Beruflich Dokumente
Kultur Dokumente
Vascular Disease in Rheumatoid Arthritis From Subclinical Lesions To
Hochgeladen von
Mihaela IonescuCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Vascular Disease in Rheumatoid Arthritis From Subclinical Lesions To
Hochgeladen von
Mihaela IonescuCopyright:
Verfügbare Formate
European Journal of Internal Medicine 20 (2009) 348354
Contents lists available at ScienceDirect
European Journal of Internal Medicine
j o u r n a l h o m e p a g e : w w w. e l s ev i e r. c o m / l o c a t e / e j i m
Review article
Vascular disease in rheumatoid arthritis: From subclinical lesions to
cardiovascular risk
Coman Tanasescu a,d,, Ciprian Jurcut b, Ruxandra Jurcut c,d, Carmen Ginghina c,d
a
Department of Internal Medicine, Colentina Clinical Hospital, Bucharest, Romania
3rd Internal Medicine Department, Carol Davila Central Clinical Emergency Military Hospital, Bucharest, Romania
Department of Cardiology, Prof. Dr. C. C. Iliescu Institute of Cardiovascular Diseases, Bucharest, Romania
d
University of Medicine and Pharmacy Carol Davila, Bucharest, Romania
b
c
a r t i c l e
i n f o
Article history:
Received 13 March 2008
Received in revised form 31 July 2008
Accepted 4 September 2008
Available online 19 October 2008
Keywords:
Rheumatoid arthritis
Cardiovascular disease
Endothelial dysfunction
Vascular stiffness
Statins
a b s t r a c t
Rheumatoid arthritis (RA) is one of the most prevalent and complex inammatory diseases affecting primarily
the joints, but also associating several extra-articular features. The vascular disease in RA encompasses a large
spectrum of lesions, from rheumatoid vasculitis to atherosclerotic lesions. During the last years the importance
of the vascular disease related to atherosclerosis in terms of cardiovascular morbidity and global mortality
became evident in RA. The inammatory hypothesis of atherosclerosis in RA implies that mediators originating
from the inamed synovial tissue or from the liver may have systemic vascular consequences, leading to
endothelial dysfunction and structural abnormalities of the vessels. Hence, the global management of patients
with RA must include the improvement of cardiovascular risk in parallel with the management of joint disease.
2008 European Federation of Internal Medicine. Published by Elsevier B.V. All rights reserved.
1. Introduction
Rheumatoid arthritis is one of the most prevalent inammatory
diseases in the general population. While the most important
pathogenic lesion is the inammatory synovitis, the extraarticular
features are equally important, considering the fact that inammation
has a systemic magnitude. From this point of view, a large spectrum of
cardiac and vascular involvements in RA (i.e. valvular, myocardial and
pericardial disease, coronary artery disease, myocardial infarction,
stroke, heart failure, vasculitis lesions, cardiac rheumatoid nodules,
echocardiographic abnormalities as diastolic dysfunction and pulmonary hypertension) was already described.
The vasculitic lesions the presence of the inammatory lesions in
the vessel walls although not very frequent, were the rst reported.
Thus, for decades, the vascular disease in RA was synonymous with
the presence of rheumatoid vasculitis. During the last years,
accumulation of new data made evident the existence of great
diversity of vascular involvement in RA (Table 1), which encompasses
the entire spectrum of vascular lesions and the clinical manifestations
determined by these lesions. Among these, large longitudinal studies
performed in the last years reported a high prevalence of athero-
Corresponding author. Department of Internal Medicine, Colentina Hospital,
Soseaua Stefan cel Mare 19-21, sect. 2, 020125 Bucharest, Romania. Tel./fax: +40
212107326.
E-mail address: ctnsescu@b.astral.ro (C. Tanasescu).
sclerosis related lesions in the patients with RA and their enormous
importance regarding the long-term prognostic. Regardless the
vascular territory involved (coronary, cerebral, renal or peripheral
arteries), the presence of these lesions leads to the occurrence of
specic symptoms and, nally, to an increased prevalence of
cardiovascular disease and increased mortality. Moreover, nowadays
most authors consider the improvement of this increased cardiovascular risk as one of the most important measures in the global
management of patients with RA, and therefore some specic
recommendations regarding this issue were released [1].
The aim of this article is to review the most important vascular
lesions in patients with RA, especially those related to atherosclerosis
and associated with an increased cardiovascular risk, and the most
clinically relevant measures to improve this risk.
2. Rheumatoid vasculitis
Classically, the main vascular involvement in RA was considered the
rheumatoid vasculitis. Regarded as an extraarticular feature, rheumatoid vasculitis is relatively rare and has specic clinical manifestations,
diagnostic criteria and therapeutic approaches (corticosteroids,
immunosupressors and, recently, the biologic therapies). The importance of subclinical vasculitis lesions, reported at systematic biopsies,
is unclear until now. The pathogenic criteria for the diagnostic of
rheumatoid vasculitis were described, the brinoid necrosis and
inammatory inltrate in the vessel's wall being the most frequent
0953-6205/$ see front matter 2008 European Federation of Internal Medicine. Published by Elsevier B.V. All rights reserved.
doi:10.1016/j.ejim.2008.09.005
C. Tanasescu et al. / European Journal of Internal Medicine 20 (2009) 348354
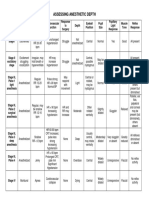
Table 1
Spectrum of vascular disease in patients with rheumatoid arthritis [24].
Rheumatoid vasculitis
Atherosclerosis related vascular disease
Subclinical arterial disease
Endothelial dysfunction
Increased arterial stiffness
Increased intima-media thickness
High prevalence of asymptomatic atherosclerotic plaques
Increased coronary artery calcications score on cardiac computed tomography
Impaired coronary ow reserve
Clinical arterial disease (especially coronary heart disease, but also cerebral or
peripheral vascular disease)
Pulmonary hypertension
Secondary to pulmonary disease (interstitial pulmonary disease)
Directly related with PR
Venous disease (increased risk for deep vein thrombosis and for thromboembolic
events)
[5]. Leucocytoclastic vasculitic lesions might be present [6], but with a
lower specicity. Ischemic symptoms in different vascular beds,
including coronary arteries, might occur and are difcult to differentiate clinically from atherosclerosis-related events. Until now, it is
unclear if the vasculitis lesions play any role as predictors for the
development of atherosclerotic lesions and for cardiovascular disease.
3. Atherosclerotic vascular disease
Recent studies showed the great importance of atherosclerosis
related lesions in patients with RA. In these patients, the atherosclerotic lesions occur earlier and have a more rapid evolution than in
general population and some authors proposed the terms accelerate
atherosclerosis or premature atherosclerosis to underline the
magnitude of this process in RA. Thus, beyond clinically overt
cardiovascular disease, most authors reported the importance of
subclinical or silent vascular disease in patients with RA.
3.1. Overt cardiovascular disease
Large studies showed the increased prevalence of overt clinical
cardiovascular disease and the great cardiovascular mortality in
patients with RA [2]. Wallberg-Jonsson et al. reported that the
mortality ratio for cardiovascular disease (1.46) and for ischemic
heart disease (1.54) were higher in patients with RA compared to
control population [7]. The analysis of the large cohort from Nurses'
Health Study [8] reveals an increased adjusted relative risk for
myocardial infarction in women with RA and the relative risk for
myocardial infarction was higher in patients with a time from
diagnosis of RA more than 10 years. Fischer et al. also reported an
increased risk for myocardial infarction in patients with RA, and this
risk was dramatically augmented by the coexistence of hyperlipidemia
[9]. Turesson et al. showed that the mortality excess in patients with
RA is mainly determined by the high prevalence of myocardial
infarction [10]. Very important, the prevalence of unrecognized
myocardial infarction and sudden death is more important in patients
with RA [11]. Also, a great prevalence for stroke [12,13] and for
peripheral arterial disease [14] was described in RA.
3.2. Subclinical vascular disease
3.2.1. Endothelial dysfunction
Dened as an abnormal or inappropriate response of the vascular
wall to physiological vasodilator stimulus, endothelial dysfunction is
considered one of the most important components of physiopathological processes which promote atherosclerosis. Endothelial dysfunction was reported in patients with RA [15], even in the early diagnosed
arthritis [16] or in young patients [17], and was correlated with the
inammatory status [18] or with the rheumatoid factor levels [19].
