Beruflich Dokumente
Kultur Dokumente
GBS in Transplant Patient
Hochgeladen von
agus susantoCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
GBS in Transplant Patient
Hochgeladen von
agus susantoCopyright:
Verfügbare Formate
0041-1337/01/7108-1169/0
TRANSPLANTATION
Copyright 2001 by Lippincott Williams & Wilkins, Inc.
Vol. 71, 11691183, No. 8, April 27, 2001
Printed in U.S.A.
Transplantation
BRIEF COMMUNICATIONS
GUILLAIN-BARRE SYNDROME IN ORGAN AND BONE MARROW
TRANSPLANT PATIENTS
KETAN R. BULSARA,1,4 PEDRO W. BARON,2 J. E. TUTTLE-NEWHALL,2 PIERRE-ALAIN CLAVIEN,2 AND
JOEL MORGENLANDER 3
Divisions of Neurosurgery, Transplant Surgery, and Neurology, Departments of General Surgery and Internal Medicine,
Duke University Medical Center, PO Box 3807, Durham, North Carolina 27705
Background. Guillain-Barre Syndrome (GBS) is believed to be caused by autoimmune mechanisms that
are predominantly T-cell mediated. We report GBS in
organ transplant patients and bone marrow transplant patients, both of whom have iatrogenically suppressed T-cell function.
Methods. We reviewed the Duke University Medical
Center database from 1989 1999 for all patients who
met the criteria for GBS. There were a total of 212
patients. Of these patients, two had undergone organ
transplantation and two had undergone autologous
bone marrow transplantation.
Results. Our report supports the notion that the humoral immune system is involved in the pathogenesis
of GBS. Contrary to previous reports, however, functional recovery can occur without return of T-cell
function.
Conclusions. This suggests that in organ transplant
patients, GBS may be humorally mediated and, even
more importantly, responds well to treatment.
Guillain-Barre syndrome (GBS) is the most common cause
of acute generalized paralysis (11). Yet, to date, the pathogenesis that underlies GBS has not been firmly established
(4,5). There is considerable evidence to suggest that aberrant
immunological mechanisms underlie this disorder (6 9).
This is supported by findings that almost one-third of patients with GBS have a preceding Campylobacter jejuni infection, (14) with an associated high titer of anti-GM1 antibody titers (24) and clonal expansion of mutant CD8
hypoxanthine guanine phosphoribosyltransferase T cells
(23). Furthermore, cytomegalovirus (CMV) infection results
in the production of anti-CMV IgM that can bind a surface
determinant of a Forssman-like lipid of human peripheral
nerve myelin (15) that can lead to a polyneuropathy.
There is widespread support that a primary lymphocytic
T-cell mechanism is responsible for the inflammation associated with GBS (11). Supporters of this concept cite evidence
that activation of T-lymphocytes has been shown to correlate
with disease activity (6, 7, 8, 9). Furthermore, injections of
antimyelin T-cell lines into animal models cause GBS (16).
One view of T-lymphocyte involvement suggests that T
cells have an aberrant response to a precipitating factor (11).
The immunological mechanism, however, seems more complex. Pathological studies of patients with GBS reveal that
perineural inflammation is infrequent or a late phenomenon
(12, 23). Some clinically typical cases of GBS have shown no
evidence of lymphocytic infiltration (13). Furthermore, patients with AIDS, who have known impairment of T-lymphocyte function, can develop GBS (17, 18).
We report two patients who had successful organ transplantation and subsequently developed GBS. We also report
two patients who underwent autologous bone marrow transplantation and later developed GBS. All these patients were
iatrogenically immunocompromised. We review other reports
of GBS in immunocompromised patients and discuss the
implications of these observations.
PATIENTS AND METHODS
We reviewed the Duke University Medical Center database from
1989 1999 for all patients who had met the criteria for GBS (1).
There were a total of 212 patients. Of these patients, two had undergone organ transplantation and two had undergone autologous
bone marrow transplantation. None of these patients had evidence of
CMV infection. The organ transplant patients had good outcomes in
regard to their transplants with none of them experiencing organ
rejection.
