Beruflich Dokumente
Kultur Dokumente
Nejm 2
Hochgeladen von
Wiwik SundariOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Nejm 2
Hochgeladen von
Wiwik SundariCopyright:
Verfügbare Formate
The
n e w e ng l a n d j o u r na l
a diagnosis of multiple primary tumors.4 In
our patient, we had identified two different
truncating germline NTHL1 mutations in trans:
the above-mentioned c.268CT,p.Q90* mutation
and c.709+1GA, which results in abnormal splicing (Fig. 1B, and Fig. S1 in the Supplementary
Appendix, available with the full text of this letter
at NEJM.org). We used several methods to study
the mutation profile of the tumors (Table S1 and
Fig. S2 and S3 in the Supplementary Appendix).
In so doing, we extended the previous report 4
to include benign and malignant extracolonic
tumors. The mutation spectrum was significantly shifted in favor of C:GT:A transitions
(Fig. S2 in the Supplementary Appendix), as reported previously.4 Among other driver mutations,
we identified the frequently reported5 FGFR3 mutation c.742CT,p.R248C in one seborrheic keratosis (Fig. S3 in the Supplementary Appendix).
A single NTHL1 mutation, p.Q90*, was identified by investigators in Nijmegen, the Netherlands,4 which is only 150 km from Dortmund,
Germany, where the paternal relatives of our
patient were born. This finding suggests that
the p.Q90* allele was inherited paternally. The
c.709+1GA mutation has been reported only once
in 118,482 alleles that were collated by the Exome
Aggregation Consortium (exac.broadinstitute.org).
This study extends the description of biallelic mutations in NTHL1 beyond the single
of
m e dic i n e
c.268CT,p.Q90* mutation that was observed
previously.4 Since the cancer phenotype of biallelic NTHL1 mutations may be very broad, referring to the NTHL1 syndrome could be a useful
way of describing this condition, rather than focusing solely on the colorectal phenotype.
Barbara Rivera, Ph.D.
Ester Castellsagu, Ph.D.
Ismal Bah, M.D.
McGill University
Montreal, QC, Canada
barbara.riverap@gmail.com
and Others
A complete list of authors is available with the full text of
this letter at NEJM.org.
Disclosure forms provided by the authors are available with
the full text of this letter at NEJM.org.
1. Mersheimer WL, Ringel A, Eisenberg H. Some characteris-
tics of multiple primary cancers. Ann N Y Acad Sci 1964;114:
896-921.
2. Muir EG, Bell AJ, Barlow KA. Multiple primary carcinomata
of the colon, duodenum, and larynx associated with kerato-acanthomata of the face. Br J Surg 1967;54:191-5.
3. Cybulski C, Nazarali S, Narod SA. Multiple primary cancers
as a guide to heritability. Int J Cancer 2014;135:1756-63.
4. Weren RD, Ligtenberg MJ, Kets CM, et al. A germline homozygous mutation in the base-excision repair gene NTHL1 causes
adenomatous polyposis and colorectal cancer. Nat Genet 2015;47:
668-71.
5. Hafner C, Toll A, Fernndez-Casado A, et al. Multiple oncogenic mutations and clonal relationship in spatially distinct benign human epidermal tumors. Proc Natl Acad Sci U S A 2010;
107:20780-5.
DOI: 10.1056/NEJMc1506878
Acquired Resistance to Bedaquiline and Delamanid
in Therapy for Tuberculosis
To the Editor: Multidrug-resistant tuberculosis
(MDR-TB) and extensively drug-resistant tuberculosis (XDR-TB) are an increasing public health
threat.1 Bedaquiline and delamanid are two drugs
that were recently approved by the Food and
Drug Administration for treatment of MDR-TB
and XDR-TB.2 Here we describe the stepwise amplification of drug resistance in a patient who
had emigrated from Tibet to Switzerland in December 2010 and who presented to a Swiss hospital with preextensively drug-resistant tuberculosis at that time.
