Beruflich Dokumente
Kultur Dokumente
BB Web Ans Focus 2010 Avances en El Tto de La Ansiedad Resistente. Lanouette
Hochgeladen von
Adriana Rodriguez PalmeroCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
BB Web Ans Focus 2010 Avances en El Tto de La Ansiedad Resistente. Lanouette
Hochgeladen von
Adriana Rodriguez PalmeroCopyright:
Verfügbare Formate
Advances in the
Management of TreatmentResistant Anxiety Disorders
Nicole M. Lanouette, M.D.
Murray B. Stein, M.D., M.P.H.
exist, many patientspossibly even 50 60%remain symptomatic despite first-line treatments. With the exception of
obsessive compulsive disorder (OCD), there are generally no universal definitions of treatment resistance and many
CLINICAL
SYNTHESIS
Abstract: Anxiety disorders are among the most common and disabling mental illnesses. While effective treatments
treatments (both pharmacologic and non-pharmacologic) have not been tested specifically in refractory cases. This article reviews the evidence for possible medication, psychotherapy, brain stimulation, and neurosurgical approaches
including some promising novel treatmentsfor managing treatment-resistant anxiety.
Anxiety disorders are among the most common and
disabling of mental disorders, making them a serious public health concern (1). Anxiety disorders are
associated with an increase in physician visits and
medical costs and with reduced productivity at
home and in the workplace (2). Although many
pharmacological (and nonpharmacological) treatments exist, the evidence suggests that these disorders in many patientsperhaps as many as 50%
60%are resistant or refractory to first-line
treatments (3). This scenario speaks to the compelling need for recommendations about managing
such patients.
There are two main challenges limiting clinicians
who aim to provide evidence-based care for treatment-resistant anxiety disorders. The first is a general lack of agreed-upon definitions as to what constitutes treatment resistance in anxiety. In broad
terms, our starting point in discussing treatmentresistant anxiety will be when a patient has not responded to one of two first-line treatments, for example, a serotonin-selective reuptake inhibitor
(SSRI) or cognitive behavior therapy (CBT). The
second challenge is that few studies have tested
strategies in treatment-refractory cases. Unless otherwise noted, the investigations reported here were
not tested after other treatments had failed. Given
this lack of specific data, the majority of this article
is a review of first-line efficacy studies. Although
not ideal, this is the best evidence currently available that holds potential utility for treatment planning after first-line treatments have been unsuccessful. Obsessive-compulsive disorder (OCD) is the
only exception; as discussed in the section on Ob-
focus.psychiatryonline.org
sessive-Compulsive Disorder, there are agreedupon definitions of treatment resistance, and strategies have been tested in patients with treatmentresistant OCD. An additional limitation of the
literature present for any disorder is publication
bias; positive findings are more likely to be published than negative results.
When facing a patient who appears to have a
treatment-refractory disorder, a critical first step is
to ensure that the patient has received adequate
first-line treatment. For example, many patients
considered to have a treatment-resistant disorder
have not yet received cognitive behavior therapy
(CBT), which is a valid first-line therapy, and once
they do receive such therapy respond well to it.
Unfortunately, access to good-quality CBT is limited in many practice settings, although computerized and Web-based delivery approaches are increasingly being investigated to increase the reach
of CBT (e.g., reference 4). Assessing adherence to
CME Disclosure
Nicole M. Lanouette, M.D., Department of Psychiatry, University of California San Diego and VA
San Diego Healthcare System, San Diego, CA
No relevant financial relationships to disclose.
Murray B. Stein, M.D., M.P.H., Department of Psychiatry, University of California San Diego, VA
San Diego Healthcare System, and Department of Family and Preventive Medicine, University of
California San Diego, San Diego, CA
Consultant: Bristol Myers Squibb
Address correspondence to Murray B. Stein, M.D., M.P.H., Professor of Psychiatry and Family &
Preventive Medicine, University of California, San Diego, 9500, Gilman Drive, Mailcode 0855,
La Jolla, CA 92093-0855, e-mail: mstein@ucsd.edu.
FOCUS
Fall 2010, Vol. VIII, No. 4
501
LANOUETTE AND STEIN
treatment is also useful to confirm that patients
have actually received an adequate trial of therapy and/or medication before moving on to therapies with a less well-established evidence base.
Another essential step is to reevaluate a patient
with a treatment-refractory disorder diagnostically to ensure that the principal diagnosis is correct and to ensure that there are not additional
comorbid disorders that would require a different treatment strategy.
We refer all readers to the up-to-date APA Practice Guideline for Panic Disorder (5) and Guideline (6) and more recent Guideline Watch (7) for
posttraumatic stress disorder (PTSD), as well as the
2007 Guideline for OCD (8), which are all excellent resources on evidence-based practice for both
initial treatment and treatment in refractory cases.
The 2008 World Federation of Societies of Biological Psychiatry guidelines for the pharmacological
treatment of anxiety and obsessive and post-traumatic stress disorders is another excellent review of
evidence-based pharmacotherapy (9). Consultation with a psychiatrist experienced in treating anxiety disorders is also recommended when one is
establishing a plan of care after first-line treatments
have failed. At the end of each section, we include a
case vignette example demonstrating possible approaches. Readers should note that in this review,
we generally do not discuss mechanisms of actions
or adverse effects of these medications and advise
readers to be familiar with these before using the
medication in clinical practice. In addition, reviewing the evidence for complementary or alternative
treatments is beyond the scope of this review.
PANIC
DISORDER
First-line treatment for panic disorder includes
any of the following: SSRI, serotonin norepinephrine reuptake inhibitor (SNRI) (venlafaxine is the
most studied, but duloxetine has a similar mechanism of action), tricyclic antidepressant (TCA) (the
most data are available for imipramine or clomipramine; TCAs often are not used as first-line treatment because of their side effect profile), benzodiazepine (not adequate monotherapy if there is a
co-occurring mood disorder), or CBT (5).
If one first-line treatment has failed or been inadequate, augmentation with or switching to another
first-line therapy is recommended. As with other
disorders, augmentation is generally preferable if a
patient has had a partial response, whereas switching to another agent will probably be more efficacious if there has been no response. Examples of
augmentation strategies include adding CBT or a
benzodiazepine to an SSRI or adding an SSRI to
502
Fall 2010, Vol. VIII, No. 4
FOCUS
CBT. A common reasonable switching strategy is
to cross-titrate from an SSRI that has been completely ineffective to another SSRI, to an SNRI, or,
less commonly, to a TCA. Only one randomized
controlled trial (RCT) (N46) has systematically
studied a series of interventions in patients with
panic disorder who failed to achieve remission with
initial SSRI monotherapy (10). Simon et al. (10)
noted that 21% of patients achieved remission after
6 weeks of initial SSRI monotherapy. Among those
who did not achieve remission, increasing the dose
of the SSRI in the next phase of the study was not
effective. In the third phase of the study, remission
rates were similarly low in both groups; CBT added
to the SSRI was comparable to clonazepam added
to the SSRI. Two open, noncontrolled studies
found CBT to be effective after failed pharmacotherapy (11, 12).
Although there is little evidence specifically addressing the question of whether therapy is effective
after failure with an SSRI, examining the more substantial data on using medication in combination
with therapy as initial treatment may be informative in guiding treatment planning for the patient
with a refractory disorder. An RCT of 150 patients
with panic disorder found that the combination of
CBT and an SSRI or SSRI alone was somewhat
superior to CBT alone at the end of treatment, but
this difference was no longer significant 6 and 12
months after treatment discontinuation (13). A
2006 meta-analysis of 21 RCTs of antidepressants
and psychotherapy (mostly behavior therapy or
CBT) for panic disorder concluded that in the initial phase of treatment, the combination of an antidepressant plus psychotherapy was better than either alone. In later phases of treatment,
combination therapy remained more effective than
antidepressants alone but was no better than psychotherapy alone (14). A recent meta-analysis of
the three RCTs that studied combining benzodiazepines with psychotherapy reported that there was
inadequate evidence to draw any definitive conclusions, but all studies found no advantage for combination treatment over monotherapy (15).
MONOAMINE
OXIDASE INHIBITORS
Although there is evidence supporting their use
in panic disorder, given their many potential adverse effects, monoamine oxidase inhibitors
(MAOIs) should generally be reserved for situations in which several first-line treatments have
failed. Phenelzine has proven effective for what
would now be called panic disorder in one open
(16) and two double-blind placebo-controlled
studies (17, 18). Most studies of MAOIs were done
THE JOURNAL OF LIFELONG LEARNING IN PSYCHIATRY
LANOUETTE AND STEIN
OTHER
ANTIDEPRESSANTS
As with MAOIs, the data on other antidepressants for panic disorder are limited to populations
with nontreatment-refractory disorders. The evidence in support of mirtazapine for panic disorder
includes three open-label studies (26 28) and one
small (N27) double-blind trial showing that mirtazapine was comparable in efficacy to fluoxetine
(29). Although three small open trials found nefazodone to be potentially beneficial for panic disorder (30 32), no RCTs have confirmed this finding,
and its use is limited by the risk of liver toxicity. In
one very small (N11) single-blind trial, trazodone
was efficacious for panic disorder (33), but two
larger RCTs found it ineffective in enhancing CBT
(34) and less effective than imipramine or alprazolam (35). There is insufficient evidence to either
support or refute the efficacy of bupropion in panic
disorder; it was found to be effective in one small
open trial (36) but not in another (37).
ANTICONVULSANTS
Anticonvulsants have been investigated for panic
disorder in small studies, only two of which were
focus.psychiatryonline.org
RCTs. In one RCT, gabapentin was efficacious in
the severely ill group, but there was no overall difference between gabapentin and placebo (38). Valproate was found to be effective in a very small open
study (N13) among patients with panic disorder
and mood instability who had not responded to
CBT and a first-line medication (39). Two other
very small open-label studies also support the use of
valproate for panic disorder, but these findings require confirmation in larger RCTs before it can be
recommended, particularly given its significant side
effects. Positive results in two case series of tiagabine (40, 41), suggested it could be beneficial for
patients with treatment-refractory disorders. However, a subsequent open trial (42) and an RCT (43)
found no difference between tiagabine and placebo.
One small (N14) controlled study found that
carbamazepine was statistically, but not clinically,
more effective than placebo (44). Positive results in
one case series (N3) of vigabatrin (45) and one
(N28) open-label study of levetiracetam (46)
suggested that further study of these agents in controlled trials is warranted.
CLINICAL
SYNTHESIS
before the publication of DSM-III and therefore
did not use the panic disorder diagnosis; however,
the description of symptoms is consistent with
panic disorder. Doses found effective in those studies were fairly low, usually up to 45 mg/day. It is
possible that higher doses may be needed for patients with treatment-resistant panic disorder, but
no trials specifically address this question.
The reversible MAOIs are appealing, given that
they do not typically require adherence to a lowtyramine diet or a 2-week washout period before
starting. However, the studies examining moclobemide (which is not currently available in the United
States) for panic disorder have yielded mixed results: two studies showed positive results, finding it
comparable to fluoxetine (19) and clomipramine
(20), whereas one showed benefit only for seriously
ill patients (21), and another found no benefit over
placebo (22). Brofaromine is a reversible MAOI
that also inhibits serotonin reuptake. It is not available for use but has been found in three RCTs to be
more effective than placebo (23) and as effective as
fluvoxamine (24) or clomipramine (25). There
have been no published studies of selegiline for
panic disorder. None of the studies of MAOIs or
reversible MAOIs were specifically conducted with
treatment-resistant patients, so it is not known how
effective they would be in patients for whom an
SSRI, benzodiazepine, or CBT has failed.
ANTIPSYCHOTICS
No evidence supports the use of first-generation
antipsychotics in panic disorder. There is only preliminary positive evidence for some second-generation antipsychotics. Two open-label studies have
examined olanzapine monotherapy (47) and olanzapine augmentation after a failed SSRI trial (48)
with positive results. Risperidone augmentation
appeared to be effective for panic disorder that had
not responded to an SSRI and/or benzodiazepine in
a small 8-week open-label study (N30) (49). A
more recent randomized, rater-blinded trial
(N56) found risperidone monotherapy equivalent to paroxetine (50). An open-label study of patients with refractory panic disorder or generalized
anxiety disorder (GAD) found that aripiprazole
augmentation of an SSRI and/or benzodiazepine
significantly reduced anxiety (51). The only data on
ziprasidone for refractory panic disorder is a small
case series with positive results (52). Given the significant risk of metabolic side effects and the lack of
conclusive evidence about their efficacy, secondgeneration antipsychotics cannot be widely recommended as second-line agents in panic disorder, but
they could have utility in severe refractory cases.
OTHER
MEDICATIONS
The evidence points to buspirone monotherapy
being ineffective for panic disorder. Randomized
double-blind placebo-controlled trials have found
FOCUS
Fall 2010, Vol. VIII, No. 4
503
LANOUETTE AND STEIN
buspirone to be comparable to placebo and less effective than imipramine (N52) (53) and alprazolam (N92) (54). Another RCT (N60) detected
no difference between buspirone, imipramine, or
placebo groups (55), which the authors attributed
in part to a strong placebo response. A small
(N16) randomized study concluded that clorazepate was significantly more effective than buspirone (56). Another RCT (N91) found that buspirone did not enhance the efficacy of CBT for
panic attacks, although there was an initial benefit
at 16 weeks for agoraphobia and generalized anxiety that did not persist (57). Because buspirone is
more commonly used clinically as an adjunctive
agent than as monotherapy, controlled trials investigating its efficacy in conjunction with first-line
agents in refractory cases would be valuable.
d-Cycloserine is a partial agonist of the N-methyl-D-aspartate receptor that has been shown to enhance extinction learning (58). A recent RCT lends
strong preliminary support for adding d-cycloserine to exposure-based CBT for panic disorder
(59). Although d-cycloserine requires further study,
particularly in patients in whom first-line treatments have failed, it holds promise in enhancing
CBT.
use of CBT, the evidence is sparse and essentially
nonexistent for treatment-resistant cases.
OTHER
There have not been any controlled investigations of electroconvulsive therapy (ECT) or repetitive transcranial magnetic stimulation (rTMS) for
refractory panic disorder. Although most commonly performed for refractory OCD, capsulotomy, the neurosurgical technique of producing bilateral lesions in the anterior limb of the internal
capsule, has rarely been performed for severe treatment-refractory panic disorder. In their case series
of 26 patients with refractory panic disorder
(N8), GAD, or social phobia, Ruck et al. (63)
reported significant 1-year and long-term reductions in anxiety but also noted that seven patients
had substantial adverse side effects, most commonly frontal lobe dysfunction. More recently,
deep brain stimulation (DBS) has been investigated
for refractory OCD, but it has not been tested in
panic disorder. At this time, psychosurgical approaches to treatment-refractory panic disorder
cannot be advocated based on the evidence.
CASE
ANTIHYPERTENSIVES
There is little evidence on the use of antihypertensives for panic disorder and even less data on
their use in treatment-resistant disorders. One
RCT of 25 patients with treatment-refractory disorders that showed positive results supports use of
pindolol to augment fluoxetine (60), but these data
have not been replicated.
OTHER
PSYCHOTHERAPIES
There is substantial evidence to support use of
CBT, either in individual or group format, as a
first-line treatment in panic disorder (5), but there
is little evidence to guide the choice of alternative
psychotherapies in a patient in whom CBT has not
worked or in a patient who prefers another type of
therapy. A manualized psychoanalytic psychotherapy called panic-focused psychodynamic psychotherapy was shown to be more effective than applied relaxation training in an RCT of 49 patients
with panic disorder (61). Forms of psychodynamic
psychotherapy other than panic-focused psychodynamic psychotherapy have not been tested in controlled trials. Emotion-focused therapy, a supportive psychotherapy, was found to be less effective
than imipramine and CBT and comparable to placebo for panic disorder (62). In general, beyond the
504
Fall 2010, Vol. VIII, No. 4
FOCUS
TREATMENTS
VIGNETTE
A 23-year-old female college student with panic
disorder with agoraphobia has been taking sertraline at 200 mg/day (the highest tolerable dose for
her) for 8 weeks. She reports a significant decrease
in the frequency and intensity of panic attacks but
continues to avoid many activities because of fear of
attacks and continues to have difficulty falling
asleep because of fear of night-time panic attacks.
You add a low dose (0.25 mg) of clonazepam twice
daily. Her sleep improves, but she reports excessive
daytime sleepiness and feels cognitively dulled and
continues to have problems with avoidance. In addition, she expresses the desire to minimize the use
of medication. You refer her for CBT, continue the
SSRI at the present dose, and reduce the clonazepam to only one 0.25-mg dose at bedtime. After
12 weeks of CBT, there has been a further significant reduction in the number and intensity of attacks, and she has resumed many of the activities
she previously avoided. She finds she needs the
clonazepam only a few nights a week. After 20
weeks, her panic disorder is in remission, she continues to practice the techniques learned in CBT,
and she no longer needs the clonazepam. You develop a treatment plan with her to continue the
SSRI for another 6 months until summer break, at
which time you successfully taper her off it, with
the help of booster CBT sessions.
THE JOURNAL OF LIFELONG LEARNING IN PSYCHIATRY
LANOUETTE AND STEIN
GENERALIZED
ANXIETY DISORDER
OTHER
ANTIDEPRESSANTS
There is a general paucity of data, including even
efficacy studies in treatment-naive patients, on use
of other antidepressants for GAD. There has been
only one double-blind placebo-controlled trial of a
TCA for GAD. In their 8-week RCT (N230)
comparing imipramine, trazodone, and diazepam,
Rickels et al. (66) found all three medications superior to placebo. Although diazepam worked most
quickly, imipramine showed comparable, and on
one measure even superior, efficacy by the studys
end. That trial is also the only investigation of trazodone, which was also found to be slightly more
efficacious than diazepam at 8 weeks. There have
been no RCTs of MAOIs or reversible MAOIs
among patients with GAD. One small (N24)
double-blind, randomized trial found bupropion
XL comparable to escitalopram in anxiolytic efficacy, but there have not yet been any larger controlled confirmatory studies. Mirtazapine (67) and
nefazodone (68) have shown promise for GAD in
open trials, but larger RCTs are needed. None of
focus.psychiatryonline.org
ANTIHYPERTENSIVES
Antihypertensives have received little study for
GAD, and neither of the two published trials focused on patients with treatment-refractory GAD.
The one published RCT of -blockers (N49) for
generalized anxiety found both propranolol and
atenolol to be significantly more efficacious than
placebo for patients awaiting therapy, but atenolol
produced more intolerable cardiovascular side effects leading to more study dropouts (69). A double-blind crossover trial of clonidine (N23) for
patients with GAD or panic disorder found that it
was it modestly superior to placebo for anxiety (70).
CLINICAL
SYNTHESIS
First-line treatment options for GAD include
SSRIs, SNRIs, benzodiazepines (not adequate
monotherapy for GAD with comorbid depression),
buspirone, and CBT. As in panic disorder, if monotherapy with one of these agents is not successful, a
reasonable next step is to either 1) augment the first
agent (usually chosen if there was a partial response
to the first treatment) or 2) switch to another firstline treatment (64).