Patients
Patient 1. P.R. was a 40-year-old patient who was status postorthotopic liver transplantation in June 1997. In October 1997, she
developed ascending muscular weakness and paresthesias. Physical
examination revealed 4/5 muscle strength in all tested groups. Her
reflexes were absent. Her albumin level was 3.8 g/dL. Cerebrospinal
fluid examination revealed protein of 78 mg/dL, glucose of 76 mg/dL,
and no cells. Her nerve conduction and EMG studies showed evidence of an acute proximal demyelinating neuropathy. She was
1
Division of Neurosurgery.
treated with a five-day course of intravenous immunoglobulins
2
Division of Transplant Surgery.
(IVIG) (0.4 g/kg/day; total 140 g) with near complete resolution of her
3
Division of Neurology.
symptoms. She had a relapse of her symptoms in December 1997.
4
Address correspondence to: Ketan R. Bulsara, MD, Duke Uni- She once again responded well to a three-day course of IVIG (0.4
versity Medical Center, Division of Neurosurgery, PO Box 3807, g/kg/day; total 84 g). Her neoral level was well within therapeutic
Durham, North Carolina 27705.
levels. She was also taking prednisone. At her two-year follow-up,
1169
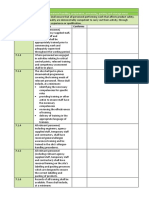
GBS 1 yr
GBS 2 wk
AIDS
AIDS
cardiac
liver
cadaveric
renal
bone marrow
bone marrow
30-year-old male (Qureshi et al.)
33-year-old male (Qureshi et al.)
66-year-old male (Qureshi et al.)
40-year-old female
53-year-old male
7-year-old male
7-year-old female
GBS 1 mo
GBS 4 mo
GBS 3 yr
unknown date
of diagnosis
unknown date
of diagnosis
GBS 3 mo
cardiac
62-year-old male (Baldwin et al.)
rejection 1 mo
GBS 3 mo
GBS 3 mo
Clinical Course
61-year-old male (Baldwin et al.)
Transplant
cadaveric
renal
cardiac
40-year-old male (Bale et al.)
Age
not reported
not reported
not reported
patient ()
donor ()
patient ()
donor ()
not reported
patient ()
patient ()
not reported
patient ()
not reported
patient ()
donor ()
patient ()
donor ()
patient ()
patient ()
positive
Posttransplant
patient ()
patient ()
Pretransplant
CMV
IVIG
IVIG
IVIG
IVIG
plasmapheresis
IVIG
plasmapheresis
IVIG and
plasmapheresis
and ganciclovir
IVIG and
plasmapheresis
not reported
Treatment
TABLE 1. Reported cases of GBS in organ and bone marrow transplant patients
full functional recovery
by 4 yr
full functional recovery
by 9 yr
almost full functional
recovery by 2 yr
improvement but
persistent
neurological deficits
1 yr
improvement but
persistent difficulty
ambulating
improvement but
difficulty ambulating
full functional recovery
by 2 yr
almost complete
functional recovery
by 4 mo
full functional recovery
within 4 mo
not reported
Outcome
1170
TRANSPLANTATION
Vol. 71, No. 8
April 27, 2001
1171
BRIEF COMMUNICATIONS
she had full strength in all of her extremities with trace reflexes. She
has continued on neoral and prednisone.
Patient 2. W.R. was a 53-year-old patient who underwent a cadaveric renal transplant in 1997. He was readmitted because of a
perforated diverticulum one year later. He was having an uneventful
recovery when he began to develop extremity weakness. Physical
examination revealed 3/5 muscle strength in all tested groups. His
reflexes were absent. EMG and nerve conduction studies showed
evidence of an acute proximal demyelinating neuropathy. His albumin level was 3.0 g/dL and total protein was 7.0 g/dL. Cerebrospinal
fluid examination revealed protein of 117 mg/dL, glucose of 55 mg/
dL, 4 nucleated cells, and 1 red blood cell. He had a therapeutic
neoral level. Patient was also taking prednisone. He was treated
with a five-day course of IVIG (0.4 gm/kg/day; total 140 g). He has
had gradual improvement of his symptoms to the point that he is
currently self-ambulatory.
Patient 3. B.C. was a 7-year-old patient who was diagnosed with
acute myelogenous leukemia. In January 1995, he was treated with
busulfan and melphalan. He was readmitted to the hospital for
treatment of Gram-negative sepsis when five days later, he developed ascending muscle weakness (4/5 diffusely). He was areflexic.