349
Gonzales-Juanatey et al. reported the inuence of HLA-DRB1 alleles on
endothelial function in these patients, nding that in the HLADRB10404 patients endothelial dysfunction was more important
[15].
3.2.2. Arterial stiffness
Arterial stiffness is regarded now as an important cardiovascular
risk factor [20] and some specic techniques are now available for its
assessment, some of which are not yet readily usable in daily clinical
practice (e.g. the pulse wave analysis techniques). In patients with RA,
an increased arterial stiffness was reported [21], which was linked
with the disease duration [22,23], the specic disease activity scores
used in RA [24], the patients age, the CRP values [25] and with the
coronary atherosclerosis [26].
3.2.3. Increased arterial intima-media thickness
The increase of intima-media thickness (IMT), evaluated in
different vascular territories, was correlated with an increased risk
for atherosclerotic lesions and cardiovascular events [27]. In patients
with RA, IMT is increased [28] and correlate not only with traditional
cardiovascular risk factors [29], but also with disease severity [30] and
duration [31], the use of corticosteroids [32], with values of CRP [33] or
erythrocyte sedimentation rate (ESR) [34], with the presence of
anticardiolipin antibodies [35] or von Willebrand factor values [36]. La
Montagna et al. showed that, in patients with RA, insulin resistance,
diastolic blood pressure and corticosteroids use were the independent
predictors of an increased IMT [32]. Almost all studies that evaluated
the presence of atherosclerotic plaques showed that an increased IMT
is an important predictor for these plaques.
3.2.4. Subclinical atherosclerotic plaques
In patients with RA, an increased prevalence of arterial atherosclerotic plaques than in controls was described. The presence of these
plaques was correlated with the traditional cardiovascular risk factors
[37,38], the systemic inammation [30], disease duration [39],
radiological damage [40], PMN levels or hypothyroid status [39,40].
While the screening for atherosclerotic plaques is not yet particularly
indicated in patients with RA, the identication of these plaques needs
an active approach of cardiovascular risk factors control.
3.2.5. Other subclinical vascular lesions
In patients with RA, the coronary ow reserve a transthoracic
echocardiography measure of coronary ow and a marker of coronary
atherosclerotic disease [41] is reduced in patients with RA, and
negatively correlated with disease duration [42]. Coronary artery
calcications score, evaluated by electron-beam computed tomography, is a non-invasive marker of coronary atherosclerosis. In patients
with RA, the calcium score at the level of coronary arteries was found
to be higher than in controls and positively correlated with the
smoking status and values of ESR [43] and with the duration of the
disease [44].
4. Physiopathological hypotheses
4.1. Traditional cardiovascular risk factors
All these observations linking RA to an increased atherosclerotic
burden and cardiovascular risk raise several physiopathological
hypotheses. The traditional risk factors were the rst studied when
the cardiovascular risk in patient with RA became evident. However,
the prevalence of traditional cardiovascular risk factors was found to
be similar in patients with RA and controls, except for smoking which
was more prevalent in RA, and the impact of these factors is less
important in RA than controls [45]. Moreover, the multivariate
analyses and the comparison with control populations failed to
bring us the clear evidence in order to consider them as independents
350
C. Tanasescu et al. / European Journal of Internal Medicine 20 (2009) 348354
risk factors for cardiovascular disease in patients with RA. Interestingly, a low BMI was associated with an increased cardiovascular risk
in patients with RA [46]. However, the qualitative modications of
HDL were reported in patients with RA and SLE. In these patients, a
proinammatory HDL a type of HDL which does not protect LDL
from oxidation was reported to be a possible link between the
inammation and atherosclerosis [47]. Moreover, in these patients,
treatment with 80 mg atorvastatin per day shifted the HDL towards
the anti-inammatory type [48], bringing the evidence supporting the
benecial role of statins in RA (see bellow).
4.2. Atherosclerosis and inammation
Atherosclerosis is regarded as an inammatory disease and several
inammation mediators and inammatory cells are interconnected in
complex mechanisms that promote vascular structural and functional
abnormalities [49]. The inammatory mechanisms were reported to
be involved in all stages of atherosclerosis and in the processes that
lead to vulnerable plaque as well as vascular events. The inammatory
cascade in the vessel wall includes: cellular inltration (including
macrophages and T lymphocytes, mainly CD4+ T-cells, and promoting Th1 response [50]), intercellular signaling (cytokines, including
TNF- and interleukin-1, adhesion molecules, chemoattractants,),
matrix metalloproteinases, oxidative stress, endothelial cells activation [49,51]. However, the precise nature of antigen stimulus that
promotes inammatory response in the vessel wall is still unknown.
4.3. Synovial and systemic inammation promoting atherosclerosis in RA
Once the atherosclerosis paradigm was shifted toward the
inammatory mechanisms, this hypothesis becomes attractive in
patients with RA, well known as a high-grade inammatory status.
Relevant hypotheses were developed in order to explain the active
implication of inammation mediators in the processes that promote
atherosclerosis and vascular lesions in patients with RA [52].
Overall, the inammatory hypothesis of atherosclerosis in RA
implies that mediators originating from inamed synovial tissue (i.e.
TNF-) or from the liver (i.e. CRP or brinogen) may have systemic
vascular consequences leading to endothelial dysfunction and
structural abnormalities of the vessels. Some characteristics of the
disease itself were reported to be linked with the cardiovascular
disease. Thus, the number of swollen joints [53] and the extraarticular features [54], reecting the magnitude of systemic inammation, was reported to be associated with the cardiovascular disease
in RA. The positivity for rheumatoid factor (RF) was related with
cardiovascular mortality in patients with early polyarthritis [55], but
the role of RF as a marker for cardiovascular disease needs further
studies.
One of the most extensively studied inammatory markers during
the last years is C-reactive protein (CRP). Large prospective studies
showed that high levels of CRP are strong predictors of cardiovascular
disease in general population [56,57] and for cardiovascular events in
patients with acute coronary syndromes [58,59]. Otherwise, recent
studies showed that CRP is not only a simple marker of an increased
cardiovascular risk, but also an active participant in several pathways
that promote atherosclerosis and endothelial dysfunction, interacting
with endothelial and inammatory cells to increase proinammatory
cytokines levels, adhesion molecules expression, inammatory cell
recruitment and oxidative stress [60]. Recent guidelines emphasized
the importance of CRP in the cardiovascular risk assessment
strategies. In RA, high levels of CRP were observed and CRP is used
in clinical practice as a useful marker of inammatory status.
Moreover, the levels of CRP were reported to predict the cardiovascular mortality in patients with inammatory polyarthritis followed
over 10 years [61]. It must be noted that values of CRP in RA are higher
than levels proposed for cardiovascular risk stratication in the
general population [62]. In consequence, and according with actual
guidelines, the determination of CRP seems not to be useful for risk
stratication and for optimal therapy decision making in patients with
RA and cardiovascular diseases. Otherwise, further studies are
required in RA patients with or without cardiovascular disease in
order to establish possible thresholds for CRP in cardiovascular risk
stratication assessment.
Representing a key factor in the mechanisms of RA, tumor necrosis
factor- (TNF-) levels are increased in this population, representing
the basis of anti TNF- therapies developed during last years [63].
Regarding the cardiovascular risk, the levels of soluble TNF receptors
were reported to predict total and cardiovascular mortality in patients
with RA [64]. In several studies performed during last years, its
pleiotropic properties, including proinammatory activity, were
linked to atherosclerosis, the high levels of TNF- being predictive
for recurrent coronary events in patients with myocardial infarction
[65]. TNF- increases the adhesion molecules expression and
interleukin-6 (IL-6) synthesis and promotes endothelial dysfunction
by reducing the NO availability [66]. Also, TNF- is one of the
determinants of insulin resistance, another important cardiovascular
risk factor [67].
Produced by several inammatory cells, IL-6 levels are also
increased in patients with RA [68]. Although the role of IL-6 in the
pathogenesis of joint inammation and damage in RA is still only
partially understood, it might be one of the humoral mediators that
promote the development of vascular changes and the occurrence of
cardiovascular events. IL-6 increases the hepatic synthesis of CRP and
brinogen, increases the expression of adhesion molecules and
enhances platelets aggregability [69].
