Beruflich Dokumente
Kultur Dokumente
Shoulder Dislocations
Hochgeladen von
khalidaharwinCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Shoulder Dislocations
Hochgeladen von
khalidaharwinCopyright:
Verfügbare Formate
CHAPTER 196
SHOULDER DISLOCATIONS
Jeffrey V. Smith
Dislocations of the shoulder are quite common. Approximately 50%
of shoulder injuries in the emergency department are dislocations.
Anterior dislocations are far more common than posterior disloca
tions. The four types of anterior dislocations account for 96% of all
shoulder dislocations.
Of the four types of anterior dislocations, subcoracoid disloca
tions occur three times more frequently than all the others (subglen
oid, subclavicular, and thoracic) combined. This chapter deals only
with care of subcoracoid, anterior dislocations. All others should be
treated with the assistance of an orthopedic surgeon.
The shoulder is the most flexible joint in the human body; con
sequently, it is the most unstable and most commonly dislocated
joint. It is designed to enable a wide range of motion of the upper
extremity, in all directions. To accomplish this feat, the actual bony
articulation occupies only a very small part of the overall functional
area of the joint. The glenohumeral joint surface and capsule are
small sliding structures without significant fixed, ligamentous limita
tions. The tendons around the joint, making up the rotator cuff (Fig.
196-1), are the structures primarily responsible for the integrity of
the joint and its complex function.
When the normal joint capsule and rotator cuff restraints are
exceeded, the shoulder moves out of joint. Most frequently the
clinician encounters a dislocation in which the humeral head has
been pulled out of joint and is then held anteriorly and medially by
spasm of the anterior chest wall muscles. This is the subcoracoid,
anterior shoulder dislocation, usually occurring when an abducted,
extended, and externally rotated upper extremity takes a major jolt.
The resulting lever forces the proximal humerus anteriorly out of
the glenoid socket. After the humeral head comes to rest under the
coracoid process, the patient usually presents to the clinician in
extreme pain with a nonfunctional arm. Dislocations may also occur
during a seizure.
The patient will have a loss of the normal shoulder contour, with
a step-off where the deltoid muscle used to be prominent. Instead,
the acromion becomes very prominent. The contour of the humeral
head may be noted in the anterior chest wall region. Clinically, a
hollow can be appreciated beneath the acromion process, due to the
missing humeral head. The arm will frequently be held in a slightly
abducted, externally rotated posture. A neurologic deficit, most fre
quently involving the axillary nerve (provides innervation for shoul
der abduction and sensation over the deltoid), may be noted on
careful examination. Additional neurovascular compromise may be
evident, but it is uncommon with subcoracoid, anterior dislocations.
Radiographs should be obtained; it is important to determine the
presence (24% of anterior dislocations) or absence of a fracture
before attempting to reduce the shoulder. Obtain standard radio
graphs of the shoulder. A single anteroposterior (AP) view of the
shoulder will usually demonstrate the abnormal location of the
humeral head. Another view at roughly 90 degrees will not only
confirm the direction of humeral head movement, but help exclude
a fracture or posterior dislocation. A lateral transcapular or a Ytype view will provide this information; an axillary view (Fig. 196-2)
is preferred by some clinicians but it is often difficult to get the
patient to move his or her arm into the necessary position. Alter
natively, in some obese individuals, a computed tomography (CT)
scan may be necessary to determine the direction of the shoulder
dislocation and the presence of concomitant fractures.
INDICATIONS
A subcoracoid, anterior shoulder dislocation is the indication for
treatment.
CONTRAINDICATIONS
The following findings or conditions should generate an immediate
orthopedic consult:
A shoulder dislocation, other than a subcoracoid, anterior
dislocation
Any fracture dislocation of the shoulder
Dislocations that are more than a few days old (higher risk of
vascular injury, especially in older patients)
Other fractures of the shoulder, neck, ribs, or upper extremity
Prior orthopedic surgery for chronic or recurrent shoulder
dislocations
Shoulder dislocations in children (if ossification centers are not
fused, there is usually an associated Salter-Harris fracture)
A patient with neurovascular compromise (other
than mild axillary nerve sensory defect) due to shoulder dislocation
should undergo immediate reduction. Although it is beyond the
scope of this book, even inferior or posterior shoulder dislocations
should undergo immediate reduction if the distal pulse is compro
mised. Although immediate orthopedic assistance is optimal, it may
not always be possible.