EMG and nerve conduction studies showed evidence of an acute
proximal demyelinating neuropathy. He was treated with two fiveday courses of IVIG (0.2 gm/kg/day; total 16 g each total therapy) and
was discharged home with home physical therapy and occupational
therapy. At his four-year follow-up visit, he had made excellent
functional recovery.
Patient 4. L.J. was a 7-year-old patient who was diagnosed with
PreB-cell acute lymphocytic leukemia in December 1990. She was
treated with methotrexate, Cytabarine, prednisone, vincristine, and
L-asparagine. She underwent autologous bone marrow transplantation. Approximately one month later, she developed lower extremity
weakness that subsequently involved her upper extremities (4/5
diffusely). She was areflexic. Her nerve conduction study and EMG
disclosed severe sensorimotor neuropathy with demyelinating features. She was treated with a five-day course of IVIG (0.4 gm/kg/day;
total 17.5 g). She had made an excellent functional recovery at her
nine-year follow-up visit.
DISCUSSION
At the onset, it is important to emphasize that GBS is a
complex autoimmune disease with many unanswered questions at both the clinical and laboratory levels. The possibility that the pathogenesis of this disorder is variable depending on the clinical situation cannot be excluded (21). All of the
patients in this study were iatrogenically immunosuppressed. When their immunosuppression regimen is considered, however, it is readily apparent that, though not absolute, the cell-mediated branch of the immune system was
most suppressed. A similar trend is noted when reviewing
previously reported cases of GBS in transplant patients (2, 3,
18) (Table 1). In reviewing the literature, it seems that male
patients are predominantly affected and that the onset of
GBS occurs within 3 months of transplant in the majority of
patients. Although previous reports have suggested a causal
role for CMV infection in the occurrence of GBS, we did not
find this to be the case in our patients. Furthermore, although both high-dose gamma globulin treatment and plasmapheresis have been used successfully to treat these patients, it appears that plasmapheresis is emerging as the
preferred treatment modality (20). Thus, it is clear from the
limited population of transplant patients that it is difficult to
establish a definitive mechanism for the pathology.
When our case series is coupled with previously reported
series, it questions the widely held notion that the resolution
of GBS correlates with the return of T-suppressor cell function (2, 3, 18). Patients with AIDS and documented absence
of T-cell function recover from GBS in a time course similar
to that of transplant patients with partially suppressed T-cell
function (Table 1). Thus, it appears that the return of Tsuppressor cell activity is not primarily responsible for the
resolution of GBS.
Mounting evidence suggests that humoral autoimmune
mechanisms are also involved in the pathogenesis of GBS (2,
8). The animal models support this notion. Experimental
allergic neuritis, a close animal model of GBS, can be elicited
by sensitizing animals to the P-2 myelin antigen or its fragments (19). The experimental disease appears to be predominantly cell-mediated; it can be transferred by lymphocytes
from sensitized animals but not by serum (11). On the other
hand, a purely humoral noninflammatory demyelination is
produced by the intraneural injection of galactocerebroside or
directly by anticerebroside antibody (19).
Clinical data are consistent with findings in animal models
that a purely humoral-mediated demyelination can occur
(23). For example, patients with Hodgkins disease who lack
lymphocyte proliferation to standard antigens in in vitro
testing develop GBS (15). Furthermore, only three cases of
GBS after cardiac transplantation and only one case after
renal transplantation have been reported (2, 3, 18). Orthotopic liver transplantation has also been associated with a
3% incidence of acute polyneuropathies (10).
As has previously been reported, our bone marrow transplant patients made excellent functional recovery (22). Although it is tempting to interpret their neurological recovery
as secondary to return of T-cell function, our organ transplant patients reveal an interesting finding. Even though
these patients continued to have cell-mediated immunosuppression, they did make functional recovery. This is in contrast to the belief that T-lymphocytes are always needed for
the down-regulation of the autoimmune process (18). What it
does suggest is that GBS in transplant patients may be
humorally mediated and, more importantly, responds well to
treatment.
Acknowledgment. The authors thank Nita K. Bulsara for her assistance in the preparation of this manuscript.