Probably, this hypothesis which links synovial and systemic
inammation to atherosclerotic burden and cardiovascular risk is
not exclusive, and other factors (see below) are also linked to
atherosclerosis in patients with RA.
4.4. Other related factors
Klimiuk et al. showed that serum levels of soluble intercellular
adhesion molecule-1 (sICAM-1), soluble vascular cell adhesion molecule-1 (sVCAM-1), E-selectin (sE-selectin) are increased in patients with
RA versus patients with osteoarthritis [70]. In the general population and
in patients with overt cardiovascular disease or acute coronary
syndromes, soluble cell adhesion molecules were related with an
increased cardiovascular risk and increased levels of these molecules are
strong predictors for future cardiovascular events [71].
In patients with RA, the levels of endothelial progenitor cells (EPC)
are lower than in controls [72]. Studies performed in general
population reported the inverse association between the levels of
endothelial progenitor cells and cardiovascular risk [73]. Thus, in
patients with RA this risk might be related with these reduced levels of
endothelial progenitor cells. Recently, Grisar et al. reported the
inuence of TNF in the reduction of EPC in patients with RA and the
effect of intermediate doses of glucocorticoids in increasing these
levels [74].
Osteoprotegerin, a member of TNF receptors super-family involved
in the bone metabolism and that was linked with coronary lesions in
general population [75], was reported to be associated with the
coronary-artery calcications in patients with RA [76]. In these
patients with RA the levels of osteoprotegerin were higher than in
controls [77].
Prothrombotic factors were equally studied in order to explain the
cardiovascular risk in RA. Thus, Jurcut et al. reported increased values
for platelets indices and for brinogen levels in RA patients with
cardiovascular disease [78]. Some alleles for PAI-1 were described in
patients with RA as carrying an increased cardiovascular risk [79].
Other factors linked with the cardiovascular disease in patients
with RA are the higher serum acid levels [80] and the increased
C. Tanasescu et al. / European Journal of Internal Medicine 20 (2009) 348354
prevalence of hypothyroidism [81]. Homocysteine was also proposed
as a potential cardiovascular factor in RA [82]. The prevalence of
metabolic syndrome was found to be higher in RA patients than
controls and its presence was correlated with the score for coronary
artery calcications [83]. The genetic background was proposed to
modulate the cardiovascular risk and HLA-DRB10404 alleles were
found to be associated with the higher risk [84]. Moreover, the
patients with RA are less physically active than general population
[85].
5. How to detect cardiovascular disease in patients with RA?
In daily clinical practice, the detection of cardiovascular disease in
patients with RA must follow the guidelines available in general
population. The European Society of Cardiology guideline regarding
the cardiovascular risk assessment in general population recommends
the use of a SCORE chart and emphasized the higher risk of those with
evidence of pre-clinical atherosclerotic disease [86].
In patients with overt cardiovascular disease, the diagnostic
modalities are the same than in general population. The exercise
test might be less important because in some patients the exercise
capacity is limited. Thus, other stress imaging modalities (e.g.
ultrasound techniques with pharmacological stress) should be
ordered in the diagnostic algorithms.
Until now, the importance of the screening for subclinical lesions,
as an increased IMT, the magnitude of prediction for the major
cardiovascular events and the role of newer biological therapies in
reducing the IMT in patients with RA are unclear. Hence, the
evaluation of subclinical vascular disease in routine clinical practice
is not particularly recommended in these patients.
6. The treatment of RA and the cardiovascular risk
Glucocorticoid therapy was associated with an increased risk for
hypertension [87,88] and for cardiovascular events [89]. Davis et al.
reported an increased risk for adverse cardiac events following
glucocorticoid treatment in patients positive for rheumatoid factor
(RF) and not in those negative for RF [90]. However, the inuence of
different doses and durations of treatment regarding the cardiovascular risk is still incompletely elucidated. The treatment with low
doses of prednisolone was not associated with a benecial effect on
endothelial function in patients with RA [91]. However, the long term
effects of different doses of glucocortocoids on the cardiovascular risk
need more evidences. Some practical recommendations regarding the
cardiovascular risk and the specic treatments in patients with RA are
presented in Table 2.
The data regarding the cardiovascular risk of the non-steroidal
anti-inammatory drugs (NSAID) are still conicting. However, data
has built in the literature suggesting to avoid coxib use, because of the
reported increase in cardiovascular risk. During the last years,
epidemiological and experimental studies brought us relevant
information regarding this risk. The selective inhibition of cyclooxygenase-2 (COX-2) leads to an imbalance between thromboxane and
prostacyclin, favoring the former and promoting a prothrombotic
status. Some of the coxibs (i.e. rofecoxib) were withdrawn from the
market, and other are now commercialized with some cautions
regarding the cardiovascular risk. Recently, Solomon et al. reported
the dose-dependent effects of celecoxib on cardiovascular risk, mainly
for the high-risk patients [92]. Thus, a careful assessment of the
individual cardiovascular risk should be performed in all candidates to
these drugs and the use of the lower doses is mandatory [93].
Regarding the traditional, nonselective NSAIDs, the data are still
conicting, and a metaanalysis of randomized studies found that high
doses of ibuprofen or diclofenac were associated with an increased
cardiovascular risk, while the high doses of naproxen were not related
with such a risk [94]. In the McGettigan metaanalysis, only diclofenac
351
Table 2
RA therapy and cardiovascular risk: some practical issues.
Glucocorticoids
Use the lower doses
Limit of the duration of the treatment
Do the cardiovascular risk factors screening and monitoring (blood pressure, blood
glucose and lipids levels) at the beginning of the treatment and periodically
Initiate the management of cardiovascular risk factors during the treatment (lipid
disorders and blood glucose control, treatment of hypertension, smoking cessation and
weight loss)
In patients positive for RF, the control of cardiovascular risk factors must be more
aggressive
Non-steroidal anti-inammatory drugs
Avoid selective COX-2 inhibitors
For nonselective NSAID the data are conicting and the prescription must be
individualized taking into account several factors (see text)
DMARDs
Methotrexate and, possibly, sulfasalazine seems to be associated with a lower
cardiovascular risk in patients with RA.
Until now, the use of the specic DMARDs must follow the guidelines for the
disease control, because there are no specic recommendations for cardiovascular risk
management
Anti-TNF treatment
Only studies in subclinical vascular disease; no studies with clinically relevant endpoints (cardiovascular death, myocardial infarction)
No specic recommendations for cardiovascular risk management
was related with an increased cardiovascular risk, while ibuprofen,
piroxicam and naproxen were not [95]. As the cardiovascular risk of
the traditional NSAIDs is still a matter of debate, American Heart
Association recently released a clinically useful stepped algorithm
regarding the prescription of the NSAIDs and cardiovascular risk. This
statement emphasizes the need of cardiovascular risk assessment and
to individualize the prescription taking into account the risk for
gastro-intestinal bleedings, the non-responsiveness to analgesics and
the need to co-administrate the aspirin in cardioprotective doses [93].
Also, this document underlies the fact that the co-administration of
aspirin and ibuprofen require some precautions.
Regarding the inuence of specic DMARDs in cardiovascular risk
in patients with RA, the dates are still insufcient. The use of
methotrexate, was associated with a reduced cardiovascular risk in
these patients [96] and with lower values of IMT than patients nontreated [97]. Sulfasalazine was reported to be associated with a lower
cardiovascular risk [98]. Hydroxychloroquine was reported to improve
the lipid prole [99] and to reduce the risk of diabetes in patients with
RA [100], but the global effects for cardiovascular risk need further
studies.