EDITORS NOTE:
EQUIPMENT
AND
SUPPLIES
Stretcher
Washcloth or small towel
Soft restraints such as sheets or blankets
Cloth tape, gauze or elastic bandage, padded wrist restraint or
commercially available device for hanging weights from wrist
Weights (5 to 15lbs) or bucket ( 1 2 to 1 gallon size and adequate
tap water or intravenous [IV] fluid)
Intra-articular anesthetic (10 to 20mL of 50:50 mixture 1% or
2% lidocaine with sterile saline), antiseptic solution (e.g.,
chlorhexidine, povidoneiodine), 10- to 20-mL syringe, 25-gauge,
2 1 2 -inch needle
Procedural sedation forms, consent, equipment (see Chapter 2,
Procedural Sedation and Analgesia) and medications (e.g., anal
gesia, muscle relaxant, narcotics, benzodiazepines, reversal
agents)
Shoulder immobilizer or sling and swath
1343
1344
ORTHOPEDICS
Humeral
head
Rotator cuff
Glenoid cavity
Humerus
Clavicle
Acromion
Rotator cuff
Figure 196-1 Anatomy of the shoulder joint and how the tendons of the
muscles (supraspinatus, infraspinatus, subscapularis, and teres minor) form
the rotator cuff. Also see Chapter 185, Musculoskeletal Ultrasonography, and
Chapter 192, Joint and Soft Tissue Aspiration and Injection (Arthrocentesis).
PREPROCEDURE PATIENT PREPARATION
Patients should be informed about the indications for shoulder
reduction, as well as any alternatives and possible complications.
They should know what to expect and try to relax as much as pos
sible. If a local anesthetic injection will be used, the patient can be
reassured that this should decrease the discomfort. Informed consent
should be obtained appropriate for the procedure(s) to be performed.
PRECAUTIONS
To be successful, this procedure takes some time and relaxationon
the part of both the patient and the clinician. The procedure is easy,
but trying to rush it may result in an unsuccessful episode. One
exception is the dislocation witnessed by the sports medicine clini
cian; if the dislocation is not associated with high-energy forces,
some clinicians will reduce the shoulder immediately, fieldside,
without radiographs and before the muscular spasm can occur.
TECHNIQUE
There are a number of available techniques, all designed to apply
gentle and persistent tension on the spasmodic chest wall muscles,
to elongate them, and to reestablish the mobility of the humeral
head. Once this is done, the humeral head will usually track or be
gently manipulated back into the glenoid fossa. The patient is prob
ably best served by the simplest technique, the one that minimizes
both operator and patient stress. Typically, this is the Stimson tech
nique, wherein weight loading and time can be used to gently
stretch the muscles and reduce the joint. Certainly, this is the least
Figure 196-2 Radiographs should include a view at 90 degrees from
the anteroposterior view, such as this axillary view. Such a projection helps
document the direction (anterior vs. posterior) of the shoulder dislocation.
traumatic technique for the shoulder and should help minimize
the chances of a fracture developing related to the reduction
process.
Other techniques may also be successful. Although many have
been described in the literature, all of the listed techniques have
been tested and are effective in a situation where the clinician is
willing to take his or her time with the reduction. Experience sug
gests that the clinician should not attempt more than two reduction
procedures. If the second attempt is unsuccessful, the resultant
muscle spasm will likely prevent closed reduction in a safe manner.
Call the orthopedic surgeon if the second attempt is unsuccessful.
Intra-articular Anesthetic
Some experts recommend the injection of intra-articular anesthetic
with every shoulder reduction (see also Chapter 192, Joint and Soft
Tissue Aspiration and Injection [Arthrocentesis]). It can also be
used if procedural sedation is contraindicated.
1. Identify the hollow area where the humeral head used to be
located, 2cm (two fingerbreadths) directly inferior to the lateral
border of the now prominent acromion process. Apply antiseptic
solution to the skin over this area and allow to dry.
