Beruflich Dokumente
Kultur Dokumente
Absenteeism
Hochgeladen von
Arga KafiCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Absenteeism
Hochgeladen von
Arga KafiCopyright:
Verfügbare Formate
Vol. 32, No.
633
Clinical Research and Methods
Alcohol-free Instant Hand Sanitizer Reduces
Elementary School Illness Absenteeism
David L. Dyer, PhD; Arnold Shinder, DO; Fay Shinder, RN
Background and Hypotheses: A substantial percentage of school absenteeism among children is related
to transmissible infection. Rates of transmission can be reduced by hand washing with soap and water,
but such washing occurs infrequently. This study tested whether an alcohol-free instant hand sanitizer
(CleanHands) could reduce illness absenteeism in school-age children. Methods: A 10-week, openlabel, crossover study was performed on 420 elementary school-age children (ages 512). Students were
given a brief orientation immediately prior to the start of the study on the relationship of germs, illness,
and hand washing. Each student in the treatment group then received the test product in individual bottles,
with instructions to apply one to two sprays to the hands after coming into the classroom, before eating,
and after using the restroom, in addition to their normal hand washing with soap and water. The control
group was instructed to continue hand washing as normal with non-medicated soap. After 4 weeks of
treatment and a 2-week wash-out period, the control and experimental groups were reversed. Data gathered on absenteeism were classified as gastrointestinal or respiratory related and normalized for nonillness-related absenteeism and school holidays. Results: Compared to the hand washing-only control
group, students using CleanHands were found to have 41.9% fewer illness-related absence days, representing a 28.9% and a 49.7% drop in gastrointestinal- and respiratory-related illnesses, respectively.
Likewise, absence incidence decreased by 31.7%, consisting of a 44.2% and 50.2% decrease in incidence
of gastrointestinal- and respiratory-related illnesses, respectively. No adverse events were reported during the study. Conclusions: Daily use of the instant hand sanitizer was associated with significantly lower
rates of illness-related absenteeism.
(Fam Med 2000;32(9):633-8.)
A leading predictive factor of academic success for elementary school-age children is attendance.1 However,
attendance optimization is impeded by illness absenteeism; the average school-age child contracts four or
more colds per year, with each such cold potentially
lasting from 5 to 14 days. 2 In public schools, illness
absenteeism can result in the loss of public monetary
compensation for the student. Absences also burden
schools with remedial work for absentees and with the
additional cost of substitute teachers to replace teachers who have fallen ill due to classroom exposure to
sick children. Finally, student absences can require parents to stay home, which adversely affects businesses.
Therefore, in addition to academic impact, illness ab-
From the Research Division, Woodward Laboratories, Los Alamitos, Calif.
senteeism slows the educational machinery and strains
the human and financial resources of our schools.
Although many factors lead to illness absenteeism,
close contact and insufficient hand washing contribute
greatly to the communicable nature of colds and gastrointestinal (GI) infections.3-4 Microbial (viral and bacterial) infections of the respiratory and GI tract cause a
significant percentage of school illnesses. A specific
example of this is rhinovirus, which is more effectively
transmitted by hand contact than by droplet dispersion.3,4 Studies that examined the relationship between
illness absenteeism and hand washing concluded that
scheduled hand washing reduces acute communicable
illnesses in school-age children.4 Also, the US Centers
for Disease Control states that hand washing is the best
way to prevent the spread of infections.5-8
In spite of positive results with regimented hand
washing routines,9-12 other studies indicate that maintaining an effective hand-washing program in US
634
October 2000
schools is difficult because many classrooms lack basic facilities for proper hand washing. Further, even with
proper facilities, the time required for 20 to 30 students
to perform minimal hand washing (3060 seconds each)
would significantly interfere with classroom instruction time.