Recently, the treatment with TNF- blockers was reported as
having favorable effects on endothelial dysfunction in patients with
RA. Interestingly, until now, the prospective studies performed in
patients with RA evaluated the inuence of some specic therapies
only in subclinical lesions. Thus, Hurlimann et al. reported the
improvement of endothelial dysfunction, evaluated by ow-mediated
dilatation in 11 patients with PR, after 12 weeks of treatment with
iniximab [101]. Cardillo et al. reported the improvement of the
response to acetylcholine (evaluated by a pletismographic method)
after the administration of iniximab in a group of patients with early
arthritis [102]. Moreover, some authors suggested a transitory effect of
iniximab on endothelial function that disappeared after one month
after perfusions, in a group of patients already treated with iniximab
over one year [103]. Thus, similarly with the possible antibody related
transitory effect of iniximab on disease activity after a period of time,
it is possible that these benecial effects on endothelial function are
transient. With regard to vascular stiffness, the treatment with an
anti-TNF- (etanercept, for 12 weeks) diminished the aortic stiffness
and improved the endothelial dysfunction [25]. Van Dornum et al.
352
C. Tanasescu et al. / European Journal of Internal Medicine 20 (2009) 348354
reported that there are not differences in arterial stiffness after
6 weeks of treatment with anti-TNF blockers (iniximab, etanercept
or adalimumab) [104]. As the great majority of studies used the
iniximab of etanercept, further studies are required in order to assess
the effects of the others TNF blockers or biological therapies
(abatacept or rituximab). Moreover, it is very important to design
long-term studies in patients treated with biological therapies using
hard end-points as total or cardiovascular mortality. There are recent
studies which reported an unfavorable effect of anti-TNF agents on
lipid prole, especially on total cholesterol, in patients with RA [105
107]. However, the data reported until now are conicting and the
results of these studies must be interpreted cautiously and taking into
account the short and long term effects and the global effects on
cardiovascular disease. Although some studies that evaluated the
effects of new biological therapies on endothelial dysfunction and
arterial rigidity are now available, the effects on cardiovascular events
and mortality need further studies.
7. Improvement of vascular disease with statins in patients
with RA
Statins, largely used in clinical practice for their hypolipemiant
effects but also having some anti-inammatory properties, were used
in patients with RA in order to reduce the inammation and disease
activity [108] and to improve the vascular function. Using the results
of the large primary and secondary prevention trials with statins in
general population, it is reasonable to think that their use in patients
with RA might improve also the cardiovascular risk.
The treatment with statins seams to be an alternative or
complementary therapeutic option in order to improve the endothelial dysfunction. Studies performed in the general population showed
the improvement of endothelial dysfunction in patients treated with
statins [109]. Fluvastatin improved the endothelial dysfunction in
mice with experimental arthritis [110], but supplementary studies are
necessary in patients with rheumatoid arthritis.
Similarly with the studies with statins performed in other
populations, the treatment with 20 mg of atorvastatin for 12 weeks,
improved the arterial stiffness in a group 29 patients with RA [111].
Not only statins, but also ezetimibe improves the endothelial
dysfunction and vascular stiffness in patients with RA and also the
disease activity score, suggesting positive anti-inammatory effects of
the cholesterol lowering itself [112].
8. Global cardiovascular risk management in patients with RA
Generally, the goals of treatment in patients with RA are the
control of inammation at the joints level and the prevention of
irreversible joint destructions. In the same time, the majority of the
guidelines emphasized the great importance of the comorbidities
management, among which the cardiovascular disease has a great
importance. The cardiovascular risk stratication process must be
performed ever since diagnosis and the efforts to improve this risk
must advances in parallel with the classical control disease management. Thus, as in general population, the lifestyle modications
(smoking cessation, optimization of the diet and weight loss), the
control of blood pressure, of the cholesterol or blood glucose values
must be regarded as an important steps in the global management of
RA, even in the absence of clinically manifested cardiovascular
disease. The administration of the lowest doses of corticoids must
be encouraged. Once the cardiovascular disease became clinically
apparent, its management must follow the general recommendations.
9. Conclusions
In patients with RA, vascular function and structure might be
altered leading to an increased prevalence for cardiovascular disease
Fig. 1. Cardiovascular disease continuum in patients with rheumatoid arthritis.
and for cardiac death (see Fig. 1). The subclinical vascular disease
encompasses a large spectrum of functional (as endothelial dysfunction, increased vascular stiffness or reduced coronary ow reserve)
and structural damage (as an increased intima-media thickness or a
high prevalence of asymptomatic plaques). In these patients, there is
also a high prevalence of clinical cardiovascular disease (i.e. myocardial
infarction) and, consequently, of cardiovascular mortality. The inammatory pathways were hypothesized to be involved in the pathogenesis of vascular disease in RA. Some specic treatments of RA might
interfere with cardiovascular risk (e.g. glucocorticoids seem to increase
this risk and methotrexate seems to reduce it). The newer treatments,
involving the TNF-alpha pathways, were reported to improve the
subclinical vascular disease in RA. Statins might also be one of the
therapeutic options in order to reduce the global cardiovascular risk.
More studies are necessary to assess the role of different therapies in
decreasing cardiovascular risk in patients with RA.
10. Learning points
Rheumatoid arthritis affects primarily the joints, but a large
spectrum of extra-articular features was described. Among these
extra-articular features, cardiovascular disease has a great importance regarding the long-term prognosis in patients with RA.
The vascular involvement in RA might be silent or subclinical, and
these morphological or functional alterations might be considered
as an early stage of atherosclerosis.
In RA a high prevalence of ischemic heart disease and particularly of
myocardial infarction was described.
Inammatory pathways seem to be linked with the cardiovascular
risk in patients with RA.
The new biological agents (e.g. TNF blockers) might improve the
endothelial dysfunction and arterial stiffness in patients with RA.
The impact of the newer therapies used in RA on global
cardiovascular risk needs further studies.
The treatment with some DMARDs (especially with metothrexate)
was associated with a reduction of cardiovascular risk. The
treatment with glucocorticoids might be associated with an
increased cardiovascular risk.
In patients with RA the management of cardiovascular risk is now
regarded as a part of global management and the evaluation and
treatment of traditional cardiovascular risk factors must be done in
every patient.
Statin therapy might be a valuable option in order to reduce the
cardiovascular risk in RA.
References
[1] Pham T, Gossec L, Constantin A, Pavy S, Bruckert E, Cantagrel A, et al.
Cardiovascular risk and rheumatoid arthritis: clinical practice guidelines based
on published evidence and expert opinion. Joint Bone Spine 2006;73:37987.
[2] Jurcut C, Jurcut R, Tanasescu C. Cardiovascular risk and rheumatoid arthritis: from
mechanisms of atherosclerosis to therapeutic approach. Rom J Intern Med
2004;42:65969.
C. Tanasescu et al. / European Journal of Internal Medicine 20 (2009) 348354
[3] Liang KP, Liang KV, Matteson EL, McClelland RL, Christianson TJ, Turesson C.
Incidence of noncardiac vascular disease in rheumatoid arthritis and relationship
to extraarticular disease manifestations. Arthritis Rheum 2006;54:6428.
[4] Dawson JK, Goodson NG, Graham DR, Lynch MP. Raised pulmonary artery
pressures measured with Doppler echocardiography in rheumatoid arthritis
patients. Rheumatology 2000;39:13205.
[5] Genta MS, Genta RM, Gabay C. Systemic rheumatoid vasculitis: a review. Semin
Arthritis Rheum 2006;36:8898.
[6] Koutkia P, Mylonakis E, Rounds S, Erickson A. Leucocytoclastic vasculitis: an
update for the clinician. Scand J Rheumatol 2001;30:31522.
[7] Wallberg-Jonsson S, Ohman ML, Dahlqvist SR. Cardiovascular morbidity and
mortality in patients with seropositive rheumatoid arthritis in Northern Sweden.
J Rheumatol 1997;24:44551.
[8] Solomon DH, Karlson EW, Rimm EB, Cannuscio CC, Mandl LA, Manson JE, et al.
Cardiovascular morbidity and mortality in women diagnosed with rheumatoid
arthritis. Circulation 2003;107:13037.
[9] Fischer LM, Schlienger RG, Matter C, Jick H, Meier CR. Effect of rheumatoid
arthritis or systemic lupus erythematosus on the risk of rst-time acute
myocardial infarction. Am J Cardiol 2004;93:198200.
[10] Turesson C, Jarenros A, Jacobsson L. Increased incidence of cardiovascular disease
in patients with rheumatoid arthritis: results from a community based study. Ann
Rheum Dis 2004;63:9525.
