Beruflich Dokumente
Kultur Dokumente
Obstructive Sleep Apnea Syndrome: Diagnosis and Management: A B S T R A C T
Hochgeladen von
safwand90Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Obstructive Sleep Apnea Syndrome: Diagnosis and Management: A B S T R A C T
Hochgeladen von
safwand90Copyright:
Verfügbare Formate
C
L I N I C A L
R A C T I C E
Obstructive Sleep Apnea
Syndrome: Diagnosis
and Management
Reginald H.B. Goodday, DDS, MSc,
FRCD(C)
David S. Precious, DDS, MSc,
FRCD(C )
Archibald D. Morrison, DDS, MSc,
FRCD(C)
Chad G. Robertson,
DDS
A b s t r a c t
Increased awareness that changes in sleeping habits and daytime behaviour may be attributable to obstructive
sleep apnea syndrome (OSAS) has led many patients to seek both information and definitive treatment. The purpose
of this article is to provide information to dentists that will enable them to identify patients who may have OSAS
and to assist these patients in making informed decisions regarding treatment options. In patients who have
identifiable anatomic abnormalities of the maxilla and mandible resulting in a narrow pharyngeal airway,
orthognathic surgery appears to be an excellent treatment option.
MeSH Key Words: sleep apnea, obstructive/diagnosis; sleep apnea, obstructive/surgery
Preval
ence
n increasing number of people are
realizing that changes in their sleeping
habits and daytime behav- iour may be
attributable to obstructive sleep apnea
syndrome (OSAS). This new awareness has
led many patients to seek both information
and definitive treatment. Because the jaws
and related structures influence the development of this syndrome, dentists play an
important role in both identifying patients
who should be assessed by sleep specialists
and instituting treatment in selected cases.
The purpose of this article is to provide
information to dentists that will enable them
to identify patients who may have OSAS and
to assist these patients in making informed
decisions regarding treatment options.
OSAS is characterized by repetitive
episodes of upper airway obstruction that
occur during sleep usually in asso- ciation
with a reduction in blood oxygen
saturation.1 The prevalence of OSAS in the
middle-aged population (30 to
60 years) is 4% in men and 2% in women. 2
However, prevalence rises dramatically
with age, to an estimated
28% to 67% for elderly men and 20% to
54% for elderly women.3
J Can Dent Assoc 2001; 67(11):652-8
This article has been peer reviewed.
Clinical Manifestations
The clinical manifestations of OSAS are
related to obstruction of the upper airway,
fragmented sleep, and the respiratory and
cardiovascular consequences of disordered
breathing. Excessive daytime somnolence is a
key feature of OSAS resulting from disrupted
sleep. Patients may report that they frequently
fall asleep during the day while driving,
working, reading and watching television.4
Thus, perform- ing activities related to
transportation or the use of machin- ery and
heavy equipment can put both the patient and
December 2001, Vol. 67, No. 11
others at significant risk of injury.5,6 Chronic
daytime sleepiness also leads to poor work
performance and decreased productivity.
Snoring, ranging in severity from mild to
extremely loud, is invariably present. The
partners of people with OSAS may witness
gasping, choking or periods of apnea, with
repeated arousals through the night. In many
cases these symptoms are significant enough
that the partner sleeps in another room.
When questioned in the morning the patient
is usually unaware of the frequency of
arousals. Other complaints include a feeling
of not being rested despite a full night of
sleep, dry mouth, morning headaches,
absence of dreams, fatigue, decreased libido
and symptoms of depression.
Journal of the Canadian Dental Association
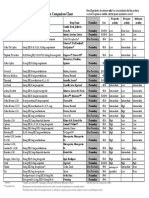
Figure 1a: Lateral cephalometric radiograph of a patient with
obstruc- tive sleep apnea syndrome (OSAS) indicates the narrow
anteroposte- rior dimension of the pharyngeal airway at the level of
the soft palate and the base of tongue (arrows).
The respiratory consequences of OSAS are
related to the extent of hypoxemia and
hypercapnia that develop as a result of the
disordered breathing. Advanced cases of
OSAS are associated with pulmonary
hypertension, corpulmonale, chronic carbon
dioxide retention and poly- cythemia.7 The
cardiovascular consequences of OSAS may
include systemic hypertension, cardiac
arrhythmias, myocardial infarction, and
cerebral vascular accidents, all of which lead
to a higher mortality rate than in the general
population.8,9
Clearly, OSAS can be a debilitating and
potentially life- threatening condition. Thus,
both proper diagnosis and appropriate
treatment are important.
Diagnostic Tools
The dental office can play an important
role in screen- ing patients who may have
OSAS by including 2 questions on the
medical questionnaire: Do you snore
loudly? Do you have difficulty staying awake
when you are inactive (e.g., while reading,
watching television or driving)? A posi- tive
response to these 2 questions should lead
the dentist to suspect OSAS. Additional
questions should then be asked to help
identify the extent of the problem: Has your
part- ner witnessed pauses in your breathing
Figure 1b: Postoperative lateral cephalometric radiograph of the
same patient after maxillomandibular advancement. Note the significant increase in the pharyngeal airway space at the level of the soft
palate and the base of tongue.
while you are asleep? Have you fallen asleep in
a potentially dangerous situation? Has your
work
performance
suffered?
Has
your
concentra- tion, memory or mood been
affected?