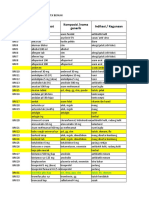
Figure 1 (facing page). Clinical Features, Treatment History, Amplification of Drug Resistance, and Phenotypic DrugSusceptibility Testing in the Patient.
Mutations that confer drug resistance are shown. Resistance to bedaquiline, intravenous capreomycin, and delamanid developed. Percentages on the y axis are based on the number of genome-sequencing reads supporting the corresponding
drug resistanceconferring mutation (details are provided in Table S4 in the Supplementary Appendix). Large colored
circles indicate measurements, and dashed lines linking these circles indicate the changes in mutation frequency. The
loss of the start codon is indicated with an asterisk, and fs indicates frame shift. The mutations listed on the left side of
the graph were detected in the first and all subsequent isolates obtained from the patient. All these mutations were seen
in 100% of sequencing reads in each isolate. X indicates the stop codon, and del indicates deletion. On the x axis, isolate
numbers are listed under the month when the isolate was obtained. TMP-SMX denotes trimethoprimsulfamethoxazole.
1986
n engl j med 373;20nejm.orgnovember 12, 2015
The New England Journal of Medicine
Downloaded from nejm.org on February 20, 2016. For personal use only. No other uses without permission.
Copyright 2015 Massachusetts Medical Society. All rights reserved.
correspondence
Treatment History
Smear:
Culture: +
Clinical cure
+
+
Relapse
Ethambutol
Ethambutol
Aminosalicylic acid
Intravenous aminosalicylic acid
Intravenous capreomycin
Intravenous capreomycin
Cycloserine
Intravenous cycloserine
Bedaquiline
Levofloxacin
Meropenem
Clavulanate
Inhaled amikacin
Clofazimine
TMP-SMX
Ju
20 ne
14 20
18 14
Ju 011
20 ly 4
14 20
18 14
60
23
20 ch
14 20
18 14
60
11
M
ar
14 0
18 13
60
11
ec
em
b
20 er
2
11
6
Au
Ja
nu
ar
20 y
11 20
18 11
60
00
gu
st
2
20 Re 013
13 lap
18 se
6
M
a
Cl rch
in 2
ica 01
lC 3
ur
e
Delamanid
Whole-Genome Sequencing
Clinical cure
100
80
Allele Frequency (%)
Relapse
RpoB S531L
RpoC D485Y
KatG S315T
RpsL K88R
GyrA D94Y
GyrB V630G
GidB R158L
PncA E107X
EthA F349del
60
MmpR V1A*
TlyA A17E
FbiA D49Y
Fgd1 G49fs
rrl G2576T
40
rrl A2572C
20
Ju
20 ne
14 20
18 14
Ju 011
20 ly 4
14 20
18 14
60
23
ar
20 ch
14 20
18 14
60
11
em
ec
D
20 r
14 20
18 13
60
11
be
11
st
2
20 Re 013
13 lap
18 se
6
gu
Au
Ja
nu
a
20 ry
11 20
18 11
60
00
M
a
Cl rch
in 2
ica 01
lC 3
ur
e
Phenotypic Drug-Susceptibility Testing
Clinical cure
Relapse
Resistance: isoniazid, rifampicin, pyrazinamide, ethionamide, linezolid, moxifloxacin, streptomycin
Resistance: bedaquiline, clofazimine
Resistance: capreomycin
Ju
20 ne
14 20
18 14
Ju 011
20 ly 4
14 20
18 14
60
23
ar
20 ch
14 20
18 14
60
11
ec
em
be
20 r
14 20
18 13
60
11
61
16
t2
20 Re 013
13 lap
18 se
gu
s
Au
Ja
nu
20 ry
11 20
18 11
60
00
M
a
Cl rch
in 2
ica 01
lC 3
ur
e
Resistance:
delamanid
Genome sequencing revealed that the initial
Mycobacterium tuberculosis isolate harbored nine
mutations in genes associated with resistance to
seven drugs (Fig. 1, and the Supplementary Ap-
pendix, available with the full text of this letter
at NEJM.org). The isolate also showed a compensatory mutation in rpoC,3 indicating a mature
preextensively drug-resistant strain that had evolved
n engl j med 373;20nejm.orgnovember 12, 2015
The New England Journal of Medicine
Downloaded from nejm.org on February 20, 2016. For personal use only. No other uses without permission.