REFERENCES
1. Announcement. Criteria for diagnosis of Guillain-Barre syndrome. Ann
Neurol 1978; 3(6): 565566.
2. Baldwin RT, Pierce RR, Frazier OH. Guillain-Barre syndrome after heart
transplantation. J Heart Lung Transplant 1992; 11: 817 819.
3. Bale JF Jr, Rote NS, Bloomer LC, Bray PF. Guillain-Barre like polyneuropathy after renal transplant: possible association with cytomegalovirus infection. Arch Neurol 1980; 37: 784.
4. Cornblath DR, McArthur JC, Kennedy PGE, Witte AS, Griffin JW. Inflammatory demyelinating peripheral neuropathies associated with human
T-cell lymphotropic virus type III infection. Ann Neurol 1987; 21: 32
40.
5. Feasby TE. Inflammatory-demyelinating polyneuropathy. Neurol Clin
1992; 10: 651 670.
6. Hartnup HP. Immune mediated demyelination. Ann Neurol 1993; 33:
563567.
7. Hartung HP, Pollard JD, Harvey GK, Toyka TV. Immunopathogenesis and
treatment of Guillain-Barre syndrome. Muscle Nerve 1985; 18: 137
153.
8. Hartung HP, Reiners K, Schmidt B, Stoll G, Toyka KV. Serum interleukin-2 concentration in Guillain-Barre Syndrome and chronic idiopathic
demyelinating polyradiculopathy: comparison with other neurological
diseases of preserved immunopathogenesis. Ann Neurol 1991; 30: 48
1172
TRANSPLANTATION
53.
9. Hartung HP, Stoll G, Toyka KV. Immune reactions in the peripheral
nervous system. Peripheral Neuropathy. Philadelphia: Saunders, 1993:
418 454:
10. Jann S, Santilli IM, Scarpini E, Gatti A, Bramerio MA. Peripheral nervous
system involvement after orthotopic liver transplantation [Abstract].
Neurology 1999; 52(2): A83.
11. Ropper AH. The Guillain-Barre Syndrome. The N Engl J Med 1992; 326:
1130 1136.
12. Haymaker W, Kernohan JW. The Landry-Guillain-Barre syndrome: clinicopathologic report of fifty fatal cases and a critique of the literature.
Medicine 1949; 28: 59 141.
13. Honaver M, Tharakan JKJ, Hughes RAC, Leibowitz S, Winer JB. A
clinicopathological study of the Guillain-Barre syndrome: nine cases
and literature review. Brain 1991; 114: 12451269.
14. Kaldor J, Speed BR. Gillain-Barre syndrome and Campylobacter jejuni, a
serological study. Br Med J 1984; 288: 18671870.
15. Koski CL, Chou DKH, Jungalwala FB. Antiperipheral nerve myelin antibodies in Guillain-Barre bind a neutral glycolipid of peripheral myelin
and cross react with Forssman antigen. J Clin Invest 1989; 80: 1492
1497.
16. Linington C, Izumo S, Suzuki M, Uyemura K, Meyermann R, Wekerle H.
A permanent rat T cell line that mediates experimental allergic neuritis
in the Lewis rat in vivo. J Immunol 1984; 133: 1946 1950.
17. Lisak R, Mitchell M, Zwieman B, Orrechio E, Asbury A. Guillain-Barre
syndrome and Hodgkins disease: three cases with immunological stud-
Vol. 71, No. 8
ies. Ann Neurol 1077; 1:7278.
18. Qureshi AI, Cook AA, Mishu HP, Krendel DA. Guillain-Barre syndrome in
immunocompromised patients: a report of three patients and review of
the literature. Muscle Nerve 1997; 20(8): 10021007.
19. Rumpl E, Mayr U, Gerstenbrand F, Hackl JM, Rosmanith P, Aichner F.
Treatment of Guillain-Barre syndrome by plasma exchange. J Neurol
1981; 225: 207217.
20. Saida T, Saida K, Dorfman SH, et al. Experimental allergic neuritis
induced by sensitization with galactocerebroside. Science 1979; 204:
11031106.
21. Saida K. The immunopathology of Guillain-Barre syndrome. Curr Opin
Neurol 1996; 9: 329 333.