[11] Maradit-Kremers H, Crowson CS, Nicola PJ, Ballman KV, Roger VL, Jacobsen SJ,
et al. Increased unrecognized coronary heart disease and sudden deaths in
rheumatoid arthritis: a population-based cohort study. Arthritis Rheum
2005;52:40211.
[12] Watson DJ, Rhodes T, Guess HA. All-cause mortality and vascular events among
patients with rheumatoid arthritis, osteoarthritis, or no arthritis in the UK
General Practice Research Database. J Rheumatol 2003;30:1196202.
[13] Solomon DH, Goodson NJ, Katz JN, Weinblatt ME, Avorn J, Setoguchi S, et al.
Patterns of cardiovascular risk in rheumatoid arthritis. Ann Rheum Dis
2006;65:160812.
[14] Han C, Robinson Jr DW, Hackett MV, Paramore LC, Fraeman KH, Bala MV.
Cardiovascular disease and risk factors in patients with rheumatoid arthritis,
psoriatic arthritis, ankylosing spondylitis. J Rheumatol 2006;33:216772.
[15] Gonzalez-Juanatey C, Testa A, Garcia-Castelo A, Garcia-Porrua C, Llorca J, Vidan J,
et al. HLA-DRB1 status affects endothelial function in treated patients with
rheumatoid arthritis. Am J Med 2003;114:64752.
[16] Bergholm R, Leirisalo-Repo M, Vehkavaara S, Mkimattila S, Taskinen MR, YkiJrvinen H. Impaired responsiveness to NO in newly diagnosed patients with
rheumatoid arthritis. Arterioscler Thromb Vasc Biol 2002;22:163741.
[17] Hansel S, Lassig G, Pistrosch F, Passauer J. Endothelial dysfunction in young
patients with long-term rheumatoid arthritis and low disease activity. Atherosclerosis 2003;170:17780.
[18] Vaudo G, Marchesi S, Gerli R, Allegrucci R, Giordano A, Siepi D, et al. Endothelial
dysfunction in young patients with rheumatoid arthritis and low-disease activity.
Ann Rheum Dis 2004;63:315.
[19] Dessein PH, Joffe BI, Singh S. Biomarkers of endothelial dysfunction, cardiovascular risk factors and atherosclerosis in rheumatoid arthritis. Arthritis Res Ther
2005;7:R63443.
[20] Arnett DK, Evans GW, Riley WA. Arterial stiffness: a new cardiovascular risk
factor? Am J Epidemiol 1994;140:66982.
[21] Roman MJ, Devereux RB, Schwartz JE, Lockshin MD, Paget SA, Davis A, et al.
Arterial stiffness in chronic inammatory diseases. Hypertension 2005;46:1949.
[22] Klocke R, Cockcroft JR, Taylor GJ, Hall IR, Blake DR. Arterial stiffness and central
blood pressure, as determined by pulse wave analysis, in rheumatoid arthritis.
Ann Rheum Dis 2003;62:4148.
[23] Arosio E, De Marchi S, Rigoni A, Prior M, Delva P, Lechi A. Forearm
haemodinamics, arterial stiffness and microcirculatory reactivity in rheumatoid
arthritis. J Hypertens 2007;25:12738.
[24] Turesson C, Jacobsson L, Rydn Ahlgren A, Sturfelt G, Wollmer P, Lnne T.
Increased stiffness of the abdominal aorta in women with rheumatoid arthritis.
Rheumatology 2005;44:896901.
[25] Mki-Petj KM, Hall FC, Booth AD, Wallace SM, Yasmin, Bearcroft PW, et al.
Rheumatoid arthritis is associated with increased aortic pulse-wave velocity,
which is reduced by anti-tumor necrosis factor- therapy. Circulation
2006;114:118592.
[26] Avalos I, Chung CP, Oeser A, Gebretsadik T, Shintani A, Kurnik D, et al. Increased
augmentation index in rheumatoid arthritis and its relationship to coronary
artery atherosclerosis. J Rheumatol 2007;34:238894.
[27] Rugin M, Ciobanu-Jurcu R, Jurcu C, Mihil M, Apetrei E. Subclinical
atherosclerosis, carotid intima-media thickness and the cardiovascular risk.
Rom J Intern Med 2003;41:35763.
[28] Carotti M, Salaf F, Mangiacotti M, Cerioni A, Giuseppetti GM, Grassi W.
Atherosclerosis in rheumatoid arthritis: the role of high-resolution B mode
ultrasound in the measurement of the arterial intima-media thickness.
Reumatismo 2007;59:3849.
[29] del Rincn I, Freeman GL, Haas RW, O'Leary DH, Escalante A. Relative contribution
of cardiovascular risk factors and rheumatoid arthritis clinical manifestations to
atherosclerosis. Arthritis Rheum 2005;52:341323.
[30] Kumeda Y, Inaba M, Goto H, Nagata M, Henmi Y, Furumitsu Y, et al. Increased
thickness of the arterial intima-media detected by ultrasonography in patients
with rheumatoid arthritis. Arthritis Rheum 2002;46:148997.
[31] Park YB, Ahn CW, Choi HK, Lee SH, In BH, Lee HC, et al. Atherosclerosis in
rheumatoid arthritis: morphologic evidence obtained by carotid ultrasound.
Arthritis Rheum 2002;46:17149.
353
[32] La Montagna G, Cacciapuoti F, Buono R, Manzella D, Mennillo GA, Arciello A, et al.
Insulin resistance is an independent risk factor for atherosclerosis in rheumatoid
arthritis. Diab Vasc Dis Res 2007;4:1305.
[33] Gonzalez-Gay MA, Gonzalez-Juanatey C, Pieiro A, Garcia-Porrua C, Testa A,
Llorca J. High-grade C-reactive protein elevation correlates with accelerated
atherogenesis in patients with rheumatoid arthritis. J Rheumatol
2005;32:121923.
[34] Del Rincn I, Williams K, Stern MP, Freeman GL, O'Leary DH, Escalante A. Association
between carotid atherosclerosis and markers of inammation in rheumatoid
arthritis patients and healthy subjects. Arthritis Rheum 2003;48:183340.
[35] Sherer Y, Gerli R, Gilburd B, Bartoloni Bocci E, Vaudo G, Mannarino E, et al.
Thickened carotid artery intima-media in rheumatoid arthritis is associated with
elevated anticardiolipin antibodies. Lupus 2007;16:25964.
[36] Daza L, Aguirre M, Jimenez M, Herrera R, Bollain JJ. Common carotid intimamedia thickness and von Willebrand factor serum levels in rheumatoid arthritis
female patients without cardiovascular risk factors. Clin Rheumatol
2007;26:5337.
[37] Pamuk ON, Unl E, Cakir N. Role of insulin resistance in increased frequency of
atherosclerosis detected by carotid ultrasonography in rheumatoid arthritis.
J Rheumatol 2006;33:244752.
[38] Jonsson SW, Backman C, Johnson O, Karp K, Lundstrm E, Sundqvist KG, et al.
Increased prevalence of atherosclerosis in patients with medium term rheumatoid arthritis. J Rheumatol 2001;28:2597602.
[39] Dessein PH, Norton GR, Woodiwiss AJ, Joffe BI, Wolfe F. Inuence of nonclassical
cardiovascular risk factors on the accuracy of predicting subclinical atherosclerosis in rheumatoid arthritis. J Rheumatol 2007;34:94351.
[40] Dessein PH, Joffe BI, Veller MG, Stevens BA, Tobias M, Reddi K, et al. Traditional
and nontraditional cardiovascular risk factors are associated with atherosclerosis
in rheumatoid arthritis. J Rheumatol 2005;32:43542.
[41] Gullu H, Erdogan D, Caliskan M, Tok D, Yildirim E, Ulus T, et al. Interrelationship
between noninvasive predictors of atherosclerosis: transthoracic coronary ow
reserve, ow-mediated dilation, carotid intima-media thickness, aortic stiffness,
aortic distensibility, elastic modulus, and brachial artery diameter. Echocardiography 2006;23:83542.
[42] Ciftci O, Yilmaz S, Topcu S, Gullu H, Erdogan D, Pamuk BO, et al. Impaired
coronary microvascular function and increased intima-media thickness in
rheumatoid arthritis. Atherosclerosis 2008;198:3327.