In response to the need for hand sanitization in situations where soap and water are not readily available,
and time is limited, antimicrobial rinse-free handsanitizing formulas have been developed. Antimicrobial product effectiveness claims reveal several limitations of the active ingredients in this category, the majority of which are alcohol based, with a few containing triclosan.13,14 Triclosan has limited antiviral activity and is generally bacteriostatic at most concentrations available to the consumer.13,14 Recent work further indicates that triclosan may promote antibiotic-resistant variants of Escherichia coli, Salmonella
typhimurium and Mycobacterium tuberculosis, through
mutation of gene products involved in fatty acid synthesis.15 Alcohol-based hand sanitizers are effective as
short-term antimicrobial preparations, but long-term,
frequent use of certain alcohol products can cause skin
irritation.13 It has been observed that frequent use of
the alcohol-based sanitizers hinders the products effectiveness and can leave the hands more susceptible
to microbial contamination.16 Further, after an alcohol
sanitizer dries, no antimicrobial agent remains on the
skin, which is readily recolonized by pathogens. In
addition, alcohol-based sanitizers are flammable and
can irritate eyes and open wounds. Products with these
active ingredients are, therefore, undesirable in school
settings and can present a safety hazard to children.
Because of these issues, a safe, effective, nonflammable, nonirritating antimicrobial instant hand sanitizer
could be useful for hand sanitization in the absence of
soap and water. Such a sanitizer containing surfactants,
allantoin, and benzalkonium chloride (SAB formulation19) has been recently developed. This product meets
federal standards for antiseptic hand washes16,17 for
health care personnel, is fast acting with a broad antimicrobial spectrum, and demonstrates a significant
persistence of activity.16 The SAB hand sanitizer is nonflammable and does not dry or damage the skin.16
The formulations effectiveness at reducing illness
absenteeism in a school setting was tested in a 10-week,
open-label, crossover study of programmed use of the
hand sanitizer in conjunction with at-will soap-andwater hand washing.
Methods
The study was conducted at Grace Christian School,
a private elementary school in Cypress, Calif. Children
(n=420) ranging from ages 512 (all grades from kindergarten through sixth grade) were included in the
study; each classroom group contained 30 students, and
Family Medicine
there were two classrooms per grade level. Although
the study protocol required exclusion of children with
known allergies to any of the ingredients in the SAB
sanitizer, no exclusions from the population were necessary during the course of the study. While the study
was not approved by a formal university institutional
review board, it was reviewed and approved by the principal and school board of education. Prior to study initiation, the school board and principal (institutional
oversight board) informed the school parents about the
purpose and nature of the study. Although parents had
the option of not letting their child participate in the
study, no objections or withdrawals were received for
the studys duration.
Subjects were grouped by classroom without formal
randomization. Seven classes received the instant sanitizer, while the remaining seven classes were assigned
to the control group. Male-to-female ratios and age distributions of the two groups did not differ significantly.
Two weeks prior to study initiation, all students received
a 30-minute presentation on germs, the relationship of
germs to colds, and the importance of washing hands
with soap and water to prevent illnesses. The students
also viewed an educational videotape presentation that
described the hand-to-hand spreading of germs between
people.
SAB Sanitizer
The SAB formulation is effective against a wide variety of pathogens, including gram-positive and gramnegative bacteria, mold, and fungi and a variety of viruses, including Haemophilus influenza, lipid-encapsulated viruses, and Hepatitis B virus. The SAB hand
sanitizer surpasses the Food and Drug Administration
(FDA) performance standards for health care personnel hand washes and meets the criteria for inclusion
into the Health Care Continuum Model (HCCM), a performance-based standard developed by industry to assist the FDA in classification of topical antimicrobial
drug products, in that it 1) is fast acting, 2) has a broad
antimicrobial spectrum, 3) displays persistence of activity, and 4) is effective under a heavy bacterial soil
load.16-18
Sanitizer Group
Children in the hand sanitizing group received a
1-oz bottle of the SAB hand sanitizer fitted with a pumpspray top, which facilitated reproducible product dispensing and dispersion. Students were instructed to use
the spray under teacher supervision to supplement normal, at-will hand washing with non-medicated (nonantibacterial) soap and water. The situations determined
for sanitizer use were 1) immediately after entering the
classroom, 2) before eating (snacks and lunch), 3) after
sneezing or coughing in the classroom, and 4) after
using the restroom facility. Students were instructed to
Clinical Research and Methods
use the sanitizer by pushing the pump once and spraying (approximately .25 ml) into the palm of the hand.