Copyright 2015 Massachusetts Medical Society. All rights reserved.
1987
The
n e w e ng l a n d j o u r na l
under drug pressure for some time. Given that
the patient reported no previous treatment for
tuberculosis, he was probably infected with a
strain that was already resistant to these drugs.
In September 2011, bedaquiline was added to
the regimen, which had consisted of four drugs
(ethambutol, aminosalicylic acid, intravenous
capreomycin, and cycloserine). The patient was
considered to be clinically cured in March 2013,
but he had a relapse in August 2013. Genome
sequencing of five follow-up isolates revealed a
mutation in mmpR that was associated with bedaquiline resistance. This mutation persisted even
though bedaquiline was discontinued in February 2012; this suggests that it did not cause any
clinically significant reduction in the virulence
of the infecting bacteria.4
Additional resistance to second-line injectable
agents (such as capreomycin) also developed. This
was reflected in the emergence of mutations in
tlyA and rrs. The latter mutation remained at low
frequency and was detected only in drug-containing bacterial cultures (Table S3 in the Supplementary Appendix). All the molecular findings
were supported by phenotypic drug-susceptibility
testing.
Following this amplification in resistance,
delamanid was added to the regimen in March
2014. However, two mutations in f biA and fgd1
increased in frequency by June 2014, which co
incided with the emergence of phenotypic resistance to delamanid. These genes have previously
been associated with delamanid resistance. The
fgd1 mutation decreased in frequency thereafter,
indicating the presence of multiple delamanidresistant clones in the patient. In August and
September 2014, the patient underwent a lobectomy. After surgery, the sputum specimens obtained from the patient were culture-negative,
and the patient received treatment on an ambulatory basis.
This case highlights the development of resistance in the context of inadequate MDR-TB and
XDR-TB treatment regimens, despite personalized
patient care in a well-resourced health care setting. It serves as a warning for the future rollout
of new antituberculosis drugs and emphasizes
the need for the use of appropriate companion
drugs when bedaquiline and delamanid are administered. Our results add to previous findings
showing that the development of drug resistance
is a dynamic process involving multiple hetero1988
of
m e dic i n e
geneous populations of bacteria within individual patients.4,5
Guido V. Bloemberg, Ph.D.
University of Zurich
Zurich, Switzerland
Sebastien Gagneux, Ph.D.
Swiss Tropical and Public Health Institute
Basel, Switzerland
sebastien.gagneux@unibas.ch
Erik C. Bttger, M.D.
University of Zurich
Zurich, Switzerland
and Others
A complete list of authors is available with the full text of this
letter at NEJM.org.
Supported by the Swiss Federal Office of Public Health, the University of Zurich, SystemsX.ch, the Novartis Foundation, and grants
from the Swiss National Science Foundation (PP00P3_150750),
the National Institutes of Health (AI090928), and the European
Research Council (309540-EVODRTB).
Disclosure forms provided by the authors are available with
the full text of this letter at NEJM.org.
1. Global tuberculosis control surveillance, planning, financ-
ing. Geneva: World Health Organization, 2014.
2. Zumla A, Memish ZA, Maeurer M, et al. Emerging novel and
antimicrobial-resistant respiratory tract infections: new drug development and therapeutic options. Lancet Infect Dis 2014;14:
1136-49.
3. Comas I, Borrell S, Roetzer A, et al. Whole-genome sequencing of rifampicin-resistant Mycobacterium tuberculosis strains identifies compensatory mutations in RNA polymerase genes. Nat
Genet 2012;44:106-10.