Only one study has examined whether a different
first-line treatment for GAD is effective after a first
has failed. Schneier et al. (63) examined whether
open-label escitalopram was beneficial for persistent symptoms of generalized anxiety after at least
12 sessions of CBT (65). Eight of the original 24
participants entering the study had clinically significant symptoms after 12 weeks of treatment. Four
of those eight subsequently completed 12 weeks of
open-label escitalopram treatment. Among those
four, there was a statistical trend toward pre to post
improvement on the primary outcome measure.
Although these results are suggestive of a possible
benefit, larger controlled trials are needed before
any conclusions can be drawn about the efficacy of
SSRIs for residual symptoms after CBT. There
have not yet been any studies addressing the question of whether CBT is effective for persistent
symptoms after SSRI or SNRI treatment. Likewise,
studies are needed to examine whether SNRIs are
effective after a failed SSRI trial and vice versa.
these antidepressants have been systematically
tested in treatment-refractory GAD. Overall the
scant available first-line efficacy evidence supports
imipramine and trazodone.
ANTIHISTAMINES
Two controlled trials, neither of which was in
treatment-refractory cases, support the use of hydroxyzine for GAD. In their RCT comparing hydroxyzine, bromazepam, and placebo (N334),
Llorca et al. (71) found that hydroxyzine was superior to placebo and comparable to the benzodiazepine. Lader et al. (72) studied hydroxyzine, buspirone, and placebo among 244 patients with GAD.
Only hydroxyzine, but not buspirone, was superior
to placebo on the primary outcome measure, the
Hamilton Anxiety Scale, but on secondary measures both hydroxyzine and buspirone were superior to placebo.
ANTICONVULSANTS
Pregabalin is an anticonvulsant approved for
treatment of GAD in Europe but not in the United
States. It is marketed in the United States with indications for various types of chronic pain. Six published double-blind RCTs have established the efficacy of pregabalin for GAD (7378). All of these
trials found pregabalin to be superior to placebo. In
the four studies that also included an active comparative agent, the efficacy of pregabalin was similar
to that of a benzodiazepine (73, 74, 76) and venlafaxine (77). Although most of the trials were
short-term, the one that examined continuation
treatment with pregabalin found it superior to placebo in preventing recurrence of symptoms (78). A
meta-analysis of the six RCTs found that pregabalin was effective for both psychic and somatic anxiety in a dose-dependent relationship that reached a
plateau at 300 mg daily (79).
FOCUS
Fall 2010, Vol. VIII, No. 4
505
LANOUETTE AND STEIN
The data for other anticonvulsants are less robust. There have been no RCTs examining gabapentin, levetiracetam, carbamazepine, or vigabatrin
for GAD. In the one published double-blind RCT
of valproate for GAD (N80, all males), significantly more patients in the valproate group responded compared with the placebo group (80),
but more controlled trials are needed, particularly
given the side effect profile of valproate. Although
one open-label study of tiagabine compared with
paroxetine was promising (81), three parallel-group
double-blind RCTs did not find it superior to placebo (82).
Therefore, pregabalin is currently the only anticonvulsant with sufficient efficacy data to warrant
considering its use for refractory GAD. Notably,
however, none of the investigations of pregabalin
focused specifically on patients with treatment-refractory GAD, so it remains unknown how efficacious pregabalin would be as an adjunct or standalone treatment among patients in whom a firstline treatment has failed.
ANTIPSYCHOTICS
Of the typical antipsychotics, trifluoperazine carries an Food and Drug Administration indication
for short-term treatment of nonpsychotic anxiety
based on a 4-week RCT (N415) that found trifluoperazine (2 6 mg daily) to be superior to placebo for moderate to severe GAD (based on DSMIII criteria) (83). This evidence must be weighed,
however, against the significant risk of tardive dyskinesia with typical antipsychotics, particularly
with longer-term use. In addition, that trial was not
focused on treatment-refractory GAD.
The evidence for atypical antipsychotics is currently primarily limited to augmentation trials.
However, many have been conducted in patients
who have treatment-refractory GAD. Pollack et al.
(84) studied olanzapine compared with placebo
added to fluoxetine among 24 participants in an
RCT who remained symptomatic after 6 weeks of
fluoxetine. Olanzapine augmentation led to significantly more responders, but not remitters, compared with placebo, but the olanzapine group also
gained significantly more weight (84). The data for
risperidone are mixed. One RCT (N40) of risperidone augmentation for persistent GAD symptoms after at least 4 weeks of anxiolytic treatment
showed a significant reduction in symptoms compared with placebo, but response rates were not
statistically significantly different (85). A larger
(N417) RCT of adjunctive risperidone among
patients with GAD who were symptomatic after 8
weeks of anxiolytic treatment found no overall dif-
506
Fall 2010, Vol. VIII, No. 4
FOCUS
ference between risperidone and placebo, but
among those participants with moderate to severe
symptoms, risperidone did outperform placebo in
symptom reduction (86). Although an open-label
study of quetiapine augmentation in 40 patients
with treatment-refractory GAD suggested that it
could be beneficial, an RCT (N70) of adjunctive
quetiapine for patients remaining symptomatic after 10 weeks of paroxetine CR monotherapy failed
to find quetiapine better than placebo (87). However a recent large (N873) RCT testing quetiapine XR monotherapy compared with paroxetine or
placebo found 150 mg daily of quetiapine XR or
paroxetine to be equally efficacious in producing
remission at 8 weeks, with the suggestion that
quetiapine XR might work faster (88). Although
the results are encouraging, it should be noted this
trial was not in patients with treatment-refractory
GAD. Two small open-label trials of aripiprazole
augmentation for treatment-resistant GAD reported a significant reduction in symptoms (51,
89), but these preliminary data require confirmation in larger controlled investigations. Ziprasidone
monotherapy or augmentation was studied in an
RCT of 62 patients with refractory GAD and was
not found to be superior to placebo (90).
OTHER
MEDICATIONS
Riluzole is a glutamate modulator used in the
treatment of patients with amyotrophic lateral sclerosis. One small open-label trial (N18) of riluzole
for GAD found that it significantly reduced anxiety
symptoms and led to a 67% response and 44%
remission rate at 8 weeks (91). Larger controlled
investigations are needed, however, particularly
given the high cost of riluzole.
d-Cycloserine has not yet been studied in human
clinical trials as therapy augmentation for GAD.
Two novel agents, agomelatine (a melatonin agonist and serotonin 5-HT2C antagonist) (92) and
deramciclane (a serotonin 5-HT2A/2C antagonist)
(93) have shown promise for GAD in RCTs in
patients with nontreatment-refractory disorders.
OTHER
PSYCHOTHERAPIES
Although CBT has the smallest average effect size
for GAD compared with the effect sizes for other
anxiety disorders (94), it and applied relaxation
therapy have the largest evidence bases in support of
them compared with other therapies in GAD (95).
Given the smaller effect sizes and the fact that some
patients might prefer other styles of therapy, it is
worth examining the evidence for other therapies.
There have not been any studies of other therapies
THE JOURNAL OF LIFELONG LEARNING IN PSYCHIATRY
LANOUETTE AND STEIN
OTHER
TREATMENTS
ECT has not been tested for refractory GAD. A
preliminary open trial of rTMS, a noninvasive technique, suggests that it could be a beneficial treatment for treatment-resistant GAD (99), but further
controlled trials are needed. There are no published
human trials of DBS in GAD. In the only published case series of capsulotomy for GAD (N13
patients with GAD), Ruck et al. (63) reported significant 1-year and long-term reductions in anxiety, but also noted that seven patients had substantial adverse side effects, most commonly frontal
lobe dysfunction. Therefore, neurosurgical techniques cannot be recommended, even for severe
treatment-refractory GAD.
CASE
VIGNETTE
A 55-year-old male veteran with GAD and major
depressive disorder and a history of alcohol abuse
(in full, sustained remission) has not responded to
40 mg/day of paroxetine (at which dose he is experiencing a lot of sedation) after 8 weeks. You switch
to fluoxetine and gradually increase the dose to 60
mg/day, which he tolerates well, and after 8 weeks
at that dose he joins a CBT group. He reports feeling so anxious that he has difficulty concentrating
in the group and continues to have difficulty sleeping at night. You add trazodone, which helps his
focus.psychiatryonline.org
sleep, but he continues to have significant daytime
anxiety and low energy and motivation. You continue the trazodone, but switch the fluoxetine to
venlafaxine XR 75 mg mg/day and gradually increase the dose to 225 mg/day. After 8 weeks at 225
mg/day, he has had significant improvement in depressive and worry symptoms and finds he is more
able to use the CBT successfully.
POSTTRAUMATIC
STRESS DISORDER
Exposure-based cognitive behavior psychotherapies [including prolonged exposure therapy and
cognitive processing therapy and eye movement desensitization and reprocessing (EMDR)] have a robust evidence base in support of their efficacy for
PTSD, and there is wide consensus that they are
first-line treatments (6, 7). The 2004 APA Practice
Guideline for PTSD recommend SSRIs as first-line
pharmacotherapy. However, since then, a 2007 Institute of Medicine review (100) concluded that
there was insufficient evidence to support the firstline use of SSRIs in PTSD because of the moderate
effect sizes (approximately 0.5) from most RCTs.
In addition, the 2009 APA Guideline Watch for
PTSD (7) concluded there has been a decrease in
the strength of evidence for SSRIs in the treatment
of combat-related PTSD based on mixed results
from recent trials of SSRIs in that specific population. While we await evidence to resolve these questions, given the relatively favorable side effect profile of SSRIs, as well as multiple RCTs (6, 7) and
meta-analyses (101, 102) in support of their use,
SSRIs continue to be a reasonable first-line pharmacotherapy choice for many patients. Another
first-line choice is an SNRI, in particular venlafaxine, for which there are multiple RCTs supporting
its efficacy in PTSD (103, 104).
Few studies have specifically looked at what to do
when one first-line treatment has failed. Simon et
al. (105) tested whether paroxetine CR added onto
prolonged exposure therapy was helpful for participants who remained symptomatic after eight individual prolonged exposure therapy sessions. They
did not find that paroxetine CR was any better than
placebo, but this result could have been due to the
fairly small sample size (N23). A randomized trial
of sertraline alone versus sertraline with culturally
tailored CBT among 10 Cambodian female refugees with PTSD who had not achieved remission
with an antidepressant found the combination
treatment highly efficacious (106), suggesting that
adding CBT to an antidepressant is a reasonable
next step option. Although there is little evidence to
guide next-step treatment choices, as with the other
disorders, a reasonable first step after failure of one
FOCUS
Fall 2010, Vol. VIII, No. 4
CLINICAL
SYNTHESIS
after nonresponse to CBT. One RCT of 57 patients
with GAD supports short-term psychodynamic
psychotherapy (STPP) as being equally effective as
CBT on the primary outcome measure (96); however, for secondary outcome measures including
trait anxiety and worry, CBT was superior. In a
randomized trial (N326) of solution focused
therapy, STPP, and long-term psychodynamic psychotherapy (LTPP) for long-standing (1 year)
depressive or anxiety disorders, STPP was initially
superior to LTPP for anxiety disorders (examined
collectively), but at the 3-year follow-up LTPP
showed better outcomes (97). It should be noted
that there was no CBT or relaxation therapy comparison included, and the anxiety disorders were
not examined individually. An 11-participant open
trial of mindfulness meditation-based cognitive
therapy produced promising results, suggesting
that further study in controlled trials would be
worthwhile (98). Similarly, a treatment called integrative therapy that incorporates CBT and interpersonal emotional processing therapy was effective
in an open study of 18 patients with GAD. Overall,
the existing data most strongly support CBT or
applied relaxation.
507
LANOUETTE AND STEIN
first-line agent is to augment with or switch to another first-line agent.
TRICYCLIC
ANTIDEPRESSANTS
Two 8-week trials support the efficacy of amitriptyline for PTSD. In their RCT of 46 combat veterans, Davidson et al. (107) found that amitriptyline
was superior to placebo but noted low overall remission rates (only 36% of amitriptyline and 28%
of placebo groups were in remission by the end of
the study). A head-to-head randomized comparison of amitriptyline (75 mg/day) and fluoxetine (60
mg/day) in 20 Bosnian combat veterans showed
that both produced a significant reduction in symptoms (70% for amitriptyline and 60% for fluoxetine) (108). Two RCTs of imipramine and
phenelzine found both medications to be superior
to placebo for PTSD (109, 110), although one
noted a small advantage for phenelzine over imipramine (110). In contrast, desipramine was not
found to be efficacious for PTSD, although this
result could be due to the small sample (N18)
and short duration (4 weeks) of the crossover RCT
(111). Notably, none of the tricyclic antidepressant
studies were performed specifically in treatmentresistant populations and most participants were
male combat veterans, limiting the potential generalizability of these findings.
ANTIPSYCHOTICS
The two RCTs of imipramine and phenelzine
described above provide evidence in support of the
efficacy of phenelzine in PTSD (109, 110). Another small (N13) double-blind placebo-controlled crossover study failed to find a difference
between phenelzine and placebo after 4 weeks
(112). Regarding the reversible MAOIs, only openlabel studies suggest the efficacy of moclobemide
for PTSD (113, 114), and the RCTs of brofaromine yielded mixed results (115, 116).
First-generation antipsychotics have not been investigated for PTSD in any published controlled
trials. The evidence for second-generation atypical
antipsychotics is largely limited to augmentation
studies. Risperidone augmentation has been investigated in five controlled trials with mixed results.
Three RCTs found that adjunctive risperidone was
effective particularly for the reexperiencing and hyperarousal symptom clusters in combat veterans
(126, 127) and in women who had experienced
childhood abuse (128). However, the two other
trials did not find risperidone augmentation beneficial for overall PTSD symptoms but did note improvement specifically for sleep (129, 130) and psychosis (130). The only RCT of adjunctive
olanzapine among 19 patients with PTSD with
only minimal response after 12 weeks of SSRI
monotherapy demonstrated significant improvement in PTSD, sleep, and depression symptoms,
but it led to a 13-pound mean weight gain (131).
There have been two RCTs of atypical antipsychotics as monotherapy for PTSD. Risperidone was effective for the primary outcome, an overall measure
of PTSD symptoms but not any secondary outcomes in a trial of 20 women who had experienced
sexual assault or domestic violence (132). In a small
RCT (N15), olanzapine monotherapy was no
better than placebo and caused significantly more
weight gain, but there was a high placebo response
rate (133). There have not been any RCTs of
quetiapine, aripiprazole, or ziprasidone as augmentive or monotherapy for PTSD. Overall, atypical
antipsychotics appear to be a promising but imperfect option for treatment-refractory PTSD.
OTHER
ANTICONVULSANTS
MONOAMINE
OXIDASE INHIBITORS
ANTIDEPRESSANTS
The only RCT of mirtazapine for PTSD found it
effective on some, but not all, measures of symptoms (117). Bupropion is not effective for PTSD as
demonstrated in two RCTs (118, 119), although
the primary focus of one trial was smoking cessation (119). Two RCTs of nefazodone support its
use in PTSD (120, 121), and an open-label study of
19 veterans in whom three previous medication trials had failed (122) suggests that nefazodone may
have a role in treatment-refractory PTSD, although
its widespread clinical use is limited by potential
508
hepatotoxicity. Although widely used as an augmenting agent for insomnia in PTSD (123, 124),
trazodone has only been studied in one very small
(N6) open-label trial (125) and not in any controlled studies.
Fall 2010, Vol. VIII, No. 4
FOCUS
Overall, there have been few studies of anticonvulsants for PTSD, and they have yielded mixed to
negative results. There are three studies with clearly
negative results: one large multicenter RCT found
no difference between tiagabine and placebo for
PTSD (134) and two RCTs in veterans found valproate monotherapy to be ineffective (135, 136). In
contrast, a small RCT (N15) showed promising
results for lamotrigine (137), but no larger follow-up studies have yet been published to confirm
or refute this finding. Topiramate monotherapy
THE JOURNAL OF LIFELONG LEARNING IN PSYCHIATRY
LANOUETTE AND STEIN
ANTIHYPERTENSIVES
Propranolol has been studied for the prevention
of PTSD in two RCTs that involved administering
it shortly after a traumatic event and then following
patients over time, with generally negative results
(140, 143). It has not been studied in chronic or
treatment-refractory PTSD. Neither other
-blockers nor calcium channel blockers have been
studied in controlled PTSD trials.
The -adrenergic antagonist prazosin has received considerable recent study specifically for
PTSD nightmares and sleep disturbance in patients
with chronic, refractory PTSD. Although there was
heterogeneity in the number and types of treatments patients had tried, all of participants had
chronic PTSD and were already taking medications
or were in therapy and could therefore be considered to have treatment-refractory PTSD. Three sequential trials (144 146) examining adjunctive
prazosin in PTSD (added to whatever stable treatment participants were already receiving) found
that it was not only effective for reducing nightmares and increasing sleep time but also helpful in
reducing overall PTSD symptoms. Raskind et al.
conducted a 20-week double-blind crossover study
(N10) (145) and a follow-up larger RCT
(N40) (144) of veterans with chronic PTSD and
found that prazosin was effective for reducing
trauma nightmares and improving sleep quality as
well as overall clinical status. Mean daily doses
(taken at bedtime) in those studies were 9.5 and 13
mg, respectively. Their third study was a randomized placebo-controlled crossover study that examined more specific sleep measures in addition to
PTSD symptoms among 13 mostly female patients
with chronic PTSD from civilian trauma (146).
They found that in addition to reducing PTSD
focus.psychiatryonline.org
symptoms overall, prazosin (mean nightly dose 3
mg) also significantly increased total sleep time,
REM sleep time, and mean REM duration.
BENZODIAZEPINES
Somewhat surprisingly, only two very small
RCTs have looked at benzodiazepines for established PTSD, with generally negative results. Braun
et al. (147) conducted a very small double-blind
crossover trial (N10) and found that alprazolam
was helpful only for nonspecific anxiety and ineffective for core posttraumatic symptoms and noted
that it produced significant rebound anxiety. Another very small (N6) randomized, single-blind
(patient), placebo-controlled crossover trial found
that clonazepam was ineffective for sleep disturbances, particularly nightmares (148). Clearly,
more work is needed to evaluate the utility of benzodiazepines for PTSD, particularly treatment-resistant cases for which benzodiazepine augmentation may be useful.
OTHER
CLINICAL
SYNTHESIS
was found to be effective in an RCT of civilian
PTSD (138). However, augmentive topiramate
was not effective in a trial of chronic PTSD in combat veterans, possibly because of a higher dropout
rate in the topiramate group (139). Gabapentin has
only been studied in one controlled 14-day trial
(N48), which compared it to propranolol and
placebo in prevention of PTSD and found it to be
ineffective in that setting (140). Pregabalin, levetiracetam, carbamazepine, tiagabine, and vigabatrin
have not been tested in controlled trials in PTSD.