Students were told to then rub their hands together, in a
normal washing motion, concentrating on the fingertips and under the nails, until the hands were dry.
Control Group
The control group was instructed to wash hands before eating, after visiting the restroom, and as otherwise necessary during the day. Students were instructed
to wash hands with warm water and non-medicated
soap, as usually performed, concentrating on the fingertips and under the fingernails. Handwashing in this
group was not supervised.
Data Collection
Data were collected for 10 weeks (March to May,
1998). In the first 4 weeks of the study, SAB sanitizer
was distributed to half of the student population, while
the other half washed at will (described above). This
first test period was followed by a 2-week wash-out
period, during which neither group of students used the
SAB sanitizer, and they were asked to wash their hands
when necessary with water and non-medicated soap and
refrain from using any other type of instant hand sanitizer. Students then received the review orientation on
germs and illness, and SAB sanitizer was distributed
to the student group that had previously served as the
control. The study proceeded for another 4 weeks.
Vol. 32, No. 9
635
illness-related absences. Relative risk of absence (RRA)
was calculated as follows: RRA = As/T divided by Ac/
T, where As=absences (sanitizer group), Ac=absences
(control group), and T=total possible days of attendance.
Statistical Analysis
Statistical significance was measured using chisquare analysis.
Results
Of the total absences in the first 4 weeks of the study
for the sanitizer-using group, 38.5% were due to GI
illness, and 61.5% were caused by respiratory illness.
This distribution was comparable to the control group,
where 40.9% were caused by GI illness and 59% by
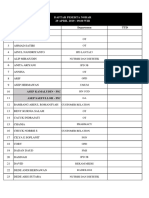
respiratory illness. However, as shown in Table 1, the
total number of absences due to communicable acute
illness was 33.6% lower in the sanitizer group (P<.001)
than in the control group.
Absence incidence in the sanitizer group was approximately 48% (P<.001) lower than in the control
group. Total GI and respiratory-related absences were
decreased by 37.5% (P<.001) and 30.9% (P<.02), respectively, compared with the control group. Likewise,
GI and respiratory absence incidences were suppressed
in the sanitizer group by 57.7% and 39.1%, respectively,
compared with the control group.
Following the 2-week nonuse period, no significant
difference was noted in GI or respiratory absences between the two groups. Test groups were then reversed
as described above, and the test proceeded for another
4 weeks. A significant decrease in total illness-related
absences was again observed in the sanitizer group,
compared with the control group (55.7%, P<.001; Table
2). Although fewer GI-related absences occurred in the
sanitizer group, the number was not significantly different than the control group (P=.66). In contrast, respiratory absences were 76% lower than the control
group (P<.001). Absence incidence was 43% less in
Scoring of Absences
Teachers were responsible for recording absences
during the study. Absence classification categories included: total absence number, total absence incidences
(discrete illness periods per student), and total days of
absence (absence caused by communicable illness).
Parents provided information on the nature of the
students absence to the health secretarys office during the study. Absences were counted as GI (symptoms
included vomiting, abdominal
pain, and diarrhea), respiratory related (symptoms included cough,
sneezing, sinus trouble, bronchitis,
Table 1
fever alone, pink eye, headache,
mononucleosis, and acute exacerPart IStudent Absence Data
bation of asthma), or non-transTOTAL
R RELATED
missible illness related (vacations, ABSENCES:
Control
SAB
Control
SAB
non-transmissible urinary tract in- Number of classes
7
7
7
7
210
210
210
210
fections, sprained or broken limbs, Participating students
Possible days of attendance
4,120
4,136
4,120
4,136
etc).
