Beruflich Dokumente
Kultur Dokumente
PET Imaging in Dementia (Stabilo)
Hochgeladen von
NoviBassoOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
PET Imaging in Dementia (Stabilo)
Hochgeladen von
NoviBassoCopyright:
Verfügbare Formate
The British Journal of Radiology, 80 (2007), S160S167
Positron emission tomography imaging in dementia
1,2
K HERHOLZ,
MD,
1,3
S F CARTER,
MSc
and 1M JONES,
MBChB, MRCP
Wolfson Molecular Imaging Centre, University of Manchester, Manchester, 2The Research School of Translational
Medicine, University of Manchester, Manchester and 3The School of Psychological Sciences, University of Manchester,
Manchester, UK
ABSTRACT. Positron emission tomography (PET) is a well-established imaging modality.
Measurement of regional cerebral glucose metabolism (rCMRglc) using PET and [18F]-2fluoro-2-deoxy-D-glucose (FDG) has become a standard technique in both oncology and
dementia research. When measuring rCMRglc in Alzheimers disease (AD), characteristic
reductions in rCMRglc are found in neocortical association areas including the posterior
cingulate, precuneus, temporoparietal and frontal multimodal association regions; the
primary visual cortex, sensorimotor cortex, basal ganglia and cerebellum are relatively
unaffected. FDG-PET has been used in the study of mild cognitive impairment (MCI) to
accurately predict the subsequent decline to AD. Impairment in rCMRglc may be seen in
individuals at high genetic risk of AD, even before clinical symptoms are apparent.
Characteristic patterns of regional hypometabolism are also seen in other degenerative
dementias such as frontotemporal dementia (FTD) and dementia with Lewy bodies
(DLB). The use of different radioisotopes and tracers increases the versatility of PET.
Tracers adopted in dementia research include 11C-PK-11195 and 11C-PIB, which have
been used to investigate neuroinflammation and amyloid deposition, respectively, in
both AD and MCI populations. It is also possible to investigate neurotransmitter systems
in dementia; targets have included the cholinergic, dopaminergic and serotonergic
systems. Imaging the brains of dementia patients using PET provides important
information about the brain function of these individuals that would otherwise be
unavailable with other imaging modalities. PET will continue to be important in future
dementia research as new tracers become available to help in the early and specific
diagnosis of increasingly well-defined clinical syndromes, and assist in the assessment of
new therapeutic interventions.
Positron emission tomography (PET) utilizes biologically active molecules in micromolar or nanomolar
concentrations that have been labelled with short-lived
positron-emitting isotopes. The physical characteristics
of the isotopes and the molecular specificity of labelled
molecules, combined with the high detection efficacy of
modern PET scanners, provide a sensitivity for human in
vivo measurement of indicator concentrations that is
several orders of magnitude higher than with the other
imaging techniques. Whereas the very short half-lives of
O-15 (2 min) and C-11 (20 min) limit their use to fully
equipped PET centres with a cyclotron and radiopharmaceutical laboratory, F-18 labelled tracers (half-life
110 min) can be produced in specialized centres and
distributed regionally to hospitals running a PET scanner
only.
Clinical use of PET is now well established in clinical
oncology and it is therefore becoming widely available in
major hospitals. In addition to its use in research, brain
PET also provides diagnostically relevant information
mainly in neurodegenerative disorders, focal epilepsy
and brain tumours [1]. In dementia, the measurement of
Address correspondence to: Karl Herholz, Wolfson Molecular
Imaging Centre, The University of Manchester, 27 Palatine Road,
Withington, Manchester M20 3LJ, UK. E-mail: Karl.Herholz@
manchester.ac.uk
S160
Received 11 December
2007
Accepted 11 December
2007
DOI: 10.1259/bjr/97295129
2007 The British Institute of
Radiology
cerebral glucose metabolism by 18F-2-fluoro-2-deoxy-Dglucose (FDG) and specific molecular imaging techniques involving tracers for amyloid and major neurotransmitters (see Table 1) are of diagnostic interest and
will therefore be reviewed in this paper.
FDG: regional cerebral glucose metabolism
Glucose is the main energy supply for the brain. Its
metabolism maintains ion gradients and glutamate turnover and is closely coupled to neuronal function at rest
and during functional activation [2]. Its measurement by
FDG is based on phosphorylation of the tracer by
hexokinase, which is the pivotal first step of that metabolic
pathway. PET images are obtained typically 3060 min
after tracer injection, with measurement times that can be
as short as 5 min. In normal subjects, typical resting state
grey matter cerebral metabolic rate for glucose (CMRglc)
values are in the range of 4060 mmol glucose/100 g/min,
and they are approximately 15 mmol glucose/100 g/min
in white matter. There are regional differences, with the
highest values in the striatum and parietal cortex close to
the parieto-occipital sulcus. Some phylogenetically older
brain structures such as the medial temporal cortex and
cerebellum have metabolic rates below the grey matter
average but are still higher than normal white matter.
The British Journal of Radiology, Special Issue 2007
PET imaging in dementia
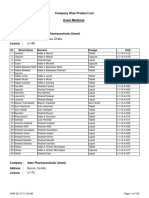
Table 1. Targets and tracers for human positron emission
tomography molecular imaging in dementia
Amyloid plaques: 11C-PIB and related compounds
Microglial activation: 11C-PK-11195
Cholinergic neurons
AChE activity: 11C-MP4A and related compounds
Nicotinic receptors: 11C-nicotine, 18F-A85380
Muscarinergic receptors: 11C-NMPB, 18F-FP-TZTP
Dopaminergic neurons
Dopa decarboxylation and vesicular storage: 18F-fluorodopa
Dopa transporter: 18F/11C-FP-CIT and related compounds
Dopamine D2 receptors: 11C-raclopride, 18F-fallypride
Serotonergic neurons
Transporter: 11C-DASB and related compounds
5HT(1A) receptors: 11C -WAY-100635, 18F-MPPF
5HT(2A) receptors: 18F/11C-Altanserin, 11C-MDL-100907
GABA/benzodiazepin receptors: 11C-flumazenil
AChE, acetyl cholinesterase; GABA, c-aminobutyric acid.
There is a moderate reduction of cerebral glucose
metabolism with age, mainly affecting the frontal association cortex [3]. Scans must be obtained under wellcontrolled standard conditions to avoid confounding
effects by uncontrolled brain activation.