Preliminary open studies of augmentive pregabalin
(N9) (141) and augmentive levetiracetam
(N23) (142) in nonresponders or partial responders to antidepressants suggest that these medications are worthy of further study in larger controlled trials of refractory PTSD.
PHARMACOTHERAPY
d-Cycloserine was investigated in one small
(N11 patients with chronic PTSD) doubleblind, placebo-controlled, crossover trial in which
it was found to be generally comparable to placebo
(149). However, this study did not include psychotherapy, so it could not answer the question of
whether d-cycloserine could enhance response to
psychotherapy for patients with PTSD.
OTHER
PSYCHOTHERAPIES
Exposure-based CBTs are first-line psychotherapeutic treatments for PTSD (6, 7). There have not
been any studies testing other therapies for refractory PTSD after CBT has failed; therefore, we cannot answer the most salient question of whether the
following therapies would work specifically in
treatment-refractory PTSD. However, we review
the evidence for them in patients with nontreatment-refractory PTSD, as it could be helpful in
guiding treatment planning after first-line strategies
have failed.
EMDR therapy incorporates exposure-based
therapy with guided eye movements, recall, and
verbalization of traumatic memories. Although
many individual EMDR studies have been small,
meta-analyses support the efficacy of EMDR for
PTSD (150, 151). There have been conflicting results of meta-analyses comparing the efficacy of
EMDR with that of CBT (152, 153). Given that
EMDR includes a type of exposure therapy, the
FOCUS
Fall 2010, Vol. VIII, No. 4
509
LANOUETTE AND STEIN
question of whether the eye movements are an essential feature of EMDR has been raised (154). A
1999 critical review (155) and a 2001 meta-analysis
(152) found that the eye movements were neither
necessary nor sufficient for efficacy of EMDR, but
this finding is still being debated (156).
One controlled trial of psychodynamic psychotherapy (N112) found it comparable to trauma
desensitization and hypnotherapy and concluded
that all three therapies were superior to a wait-list
control (157, 158). A meta-analysis that included
psychodynamic psychotherapy also supports its efficacy for PTSD (158). A more recent randomized
trial of 32 veterans with chronic PTSD comparing
hypnotherapy or zolpidem added to an SSRI and
supportive therapy found hypnotherapy effective in
reducing PTSD symptoms and as effective as zolpidem in number of hours of sleep but superior in
improving sleep quality (159).
OTHER
TREATMENTS
Although ECT has not been studied in controlled trials of PTSD, there have been recent
promising results from studies of rTMS, particularly higher frequency right-sided rTMS. In their
RCT of low-frequency (1 Hz) rTMS, high-frequency (10 Hz) TMS, and sham rTMS for 24 patients with PTSD, Cohen et al. (160) found that 10
daily treatments over 2 weeks of 10-Hz rTMS applied to the right dorsolateral prefrontal cortex
(DLPFC) were superior to both low-frequency and
sham TMS in producing a significant reduction in
PTSD symptoms. In a recent RCT, Boggio et al.
(161) compared 20-Hz rTMS applied to either the
right or left DLPFC with sham rTMS. Similar to
the study of Cohen et al., the treatments were administered in 10 daily sessions over 2 weeks. They
found that both right and left DLPFC rTMS were
effective in reducing PTSD symptoms, but right
rTMS had a greater effect and led to additional
improvements in mood and overall anxiety. These
benefits persisted at the 3-month follow-up. Osuch
et al. (161) examined in a sham-controlled crossover study whether 20 sessions of 1 Hz rTMS therapy delivered over 35 sessions per week could enhance prolonged exposure therapy among nine
patients with chronic, treatment-refractory PTSD
(162). Overall, they did not find a statistically significant difference between the sham and active
treatment, but hyperarousal symptoms were more
improved in the active group.
No neurosurgical techniques have been investigated for PTSD.
In summary, despite many cases of PTSD being
resistant to existing treatments, very little available
510
Fall 2010, Vol. VIII, No. 4
FOCUS
evidence exists to guide treatment decisions. Lacking this evidence, the available literature suggests
that augmentation with atypical antipsychotics
may be beneficial in some patients. Given its preliminary promising results, prazosin should be
more formally studied in treatment-resistant PTSD
algorithms.
CASE
VIGNETTE
A 45-year-old female business executive with
PTSD from a rape in college was unable to tolerate
one SSRI (escitalopram) because of initial activation and increase in anxiety. She has a history of
alcohol abuse in full, sustained remission, so she
asks to avoid any potentially addictive medications.
You start a more sedating SSRI (paroxetine) at
night, which she is better able to tolerate. After 4
weeks of a full dose, she reports improvement but
continues to have poor sleep and nightmares. She
declines CBT because of schedule constraints. You
maximize the dose of the SSRI and add prazosin
initially 1 mg at bedtime for a week. You gradually
increase the prazosin 1 mg every 12 weeks, and
once you reach 4 mg nightly, she reports a significant decrease in nightmares and improvement in
her sleep. She also reports that her daytime concentration and irritability have improved and she feels
less on guard and is better able to tolerate reminders of the rape.
OBSESSIVE-COMPULSIVE
DISORDER
First-line treatment for OCD includes CBT
[specifically exposure and response prevention
(ERP), at least 1320 weekly sessions with daily
homework] and/or an SSRI, typically at high doses
for at least 8 12 weeks (8). Clomipramine is also
highly effective for OCD, but it is generally recommended that an SSRI be tried first, given the more
favorable side effect profile of SSRIs (8).
OCD is the only anxiety disorder for which there
are generally agreed-upon definitions of nonresponse. In OCD trials, nonresponders are typically participants whose Yale-Brown Obsessive
Compulsive Disorder Scale (Y-BOCS) score has
decreased 25% or less from baseline or who have
been rated less than much improved on the Clinical
Global Impressions-Improvement scale (163).
These definitions are not, however, universally
used, and considerable heterogeneity among nonresponders remains, leading experts in the field to
call for more scientifically validated measures of response (163). In addition, many patients called responders remain symptomatic (8, 163).
If one first-line treatment has failed or has been
THE JOURNAL OF LIFELONG LEARNING IN PSYCHIATRY
LANOUETTE AND STEIN
MONOAMINE
OXIDASE INHIBITORS
MAOIs have not been investigated for treatment-refractory OCD in controlled trials. The
only published RCT of an MAOI as initial therapy for OCD generally found that phenelzine
was ineffective and fluoxetine was effective, although the subgroup with symmetry obsessions
did respond to phenelzine (172). The reversible
MAOIs including moclobemide, brofaromine,
and selegiline have not been investigated in controlled trials of OCD.
OTHER
ANTIDEPRESSANTS
The other antidepressants have not been studied
specifically for OCD that has not responded to
first-line treatments. An initial treatment trial of 12
focus.psychiatryonline.org
weeks of open-label mirtazapine followed by 8
weeks of double-blind placebo-controlled discontinuation found it to be effective for OCD (173),
but additional RCTs have not yet been conducted.
A single-blind, randomized, placebo-controlled
trial found that mirtazapine added to citalopram
accelerated treatment response, but responder rates
at the end of the trial were similar in the citalopram
plus placebo and citalopram plus mirtazapine
groups (174). There have not been any RCTs of
nefazodone for OCD. A small open investigation of
bupropion did not find it effective for OCD (175).
The only RCT of trazodone for OCD found that it
was ineffective for OCD (176).
ANTICONVULSANTS
CLINICAL
SYNTHESIS
inadequate, augmenting with or switching to another first-line therapy is recommended. As with
other disorders, augmentation is generally preferable if a patient has had a partial response, whereas
switching to another agent will probably be more
efficacious if there has been no response. Examples
of augmentation strategies include adding CBT to
an SSRI or adding an SSRI to CBT. There is evidence, mostly open trials (164 166), but also two
controlled trials (167, 168), in support of adding
CBT after inadequate response to an SSRI. There
have not been any trials examining whether an
SSRI is effective either as monotherapy or augmenting treatment after nonresponse or a partial
response to CBT. A common reasonable switching
strategy is to cross-titrate from an SSRI that has
been completely ineffective to another SSRI, clomipramine, or an SNRI (8). Surprisingly, few controlled studies specifically addressed the question of
whether a second serotonergic antidepressant is effective after another failed. In one randomized,
double-blind, crossover trial, 150 patients with
OCD were randomly assigned to receive either paroxetine or venlafaxine ER. After 12 weeks, the 43
nonresponders were switched to the other agent for
12 weeks. The authors found that 42% of nonresponders benefited from switching to the other
agent (169). Although venlafaxine ER and paroxetine were both initially comparably effective
(170), in the latter part of the trial, paroxetine was
superior to venlafaxine among nonresponders to
the previous agent (169). Interestingly, a placebocontrolled trial of intravenous clomipramine found
it effective for patients with OCD who had not
responded to oral clomipramine (171), but the
clinical use of intravenous clomipramine is limited
by the need for cardiac monitoring.
There have not been any controlled trials of anticonvulsant monotherapy either for initial treatment or treatment for nonresponders. The one randomized, but open-label study of gabapentin added
onto fluoxetine suggested that it could accelerate
the treatment response but did not lead to better
outcomes at any time point after 2 weeks (177).
ANTIPSYCHOTICS
The vast majority of published RCTs of antipsychotics for OCD have studied adding an antipsychotic after insufficient response to an SSRI. The
overall results have been mixed, with the exception
of risperidone, for which results were generally positive. In an RCT, haloperidol added to fluvoxamine
was effective for treatment-refractory OCD, but
only among those patients with both OCD and tics
(178). Randomized placebo-controlled trials of
olanzapine and quetiapine augmentation have
yielded mixed results. One RCT found that olanzapine augmentation was efficacious (179),
whereas another found no difference compared
with continuing monotherapy with an SSRI (180).
Two RCTs with positive results support quetiapine
augmentation (181, 182), but three RCTs with
negative results did not find it effective (183185).
The two published RCTs comparing augmentive
risperidone with placebo for refractory OCD found
it efficacious (186, 187). A head-to-head, singleblind, randomized study comparing olanzapine to
risperidone augmentation in SSRI nonresponders
found that both medications were effective for
OCD but found limited tolerability for both (due
to amenorrhea with risperidone and weight gain
with olanzapine) (188). Li et al. (189) studied risperidone and haloperidol in a double-blind placebo-controlled crossover trial and found them to be
equally efficacious, but risperidone was superior for
FOCUS
Fall 2010, Vol. VIII, No. 4
511
LANOUETTE AND STEIN
depressive symptoms and was better tolerated overall. Using these data, Bloch et al. (190) conducted a
meta-analysis and concluded that atypical antipsychotics, particularly risperidone, could be useful for
augmentation in treatment-refractory cases of
OCD. They noted that the evidence was too mixed
to conclusively either support or refute using olanzapine and quetiapine (190). Matsunaga et al.
(191) conducted a 1-year study of antipsychotic
augmentation for SSRI nonresponders (191). In
that trial, 90 patients were initially treated with an
SSRI for 12 weeks, followed by the addition of
CBT for 1 year. Patients who had less than 10%
reduction in OCD symptoms after 12 weeks of the
SSRI (N44) were also randomly assigned to receive olanzapine, quetiapine, or risperidone augmentation of the SSRI for 1 year in addition to
CBT. The authors noted that although the SSRI
nonresponders had a significant reduction in OCD
symptoms, their initial and final Y-BOCS scores
were higher than those of the SSRI responders, and
they experienced significant side effects from the
antipsychotic augmentation (191). One promising
open-label investigation of aripiprazole augmentation for treatment-refractory OCD (192) suggests
that it is worthy of further study in larger controlled
trials.
OTHER
MEDICATIONS
Benzodiazepines have received surprisingly little
study for OCD, and there have not been any controlled trials in treatment-refractory cases. Clonazepam has been studied as an initial therapy with
mixed results. Of the monotherapy studies, one
found that it was effective (193), whereas another
did not (194), and the one augmentation study
found no difference with placebo (195). Although
one small RCT (N18) found that buspirone
monotherapy was comparable to clomipramine for
treatment-naive patients (196), when studied as an
adjunctive agent for refractory OCD, its efficacy
was not supported by the results of controlled trials
(197199). An open-label investigation of riluzole
with positive results suggests that it could be worthy
of further study (200). Lithium was not found to be
an effective adjuvant treatment for refractory OCD
in two small controlled trials (201, 202). One of
those small studies also failed to find that triiodothyronine added onto clomipramine was helpful
for clomipramine nonresponders (202). A small
(N23) randomized, placebo-controlled crossover
study found that adding once-weekly morphine
(30 45 mg) to SSRIs outperformed placebo
among participants in whom two to six previous
SSRI trials had failed (203), but further investiga-
512
Fall 2010, Vol. VIII, No. 4
FOCUS
tions are needed. Likewise, promising results of a
single-blind case-control study of 44 patients with
severe treatment-refractory OCD suggests that memantine is worthy of further study (204).
Two small double-blind placebo-controlled
studies, one in chronic OCD (205), of single-dose
dextroamphetamine (30 mg) found that it produced a significantly greater reduction in symptoms compared with placebo (205, 206). A more
recent 5-week double-blind study (N24) of dextroamphetamine (30 mg/day) or caffeine (300 mg/
day) added to an SSRI/SNRI after nonresponse
(207) found that both agents produced significant
decreases in OCD symptoms.
Two randomized, double-blind, placebo-controlled trials of d-cycloserine added to CBT found
that it enhanced response to CBT, particularly in
the initial phases of treatment (208, 209). Neither
of these studies was conducted specifically with a
medication-resistant population, so it is still not
clear whether d-cycloserine would be beneficial in
treatment-refractory OCD.
ANTIHYPERTENSIVES
Pindolol augmentation was found to be effective
in one small RCT in treatment-refractory OCD
(210), but it did not show benefit in augmenting
the initial response to fluvoxamine in another small
RCT in treatment-naive patients (211). The sole
randomized double-blind study of clonidine in patients with nontreatment-refractory OCD found
that it was ineffective (193).
ANTIHISTAMINES
The same study that found clonidine ineffective
for OCD also found that diphenhydramine produced a significant reduction in symptoms, although it was intended to be a nonactive comparator (193). However, this study was not in patients
with treatment-refractory OCD, and there have
not been any other studies of it. There have been no
investigations of hydroxyzine in OCD.
PSYCHOTHERAPY AND OTHER PSYCHOSOCIAL
TREATMENTS
CBT for OCD can focus primarily on behavioral
techniques as in ERP therapy or primarily on cognitive techniques. ERP in a variety of different settings (individual, group, therapist guided, and patient-controlled) has been the most extensively
studied and consistently has demonstrated efficacy
for OCD, leading to its being a first-line treatment
for OCD (8). No controlled trials studying other
THE JOURNAL OF LIFELONG LEARNING IN PSYCHIATRY
LANOUETTE AND STEIN
therapies after a failed trial of ERP have been conducted.
Although there have not been controlled trials,
large open studies of both partial hospitalization
(212, 213) and intensive residential treatment
(214 218), including long-term follow-up after
discharge (212, 217), suggest these are worthy of
consideration for severe treatment-refractory
OCD.
TREATMENTS
Various ablative neurosurgical techniques, including anterior capsulotomy, gamma-knife radiosurgery, and cingulotomy, have been tried for severe treatment-refractory OCD, but only in case
reports and uncontrolled studies (219 224).
Therefore, it is difficult to interpret the reported
response rates of up to 50%. In addition, the potential adverse effects, including psychosis, seizures,
personality change, hydrocephalus, and executive
dysfunction, indicate that ablative neurosurgery
should be reserved for only patients with severe
OCD for whom multiple first- and second-line
agents have failed (8). More recently, the less-invasive technique of DBS (in which electrodes connected to a stimulator are neurosurgically placed
into the ventral anterior limb of the internal capsule
and ventral striatum) has shown promise in two
small studies. A small (N4) study of DBS that
included a blinded on/off phase showed significant
benefit during the blinded treatment in one participant and moderate benefit for another during open
follow-up (225). More recently, Goodman et al.
(226) conducted a sham stimulation-controlled
study of six patients with severe treatment-refractory OCD and found that DBS led to a significant
response in four participants after 12 months of
stimulation.
The only evidence in support of ECT in treatment-refractory OCD is a case series of 32 patients
(227). Therefore, although the case series reported
generally positive results, given the risks of anesthesia and memory loss, there is insufficient evidence
to support the use of ECT for OCD, although it
may have utility when there are co-occurring conditions for which ECT is indicated, such as depression (8).
Recently rTMS, a noninvasive technique, has
been investigated for a variety of psychiatric disorders including OCD. The early sham-controlled
studies of rTMS for OCD used a low frequency (1
Hz) over the left dorsolateral prefrontal cortex
(228, 229) or right prefrontal cortex (230); none
showed benefit for OCD symptoms. With use of
those three studies, a recent meta-analysis (231)
focus.psychiatryonline.org
CASE
CLINICAL
SYNTHESIS
OTHER
concluded that rTMS was ineffective for OCD.
Consistent with those studies, a more recent shamcontrolled trial of 10 sessions of high-frequency (10
Hz) rTMS over the right prefrontal cortex failed to
find benefit for OCD symptoms but did note significant decreases in depression and overall anxiety
symptoms (232). In contrast, two recent sham-controlled studies of low-frequency (1 Hz) rTMS to
different brain regions, including the orbital frontal
cortex (233) and bilateral supplementary motor
area (234), showed significant benefit for OCD
symptoms in patients with medication-resistant
OCD, suggesting that larger trials of rTMS on
these brain regions are warranted.
In summary, there have been more studies done
for treatment-refractory OCD than for any other
anxiety disorder. Although further investigations
are needed, particularly for patients in whom multiple first- and second-line treatments have failed,
there was sufficient evidence for the authors of the
OCD APA Practice Guideline to outline a treatment algorithm (8).
VIGNETTE
A 33-year-old unemployed man with severe
OCD who you see through a public mental health
clinic had no appreciable improvement in symptoms after 10 weeks of citalopram 60 mg/day. You
switch to another SSRI (fluoxetine) and titrate up
to his maximally tolerated dose (80 mg/day). After
8 weeks, he reports a decrease in the intensity of
obsessions and a slight decrease in time spent on
compulsions but continues to have significant distress. CBT for OCD is not available in your community. You add low-dose risperidone augmentation (initially 0.5 mg at bedtime and then increase
to 1 mg at bedtime after 1 week) and continue the
high-dose SSRI. After another 4 weeks, he has had
a significant reduction in symptoms but not
enough that he has improved functionally (i.e., he
still spends many hours per day performing compulsions). You increase the risperidone to 1 mg
b.i.d., and within 2 weeks he notices that it is easier
to distract himself from his obsessions and the time
spent on compulsions has reduced enough that he
is able to start searching for work.
SOCIAL
PHOBIA
First-line therapy for social anxiety disorder, also
called social phobia, includes SSRIs, the SNRI venlafaxine ER, and/or CBT (9, 235). Phenelzine is
also effective for social anxiety disorder but given
the more favorable side effect profile of SSRIs or
venlafaxine ER, it is recommended that phenelzine
FOCUS
Fall 2010, Vol. VIII, No. 4
513
LANOUETTE AND STEIN
be tried second-line (9). Clonazepam also has demonstrated efficacy for social phobia, but only for
short-term treatment; therefore, it is typically best
used as an addition to an SSRI or SNRI, either
when starting the SSRI/SNRI to give initial symptom relief or in treatment-refractory cases (9).