2. Using sterile technique, insert the 25-gauge, 2 1 2 -inch needle into
this area, perpendicular to the skin, to a depth of 2cm. Inject 10
to 20mL of a 50:50 mixture of local anesthetic and sterile saline
solution.
Stimson Technique
1. Using this technique, procedural sedation is often unnecessary;
some experts use the injected local intra-articular anesthetic.
Also, there are reports of a 96% success rate, and there is no need
for an assistant. Conversely, the prone position may be impos
sible to use because of other injuries; procedural sedation is also
not recommended because the prone position may interfere with
respiration. Procedural sedation is even relatively contraindi
cated because of the prolonged nature of this technique.
2. The patient is placed in the prone position on a stretcher with
the affected arm hanging over the side. A rolled-up washcloth or
small towel can be placed beneath the coracoid process and
pectoralis major muscle as needed for comfort. The clinician may
want to wrap soft restraints (sheets or blankets) around the bed
and the patient at the hips to prevent him or her from falling off
the stretcher. A weight (usually from 5 to 15lbs) is affixed to the
wrist to provide longitudinal, sustained traction. Wrapping tape,
a gauze or elastic bandage, or a padded wrist restraint around the
wrist should provide secure fixation of the weight to the limb.
Commercial devices are also available for securing and hanging
a weight from the wrist. A bucket of water can be used if weights
are not available; the disadvantage for the patient is having to
hold the bucket for a considerable length of time. IV fluid can
be used to gradually increase the traction as the bucket fills up
(Fig. 196-3).
3. With time (usually 15 to 30 minutes) and relaxation, the shoul
der will usually reduce itself. Occasionally (perhaps after 30
minutes), the clinician will need to facilitate the reduction by
grasping the forearm and gently twisting it, externally first and
then internally, while the arm is still under traction. Either the
patient or clinician may feel a clunk as the joint is reduced,
and there may be brief fasciculations of the deltoid muscle.
However, the reduction may be more subtle; if the patient can
touch his or her nose or the opposite shoulder with the index
finger of the affected upper extremity, it usually indicates a suc
cessful reduction.
4. After the shoulder has been reduced, hold the limb in internal
rotation against the abdomen and adduction (humerus against
the lateral trunk) with a shoulder immobilizer or sling and swath
196 SHOULDER DISLOCATIONS
1345
A
Figure 196-3 Gentle, sustained distal traction can provide an effective
means for closed reduction of an anterior dislocation. As the intravenous
fluid slowly empties into the bucket, the traction force gradually increases.
device. A careful postreduction neurovascular assessment is
required.
5. While keeping the shoulder immobilized, obtain appropriate
postreduction radiographs to determine whether adequate reduc
tion of the joint surfaces has been achieved. A congruousappearing joint without significant distraction (interposed tissue)
between the glenoid and the humerus should be noted. Occa
sionally, comparison shoulder radiographs or a postreduction CT
scan may be required. Some recent studies question the value of
postreduction imaging, but in most communities it is still the
standard of care.
Scapular Manipulation Technique
The patient may or may not require analgesia or injected anesthesia
for this technique because there is somewhat less manipulation
required (and less chance of injury) than with most other tech
niques. Using this technique, the glenoid fossa is repositioned rather
than just the humeral head. Scapular manipulation may be per
formed with the patient prone, sitting, or supine. When the patient
is prone or supine, traction is applied to the arm by an assistant (or
by attached weights if the patient is prone). The shoulder is gently
and gradually flexed by an assistant to a 90-degree position, and from
5 to 15lbs of traction is required. The clinician then uses one hand
to rotate the inferior aspect of the scapula upward and medially, and
the other hand to rotate the superior aspect laterally (Fig. 196-4).
When the patient is sitting, an assistant provides forward traction
on the affected arm with countertraction against the head of the
humerus to obtain the same 90 degrees of flexion. From behind the
patient, the clinician manipulates the scapula as described previ
ously. If reduction does not occur within 1 to 3 minutes, a small
degree of dorsal displacement of the inferior scapular tip may be
helpful. At this point, slight external rotation of the humerus by an
assistant while traction is maintained on the humerus and the
scapula is being manipulated may also be helpful. There have never
been complications reported from using this technique; however, it
is a cumbersome process. Reduction may also be very subtle when
accomplished by this technique, without a perceived clunk. This
technique may be used when other injuries limit repositioning the
patient.