Figure 1. Fluorodeoxyglucose positron emission tomogra-
Main findings in Alzheimers disease
Multiple studies over more than 20 years have
demonstrated that glucose metabolism and blood flow
are impaired in temporoparietal association cortices,
with the angular gyrus usually being the centre of the
metabolic impairment (see [4] for a review). Frontal
association cortex may also be involved, but this is more
variable and is seen only during progression of AD. The
affected association cortices are those that become
myelinated last during brain maturation and are also
prone to cortical amyloid deposition [5]. There may be a
distinct hemispheric asymmetry, which usually corresponds to the predominant cognitive deficits (language
impairment in the dominant and visuospatial disorientation in the subdominant hemisphere). In contrast to other
dementia types, glucose metabolism in the basal ganglia,
primary motor and visual cortex, and the cerebellum is
usually well preserved. This pattern generally reflects
AD clinical symptoms, with impairment of memory and
associative thinking, including higher-order sensory
processing and planning of action but with relative
preservation of primary motor and sensory function.
Voxel-based comparisons with normal reference samples clearly showed that the posterior cingulate gyrus
and the precuneus are also impaired at an early stage
(Figure 1) [6]. This is usually not directly obvious by
mere inspection of FDG-PET scans because metabolism
in that area is above the cortical average in normal brain
[7] and as impairment occurs it returns to the level of the
surrounding cortex. Consequently, this important diagnostic sign is easily missed by standard visual interpretation of FDG-PET brain scans. It is therefore
becoming standard practice to base the interpretation
of patient studies on quantitative mapping with reference to an appropriate normal sample [810].
More advanced approaches go beyond detection of
abnormal voxels and aim at automatic recognition of the
The British Journal of Radiology, Special Issue 2007
phy/MRI fusion image in very mild Alzheimers disease
(MMSE 28) showing severe impairment of posterior cingulate glucose metabolism (compared with the normal high
activity in that structure under cognitive resting conditions).
Hippocampal atrophy and associated metabolic impairment
is also evident.
typical anatomical distribution of metabolic abnormalities in AD. In a multicentre study involving 395 patients,
the sum of t-scores in those brain areas that are typically
affected in AD discriminated patients from control
subjects with 93% accuracy [8]. Discriminant functions
derived by multiple regression of regional data achieved
87% correct classification of AD patients vs control
subjects [11], and a neural network classifier arrived at
90% accuracy [12]. Several discriminant functions combined with principal component analysis or partial least
squares have been tested for discrimination between AD
and FTD in a sample of 48 patients with autopsyconfirmed diagnosis and achieved accuracies between
80% and 90% [13].
The abnormalities found in AD with FDG-PET mirror
those found with SPECT, and MRI [14] using blood flow
techniques; however, most direct comparison studies
have shown superior accuracy with PET [15, 16]. As
cerebral blood flow (CBF) is dependent on arterial pCO2
and therefore physiologically more variable than glucose
metabolism in normal subjects, CBF measurements using
PET (H215O) have relatively lower diagnostic power for
AD [17] than FDG-PET studies.
Longitudinal studies and trials
Longitudinal studies have demonstrated the severity
and extent of metabolic impairment in temporal and
parietal cortex increases as dementia progresses, and
frontal lobe reductions become more evident [18, 19].
The reduction of metabolism is in the order of 1619%
S161
K Herholz, S F Carter and M Jones
over 3 years in association cortices, which contrasts with
an absence of significant decline in normal control
subjects [20]. Asymmetrical metabolic impairment and
associated predominance of language or visuospatial
impairment tends to persist during progression [21, 22].
Based on these observations, FDG-PET can serve as a
biomarker in therapeutic trials [23]. When monitoring
the change due to disease progression over 1 year using
standard neuropsychological testing by Mini Mental
State Examination (MMSE) and Alzheimers Disease
Assessment Scalecognitive (ADAS-cog) one typically
obtains coefficients of variation (COV) around 100% for
these changes, whereas COV from PET measurements
are in the region of 50%, resulting in a reduction in the
sample size required by about 75% at the same study
power [24, 25].
Mild cognitive impairment and early diagnosis
of AD
Impairment of rCMRglc has been observed in an
asymptomatic stage in individuals at high risk for AD
due to family history of AD and possession of the ApoE
e4 allele [26, 27] and this abnormality is seen decades
before the likely onset of dementia [28]. In middle-aged
and elderly asymptomatic ApoE e4-positive individuals
temporoparietal and posterior cingulate rCMRglc decline
by about 2% per year [29].
The first study noting the predictive power of posterior cingulate metabolism in patients with severe memory
deficits for predicting progression was performed by
Minoshima et al [6] in 1997. This observation was
followed by several studies indicating a high predictive
power with sensitivity and specificity above 80% for
prediction of rapid progression (Table 2). Recent studies
found FDG-PET clearly superior to ApoE e4 testing [30]
and demonstrated that a normal FDG-PET in MCI
indicates a low chance of progression within 1 year,
even if there is a severe memory deficit on neuropsychological testing [31].
Mesial temporal metabolic impairment has been
observed as a general feature in patients with memory
impairment, including but not limited to patients with
MCI and AD [3234]. Hippocampal and entorhinal
metabolic impairment is difficult to assess visually on
PET scans because of small size, lower normal metabolism than the neocortical association cortices, and partial
volume effects due to early and significant hippocampal
atrophy in MCI and AD. Nevertheless, the predictive
power for development of MCI has been demonstrated
in a 3-year follow-up study of cognitively normal
subjects [35].
Frontotemporal lobar degeneration
This group of diseases comprises frontotemporal
dementia (FTD) as the most frequent manifestation and
also more focal degenerative processes such as primary
progressive aphasia and semantic dementia [36].
Cerebral glucose metabolism is impaired mostly in the
frontal cortex, especially in the mesial frontal cortex [3].
Frontolateral and anterior temporal cortices are often
S162
also severely impaired. This impairment may be very
asymmetric and is related to the clinical symptoms of
aphasia or semantic memory deficits [38, 39]. Milder
metabolic change often involves large parts of the brain
[40]. The regional pattern of predominantly frontal
impairment usually allows clear distinction from AD,
although there may be overlap as AD can involve frontal
regions and FTD may not spare temporoparietal cortex.