As with the other anxiety disorders, if one firstline treatment has failed or been inadequate, augmenting with or switching to another first-line
therapy is the recommended next step. If a patient
has had a partial response, augmentation is typically
recommended, whereas switching to another firstline agent will probably be more efficacious if there
has been no response. Examples of augmentation
strategies include adding CBT and/or clonazepam
to an SSRI or adding an SSRI to CBT. Although
there is little specific data to guide switching after
SSRI nonresponse, most experts recommend
switching from a failed SSRI to another SSRI, venlafaxine ER, or phenelzine (9).
There are no studies on augmenting CBT with
medication or vice versa after monotherapy with either has failed. However, studies on combining medication and therapy for initial treatment of social anxiety disorder have been conducted with mixed results.
Recently Blanco et al. (236) reported the results of
their RCT (N128) comparing phenelzine, cognitive behavior group therapy (CBGT), or their combination for initial treatment of social anxiety disorder.
They found that combination treatment was most efficacious; in addition, phenelzine was superior to placebo but CBGT was not. In contrast, an RCT
(N295) of fluoxetine, CBGT, or their combination
found that all treatments were superior to placebo by
the end of the study, with no advantage for combination therapy (237). Therefore, although there is no
specific evidence to guide second-step treatment
choices after failure of one first-line agent, given the
strong evidence base for SSRIs, venlafaxine, phenelzine, and CBT, switching to another of these agents or
combining medication and CBT would be a reasonable next step. Extremely limited evidence exists on
what to do for social anxiety disorder after two firstline treatments have failed. Therefore, in the following
we review available evidence for other treatments,
most of which is from nontreatment-refractory cases.
MONOAMINE OXIDASE INHIBITORS AND
TRICYCLIC ANTIDEPRESSANTS
As described above, four RCTs support of the
efficacy of phenelzine as an initial treatment for
social anxiety disorder and, therefore, it should be
considered in patients for whom a first-line treatment has failed (9). Multiple double-blind trials
demonstrate the efficacy of the reversible MAOIs
514
Fall 2010, Vol. VIII, No. 4
FOCUS
including moclobemide (238 242) and brofaromine (243245) in nontreatment-refractory social
anxiety disorder, although brofaromine is not currently available for use, and moclobemide is not
currently approved for use in the United States. A
small 6-week open-label study of low-dose oral selegiline (10 mg/d) suggested that it had modest efficacy for social phobia (246).
There are no controlled trials of TCAs for social
anxiety disorder.
OTHER
ANTIDEPRESSANTS
The data in support of mirtazapine are limited to
one open trial with positive results (247) and one
RCT with positive results among 66 women with
social anxiety disorder (248); neither study was in
patients with treatment-resistant disorders. The
one RCT (N105) of nefazodone found that it
was ineffective for social phobia. Bupropion and
trazodone have not been studied in controlled trials
of social anxiety disorder.
BENZODIAZEPINES
Clonazepam is the only benzodiazepine that has
been studied in controlled trials for the treatment of
social anxiety disorder. Clonazepam monotherapy
has been shown to be more efficacious than placebo
(249 251), including use for long-term treatment
(249), and with efficacy comparable to that of CBT
(252). One RCT of 28 patients with social anxiety
disorder found clonazepam added to paroxetine to
be more efficacious than paroxetine alone on some,
but not all, outcome measures, although the authors noted that this result could be attributable to
inadequate power (253). Although none of these
investigations were in patients with treatment-refractory disorders, the first-line efficacy of clonazepam and the different mechanisms of action of
benzodiazepines and SSRIs/SNRIs suggest there
may be a role for adding clonazepam to an SSRI or
SNRI after a partial response.
ANTICONVULSANTS
None of the investigations of anticonvulsants
have focused on patients with treatment-refractory
social anxiety disorder. The most promising data
for anticonvulsants in patients with nontreatmentrefractory disorders are RCTs in support of gabapentin (N69) (254) and high-dose (600 mg/day)
but not low-dose (150 mg/day) pregabalin
(N135) (255). Although levetiracetam initially
appeared promising in an open-label study (256), it
was subsequently found to be ineffective for social
THE JOURNAL OF LIFELONG LEARNING IN PSYCHIATRY
FOCUS
Fall 2010, Vol. VIII, No. 4
Quetiapine (a)
Risperidone (m)
Olanzapine (a)
Olanzapine (m)
Tiagabine
Trifluoperazine (m)
Olanzapine (a)
Risperidone (a)
First line
Propranolol
Carbamazepine
Risperidone (m)
Monotherapy
Pindolol (a)
No data
d-Cycloserine
No data
No data
Antipsychotics
Buspirone
Adrenergic agents
Antihistamines
Other medications
rTMS
DBS
No data
Atenolol (m)
d-Cycloserine (a)
Oxytocin (a)
Morphine (a)
Lithium (a)
No data
No data
rTMS
Dextroamphetamine
Triiodothyronine (a)
Atomoxetine
d-Cycloserine (a)
No data
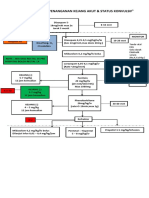
, RCT with positive results; , RCT with negative results; , RCT with mixed results (e.g., benefit for one subgroup only). The number of the above symbols next to a particular treatment indicates the total number of RCTs
that have been published testing that treatment for that disorder. First-line: the treatment has enough evidence that it is considered a first-line option. No data: there have been no published RCTs of this treatment. Insufficient
data: the RCTs of this treatment were too small to draw conclusions. Bold entries indicate that the study was in patients with treatment-refractory disorders. (a), treatment was studied as an augmentation strategy; (m), treatment was studied as a monotherapy strategy.
Note that this table summarizes the data only from published randomized, controlled trials of treatments that are available in the United States. Please see the text for details of these studies as well as for a summary of openlabel trials and studies of treatments not currently available in the United States.
No data
uncontrolled study only
d-Cycloserine (m)
Diphenhydramine
No data
Hydroxyzine
Pindolol (a)
Augmentation
Pindolol (a)
Monotherapy
Augmentation
Quetiapine (m)
Olanzapine (m)
Levetiracetam
Pregabalin
Gabapentin
Clonazepam first line
Nefazodone
Mirtazapine
Phenelzine first line
No data
Social Phobia
Monotherapy
Risperidone (a)
Haloperidol (a)
No data
Clonidine
Prazosin (for nightmares/sleep)
Insufficient data
Topiramate (a)
Topiramate (m)
Lamotrigine
Valproate
Clonidine
Ziprasidone (m, a)
Quetiapine XR (m)
Quetiapine (a)
Olanzapine (a)
Risperidone (a)
Valproate
Tiagabine
Pregabalin
Clonazepam (a)
Gabapentin
Clonazepam (m)
Trazodone
Tiagabine
Insufficient data
Nefazodone
Bupropion
Mirtazapine (a)
Phenelzine
Anticonvulsants
Bupropion XL
Trazodone
Mirtazapine
Phenelzine
First-line
Trazodone
Mirtazapine
Other antidepressants
Desipramine
Clomipramine first line
OCD
First-line
No data
Phenelzine
MAOIs
Imipramine
Amitriptyline
PTSD
CLINICAL
SYNTHESIS
focus.psychiatryonline.org
Benzodiazepines
Imipramine
GAD
Imipramine and clomipramine first line
Panic Disorder
RCTs of non-first-line treatments tested for anxiety disorders
Tricyclic antidepressants
Treatment
Table 1.
LANOUETTE AND STEIN
515
LANOUETTE AND STEIN
anxiety disorder in two RCTs (257), one of which
was large (N217) (258). Open trials of tiagabine
(259), topiramate (260), and valproic acid (261) as
initial monotherapy for social anxiety disorder suggest that they are worthy of further study in controlled trials.
ANTIPSYCHOTICS
In the one investigation of antipsychotic augmentation for refractory social anxiety disorder, Simon et al. (49) studied open-label risperidone augmentation (N7 participants with social anxiety
disorder) of an SSRI or benzodiazepine that patients had not fully responded to after 8 previous
weeks of treatment. Although the results were
promising, further study in large, controlled trials is
needed before this can be a recommended treatment. A small RCT (N12) found that olanzapine
monotherapy was superior to placebo in a population with nontreatment-refractory disorders (262).
Whereas an open-label study (263) suggested a role
for quetiapine monotherapy in social anxiety disorder, subsequent RCTs of monotherapy for generalized social anxiety (264) and of single-dose quetiapine before a public speaking virtual exposure (265)
did not find benefit. Given the generally high side
effect burden of these agents, further study is
needed before they become part of standard treatment options for treatment-resistant social anxiety
disorder.
OTHER
PHARMACOTHERAPY
Diphenhydramine and hydroxyzine have not
been investigated for social anxiety disorder.
The two randomized, placebo-controlled trials of
d-cycloserine in social anxiety disorder found that it
was efficacious in enhancing response to CBT (exposure therapy) (279, 280). Although these studies
were not in patients with treatment-resistant disorders, they suggest that d-cycloserine is worthy of
consideration for enhancing an exposure therapy
trial in this population. The hormone, oxytocin,
was also studied in an RCT (N25) as a potential
enhancer of exposure therapy for social anxiety disorder but was found to be ineffective (281).
OTHER
PSYCHOTHERAPIES
Although buspirone appeared to have some efficacy in open studies as monotherapy (266) and as
an SSRI augmentation (267), two RCTs failed to
find any benefit over placebo (268, 269) or any
augmentive effect with CBT (268, 269) for social
phobia. Riluzole has not been investigated in social
anxiety disorder. One open-label trial with positive
results in patients previously treated with antidepressants suggests that reboxetine (270) should be
investigated in larger RCTs for refractory social
phobia. A small RCT (N27) of atomoxetine
found that it was not effective for social anxiety
disorder (271).
CBT, particularly exposure therapy but also cognitive therapy, has been shown to be effective for
social phobia and is a first-line treatment (9). There
have not been any controlled investigations of other
therapies in patients in whom CBT has yielded a
partial or nonresponse. Other psychotherapies,
however, have shown utility for social anxiety in
controlled trials and may be worthy of consideration if CBT has not been effective or if it is unavailable. Two recent controlled trials of a computerized attention training found it highly effective
for social anxiety disorder (282, 283), although another controlled study did not find that attention
training enhanced CBGT (284). One trial (N58)
found that psychodynamic group therapy and clonazepam were more effective than clonazepam alone
for social anxiety disorder (285). Mindfulnessbased stress reduction was found to be less effective
than CBGT for generalized social anxiety disorder
in a head-to-head randomized trial (286).
ANTIHYPERTENSIVES
OTHER
Although -blockers may be useful for specific
performance or test anxiety (272275), they appear
to be ineffective for generalized social anxiety disorder, including treatment-refractory cases. Pindolol augmentation of paroxetine was not found to be
superior to placebo in a small (N14) double-
There are no reported trials or case series of ECT,
rTMS, or DBS for social anxiety disorder. In their
case series (N26) of capsulotomy that included
five patients with social phobia, Ruck et al. (63)
reported significant 1-year and long-term reductions in anxiety, but also noted that seven patients
OTHER
516
blind, placebo-controlled crossover study among
patients who had not responded to 10 previous
weeks of paroxetine monotherapy (276). Atenolol
was shown to be ineffective as initial monotherapy
for social anxiety disorder in two randomized, controlled trials (276 278). The -adrenergic antagonists have not been investigated for the treatment of
social phobia.
Fall 2010, Vol. VIII, No. 4
MEDICATIONS
FOCUS
TREATMENTS
THE JOURNAL OF LIFELONG LEARNING IN PSYCHIATRY
LANOUETTE AND STEIN
had substantial adverse side effects, most commonly frontal lobe dysfunction. Given this extremely limited evidence base and the substantial
side effects, capsulotomy cannot be recommended
even for the most treatment-refractory social phobia.
CASE
VIGNETTE
SUMMARY
A paucity of data addresses the management of
patients with treatment-resistant anxiety disorders.
For most anxiety disorders, with the exception of
OCD, there are no consistent definitions of treatment resistance in the literature, making it difficult
to judge and compare the data that do exist across
studies. These severe limitations notwithstanding,
there is beginning to emerge both within and across
disorders a literature on approaches to patients with
treatment-resistant disorders. At the present time,
the data cannot be considered compelling for any
anxiety treatment-resistant indication, but clinicians are nonetheless frequently faced with anxiety
treatment resistance, and so we present the following suggested approach based on what little published evidence is available, buttressed and expanded upon by our own clinical experience and by
other published treatment recommendation guidelines (59).
As described in the Introduction, this approach
should be used only after thorough diagnostic assessment, evaluation of adequacy of prior treat-
focus.psychiatryonline.org
CLINICAL
SYNTHESIS
A 29-year-old male graduate student with generalized social phobia has not responded to 12 weeks
of sertraline 150 mg/day (his maximally tolerated
dose). You switch to escitalopram, which, after 8
weeks at 30 mg/day, yields only slight improvement in his self-consciousness and no change in his
avoidance. You add CBT, which he finds very helpful, but he continues to have great difficulty in any
group meetings, which he needs to attend for his
program. You continue CBT, but, after a 2-week
washout period and careful explanation of dietary
and medication restrictions, switch the SRRI to
phenelzine and gradually increase the dose to 60
mg/day. He gradually improves to the point of being able to more effectively use the skills learned in
CBT when attending the group meetings. After
practicing a public speaking exposure exercise in
CBT, he is able to successfully present his work
during a talk at a national meeting. His ability to
interact with colleagues in less formal situations
also improves, and he is able to make contacts for a
future fellowship job.
ment, and, ideally, consultation with colleagues experienced in treatment of refractory anxiety
disorders. When faced with a patient with an anxiety disorder who remains symptomatic after an
adequate trial of a first-line treatment, we recommend either switching to (in the case of nonresponse) or augmenting with (in the case of partialresponse) another first-line treatment. If that is
ineffective, we recommend successive complete trials of first-line agents (if any remain untried) or
second-line agents (with augmentation if clinically
indicated). In general, a complete medication trial
would be 8 12 weeks at the highest tolerable dose.
If a medication is effective, there are scant data to
guide length of maintenance treatment; using good
clinical judgment, taking into account patient preference and a risk/benefit assessment on a case-bybase basis, is advised. Although there is some variation by disorder, an adequate trial of CBT would
typically consist of at least 1220 sessions with the
patient doing daily homework. If all first-line and
second-line treatments have been exhausted or are
clinically inappropriate, Table 1 presents the evidence for and against possible next-step strategies.
Although large gaps remain in our knowledge of
how best to manage treatment-refractory anxiety
disorders, recent advances offer promise.
REFERENCES
1. Kessler RC, Wang PS, Kessler RC, Wang PS: The descriptive epidemiology of commonly occurring mental disorders in the United States.
Annu Rev Public Health 2008; 29:115129
2. Saarni SI, Suvisaari J, Sintonen H, Pirkola S, Koskinen S, Aromaa A,
Lonnqvist J: Impact of psychiatric disorders on health-related quality of
life: general population survey. Br J Psychiatry 2007; 190:326 332.
3. Ravindran LN, Stein MB: Anxiety disorders: somatic treatment, in Kaplan
and Sadock Comprehensive Textbook of Psychiatry. Edited by Sadock
BJ, Sadock VA. Philadelphia, Lippincott Williams & Wilkins, 2009, pp
1906 1914.
4. Furmark T, Carlbring P, Hedman E, Sonnenstein A, Clevberger P,
Bohman B, Eriksson A, Hllen A, Frykman M, Holmstrom A, Sparthan E,
Tillfors M, Ihrfelt EN, Spak M, Eriksson A, Ekselius L, Andersson G:
Guided and unguided self-help for social anxiety disorder: randomised
controlled trial. Br J Psychiatry 2009; 195:440 447
5. Stein MB, Goin MK, Pollack MH, Roy-Byrne P, Sareen J, Simon NM:
Practice Guideline for the Treatment of Patients with Panic Disorder.
Alexandria, Va., American Psychiatric Association, 2009
6. Ursano RJ, Bell C, Eth S, Friedman M, Norwood A, Pfefferbaum B,
Pynoos RS, Zatzick DF, Benedek DM: Practice Guidelines for the Treatment of Patients with Acute Stress Disorder and Posttraumatic Stress
Disorder. Alexandria, Va., American Psychiatric Association, 2004
7. Benedek DM, Friedman MJ, Zatazick D, Ursano RJ: Guideline Watch:
Practice Guideline for the Treatment of Patients with Acute Stress
Disorder and Posttraumatic Stress Disorder. Alexandria, Va., American
Psychiatric Association, 2009
8. Koran LM, Hanna GL, Hollander E, Nestadt G, Simpson HB: Practice
Guideline for the Treatment of Patients with Obsessive-Compulsive
Disorder. Arlington, Va., American Psychiatric Association, 2007
9. Bandelow B, Zohar J, Hollander E, Kasper S, Moller HJ, WFSBP Task
Force on Treatment Guidelines for Anxiety, Obsessive-Compulsive and
Post-Traumatic Stress Disoders, Zohar J, Hollander E, Kasper S, Moller
HJ, Bandelow B, Allgulander C, Ayuso-Gutierrez J, Baldwin DS, Buenvicius R, Cassano G, Fineberg N, Gabriels L, Hindmarch I, Kaiya H, Klein
DF, Lader M, Lecrubier Y, Lepine JP, Liebowitz MR, Lopez-Ibor JJ,
Marazziti D, Miguel EC, Oh KS, Preter M, Rupprecht R, Sato M, Starcevic
V, Stein DJ, van Ameringen M, Vega J: World Federation of Societies of
FOCUS
Fall 2010, Vol. VIII, No. 4
517
LANOUETTE AND STEIN
10.
11.
12.
13.
14.
15.
16.
17.
18.
19.
20.
21.
22.
23.
24.
25.
26.
27.
28.
29.
30.
31.
32.
518
Fall 2010, Vol. VIII, No. 4
Biological Psychiatry (WFSBP) guidelines for the pharmacological treatment of anxiety, obsessive-compulsive and post-traumatic stress disordersfirst revision. World J Biol Psychiatry 2008; 9:248 312
Simon NM, Otto MW, Worthington JJ, Hoge EA, Thompson EH, Lebeau
RT, Moshier SJ, Zalta AK, Pollack MH. Next-step strategies for panic
disorder refractory to initial pharmacotherapy: a 3-phase randomized
clinical trial. J Clin Psychiatry 2009; 70:15631570
Pollack MH, Otto MW, Kaspi SP, Hammerness PG, Rosenbaum JF:
Cognitive behavior therapy for treatment-refractory panic disorder.