4. Shcherbakov D, Akbergenov R, Matt T, Sander P, Andersson
DI, Bttger EC. Directed mutagenesis of Mycobacterium smegmatis
16S rRNA to reconstruct the in vivo evolution of aminoglycoside
resistance in Mycobacterium tuberculosis. Mol Microbiol 2010;77:
830-40.
5. Sun G, Luo T, Yang C, et al. Dynamic population changes in
Mycobacterium tuberculosis during acquisition and fixation of drug
resistance in patients. J Infect Dis 2012;206:1724-33.
DOI: 10.1056/NEJMc1505196
Correspondence Copyright 2015 Massachusetts Medical Society.
instructions for letters to the editor
Letters to the Editor are considered for publication, subject
to editing and abridgment, provided they do not contain
material that has been submitted or published elsewhere.
Please note the following:
Letters in reference to a Journal article must not exceed 175
words (excluding references) and must be received within
3 weeks after publication of the article.
Letters not related to a Journal article must not exceed 400
words.
A letter can have no more than five references and one figure
or table.
A letter can be signed by no more than three authors.
Financial associations or other possible conflicts of interest
must be disclosed. Disclosures will be published with the
letters. (For authors of Journal articles who are responding
to letters, we will only publish new relevant relationships
that have developed since publication of the article.)
n engl j med 373;20nejm.orgnovember 12, 2015
The New England Journal of Medicine
Downloaded from nejm.org on February 20, 2016. For personal use only. No other uses without permission.
Copyright 2015 Massachusetts Medical Society. All rights reserved.
Das könnte Ihnen auch gefallen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Questions:: Exercise 4. Bioethical Dilemma of Gene TherapyDokument2 SeitenQuestions:: Exercise 4. Bioethical Dilemma of Gene Therapyrjay manaloNoch keine Bewertungen
- Pulp Exposure in Permanent Teeth CG-A012-04 UpdatedDokument7 SeitenPulp Exposure in Permanent Teeth CG-A012-04 UpdatedmahmoudNoch keine Bewertungen
- Morgan Mikhails Clinical Anesthesiology 6th Ed 2018 (2114-2211)Dokument98 SeitenMorgan Mikhails Clinical Anesthesiology 6th Ed 2018 (2114-2211)Wiwik SundariNoch keine Bewertungen
- Chronic Breast Abscess Due To Mycobacterium Fortuitum: A Case ReportDokument3 SeitenChronic Breast Abscess Due To Mycobacterium Fortuitum: A Case ReportWiwik SundariNoch keine Bewertungen
- Morgan Mikhails Clinical Anesthesiology 6th Ed 2018 (2018-2114)Dokument97 SeitenMorgan Mikhails Clinical Anesthesiology 6th Ed 2018 (2018-2114)Wiwik SundariNoch keine Bewertungen
- Pola Asuh Pemberian Makan Pada Bayi Stun PDFDokument12 SeitenPola Asuh Pemberian Makan Pada Bayi Stun PDFRahma AR AslNoch keine Bewertungen
- Case PresentationDokument15 SeitenCase PresentationCintya Risti MawarniNoch keine Bewertungen
- 18 22 Breast AbscessDokument9 Seiten18 22 Breast AbscessWiwik SundariNoch keine Bewertungen
- Morgan Mikhails Clinical Anesthesiology 6th Ed 2018 (0509-0527)Dokument19 SeitenMorgan Mikhails Clinical Anesthesiology 6th Ed 2018 (0509-0527)Wiwik SundariNoch keine Bewertungen