It has been shown recently in a series of 45 patients with
pathologically confirmed diagnosis that FDG-PET can
discriminate FTD from AD with more than 85%
sensitivity and specificity [41].
Dementia with Lewy bodies
Dementia with Lewy bodies (DLB) is clinically
characterized by fluctuating consciousness, possible
Parkinsonian motor features and impairment of visual
perception including hallucinations. The hallucinations
are the likely correlate of a reduction of glucose
metabolism in primary visual cortex that has been
described with FDG-PET in DLB in addition to an
impairment of posterior association areas as is seen in
AD [42]. In contrast, metabolic activity in the primary
visual cortex is usually well preserved in AD, but in
practice the distinction may be difficult as the metabolic
activity in that area is subject to considerable variability
and depends on examination conditions (eyes open or
eyes closed). A more reliable imaging feature to
differentiate DLB from AD is the impairment of
dopamine synthesis and transport [43] that can be
assessed with 18F-fluorodopa, as described later.
Table 2. Longitudinal studies in the predictive value of FDGPET in MCI
Studies before MCI was used as a diagnostic term
Minoshima et al (1997) [6] very early AD
Posterior cingulate impaired in converters (compared to
normal control subjects)
Herholz et al (1999) [87] possible AD
Progression within 2 years: 65% of subjects with impaired
metabolism compared with 14% with normal metabolism
Berent et al (1999) [88] isolated memory impairment
Progression within 3 years: 70% with abnormal PET, in
30% with normal PET
Recent studies
Arnaiz et al (2001) [89] MCI
75% correct prediction of progression within 3 years
90% correct when combined with neuropsychological
testing
Chetelat et al (2003) [90] amnesic MCI
100% correspondence with progression by logistic regression
Drzezga et al (2005) [30] MCI
16 months follow-up
ApoE sensitivity 75%; specificity 56%
PET sensitivity 92%; specificity 89%
Anchisi et al (2005) [31] MCI
1 year follow-up
Memory sensitivity 97%; specificity 59%
PET sensitivity 93%; specificity 82%
AD, Alzheimers disease; FDG, fluorodeoxyglucose; MCI, mild
cognitive impairment; PET, positron emission tomography.
The British Journal of Radiology, Special Issue 2007
PET imaging in dementia
Imaging key pathophysiological processes:
amyloid and microglial activation
Amyloid
The development of PET tracers designed to label
amyloid plaques in vivo is currently an area of great
research interest. The deposition of amyloid-b (Ab) is an
early event in the pathogenesis of AD [44] and is central
in the amyloid cascade hypothesis [45]. The first tracer to
be used to label Ab selectively in vivo was 11C-labelled
thioflavin analogue, named for convenience Pittsburgh
compound B (11C-PIB) [46]. Dynamic scanning provides
quantitation of binding potentials, and a relatively
simple and practical way of quantifying uptake in a
clinical setting is based on scans obtained approximately
60 min after i.v. injection of the tracer with the
cerebellum as an unaffected reference region [47].
Since its introduction, this tracer has been used by
multiple research groups and has consistently proved to
provide high sensitivity in detecting amyloid plaques
and vascular amyloid in vivo [4850]. In normal subjects,
some unspecific binding is observed mainly in white
matter, which is probably due to the compounds
lipophilicity; however, in patients with AD, specific
binding, mostly in the frontal, temporal and parietal
association cortex, typically exceeds twice the background level. Follow-up studies with 11C-PIB in AD
indicate that there is no further increase in tracer uptake
during progression of the disease [51].
When used in tracer amounts, 11C-PIB is specific for
amyloids and does not bind to neurofibrillary tangles
[52]. Its clinical specificity for AD is currently being
studied and it has been shown that patients with
frontotemporal dementia do not show increased 11C-PIB
binding [53]. Findings in patients with MCI are heterogeneous, some show intensely increased binding, such as
AD patients, whereas others are within normal limits.
First results from follow-up studies of up to 18 months
indicate that patients with increased binding may indeed
progress to AD, but there are also patients and even a few
normal control subjects with increased uptake who
remain entirely stable [54]. Thus, it remains to be
determined whether increased 11C-PIB uptake in elderly
individuals who are cognitively normal represents
false-positive findings or a presymptomatic stage of AD
that could become clinically manifest up to a decade later
(Figure 2).
A number of other compounds have been tested for
amyloid imaging in humans, and most of them have
properties similar to 11C-PIB without, so far, offering
clear advantages [52]. One compound, 18F-FDDNP, binds
to neurofibrillary tangles as well as amyloid plaques and
differentiates persons with mild cognitive impairment
from those with Alzheimers disease and those with no
cognitive impairment [55], but provides a substantially
weaker imaging signal that 11C-PIB.
Microglial activation
The peripheral benzodiazepine receptor site (PBBS) is
found on the outer membrane of mitochondria and is
expressed only at low levels in the healthy human brain.
Increased expression has been observed using the
specific ligand 11C-PK11195, which has been shown to
reflect the distribution of activated microglia in experimental and human brain disease [56, 57]. Activated
microglia are present at sites of aggregated Ab deposition in the brains of AD subjects, although their precise
role in the disease process remains unclear [58]. A
moderate yet significant increase in 11C-PK11195 binding
was observed in patients with AD compared with
healthy control subjects [59] and also in other neurodegenerative diseases such as frontotemporal lobar degeneration [60] and Huntingtons disease [61].
Imaging neurotransmitter systems
Major transmitter systems that are known to be
impaired in AD are the cholinergic, serotonergic and
noradrenergic innervations of the cerebral cortex. In
Parkinsons disease (PD) and related dementia, the
dopaminergic system is also impaired. The contribution
of these systems to the symptomatology has not yet been
studied in depth in humans, and there are indications
that impairment of these diffuse ascending projections
may interact with the formation of pathological protein
deposits such as amyloid plaques and a-synuclein in
dementia [62, 63].
Figure 2. Normal unspecific background of 11C-PIB binding in normal
control and one subject with mild
cognitive impairment (MCI) (MCI2) compared with increased cerebral cortical binding of this tracer to
amyloid in Alzheimers disease and
in another subject with MCI (MCI4), demonstrating the heterogeneity of findings in MCI. Permission
by William Klunk, University of Pittsburg. Copyright release by Informa
Healthcare/Taylor & Francis, NY.