J Clin Psychiatry 1994; 55:200 205
Heldt E, Gus Manfro G, Kipper L, Blaya C, Isolan L, Otto MW: One-year
follow-up of pharmacotherapy-resistant patients with panic disorder
treated with cognitive-behavior therapy: outcome and predictors of
remission. Behav Res Ther 2006; 44:657 665
van Apeldoorn FJ, Timmerman ME, Mersch PP, van Hout WJ, Visser S,
van Dyck R, den Boer JA: A randomized trial of cognitive-behavioral
therapy or selective serotonin reuptake inhibitor or both combined for
panic disorder with or without agoraphobia: treatment results through
1-year follow-up. J Clin Psychiatry 2010; 71:574 586
Furukawa TA, Watanabe N, Churchill R: Psychotherapy plus antidepressant for panic disorder with or without agoraphobia: systematic review.
Br J Psychiatry 2006; 188:305312.
Watanabe N, Churchill R, Furukawa TA: Combined psychotherapy plus
benzodiazepines for panic disorder. Cochrane Database Syst Rev 2009;
CD005335
Buigues J, Vallejo J: Therapeutic response to phenelzine in patients with
panic disorder and agoraphobia with panic attacks. J Clin Psychiatry
1987; 48:5559
Sheehan DV, Ballenger J, Jacobsen G: Treatment of endogenous anxiety
with phobic, hysterical, and hypochondriacal symptoms. Arch Gen
Psychiatry 1980; 37:5159
Mountjoy CQ, Roth M, Garside RF, Leitch IM: A clinical trial of phenelzine
in anxiety depressive and phobic neuroses. Br J Psychiatry 1977;
131:486 492.
Tiller JW, Bouwer C, Behnke K: Moclobemide and fluoxetine for panic
disorder. International Panic Disorder Study Group. Eur Arch Psychiatry
Clin Neurosci 1999; 249(suppl 1):S7S10.
Kruger MB, Dahl AA: The efficacy and safety of moclobemide compared
to clomipramine in the treatment of panic disorder. Eur Arch Psychiatry
Clin Neurosci 1999; 249(Suppl 1):S19 S24
Ross DC, Klein DF, Uhlenhuth EH: Improved statistical analysis of
moclobemide dose effects on panic disorder treatment. Eur Arch Psychiatry Clin Neurosci 2010; 260:243248
Loerch B, Graf-Morgenstern M, Hautzinger M, Schlegel S, Hain C,
Sandmann J, Benkert O: Randomised placebo-controlled trial of moclobemide, cognitive-behavioural therapy and their combination in panic
disorder with agoraphobia. Br J Psychiatry 1999; 174:205212.
van Vliet IM, Westenberg HG, Den Boer JA: MAO inhibitors in panic
disorder: clinical effects of treatment with brofaromine. A double blind
placebo controlled study. Psychopharmacology (Berl) 1993; 112:483
489
van Vliet IM, den Boer JA, Westenberg HG, Slaap BR: A double-blind
comparative study of brofaromine and fluvoxamine in outpatients with
panic disorder. J Clin Psychopharmacol 1996; 16:299 306
Bakish D, Saxena BM, Bowen R, DSouza J: Reversible monoamine
oxidasea inhibitors in panic disorder. Clin Neuropharmacol 1993;
16(suppl 2):S77S82.
Carpenter LL, Leon Z, Yasmin S, Price LH: Clinical experience with
mirtazapine in the treatment of panic disorder. Ann Clin Psychiatry
1999; 11:81 86
Boshuisen ML, Slaap BR, Vester-Blokland ED, den Boer JA: The effect
of mirtazapine in panic disorder: an open label pilot study with a
single-blind placebo run-in period. Int Clin Psychopharmacol 2001;
16:363368
Sarchiapone M, Amore M, De Risio S, Carli V, Faia V, Poterzio F, Balista
C, Camardese G, Ferrari G: Mirtazapine in the treatment of panic
disorder: an open-label trial. Int Clin Psychopharmacol 2003; 18:3538
Ribeiro L, Busnello JV, Kauer-SantAnna M, Madruga M, Quevedo J,
Busnello EA, Kapczinski F: Mirtazapine versus fluoxetine in the treatment of panic disorder. Braz J Med Biol Res 2001; 34:13031307
DeMartinis NA, Schweizer E, Rickels K: An open-label trial of nefazodone in high comorbidity panic disorder. J Clin Psychiatry 1996;
57:245248
Bystritsky A, Rosen R, Suri R, Vapnik T: Pilot open-label study of
nefazodone in panic disorder. Depress Anxiety 1999; 10:137139
Papp LA, Coplan JD, Martinez JM, de Jesus M, Gorman JM: Efficacy of
open-label nefazodone treatment in patients with panic disorder. J Clin
Psychopharmacol 2000; 20:544 546
FOCUS
33. Mavissakalian M, Perel J, Bowler K, Dealy R: Trazodone in the treatment
of panic disorder and agoraphobia with panic attacks. Am J Psychiatry
1987; 144:785787
34. Spinhoven P, Onstein E, Klinkhaer R, Knoppert-van der Klein E: Panic
management, trazodone, and a combination of both in the treatment of
panic disorder. Clin Psychol Psychother 1999; 3:86 92
35. Charney DS, Woods SW, Goodman WK, Rifkin B, Kinch M, Aiken B,
Quadrino LM, Heninger GR: Drug treatment of panic disorder: the
comparative efficacy of imipramine, alprazolam, and trazodone. J Clin
Psychiatry 1986; 47:580 586
36. Simon NM, Emmanuel N, Ballenger J, Worthington JJ, Kinrys G, Korbly
NB, Farach FJ, Pollack MH: Bupropion sustained release for panic
disorder. Psychopharmacol Bull 2003; 37:66 72
37. Sheehan DV, Davidson J, Manschreck T, Van Wyck Fleet J: Lack of
efficacy of a new antidepressant (bupropion) in the treatment of panic
disorder with phobias. J Clin Psychopharmacol 1983; 3:28 31
38. Pande AC, Pollack MH, Crockatt J, Greiner M, Chouinard G, Lydiard RB,
Taylor CB, Dager SR, Shiovitz T: Placebo-controlled study of gabapentin
treatment of panic disorder. J Clin Psychopharmacol 2000; 20:467 471
39. Woodman CL, Noyes R Jr: Panic disorder: treatment with valproate.
J Clin Psychiatry 1994; 55:134 136
40. Zwanzger P, Baghai TC, Schule C, Minov C, Padberg F, Moller HJ,
Rupprecht R: Tiagabine improves panic and agoraphobia in panic
disorder patients. J Clin Psychiatry 2001; 62:656 657
41. Schwartz TL: The use of tiagabine augmentation for treatment-resistant
anxiety disorders: a case series. Psychopharmacol Bull 2002; 36:5357
42. Sheehan DV, Sheehan KH, Raj BA, Janavs J: An open-label study of
tiagabine in panic disorder. Psychopharmacol Bull 2007; 40:32 40
43. Zwanzger P, Eser D, Nothdurfter C, Baghai TC, Moller HJ, Padberg F,
Rupprecht R: Effects of the GABA-reuptake inhibitor tiagabine on panic
and anxiety in patients with panic disorder. Pharmacopsychiatry 2009;
42:266 269
44. Uhde TW, Stein MB, Post RM: Lack of efficacy of carbamazepine in the
treatment of panic disorder. Am J Psychiatry 1988; 145:1104 1109
45. Zwanzger P, Baghai T, Boerner RJ, Moller HJ, Rupprecht R: Anxiolytic
effects of vigabatrin in panic disorder. J Clin Psychopharmacol 2001;
21:539 540
46. Papp LA: Safety and efficacy of levetiracetam for patients with panic
disorder: results of an open-label, fixed-flexible dose study. J Clin
Psychiatry 2006; 67:15731576
47. Hollifield M, Thompson PM, Ruiz JE, Uhlenhuth EH: Potential effectiveness and safety of olanzapine in refractory panic disorder. Depress
Anxiety 2005; 21:33 40
48. Sepede G, De Berardis D, Gambi F, Campanella D, La Rovere R, DAmico
M, Cicconetti A, Penna L, Peca S, Carano A, Mancini E, Salerno RM,
Ferro FM: Rovere R, DAmico M, Cicconetti A, Penna L, Peca S, Carano
A, Mancini E, Salerno RM, Ferro FM: Olanzapine augmentation in
treatment-resistant panic disorder: a 12-week, fixed-dose, open-label
trial. J Clin Psychopharmacol 2006; 26:45 49
49. Simon NM, Hoge EA, Fischmann D, Worthington JJ, Christian KM, Kinrys
G, Pollack MH: An open-label trial of risperidone augmentation for
refractory anxiety disorders. J Clin Psychiatry 2006; 67:381385
50. Prosser JM, Yard S, Steele A, Cohen LJ, Galynker II: A comparison of
low-dose risperidone to paroxetine in the treatment of panic attacks: a
randomized, single-blind study. BMC Psychiatry 2009; 9:25
51. Hoge EA, Worthington JJ, 3rd, Kaufman RE, Delong HR, Pollack MH,
Simon NM: Aripiprazole as augmentation treatment of refractory generalized anxiety disorder and panic disorder. CNS Spectr 2008; 13:522
527
52. Crane DL: Ziprasidone as an augmenting agent in the treatment of
anxiety-spectrum disorders. CNS Spectr 2005; 10:176 179
53. Sheehan DV, Raj AB, Sheehan KH, Soto S: Is buspirone effective for
panic disorder? J Clin Psychopharmacol 1990; 10:311
54. Sheehan DV, Raj AB, Harnett-Sheehan K, Soto S, Knapp E: The relative
efficacy of high-dose buspirone and alprazolam in the treatment of
panic disorder: a double-blind placebo-controlled study. Acta Psychiatr
Scand 1993; 88:111
55. Pohl R, Balon R, Yeragani VK, Gershon S: Serotonergic anxiolytics in the
treatment of panic disorder: a controlled study with buspirone. Psychopathology 1989; 22(suppl 1):60 67.
56. Schweizer E, Rickels K: Buspirone in the treatment of panic disorder: a
controlled pilot comparison with clorazepate. J Clin Psychopharmacol
1988; 8:303.
57. Cottraux J, Note ID, Cungi C, Legeron P, Heim F, Chneiweiss L, Bernard
G, Bouvard M: A controlled study of cognitive behaviour therapy with
buspirone or placebo in panic disorder with agoraphobia. Br J Psychiatry
1995; 167:635 641
58. Davis M, Ressler K, Rothbaum BO, Richardson R: Effects of D-cy-
THE JOURNAL OF LIFELONG LEARNING IN PSYCHIATRY
LANOUETTE AND STEIN
59.
60.
61.
62.
64.
65.
66.
67.
68.
69.
70.
71.
72.
73.
74.
75.
76.
77.
78.
79.
focus.psychiatryonline.org
80. Aliyev NA, Aliyev ZN: Valproate (depakine-chrono) in the acute treatment
of outpatients with generalized anxiety disorder without psychiatric
comorbidity: randomized, double-blind placebo-controlled study. Eur
Psychiatry 2008; 23:109 114
81. Rosenthal M: Tiagabine for the treatment of generalized anxiety
disorder: a randomized, open-label, clinical trial with paroxetine as a
positive control. J Clin Psychiatry 2003; 64:12451249
82. Pollack MH, Tiller J, Xie F, Trivedi MH: Tiagabine in adult patients with
generalized anxiety disorder: results from 3 randomized, double-blind,
placebo-controlled, parallel-group studies. J Clin Psychopharmacol
2008; 28:308 316
83. Mendels J, Krajewski TF, Huffer V, Taylor RJ, Secunda S, Schless A,
Sebastian JA, Semchyshyn G, Durr MJ, Melmed AS: Effective short-term
treatment of generalized anxiety disorder with trifluoperazine. J Clin
Psychiatry 1986; 47:170 174
84. Pollack MH, Simon NM, Zalta AK, Worthington JJ, Hoge EA, Mick E,
Kinrys G, Oppenheimer J: Olanzapine augmentation of fluoxetine for
refractory generalized anxiety disorder: a placebo controlled study. Biol
Psychiatry 2006; 59:211215
85. Brawman-Mintzer O, Knapp RG, Nietert PJ: Adjunctive risperidone in
generalized anxiety disorder: a double-blind, placebo-controlled study.
J Clin Psychiatry 2005; 66:13211325
86. Pandina GJ, Canuso CM, Turkoz I, Kujawa M, Mahmoud RA: Adjunctive
risperidone in the treatment of generalized anxiety disorder: a doubleblind, prospective, placebo-controlled, randomized trial. Psychopharmacol Bull 2007; 40:4157
87. Simon NM, Connor KM, LeBeau RT, Hoge EA, Worthington JJ 3rd, Zhang
W, Davidson JR, Pollack MH: Quetiapine augmentation of paroxetine CR
for the treatment of refractory generalized anxiety disorder: preliminary
findings. Psychopharmacology (Berl) 2008; 197:675 681
88. Bandelow B, Chouinard G, Bobes J, Ahokas A, Eggens I, Liu S, Eriksson
H: Extended-release quetiapine fumarate (quetiapine XR): a once-daily
monotherapy effective in generalized anxiety disorder. Data from a
randomized, double-blind, placebo- and active-controlled study. Int
J Neuropsychopharmacol 2010; 13:305320
89. Menza MA, Dobkin RD, Marin H: An open-label trial of aripiprazole
augmentation for treatment-resistant generalized anxiety disorder.
J Clin Psychopharmacol 2007; 27:207210
90. Lohoff FW, Etemad B, Mandos LA, Gallop R, Rickels K: Ziprasidone
treatment of refractory generalized anxiety disorder: a placebo-controlled, double-blind study. J Clin Psychopharmacol 2010; 30:185189
91. Mathew SJ, Amiel JM, Coplan JD, Fitterling HA, Sackeim HA, Gorman
JM: Open-label trial of riluzole in generalized anxiety disorder. Am J
Psychiatry 2005; 162:2379 2381
92. Stein DJ, Ahokas AA, de Bodinat C: Efficacy of agomelatine in generalized anxiety disorder: a randomized, double-blind, placebo-controlled
study. J Clin Psychopharmacol 2008; 28:561566
93. Naukkarinen H, Raassina R, Penttinen J, Ahokas A, Jokinen R, Koponen
H, Lepola U, Kanerva H, Lehtonen L, Pohjalainen T, Partanen A, MakiIkola O, Rouru J, Deramciclane Dose-Finding Study Group: Deramciclane in the treatment of generalized anxiety disorder: a placebo-controlled,
double-blind, dose-finding study. Eur Neuropsychopharmacol 2005; 15:
617 623
94. Hofmann SG, Smits JA: Cognitive-behavioral therapy for adult anxiety
disorders: a meta-analysis of randomized placebo-controlled trials.
J Clin Psychiatry 2008; 69:621 632
95. Fisher PL, Durham RC: Recovery rates in generalized anxiety disorder
following psychological therapy: an analysis of clinically significant
change in the STAI-T across outcome studies since 1990. Psychol Med
1999; 29:14251434
96. Leichsenring F, Salzer S, Jaeger U, Kachele H, Kreische R, Leweke F,
Ruger U, Winkelbach C, Leibing E: Short-term psychodynamic psychotherapy and cognitive-behavioral therapy in generalized anxiety
disorder: a randomized, controlled trial. Am J Psychiatry 2009; 166:
875 881
97. Knekt P, Lindfors O, Harkanen T, Valikoski M, Virtala E, Laaksonen MA,
Marttunen M, Kaipainen M, Renlund C, Helsinki Psychotherapy Study
Group: Randomized trial on the effectiveness of long-and short-term
psychodynamic psychotherapy and solution-focused therapy on psychiatric symptoms during a 3-year follow-up. Psychol Med 2008; 38:689
703
98. Evans S, Ferrando S, Findler M, Stowell C, Smart C, Haglin D: Mindfulness-based cognitive therapy for generalized anxiety disorder. J
Anxiety Disord 2008; 22:716 721
99. Bystritsky A, Kaplan JT, Feusner JD, Kerwin LE, Wadekar M, Burock M,
Wu AD, Iacoboni M: A preliminary study of fMRI-guided rTMS in the
treatment of generalized anxiety disorder. J Clin Psychiatry 2008;
69:10921098
FOCUS
Fall 2010, Vol. VIII, No. 4
CLINICAL
SYNTHESIS
63.
closerine on extinction: translation from preclinical to clinical work. Biol
Psychiatry 2006; 60:369 375
Otto MW, Tolin DF, Simon NM, Pearlson GD, Basden S, Meunier SA,
Hofmann SG, Eisenmenger K, Krystal JH, Pollack MH: Efficacy of
D-cycloserine for enhancing response to cognitive-behavior therapy for
panic disorder. Biol Psychiatry 2010; 67:365370
Hirschmann S, Dannon PN, Iancu I, Dolberg OT, Zohar J, Grunhaus L:
Pindolol augmentation in patients with treatment-resistant panic
disorder: a double-blind, placebo-controlled trial. J Clin Psychopharmacol 2000; 20:556 559
Milrod B, Leon AC, Busch F, Rudden M, Schwalberg M, Clarkin J,
Aronson A, Singer M, Turchin W, Klass ET, Graf E, Teres JJ, Shear MK:
A randomized controlled clinical trial of psychoanalytic psychotherapy
for panic disorder. Am J Psychiatry 2007; 164:265272
Shear MK, Houck P, Greeno C, Masters S: Emotion-focused psychotherapy for patients with panic disorder. Am J Psychiatry 2001; 158:
19931998
Ruck C, Andreewitch S, Flyckt K, Edman G, Nyman H, Meyerson BA,
Lippitz BE, Hindmarsh T, Svanborg P, Mindus P, Asberg M: Capsulotomy
for refractory anxiety disorders: long-term follow-up of 26 patients.
Am J Psychiatry 2003; 160:513521
Davidson JR: First-line pharmacotherapy approaches for generalized
anxiety disorder. J Clin Psychiatry 2009; 70(suppl 2):2531.
Schneier FR, Belzer KD, Kishon R, Amsel L, Simpson HB: Escitalopram
for persistent symptoms of generalized anxiety disorder after CBT: a
pilot study. J Nerv Ment Dis 2010; 198:458 461
Rickels K, Downing R, Schweizer E, Hassman H: Antidepressants for the
treatment of generalized anxiety disorder. A placebo-controlled comparison of imipramine, trazodone, and diazepam. Arch Gen Psychiatry
1993; 50:884 895
Gambi F, De Berardis D, Campanella D, Carano A, Sepede G, Salini G,
Mezzano D, Cicconetti A, Penna L, Salerno RM, Ferro FM: Mirtazapine
treatment of generalized anxiety disorder: a fixed dose, open label
study. J Psychopharmacol 2005; 19:483 487
Hedges DW, Reimherr FW, Strong RE, Halls CH, Rust C: An open trial of
nefazodone in adult patients with generalized anxiety disorder. Psychopharmacol Bull 1996; 32:671 676
Peet M, Ali S: Propranolol and atenolol in the treatment of anxiety. Int
Clin Psychopharmacol 1986; 1:314 319
Hoehn-Saric R, Merchant AF, Keyser ML, Smith VK: Effects of clonidine
on anxiety disorders. Arch Gen Psychiatry 1981; 38:1278 1282
Llorca PM, Spadone C, Sol O, Danniau A, Bougerol T, Corruble E, Faruch
M, Macher JP, Sermet E, Servant D: Efficacy and safety of hydroxyzine
in the treatment of generalized anxiety disorder: a 3-month double-blind
study. J Clin Psychiatry 2002; 63:1020 1027
Lader M, Scotto JC: A multicentre double-blind comparison of hydroxyzine, buspirone and placebo in patients with generalized anxiety
disorder. Psychopharmacology (Berl) 1998; 139:402 406
Feltner DE, Crockatt JG, Dubovsky SJ, Cohn CK, Shrivastava RK, Targum
SD, Liu-Dumaw M, Carter CM, Pande AC: A randomized, double-blind,
placebo-controlled, fixed-dose, multicenter study of pregabalin in patients with generalized anxiety disorder. J Clin Psychopharmacol 2003;
23:240 249
Pande AC, Crockatt JG, Feltner DE, Janney CA, Smith WT, Weisler R,
Londborg PD, Bielski RJ, Zimbroff DL, Davidson JR, Liu-Dumaw M:
Pregabalin in generalized anxiety disorder: a placebo-controlled trial.