- 85 1 147 1 10 20170210 PDFDokument8 Seiten85 1 147 1 10 20170210 PDFnunuyNoch keine Bewertungen
- Trigger Finger HuaDokument1 SeiteTrigger Finger HuaWiwik SundariNoch keine Bewertungen
- TriggerFinger PDFDokument1 SeiteTriggerFinger PDFNandaSuryaWijayaNoch keine Bewertungen
- Trigger FingerDokument8 SeitenTrigger FingerWiwik SundariNoch keine Bewertungen
- 18 22 Breast AbscessDokument9 Seiten18 22 Breast AbscessWiwik SundariNoch keine Bewertungen
- AlzheimerDokument1 SeiteAlzheimerWiwik SundariNoch keine Bewertungen
- 2007 Article 9012Dokument5 Seiten2007 Article 9012Karen PinemNoch keine Bewertungen
- AlzheimerDokument1 SeiteAlzheimerWiwik SundariNoch keine Bewertungen
- Penyakit Kulit UrtikariaDokument10 SeitenPenyakit Kulit UrtikariaSi PuputNoch keine Bewertungen
- Childhood Bipolar Disorder: A Clinical VignetteDokument4 SeitenChildhood Bipolar Disorder: A Clinical VignetteWiwik SundariNoch keine Bewertungen
- Dementia 3Dokument6 SeitenDementia 3Wiwik SundariNoch keine Bewertungen
- Trigger FingerDokument8 SeitenTrigger FingerWiwik SundariNoch keine Bewertungen
- Alzheimer MarkerDokument2 SeitenAlzheimer MarkerWiwik SundariNoch keine Bewertungen
- DTSCH Arztebl Int-112-0423 PDFDokument12 SeitenDTSCH Arztebl Int-112-0423 PDFyurni dwi astutiNoch keine Bewertungen
- 2007 Article 9012Dokument5 Seiten2007 Article 9012Karen PinemNoch keine Bewertungen
- Childhood Bipolar Disorder: A Clinical VignetteDokument4 SeitenChildhood Bipolar Disorder: A Clinical VignetteWiwik SundariNoch keine Bewertungen
- Varicela ZosterDokument16 SeitenVaricela ZosterMartin Hernàndez CruzNoch keine Bewertungen
- Aair 9 212Dokument8 SeitenAair 9 212Rio Mulya RihartaNoch keine Bewertungen
- Childhood Bipolar Disorder: A Clinical VignetteDokument4 SeitenChildhood Bipolar Disorder: A Clinical VignetteWiwik SundariNoch keine Bewertungen
- Comparison of Specific Antiviral Agents in Herpes Simplex KeratitisDokument7 SeitenComparison of Specific Antiviral Agents in Herpes Simplex KeratitisWiwik SundariNoch keine Bewertungen
- Regression of Herpes Viral Infection Symptoms UsinDokument7 SeitenRegression of Herpes Viral Infection Symptoms UsinAnonymous svz5xkTaNoch keine Bewertungen
- 2010 Age-Related Changes in The Musculoskeletal System and The Development of OsteoarthritisDokument18 Seiten2010 Age-Related Changes in The Musculoskeletal System and The Development of OsteoarthritisWiwik SundariNoch keine Bewertungen
- Isoroku Yamamoto: 3. Omar BradleyDokument3 SeitenIsoroku Yamamoto: 3. Omar BradleyWiwik SundariNoch keine Bewertungen
- Live - Yourself - Happy - Ed NewDokument132 SeitenLive - Yourself - Happy - Ed NewMartaNoch keine Bewertungen
- Nama Obat Indikasi / Kegunaan Komposisi /nama Generik: Brochifar Plus Kap PCT, DMP, Ppa, CTM Batuk, Flu, DemamDokument52 SeitenNama Obat Indikasi / Kegunaan Komposisi /nama Generik: Brochifar Plus Kap PCT, DMP, Ppa, CTM Batuk, Flu, Demamrio1995Noch keine Bewertungen
- Ultrasonography of The EyeDokument8 SeitenUltrasonography of The Eyetaner_soysurenNoch keine Bewertungen
- Specialize Immunity at Epithelial Barriers and in Immune Privilege TissuesDokument27 SeitenSpecialize Immunity at Epithelial Barriers and in Immune Privilege TissuesUmar UsmanNoch keine Bewertungen