The British Journal of Radiology, Special Issue 2007
S163
K Herholz, S F Carter and M Jones
Figure 3. Parametric images (orthogonal slices with masking of subcortical areas) of 11C-MP4A
hydrolysis rates, indicating reduced
acetyl cholinesterase activity in
Alzheimers disease compared with
normal control subjects.
Cholinergic receptors
Dopamine
The main receptor types for acetylcholine in the central
nervous system (CNS) are muscarinergic, with subtypes
M1 and M2, and nicotinergic. Tracers for imaging of these
receptors that have been used clinically are listed in
Table 1. Nicotinic receptors have attracted most interest
but available tracers still suffer from methodological
limitations. 11C-nicotine has a high level of unspecific
binding [64] and 18F-A85380 suffers from very slow
binding kinetics [65, 66]. There is reduced cortical
binding of 11C-nicotine in AD [67, 68].
The most widely used tracer to examine dopamine
synthesis and vesicular storage is 18F-fluorodopa [82]. A
deficit of dopamine synthesis similar to PD has been
found in DLB, even at a stage when Parkinsonism may
not yet be prominent [43], although no similar abnormality is seen in patients with AD. In contrast to the
cholinergic impairment, which is severe in DLB but only
mild in PD without dementia, the dopaminergic deficit
does not appear to be related to dementia [83].
Dopaminergic D2 receptors have received a lot of
attention, mostly in the context of normal ageing, which
is associated with a reduction of receptors [84], and
dopaminergic innervation may modulate cognitive function [85]. The most frequently used tracer for receptorbinding studies of the basal ganglia is 11C-raclopride,
which has largely replaced earlier studies with labelled
benzamides, whereas quantitation of cortical D2 receptors requires high-affinity ligands such as 18F-fallypride
[86]. So far, no major abnormalities have been found in
the major dementing diseases.
Acetylcholine esterase activity
The most important degrading enzyme for acetylcholine in the human cortex is acetyl cholinesterase (AChE),
which is present in cholinergic axons and relatively few
cholinoceptive neurons. As the cholinergic axons degenerate AChE activity is reduced [69]. Labelled analogues
of acetylcholine which are also substrates for AChE can
be used to measure and image its activity in vivo. These
are C-11-N-methyl-4-piperidyl-acetate (MP4A, also
known as AMP) [70], which is 94% specific for AChE
in human brain, and C-11-N-methyl-4-piperidyl-propionate (MP4P, or PMP) [71]. There have been several
studies measuring AChE activity and all of them found a
reduction of cortical activity in AD [7275] that most
severely affected the temporal cortex (Figure 3). The
technique has also been used to measure drug-induced
AChE inhibition in AD patients, which for all currently
available cholinesterase inhibitors at the standard clinical
dose is in the range of 3040% [7678].
Serotonin
Impairment of serotonergic innervation has mostly
been studied in the context of depression, and depression is also a major clinical issue in dementia. A
reduction of receptor-binding potential in AD has been
observed mainly for 5-HT(2A) receptors [79, 80]. In MCI,
reduced 5-HT(2A) binding in the striatum was correlated
with depression and anxiety scores [81].
S164
Summary
Brain PET using FDG is a firmly established technique
for demonstration of regional functional impairment in
neurodegenerative disease. AD is associated with typical
regional impairment of posterior cortical association
areas that allow very early diagnosis before clinical
manifestation of dementia and monitoring of progression and treatment effects. DLB additionally involves
metabolic impairment of the primary visual cortex.
Predominant impairment of the frontal and anterior
temporal regions is seen in FTD, primary progressive
aphasia and semantic dementia. New perspectives are
opened by tracers for imaging amyloids, which appear to
be very sensitive for detecting even preclinical AD cases,
although confirmation of the specificity remains to be
demonstrated. Tracers for measuring local AChE activity
and the binding capacity of nicotinic and serotonergic
receptors address neurotransmitter deficits in dementia.
Impairment of dopamine synthesis that is characteristic
for DLB can be demonstrated by 18F-fluorodopa PET.
The British Journal of Radiology, Special Issue 2007
PET imaging in dementia
References
1. Herholz K, Herscovitch P, Heiss WD. NeuroPET. Berlin/
New York: Springer, 2004.
2. Sokoloff L. Relation between physiological function and
energy metabolism in the central nervous system. [Review].
Journal of Neurochemistry 1977;29:1326.
3. Kuhl DE, Metter EJ, Riege WH, Phelps ME. Effects of
human aging on patterns of local cerebral glucose utilization determined by the [18F]fluorodeoxyglucose method.
Journal of Cerebral Blood Flow & Metabolism 1982;2:
16371.
4. Herholz K. PET studies in dementia. Annals of Nuclear
Medicine 2003;17:7989.
5. Bartzokis G, Lu PH, Mintz J. Human brain myelination and
amyloid beta deposition in Alzheimers disease.
Alzheimers and Dement 2007;3:1225.
6. Minoshima S, Giordani B, Berent S, Frey KA, Foster NL,
Kuhl DE. Metabolic reduction in the posterior cingulate
cortex in very early Alzheimers disease. Ann Neurol
1997;42:8594.
7. Gusnard DA, Raichle ME, Raichle ME. Searching for a
baseline: functional imaging and the resting human brain.
Nat Rev Neurosci 2001;2:68594.
8. Herholz K, Salmon E, Perani D, Baron JC, Holthoff V,
Frolich L, et al. Discrimination between Alzheimer dementia and controls by automated analysis of multicenter FDG
PET. NeuroImage 2002;17:30216.
9. Burdette JH, Minoshima S, Vander Borght T, Tran DD, Kuhl
DE. Alzheimer disease: improved visual interpretation of
PET images by using three-dimensional stereotaxic surface
projections. Radiology 1996;198:83743.
10. Ishii K, Willoch F, Minoshima S, Drzezga A, Ficaro EP,
Cross DJ, et al. Statistical brain mapping of 18F-FDG PET in
Alzheimers disease: validation of anatomic standardization
for atrophied brains. J Nucl Med 2001;42:54857.
11. Azari NP, Pettigrew KD, Schapiro MB, Haxby JV, Grady
CL, Pietrini P, et al. Early detection of Alzheimers disease:
a statistical approach using positron emission tomographic
data. Journal of Cerebral Blood Flow & Metabolism
1993;13:43847.