Am J Psychiatry 2003; 160:533540
Pohl RB, Feltner DE, Fieve RR, Pande AC: Efficacy of pregabalin in the
treatment of generalized anxiety disorder: double-blind, placebo-controlled comparison of BID versus TID dosing. J Clin Psychopharmacol
2005; 25:151158
Rickels K, Pollack MH, Feltner DE, Lydiard RB, Zimbroff DL, Bielski RJ,
Tobias K, Brock JD, Zornberg GL, Pande AC: Pregabalin for treatment of
generalized anxiety disorder: a 4-week, multicenter, double-blind, placebo-controlled trial of pregabalin and alprazolam. Arch Gen Psychiatry
2005; 62:10221030
Montgomery SA, Tobias K, Zornberg GL, Kasper S, Pande AC: Efficacy
and safety of pregabalin in the treatment of generalized anxiety
disorder: a 6-week, multicenter, randomized, double-blind, placebocontrolled comparison of pregabalin and venlafaxine. J Clin Psychiatry
2006; 67:771782
Feltner D, Wittchen HU, Kavoussi R, Brock J, Baldinetti F, Pande AC:
Long-term efficacy of pregabalin in generalized anxiety disorder. Int Clin
Psychopharmacol 2008; 23:18 28
Lydiard RB, Rickels K, Herman B, Feltner DE: Comparative efficacy of
pregabalin and benzodiazepines in treating the psychic and somatic
symptoms of generalized anxiety disorder. Int J Neuropsychopharmacol
2010; 13:229 241
519
LANOUETTE AND STEIN
100. Treatment of PTSD: An Assessment of the Evidence. Washington, DC,
Institute of Medicine, National Academies Press, 2007
101. Stein DJ, Seedat S, van der Linden GJ, Zungu-Dirwayi N: Selective
serotonin reuptake inhibitors in the treatment of post-traumatic stress
disorder: a meta-analysis of randomized controlled trials. Int Clin Psychopharmacol 2000; 15(suppl 2):S31S39.
102. Stein DJ, Ipser JC, Seedat S: Pharmacotherapy for post traumatic stress
disorder (PTSD). Cochrane Database Syst Rev 2006; CD002795;
103. Davidson J, Baldwin D, Stein DJ, Kuper E, Benattia I, Ahmed S,
Pedersen R, Musgnung J: Treatment of posttraumatic stress disorder
with venlafaxine extended release: a 6-month randomized controlled
trial. Arch Gen Psychiatry 2006; 63:1158 1165
104. Davidson J, Rothbaum BO, Tucker P, Asnis G, Benattia I, Musgnung JJ:
Venlafaxine extended release in posttraumatic stress disorder: a sertraline- and placebo-controlled study. J Clin Psychopharmacol 2006;
26:259 267
105. Simon NM, Connor KM, Lang AJ, Rauch S, Krulewicz S, LeBeau RT,
Davidson JR, Stein MB, Otto MW, Foa EB, Pollack MH: Paroxetine CR
augmentation for posttraumatic stress disorder refractory to prolonged
exposure therapy. J Clin Psychiatry 2008; 69:400 405
106. Otto MW, Hinton D, Korbly NB, Chea A, Ba P, Gershuny BS, Pollack MH:
Treatment of pharmacotherapy-refractory posttraumatic stress disorder
among Cambodian refugees: a pilot study of combination treatment with
cognitive-behavior therapy vs sertraline alone. Behav Res Ther 2003;
41:12711276
107. Davidson J, Kudler H, Smith R, Mahorney SL, Lipper S, Hammett E,
Saunders WB, Cavenar JO Jr: Treatment of posttraumatic stress disorder with amitriptyline and placebo. Arch Gen Psychiatry 1990; 47:259
266
108. Cavaljuga S, Licanin I, Mulabegovic N, Potkonjak D: Therapeutic effects
of two antidepressant agents in the treatment of posttraumatic stress
disorder (PTSD). Bosn J Basic Med Sci 2003; 3:1216
109. Frank JB, Kosten TR, Giller EL Jr, Dan E: A randomized clinical trial of
phenelzine and imipramine for posttraumatic stress disorder. Am J
Psychiatry 1988; 145:1289 1291
110. Kosten TR, Frank JB, Dan E, McDougle CJ, Giller EL Jr: Pharmacotherapy for posttraumatic stress disorder using phenelzine or imipramine.
J Nerv Ment Dis 1991; 179:366 370
111. Reist C, Kauffmann CD, Haier RJ, Sangdahl C, DeMet EM, Chicz-DeMet
A, Nelson JN: A controlled trial of desipramine in 18 men with posttraumatic stress disorder. Am J Psychiatry 1989; 146:513516
112. Shestatzky M, Greenberg D, Lerer B: A controlled trial of phenelzine in
posttraumatic stress disorder. Psychiatry Res 1988; 24:149 155
113. Neal LA, Shapland W, Fox C: An open trial of moclobemide in the
treatment of post-traumatic stress disorder. Int Clin Psychopharmacol
1997; 12:231237
114. Onder E, Tural U, Aker T: A comparative study of fluoxetine, moclobemide, and tianeptine in the treatment of posttraumatic stress disorder
following an earthquake. Eur Psychiatry 2006; 21:174 179
115. Baker DG, Diamond BI, Gillette G, Hamner M, Katzelnick D, Keller T,
Mellman TA, Pontius E, Rosenthal M, Tucker P. A double-blind, randomized, placebo-controlled, multi-center study of brofaromine in the
treatment of post-traumatic stress disorder. Psychopharmacology (Berl)
1995; 122:386 389
116. Katz RJ, Lott MH, Arbus P, Crocq L, Herlobsen P, Lingjaerde O, Lopez G,
Loughrey GC, MacFarlane DJ, McIvor R: Pharmacotherapy of posttraumatic stress disorder with a novel psychotropic. Anxiety 1994;
1:169 174
117. Davidson JR, Weisler RH, Butterfield MI, Casat CD, Connor KM, Barnett
S, van Meter S: Mirtazapine vs. placebo in posttraumatic stress
disorder: a pilot trial. Biol Psychiatry 2003; 53:188 191
118. Becker ME, Hertzberg MA, Moore SD, Dennis MF, Bukenya DS, Beckham JC: A placebo-controlled trial of bupropion SR in the treatment of
chronic posttraumatic stress disorder. J Clin Psychopharmacol 2007;
27:193197
119. Hertzberg MA, Moore SD, Feldman ME, Beckham JC: A preliminary
study of bupropion sustained-release for smoking cessation in patients
with chronic posttraumatic stress disorder. J Clin Psychopharmacol
2001; 21:94 98
120. Davis LL, Jewell ME, Ambrose S, Farley J, English B, Bartolucci A, Petty
F: A placebo-controlled study of nefazodone for the treatment of chronic
posttraumatic stress disorder: a preliminary study. J Clin Psychopharmacol 2004; 24:291297
121. McRae AL, Brady KT, Mellman TA, Sonne SC, Killeen TK, Timmerman
MA, Bayles-Dazet W: Comparison of nefazodone and sertraline for the
treatment of posttraumatic stress disorder. Depress Anxiety 2004;
19:190 196
122. Zisook S, Chentsova-Dutton YE, Smith-Vaniz A, Kline NA, Ellenor GL,
520
Fall 2010, Vol. VIII, No. 4
FOCUS
123.
124.
125.
126.
127.
128.
129.
130.
131.
132.
133.
134.
135.
136.
137.
138.
139.
140.
141.
142.
143.
144.
Kodsi AB, Gillin JC: Nefazodone in patients with treatment-refractory
posttraumatic stress disorder. J Clin Psychiatry 2000; 61:203208
Mellman TA, Clark RE, Peacock WJ: Prescribing patterns for patients
with posttraumatic stress disorder. Psychiatr Serv 2003; 54:1618 1621
Rosen CS, Chow HC, Finney JF, Greenbaum MA, Moos RH, Sheikh JI,
Yesavage JA: VA practice patterns and practice guidelines for treating
posttraumatic stress disorder. J Trauma Stress 2004; 17:213222
Hertzberg MA, Feldman ME, Beckham JC, Davidson JR: Trial of trazodone for posttraumatic stress disorder using a multiple baseline group
design. J Clin Psychopharmacol 1996; 16:294 298
Bartzokis G, Lu PH, Turner J, Mintz J, Saunders CS: Adjunctive risperidone in the treatment of chronic combat-related posttraumatic stress
disorder. Biol Psychiatry 2005; 57:474 479
Monnelly EP, Ciraulo DA, Knapp C, Keane T: Low-dose risperidone as
adjunctive therapy for irritable aggression in posttraumatic stress disorder. J Clin Psychopharmacol 2003; 23:193196
Reich DB, Winternitz S, Hennen J, Watts T, Stanculescu C: A preliminary
study of risperidone in the treatment of posttraumatic stress disorder
related to childhood abuse in women. J Clin Psychiatry 2004; 65:1601
1606
Rothbaum BO, Killeen TK, Davidson JR, Brady KT, Connor KM, Heekin
MH: Placebo-controlled trial of risperidone augmentation for selective
serotonin reuptake inhibitor-resistant civilian posttraumatic stress disorder. J Clin Psychiatry 2008; 69:520 525
Hamner MB, Faldowski RA, Ulmer HG, Frueh BC, Huber MG, Arana GW:
Adjunctive risperidone treatment in post-traumatic stress disorder: a
preliminary controlled trial of effects on comorbid psychotic symptoms.
Int Clin Psychopharmacol 2003; 18:1 8
Stein MB, Kline NA, Matloff JL: Adjunctive olanzapine for SSRI-resistant
combat-related PTSD: a double-blind, placebo-controlled study. Am J
Psychiatry 2002; 159:17771779
Padala PR, Madison J, Monnahan M, Marcil W, Price P, Ramaswamy S,
Din AU, Wilson DR, Petty F: Risperidone monotherapy for post-traumatic
stress disorder related to sexual assault and domestic abuse in women.
Int Clin Psychopharmacol 2006; 21:275280
Butterfield MI, Becker ME, Connor KM, Sutherland S, Churchill LE,
Davidson JR: Olanzapine in the treatment of post-traumatic stress
disorder: a pilot study. Int Clin Psychopharmacol 2001; 16:197203
Davidson JR, Brady K, Mellman TA, Stein MB, Pollack MH: The efficacy
and tolerability of tiagabine in adult patients with post-traumatic stress
disorder. J Clin Psychopharmacol 2007; 27:85 88
Davis LL, Davidson JR, Ward LC, Bartolucci A, Bowden CL, Petty F:
Divalproex in the treatment of posttraumatic stress disorder: a randomized, double-blind, placebo-controlled trial in a veteran population.
J Clin Psychopharmacol 2008; 28:84 88
Hamner MB, Faldowski RA, Robert S, Ulmer HG, Horner MD, Lorberbaum JP: A preliminary controlled trial of divalproex in posttraumatic
stress disorder. Ann Clin Psychiatry 2009; 21:89 94
Hertzberg MA, Butterfield MI, Feldman ME, Beckham JC, Sutherland
SM, Connor KM, Davidson JR: A preliminary study of lamotrigine for the
treatment of posttraumatic stress disorder. Biol Psychiatry 1999; 45:
1226 1229
Tucker P, Trautman RP, Wyatt DB, Thompson J, Wu SC, Capece JA,
Rosenthal NR: Efficacy and safety of topiramate monotherapy in civilian
posttraumatic stress disorder: a randomized, double-blind, placebocontrolled study. J Clin Psychiatry 2007; 68:201206
Lindley SE, Carlson EB, Hill K: A randomized, double-blind, placebocontrolled trial of augmentation topiramate for chronic combat-related
posttraumatic stress disorder. J Clin Psychopharmacol 2007; 27:677
681
Stein MB, Kerridge C, Dimsdale JE, Hoyt DB: Pharmacotherapy to
prevent PTSD: Results from a randomized controlled proof-of-concept
trial in physically injured patients. J Trauma Stress 2007; 20:923932
Pae CU, Marks DM, Han C, Masand PS, Patkar AA: Pregabalin augmentation of antidepressants in patients with accident-related posttraumatic
stress disorder: an open label pilot study. Int Clin Psychopharmacol
2009; 24:29 33
Kinrys G, Wygant LE, Pardo TB, Melo M: Levetiracetam for treatmentrefractory posttraumatic stress disorder. J Clin Psychiatry 2006; 67:
211214
Pitman RK, Sanders KM, Zusman RM, Healy AR, Cheema F, Lasko NB,
Cahill L, Orr SP: Pilot study of secondary prevention of posttraumatic
stress disorder with propranolol. Biol Psychiatry 2002; 51:189 192
Raskind MA, Peskind ER, Hoff DJ, Hart KL, Holmes HA, Warren D, Shofer
J, OConnell J, Taylor F, Gross C, Rohde K, McFall ME: A parallel group
placebo controlled study of prazosin for trauma nightmares and sleep
disturbance in combat veterans with post-traumatic stress disorder. Biol
Psychiatry 2007; 61:928 934
THE JOURNAL OF LIFELONG LEARNING IN PSYCHIATRY
LANOUETTE AND STEIN
focus.psychiatryonline.org
168.
169.
170.
171.
172.
173.
174.
175.
176.
177.
178.
179.
180.
181.
182.
183.
184.
185.
186.
187.
188.
for augmenting pharmacotherapy in obsessive-compulsive disorder.
Am J Psychiatry 2008; 165:621 630
Tenneij NH, van Megen HJ, Denys DA, Westenberg HG: Behavior therapy
augments response of patients with obsessive-compulsive disorder
responding to drug treatment. J Clin Psychiatry 2005; 66:1169 1175
Denys D, de Geus F, van Megen HJ, Westenberg HG: A double-blind,
randomized, placebo-controlled trial of quetiapine addition in patients
with obsessive-compulsive disorder refractory to serotonin reuptake
inhibitors. J Clin Psychiatry 2004; 65:1040 1048
Denys D, van der Wee N, van Megen HJ, Westenberg HG: A double blind
comparison of venlafaxine and paroxetine in obsessive-compulsive
disorder. J Clin Psychopharmacol 2003; 23:568 575
Fallon BA, Liebowitz MR, Campeas R, Schneier FR, Marshall R, Davies
S, Goetz D, Klein DF: Intravenous clomipramine for obsessive-compulsive disorder refractory to oral clomipramine: a placebo-controlled
study. Arch Gen Psychiatry 1998; 55:918 924
Jenike MA, Baer L, Minichiello WE, Rauch SL, Buttolph ML: Placebocontrolled trial of fluoxetine and phenelzine for obsessive-compulsive
disorder. Am J Psychiatry 1997; 154:12611264
Koran LM, Gamel NN, Choung HW, Smith EH, Aboujaoude EN: Mirtazapine for obsessive-compulsive disorder: an open trial followed by
double-blind discontinuation. J Clin Psychiatry 2005; 66:515520
Pallanti S, Quercioli L, Bruscoli M: Response acceleration with mirtazapine augmentation of citalopram in obsessive-compulsive disorder patients without comorbid depression: a pilot study. J Clin Psychiatry
2004; 65:1394 1399
Vulink NC, Denys D, Westenberg HG: Bupropion for patients with
obsessive-compulsive disorder: an open-label, fixed-dose study. J Clin
Psychiatry 2005; 66:228 230
Pigott TA, LHeureux F, Rubenstein CS, Bernstein SE, Hill JL, Murphy DL:
A double-blind, placebo controlled study of trazodone in patients with
obsessive-compulsive disorder. J Clin Psychopharmacol 1992; 12:156
162
Onder E, Tural U, Gokbakan M: Does gabapentin lead to early symptom
improvement in obsessive-compulsive disorder? Eur Arch Psychiatry
Clin Neurosci 2008; 258:319 323
McDougle CJ, Goodman WK, Leckman JF, Lee NC, Heninger GR, Price
LH: Haloperidol addition in fluvoxamine-refractory obsessive-compulsive disorder. A double-blind, placebo-controlled study in patients with
and without tics. Arch Gen Psychiatry 1994; 51:302308
Bystritsky A, Ackerman DL, Rosen RM, Vapnik T, Gorbis E, Maidment
KM, Saxena S: Augmentation of serotonin reuptake inhibitors in refractory obsessive-compulsive disorder using adjunctive olanzapine: a placebo-controlled trial. J Clin Psychiatry 2004; 65:565568
Shapira NA, Ward HE, Mandoki M, Murphy TK, Yang MC, Blier P,
Goodman WK: A double-blind, placebo-controlled trial of olanzapine
addition in fluoxetine-refractory obsessive-compulsive disorder. Biol
Psychiatry 2004; 55:553555
Denys D, van Megen HJ, van der Wee N, Westenberg HG: A double-blind
switch study of paroxetine and venlafaxine in obsessive-compulsive
disorder. J Clin Psychiatry 2004; 65:37 43
Atmaca M, Kuloglu M, Tezcan E, Gecici O: Quetiapine augmentation in
patients with treatment resistant obsessive-compulsive disorder: a single-blind, placebo-controlled study. Int Clin Psychopharmacol 2002;
17:115119
Carey PD, Vythilingum B, Seedat S, Muller JE, van Ameringen M, Stein
DJ: Quetiapine augmentation of SRIs in treatment refractory obsessivecompulsive disorder: a double-blind, randomised, placebo-controlled
study [ISRCTN83050762]. BMC Psychiatry 2005; 5:5
Fineberg NA, Sivakumaran T, Roberts A, Gale T: Adding quetiapine to
SRI in treatment-resistant obsessive-compulsive disorder: a randomized
controlled treatment study. Int Clin Psychopharmacol 2005; 20:223226
Kordon A, Wahl K, Koch N, Zurowski B, Anlauf M, Vielhaber K, Kahl KG,
Broocks A, Voderholzer U, Hohagen F: Quetiapine addition to serotonin
reuptake inhibitors in patients with severe obsessive-compulsive
disorder: a double-blind, randomized, placebo-controlled study. J Clin
Psychopharmacol 2008; 28:550 554
Hollander E, Baldini Rossi N, Sood E, Pallanti S: Risperidone augmentation in treatment-resistant obsessive-compulsive disorder: a doubleblind, placebo-controlled study. Int J Neuropsychopharmacol 2003;
6:397 401
McDougle CJ, Epperson CN, Pelton GH, Wasylink S, Price LH: A doubleblind, placebo-controlled study of risperidone addition in serotonin
reuptake inhibitor-refractory obsessive-compulsive disorder. Arch Gen
Psychiatry 2000; 57:794 801
Maina G, Pessina E, Albert U, Bogetto F: 8-week, single-blind, randomized trial comparing risperidone versus olanzapine augmentation of
FOCUS
Fall 2010, Vol. VIII, No. 4
CLINICAL
SYNTHESIS
145. Raskind MA, Peskind ER, Kanter ED, Petrie EC, Radant A, Thompson CE,
Dobie DJ, Hoff D, Rein RJ, Straits-Troster K, Thomas RG, McFall MM:
Reduction of nightmares and other PTSD symptoms in combat veterans
by prazosin: a placebo-controlled study. Am J Psychiatry 2003; 160:
371373
146. Taylor FB, Martin P, Thompson C, Williams J, Mellman TA, Gross C,
Peskind ER, Raskind MA: Prazosin effects on objective sleep measures
and clinical symptoms in civilian trauma posttraumatic stress disorder:
a placebo-controlled study. Biol Psychiatry 2008; 63:629 632
147. Braun P, Greenberg D, Dasberg H, Lerer B: Core symptoms of posttraumatic stress disorder unimproved by alprazolam treatment. J Clin
Psychiatry 1990; 51:236 238
148. Cates ME, Bishop MH, Davis LL, Lowe JS, Woolley TW: Clonazepam for
treatment of sleep disturbances associated with combat-related posttraumatic stress disorder. Ann Pharmacother 2004; 38:13951399
149. Heresco-Levy U, Kremer I, Javitt DC, Goichman R, Reshef A, Blanaru M,
Cohen T: Pilot-controlled trial of D-cycloserine for the treatment of
post-traumatic stress disorder. Int J Neuropsychopharmacol 2002;
5:301307
150. Bisson JI, Ehlers A, Matthews R, Pilling S, Richards D, Turner S:
Psychological treatments for chronic post-traumatic stress disorder.
