Microbiol Infect Dis. 2009;64:422-6.
2. Capoor MR, Rawat D, Nair D, Hasan AS, Deb M,
Aggarwal P, et al. In vitro activity of azithromycin, newer
quinolones and cephalosporins in ciprofloxacin-resistant
Salmonella causing enteric fever. J Med Microbiol.
2007;56:1490-4.
3. Dolecek C, Tran TP, Nguyen NR, Le TP, Ha V, Phung
QT, et al. A multi-center randomised controlled trial of
gatifloxacin versus azithromycin for the treatment of
uncomplicated typhoid fever in children and adults in
Vietnam. PLoS ONE. 2008;3: e2188.
4. Parry CM, Ho VA, Phuong le T, Bay PV, Lanh MN, Tung
le T, et al. Randomized controlled comparison of
INDIAN PEDIATRICS
5.
6.
7.
8.
556
ofloxacin, azithromycin, and an ofloxacin-azithromycin
combination for treatment of multidrug-resistant and
nalidixic acid-resistant typhoid fever. Antimicrob Agents
Chemother. 2007;51:819-25.
Frenck RW Jr, Mansour A, Nakhla I, Sultan Y, Putnam S,
Wierzba T, et al. Short-course azithromycin for the
treatment of uncomplicated typhoid fever in children and
adolescents. Clin Infect Dis.. 2004;38:951-7.
Islam MN, Khaleque MA, Siddika M, Hossain MA.
Efficacy of azithromycin in the treatment of childhood
typhoid Fever. Mymensingh Med J. 2007;16:149-53.
Ratika RM, Jacques-palaz K, Murray BE. Intracellular
activity of azithromycin against bacterial enteric
pathogens. Antimicrob Agents Chemother. 2007;51:81925.
Verma M, Parashar Y, Singh A, Kamoji R. Current
pattern of enteric fever: A prospective clinical and
microbiological study. J Indian Med Assoc.
2007;105:582-91.
VOLUME 48__JULY 17, 2011
Das könnte Ihnen auch gefallen
- Current AntibioticsDokument7 SeitenCurrent AntibioticsClarestaNoch keine Bewertungen
- Comparison of Amoxicillin/Clavulanic Acid High Dose With Cef Dinir in The Treatment of Acute Otitis MediaDokument8 SeitenComparison of Amoxicillin/Clavulanic Acid High Dose With Cef Dinir in The Treatment of Acute Otitis Mediaenggainget8663Noch keine Bewertungen
- Efficacy of Cefuroxime Axetil Suspension Compared To Penicillin V Susp in Children With Group A Streptococcal PharyngitisDokument5 SeitenEfficacy of Cefuroxime Axetil Suspension Compared To Penicillin V Susp in Children With Group A Streptococcal PharyngitisRobin ScherbatskyNoch keine Bewertungen
- PneumoniaDokument7 SeitenPneumoniaAldora OktavianaNoch keine Bewertungen
- EBN - Typhoid Fever FinalDokument5 SeitenEBN - Typhoid Fever FinalHeart CarambasNoch keine Bewertungen
- Current Antibiotic Use in The Treatment of EntericDokument26 SeitenCurrent Antibiotic Use in The Treatment of EntericReka Vikaria AnggreliaNoch keine Bewertungen
- Milk Oral Immunotherapy Is Effective in School-Aged ChildrenDokument6 SeitenMilk Oral Immunotherapy Is Effective in School-Aged ChildrenAnry UmarNoch keine Bewertungen
- A Multicenter, Double Blind Comparison of - MCLINN, SAMUELDokument15 SeitenA Multicenter, Double Blind Comparison of - MCLINN, SAMUELPutri FebrinaNoch keine Bewertungen
- Comparing Once-Daily Versus Twice-Daily Gentamicin Dosing in Preterm InfantsDokument31 SeitenComparing Once-Daily Versus Twice-Daily Gentamicin Dosing in Preterm InfantserniyulihapsariNoch keine Bewertungen