12. Kippenhan JS, Barker WW, Nagel J, Grady C, Duara R.
Neural-network classification of normal and Alzheimers
disease subjects using high-resolution and low-resolution
PET cameras. Journal of Nuclear Medicine 1994;35:715.
13. Higdon R, Foster NL, Koeppe RA, DeCarli CS, Jagust WJ,
Clark CM, et al. A comparison of classification methods for
differentiating fronto-temporal dementia from Alzheimers
disease using FDG-PET imaging. Stat Med 2004;23:31526.
14. Johnson NA, Jahng GH, Weiner MW, Miller BL, Chui HC,
Jagust WJ, et al. Pattern of cerebral hypoperfusion in
Alzheimer disease and mild cognitive impairment measured with arterial spin-labeling MR imaging: initial
experience. Radiology 2005;234:8519.
15. Herholz K, Schopphoff H, Schmidt M, Mielke R, Eschner
W, Scheidhauer K, et al. Direct comparison of spatially
normalized PET and SPECT scans in Alzheimer disease.
Journal of Nuclear Medicine 2002;43:216.
16. Messa C, Perani D, Lucignani G, Zenorini A, Zito G, et al.
High-resolution technetium-99m-HMPAO SPECT in
patients with probable Alzheimers disease: comparison
with fluorine-18-FDG PET. Journal of Nuclear Medicine
1994;35:21016.
17. Powers WJ, Perlmutter JS, Videen TO, Herscovitch P,
Griffeth LK, Royal HD, et al. Blinded clinical evaluation
of positron emission tomography for diagnosis of probable
Alzheimers disease. Neurology 1992;42:76570.
18. Jagust WJ, Friedland RP, Budinger TF, Koss E, Ober B.
Longitudinal studies of regional cerebral metabolism in
Alzheimers disease. Neurology 1988;38:90912.
The British Journal of Radiology, Special Issue 2007
19. Mielke R, Herholz K, Grond M, Kessler J, Heiss WD.
Clinical deterioration in probable Alzheimers disease
correlates with progressive metabolic impairment of association areas. Dementia 1994;5:3641.
20. Smith GS, de Leon MJ, George AE, Kluger A, Volkow ND,
McRae T, et al. Topography of cross-sectional and longitudinal glucose metabolic deficits in Alzheimers disease.
Pathophysiologic implications. Arch Neurol 1992;49:
11421150.
21. Grady CL, Haxby JV, Schlageter NL, Berg G, Rapoport SI.
Stability of metabolic and neuropsychological asymmetries
in dementia of the Alzheimer type. Neurology
1986;36:13902.
22. Haxby JV, Grady CL, Koss E, Horwitz B, Heston L,
Schapiro M, et al. Longitudinal study of cerebral metabolic
asymmetries and associated neuropsychological patterns in
early dementia of the Alzheimer type. Archives in
Neurology 1990;47:75360.
23. Heiss WD, Kessler J, Mielke R, Szelies B, Herholz K. Longterm effects of phosphatidylserine, pyritinol, and cognitive
training in Alzheimers disease. A neuropsychological,
EEG, and PET investigation. Dementia 1994;5:8898.
24. Alexander GE, Chen K, Pietrini P, Rapoport SI, Reiman EM.
Longitudinal PET evaluation of cerebral metabolic decline
in dementia: a potential outcome measure in Alzheimers
disease treatment studies. Am. J Psychiatry 2002;159:
73845.
25. Hirono N, Hashimoto M, Ishii K, Kazui H, Mori E. Oneyear change in cerebral glucose metabolism in patients with
Alzheimers disease. J Neuropsychiatry Clin Neurosci
2004;16:48892.
26. Small GW, Mazziotta JC, Collins MT, Baxter LR, Phelps ME,
Mandelkern MA, et al. Apolipoprotein E type 4 allele and
cerebral glucose metabolism in relatives at risk for familial
Alzheimer disease. JAMA 1995;273:9427.
27. Reiman EM, Caselli RJ, Yun LS, Chen K, Bandy D,
Minoshima S, et al. Preclinical evidence of Alzheimers
disease in persons homozygous for the epsilon 4 allele for
apolipoprotein E. New England Journal of Medicine
1996;334:7528.
28. Reiman EM, Chen K, Alexander GE, Caselli RJ, Bandy D,
Osborne D, et al. Functional brain abnormalities in young
adults at genetic risk for late-onset Alzheimers dementia.
Proc Natl Acad Sci USA 2004;101:2849.
29. Small GW, Ercoli LM, Silverman DH, Huang SC, Komo S,
Bookheimer SY, et al. Cerebral metabolic and cognitive
decline in persons at genetic risk for Alzheimers disease.
Proc Natl Acad Sci USA 2000;97:603742.
30. Drzezga
A,
Grimmer
T,
Riemenschneider
M,
Lautenschlager N, Siebner H, Alexopoulus P, et al.
Prediction of individual clinical outcome in MCI by means
of genetic assessment and (18)F-FDG PET. J Nucl Med
2005;46:162532.
31. Anchisi D, Borroni B, Franceschi M, Kerrouche N, Kalbe E,
Beuthien-Beumann B, et al. Heterogeneity of brain glucose
metabolism in mild cognitive impairment and clinical
progression to Alzheimer disease. Arch Neurol 2005;62:
172833.
32. Heiss WD, Pawlik G, Holthoff V, Kessler J, Szelies B. PET
correlates of normal and impaired memory functions
[Review]. Cerebrovascular & Brain Metabolism Reviews
1992;4:127.
33. Nestor PJ, Fryer TD, Smielewski P, Hodges JR. Limbic
hypometabolism in Alzheimers disease and mild cognitive
impairment. Ann Neurol 2003;54:34351.
34. Mosconi L, Tsui WH, DeSanti S, Li J, Rusinek H, Convit A,
et al. Reduced Hippocampal metabolism in MCI and AD:
automated
FDG-PET
image
analysis.
Neurology
2005;64:18607.
S165
K Herholz, S F Carter and M Jones
35. de Leon MJ, Convit A, Wolf OT, Tarshish CY, DeSanti S,
Rusinek H, et al. Prediction of cognitive decline in normal
elderly subjects with 2-F-18-fluoro-2-deoxy-D-glucose positron-emission tomography (FDG PET). Proc Natl Acad Sci
USA 2001;98:1096671.