Hennepin Technique
The Hennepin technique is named after the Hennepin County
Emergency Medical Center (Minnesota), where the technique was
B
Figure 196-4 Scapular manipulation technique. A, An assistant flexes
the patients arm (or if the patient is prone, it can be flexed by gravity
and weights, as with the Stimson technique). It must be slowly brought
to a 90-degree position. The clinician then rotates the inferior scapular tip
upward and medially, and the superior aspect laterally (clockwise on the right
shoulder when viewed from back, counterclockwise on the left shoulder).
B, The same technique with the patient in supine position. With the patients
shoulder and elbow both flexed 90 degrees, and the shoulder adducted,
gentle upward pressure is maintained by an assistant while the scapula is
manipulated as described.
first described. It is the technique preferred by some authors for
anterior shoulder dislocations. There is less manipulation than with
most other techniques, a lower probability of neurovascular or mus
culoskeletal damage, and little or no need for analgesia (although
an injection of intra-articular anesthesia may be beneficial). The
patient is seated upright, reclining at 45 degrees, or supine. With
the clinician stabilizing the patients elbow joint of the affected arm
with one hand, the clinicians other hand is used to grasp the
patients wrist. Slowly (it can take up to 10 minutes to accomplish),
the patients forearm is externally rotated until there is 90 degrees
of external rotation (Fig. 196-5). The procedure should be stopped
if the patient experiences pain or discomfort, but do not release the
arm or allow it to return to its original position. Usually, after allow
ing the musculature or spasm to relax, the procedure can be contin
ued without analgesia. If pain or discomfort persists, the patient may
require analgesia. The reduction usually occurs by the time the
forearm has reached 90 degrees of external rotation; if it has not,
the arm is slowly elevated. Occasionally, it will need to be elevated
to the level that the patient can touch his or her contralateral ear
(over the head). If reduction still does not occur, the humeral head
is gently manipulated toward the glenoid until it reduces.
Modified Kocher Maneuver
The modified Kocher maneuver is similar to the Hennepin tech
nique. The patient is placed supine with the arm of the affected
shoulder over the edge of the gurney, and analgesia or injected
anesthesia is provided if necessary. The patients forearm, with the
1346
ORTHOPEDICS
Fulcrum Technique
With the patient supine or sitting, a firmly rolled towel, sheet, or
blanket, 6 to 8 inches in diameter, is placed as a fulcrum within the
axilla of the affected shoulder. The distal humerus is used as a lever
and is adducted gently, with simultaneous posterolateral manipula
tion of the humeral head. This technique increases the forces
applied; therefore, the risk of complications is increased.
Boss-Holzach-Matter Technique
The patient sits against the maximally raised head of a gurney and
wraps his or her forearms around the ipsilateral knee, which is flexed
at 90 degrees. The head of the gurney is then lowered. The patient
is asked to hyperextend the neck while leaning back and shrugging
the shoulders anteriorly. This technique reportedly does not require
analgesia.
Hippocratic Technique
Because the Hippocratic technique is no longer recommended, it is
included only for historical interest. The clinician places his or her
foot against the chest wall to provide countertraction and then
manipulates the arm. This technique can cause serious neurovascu
lar trauma.
C
Figure 196-5 Hennepin and modified Kocher techniques. Both techniques start with the elbow flexed to 90 degrees (A), and then fully externally
rotated (B). For the modified Kocher, the forearm is then returned to complete internal rotation while gentle shoulder joint pressure is applied. The
Hennepin technique (C) is continued from (B), if necessary, with elevation
of the arm and manipulation of the joint posteriorly until the arm is overhead
and the dislocation is reduced.
A
elbow held at 90 degrees, is then rotated externally (abducting
superiorly) over at least a 5-minute period (see Fig. 196-5), with
simultaneous gentle downward pressure applied on the dislocation.