If the history supports the diagnosis of OSAS,
the patient should be referred to a sleep
disorders laboratory for
Obstructive Sleep Apnea Syndrome: Diagnosis and
overnight polysomnography, the objective
method of estab- lishing the diagnosis and
assessing
the
potential
success
of
treatment. The most important variables
used in determin- ing the presence and
severity of OSAS are the apnea index, the
hypopnea
index,
the
respiratory
disturbance index (RDI) and the lowest
oxyhemoglobin saturation.10 Apnea is
defined as cessation in air flow for 10
seconds or more, and the apnea index is
the number of apneic episodes occurring in
a 1-hour period.11 Hypopnea has been
defined as a 50% reduction in tidal volume
for more than 10 seconds, and the
hypopnea index is the number of
hypopneic episodes in a 1-hour period.11
The RDI is defined as the number of
apneic and hypopneic episodes per hour of
sleep.11
The
lowest
oxyhemoglobin
Management
saturation
is simply the lowest oxygen
saturation measured by pulse oximetry
during the study. OSAS is diagnosed if the
RDI reaches a certain threshold level,
typically 5 or 10.3,11 OSAS becomes clinically significant when the RDI is greater than
20 and oxygen desaturation events fall to
a level below 80% to 85%.12
Caus
es
Obstructive sleep apnea can be caused by
an anatomic abnormality that narrows or
obstructs the airway. Investigations to
localize the site of functional obstruction in
the upper airway have shown that there is
rarely a single site of occlusion. Obstruction
more commonly occurs at multiple levels of
the upper airway during episodes of
hypopnea and apnea13 (Figs. 1a, 1b).
Figure 2: Preoperative photograph of the patient depicted in Figure
1. Patients without a clinically obvious facial deformity may
benefit from maxillomandibular advancement. As this photograph
indicates, patients with OSAS may not be obese.
In any patient, upper airway patency is
maintained
through
many
interrelated
anatomic and physiologic factors.14 Normally,
negative intrapharyngeal pressure devel- ops
during inspiration. Collapse of the airway is
prevented by the action of the pharyngeal
abductor and dilator muscles. The pharynx
consists of 3 segments: the naso- pharynx,
the oropharynx and the hypopharynx. The
muscles become hypotonic during sleep, and
airway stability becomes dependent
on
pharyngeal size and pharyngeal tissue
compliance in these 3 segments.14,15 If the
compliance of the soft tissues in the narrowed
segments of the passive airway is inadequate
to offset the negative intraluminal pres- sure
created during inspiration, airway obstruction
occurs. As a result, the central nervous
system adjusts to a lighter level of sleep by
increasing muscle tone to allow opening of
the airway and resumption of the breathing
cycle.
Once the diagnosis of OSAS has been
confirmed but before treatment is instituted,
upper airway imaging is often performed to
obtain additional information regarding the
anatomy of the airway. For example, clinical
examination does not always reveal a gross
facial deformity (Fig. 2), but cephalometric
radiography can help in determining the
Figure 3: Lateral cephalometric radiograph of a patient with OSAS
who underwent uvulopalatopharyngoplasty demonstrates a thick,
bulbous soft palate (arrow) associated with a narrow
nasopharyngeal airway.
anatomic factors contributing to OSAS.
This information can then be used to direct
treatment, particularly surgery, and may
lead to more predictable treatment
outcomes. Studies involving cephalometric
radiography in patients with OSAS have
demonstrated that these patients have
smaller
retropositioned
mandibles,
narrower posterior airway spaces, and
larger tongues and soft palates than
control patients, as well as inferiorly positioned
hyoid bones and retropositioned maxillae.16
Management
OSAS can be managed nonsurgically or
surgically. The treatment should target the
potential contributing factors identified by the
history, the physical examination and upper
airway imaging. The severity of the patients
condition must also be considered in developing
a treatment plan.
Nonsurgical Management
Because obesity is a risk factor for OSAS, a
reduction in body weight can reduce sleep
apnea.17,18 However, the patient may have
difficulty losing weight, particularly in more
severe cases, because excessive daytime
somnolence and fatigue may discourage the
patient from exercising. The severity of the
OSAS may have to be reduced through some
other form of treatment before an exercise
program can be started. It is important to
note, however, that many patients with OSAS
are not obese (Fig. 2).
The most successful nonsurgical treatment
is continuous positive airway pressure
(CPAP). The use of CPAP in the treatment of
OSAS was first described in 1981.19 Since
then it has become the gold standard in the
treatment of this condition.10
However,
because of physical discomfort asso- ciated
with wearing the unit, drying of the nasal and
oral mucosal membranes, dislodgement
during
sleep,
noise
and
the
social
consequences of using the unit, compliance
may be as low as 46%.20
Oral appliances can also be used in the
treatment of OSAS.21 A review of 20 studies,
involving a total of 304 patients, revealed
that oral appliances were effective in 51% of
cases, as defined by achievement of an RDI
of less than
10.22
In 2 studies that compared oral
appliances for mandibular advancement with
CPAP, the oral appliances were effective in
mild to moderate cases but were less effective than nasal CPAP in more severe
cases.23,24 In both these studies the patients
strongly preferred the oral appliance over
nasal CPAP for reasons of comfort. The most
signifi- cant negative long-term effects of oral
appliances are temporomandibular joint
problems and movement of teeth.25-27 Tooth
movements may result in a posterior open
bite and decreased anterior overjet.21
Other nonsurgical treatments for OSAS
include medica- tions such as protriptyline
and medroxyprogesterone. Protriptyline, a
tricyclic antidepressant, has shown reasonable symptomatic improvement of OSAS and
may
reduce
the
degree
of
oxygen
desaturation, but anticholinergic side effects
and incomplete efficacy limit its use.7
Medroxy- progesterone has limited value in
the treatment of OSAS but it may be effective
in cases of obesity hypoventilation syndrome
with chronic hypercapnia.7
Surgical
Management
Tracheostomy was the first successful
surgical treatment for
OSAS.