Systematic review and meta-analysis. Br J Psychiatry 2007; 190:97
104.
151. Shepherd J, Stein K, Milne R: Eye movement desensitization and
reprocessing in the treatment of post-traumatic stress disorder: a
review of an emerging therapy. Psychol Med 2000; 30:863 871
152. Davidson PR, Parker KC: Eye movement desensitization and reprocessing (EMDR): a meta-analysis. J Consult Clin Psychol 2001; 69:305316
153. Seidler GH, Wagner FE: Comparing the efficacy of EMDR and traumafocused cognitive-behavioral therapy in the treatment of PTSD: a metaanalytic study. Psychol Med 2006; 36:15151522
154. Herbert JD, Lilienfeld SO, Lohr JM, Montgomery RW, ODonohue WT,
Rosen GM, Tolin DF: Science and pseudoscience in the development of
eye movement desensitization and reprocessing: implications for clinical
psychology. Clin Psychol Rev 2000; 20:945971
155. Cahill SP, Carrigan MH, Frueh BC: Does EMDR work? And if so, why?:
a critical review of controlled outcome and dismantling research. J
Anxiety Disord 1999; 13:533.
156. Lipke H: Comment on Hembree and Foa (2003) and EMDR: J Trauma
Stress 2003; 16:573574; discussion 575577
157. Brom D, Kleber RJ, Defares PB: Brief psychotherapy for posttraumatic
stress disorders. J Consult Clin Psychol 1989; 57:607 612
158. Sherman JJ: Effects of psychotherapeutic treatments for PTSD: a
meta-analysis of controlled clinical trials. J Trauma Stress 1998; 11:
413 435
159. Abramowitz EG, Barak Y, Ben-Avi I, Knobler HY: Hypnotherapy in the
treatment of chronic combat-related PTSD patients suffering from
insomnia: a randomized, zolpidem-controlled clinical trial. Int J Clin Exp
Hypn 2008; 56:270 280
160. Cohen H, Kaplan Z, Kotler M, Kouperman I, Moisa R, Grisaru N:
Repetitive transcranial magnetic stimulation of the right dorsolateral
prefrontal cortex in posttraumatic stress disorder: a double-blind, placebo-controlled study. Am J Psychiatry 2004; 161:515524
161. Boggio PS, Rocha M, Oliveira MO, Fecteau S, Cohen RB, Campanha C,
Ferreira-Santos E, Meleiro A, Corchs F, Zaghi S, Pascual-Leone A,
Fregni F. Noninvasive brain stimulation with high-frequency and lowintensity repetitive transcranial magnetic stimulation treatment for posttraumatic stress disorder. J Clin Psychiatry 2010; 71:992999
162. Osuch EA, Benson BE, Luckenbaugh DA, Geraci M, Post RM, McCann U:
Repetitive TMS combined with exposure therapy for PTSD: a preliminary
study. J Anxiety Disord 2009; 23:54 59
163. Pallanti S, Quercioli L: Treatment-refractory obsessive-compulsive
disorder: methodological issues, operational definitions and therapeutic
lines. Prog Neuropsychopharmacol Biol Psychiatry 2006; 30:400 412
164. Kampman M, Keijsers GP, Hoogduin CA, Verbraak MJ: Addition of
cognitive-behaviour therapy for obsessive-compulsive disorder patients
non-responding to fluoxetine. Acta Psychiatr Scand 2002; 106:314 319
165. Tolin DF, Maltby N, Diefenbach GJ, Hannan SE, Worhunsky P: Cognitivebehavioral therapy for medication nonresponders with obsessive-compulsive disorder: a wait-list-controlled open trial. J Clin Psychiatry 2004;
65:922931
166. Tundo A, Salvati L, Busto G, Di Spigno D, Falcini R: Addition of
cognitive-behavioral therapy for nonresponders to medication for obsessive-compulsive disorder: a naturalistic study. J Clin Psychiatry
2007; 68:15521556
167. Simpson HB, Foa EB, Liebowitz MR, Ledley DR, Huppert JD, Cahill S,
Vermes D, Schmidt AB, Hembree E, Franklin M, Campeas R, Hahn CG,
Petkova E: A randomized, controlled trial of cognitive-behavioral therapy
521
LANOUETTE AND STEIN
189.
190.
191.
192.
193.
194.
195.
196.
197.
198.
199.
200.
201.
202.
203.
204.
205.
206.
207.
208.
209.
522
Fall 2010, Vol. VIII, No. 4
serotonin reuptake inhibitors in treatment-resistant obsessive-compulsive disorder. Eur Neuropsychopharmacol 2008; 18:364 372
Li X, May RS, Tolbert LC, Jackson WT, Flournoy JM, Baxter LR:
Risperidone and haloperidol augmentation of serotonin reuptake inhibitors in refractory obsessive-compulsive disorder: a crossover study.
J Clin Psychiatry 2005; 66:736 743
Bloch MH, Landeros-Weisenberger A, Kelmendi B, Coric V, Bracken MB,
Leckman JF: A systematic review: antipsychotic augmentation with
treatment refractory obsessive-compulsive disorder. Mol Psychiatry
2006; 11:622 632
Matsunaga H, Nagata T, Hayashida K, Ohya K, Kiriike N, Stein DJ: A
long-term trial of the effectiveness and safety of atypical antipsychotic
agents in augmenting SSRI-refractory obsessive-compulsive disorder.
J Clin Psychiatry 2009; 70:863 868
Pessina E, Albert U, Bogetto F, Maina G: Aripiprazole augmentation of
serotonin reuptake inhibitors in treatment-resistant obsessive-compulsive disorder: a 12-week open-label preliminary study. Int Clin Psychopharmacol 2009; 24:265269
Hewlett WA, Vinogradov S, Agras WS: Clomipramine, clonazepam, and
clonidine treatment of obsessive-compulsive disorder. J Clin Psychopharmacol 1992; 12:420 430
Hollander E, Kaplan A, Stahl SM: A double-blind, placebo-controlled trial
of clonazepam in obsessive-compulsive disorder. World J Biol Psychiatry 2003; 4:30 34
Crockett BA, Churchill E, Davidson JR: A double-blind combination study
of clonazepam with sertraline in obsessive-compulsive disorder. Ann
Clin Psychiatry 2004; 16:127132
Pato MT, Pigott TA, Hill JL, Grover GN, Bernstein S, Murphy DL:
Controlled comparison of buspirone and clomipramine in obsessivecompulsive disorder. Am J Psychiatry 1991; 148:127129
Grady TA, Pigott TA, LHeureux F, Hill JL, Bernstein SE, Murphy DL:
Double-blind study of adjuvant buspirone for fluoxetine-treated patients
with obsessive-compulsive disorder. Am J Psychiatry 1993; 150:819
821
McDougle CJ, Goodman WK, Leckman JF, Holzer JC, Barr LC, McCanceKatz E, Heninger GR, Price LH: Limited therapeutic effect of addition of
buspirone in fluvoxamine-refractory obsessive-compulsive disorder.
Am J Psychiatry 1993; 150:647 649
Pigott TA, LHeureux F, Hill JL, Bihari K, Bernstein SE, Murphy DL: A
double-blind study of adjuvant buspirone hydrochloride in clomipramine-treated patients with obsessive-compulsive disorder. J Clin Psychopharmacol 1992; 12:1118
Coric V, Taskiran S, Pittenger C, Wasylink S, Mathalon DH, Valentine G,
Saksa J, Wu YT, Gueorguieva R, Sanacora G, Malison RT, Krystal JH:
Riluzole augmentation in treatment-resistant obsessive-compulsive
disorder: an open-label trial. Biol Psychiatry 2005; 58:424 428
McDougle CJ, Price LH, Goodman WK, Charney DS, Heninger GR: A
controlled trial of lithium augmentation in fluvoxamine-refractory obsessive-compulsive disorder: lack of efficacy. J Clin Psychopharmacol
1991; 11:175184
Pigott TA, Pato MT, LHeureux F, Hill JL, Grover GN, Bernstein SE,
Murphy DL: A controlled comparison of adjuvant lithium carbonate or
thyroid hormone in clomipramine-treated patients with obsessive-compulsive disorder. J Clin Psychopharmacol 1991; 11:242248
Koran LM, Aboujaoude E, Bullock KD, Franz B, Gamel N, Elliott M:
Double-blind treatment with oral morphine in treatment-resistant obsessive-compulsive disorder. J Clin Psychiatry 2005; 66:353359
Stewart SE, Jenike EA, Hezel DM, Stack DE, Dodman NH, Shuster L,
Jenike MA: A single-blinded case-control study of memantine in severe
obsessive-compulsive disorder. J Clin Psychopharmacol 2010; 30:
34 39
Insel TR, Hamilton JA, Guttmacher LB, Murphy DL: D-Amphetamine in
obsessive-compulsive disorder. Psychopharmacology (Berl) 1983; 80:
231235
Joffe RT, Swinson RP, Levitt AJ: Acute psychostimulant challenge in
primary obsessive-compulsive disorder. J Clin Psychopharmacol 1991;
11:237241
Koran LM, Aboujaoude E, Gamel NN: Double-blind study of dextroamphetamine versus caffeine augmentation for treatment-resistant obsessive-compulsive disorder. J Clin Psychiatry 2009; 70:1530 1535
Kushner MG, Kim SW, Donahue C, Thuras P, Adson D, Kotlyar M,
McCabe J, Peterson J, Foa EB: D-Cycloserine augmented exposure
therapy for obsessive-compulsive disorder. Biol Psychiatry 2007; 62:
835 838
Wilhelm S, Buhlmann U, Tolin DF, Meunier SA, Pearlson GD, Reese HE,
Cannistraro P, Jenike MA, Rauch SL. Augmentation of behavior therapy
with D-cycloserine for obsessive-compulsive disorder. Am J Psychiatry
2008; 165:335341; quiz 409
FOCUS
210. Dannon PN, Sasson Y, Hirschmann S, Iancu I, Grunhaus LJ, Zohar J:
Pindolol augmentation in treatment-resistant obsessive compulsive
disorder: a double-blind placebo controlled trial. Eur Neuropsychopharmacol 2000; 10:165169
211. Mundo E, Guglielmo E, Bellodi L: Effect of adjuvant pindolol on the
antiobsessional response to fluvoxamine: a double-blind, placebo-controlled study. Int Clin Psychopharmacol 1998; 13:219 224
212. Bystritsky A, Munford PR, Rosen RM, Martin KM, Vapnik T, Gorbis EE,
Wolson RC: A preliminary study of partial hospital management of
severe obsessive-compulsive disorder. Psychiatr Serv 1996; 47:170
174
213. Bystritsky A, Saxena S, Maidment K, Vapnik T, Tarlow G, Rosen R:
Quality-of-life changes among patients with obsessive-compulsive disorder in a partial hospitalization program. Psychiatr Serv 1999; 50:412
414
214. Calvocoressi L, McDougle CI, Wasylink S, Goodman WK, Trufan SJ, Price
LH: Inpatient treatment of patients with severe obsessive-compulsive
disorder. Hosp Community Psychiatry 1993; 44:1150 1154
215. McKenzie N, Marks I: Routine monitoring of outcome over 11 years in
a residential behavioural psychotherapy unit. Psychother Psychosom
2003; 72:223227
216. Stewart SE, Stack DE, Farrell C, Pauls DL, Jenike MA: Effectiveness of
intensive residential treatment (IRT) for severe, refractory obsessivecompulsive disorder. J Psychiatr Res 2005; 39:603 609
217. Stewart SE, Stack DE, Tsilker S, Alosso J, Stephansky M, Hezel DM,
Jenike EA, Haddad SA, Kant J, Jenike MA: Long-term outcome following
intensive residential treatment of obsessive-compulsive disorder. J Psychiatr Res 2009; 43:1118 1123
218. Thornicroft G, Colson L, Marks I: An in-patient behavioural psychotherapy unit. Description and audit. Br J Psychiatry 1991; 158:362367
219. Jenike MA, Baer L, Ballantine T, Martuza RL, Tynes S, Giriunas I,
Buttolph ML, Cassem NH: Cingulotomy for refractory obsessive-compulsive disorder. A long-term follow-up of 33 patients. Arch Gen Psychiatry 1991; 48:548 555
220. Kim CH, Chang JW, Koo MS, Kim JW, Suh HS, Park IH, Lee HS: Anterior
cingulotomy for refractory obsessive-compulsive disorder. Acta Psychiatr Scand 2003; 107:283290
221. Lopes AC, Greenberg BD, Noren G, Canteras MM, Busatto GF, de Mathis
ME, Taub A, DAlcante CC, Hoexter MQ, Gouvea FS, Cecconi JP, Gentil
AF, Ferrao YA, Fuentes D, de Castro CC, Leite CC, Salvajoli JV, Duran FL,
Rasmussen S, Miguel EC: Treatment of resistant obsessive-compulsive
disorder with ventral capsular/ventral striatal gamma capsulotomy: a
pilot prospective study. J Neuropsychiatry Clin Neurosci 2009; 21:381
392
222. Oliver B, Gascon J, Aparicio A, Ayats E, Rodriguez R, Maestro De Leon
JL, Garca-Bach M, Soler PA. Bilateral anterior capsulotomy for refractory obsessive-compulsive disorders. Stereotact Funct Neurosurg 2003;
81:90 95
223. Rasmussen S, Greenberg B, Mindus P, Friehs G, Noren G: Neurosurgical
approaches to intractable obsessive-compulsive disorder. CNS Spectr
2000; 5:2334
224. Ruck C, Karlsson A, Steele JD, Edman G, Meyerson BA, Ericson K,
Nyman H, Asberg M, Svanborg P: Capsulotomy for obsessive-compulsive disorder: long-term follow-up of 25 patients. Arch Gen Psychiatry
2008; 65:914 921
225. Abelson JL, Curtis GC, Sagher O, Albucher RC, Harrigan M, Taylor SF,
Martis B, Giordani B: Deep brain stimulation for refractory obsessivecompulsive disorder. Biol Psychiatry 2005; 57:510 516
226. Goodman WK, Foote KD, Greenberg BD, Ricciuti N, Bauer R, Ward H,
Shapira NA, Wu SS, Hill CL, Rasmussen SA, Okun MS: Deep brain
stimulation for intractable obsessive compulsive disorder: pilot study
using a blinded, staggered-onset design. Biol Psychiatry 2010; 67:535
542
227. Maletzky B, McFarland B, Burt A: Refractory obsessive compulsive
disorder and ECT. Convuls Ther 1994; 10:34 42
228. Prasko J, Paskova B, Zalesky R, Novak T, Kopecek M, Bares M, Horacek
J: The effect of repetitive transcranial magnetic stimulation (rTMS) on
symptoms in obsessive compulsive disorder. A randomized, double
blind, sham controlled study. Neuro Endocrinol Lett 2006; 27:327332
229. Sachdev PS, Loo CK, Mitchell PB, McFarquhar TF, Malhi GS: Repetitive
transcranial magnetic stimulation for the treatment of obsessive compulsive disorder: a double-blind controlled investigation. Psychol Med
2007; 37:16451649
230. Alonso P, Pujol J, Cardoner N, Benlloch L, Deus J, Menchon JM,
Capdevila A, Vallejo J: Right prefrontal repetitive transcranial magnetic
stimulation in obsessive-compulsive disorder: a double-blind, placebocontrolled study. Am J Psychiatry 2001; 158:11431145
231. Slotema CW, Blom JD, Hoek HW, Sommer IE: Should we expand the
THE JOURNAL OF LIFELONG LEARNING IN PSYCHIATRY
LANOUETTE AND STEIN
232.
233.
234.
236.
237.
238.
239.
240.
241.
242.
243.
244.
245.
246.
247.
248.
249.
250.
251.
252.
focus.psychiatryonline.org
253.
254.
255.
256.
257.
258.
259.
260.
261.
262.
263.
264.
265.
266.
267.
268.
269.
270.
271.
272.
273.
274.
275.