After the arm reaches 120 degrees of rotation, the arm is brought
back to internal rotation, at which time the reduction usually
occurs.
1020
Milch Technique
With the patient sitting or supine, the arm is moved to 10 to 20
degrees of forward flexion with slight abduction. One of the clini
cians hands is then used to gently guide the patients arm (grasping
at the elbow) in this slightly abducted position and using slight
traction, until it is directly overhead (Fig. 196-6). The patient may
be able to move the arm without assistance to this position; however,
there is usually too much pain and spasm. While this is occurring,
the clinicians other hand is placed on the humeral head to prevent
it from moving downward. When the arm is located directly over
head, the rotator cuff muscles are all in alignment, and all crossstresses are eliminated. Using just his or her thumb, the clinician
should be able to direct the humeral head superiorly over the rim of
the glenoid and into the fossa. Otherwise, abduction of the arm and
outward traction at the shoulder are increased and the arm brought
through a full, lateral downward arc. Reduction is usually signified
by an audible or palpable clunk.
C
Figure 196-6 Milch technique. A, The arm is started at 10 to 20 degrees
of flexion and slight abduction. B, Elevation continues slowly, with slight distal
traction, until the arm is directly overhead. The patient may be able to raise
the arm on his or her own. The head of humerus should be held immobile
at this stage of maneuver. C, If no reduction occurs with gentle, direct
manipulation of the head of the humerus, the arm is then slowly brought
through a full, lateral downward arc, maintaining constant outward traction
until reduction occurs. Note that this is the only step of the procedure in
which outward traction is maintained.
196 SHOULDER DISLOCATIONS
COMPLICATIONS
CPT/BILLING CODES
If the shoulder dislocation proves irreducible, an orthopedic surgeon
should be consulted and the use of general anesthesia considered.
Fracture (due to the dislocation or reduction [iatrogenic]) and neurovascular damage are ever-present risks. Up to 50% of anterior
dislocations have a Hill-Sachs deformity, an impaction fracture
defect in the posterolateral portion of the humeral head. A Bankart
lesion may also be noted, which is an avulsed fragment of the
glenoid labrum with contiguous bone. Both lesions tend to get worse
the longer the humeral head remains dislocated.
Many clinicians obtain postreduction radiographs to document
reduction of the joint, any injury associated with the reduction, and
any bony abnormalities such as the aforementioned lesions.
Another risk after a shoulder dislocation is redislocation. In
patients followed for 10 years, age at initial dislocation was the only
predictor of recurrence; duration of subsequent immobilization had
no effect. Rotator cuff tears and hemarthrosis are more common with
inferior dislocation and in patients older than 60 years of age. To
avoid serious complications of procedural sedation, adequate respiratory
support measures and monitoring should be present. Patients need
to be observed after such sedation to ensure they are awake, alert,
and oriented before discharge.
23650
POSTPROCEDURE EDUCATION
AND
CARE
Patients may need oral analgesic medications, possibly even narcot
ics, for a few days. Those younger than 20 years of age should be
immobilized for 3 weeks, patients aged 20 to 40 years should be
immobilized for 1 to 2 weeks, and patients older than 60 years should
have less than 1 week of immobilization. Appropriate clinical, neu
rologic, and radiographic follow-up examinations should be made
throughout this time to confirm maintenance of the reduction. After
the designated period of immobilization, assign a gentle strengthen
ing program, with particular emphasis on the shoulder internal rota
tors. Unrestricted external rotation, abduction, and lifting activities
are usually not permitted for a period of 3 months. Even combing
the hair combines external rotation and abduction and should be
avoided indefinitely on the side of dislocation. With recurrent dis
locations, an arthrogram, CT arthrogram, magnetic resonance
imaging, or arthroscopy might be warranted to help identify an
anatomic variant that might make the patient more prone to redis
location. Patients with peripheral neuropathies, syringomyelia, and
psychiatric histories may be more prone to dislocating their shoul
ders, and these underlying conditions should be considered in
patients with repeated dislocations.