36. Neary D, Snowden J, Mann D. Frontotemporal dementia.
Lancet Neurol 2005;4:77180.
37. Salmon E, Garraux G, Delbeuck X, Collette F, Kalbe E,
Zuendorf G, et al. Predominant ventromedial frontopolar
metabolic impairment in frontotemporal dementia.
NeuroImage 2003;20:43540.
38. Diehl J, Grimmer T, Drzezga A, Riemenschneider M, Forstl
H, Kurz A. Cerebral metabolic patterns at early stages of
frontotemporal dementia and semantic dementia. A PET
study. Neurobiol Aging 2004;25:10516.
39. Chawluk JB, Mesulam MM, Hurtig H, Kushner M,
Weintraub S, Saykin A, et al. Slowly progressive aphasia
without generalized dementia: studies with positron emission tomography. Annals of Neurology 1986;19:6874.
40. Ishii K, Sakamoto S, Sasaki M, Kitagaki H, Yamaji S,
Hashimoto M, et al. Cerebral glucose metabolism in
patients with frontotemporal dementia. Journal of Nuclear
Medicine 1998;39:18758.
41. Foster NL, Heidebrink JL, Clark CM, Jagust WJ, Arnold SE,
Barbas NR, et al. FDG-PET improves accuracy in distinguishing frontotemporal dementia and Alzheimers disease. Brain 2007;130:261635.
42. Minoshima S, Foster NL, Sima AA, Frey KA, Albin RL,
Kuhl DE. Alzheimers disease versus dementia with Lewy
bodies: cerebral metabolic distinction with autopsy confirmation. Ann Neurol 2001;50:35865.
43. Hu XS, Okamura N, Arai H, Higuchi M, Matsui T, Tashiro
M, et al. 18F-fluorodopa PET study of striatal dopamine
uptake in the diagnosis of dementia with lewy bodies.
Neurology 2000;55:15757.
44. Braak H, Braak E. Neuropathological staging of Alzheimerrelated changes. Acta Neuropathologica 1991;82:23959.
45. Hardy JA, Higgins GA. Alzheimers disease: the amyloid
cascade hypothesis. (Perspective). Science 1992;256:184.
46. Klunk WE, Engler H, Nordberg A, Wang Y, Blomqvist G,
Holt DP, et al. Imaging brain amyloid in Alzheimers
disease with Pittsburgh Compound-B. Annals of Neurology
2004;55:30619.
47. Price JC, Klunk WE, Lopresti BJ, Lu X, Hoge JA, Ziolko SK,
et al. Kinetic modeling of amyloid binding in humans using
PET imaging and Pittsburgh Compound-B. J Cereb Blood
Flow Metab 2005;25:152847.
48. Edison P, Archer HA, Hinz R, Hammers A, Pavese N, Tai
YF, et al. Amyloid, hypometabolism, and cognition in
Alzheimer disease: an [11C]PIB and [18F]FDG PET study.
Neurology 2007;68:5018.
49. Kemppainen NM, Aalto S, Wilson IA, Nagren K, Helin S,
Bruck A, et al. Voxel-based analysis of PET amyloid ligand
[11C]PIB uptake in Alzheimer disease. Neurology
2006;67:157580.
50. Nordberg A. PET imaging of amyloid in Alzheimers
disease. Lancet Neurology 2004;3:519527.
51. Engler H, Forsberg A, Almkvist O, Blomquist G, Larsson E,
Savitcheva I, et al. Two-year follow-up of amyloid deposition in patients with Alzheimers disease. Brain
2006;129:285666.
52. Klunk WE, Lopresti B, Nebes RD, Price JC, Tsopelas N,
DeKosky ST, et al. Development and Application of betaamyloid imaging agents in Alzheimers Disease. In:
Herholz K, Perani D, Morris CM, editors. The dementias:
Early Diagnosis and Evaluation. New York: Dekker;
2006:279303.
53. Rabinovici GD, Furst AJ, ONeil JP, Racine CA, Mormino
EC, Baker SL, et al. 11C-PIB PET imaging in Alzheimer
S166
54.
55.
56.
57.
58.
59.
60.
61.
62.
63.
64.
65.
66.
67.
68.
69.
70.
71.
disease and frontotemporal lobar degeneration. Neurology
2007;68:120512.
Forsberg A, Engler H, Almkvist O, Bolmquist G, Hagman
G, Wall A, et al. PET imaging of amyloid deposition in
patients with mild cognitive impairment. Neurobiol Aging
2007 [epub ahead of print].
Small GW, Kepe V, Ercoli LM, Siddarth P, Bookheimer SY,
Miller KJ, et al. PET of brain amyloid and tau in mild
cognitive impairment. N Engl J Med 2006;355:265263.
Cagnin A, Brooks DJ, Kennedy AM, Gunn RN, Myers R,
Turkheimer FE, et al. In-vivo measurement of activated
microglia in dementia. Lancet 2001;358:4617.
Banati RB, Newcombe J, Gunn RN, Cagnin A, Turkheimer
F, Heppner F, et al. The peripheral benzodiazepine binding
site in the brain in multiple sclerosis: quantitative in vivo
imaging of microglia as a measure of disease activity. Brain
2000;123:232137.
McGeer PL, Rogers J. Anti-inflammatory agents as a therapeutic approach to Alzheimers disease. Neurology 1992;42:4479.
Cagnin A, Brooks DJ, Kennedy AM, Gunn RN, Myers R,
Turkheimer FE, et al. In-vivo measurement of activated
microglia in dementia. Lancet 2001;358:4617.
Cagnin A, Rossor M, Sampson EL, Mackinnon T, Banati RB.
In vivo detection of microglial activation in frontotemporal
dementia. Ann Neurol 2004;56:8947.
Pavese N, Gerhard A, Tai YF, Ho AK, Turkheimer F, Barker
RA, et al. Microglial activation correlates with severity in
Huntington disease: A clinical and PET study. Neurology
2006;66:163843.
Heneka MT, Ramanathan M, Jacobs AH, DumitrescuOzimek L, Bilkei-Gorzo A, Debeir T, et al. Locus ceruleus
degeneration promotes Alzheimer pathogenesis in amyloid
precursor protein 23 transgenic mice. J Neurosci
2006;26:134354.