- Polyethylene Glycol vs. Lactulose in Infants and Children With Functional ConstipationDokument5 SeitenPolyethylene Glycol vs. Lactulose in Infants and Children With Functional ConstipationGabriela Peláez silvaNoch keine Bewertungen
- 10.1007@s12098 020 03454 1Dokument6 Seiten10.1007@s12098 020 03454 1rayhantaswinNoch keine Bewertungen
- JurnalDokument5 SeitenJurnalDio PattersonNoch keine Bewertungen
- Cefpodoxime Vs Cefixime in LRTI, IndianJPediatrDokument5 SeitenCefpodoxime Vs Cefixime in LRTI, IndianJPediatrAnonymous so6ZnlKyw100% (1)
- With Intravenous Antibiotics Urinary Tract Infections in 1-To 3-Month-Old Infants: Ambulatory TreatmentDokument9 SeitenWith Intravenous Antibiotics Urinary Tract Infections in 1-To 3-Month-Old Infants: Ambulatory Treatmentsri_jva8Noch keine Bewertungen
- Effect of Lactobacillus Sakei Supplementation in Children With Atopic Eczema - Dermatitis SyndromeDokument6 SeitenEffect of Lactobacillus Sakei Supplementation in Children With Atopic Eczema - Dermatitis SyndromePutri Halla ShaviraNoch keine Bewertungen
- Short-Course Antimicrobial Therapy For Pediatric Community-Acquired Pneumonia - PMCDokument19 SeitenShort-Course Antimicrobial Therapy For Pediatric Community-Acquired Pneumonia - PMCFrances Jean T. DoblasNoch keine Bewertungen
- Subjective Global Nutritional Assessment For Children: Donna J Secker and Khursheed N JeejeebhoyDokument7 SeitenSubjective Global Nutritional Assessment For Children: Donna J Secker and Khursheed N Jeejeebhoynurul_putrieNoch keine Bewertungen
- Efficacy of A New Hypotonic Oral Rehydration Solution Containing Zinc and Prebiotics in The Treatment of Childhood Acute Diarrhea: A Randomized Controlled TrialDokument6 SeitenEfficacy of A New Hypotonic Oral Rehydration Solution Containing Zinc and Prebiotics in The Treatment of Childhood Acute Diarrhea: A Randomized Controlled TrialOlpinNoch keine Bewertungen
- Multicenter Trial of A Combination Probiotic For Children With GastroenteritisDokument12 SeitenMulticenter Trial of A Combination Probiotic For Children With GastroenteritisCTV CalgaryNoch keine Bewertungen
- Lactobacillus Acidophilus and Bifidobacterium Bifidum Atored at Ambient Temperature Are Effective in The Treatment of Acute DiarrhoeaDokument7 SeitenLactobacillus Acidophilus and Bifidobacterium Bifidum Atored at Ambient Temperature Are Effective in The Treatment of Acute DiarrhoeaEvelynRuizNoch keine Bewertungen
- 388Dokument6 Seiten388anhiramdhaniNoch keine Bewertungen
- Saccharomyces boulardii May Shorten Diarrhea in ChildrenDokument5 SeitenSaccharomyces boulardii May Shorten Diarrhea in ChildrenShankar YadavNoch keine Bewertungen
- Oral Food Challenges in Children With A Diagnosis of Food AllergyDokument7 SeitenOral Food Challenges in Children With A Diagnosis of Food Allergyastuti susantiNoch keine Bewertungen
- Art:10.1007/s00431 007 0419 XDokument8 SeitenArt:10.1007/s00431 007 0419 XDini NanamiNoch keine Bewertungen
- Jurnal 2 AnakDokument5 SeitenJurnal 2 AnakHafich ErnandaNoch keine Bewertungen
- Andi PosterDokument10 SeitenAndi PosterChijioke Chioli PascalNoch keine Bewertungen
- Journal LL LL PediatriDokument4 SeitenJournal LL LL PediatriIndra PermanaNoch keine Bewertungen
- Gaviscon ClinicalDokument7 SeitenGaviscon ClinicalMuhammad Nadzri NoorhayatuddinNoch keine Bewertungen