It
was
introduced for this purpose in the
1970s.28 This procedure, which bypasses the
upper airway, is successful in virtually 100%
of cases.29 Complications associated with
tracheostomy include hemorrhage, recurrent infections, airway granulations, and
tracheal or stomal stenosis.29 The medical
and obvious social problems asso- ciated
with tracheostomy have stimulated the
search for alternatives.7
Fujita and others30 first described the use
of the uvulopalatopharyngoplasty (UPPP) for
the treatment of OSAS in 1981. This
procedure involves shortening the soft
palate, amputating the uvula, and removing
redundant lateral and posterior pharyngeal
wall mucosa from the oral pharynx. Despite
the popularity of this procedure, reviews
have reported improvement in less than 50%
of patients and complete control of OSAS
in 25% or less.31,32
Postoperative
lateral
cephalometric
radiographs of patients who have undergone
UPPP and whose symptoms persist reveal that
the soft palate has been shortened but is much
thicker,
which
results
in
a
narrow
nasopharyngeal
airway
(Fig.
3).
The
unsatisfactory results obtained with UPPP have
contributed to the realization that there are
usually multiple sites of obstruction in the
upper airway. When patients are selected on
the
basis
of
retropalatal
obstruction
demonstrated by computed tomography during
wakeful- ness or by catheter measurements of
nasal pharyngeal pressure, the success rate of
UPPP is only 50%.16
UPPP also carries a risk of significant
hemorrhage,
and
patients
report
substantial postoperative pain, which may
last
for
an
extended
period.
Velopharyngeal
insufficiency
and
nasophyaryngeal
stenosis
may
also
complicate UPPP.10
Use of orthognathic surgery to treat
OSAS began toward the end of the 1970s,
when
mandibular
advancement
was
reported to have reversed the symptoms
of OSAS.33,34 Since then, this procedure
has become widely accepted.11,35-42
Orthognathic treatment for OSAS may
involve advance- ment of the maxilla,
mandible or chin (Fig. 4). These 3
procedures can be performed in any
combination, but advancement of the
maxilla and the mandible, with or without
advancement genioplasty, is the most
common procedure. The treatment plan is
based
on
craniofacial
cephalometric
analysis, which determines whether the
position of the maxilla, mandible and chin
are normal or abnormal. The architectural
and structural craniofacial analysis of
Delaire43 allows precise planning of the
surgical advancement to maximize the
increase in pharyngeal dimensions while
maintaining normal facial balance.
Hochban and others35 reported a series
of 38 consecu- tive patients with OSAS
treated by 10 mm maxillo- mandibular
advancement. Patients were selected on
the basis of the results of lateral
cephalometric radiography; those who had
pharyngeal narrowing, with or without
retrognathic mandibles, were offered the
procedure.
Polysomnographic
sleep
studies were performed preopera- tively
and 2 months after surgery. In 37 of the 38
patients, postoperative RDI was reduced to
below 10.
Waite
and
others44
performed
maxillomandibular
advancement in 23
patients with obstructive sleep apnea. All of
the patients had preoperative RDI of greater
than 20 and some form of craniofacial
deformity. Adjunctive procedures such as
partial turbinectomy, septal reconstruction
and advancement genioplasty were also
performed, depending on individual variation.
Sleep studies were performed and lateral
cephalometric measurements obtained 1 and
6 weeks after surgery. Surgical success,
defined as RDI of less than
10, was 65%, although 96% of the patients
showed both subjective and objective
improvement.
Goodday
and
others45
compared
preoperative
and
postoperative
cephalometric radiographs in 25 consecutive
patients who had undergone orthognathic
surgery for the treatment of OSAS. The
median increase in the distance between the
posterior pharyngeal wall and the soft palate
was
100%. Similarly, the median increase in the
distance between the posterior pharyngeal
wall and the base of tongue was
81%. These findings help explain why
selected patients experience improvement
after orthognathic surgery.
Robertson
and
others46
studied
subjective
outcomes
after
maxillomandibular advancement for the
treatment of OSAS. Twenty-four patients
completed a questionnaire a mean of 24
months after surgery. They reported an
Figure 4a: Preoperative photograph of a patient with OSAS.
Figure 4b: Postoperative photograph of the same patient 6 months
after maxillomandibular advancement.
Figure 4c: Preoperative lateral cephalometric radiograph of the
same patient shows the narrow pharyngeal airway space.
Figure 4d: Lateral cephalometric radiograph of the same patient
after
maxillomandibular
advancement
shows
significant
improvement in the pharyngeal airway space.
improvement in daytime sleepiness from the
levels seen in patients with severe OSAS to
levels similar to those seen in normal
controls. Statistically significant reductions
were observed in the number of patients
reporting
problems
with
memory,
concentration and stress. Of patients who
snored preoperatively, 45% stopped snoring
and 45% reported a reduction in snoring
severity.
Compliance is not a factor in the success
of orthognathic
surgery as it is for CPAP and oral appliances.
Relative
to
tracheostomy
and
CPAP,
orthognathic surgery is more socially accepted.
It is also more successful in treating severe
OSAS than UPPP and oral appliances. Recent
studies
have
demonstrated
significant
improvements in OSAS symp- toms in
patients who have undergone orthognathic
surgery, and this procedure is associated with
a high level of patient satisfaction and low
risk.47
Conclusions
OSAS is a common condition associated
with significant
morbidity and mortality. It is therefore
important that
dental professionals be aware of the signs
and symptoms of
OSAS, so that the diagnosis can be
confirmed and treatment initiated as soon as possible. As
knowledge about the
pathophysiology of OSAS improves,
treatments may be
designed to address the specific causes of
the condition. In
patients with identifiable anatomic
abnormalities of the
maxilla and mandible resulting in a narrow
pharyngeal
airway, orthognathic surgery appears to be
an excellent
treatment option. C
Dr. Goodday is associate professor and head, division of oral and
maxillofacial surgery, Dalhousie University.