Braak H, Rub U, Schultz C, Del Tredici K. Vulnerability of
cortical neurons to Alzheimers and Parkinsons diseases. J
Alzheimers Dis 2006;9:3544.
Nordberg A, Lundqvist H, Hartvig P, Lilja A, Langstrom B.
Kinetic analysis of regional (S)(-)11C-nicotine binding in
normal and Alzheimer brains in vivo assessment using
positron emission tomography. Alzheimer Dis Assoc
Disord 1995;9:217.
Bottlaender M, Valette H, Roumenov D, Dolle F, Coulon C,
Ottaviani M, et al. Biodistribution and radiation dosimetry
of (18)f-fluoro-a-85380 in healthy volunteers. Journal of
Nuclear Medicine 2003;44:596601.
Mamede M, Ishizu K, Ueda M, Mukai T, Iida Y, Fukuyama
H, et al. Quantification of human nicotinic acetylcholine
receptors with 123I-5IA SPECT. Journal of Nuclear
Medicine 2004;45:145870.
Nordberg A, Lundqvist H, Hartvig P, Lilja A, Langstrom B.
Kinetic analysis of regional (S)(-)11C-nicotine binding in
normal and Alzheimer brains in vivo assessment using
positron emission tomography. Alzheimer Disease &
Associated Disorders 1995;9:217.
Kadir A, Almkvist O, Wall A, Langstrom B, Nordberg A.
PET imaging of cortical 11C-nicotine binding correlates
with the cognitive function of attention in Alzheimers
disease. Psychopharmacology (Berl) 2006;188:50920.
Mesulam M, Giacobini E. Neuroanatomy of cholinesterases
in the normal human brain and in Alzheimers disease. In:
Cholinesterases and cholinesterase inhibitors. London, UK:
Martin Dunitz, 2000: 12137.
Namba H, Irie T, Fukushi K, Iyo M. In vivo measurement of
acetylcholinesterase activity in the brain with a radioactive
acetylcholine analog. Brain Research 1994;667:27882.
Kilbourn MR, Snyder SE, Sherman PS, Kuhl DE. In vivo
studies of acetylcholinesterase activity using a labeled
substrate, n-[C-11]methylpiperdin-4-yl propionate ([C11]PMP). Synapse 1996;22:12331.
The British Journal of Radiology, Special Issue 2007
PET imaging in dementia
72. Kuhl DE, Koeppe RA, Minoshima S, Snyder SE, Ficaro EP,
Foster NL, et al. In vivo mapping of cerebral acetylcholinesterase activity in aging and Alzheimers disease.
Neurology 1999;52:6919.
73. Iyo M, Namba H, Fukushi K, Shinotoh H, Nagatsuka S,
Suhara T, et al. Measurement of acetylcholinesterase by
positron emission tomography in the brains of healthy
controls and patients with Alzheimers disease. Lancet
1997;349:18059.
74. Herholz K, Bauer B, Wienhard K, Kracht L, Mielke R, Lenz
O, et al. In-vivo measurements of regional acetylcholine
esterase activity in degenerative dementia: comparison with
blood flow and glucose metabolism. J Neural Transm
2000;12:145768.
75. Rinne JO, Kaasinen V, Jarvenpaa T, Nagren K, Roivainen A, Yu
M, et al. Brain acetylcholinesterase activity in mild cognitive
impairment and early Alzheimers disease. Journal of
Neurology, Neurosurgery, and Psychiatry 2003;74:11315.
76. Bohnen NI, Kaufer DI, Hendrickson R, Ivanco LS, Lopresti
BJ, Koeppe RA, et al. Degree of inhibition of cortical
acetylcholinesterase activity and cognitive effects by donepezil treatment in Alzheimers disease. Journal of
Neurology, Neurosurgery, and Psychiatry 2005;76:31519.
77. Kaasinen V, Nagren K, Jarvenpaa T, Roivainen A, Yu M,
Oikonen V, et al. Regional effects of donepezil and
rivastigmine on cortical acetylcholinesterase activity in
Alzheimers disease. J Clin Psychopharmacol 2002;22:61520.
78. Kadir A, Darreh-Shori T, Almkvist O, Wall A, Grut M,
Strandberg B, et al. PET imaging of the in vivo brain
acetylcholinesterase activity and nicotine binding in galantamine-treated patients with AD. Neurobiol Aging 2007
[epub ahead of print].
79. Blin J, Crouzel C. Blood-cerebrospinal fluid and blood-brain
barriers imaged by 18F-labeled metabolites of 18F-setoperone studied in humans using positron emission tomography. Journal of Neurochemistry 1992;58:230310.
80. Meltzer CC, Price JC, Mathis CA, Greer PJ, Cantwell MN,
Houck PR, et al. PET imaging of serotonin type 2A
receptors in late-life neuropsychiatric disorders. Am J
Psychiatry 1999;156:18718.
The British Journal of Radiology, Special Issue 2007
81. Hasselbalch SG, Madsen K, Svarer C, Pinborg LH, Holm S,
Paulson OB, et al. Reduced 5-HT(2A) receptor binding in
patients with mild cognitive impairment. Neurobiol Aging
2007 [epub ahead of print].
82. Brooks DJ. Advances in imaging Parkinsons disease. Curr
Opin Neurol 1997;10:32731.
83. Hilker R, Thomas A, Klein JC, Weisenbach S, Kalbe E,
Burghaus L, et al. Dementia in Parkinsons disease:
functional imaging of cholinergic and dopaminergic pathways. Neurology 2005;65:171622.
84. Rinne JO, Hietala J, Ruotsalainen U, Sako E, Laihinen A,
Nagren K, et al. Decrease in human striatal dopamine D2
receptor density with age: a PET study with
[11C]raclopride. Journal of Cerebral Blood Flow &
Metabolism 1993;13:31014.
85. Kaasinen V, Rinne JO. Functional imaging studies of
dopamine system and cognition in normal aging and
Parkinsons disease. Neurosci Biobehav Rev 2002;26:78593.
86. Slifstein M, Hwang DR, Huang Y, Guo N, Sudo Y,
Narendran R, et al. In vivo affinity of [(18)F]fallypride for
striatal and extrastriatal dopamine D(2) receptors in nonhuman primates. Psychopharmacology (Berl) 2004;175:27486.