23655
1347
Closed treatment of shoulder dislocation, with manipula
tion, without anesthesia
Closed treatment of shoulder dislocation, with manipula
tion, requiring anesthesia
ICD-9-CM DIAGNOSTIC CODES
718.01
718.11
718.31
831
831.0
831.1
Articular cartilage disorder, shoulder region (old rupture
of ligaments)
Loose body in joint, shoulder region
Recurrent dislocation of joint, shoulder region
Dislocation of shoulder
The following five-digit subclassification is for use with
category 831:
0 Shoulder, unspecified (humerus NOS)
1 Anterior dislocation of humerus
2 Posterior dislocation of humerus
3 Inferior dislocation of humerus
4 Acromioclavicular (joint) (clavicle)
9 Other (scapula)
Closed dislocation
Open dislocation
ACKNOWLEDGMENT
The editors wish to recognize the many contributions by Fred M.
Hankin, MD, and J. Mark Wiedemann, MD, MS, to this chapter in
the previous two editions of this text.
BIBLIOGRAPHY
Doyle WL, Ragar T: Use of the scapular manipulation method to reduce
an anterior shoulder dislocation in the supine position. Ann Emerg Med
27:9294, 1996.
Eiff MP, Hatch RL, Calmbach WL: Fracture Management for Primary Care,
2nd ed. Philadelphia, Saunders, 2003.
Roberts JR, Hedges JR (eds): Clinical Procedures in Emergency Medicine,
4th ed. Philadelphia, Saunders, 2004.
Sineff SS, Reichman EF: Shoulder joint dislocation reduction. In Reich
man EF, Simon RR (eds): Emergency Medicine Procedures. New York,
McGraw-Hill, 2004, pp 593613.
Stimson LA: An easy method of reducing dislocations of the shoulder and
hip. Med Rec 57:356357, 1900.
Tuggy M, Garcia J: Procedures Consult. Available at www.procedures
consult.com, and as an application at www.apple.com/iTunes.
Das könnte Ihnen auch gefallen
- Bab IDokument2 SeitenBab IkhalidaharwinNoch keine Bewertungen
- Menu Ramadhan Umi CateringDokument2 SeitenMenu Ramadhan Umi CateringkhalidaharwinNoch keine Bewertungen
- Parasit Malaria Dan FilariaDokument25 SeitenParasit Malaria Dan FilariaVithiya Chandra SagaranNoch keine Bewertungen
- GGDokument2 SeitenGGkhalidaharwinNoch keine Bewertungen
- Termination of AED Treatment in Patients in RemissionDokument21 SeitenTermination of AED Treatment in Patients in RemissionkhalidaharwinNoch keine Bewertungen
- Daftar - PustakaDokument4 SeitenDaftar - Pustakaelfon_gleeNoch keine Bewertungen
- Daftar - PustakaDokument4 SeitenDaftar - Pustakaelfon_gleeNoch keine Bewertungen
- Motion Sickness yDokument2 SeitenMotion Sickness ykhalidaharwinNoch keine Bewertungen
- Guidelines Pptpresentation 001Dokument43 SeitenGuidelines Pptpresentation 001khalidaharwinNoch keine Bewertungen
- 3) Abstrak dst1Dokument8 Seiten3) Abstrak dst1khalidaharwinNoch keine Bewertungen
- Diagnosis and Management of Miliary TuberculosisDokument28 SeitenDiagnosis and Management of Miliary TuberculosiskhalidaharwinNoch keine Bewertungen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- SOAP Progress NotesDokument11 SeitenSOAP Progress NotesShan SicatNoch keine Bewertungen
- Leoline Installation and MaintenanceDokument8 SeitenLeoline Installation and MaintenanceFloorkitNoch keine Bewertungen
- CPVC Price ListDokument8 SeitenCPVC Price ListYashwanth GowdaNoch keine Bewertungen
- OGJ Worldwide Refining Survey 2010Dokument67 SeitenOGJ Worldwide Refining Survey 2010Zahra GhNoch keine Bewertungen
- hw410 Unit 9 Assignment 1Dokument8 Seitenhw410 Unit 9 Assignment 1api-600248850Noch keine Bewertungen