Dr. Precious is professor and chair, department of oral and
maxillofa- cial sciences, Dalhousie University; head, department of
maxillofacial surgery, Queen Elizabeth II Health Sciences Centre
(Victoria General Hospital) and director of the 6-year MD/MSc
graduate oral and maxillofacial surgery programme, Dalhousie
University.
Dr. Morrison is an assistant professor of oral and maxillofacial
surgery, Dalhousie University.
Dr. Robertson is a resident in oral and maxillofacial surgery,
Dalhousie University.
Correspondence to: Dr. Reginald H.B. Goodday, Division of
Oral and Maxillofacial Surgery, Dalhousie University, Halifax, NS
B3H 3J5. E-mail: reginald.goodday@dal.ca.
The authors have no declared financial interest.
References
1. Diagnostic Classifications Steering Committee:
The international
classification system of sleep disorders diagnostic and
coding manual.
Rochester, MN: American Sleep Disorders Association,
1990.
2. Young T, Palta M, Dempsey J, Skatrud J, Weber S,
Badr S. The occurrence of sleep-disordered breathing in middle-aged
adults. N Engl J Med
1993; 328(17):1230-5.
3. Goodday RH. Nasal respiration, nasal airway
resistance, and obstructive sleep apnea syndrome. Oral Maxillofac Surg Clin
North Am 1997;
9(2):167-77.
4. Bahammam A, Kryger M. Decision making in
obstructive sleep-
disordered breathing: putting it all together. Otolaryngol
Clin North Am
1999; 32(2):333-48.
5. Findley LJ, Fabrizio MM, Knight H, Norcross BB, LaForte
AJ, Surratt
PM. Driving simulated performance in patients with sleep
apnea. Am Rev
Respir Dis 1989; 140(2):529-30.
6. George CF, Boudreau AC, Smiley A. Simulated driving
performance
in patients with obstructive sleep apnea. Am J Respir Crit
Care Med 1996;
154(1):175-81.
7. Wiggins RV, Schmidt-Nowara WW. Treatment of the
obstructive sleep
apnea syndrome. West J Med 1987; 147(5):561-8.
8. He J, Kryger MH, Zorick FJ, Conway W, Roth T. Mortality
and apnea
index in obstructive sleep apnea. Experience in 385 male
patients. Chest
1988; 94(1):9-14.
9. Shepard JW Jr. Hypertension, cardiac arrhythmias,
myocardial infarction, and stroke in relation to obstructive sleep apnea.
Clin Chest Med
1992; 13(3):437-58.
10. Troell RJ, Riley RW, Powell NB, Li K. Surgical
management of the
hypopharyngeal airway in sleep disordered breathing.
Otolaryngol Clin
North Am 1998; 31(6):979-1012.
11. Riley RW, Powell NB, Guilleminault C. Maxillary,
mandibular, and
hyoid advancement for treatment of obstructive sleep
apnea: a review of
40 patients. J Oral Maxillofac Surg 1990; 48(1):20-6.
12. Riley RW, Powell N, Guilleminault C. Current
surgical concepts for treating obstructive sleep
apnea syndrome. J Oral Maxillofac Surg 1987;
45(2):149-57.
13. Guilleminault C, Hill MW, Simmons FB, Dewent WC.
Obstructive
sleep apnea: electromyographic and fiberoptic studies.
Exp Neurol 1978;
62(1):48-67.
14. Remmers JE, DeGroot WJ, Sauerland EK, Anch AM.
Pathogenesis
of upper airway occlusion during sleep. J Appl Physiol
1978; 44(8):931-8.
15. Lowe AA, Santamaria JD, Fleetham JA, Price C. Facial
morphology
and obstructive sleep apnea. Am J Orthod
Dentofacial Orthop 1986;
90(6):484-91.
16. Schwab RJ, Goldbert AN. Upper airway assessment:
radiographic
and other imaging techniques. Otolaryngol Clin
North Am 1998;
31(6):931-68.
17. Loube DI, Loube AA, Mitler MM. Weight loss for
obstructive sleep
apnea: the optimal therapy for obese patients. J Am
Diet Assoc 1994;
94(11):1291-5.
18. Strobel RJ, Rosen RC. Obesity and weight loss in
obstructive sleep
apnea: a critical review. Sleep 1996; 19(2):104-15.
19. Sullivan CE, Issa FG, Berthon-Jones M, Eves L.
Reversal of obstructive sleep apnea by continuous positive airway pressure
applied through
the nares. Lancet 1981; 1(8225):862-5.
20. Sanders MH, Gruendl CA, Rogers RM. Patient
compliance with
nasal CPAP therapy for sleep apnea. Chest 1986;
90(3):330-3.
21. Millman RP, Rosenberg Cl, Kramer NR. Oral
appliances in the treatment of snoring and sleep apnea. Otolaryngol Clin
North Am 1998;
31(6):1039-48.
22. Schmidt-Nowara W, Lowe A, Wiegand L,
Cartwright R, PerezGuerra F, Menn S. Oral appliances for the treatment
of snoring and
obstructive sleep apnea: a review. Sleep 1995;
18(6):501-10.