Absence incidence
69
36
36
22
Total possible student days of Days of illness
105
70
62
43
57
31
26
19
attendance was defined as the Different students absent
1.84
2.26
2.38
2.26
number of students in the study Days absent per student
group multiplied by the number of Rrespiratory
study days, minus the number of GIgastrointestinal
days of other non-transmissible SABhand sanitizer
GI RELATED
Control
SAB
7
7
210
210
4,120
4,136
33
14
43
27
31
12
1.39
2.25
636
Family Medicine
October 2000
Table 2
Part IIStudent Absence Data
ABSENCES:
Number of classes
Participating students
Possible days of attendance
Absence incidence
Days of illness
Different students absent
Days absent per student
TOTAL
Control
SAB
7
7
210
210
4,140
4,156
43
23
63
28
37
17
1.70
1.65
R RELATED
Control
SAB
7
7
210
210
4,140
4,156
26
9
43
10
20
8
1.00
2.25
Rrespiratory
GIgastrointestinal
SABhand sanitizer
the sanitizer group than in the control group for total
absences (P<.05) and 65% lower for respiratory absences (P<.001). The absence incidence for GI was
not significantly different than the control group. The
distribution of GI and respiratory illness as a percentage of the total illnesses differed between the two
groups in the second half of the test: in the sanitizer
group, 64.3% of the illness absenteeism recorded was
assessed to be GI and 35.7% respiratory in origin, while
in the control group, 31.7% was assessed to be GI and 68.3% respiratory in origin.
As shown in Table 3 and Figure
1, a summation of absence data
over the entire 8 weeks of the saniGI RELATED
Control
SAB
tizer use indicates that the number
7
7
of absences and absence incidence
210
210
was significantly lower in the sani4,140
4,156
17
14
tizer group. Throughout the study
20
18
on a weekly basis, students were
17
9
monitored by teachers for adverse
2.53
1.11
reactions (edema, rash, erythema)
to the instant hand sanitizer, with
instructions to discontinue product
use on any indication of adverse
reaction. No adverse events were
observed or reported during or following the study in
either use group.
Discussion
The results from this study indicated that, overall,
the SAB sanitizer use, in conjunction with at-will hand
washing with non-medicated soap, significantly decreased illness absenteeism in terms of total absence
days and absence incidence. Further, the relative risk
of absence for students in the sanitizer group was 41% lower than
that of students in the control
Figure 1
group. The SAB sanitizer was apparently mainly effective at supCombined Absences and Absence Incidences
pressing respiratory absences,
even though significant suppression of GI-related absences was
also observed.
Master et al2 emphasize the concept that basic soap-and-water
hand washing prevents the spread
of infection and should be encouraged as a standard infection control measure. In that study, programmed hand washing significantly decreased overall illness
absenteeism (25% reduction). In
spite of these and others similar
findings,2,9-12 hand washing is not
consistently practiced or promoted
in public school systems. It appears that the main reasons include
a lack of proper washing facilities
and less-than-optimal teacher parRrespiratory
ticipation in continuously educatGIgastrointestinal
ing students about the health benBlack bars: control group. White bars: SAB hand-sanitizer use group. All SAB sanitizer use group measures
efits of hand washing,2,9,11 as well
were statistically significant (P.05, see text).
as the excessive time requirement.
While teacher motivation can be
Clinical Research and Methods
Vol. 32, No. 9
Table 3
Combined Student Absence Data
ABSENCES:
Number of classes
Participating students
Possible days of attendance
Absence incidence
Days of illness
Different students absent
Days absent per student
TOTAL
Control
SAB
7
7
210
210
8,260
8,292
112
59
168
98
94
48
1.79
2.04
R RELATED
Control
SAB
7
7
210
210
8,260
8,292
62
31
105
53
46
27
1.78
2.26
Rrespiratory
GIgastrointestinal
SABhand sanitizer
addressed at an educational and/or institutional policy
level, a lack of proper and sufficient washing facilities
(ie, clean water source/sink and soap) is a more difficult issue to address from a logistics perspective. Recent legislation from the California State Government
that encourages class downsizing, together with the
steady increase in overall student enrollment, have
forced schools to use classrooms that lack washing facilities. Therefore, structural limitations are a substantial barrier to implementing an effective scheduled handwashing program.