- Geotechnical Engineering GATE Previous QuestionsDokument35 SeitenGeotechnical Engineering GATE Previous QuestionsSurya ChejerlaNoch keine Bewertungen
- Leader Ship Assessment: Student No 374212036Dokument4 SeitenLeader Ship Assessment: Student No 374212036Emily KimNoch keine Bewertungen
- Competitor Analysis: Square PharmaceuticalsDokument5 SeitenCompetitor Analysis: Square PharmaceuticalsShoaib HussainNoch keine Bewertungen
- Supplementary Spec To API Specification 17D Subsea Wellhead and Tree Equipment With Justifications S 561Jv2022 11Dokument81 SeitenSupplementary Spec To API Specification 17D Subsea Wellhead and Tree Equipment With Justifications S 561Jv2022 11maximusala83Noch keine Bewertungen
- LabStan - July 16-17, 23-24, 30-31, Aug 6-7Dokument25 SeitenLabStan - July 16-17, 23-24, 30-31, Aug 6-7CandypopNoch keine Bewertungen
- Lead in Water: Standard Test Methods ForDokument17 SeitenLead in Water: Standard Test Methods ForAMMARNoch keine Bewertungen
- Jurnal Aquaponik Jada BahrinDokument36 SeitenJurnal Aquaponik Jada BahrinbrentozNoch keine Bewertungen
- Surveys For Maint'Ce ClassDokument7 SeitenSurveys For Maint'Ce ClassSuhe EndraNoch keine Bewertungen
- SurveyDokument1 SeiteSurveyJainne Ann BetchaidaNoch keine Bewertungen
- LaserDokument12 SeitenLasercabe79Noch keine Bewertungen
- Lesson 3.3 Inside An AtomDokument42 SeitenLesson 3.3 Inside An AtomReign CallosNoch keine Bewertungen
- Fitting in and Fighting Back: Stigma Management Strategies Among Homeless KidsDokument24 SeitenFitting in and Fighting Back: Stigma Management Strategies Among Homeless KidsIrisha AnandNoch keine Bewertungen
- Cell Division-Mitosis Notes: 2 New CellsDokument21 SeitenCell Division-Mitosis Notes: 2 New CellsCristina MariaNoch keine Bewertungen
- Dingenen 2017Dokument14 SeitenDingenen 2017pedro.coleffNoch keine Bewertungen
- Allowable Stresses of Typical ASME Materials - Stainless SteelDokument5 SeitenAllowable Stresses of Typical ASME Materials - Stainless SteelChanchal K SankaranNoch keine Bewertungen
- Bars Performance AppraisalDokument6 SeitenBars Performance AppraisalPhillip Miler0% (1)
- Neicchi 270 ManualDokument33 SeitenNeicchi 270 Manualmits2004Noch keine Bewertungen
- Bycatch Reduction Devices - PresentationDokument92 SeitenBycatch Reduction Devices - PresentationSujit Shandilya0% (1)
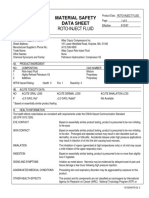
- Material Safety Data Sheet Roto-Inject FluidDokument5 SeitenMaterial Safety Data Sheet Roto-Inject FluidQuintana JoseNoch keine Bewertungen
- UNIT-5 International Dimensions To Industrial Relations: ObjectivesDokument27 SeitenUNIT-5 International Dimensions To Industrial Relations: ObjectivesManish DwivediNoch keine Bewertungen
- Mechanism of Enzyme ActionDokument19 SeitenMechanism of Enzyme ActionRubi AnnNoch keine Bewertungen
- Vertical Mills V2 0Dokument56 SeitenVertical Mills V2 0recai100% (1)
- Ableism - What It Is and Why It Matters To EveryoneDokument28 SeitenAbleism - What It Is and Why It Matters To Everyonellemma admasNoch keine Bewertungen
- Eastman Methyl N-Amyl Ketone (MAK) and Eastman Methyl Isoamyl Ketone (MIAK)Dokument4 SeitenEastman Methyl N-Amyl Ketone (MAK) and Eastman Methyl Isoamyl Ketone (MIAK)Chemtools Chemtools100% (1)
- 900 ADA - Rev13Dokument306 Seiten900 ADA - Rev13Miguel Ignacio Roman BarreraNoch keine Bewertungen