23. Clark GT, Blumenfeld I, Yoffe N, Peled E, Lavie P. A
crossover study
comparing the efficacy of continuous positive airway
pressure with
anterior mandibular positioning devices on patients
with obstructive
sleep apnea. Chest 1996; 109(6):1477-83.
24. Ferguson KA, Ono T, Lowe AA, Keenan SP, Fleetham
JA. A randomized crossover study of an oral appliance vs nasalcontinuous positive
airway pressure in the treatment of mild-moderate
obstructive sleep
apnea. Chest 1996; 10(5)9:1269-75.
25. Panula K, Keski-Nisula, K. Irreversible alteration in
occlusion caused
by a mandibular advancement appliance: an unexpected
complication of
sleep apnea treatment. Int J Adult Orthodon
Orthognath Surg 2000;
15(3):192-6.
26. Clark GT, Sohn JW, Hong CN. Treating obstructive sleep
apnea and
snoring: assessment of an anterior mandibular positioning
device. J Am
Dent Assoc 2000; 131(6):765-71.
27. Bloch KE, Iseli A, Zhang JN, Xie X, Kaplan V, Stoeckli
PW, and
other. A randomized, controlled crossover trial of two oral
appliances for
sleep apnea treatment. Am J Respir Crit Care Med 2000;
162(1):246-51.
28. Fee WE Jr, Ward PH. Permanent tracheostomy: a
new surgical
technique. Ann Otol Rhinol Laryngol 1977; 86(5 Pt 1):635-8.
29. Mickelson SA. Upper airway bypass surgery for
obstructive sleep
apnea syndrome. Otolaryngol Clin North Am 1998;
31(6):1013-23.
30. Fujita S, Conway W, Zorick F, Roth T. Surgical correction
of anatomic
abnormalities of obstructive sleep apnea syndrome:
uvulopalatopharyngoplasty. Otolaryngol Head Neck Surg 1981; 89(6):923-34.
31. Guilleminault C, Hayes B, Smith L, Simmons FB.
Palatopharyngoplasty and obstructive sleep apnea: a review of 35
cases. Bull Eur
Physiopathol Respir 1983; 19(6):595-9.
32. Conway W, Fujita S, Zorick F, Sicklesteel J, Roehrs T,
Wittig R, and
other. Uvulopalatopharyngoplasty: one year follow-up.
Chest 1985;
88(3):385-7.
33. Bear SE, Priest JH. Sleep apnea syndrome: correction
with surgical
advancement of the mandible. J Oral Surg 1980; 38(7):5439.
34. Kuo PC, West RA, Bloomquist DS, McNeil RW. The
effect of
mandibular osteotomy in three patients with hypersomnia
sleep apnea.
Oral Surg Oral Med Oral Pathol 1979; 48(5):385-92.
35. Hochban W, Conradt R, Brandenburg U, Heitmann J,
Peter JH.
Surgical maxillofacial treatment of obstructive sleep apnea.
Plast Reconstr
Surg 1997; 99(3):619-26.
36. Riley RW, Powell NB, Builleminault C. Obstructive
sleep apnea
syndrome: a review of 306 consecutively treated
surgical patients.
Otolaryngol Head Neck Surg 1993; 108:117-25.
37. Powell NB, Riley RW. Obstructive sleep apnea:
orthognathic surgery
perspectives, past, present, and future. Oral Maxillofac
Surg Clin North
Am 1990; 2(4):843-56.
38. Powell NB, Riley RW, Guilleminault C. Maxillofacial
surgery for
obstructive sleep apnea. In: Partinan M,
Guilleminault C, editors.
obstructive sleep apnea syndrome: clinical research
and treatment.
New York: Raven Press; 1989. p. 153-82.
39. Riley RW, Powell NB, Guilleminault C. Obstructive
sleep apnea
syndrome: a surgical protocol for dynamic upper
airway reconstruction.
J Oral Maxillofac Surg 1993; 51(7):742-7.
40. Riley RW, Powell NB, Guilleminault C. Maxillofacial
surgery and
nasal CPAP. A comparison of treatment for
obstructive sleep apnea
syndrome. Chest 1990; 98(6):1421-5.
41. Riley RW, Powell NB, Guilleminault C, Nino-Murcia
G. Maxillary,
mandibular, and hyoid advancement: An alternative to
tracheostomy in
obstructive sleep apnea syndrome. Otolaryngol Head
Neck Surg 1986;
94(5):584-8.
42. Waite PD, Wooten V, Lachner J, Guyette RF.
Maxillomandibular
advancement surgery in 23 patients with
obstructive sleep apnea
syndrome. J Oral Maxillofac Surg 1989; 47(12):1256-61.
43. Delaire J, Schendel SA, Tulasne JF. An architectural
and structural
craniofacial analysis: a new lateral cephalometric
analysis. Oral Surg Oral
Med Oral Pathol 1981; 52(3):226-38.
44. Waite PD, Wooten V, Lachner J, Guyette RF.
Maxillomandibular
advancement surgery in 23 patients with
obstructive sleep apnea
syndrome. J Oral Maxillofacial Surg 1989; 47(12):125661.
45. Goodday RH, Precious DS, Morrison A, Robertson C.
Post-surgical
pharyngeal airway changes following orthognathic
surgery in OSAS
patients. J Oral Maxillofac Surg 1999; 57(8)Suppl. 1:80.
46. Robertson CG, Goodday R, Precious D, Morrison A,
Shukla S.
Subjective evaluation of orthognathic surgical
outcomes in OSAS
patients. J Oral Maxillofac Surg 2000; 58(8)Suppl. 1:57.
47. Precious DS, Lanigan DT, editors. Oral and
Maxillofacial Surgery
Clinics of North America: Risks and Benefits of
Orthognathic Surgery.