- Comparing Efficacy and Tolerability of Ibuprofen Paracetamol FeverDokument4 SeitenComparing Efficacy and Tolerability of Ibuprofen Paracetamol FeverMonica Lauretta SembiringNoch keine Bewertungen
- What Is The Role of Antiemetics For Children With Acute Gastroenteritis in The Developing World?Dokument4 SeitenWhat Is The Role of Antiemetics For Children With Acute Gastroenteritis in The Developing World?Shafa AudryNoch keine Bewertungen
- Pediatrics 2013 Bivins S47Dokument3 SeitenPediatrics 2013 Bivins S47phobicmdNoch keine Bewertungen
- Pediatrics 2014 Queen E23 9Dokument10 SeitenPediatrics 2014 Queen E23 9Desrainy InhardiniNoch keine Bewertungen
- Lactobacillus Reuteri Helicobacter PyloriDokument8 SeitenLactobacillus Reuteri Helicobacter PyloriSrisailan KrishnamurthyNoch keine Bewertungen
- Gastroenteritis Therapies in Developed Countries: Systematic Review and Meta-AnalysisDokument21 SeitenGastroenteritis Therapies in Developed Countries: Systematic Review and Meta-AnalysisMarinaNoch keine Bewertungen
- SGNA NinosDokument7 SeitenSGNA NinosjorgeNoch keine Bewertungen
- Placebo-Controlled Trial of Antimicrobial Treatment for Acute Otitis MediaDokument6 SeitenPlacebo-Controlled Trial of Antimicrobial Treatment for Acute Otitis MediaegieprajaNoch keine Bewertungen
- Subjective Global Nutrition Assessment ChildrenDokument7 SeitenSubjective Global Nutrition Assessment Childrenmaricarmen IbarraNoch keine Bewertungen
- Controlled Trial Lansoprazole For Children With Poorly Controlled Asthma: A RandomizedDokument4 SeitenControlled Trial Lansoprazole For Children With Poorly Controlled Asthma: A RandomizedJames HollandNoch keine Bewertungen
- RCT Finds Gelatine Tannate Ineffective for Childhood GastroenteritisDokument39 SeitenRCT Finds Gelatine Tannate Ineffective for Childhood Gastroenteritiszaky ariandyNoch keine Bewertungen
- General Practice: Are Antibiotics Indicated As Initial Treatment For Children With Acute Otitis Media? A Meta-AnalysisDokument5 SeitenGeneral Practice: Are Antibiotics Indicated As Initial Treatment For Children With Acute Otitis Media? A Meta-AnalysisJuan Carlos Aguayo RomeroNoch keine Bewertungen
- Nutrients 10 01678Dokument11 SeitenNutrients 10 01678zulfa nadiaNoch keine Bewertungen
- High-Dose Versus Standard-Dose Amoxicillin/ Clavulanate For Clinically-Diagnosed Acute Bacterial Sinusitis: A Randomized Clinical TrialDokument15 SeitenHigh-Dose Versus Standard-Dose Amoxicillin/ Clavulanate For Clinically-Diagnosed Acute Bacterial Sinusitis: A Randomized Clinical TrialHendra EfendiNoch keine Bewertungen
- Tatistical Eview and Valuation: Linical TudiesDokument18 SeitenTatistical Eview and Valuation: Linical TudiesjoelrequenaNoch keine Bewertungen
- Efficacy of Probiotics in Acute Diarrhoea in Children: Original Research ArticleDokument5 SeitenEfficacy of Probiotics in Acute Diarrhoea in Children: Original Research ArticledwimellyndaNoch keine Bewertungen
- Lactobacillus rhamnosus GG vs Placebo for Acute Gastroenteritis in ChildrenDokument21 SeitenLactobacillus rhamnosus GG vs Placebo for Acute Gastroenteritis in ChildrenMarsella Epifania SuwignyoNoch keine Bewertungen