Another consequence to scheduled hand washing in
schools is the loss of instruction time. A 30-second hand
wash with soap and water for each of 20 students in an
average size classroom, with proper hand-washing facilities, requires 10 minutes for hand washing alone,
with a net loss in instruction time of 3040 minutes per
day (for three to four hand wash runs). It has been observed, however, that the educational benefits of a
students daily presence in school outweigh any potential detriment of entire days of absence, even if each
days instruction period was shortened by several minutes.2 Prior to the start of the present study, teachers
were given the choice of directly dispensing the sanitizer themselves onto students hands or letting the students apply it themselves. All teachers chose to let students apply the SAB hand sanitizer themselves at the
appropriate times during the day. In this situation, the
teachers verbally instructed students when to use the
SAB formula and visually monitored the application
process. There were no reports of inappropriate product use. Given the sanitizers quick drying time (3045
seconds), time lost from instruction is minimized; moreover, the entire sanitization procedure required at most
1 minute per application period, for a total of 5 minutes per day.
The majority of instant hand sanitizers available commercially contain alcohol at a concentration of 62%
70% by weight. Due to their flammability and potential for drying and irritating the skin, alcohol sanitizers
GI RELATED
Control
SAB
7
7
210
210
8,260
8,292
50
28
63
45
48
21
1.79
1.76
637
are not compatible with school
hand-sanitization programs. The
SAB formulation used in this
study differs from alcohol-containing instant hand sanitizers because it is not flammable, does not
contain organic solvents, and contains allantoin, a well-accepted
skin conditioner (Chodosh D. US
Patents 5,661,107 and 5,827,870,
1998). The lack of adverse events
reported during the course of the
study supports its safety as a dailyuse sanitizer.
Limitations
Although the present study was
prospective, controlled, and involved a sufficient number of participants, it had some limitations in design.
These included limited socioeconomic diversity in the
study population, limitation to a single study site, and
lack of blinding. Further, soap-and-water washing was
not monitored. It is, therefore, possible that the effect
yielded in this study was in part due to lack of soapand-water washing in the control group. In both study
groups, however, at-will hand washing with soap and
water was recommended equally and simultaneously
and reinforced by providing educational material on
the importance of hand washing. Also, soap and water
hand washing compliance in school populations has
been shown to range from 8%28%.19 Further, control
group baseline absences in the present study were similar to those reported previously.2 Therefore, it is likely
that unmonitored soap-and-water hand washing was
similar and minimal for both groups in this study.
Implications
In response to the antimicrobial consumer and health
care product proliferation, the FDA has questioned
whether such products provide any real-life benefits.
In fact, such demonstrations are scarce in the literature. However, a recent open-label, non-placebo controlled, non-crossover study of an alcohol-based hand
sanitizer at suppression of illness absenteeism demonstrated approximately a 25% overall reduction.20 In contrast, the present study demonstrated approximately a
41% reduction in absenteeism, with the added stringency of population crossover.
The family physician, as the medical liaison to the
community, has the opportunity to educate and inform
key individuals such as teachers, school nurses, school
board members, and others responsible for students
health and well-being. Even if one doesnt have schoolage children, it is necessary to understand the importance and benefits of good hand hygiene, not only in
clinical practice but also in the greater community.
Vital tax dollars will be saved on expenses for remedial
638
Family Medicine
October 2000
student services and lost employee work time by this
simple and effective way to decrease illness-related
absenteeism.
Conclusions
In summary, this study determined that daily use of
the SAB instant hand sanitizer with at-will hand washing using soap and water significantly decreased absences due to acute communicable illness. While a
larger, placebo-controlled study should be performed
to further support these findings, these initial results
suggest that the alcohol-free SAB instant hand sanitizer allows optimization of student attendance with
minimal financial and instruction time impact.
Corresponding Author: Address correspondence to Dr Dyer, Woodward
Laboratories, 11132 Winners Circle, Suite 100, Los Alamitos, CA 90720.
562-598-0800. Fax: 562-598-0010. E-mail: dldyer@woodwardlabs.com.
REFERENCES
1. The Buckeye Institute for Public Policy Solutions. Public choices, private costs: an analysis of spending and achievement in Ohio public
schools. Buckeye Institute Journal 1998;Sept.