Philadelphia: WB Saunders; 1997. 9(2):133-278.
C D A R E S
C E N T R E
O U R C E
The Resource Centre has compiled an
Information Package on Sleep Apnea.
CDA members can order the package by
contacting the Resource Centre at tel.:
1-800-267-6354 or (613) 523-1770, ext.
2223; fax: (613) 523-6574; e-mail:
info@cda-adc.ca. There is a charge of $10
(plus tax) for the package.
Das könnte Ihnen auch gefallen
- Fast Facts: Excessive Daytime Sleepiness Associated with Obstructive Sleep ApneaVon EverandFast Facts: Excessive Daytime Sleepiness Associated with Obstructive Sleep ApneaNoch keine Bewertungen
- Seminar: Amy S Jordan, David G Mcsharry, Atul MalhotraDokument12 SeitenSeminar: Amy S Jordan, David G Mcsharry, Atul MalhotraSerkan KüçüktürkNoch keine Bewertungen
- Research Paper On Obstructive Sleep ApneaDokument6 SeitenResearch Paper On Obstructive Sleep Apneaafeatoxmo100% (1)
- Sleep Apnea Term PaperDokument8 SeitenSleep Apnea Term Paperf1gisofykyt3100% (1)
- Pi Is 1089947215001434Dokument18 SeitenPi Is 1089947215001434Anonymous 0Mnt71Noch keine Bewertungen
- SAHOS y AnestesiaDokument10 SeitenSAHOS y AnestesiaEzequielNoch keine Bewertungen
- Modern Management of Obstructive Sleep ApneaVon EverandModern Management of Obstructive Sleep ApneaSalam O. SalmanNoch keine Bewertungen
- 152 Obstructive Sleep Apnoea and Anaesthesia 1Dokument6 Seiten152 Obstructive Sleep Apnoea and Anaesthesia 1Echo WahyudiNoch keine Bewertungen
- Κουτσουρελάκης ΩΡΛDokument5 SeitenΚουτσουρελάκης ΩΡΛΚουτσουρελακης ΩΡΛNoch keine Bewertungen
- State of The Art: Epidemiology of Obstructive Sleep ApneaDokument23 SeitenState of The Art: Epidemiology of Obstructive Sleep ApneaMelly NoviaNoch keine Bewertungen
- Pats 200709-155mgDokument8 SeitenPats 200709-155mgDea MaulidiaNoch keine Bewertungen
- Obstructive Sleep Apnea Research PaperDokument7 SeitenObstructive Sleep Apnea Research Paperefe8zf19100% (1)
- Jurnal OSADokument10 SeitenJurnal OSAflorensiaNoch keine Bewertungen
- Treating Obstructive Sleep Apnea Improves Essential Hypertension and Quality of LifeDokument8 SeitenTreating Obstructive Sleep Apnea Improves Essential Hypertension and Quality of Life'ArifahAhmadNoch keine Bewertungen
- Orthodontics in Obstructive Sleep Apnea Patients: A Guide to Diagnosis, Treatment Planning, and InterventionsVon EverandOrthodontics in Obstructive Sleep Apnea Patients: A Guide to Diagnosis, Treatment Planning, and InterventionsSu-Jung KimNoch keine Bewertungen
- Obstructive Sleep Apnea (OSA) - Pulmonary Disorders - MSD Manual Professional EditionDokument15 SeitenObstructive Sleep Apnea (OSA) - Pulmonary Disorders - MSD Manual Professional Editionpeterpavel112Noch keine Bewertungen
- Punjabi, 2008Dokument8 SeitenPunjabi, 2008a3llamNoch keine Bewertungen
- Obstructive Sleep Apnoea and AnaesthesiaDokument21 SeitenObstructive Sleep Apnoea and AnaesthesiajahangirealamNoch keine Bewertungen
- Management of Obstructive Sleep Apnea: A Dental Perspective: Eview RticleDokument9 SeitenManagement of Obstructive Sleep Apnea: A Dental Perspective: Eview RticleFourthMolar.comNoch keine Bewertungen
- Hypoxia and Stroke: "2% in Younger Adults, But in Healthy Older PeopleDokument3 SeitenHypoxia and Stroke: "2% in Younger Adults, But in Healthy Older PeopleJerahmeel Sombilon GenillaNoch keine Bewertungen
- Review Article Obstructive Sleep Apnea and Cardiovascular Diseases: Sad Realities and Untold Truths Regarding Care of Patients in 2022Dokument10 SeitenReview Article Obstructive Sleep Apnea and Cardiovascular Diseases: Sad Realities and Untold Truths Regarding Care of Patients in 2022Hashan AbeyrathneNoch keine Bewertungen
- Obstructive Sleep ApnoeaDokument69 SeitenObstructive Sleep ApnoeaPrasanna Datta100% (1)
- Surgicaloptionsforthe Treatmentofobstructive Sleepapnea: Jon-Erik C. Holty,, Christian GuilleminaultDokument37 SeitenSurgicaloptionsforthe Treatmentofobstructive Sleepapnea: Jon-Erik C. Holty,, Christian GuilleminaultJuan Pablo Mejia BarbosaNoch keine Bewertungen
- Surgical Management of Snoring and Obstructive Sleep Apnea: Wisconsin Medical JournalDokument5 SeitenSurgical Management of Snoring and Obstructive Sleep Apnea: Wisconsin Medical JournaladityakurniantoNoch keine Bewertungen
- Sleep Apnea White Paper Amended March 2019Dokument53 SeitenSleep Apnea White Paper Amended March 2019emanNoch keine Bewertungen