[43] Chung CP, Oeser A, Raggi P, Gebretsadik T, Shintani AK, Sokka T, et al. Increased
coronary-artery atherosclerosis in rheumatoid arthritis: relationship to disease
duration and cardiovascular risk factors. Arthritis Rheum 2005;52:304553.
[44] Kao AH, Krishnaswami S, Cunningham A, Edmundowicz D, Morel PA, Kuller
LH, et al. Subclinical coronary artery calcication and relationship to disease
duration in women with rheumatoid arthritis. J Rheumatol 2008;35:619.
[45] Gonzalez A, Maradit Kremers H, Crowson CS, Ballman KV, Roger VL, Jacobsen SJ,
et al. Do cardiovascular risk factors confer the same risk for cardiovascular
outcomes in rheumatoid arthritis patients as in non-rheumatoid arthritis
patients? Ann Rheum Dis 2008;67:649.
[46] Kremers HM, Nicola PJ, Crowson CS, Ballman KV, Gabriel SE. Prognostic
importance of low body mass index in relation to cardiovascular mortality in
rheumatoid arthritis. Arthritis Rheum 2004;50:34507.
[47] McMahon M, Grossman J, FitzGerald J, Dahlin-Lee E, Wallace DJ, Thong BY, et al.
Proinammatory high-density lipoprotein as a biomarker for atherosclerosis in
patients with systemic lupus erythematosus and rheumatoid arthritis. Arthritis
Rheum 2006;54:25419.
[48] Charles-Schoeman C, Khanna D, Furst DE, McMahon M, Reddy ST, Fogelman AM,
et al. Effects of high-dose atorvastatin on antiinammatory properties of high
density lipoprotein in patients with rheumatoid arthritis: a pilot study.
J Rheumatol 2007;34:145964.
[49] Ross R. Atherosclerosis an inammatory disease. N Engl J Med 1999;340:11526.
[50] Benagiano M, Azzurri A, Ciervo A, Amedei A, Tamburini C, Ferrari M, et al. T helper
type 1 lymphocytes drive inammation in human atherosclerotic lesions. Proc
Natl Acad Sci U S A 2003;100:665863.
[51] Abou-Raya A, Abou-Raya S. Inammation: a pivotal link between autoimmune
diseases and atherosclerosis. Autoimmun Rev 2006;5:3317.
[52] Sattar N, McCarey DW, Capell H, McInnes IB. Explaining how high-grade
systemic inammation accelerates vascular risk in rheumatoid arthritis. Circulation 2003;108:295763.
[53] Jacobsson LT, Turesson C, Hanson RL, Pillemer S, Sievers ML, Pettitt DJ, et al. Joint
swelling as a predictor of death from cardiovascular disease in a population study
of Pima Indians. Arthritis Rheum 2001;44:11706.
[54] Turesson C, McClelland RL, Christianson TJ, Matteson EL. Severe extra-articular
disease manifestations are associated with an increased risk of rst ever
cardiovascular events in patients with rheumatoid arthritis. Ann Rheum Dis
2007;66:705.
[55] Goodson NJ, Wiles NJ, Lunt M, Barrett EM, Silman AJ, Symmons DP. Mortality in
early inammatory polyarthritis: cardiovascular mortality is increased in
seropositive patients. Arthritis Rheum 2002;46:20109.
[56] Ridker PM, Buring JE, Shih J, Matias M, Hennekens CH. Prospective study of Creactive protein and the risk of future cardiovascular events among apparently
healthy women. Circulation 1998;98:7313.
[57] Ridker PM, Cushman M, Stampfer MJ, Tracy RP, Hennekens CH. Inammation,
aspirin, and the risk of cardiovascular disease in apparently healthy men. N Engl J
Med 1997;336:9739.
[58] Apetrei E, Ciobanu-Jurcut R, Rugina M, Gavrila A, Uscatescu V. C-reactive protein,
prothrombotic imbalance and endothelial dysfunction in acute coronary
syndromes without ST elevation. Rom J Intern Med 2004;42:95102.
354
C. Tanasescu et al. / European Journal of Internal Medicine 20 (2009) 348354
[59] Gavrila A, Ciobanu-Jurcut R, Rugina M, Serban I, Puscariu T, Uscatescu V, et al. Plasmatic
levels of homocysteine and C-reactive protein: which one correlates better with TIMI
score in unstable angina patients? Arch Mal Coeur Vaiss 2003;96(suppl II):62.
[60] Jialal I, Devaraj S, Venugopal SK. C-reactive protein: risk marker or mediator in
atherosclerosis? Hypertension 2004;44:611.
[61] Goodson NJ, Symmons DP, Scott DG, Bunn D, Lunt M, Silman AJ. Baseline levels of
C-reactive protein and prediction of death from cardiovascular disease in patients
with inammatory polyarthritis: a ten-year followup study of a primary carebased inception cohort. Arthritis Rheum 2005;52:22939.
[62] Pearson TA, Mensah GA, Alexander RW, Anderson JL, Cannon RO 3rd, Criqui M,
et al. Centers for Disease Control and Prevention; American Heart Association.
Markers of inammation and cardiovascular disease: application to clinical and
public health practice: a statement for healthcare professionals from the Centers
for Disease Control and Prevention and the American Heart Association. Circulation
2003;107:499511.
[63] Choy EH, Panayi GS. Cytokine pathways and joint inammation in rheumatoid
arthritis. N Engl J Med 2001;344:90716.
[64] Mattey DL, Glossop JR, Nixon NB, Dawes PT. Circulating levels of tumor necrosis
factor receptors are highly predictive of mortality in patients with rheumatoid
arthritis. Arthritis Rheum 2007;56:39408.
[65] Ridker PM, Rifai N, Pfeffer, Sacks F, Lepage S, Braunwald E. Elevation of TNF- and
increased risk of recurrent coronary events after myocardial infarction. Circulation 2000;101:214953.
[66] Blake GJ, Ridker PM. Tumour necrosis factor-, inammatory biomarkers, and
atherogenesis. Eur Heart J 2002;23:3457.
[67] Moller DE. Potential role of TNF-alpha in the pathogenesis of insulin resistance
and type-2 diabetes. Trends Endocrinol Metab 2000;6:2127.
[68] Choy E. Interleukin 6 receptor as a target for the treatment of rheumatoid
arthritis. Ann Rheum Dis 2003;62(Suppl II):ii689.
[69] Ikeda U, Ito T, Shimada K. Interleukin-6 and acute coronary syndrome. Clin
Cardiol 2001;24:7014.
[70] Klimiuk PA, Sierakowski S, Latosiewicz R, Cylwik JP, Cylwik B, Skowronski J, et al.
Soluble adhesion molecules (ICAM-1, VCAM-1,and E-selectin) and vascular
endothelial growth factor (VEGF) in patients with distinct variants of rheumatoid
arthritis. Ann Rheum Dis 2002;61:8049.
[71] Mulvihill NT, Foley JB, Crean P, Walsh M. Prediction of cardiovascular risk using
soluble cell adhesion molecules. Eur Heart J 2002;23:156974.
[72] Grisar J, Aletaha D, Steiner CW, Kapral T, Steiner S, Seidinger D, et al. Depletion of
endothelial progenitor cells in the peripheral blood of patients with rheumatoid
arthritis. Circulation 2005;111:20411.
[73] Werner N, Kosiol S, Schiegl T, Ahlers P, Walenta K, Link A, et al. Circulating endothelial
progenitor cells and cardiovascular outcomes. N Engl J Med 2005;353:9991007.
[74] Grisar J, Aletaha D, Steiner CW, Kapral T, Steiner S, Semann M, et al. Endothelial
progenitor cells in active rheumatoid arthritis: effects of tumour necrosis factor
and glucocorticoid therapy. Ann Rheum Dis 2007;66:12848.
[75] Jono S, Ikari Y, Shioi A, Mori K, Miki T, Hara K, et al. Serum osteoprotegerin levels
are associated with the presence and severity of coronary artery disease.
Circulation 2002;106:11924.