2. Master D, Hess-Longe S, Dickson H. Scheduled hand washing in an
elementary school population. Fam Med 1997;29(5):336-9
3. Middleton D. Upper respiratory tract infections of childhood, part I.
The common cold. Family Practice Recertification 1993;15(8).
4. Gwaltney J, Moskalski P, Hendly O. Hand-to-hand transmission of rhinovirus colds. Ann Intern Med 1978;88:463-7.
5. Garner JS, Favero MS. Handwashing. Guideline for handwashing and
hospital environmental control. Section 1. Atlanta: Hospital Infections
Program Center for Infectious Diseases, Centers for Disease Control
and Prevention, 1985.
6. Steere AC, Mallison GF. Hand-washing practices for the prevention of
nosocomial infections. Ann Intern Med 1975;83:683-90.
7. Ayliffe GAJ. Nosocomial infectionthe irreducible minimum. Infect
Control 1986;7:92-5.
8. Larson EA. A causal link between hand washing and risk of infection?
Examination of the evidence. Infect Control Hosp Epidemiol 1988;
9(4):445-51.
9. Black R, Aubert D, Kern A. Hand washing to prevent diarrhea in day
care centers. Am J Epidemiol 1981;113(4):445-51.
10. Day R, St Arnaud S. Effectiveness of a hand-washing program. Clin
Nurs Res 1992;2(1):24-40.
11. Monsma M, Day R, St Arnaud S. Hand washing makes a difference. J Sch Health 1992;62(3):109-11.
12. Pete J. Hand-washing practices among various school-age students.
Health Educ 1986;17(6):37-9.
13. Harvey S. Antiseptics and disinfectants, fungicides, ectoparasiticides.
In: Goodman LS, Gilman AG, Gilman A, eds. The pharmacological
basis of therapeutics, sixth edition. New York: Macmillan Publishing
Company, Inc, 1980;chap 41.
14. Department of Health, Education, and Welfare. OTC topical antimicrobial products; tentative final monograph for 21CFR333. Washington,
DC: Federal Register, 1978;43(4):part II.
15. McMurray LM, Oethinger M, Levy SB. Triclosan targets lipid synthesis. Nature 1998;394:531-2.
16. Dyer DL, Gerenraich KB, Wadhams PS. Testing a new, alcohol-free
sanitizer to combat infection. AORN J 1998;68(2):239-51.
17. Department of Health and Human Services, Food and Drug Administration. Effectiveness testing of an antiseptic hand wash or health care
personnel hand wash. 21CFR Parts 333 and 369. Tentative final monograph for health care antiseptic drug products; proposed rule. Washington, DC: Federal Register, June 17, 1994;31444-52.
18. Federal Drug Administration. Antimicrobial hand sanitizers position
in continuum model challenged. FDA tan sheet. Washington, DC:
Federal Drug Administration,1998;July 27:5-6.
19. Guinan ME, McGuckin-Guinan M, Sevareid A. Who washes hands after using the bathroom? Am J Infect Control 1997;25:424-5.
20. Gojo Sponsored Study. Effect of hand sanitizer use on elementary school
absenteeism. Waldens Convention Daily 1999 Oct 14:3-4.