- OSA and Periop Complications 2012Dokument9 SeitenOSA and Periop Complications 2012cjbae22Noch keine Bewertungen
- OSADokument5 SeitenOSAtherese BNoch keine Bewertungen
- Cephalometric Analysis of Nonobese Snorers Either With or Without Obstructive Sleep Apnea SyndromeDokument8 SeitenCephalometric Analysis of Nonobese Snorers Either With or Without Obstructive Sleep Apnea SyndromeDiego SolaqueNoch keine Bewertungen
- Sleep Apnea Research PaperDokument9 SeitenSleep Apnea Research Paperaflbuagdw100% (3)
- Retrospective Analysis of Real-World Data For The Treatment ofDokument10 SeitenRetrospective Analysis of Real-World Data For The Treatment ofvenancioNoch keine Bewertungen
- Prov Prot 20118Dokument17 SeitenProv Prot 20118IlhamNoch keine Bewertungen
- Conference Proceedings: Obstructive Sleep Apnea: Diagnosis, Epidemiology, and EconomicsDokument13 SeitenConference Proceedings: Obstructive Sleep Apnea: Diagnosis, Epidemiology, and EconomicsMihaela-Alexandra PopNoch keine Bewertungen
- O S A A O: Bstructive Leep Pnea ND BesityDokument4 SeitenO S A A O: Bstructive Leep Pnea ND BesityBodi EkoNoch keine Bewertungen
- Demetriades 2010Dokument6 SeitenDemetriades 2010Sai Rakesh ChavaNoch keine Bewertungen
- Treatment of Obstructive Sleep Apnea With Oral Appliances: Research Open AccessDokument9 SeitenTreatment of Obstructive Sleep Apnea With Oral Appliances: Research Open AccessVinay MuppanaNoch keine Bewertungen
- Nasal Obstruction Considerations in Sleep Apnea: Mahmoud I. Awad,, Ashutosh KackerDokument7 SeitenNasal Obstruction Considerations in Sleep Apnea: Mahmoud I. Awad,, Ashutosh KackerSiska HarapanNoch keine Bewertungen
- Surgical Treatment of Snoring & Obstructive Sleep Apnoea: Review ArticleDokument10 SeitenSurgical Treatment of Snoring & Obstructive Sleep Apnoea: Review ArticleSiddharth DhanarajNoch keine Bewertungen
- Surgical Treatment of A Pattern I Obstructive Sleep Apnea Syndrome Individual - Clinical Case ReportDokument6 SeitenSurgical Treatment of A Pattern I Obstructive Sleep Apnea Syndrome Individual - Clinical Case ReportMatheus CorreaNoch keine Bewertungen
- Obstructive Sleep ApneaDokument8 SeitenObstructive Sleep ApneasinanhadeedNoch keine Bewertungen
- Association Between Breathing Route, Oxygen Desaturation, and Upper Airway MorphologyDokument6 SeitenAssociation Between Breathing Route, Oxygen Desaturation, and Upper Airway MorphologyMark Burhenne DDSNoch keine Bewertungen
- Jun Jul Page62Dokument7 SeitenJun Jul Page62Rika FitriaNoch keine Bewertungen
- Using The Pathophysiology of Obstructive Sleep Apnea To Teach Cardiopulmonary IntegrationDokument7 SeitenUsing The Pathophysiology of Obstructive Sleep Apnea To Teach Cardiopulmonary IntegrationAdiel OjedaNoch keine Bewertungen
- Respiratory Medicine CME: Athanasia Pataka, Renata L. RihaDokument7 SeitenRespiratory Medicine CME: Athanasia Pataka, Renata L. RihaalgaesNoch keine Bewertungen
- Shiffman Et Al 2021 Minimally Invasive Combined ND Yag and Er Yag Laser Assisted Uvulopalatoplasty For Treatment ofDokument8 SeitenShiffman Et Al 2021 Minimally Invasive Combined ND Yag and Er Yag Laser Assisted Uvulopalatoplasty For Treatment ofMário LúcioNoch keine Bewertungen
- JcsmJC1900562 W22pod AnsweredDokument13 SeitenJcsmJC1900562 W22pod Answeredlion5835Noch keine Bewertungen
- Sleep Apnea PresentationDokument73 SeitenSleep Apnea PresentationChad WhiteheadNoch keine Bewertungen
- Maxillomandibular Advancement For Obstructive Sleep Apnea: Kasey K. Li, DDS, MDDokument8 SeitenMaxillomandibular Advancement For Obstructive Sleep Apnea: Kasey K. Li, DDS, MDashajangamNoch keine Bewertungen
- Research Paper On Sleep ApneaDokument4 SeitenResearch Paper On Sleep Apneafvja66n5100% (1)
- Sleep Disorders in Pediatric Dentistry: Clinical Guide on Diagnosis and ManagementVon EverandSleep Disorders in Pediatric Dentistry: Clinical Guide on Diagnosis and ManagementEdmund LiemNoch keine Bewertungen
- Consequences of OSADokument11 SeitenConsequences of OSAhammodihotmailcomNoch keine Bewertungen
- Sleep Apnea in Renal Patients: Disease of The MonthDokument6 SeitenSleep Apnea in Renal Patients: Disease of The MonthwibowomustokoNoch keine Bewertungen
- Obstructive Sleep Apnoea Syndrome A Systematic Literature ReviewDokument4 SeitenObstructive Sleep Apnoea Syndrome A Systematic Literature Reviewc5nah867Noch keine Bewertungen
- Literature Review On Sleep ApneaDokument7 SeitenLiterature Review On Sleep Apneafvfj1pqe100% (1)