22. Van den Berg LH, Mollee I, Wokke JHJ, Logtenberg T. Increased frequencies of HPRT mutant T-lymphocytes in patients with Buillain-Barre
syndrome and chronic inflammatory demylinating polyneuropathy: further evidence for a role of T-cells in the etiopathogenesis of peripheral
demylinating diseases. J Neuroimmunol 1995; 58: 3 42.
23. Wen P, Alyea EP, Simon D, Herbst RS, Soiffer RJ, Antin JH. GuillainBarre syndrome following allogenic bone marrow transplantation. Neurology 1997; 49: 17111714.
24. Yuki N, Yoshino H, Sato S, Miyatake T. Acute axonal polyneuropathy
associated with anti-GM1 antibodies following Campylobacter enteritis.
Neurology 1990; 40: 1900 1902.
Received 14 March 2000.
Accepted 15 August 2000.
HELICOBACTER PYLORIASSOCIATED GASTRIC MALT
LYMPHOMA IN LIVER TRANSPLANT RECIPIENTS
THOMAS M. SHEHAB,1 ERIC D HSI,2 JOHN J. POTERUCHA,3 NARESH T. GUNARATNAM,1 AND
ROBERT J. FONTANA1,4
Department of Internal Medicine, University of Michigan Medical School, Ann Arbor, Michigan 48109-0362; Department
of Clinical Pathology, Cleveland Clinic Foundation, Cleveland, Ohio 44195; and Division of Gastroenterology and
Hepatology, Mayo Clinic, Rochester, Minnesota 55905
Background. Immunosuppressed transplant recipients are at increased risk of developing several forms
of malignancy. The aim of this study is to report the
clinical presentation, treatment, and outcome of four
liver transplant recipients with Helicobacter pylori
associated gastric mucosae-associated lymphoid tissue (MALT) lymphoma.
Methods. The medical records of four liver transplant recipients with gastric MALT lymphoma were
reviewed. In situ hybridization for Epstein-Barr encoded ribonucleic acid was performed on formalinfixed tissues.
Results. All four subjects presented with abdominal
symptoms at a mean of 6.1 years posttransplant. Ulcerative lesions biopsied at endoscopy demonstrated earlystage gastric MALT lymphoma with associated Helicobacter pylori gastritis. In situ hybridization revealed no
evidence of Epstein-Barr virus infection in examined
tissues. Antibiotic eradication of Helicobacter pylori
1
Department of Internal Medicine, University of Michigan Medical School, 3912 Taubman Center, Ann Arbor, MI 48109-0362.
2
Department of Clinical Pathology, L-11, Cleveland Clinic Foundation, 9500 Euclid Avenue, Cleveland, OH 44195.
3
Division of Gastroenterology and Hepatology, Mayo Clinic, 200
First Street SW, Rochester, MN 55905.
4
Address correspondence to: Robert J. Fontana, MD, Assistant
Professor of Medicine, 3912 Taubman Center, Ann Arbor, MI
48109-0362.
lead to disease remission in three subjects with a mean
follow-up of 21 months, and one subject failed to respond
to antibiotics and radiation therapy and died from metastatic gastric adenocarcinoma.
Conclusions. Early-stage, low-grade gastric MALT
lymphoma that was associated with Helicobacter pylori gastritis responded to antibiotic therapy with a
sustained clinical remission in three of four treated
subjects. If other studies confirm a higher than expected incidence of gastric MALT lymphoma in immunosuppressed transplant recipients with Helicobacter
pylori infection, screening and treating Helicobacter
pylori infection in selected transplant patients may
prove beneficial.