87. Herholz K, Nordberg A, Salmon E, Perani D, Kessler J,
Mielke R, et al. Impairment of neocortical metabolism
predicts progression in Alzheimers disease. Dement
Geriatr Cogn Disord 1999;10:494504.
88. Berent S, Giordani B, Foster N, Minoshima S, LajinessONeill R, Koeppe R, et al. Neuropsychological function
and cerebral glucose utilization in isolated memory
impairment and Alzheimers disease. J Psychiatr Res
1999;33:716.
89. Arnaiz E, Jelic V, Almkvist O, Wahlund LO, Winblad B,
Valind S, et al. Impaired cerebral glucose metabolism and
cognitive functioning predict deterioration in mild cognitive impairment. Neuroreport 2001;12:8515.
90. Chetelat G, Desgranges B, de la Sayette V, Viader F,
Eustache F, Baron JC. Mild cognitive impairment: Can
FDG-PET predict who is to rapidly convert to Alzheimers
disease? Neurology 2003;60:13747.
S167
Das könnte Ihnen auch gefallen
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5795)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- A Mini Project Report On "Issues Challenge and Application of Emerging Technologies in The Pharmaceutical Industry"Dokument42 SeitenA Mini Project Report On "Issues Challenge and Application of Emerging Technologies in The Pharmaceutical Industry"Raja Medical StoreNoch keine Bewertungen
- A Case Study of Hospital Operations ManagementDokument10 SeitenA Case Study of Hospital Operations ManagementDaniel Goncalves50% (2)
- PRACTICE GUIDELINE For The Treatment of Patients With SchizophreniaDokument184 SeitenPRACTICE GUIDELINE For The Treatment of Patients With SchizophreniabencortesmoralesNoch keine Bewertungen
- Ruppels Manual of Pulmonary Function Testing 11th EditionDokument61 SeitenRuppels Manual of Pulmonary Function Testing 11th Editiondanny.johnson566100% (43)
- National Quality Assurance Standards: Mandatory Requirements PHC/CHCDokument14 SeitenNational Quality Assurance Standards: Mandatory Requirements PHC/CHCSathish KumaarNoch keine Bewertungen
- Morning Report: Supervisor: Dr. Rusdhy A.H., SP - OG Medical StudentsDokument8 SeitenMorning Report: Supervisor: Dr. Rusdhy A.H., SP - OG Medical StudentsEra MoetzNoch keine Bewertungen
- IHSCforAll2024Dokument510 SeitenIHSCforAll2024Gvidas MikalauskasNoch keine Bewertungen
- Ymaa TrainingDokument4 SeitenYmaa TraininganattāNoch keine Bewertungen
- Quality of Operation Notes Audit PresentationDokument31 SeitenQuality of Operation Notes Audit PresentationPushpinder Singh SandhuNoch keine Bewertungen
- Interpretation of Peripheral SmearDokument34 SeitenInterpretation of Peripheral Smearswathi bs100% (1)
- Surgical Correction Subglottic Stenosis of The Larynx: AnnoldDokument6 SeitenSurgical Correction Subglottic Stenosis of The Larynx: Annoldcanndy202Noch keine Bewertungen
- HfiDokument4 SeitenHfiakalaw3Noch keine Bewertungen
- Phytochemical Analysis of Bryophyllum Pinnatum Leaves Exposed To Water PollutionDokument14 SeitenPhytochemical Analysis of Bryophyllum Pinnatum Leaves Exposed To Water PollutionMarlonNoch keine Bewertungen
- Hazard Vulnerability Analysis WorkheetDokument10 SeitenHazard Vulnerability Analysis WorkheetFines AdemukhlisNoch keine Bewertungen
- Callyspongia SP Callyspongia SP: Identification of Antioxidant Compounds in The Sponge The SpongeDokument7 SeitenCallyspongia SP Callyspongia SP: Identification of Antioxidant Compounds in The Sponge The SpongeZulfajriNoch keine Bewertungen
- Osteopathic Considerations in Systemic Dysfunction (2nd Ed)Dokument296 SeitenOsteopathic Considerations in Systemic Dysfunction (2nd Ed)Natan Babek100% (1)
- The Accidental AddictsDokument6 SeitenThe Accidental AddictsnorthandsouthnzNoch keine Bewertungen
- Gongsun Sp-4: Grandfather GrandsonDokument2 SeitenGongsun Sp-4: Grandfather Grandsonray72roNoch keine Bewertungen
- Demographics: Discharge DocumentationDokument8 SeitenDemographics: Discharge Documentationjenny100% (1)
- Palpation and Assessment SkillsDokument305 SeitenPalpation and Assessment SkillsElin Taopan97% (34)
- Stratification in The Cox Model: Patrick BrehenyDokument20 SeitenStratification in The Cox Model: Patrick BrehenyRaiJúniorNoch keine Bewertungen
- USMLE - VirusesDokument120 SeitenUSMLE - Viruseszeal7777100% (1)
- Ownership, Operation, Maintenance, and Inspection of Amusement Rides and DevicesDokument4 SeitenOwnership, Operation, Maintenance, and Inspection of Amusement Rides and DevicesMarlon Piarpuito Enriquez0% (1)
- Bioplan Nieto Nahum)Dokument6 SeitenBioplan Nieto Nahum)Claudia Morales UlloaNoch keine Bewertungen
- RetailerPriceList OHDokument1 SeiteRetailerPriceList OHMuhammad Samiur RahmanNoch keine Bewertungen
- A Social Worker's Guide To Narrative Therapy - Daniel-StewartDokument3 SeitenA Social Worker's Guide To Narrative Therapy - Daniel-StewartangelaNoch keine Bewertungen
- Unani Product List PDFDokument109 SeitenUnani Product List PDFAK50% (2)
- MSDS Berkat Saintifindo PDFDokument27 SeitenMSDS Berkat Saintifindo PDFDianSelviaNoch keine Bewertungen
- Pneumonia Case StudyDokument21 SeitenPneumonia Case StudyEmel Brant Jallores0% (1)
- Xerostomia As A Potential Condition in PDokument4 SeitenXerostomia As A Potential Condition in PAlamsyah PiliangNoch keine Bewertungen