- Effect of A Probiotic Infant Formula On Infections in Child Care Centers Pediatrics-2005-Weizman-5-9Dokument7 SeitenEffect of A Probiotic Infant Formula On Infections in Child Care Centers Pediatrics-2005-Weizman-5-9Yuktika RiYuNoch keine Bewertungen
- On Dan SentronDokument7 SeitenOn Dan SentronLia MirawatiNoch keine Bewertungen
- High vs Standard Dose Amoxicillin for SinusitisDokument3 SeitenHigh vs Standard Dose Amoxicillin for SinusitisMarjhory Gianella Cardenas GutierrezNoch keine Bewertungen
- Acute Management of Pediatric Cyclic Vomiting Syndrome A Systematic ReviewDokument11 SeitenAcute Management of Pediatric Cyclic Vomiting Syndrome A Systematic ReviewNanda WibowoNoch keine Bewertungen
- Complementary and Alternative Medical Lab Testing Part 5: GastrointestinalVon EverandComplementary and Alternative Medical Lab Testing Part 5: GastrointestinalNoch keine Bewertungen
- Safety and Preliminary Efficacy On Cognitive Performance and Ada 2022 GenetiDokument10 SeitenSafety and Preliminary Efficacy On Cognitive Performance and Ada 2022 Genetironaldquezada038Noch keine Bewertungen
- Fernandez, John Michael BSN403 Group 10: I. Clinical QuestionDokument5 SeitenFernandez, John Michael BSN403 Group 10: I. Clinical QuestionJohn Michael FernandezNoch keine Bewertungen
- Children in The Tropics: Lactobacillus GG and Acute Diarrhoea in YoungDokument4 SeitenChildren in The Tropics: Lactobacillus GG and Acute Diarrhoea in YoungRaluca ElenaNoch keine Bewertungen
- Lactobacillus GG (LGG) and Smectite Versus LGG Alone For Acute Gastroenteritis: A Double-Blind, Randomized Controlled TrialDokument7 SeitenLactobacillus GG (LGG) and Smectite Versus LGG Alone For Acute Gastroenteritis: A Double-Blind, Randomized Controlled TrialTitis Sekar NingrumNoch keine Bewertungen
- Dietary Treatment of Atopic EczemaDokument5 SeitenDietary Treatment of Atopic EczemaClaudia CorjăuceanuNoch keine Bewertungen
- Thomas 1992Dokument9 SeitenThomas 1992ditaNoch keine Bewertungen
- Polyethylene Glycol 3350 in The Treatment of Chronic IdiopathicDokument8 SeitenPolyethylene Glycol 3350 in The Treatment of Chronic IdiopathicJose SalazarNoch keine Bewertungen
- TELAAH JURNAL INTERNASIONAL - Antik KritiyaniDokument12 SeitenTELAAH JURNAL INTERNASIONAL - Antik Kritiyaniandrea viqiNoch keine Bewertungen
- Pediatric Food Allergy: A Clinical GuideVon EverandPediatric Food Allergy: A Clinical GuideRuchi S. GuptaNoch keine Bewertungen
- Antibiotic Therapy of Pneumonia in The Obese PatientDokument12 SeitenAntibiotic Therapy of Pneumonia in The Obese PatientNadia DesiNoch keine Bewertungen
- Fast Exam2Dokument30 SeitenFast Exam2Kelvin MandelaNoch keine Bewertungen
- Aggressive vs. Conservative Phototherapy For Infants With Extremely Low Birth WeightDokument12 SeitenAggressive vs. Conservative Phototherapy For Infants With Extremely Low Birth WeightNadia DesiNoch keine Bewertungen
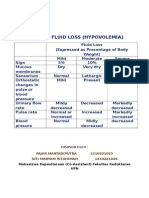
- Signs of Fluid LossDokument3 SeitenSigns of Fluid LossSheilla RatnasariNoch keine Bewertungen
- Epilepsy DR LindaDokument8 SeitenEpilepsy DR LindaLaylaNoch keine Bewertungen
- Chapter 3: Bacteria: Thiomargarita Namibiensis - 5 M in DiameterDokument6 SeitenChapter 3: Bacteria: Thiomargarita Namibiensis - 5 M in DiameterShairaMNoch keine Bewertungen