[76] Asanuma Y, Chung CP, Oeser A, Solus JF, Avalos I, Gebretsadik T, et al. Serum
osteoprotegerin is increased and independently associated with coronary-artery atherosclerosis in patients with rheumatoid arthritis. Atherosclerosis 2007;195:e13541.
[77] Ziolkowska M, Kurowska M, Radzikowska A, Luszczykiewicz G, Wiland P,
Dziewczopolski W, et al. High levels of osteoprotegerin and soluble receptor
activator of nuclear factor kappa B ligand in serum of rheumatoid arthritis
patients and their normalization after anti-tumor necrosis factor alpha
treatment. Arthritis Rheum 2002;46:174453.
[78] Jurcut C, Jurcut R, Blaj S, Tanasescu C. Inammation and platelet activation in
patients with rheumatoid arthritis: possible determinants of increased cardiovascular risk. Atheroscler Suppl 2006;7(3):414 [P12:308].
[79] Arlestig L, Wllberg Jonsson S, Stegmayr B, Rantap-Dahlqvist S. Polymorphism
of genes related to cardiovascular disease in patients with rheumatoid arthritis.
Clin Exp Rheumatol 2007;25:86671.
[80] Panoulas VF, Milionis HJ, Douglas KM, Nightingale P, Kita MD, Klocke R, et al.
Association of serum uric acid with cardiovascular disease in rheumatoid
arthritis. Rheumatology (Oxford) 2007;46:146670.
[81] Raterman HG, van Halm VP, Voskuyl AE, Simsek S, Dijkmans BA, Nurmohamed
MT. Rheumatoid arthritis is associated with a high prevalence of hypothyroidism
that amplies its cardiovascular risk. Ann Rheum Dis 2008;67:22932.
[82] Hernanz A, Plaza A, Martin-Mola E, De Miguel E. Increased plasma levels of
homocysteine and other thiol compounds in rheumatoid arthritis women. Clin
Biochem 1999;32:6570.
[83] Chung CP, Oeser A, Solus JF, Avalos I, Gebretsadik T, Shintani A, et al. Prevalence of
the metabolic syndrome is increased in rheumatoid arthritis and is associated
with coronary atherosclerosis. Atherosclerosis 2008;196:75663.
[84] Gonzalez-Gay MA, Gonzalez-Juanatey C, Lopez-Diaz MJ, Pieiro A, Garcia-Porrua C,
Miranda-Filloy JA, et al. HLA-DRB1 and persistent chronic inammation contribute
to cardiovascular events and cardiovascular mortality in patients with rheumatoid
arthritis. Arthritis Rheum 2007;57:12532.
[85] van den Berg MH, de Boer IG, le Cessie S, Breedveld FC, Vliet Vlieland TP. Are
patients with rheumatoid arthritis less physically active than the general
population? J Clin Rheumatol 2007;13:1816.
[86] Graham I, Atar D, Borch-Johnsen K, Boysen G, Burell G, Cifkova R, et al, Fourth
Joint Task Force of the European Society of Cardiology and Other Societies on
Cardiovascular Disease Prevention in Clinical Practice. European guidelines on
[87]
[88]
[89]
[90]
[91]
[92]
[93]
[94]
[95]
[96]
[97]
[98]
[99]
[100]
[101]
[102]
[103]
[104]
[105]
[106]
[107]
[108]
[109]
[110]
[111]
[112]
cardiovascular disease prevention in clinical practice: executive summary.
Eur Heart J 2007;28:2375414.
Panoulas VF, Douglas KM, Stavropoulos-Kalinoglou A, Metsios GS, Nightingale P,
Kita MD, et al. Long-term exposure to medium-dose glucocorticoid therapy
associates with hypertension in patients with rheumatoid arthritis. Rheumatology (Oxford) 2008;47:725.
Panoulas VF, Douglas KM, Milionis HJ, Stavropoulos-Kalinglou A, Nightingale P,
Kita MD, et al. Prevalence and associations of hypertension and its control in
patients with rheumatoid arthritis. Rheumatology (Oxford) 2007;46:147782.
Solomon DH, Avorn J, Katz JN, Weinblatt ME, Setoguchi S, Levin R, et al.
Immunosuppressive medications and hospitalization for cardiovascular events in
patients with rheumatoid arthritis. Arthritis Rheum 2006;54:37908.
Davis III JM, Maradit Kremers H, Crowson CS, Nicola PJ, Ballman KV, Therneau TM,
et al. Glucocorticoids and cardiovascular events in rheumatoid arthritis: a
population-based cohort study. Arthritis Rheum 2007;56:82030.
Hafstrm I, Rohani M, Deneberg S, Wrnert M, Jogestrand T, Frostegrd J. Effects
of low-dose prednisolone on endothelial function, atherosclerosis, and traditional risk factors for atherosclerosis in patients with rheumatoid arthritis a
randomized study. J Rheumatol 2007;34:18106.
Solomon SD, Wittes J, Finn PV, Fowler R, Viner J, Bertagnolli MM, et al.
Cardiovascular risk of celecoxib in six randomized placebo-controlled trials: the
Cross Trial Safety analysis. Circulation 2008;117:210413.
Antman EM, Bennett JS, Daugherty A, Furberg C, Roberts H, Taubert KA. Use of
nonsteroidal antiinammatory drugs: an update for clinicians: a scientic
statement from the American Heart Association. Circulation 2007;115:163442.
Kearney PM, Baigent C, Godwin J, Halls H, Emberson JR, Patrono C. Do selective
cyclo-oxygenase-2 inhibitors and traditional non-steroidal anti-inammatory
drugs increase the risk of atherothrombosis? Meta-analysis of randomized trials.
BMJ 2006;332:13028.
McGettigan P, Henry D. Cardiovascular risk and inhibition of Cyclooxygenase: a
systematic review of the observational studies of selective and nonselective
inhibitors of Cyclooxygenase 2. JAMA 2006;296:163344.
Choi HK, Hernn MA, Seeger JD, Robins JM, Wolfe F. Methotrexate and mortality in
patients with rheumatoid arthritis: a prospective study. Lancet 2002;359:11737.
Wallberg-Jonsson S, Ohman M, Rantapaa-Dahlqvist S. Which factors are related
to the presence of atherosclerosis in rheumatoid arthritis? Scand J Rheumatol
2004;33:3739.
van Halm VP, Nurmohamed MT, Twisk JW, Dijkmans BA, Voskuyl AE. Diseasemodifying antirheumatic drugs are associated with a reduced risk for
cardiovascular disease in patients with rheumatoid arthritis: a case control
study. Arthritis Res Ther 2006;8:R151.
Munro R, Morrison E, McDonald AG, Hunter JA, Madhok R, Capell HA. Effect of
disease modifying agents on the lipid proles of patients with rheumatoid
arthritis. Ann Rheum Dis 1997;56:3747.
Wasko MC, Hubert HB, Lingala VB, Elliott JR, Luggen ME, Fries JF, et al.
Hydroxychloroquine and risk of diabetes in patients with rheumatoid arthritis.
JAMA 2007;298:18793.
Hrlimann D, Forster A, Noll G, Enseleit F, Chenevard R, Distler O, et al. Antitumor necrosis factor- treatment improves endothelial function in patients
with rheumatoid arthritis. Circulation 2002;106:21847.
Cardillo C, Schinzari F, Mores N, Mettimano M, Melina D, Zoli A, et al.
Intravascular tumor necrosis factor- blockade reverses endothelial dysfunction
in rheumatoid arthritis. Clin Pharmacol Ther 2006;80:27581.
Gonzalez-Juanatey C, Testa A, Garcia-Castelo A, Garcia-Porrua C, Llorca J,
Gonzalez-Gay MA. Active but transient improvement of endothelial function in
rheumatoid arthritis patients undergoing long-term treatment with anti-tumor
necrosis factor alpha antibody. Arthritis Rheum 2004;51:44750.
Van Dornum S, McColl G, Wicks IP. Tumor necrosis factor antagonists improve
disease activity but not arterial stiffness in rheumatoid arthritis. Rheumatology
2005;44:142832.
Seriolo B, Paolino S, Sulli A, Fasciolo D, Cutolo M. Effects of anti-TNF-alpha
treatment on lipid prole in patients with active rheumatoid arthritis. Ann N Y
Acad Sci 2006;1069:4149.