Liver transplant and other solid organ transplant recipients are at increased risk of developing several malignancies
due to reduced immune surveillance (1). In addition, infection with oncogenic viruses is associated with the development of several of these posttransplant malignancies such as
Epstein-Barr virus (EBV) infection and posttransplant lymphoproliferative disorders (PTLD) and human papilloma virus infection and cervical cancer (13). Helicobacter pylori
(HP) infection of the gastric mucosae is present in 30% to 50%
of the general population and a comparable proportion of
patients with cirrhosis (4). In addition to its recognized importance in the development of peptic ulcer disease, a minor-
Das könnte Ihnen auch gefallen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (894)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (587)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (119)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2219)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Benchmark Capstone Project Change Proposal Week 8Dokument15 SeitenBenchmark Capstone Project Change Proposal Week 8Kerry-Ann Brissett-SmellieNoch keine Bewertungen
- Multiple Choice Questions - Paper 1 MCQ ExamDokument21 SeitenMultiple Choice Questions - Paper 1 MCQ ExamRobert Edwards100% (9)
- Powerplugs: Templates For PowerpointDokument2 SeitenPowerplugs: Templates For Powerpointagus susantoNoch keine Bewertungen
- Stop Service HR PDFDokument39 SeitenStop Service HR PDFagus susantoNoch keine Bewertungen
- Theme LessonDokument11 SeitenTheme LessonGiovanna AdlimNoch keine Bewertungen
- Embedded and Impacted TeethDokument2 SeitenEmbedded and Impacted TeethAhmed MawardiNoch keine Bewertungen
- Early Infant Diagnosis PDFDokument24 SeitenEarly Infant Diagnosis PDFagus susantoNoch keine Bewertungen
- Non Operative Treatment OA MadiunDokument46 SeitenNon Operative Treatment OA Madiunagus susantoNoch keine Bewertungen
- Un SMP 2017 B IngDokument14 SeitenUn SMP 2017 B IngnunikNoch keine Bewertungen
- Lagu BaratDokument3 SeitenLagu Baratagus susantoNoch keine Bewertungen
- NO Nama Tindakan Kode TindakanDokument1 SeiteNO Nama Tindakan Kode Tindakanagus susantoNoch keine Bewertungen
- OA Seminar IDIDokument68 SeitenOA Seminar IDIagus susantoNoch keine Bewertungen
- Surgery in OA: Spine, Hip, Knee Options at Dr. Soetomo HospitalDokument75 SeitenSurgery in OA: Spine, Hip, Knee Options at Dr. Soetomo Hospitalagus susantoNoch keine Bewertungen
- Hbs AbDokument1 SeiteHbs Abagus susantoNoch keine Bewertungen
- OA Seminar IDIDokument68 SeitenOA Seminar IDIagus susantoNoch keine Bewertungen
- Dr. Mirza Koeshardiandi ABC of BurnDokument35 SeitenDr. Mirza Koeshardiandi ABC of Burnagus susantoNoch keine Bewertungen
- Stop Service HR PDFDokument39 SeitenStop Service HR PDFagus susantoNoch keine Bewertungen
- What Is Hirschsprung DiseaseDokument8 SeitenWhat Is Hirschsprung Diseaseagus susantoNoch keine Bewertungen
- Handout Lagu-SurabayaDokument7 SeitenHandout Lagu-Surabayaagus susantoNoch keine Bewertungen
- Chronic ComplicationDokument41 SeitenChronic Complicationagus susantoNoch keine Bewertungen
- Dr. Mirza Koeshardiandi ABC of BurnDokument35 SeitenDr. Mirza Koeshardiandi ABC of Burnagus susantoNoch keine Bewertungen
- Acute Complication - Final1Dokument32 SeitenAcute Complication - Final1agus susantoNoch keine Bewertungen
- What Is Hirschsprung DiseaseDokument8 SeitenWhat Is Hirschsprung Diseaseagus susantoNoch keine Bewertungen
- Indications For Abilify Oral SolutionDokument2 SeitenIndications For Abilify Oral Solutionagus susantoNoch keine Bewertungen
- Tugas EBM PICO (Headache)Dokument4 SeitenTugas EBM PICO (Headache)Len-chanNoch keine Bewertungen
- Hendra P PamuktiDokument2 SeitenHendra P Pamuktiagus susantoNoch keine Bewertungen