- Prestigi0us BiochemistryDokument30 SeitenPrestigi0us Biochemistrybovey69015Noch keine Bewertungen
- CU DFScience Notes Bacteria General Dairy Micro 06 10 PDFDokument10 SeitenCU DFScience Notes Bacteria General Dairy Micro 06 10 PDFjoel osortoNoch keine Bewertungen
- Atc DDD OlukaDokument65 SeitenAtc DDD Olukarini setyawatiNoch keine Bewertungen
- Group 2 Research G8Dokument24 SeitenGroup 2 Research G8aurasaliseNoch keine Bewertungen
- DR.ZHU'S SCALP ACUPUNCTURE GUIDEDokument25 SeitenDR.ZHU'S SCALP ACUPUNCTURE GUIDEMajid Mushtaq100% (2)
- CPT Exam Study Guide: Health AssessmentsDokument3 SeitenCPT Exam Study Guide: Health Assessmentssiriamma wiliamsNoch keine Bewertungen
- Principles and Practice of Single Implant and Restoration - Saunders 1 Edition (March 26, 2013)Dokument204 SeitenPrinciples and Practice of Single Implant and Restoration - Saunders 1 Edition (March 26, 2013)Sergiu Pinte100% (1)
- Safety Data Sheet for Fiber Glass Fabric FG-100Dokument5 SeitenSafety Data Sheet for Fiber Glass Fabric FG-100Chukwuma Emmanuel OnwufujuNoch keine Bewertungen
- RT MapehDokument2 SeitenRT MapehRowan ImperialNoch keine Bewertungen
- Teriparatide, Vitamin D, Cinacalcet, SevelamerDokument2 SeitenTeriparatide, Vitamin D, Cinacalcet, SevelamerJosh KalishNoch keine Bewertungen
- Nettle Rash Symptoms, Causes, TreatmentDokument2 SeitenNettle Rash Symptoms, Causes, TreatmentArdave Laurente100% (1)
- Pneumonia: Causes, Signs, Symptoms and Nursing CareDokument16 SeitenPneumonia: Causes, Signs, Symptoms and Nursing CareMelissa David100% (1)
- Med 1 Block 2 - Wet Lab NotesDokument36 SeitenMed 1 Block 2 - Wet Lab NotesluckyNoch keine Bewertungen
- Chiropractic Treatment Techniques-2016Dokument9 SeitenChiropractic Treatment Techniques-2016Dr. Mateen ShaikhNoch keine Bewertungen
- Emropub 2016 en 19266Dokument45 SeitenEmropub 2016 en 19266jamshaidjiNoch keine Bewertungen
- Mark Scheme Unit f211 Cells Exchange and Transport June PDFDokument17 SeitenMark Scheme Unit f211 Cells Exchange and Transport June PDFAngkelova ChristinaNoch keine Bewertungen
- TS Report en WebdownloadDokument175 SeitenTS Report en WebdownloadMartin NardoNoch keine Bewertungen
- A Novel Technique For Pudendal Nerve BlockDokument4 SeitenA Novel Technique For Pudendal Nerve Blockmohs2007100% (1)
- AntihypertensivesDokument35 SeitenAntihypertensivesjanuajipatriaNoch keine Bewertungen
- Internship Report JackDokument85 SeitenInternship Report JackdamarismagererNoch keine Bewertungen
- Aapi Ebook June 19 2017Dokument621 SeitenAapi Ebook June 19 2017AAPIUSANoch keine Bewertungen
- Chronic Medical IssuesDokument9 SeitenChronic Medical IssuesomoshNoch keine Bewertungen
- The Concept of NeuropsychiatryDokument10 SeitenThe Concept of NeuropsychiatryOscar Adrian Carmona NietoNoch keine Bewertungen
- Iet Me Introduce My Name Najib MahfuzhDokument2 SeitenIet Me Introduce My Name Najib MahfuzhnajibNoch keine Bewertungen
- Biology Curriculum MapDokument2 SeitenBiology Curriculum Mapapi-644434957Noch keine Bewertungen
- Kidney 4.1.0.0.rel CapcpDokument18 SeitenKidney 4.1.0.0.rel CapcpkarimahihdaNoch keine Bewertungen
- Zbornik Limes Vol 2Dokument354 SeitenZbornik Limes Vol 2Morrigan100% (1)
- Medication SafetyDokument180 SeitenMedication SafetyAengus JoyceNoch keine Bewertungen