Das könnte Ihnen auch gefallen
- Patkin 1Dokument9 SeitenPatkin 1Arga KafiNoch keine Bewertungen
- Trisomy 21 Fetus Co-Existent With A Partial Molar Pregnancy: Case ReportDokument2 SeitenTrisomy 21 Fetus Co-Existent With A Partial Molar Pregnancy: Case ReportArga KafiNoch keine Bewertungen
- Patklin 2Dokument9 SeitenPatklin 2Arga KafiNoch keine Bewertungen
- Patkin 1Dokument9 SeitenPatkin 1Arga KafiNoch keine Bewertungen
- Lembar PhantomqqeqDokument4 SeitenLembar PhantomqqeqArga KafiNoch keine Bewertungen
- Lembar Phantom 1-4 November 2021 23.00Dokument5 SeitenLembar Phantom 1-4 November 2021 23.00Arga KafiNoch keine Bewertungen
- Absen ResidenDokument1 SeiteAbsen ResidenArga KafiNoch keine Bewertungen
- Dept. of Obstetrics & Gynecology Case Report Dr. M. Djamil Central General Hospital 13 - 15 October, 2020Dokument3 SeitenDept. of Obstetrics & Gynecology Case Report Dr. M. Djamil Central General Hospital 13 - 15 October, 2020Olivia Oktaviani PrastiwiNoch keine Bewertungen
- Bag/Smf Obstetri & Ginekologi Laporan Jaga FK Unand/Rs Dr. M. Djamil Padang 28 Oktober-01 November 2021Dokument4 SeitenBag/Smf Obstetri & Ginekologi Laporan Jaga FK Unand/Rs Dr. M. Djamil Padang 28 Oktober-01 November 2021Arga KafiNoch keine Bewertungen
- Webinar Airway ManagementDokument2 SeitenWebinar Airway ManagementArga KafiNoch keine Bewertungen
- Dept. of Obstetrics & Gynecology Case Report Dr. M. Djamil Central General Hospital 13 - 15 October, 2020Dokument3 SeitenDept. of Obstetrics & Gynecology Case Report Dr. M. Djamil Central General Hospital 13 - 15 October, 2020Olivia Oktaviani PrastiwiNoch keine Bewertungen
- Update Peserta Nobar 2019Dokument24 SeitenUpdate Peserta Nobar 2019Arga KafiNoch keine Bewertungen
- Phantom 9-12 Jan 2018Dokument4 SeitenPhantom 9-12 Jan 2018Arga KafiNoch keine Bewertungen
- Phantom Jumat 28 - 02Dokument5 SeitenPhantom Jumat 28 - 02Arga KafiNoch keine Bewertungen
- Aug19 - AnafilaksisDokument14 SeitenAug19 - AnafilaksisArga KafiNoch keine Bewertungen
- Phantom 23-25 Mei Eng Semi FixDokument4 SeitenPhantom 23-25 Mei Eng Semi FixGunawan Efri SNoch keine Bewertungen
- Lembar Fantom 26-30 Jan 2018 EditDokument3 SeitenLembar Fantom 26-30 Jan 2018 EditArga KafiNoch keine Bewertungen
- Burn Injury (Modified From DR James Roring)Dokument23 SeitenBurn Injury (Modified From DR James Roring)Arga KafiNoch keine Bewertungen
- Acute Abdomen (Modified From DR James Roring)Dokument18 SeitenAcute Abdomen (Modified From DR James Roring)Arga KafiNoch keine Bewertungen
- Phantom 23-25 Mei Eng Semi FixDokument4 SeitenPhantom 23-25 Mei Eng Semi FixGunawan Efri SNoch keine Bewertungen
- Data IndukDokument9 SeitenData IndukArga KafiNoch keine Bewertungen
- Aug19 - Breastfeeding LactationDokument12 SeitenAug19 - Breastfeeding LactationArga KafiNoch keine Bewertungen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (120)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- StressDokument4 SeitenStressPinky Juntilla RuizNoch keine Bewertungen
- Lecture 1 Health, Safety & Environment (HSE)Dokument23 SeitenLecture 1 Health, Safety & Environment (HSE)A to z type videosNoch keine Bewertungen
- FEDIAF Nutritional Guidelines 2020 20200917Dokument96 SeitenFEDIAF Nutritional Guidelines 2020 20200917luciana ribeiroNoch keine Bewertungen
- SuctioningDokument6 SeitenSuctioningCriselda Ultado100% (2)
- Shaikh Sohail Shaikh KaleemDokument1 SeiteShaikh Sohail Shaikh KaleemMantra SriNoch keine Bewertungen