- Hendra P Pamukti MRDokument2 SeitenHendra P Pamukti MRagus susantoNoch keine Bewertungen
- Water Borne Disease: For The Ethiopian Health Center TeamDokument96 SeitenWater Borne Disease: For The Ethiopian Health Center Teamgirma shimelisNoch keine Bewertungen
- Hazardous Materials Management Plan SMDokument26 SeitenHazardous Materials Management Plan SMdarmayunitaNoch keine Bewertungen
- Assessment of Preparedness Against Emerging Infectious Disease Among Private Hospitals in A District of South IndiaDokument5 SeitenAssessment of Preparedness Against Emerging Infectious Disease Among Private Hospitals in A District of South IndiaNurulfitrahhafidNoch keine Bewertungen
- Applying HACCP PrinciplesDokument88 SeitenApplying HACCP Principlesbbeard90% (1)
- Package Insert - API 50 CHL MediumDokument7 SeitenPackage Insert - API 50 CHL MediumMaria Dapkevicius100% (2)
- Estafilococo Aureus Patogenicidad. Virulencia 2021Dokument23 SeitenEstafilococo Aureus Patogenicidad. Virulencia 2021Gabriela ChaconNoch keine Bewertungen
- Calset CeaDokument1 SeiteCalset CeaModestusNoch keine Bewertungen
- BH00078 Huyen ASM1 RPDokument23 SeitenBH00078 Huyen ASM1 RPTrần Khánh HuyềnNoch keine Bewertungen
- DiseasesDokument11 SeitenDiseasesapi-307430346Noch keine Bewertungen
- Frequencies 171.160 Hz, 174.989 Hz, and 1185.131 Hz may help combat COVID-19Dokument28 SeitenFrequencies 171.160 Hz, 174.989 Hz, and 1185.131 Hz may help combat COVID-19Stere StereNoch keine Bewertungen
- Dengue Pregnancy PDFDokument2 SeitenDengue Pregnancy PDFSuhayatra PutraNoch keine Bewertungen
- Cbic Course Proposal 2022Dokument11 SeitenCbic Course Proposal 2022Soha GalalNoch keine Bewertungen
- Part VII - Deadly Injection: The Hidden Ingredients in VaccinesDokument19 SeitenPart VII - Deadly Injection: The Hidden Ingredients in VaccinesGary Null100% (2)
- BRC Isse 8 Clause 7Dokument6 SeitenBRC Isse 8 Clause 7jacky786Noch keine Bewertungen
- Immune System Overview - Understanding The Immune SystemDokument60 SeitenImmune System Overview - Understanding The Immune Systemlourdesbr100% (2)
- New Insights On Antiviral ProbioticsDokument126 SeitenNew Insights On Antiviral ProbioticsDevvvNoch keine Bewertungen
- Salus Silver TSL2 - FormattedDokument52 SeitenSalus Silver TSL2 - Formattedhilajo1363Noch keine Bewertungen
- Arogya Setu App Is SafeDokument3 SeitenArogya Setu App Is SafeSwastik GroverNoch keine Bewertungen
- Lesson 3.2 CoccidiosisDokument113 SeitenLesson 3.2 CoccidiosisnickswipoNoch keine Bewertungen
- ERC Panel Structure 2024 CallsDokument12 SeitenERC Panel Structure 2024 CallsjapNoch keine Bewertungen
- Test Bank For Microbiology With Diseases by Body System 3rd Edition Robert W BaumanDokument35 SeitenTest Bank For Microbiology With Diseases by Body System 3rd Edition Robert W Baumaneyeletgoober.3kvzwt98% (45)
- 4TH Year Stuide Guide Community MedicineDokument30 Seiten4TH Year Stuide Guide Community MedicineMohammad Jibran KhanNoch keine Bewertungen
- Inhibitory Effects of Ribbon Sea Lettuce (Ulva Reticulata) Extracts Against Klebsiella PneumoniaeDokument45 SeitenInhibitory Effects of Ribbon Sea Lettuce (Ulva Reticulata) Extracts Against Klebsiella PneumoniaeVanessa Marie MatutesNoch keine Bewertungen
- Proiect Formular InscriereDokument5 SeitenProiect Formular InscriereAdriana Sorina VoicilaNoch keine Bewertungen
- Biosafety in Microbiological and Biomedical LaboratoriesDokument438 SeitenBiosafety in Microbiological and Biomedical LaboratoriesRyan Cilsick100% (1)
- Myths COVIDDokument19 SeitenMyths COVIDPGNoch keine Bewertungen
- (Đề thi có 04 trang) Thời gian làm bài: 60 phút không kể thời gian phát đềDokument15 Seiten(Đề thi có 04 trang) Thời gian làm bài: 60 phút không kể thời gian phát đềhai mai ducNoch keine Bewertungen
- Detect Malaria ProtozoaDokument81 SeitenDetect Malaria ProtozoaMoses Tamba MomohNoch keine Bewertungen