- Breast Cancer Diagnostic Imaging in Dharmais Cancer HospitalDokument32 SeitenBreast Cancer Diagnostic Imaging in Dharmais Cancer HospitalIndonesian Journal of CancerNoch keine Bewertungen
- KodingDokument12 SeitenKodingAva Vav100% (1)
- New York Imaging Specialists Announces Grand Opening in Port Jefferson StationDokument2 SeitenNew York Imaging Specialists Announces Grand Opening in Port Jefferson StationPR.comNoch keine Bewertungen
- Acts Reinforcement Mar2020 PDFDokument8 SeitenActs Reinforcement Mar2020 PDFErika Kate MedadoNoch keine Bewertungen
- Heart Rate Variability Today PDFDokument11 SeitenHeart Rate Variability Today PDFVictor SmithNoch keine Bewertungen
- ADULT Nutrition Screening Questionnaire 2Dokument1 SeiteADULT Nutrition Screening Questionnaire 2Alejandra López SalasNoch keine Bewertungen
- Rab Flow CHT 3 PeopleDokument2 SeitenRab Flow CHT 3 PeopleWDIV/ClickOnDetroitNoch keine Bewertungen
- Medicine 018 Final PDFDokument22 SeitenMedicine 018 Final PDFdrkefyalewtayeNoch keine Bewertungen
- New School Health FormsDokument42 SeitenNew School Health FormsJoanna MarieNoch keine Bewertungen
- Mri Report - Left Knee Joint: Name Patient ID Accession No Age/Gender Referred by DateDokument2 SeitenMri Report - Left Knee Joint: Name Patient ID Accession No Age/Gender Referred by Datefaiyaz432Noch keine Bewertungen
- Drugs For Eyes and Ears 106Dokument2 SeitenDrugs For Eyes and Ears 106Asniya DiamelNoch keine Bewertungen
- Basic Anaestetic DrugsDokument1 SeiteBasic Anaestetic DrugsLuthfi AfiatNoch keine Bewertungen
- Rih - Lower Extremity Runoff Cta Ge Lightspeed 16 / Optima Ct580 ProtocolDokument1 SeiteRih - Lower Extremity Runoff Cta Ge Lightspeed 16 / Optima Ct580 ProtocolRafieLugassektiNoch keine Bewertungen
- Neoblade Trial Slides For NCRI Bladder Cancer MeetingDokument10 SeitenNeoblade Trial Slides For NCRI Bladder Cancer MeetingProf_Nick_JamesNoch keine Bewertungen
- TetanusDokument22 SeitenTetanusAlec AnonNoch keine Bewertungen
- Cardiolab Practical-PharmacologyDokument2 SeitenCardiolab Practical-PharmacologyGul HassanNoch keine Bewertungen
- Corynebacterium DiphtheriaDokument39 SeitenCorynebacterium DiphtheriaSubhada GosaviNoch keine Bewertungen
- VDL Biopsy SubmissionDokument26 SeitenVDL Biopsy SubmissionThomas Karl Anthony QUILANGNoch keine Bewertungen
- Opioid-Free AnesthesiaDokument8 SeitenOpioid-Free AnesthesiaPaulina LugoNoch keine Bewertungen
- Charcot Marie Tooth DiseaseDokument4 SeitenCharcot Marie Tooth DiseaseAbdul QuyyumNoch keine Bewertungen
- Gra ViolaDokument8 SeitenGra ViolaAnthony SullivanNoch keine Bewertungen
- Dialysis MachineDokument1 SeiteDialysis MachineMarifer NazNoch keine Bewertungen
- Ake Quick Action If Someone Is Choking On A Swallowed ObjectDokument29 SeitenAke Quick Action If Someone Is Choking On A Swallowed ObjectYAMINIPRIYANNoch keine Bewertungen
- Recent Advances in Diagnosis, Treatment and Prevention of Hepatocellular Carcinoma (HCC)Dokument65 SeitenRecent Advances in Diagnosis, Treatment and Prevention of Hepatocellular Carcinoma (HCC)amal.fathullahNoch keine Bewertungen