- OrphenadrineDokument4 SeitenOrphenadrineGermin CesaNoch keine Bewertungen
- g8 Health q3 LM Disease 130908005904 PDFDokument64 Seiteng8 Health q3 LM Disease 130908005904 PDFkenneth cannillNoch keine Bewertungen
- Misericordia LetterDokument2 SeitenMisericordia LetterKatie DangerfieldNoch keine Bewertungen
- Ecological Analysis of The Prevalence of PulmonaryDokument10 SeitenEcological Analysis of The Prevalence of PulmonaryLazy SlothNoch keine Bewertungen
- 7 Legal Dimensions of Nursing Chapter ReviewDokument2 Seiten7 Legal Dimensions of Nursing Chapter ReviewAmy AnonymousNoch keine Bewertungen
- IJHPM - Volume 7 - Issue 12 - Pages 1073-1084 Complex LeadershipDokument12 SeitenIJHPM - Volume 7 - Issue 12 - Pages 1073-1084 Complex Leadershipkristina dewiNoch keine Bewertungen
- Dibasic Sodium PhosphateDokument0 SeitenDibasic Sodium PhosphateWilliam ChandraNoch keine Bewertungen
- Shoulder Pain and Disability Index (SPADI) PDFDokument2 SeitenShoulder Pain and Disability Index (SPADI) PDFIvro Linda cahyaniNoch keine Bewertungen
- Reducing Maternal Mortality: Theories, Models, and PracticeDokument17 SeitenReducing Maternal Mortality: Theories, Models, and PracticeRavi Pamnani100% (2)
- Understanding PTSD: Arleen Cerbone Faustina, PH.DDokument85 SeitenUnderstanding PTSD: Arleen Cerbone Faustina, PH.DMuthu SelvanNoch keine Bewertungen
- The Chameleon Enthusiast by Noelle SenchynaDokument58 SeitenThe Chameleon Enthusiast by Noelle SenchynaDragoș DrăniceanuNoch keine Bewertungen
- Personality Disorders PDFDokument35 SeitenPersonality Disorders PDFABHINAVNoch keine Bewertungen
- Quadruple Aim in HealthcareDokument2 SeitenQuadruple Aim in HealthcareMarimiel PagulayanNoch keine Bewertungen
- Thinking CriticallyDokument31 SeitenThinking CriticallyAnonymous HU37mJ50% (2)
- Job Chart of Physical Education Teachers - AP GOVTDokument3 SeitenJob Chart of Physical Education Teachers - AP GOVTRamachandra Rao100% (1)
- 2018 MUSE Inspire Conference - Show and Tell SessionsDokument13 Seiten2018 MUSE Inspire Conference - Show and Tell SessionsMichele LambertNoch keine Bewertungen
- Vaccination BOON or BANEDokument5 SeitenVaccination BOON or BANERushil BhandariNoch keine Bewertungen
- Notice: Agency Information Collection Activities Proposals, Submissions, and ApprovalsDokument2 SeitenNotice: Agency Information Collection Activities Proposals, Submissions, and ApprovalsJustia.comNoch keine Bewertungen
- General Practitioner Sample Resume WWW - Careerfaqs.com - AuDokument3 SeitenGeneral Practitioner Sample Resume WWW - Careerfaqs.com - AuSubhash RitwalNoch keine Bewertungen
- Medical Surgical Nursing 3 BulletsDokument4 SeitenMedical Surgical Nursing 3 BulletsQueen ElizabethNoch keine Bewertungen
- Test Bank For Occupational Therapy in Mental Health A Vision For Participation 2nd Edition Catana Brown Virginia C Stoffel Jaime MunozDokument3 SeitenTest Bank For Occupational Therapy in Mental Health A Vision For Participation 2nd Edition Catana Brown Virginia C Stoffel Jaime MunozDavid Ortiz97% (36)
- Test AaDokument55 SeitenTest AaKaye PatanindagatNoch keine Bewertungen
- MOHAN Di. RAJU....... MOHAN Di. RAJU......Dokument32 SeitenMOHAN Di. RAJU....... MOHAN Di. RAJU......Nagaraja ReddyNoch keine Bewertungen
- Coma ManagementDokument5 SeitenComa ManagementElena DocNoch keine Bewertungen
- Introduction To Occupational Therapy PDFDokument291 SeitenIntroduction To Occupational Therapy PDFMurat Hasan BaşaranNoch keine Bewertungen