- DescargaDokument7 SeitenDescargaJoel DiazNoch keine Bewertungen
- Obstructive Sleep Apnoea: Definitions, Epidemiology & Natural HistoryDokument6 SeitenObstructive Sleep Apnoea: Definitions, Epidemiology & Natural HistoryRika FitriaNoch keine Bewertungen
- Updates On Definition, Consequences, and Management of Obstructive Sleep ApneaDokument7 SeitenUpdates On Definition, Consequences, and Management of Obstructive Sleep ApneapvillagranNoch keine Bewertungen
- Capitol SASODokument12 SeitenCapitol SASOClaudia ToncaNoch keine Bewertungen
- Ocular Auscultation: A ReviewDokument5 SeitenOcular Auscultation: A ReviewMihnea GamanNoch keine Bewertungen
- Pathophysiological Mechanisms and Therapeutic Approaches in Obstructive Sleep Apnea SyndromeDokument46 SeitenPathophysiological Mechanisms and Therapeutic Approaches in Obstructive Sleep Apnea SyndromeFrancisco Javier MacíasNoch keine Bewertungen
- The Science of Emotion (Harvard Medicine)Dokument28 SeitenThe Science of Emotion (Harvard Medicine)Ralphie_BallNoch keine Bewertungen
- Emotionally Focused Therapy For Couples and Childhood Sexual Abuse SurvivorsDokument19 SeitenEmotionally Focused Therapy For Couples and Childhood Sexual Abuse SurvivorsEFTcouplesNoch keine Bewertungen
- 3b. Bipolar Affective Disorder 2022Dokument53 Seiten3b. Bipolar Affective Disorder 2022mirabel IvanaliNoch keine Bewertungen
- CA Treatment Phyllodes Web AlgorithmDokument4 SeitenCA Treatment Phyllodes Web AlgorithmMuhammad SubhiNoch keine Bewertungen
- Enraf-Nonius Endolaser 422 ENDokument3 SeitenEnraf-Nonius Endolaser 422 ENRehabilitasi AwesomeNoch keine Bewertungen
- Special Topics in Pediatric NursingDokument60 SeitenSpecial Topics in Pediatric NursingRichard S. RoxasNoch keine Bewertungen
- WFWFDokument4 SeitenWFWFSantosh Kumar SinghNoch keine Bewertungen
- ALAXAN Module Part1Dokument30 SeitenALAXAN Module Part1api-19864075Noch keine Bewertungen
- Personal Statement For Master in Public Health - 2Dokument2 SeitenPersonal Statement For Master in Public Health - 2fopoku2k2100% (2)
- Treatment Plan TemplatesDokument2 SeitenTreatment Plan TemplatesShalini Dass100% (3)
- The Doctor Will Sue You NowDokument11 SeitenThe Doctor Will Sue You NowMateja MijačevićNoch keine Bewertungen
- Electrotherapy: DR Ramaiah Choudhary PhysiotherapistDokument13 SeitenElectrotherapy: DR Ramaiah Choudhary Physiotherapistvenkata ramakrishnaiahNoch keine Bewertungen
- Grounding TechniquesDokument2 SeitenGrounding TechniquesEderson Vertuan50% (2)
- CompendiumDokument3 SeitenCompendiumKhuong LamNoch keine Bewertungen
- MORAXELLADokument2 SeitenMORAXELLAMarcelo Jover RojasNoch keine Bewertungen
- Journal of Dental Problems and SolutionsDokument4 SeitenJournal of Dental Problems and SolutionsPeertechz Publications Inc.Noch keine Bewertungen
- Acute Decompensated Heart FailureDokument31 SeitenAcute Decompensated Heart Failure568563Noch keine Bewertungen
- Eating Disorders PaperDokument7 SeitenEating Disorders Paperapi-237474804Noch keine Bewertungen
- Cigna Leave Solutions® Claims Service Center P.O. Box 703509 Dallas, TX 75370Dokument13 SeitenCigna Leave Solutions® Claims Service Center P.O. Box 703509 Dallas, TX 75370Jose N Nelly GarciaNoch keine Bewertungen
- A Development of Freudian Metapsychology For Schisophrenia Artaloytia2014Dokument26 SeitenA Development of Freudian Metapsychology For Schisophrenia Artaloytia2014Fredy TolentoNoch keine Bewertungen
- Contraceptive Comparison ChartDokument1 SeiteContraceptive Comparison ChartdryasirsaeedNoch keine Bewertungen
- Acca Toolkit 2018Dokument212 SeitenAcca Toolkit 2018daltonngangi100% (3)
- Cpi Final Assessment ErmcDokument9 SeitenCpi Final Assessment Ermcapi-528037163Noch keine Bewertungen
- All Other NZ McqsDokument36 SeitenAll Other NZ McqsTran Thai SonNoch keine Bewertungen
- @MedicalBooksStore 2017 Pharmaceutical PDFDokument469 Seiten@MedicalBooksStore 2017 Pharmaceutical PDFeny88% (8)
- Health Services For Older Population in ThailandDokument27 SeitenHealth Services For Older Population in ThailandTino PriyudhaNoch keine Bewertungen
- Acute Lymphoblastic LeukemiaDokument5 SeitenAcute Lymphoblastic LeukemiaernitaNoch keine Bewertungen
- BarsDokument2 SeitenBarsrichieerishiNoch keine Bewertungen
- BURNS - Concept MapDokument1 SeiteBURNS - Concept MapMayaPopbozhikova89% (9)
- NCP MyomaDokument6 SeitenNCP MyomaIzza Mae Ferrancol PastranaNoch keine Bewertungen