Vis M, Nurmohamed MT, Wolbink G, Voskuyl AE, de Koning M, van de Stadt R,
et al. Short term effects of iniximab on the lipid prole in patients with
rheumatoid arthritis. J Rheumatol 2005;32:2525.
Popa C, van den Hoogen FH, Radstake TR, Netea MG, Eijsbouts AE, den Heijer M,
et al. Modulation of lipoprotein plasma concentrations during long-term
anti-TNF therapy in patients with active rheumatoid arthritis. Ann Rheum Dis
2007;66:15037.
McCarey DW, McInnes IB, Madhok R, Hampson R, Scherbakov O, Ford I, et al. Trial
of atorvastatin in rheumatoid arthritis (TARA): double-blind, randomized
placebo-controlled trial. Lancet 2004;363:201521.
O'Driscoll G, Green D, Taylor RR. Simvastatin, an HMG-coenzyme A reductase
inhibitor, improves endothelial function within 1 month. Circulation 1997;95:112631.
Haruna Y, Morita Y, Yada T, Satoh M, Fox DA, Kashihara N. Fluvastatin reverses
endothelial dysfunction and increased vascular oxidative stress in rat adjuvantinduced arthritis. Arthritis Rheum 2007;56:182735.
Van Dornum S, McColl G, Wicks IP. Atorvastatin reduces arterial stiffness in
patients with rheumatoid arthritis. Ann Rheum Dis 2004;63:15715.
Mki-Petj KM, Booth AD, Hall FC, Wallace SM, Brown J, McEniery CM, et al.
Ezetimibe and simvastatin reduce inammation, disease activity, and aortic
stiffness and improve endothelial function in rheumatoid arthritis. J Am Coll
Cardiol 2007;50:8528.
Das könnte Ihnen auch gefallen
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Studiu Spania CARMADokument9 SeitenStudiu Spania CARMAMihaela IonescuNoch keine Bewertungen
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Articol InterdiabDokument6 SeitenArticol InterdiabMihaela IonescuNoch keine Bewertungen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- Resistant Hypertension, Obstructive Sleep Apnea and Chronic Kidney Disease: A Menacing TriangleDokument4 SeitenResistant Hypertension, Obstructive Sleep Apnea and Chronic Kidney Disease: A Menacing TriangleMihaela IonescuNoch keine Bewertungen
- Optimisation of Colour Flow Doppler ImagesDokument1 SeiteOptimisation of Colour Flow Doppler ImagesMihaela IonescuNoch keine Bewertungen
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- InterdiabDokument385 SeitenInterdiabMihaela Ionescu100% (1)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- 2014 ESC/ESA Guidelines On Non-Cardiac Surgery: Cardiovascular Assessment and ManagementDokument49 Seiten2014 ESC/ESA Guidelines On Non-Cardiac Surgery: Cardiovascular Assessment and ManagementNovi Yanti NyNoch keine Bewertungen
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Dosing Titration For Beta Blockers Proven To Be Effective in Heart FailureDokument1 SeiteDosing Titration For Beta Blockers Proven To Be Effective in Heart FailureMihaela IonescuNoch keine Bewertungen
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- IMA CursDokument116 SeitenIMA CursMihaela Ionescu100% (1)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Cancer PDFDokument9 SeitenCancer PDFMihaela IonescuNoch keine Bewertungen
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Lecture Signs and Symptoms of Cardiovascular System DiseasesDokument240 SeitenLecture Signs and Symptoms of Cardiovascular System DiseasesMihaela IonescuNoch keine Bewertungen
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Girl InterruptedDokument7 SeitenGirl Interruptedapi-365678992Noch keine Bewertungen
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- A Silent KillerDokument3 SeitenA Silent KillerLinhNguyeNoch keine Bewertungen
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- Physics and Imaging in Radiation OncologyDokument6 SeitenPhysics and Imaging in Radiation Oncologydarr artNoch keine Bewertungen
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- Suicide in Adolescent - A Case ReportDokument5 SeitenSuicide in Adolescent - A Case ReportRebecca SilaenNoch keine Bewertungen
- Festival Dance Lesson - Module 2 - P.E. 3rd Quarter PPT 2 of 2Dokument29 SeitenFestival Dance Lesson - Module 2 - P.E. 3rd Quarter PPT 2 of 2Maria Fe VibarNoch keine Bewertungen
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Sheet 2 (Local Anesthesia 2)Dokument14 SeitenSheet 2 (Local Anesthesia 2)ardesh abdilleNoch keine Bewertungen
- Body Parts Governed by PlanetsDokument2 SeitenBody Parts Governed by PlanetsBratva Ankit Mishra100% (1)
- Acadia PharmaceuticalsDokument3 SeitenAcadia PharmaceuticalsAman DecoraterNoch keine Bewertungen
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- Insulin SensitizersDokument17 SeitenInsulin SensitizersGautam SharmaNoch keine Bewertungen
- Exercise PrescriptionDokument53 SeitenExercise PrescriptionEvangeline A. Alegre100% (1)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- Anesthesia-Assessing Depth PDFDokument1 SeiteAnesthesia-Assessing Depth PDFAvinash Technical ServiceNoch keine Bewertungen
- Understanding The RelapseDokument12 SeitenUnderstanding The RelapseruziyanaNoch keine Bewertungen
- Total Hip and Total Knee Replacement Post Operatif Nursing ManagementDokument5 SeitenTotal Hip and Total Knee Replacement Post Operatif Nursing ManagementAnas KhafidNoch keine Bewertungen
- Anxiety: What Are Some Symptoms of Anxiety?Dokument3 SeitenAnxiety: What Are Some Symptoms of Anxiety?Khairil AshrafNoch keine Bewertungen
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- On and Off Male Birth Control MethodsDokument2 SeitenOn and Off Male Birth Control MethodsLeón L.PNoch keine Bewertungen
- Proximal Humerus Fractures Epidemiology and TrendsDokument5 SeitenProximal Humerus Fractures Epidemiology and TrendsHelena Sofia Fonseca Paiva De Sousa TelesNoch keine Bewertungen
- Classification of Tongue Cancer Resection and Treatment AlgorithmDokument8 SeitenClassification of Tongue Cancer Resection and Treatment AlgorithmRahma WatiNoch keine Bewertungen
- Worksheet TherapyDokument2 SeitenWorksheet TherapymermerytaNoch keine Bewertungen
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- SP42 Thoracentesis (Adult)Dokument7 SeitenSP42 Thoracentesis (Adult)Adam HuzaibyNoch keine Bewertungen
- Energy Drinks Are Bad RealDokument4 SeitenEnergy Drinks Are Bad RealMadihi NorhadiNoch keine Bewertungen
- ApendikDokument4 SeitenApendikSepti AyaNoch keine Bewertungen
- +++A Short Survey in Application of Ordinary Differential Equations On Cancer ResearchDokument5 Seiten+++A Short Survey in Application of Ordinary Differential Equations On Cancer ResearchEnes ÇakmakNoch keine Bewertungen
- Aneurysm: Symptoms of An AneurysmDokument3 SeitenAneurysm: Symptoms of An AneurysmArun MuralidharanNoch keine Bewertungen
- Operative ProcedureDokument22 SeitenOperative Procedurezianab aliNoch keine Bewertungen
- Glaser, R., & Kiecolt-Glaser, J. K. (2005) - Stress-Induced Immune DysfunctionDokument9 SeitenGlaser, R., & Kiecolt-Glaser, J. K. (2005) - Stress-Induced Immune DysfunctionFranco Paolo Maray-GhigliottoNoch keine Bewertungen
- ABC First Aid GuideDokument66 SeitenABC First Aid GuideTze Ming VoonNoch keine Bewertungen
- Using Pediatric Pain Scales Neonatal Infant Pain Scale (NIPSDokument2 SeitenUsing Pediatric Pain Scales Neonatal Infant Pain Scale (NIPSSevina Eka ChannelNoch keine Bewertungen
- Case Report Acute Idiopathic Scrotal Edema MILMED-D-13-00103Dokument3 SeitenCase Report Acute Idiopathic Scrotal Edema MILMED-D-13-00103YJanitorNoch keine Bewertungen
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- DctsDokument30 SeitenDctsInuyashayahoo100% (1)