276.
cognitive-behavioral group therapy for the treatment of social phobia. J
Anxiety Disord 2000; 14:345358
Seedat S, Stein MB: Double-blind, placebo-controlled assessment of
combined clonazepam with paroxetine compared with paroxetine
monotherapy for generalized social anxiety disorder. J Clin Psychiatry
2004; 65:244 248
Pande AC, Davidson JR, Jefferson JW, Janney CA, Katzelnick DJ,
Weisler RH, Greist JH, Sutherland SM: Treatment of social phobia with
gabapentin: a placebo-controlled study. J Clin Psychopharmacol 1999;
19:341348
Pande AC, Feltner DE, Jefferson JW, Davidson JR, Pollack M, Stein MB,
Lydiard RB, Futterer R, Robinson P, Slomkowski M, DuBoff E, Phelps M,
Janney CA, Werth JL: Efficacy of the novel anxiolytic pregabalin in social
anxiety disorder: a placebo-controlled, multicenter study. J Clin Psychopharmacol 2004; 24:141149
Simon NM, Worthington JJ, Doyle AC, Hoge EA, Kinrys G, Fischmann D,
Link N, Pollack MH: An open-label study of levetiracetam for the
treatment of social anxiety disorder. J Clin Psychiatry 2004; 65:1219
1222
Zhang W, Connor KM, Davidson JR: Levetiracetam in social phobia: a
placebo controlled pilot study. J Psychopharmacol 2005; 19:551553
Stein MB, Ravindran LN, Simon NM, Liebowitz MR, Khan A, BrawmanMintzer O, Lydiard RB, Pollack MH: Levetiracetam in generalized social
anxiety disorder: a double-blind, randomized controlled trial. J Clin
Psychiatry 2010; 71:627 631
Dunlop BW, Papp L, Garlow SJ, Weiss PS, Knight BT, Ninan PT:
Tiagabine for social anxiety disorder. Hum Psychopharmacol 2007;
22:241244
Van Ameringen M, Mancini C, Pipe B, Oakman J, Bennett M: An open
trial of topiramate in the treatment of generalized social phobia. J Clin
Psychiatry 2004; 65:1674 1678
Kinrys G, Pollack MH, Simon NM, Worthington JJ, Nardi AE, Versiani M:
Valproic acid for the treatment of social anxiety disorder. Int Clin
Psychopharmacol 2003; 18:169 172
Barnett SD, Kramer ML, Casat CD, Connor KM, Davidson JR: Efficacy of
olanzapine in social anxiety disorder: a pilot study. J Psychopharmacol
2002; 16:365368
Schutters SI, van Megen HJ, Westenberg HG: Efficacy of quetiapine in
generalized social anxiety disorder: results from an open-label study.
J Clin Psychiatry 2005; 66:540 542
Vaishnavi S, Alamy S, Zhang W, Connor KM, Davidson JR: Quetiapine as
monotherapy for social anxiety disorder: a placebo-controlled study.
Prog Neuropsychopharmacol Biol Psychiatry 2007; 31:1464 1469
Donahue CB, Kushner MG, Thuras PD, Murphy TG, Van Demark JB,
Adson DE: Effect of quetiapine vs. placebo on response to two virtual
public speaking exposures in individuals with social phobia. J Anxiety
Disord 2009; 23:362368
Schneier FR, Saoud JB, Campeas R, Fallon BA, Hollander E, Coplan J,
Liebowitz MR: Buspirone in social phobia. J Clin Psychopharmacol
1993; 13:251256
Van Ameringen M, Mancini C, Wilson C: Buspirone augmentation of
selective serotonin reuptake inhibitors (SSRIs) in social phobia. J Affect
Disord 1996; 39:115121
Clark DB, Agras WS: The assessment and treatment of performance
anxiety in musicians. Am J Psychiatry 1991; 148:598 605
van Vliet IM, den Boer JA, Westenberg HG, Pian KL: Clinical effects of
buspirone in social phobia: a double-blind placebo-controlled study.
J Clin Psychiatry 1997; 58:164 168
Atmaca M, Tezcan E, Kuloglu M: An open clinical trial of reboxetine in
the treatment of social phobia. J Clin Psychopharmacol 2003; 23:417
419
Ravindran LN, Kim DS, Letamendi AM, Stein MB: A randomized controlled trial of atomoxetine in generalized social anxiety disorder. J Clin
Psychopharmacol 2009; 29:561564
Drew PJ, Barnes JN, Evans SJ: The effect of acute beta-adrenoceptor
blockade on examination performance. Br J Clin Pharmacol 1985;
19:783786
Elman MJ, Sugar J, Fiscella R, Deutsch TA, Noth J, Nyberg M, Packo K,
Anderson RJ. The effect of propranolol versus placebo on resident
surgical performance. Trans Am Ophthalmol Soc 1998; 96:283291;
discussion 9194
Hartley LR, Ungapen S, Davie I, Spencer DJ: The effect of adrenergic
blocking drugs on speakers performance and memory. Br J Psychiatry
1983; 142:512517
James IM, Burgoyne W, Savage IT: Effect of pindolol on stress-related
disturbances of musical performance: preliminary communication. J R
Soc Med 1983; 76:194 196
Stein MB, Sareen J, Hami S, Chao J: Pindolol potentiation of paroxetine
FOCUS
Fall 2010, Vol. VIII, No. 4
CLINICAL
SYNTHESIS
235.
toolbox of psychiatric treatment methods to include repetitive transcranial magnetic stimulation (rTMS)? A meta-analysis of the efficacy of
rTMS in psychiatric disorders. J Clin Psychiatry 2010; 71:873 884
Sarkhel S, Sinha VK, Praharaj SK: Adjunctive high-frequency right
prefrontal repetitive transcranial magnetic stimulation (rTMS) was not
effective in obsessive-compulsive disorder but improved secondary
depression. J Anxiety Disord 2010; 24:535539
Ruffini C, Locatelli M, Lucca A, Benedetti F, Insacco C, Smeraldi E:
Augmentation effect of repetitive transcranial magnetic stimulation over
the orbitofrontal cortex in drug-resistant obsessive-compulsive disorder
patients: a controlled investigation. Prim Care Companion J Clin Psychiatry 2009; 11:226 230
Mantovani A, Simpson HB, Fallon BA, Rossi S, Lisanby SH: Randomized
sham-controlled trial of repetitive transcranial magnetic stimulation in
treatment-resistant obsessive-compulsive disorder. Int J Neuropsychopharmacol 2010; 13:217227
Muller JE, Koen L, Seedat S, Stein DJ: Social anxiety disorder: current
treatment recommendations. CNS Drugs 2005; 19:377391
Blanco C, Heimberg RG, Schneier FR, Fresco DM, Chen H, Turk CL,
Vermes D, Erwin BA, Schmidt AB, Juster HR, Campeas R, Liebowitz MR:
A placebo-controlled trial of phenelzine, cognitive behavioral group
therapy, and their combination for social anxiety disorder. Arch Gen
Psychiatry 2010; 67:286 295
Davidson JR, Foa EB, Huppert JD, Keefe FJ, Franklin ME, Compton JS,
Zhao N, Connor KM, Lynch TR, Gadde KM: Fluoxetine, comprehensive
cognitive behavioral therapy, and placebo in generalized social phobia.
Arch Gen Psychiatry 2004; 61:10051013
Atmaca M, Kuloglu M, Tezcan E, Unal A: Efficacy of citalopram and
moclobemide in patients with social phobia: some preliminary findings.
Hum Psychopharmacol 2002; 17:401 405
Schneier FR, Goetz D, Campeas R, Fallon B, Marshall R, Liebowitz MR:
Placebo-controlled trial of moclobemide in social phobia. Br J Psychiatry
1998; 172:70 77
Stein DJ, Cameron A, Amrein R, Montgomery SA, Moclobemide Social
Phobia Clinical Study Group: Moclobemide is effective and well tolerated
in the long-term pharmacotherapy of social anxiety disorder with or
without comorbid anxiety disorder. Int Clin Psychopharmacol 2002;
17:161170
Versiani M, Nardi AE, Mundim FD, Alves AB, Liebowitz MR, Amrein R:
Pharmacotherapy of social phobia. A controlled study with moclobemide
and phenelzine. Br J Psychiatry 1992; 161:353360
Versiani M, Nardi AE, Mundim FD, Pinto S, Saboya E, Kovacs R: The
long-term treatment of social phobia with moclobemide. Int Clin Psychopharmacol 1996; 11(suppl 3):83 88
Fahlen T, Nilsson HL, Borg K, Humble M, Pauli U: Social phobia: the
clinical efficacy and tolerability of the monoamine oxidase-A and serotonin uptake inhibitor brofaromine. A double-blind placebo-controlled
study. Acta Psychiatr Scand 1995; 92:351358
Lott M, Greist JH, Jefferson JW, Kobak KA, Katzelnick DJ, Katz RJ,
Schaettle SC: Brofaromine for social phobia: a multicenter, placebocontrolled, double-blind study. J Clin Psychopharmacol 1997; 17:255
260
van Vliet IM, den Boer JA, Westenberg HG: Psychopharmacological
treatment of social phobia: clinical and biochemical effects of brofaromine, a selective MAO-A inhibitor. Eur Neuropsychopharmacol 1992;
2:2129
Simpson HB, Schneier FR, Marshall RD, Campeas RB, Vermes D,
Silvestre J, Davies S, Liebowitz MR: Low dose selegiline (L-Deprenyl) in
social phobia. Depress Anxiety 1998; 7:126 129
Van Veen JF, Van Vliet IM, Westenberg HG: Mirtazapine in social anxiety
disorder: a pilot study. Int Clin Psychopharmacol 2002; 17:315317
Muehlbacher M, Nickel MK, Nickel C, Kettler C, Lahmann C, Pedrosa Gil
F, Leiberich PK, Rother N, Bachler E, Fartacek R, Kaplan P, Tritt K,
Mitterlehner F, Anvar J, Rother WK, Loew TH, Egger C: Mirtazapine
treatment of social phobia in women: a randomized, double-blind,
placebo-controlled study. J Clin Psychopharmacol 2005; 25:580 583
Connor KM, Davidson JR, Potts NL, Tupler LA, Miner CM, Malik ML,
Book SW, Colket JT, Ferrell F: Discontinuation of clonazepam in the
treatment of social phobia. J Clin Psychopharmacol 1998; 18:373378
Davidson JR, Potts N, Richichi E, Krishnan R, Ford SM, Smith R, Wilson
WH: Treatment of social phobia with clonazepam and placebo. J Clin
Psychopharmacol 1993; 13:423 428
Munjack DJ, Baltazar PL, Bohn PB, Cabe DD, Appleton AA: Clonazepam
in the treatment of social phobia: a pilot study. J Clin Psychiatry 1990;
51(suppl):35 40; discussion 50 53
Otto MW, Pollack MH, Gould RA, Worthington JJ 3rd, McArdle ET,
Rosenbaum JF: A comparison of the efficacy of clonazepam and
523
LANOUETTE AND STEIN
277.
278.
279.
280.
281.
for generalized social phobia: a double-blind, placebo-controlled, crossover study. Am J Psychiatry 2001; 158:17251727
Liebowitz MR, Schneier F, Campeas R, Hollander E, Hatterer J, Fyer A,
Gorman J, Papp L, Davies S, Gully R: Phenelzine vs atenolol in social
phobia. A placebo-controlled comparison. Arch Gen Psychiatry 1992;
49:290 300
Turner SM, Beidel DC, Jacob RG: Social phobia: a comparison of
behavior therapy and atenolol. J Consult Clin Psychol 1994; 62:350
358
Guastella AJ, Richardson R, Lovibond PF, Rapee RM, Gaston JE, Mitchell
P, Dadds MR: A randomized controlled trial of D-cycloserine enhancement of exposure therapy for social anxiety disorder. Biol Psychiatry
2008; 63:544 549
Hofmann SG, Meuret AE, Smits JA, Simon NM, Pollack MH, Eisenmenger K, Shiekh M, Otto MW: Augmentation of exposure therapy with
D-cycloserine for social anxiety disorder. Arch Gen Psychiatry 2006;
63:298 304
Guastella AJ, Howard AL, Dadds MR, Mitchell P, Carson DS: A randomized controlled trial of intranasal oxytocin as an adjunct to exposure
282.
283.
284.
285.
286.
therapy for social anxiety disorder. Psychoneuroendocrinology 2009;
34:917923
Amir N, Beard C, Taylor CT, Klumpp H, Elias J, Burns M, Chen X:
Attention training in individuals with generalized social phobia: a randomized controlled trial. J Consult Clin Psychol 2009; 77:961973
Schmidt NB, Richey JA, Buckner JD, Timpano KR: Attention training for
generalized social anxiety disorder. J Abnorm Psychol 2009; 118:514
McEvoy PM, Perini SJ: Cognitive behavioral group therapy for social
phobia with or without attention training: a controlled trial. J Anxiety
Disord 2009; 23:519 528
Knijnik DZ, Blanco C, Salum GA, Moraes CU, Mombach C, Almeida E,
Pereira M, Strapasson A, Manfro GG, Eizirik CL: A pilot study of
clonazepam versus psychodynamic group therapy plus clonazepam in
the treatment of generalized social anxiety disorder. Eur Psychiatry
2008; 23:567574
Koszycki D, Benger M, Shlik J, Bradwejn J: Randomized trial of a
meditation-based stress reduction program and cognitive behavior therapy in generalized social anxiety disorder. Behav Res Ther 2007;
45:2518 2526
NOTES
524
Fall 2010, Vol. VIII, No. 4
FOCUS
THE JOURNAL OF LIFELONG LEARNING IN PSYCHIATRY
Das könnte Ihnen auch gefallen
- Manual K BITDokument109 SeitenManual K BITJosé María López86% (14)
- Tecnicas para Cartas de Amor U OdioDokument4 SeitenTecnicas para Cartas de Amor U OdioChristian Gabriel Stampacchio100% (16)
- Tecnicas para Cartas de Amor U OdioDokument4 SeitenTecnicas para Cartas de Amor U OdioChristian Gabriel Stampacchio100% (16)
- BB Web TP Focus 2011 Diag y Tto Del TPanico Resistente. LydiardDokument11 SeitenBB Web TP Focus 2011 Diag y Tto Del TPanico Resistente. LydiardAdriana Rodriguez PalmeroNoch keine Bewertungen
- BB Web TP AJP 2000 Hipotesis Neuroanatomica Del TP. Revisited. GormanDokument13 SeitenBB Web TP AJP 2000 Hipotesis Neuroanatomica Del TP. Revisited. GormanAdriana Rodriguez PalmeroNoch keine Bewertungen
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (587)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (265)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (119)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Pharmacokinetic ModelsDokument36 SeitenPharmacokinetic ModelsNeeraj Kumar100% (1)
- (Charles J. Gelso, Jeffrey Hayes) CountertransfereDokument186 Seiten(Charles J. Gelso, Jeffrey Hayes) CountertransfereArtis Ozols100% (3)
- Live music reduces pediatric distressDokument5 SeitenLive music reduces pediatric distressandreaNoch keine Bewertungen
- The Quality of Life of Breast Cancer Patients, Experience of The Mohamed 6 Center For The Treatment of Gynecological Breast CancerDokument19 SeitenThe Quality of Life of Breast Cancer Patients, Experience of The Mohamed 6 Center For The Treatment of Gynecological Breast CancerIJAR JOURNALNoch keine Bewertungen
- Mentor Interview QuestionsDokument3 SeitenMentor Interview Questionsapi-377093974Noch keine Bewertungen
- Intro Rebt CBTDokument3 SeitenIntro Rebt CBTnurulfarihah23Noch keine Bewertungen
- TechniquesDokument13 SeitenTechniquesMirela Cojocaru StetcoNoch keine Bewertungen
- EFPT Psychotherapy Guidebook PDFDokument62 SeitenEFPT Psychotherapy Guidebook PDFJackye BurgaNoch keine Bewertungen
- Cognitive Behavioral Therapy (Group Counselling)Dokument28 SeitenCognitive Behavioral Therapy (Group Counselling)Zed Idiaz100% (2)
- NICCA Implementing Rules and RegulationsDokument34 SeitenNICCA Implementing Rules and RegulationsFaith MorillaNoch keine Bewertungen
- ZGH ART Pharmacy InventoryDokument8 SeitenZGH ART Pharmacy InventorywondwossenNoch keine Bewertungen
- Strategic Alternatives in The Pharmaceutical Industry: Jeff Cohen William Gangi Jason Lineen Alice ManardDokument37 SeitenStrategic Alternatives in The Pharmaceutical Industry: Jeff Cohen William Gangi Jason Lineen Alice ManardRevanth KalyanamNoch keine Bewertungen
- Cancer and Its Treatment: An OverviewDokument7 SeitenCancer and Its Treatment: An OverviewIJAR JOURNALNoch keine Bewertungen
- Cognitive Behavioral Treatment of Generalized Anxiety DisorderDokument13 SeitenCognitive Behavioral Treatment of Generalized Anxiety DisorderTea Tsitou100% (1)
- Algoritma Penanganan Kejang AkutDokument1 SeiteAlgoritma Penanganan Kejang AkutEwa ClaudiaNoch keine Bewertungen
- Rechilding Creating A New Past in The Present As A Support For The FutureDokument10 SeitenRechilding Creating A New Past in The Present As A Support For The FutureBojanaNoch keine Bewertungen
- Rekapitulasi Februari 2023Dokument13 SeitenRekapitulasi Februari 2023hanafiNoch keine Bewertungen
- Anatomy Trains Video Series by Tom MyersDokument5 SeitenAnatomy Trains Video Series by Tom MyersRudaGica100% (1)
- The Word "Reiki" Means "Mysterious Atmosphere, Miraculous Sign." It Comes From The Japanese Words "Rei" (Universal) and Ki" (Life Energy)Dokument3 SeitenThe Word "Reiki" Means "Mysterious Atmosphere, Miraculous Sign." It Comes From The Japanese Words "Rei" (Universal) and Ki" (Life Energy)Đặng Ngọc ThạchNoch keine Bewertungen
- Early Complementary Acupuncture Improves The CliniDokument8 SeitenEarly Complementary Acupuncture Improves The ClinikhalisahnNoch keine Bewertungen
- Tic Poster FinalDokument1 SeiteTic Poster Finalapi-337168518Noch keine Bewertungen
- Seeing is Touch at a DistanceDokument1 SeiteSeeing is Touch at a Distancepradeep6288Noch keine Bewertungen
- Managing Difficult Patient Encounters (AAFP 2023)Dokument7 SeitenManaging Difficult Patient Encounters (AAFP 2023)Breno Resende Rodrigues CunhaNoch keine Bewertungen
- Handbook For Principles and Practice of Gynecologic Oncology-1Dokument379 SeitenHandbook For Principles and Practice of Gynecologic Oncology-1shivNoch keine Bewertungen
- Mapeh 6: Quarter 4 - Module 1Dokument10 SeitenMapeh 6: Quarter 4 - Module 1ALEX CORPORALNoch keine Bewertungen
- Jurnal Melasma PDFDokument3 SeitenJurnal Melasma PDFYessi KoruaNoch keine Bewertungen
- Tariffs Operation Manual v22Dokument147 SeitenTariffs Operation Manual v22Nanayaw CasperNoch keine Bewertungen
- Physical Therapy Cover Letter New GraduateDokument4 SeitenPhysical Therapy Cover Letter New Graduatebcrqs9hr100% (2)
- Sacubitril/Valsartan (Entresto) : Safe Prescribing and Use ofDokument1 SeiteSacubitril/Valsartan (Entresto) : Safe Prescribing and Use ofpatricia wageyNoch keine Bewertungen
- CaNaMed 01.01.2024Dokument273 SeitenCaNaMed 01.01.2024roxanamihaelapepiNoch keine Bewertungen