Beruflich Dokumente
Kultur Dokumente
Drawing Disorders in Alzheimer's Disease
Hochgeladen von
IcaroCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Drawing Disorders in Alzheimer's Disease
Hochgeladen von
IcaroCopyright:
Verfügbare Formate
See
discussions, stats, and author profiles for this publication at:
https://www.researchgate.net/publication/301592114
Drawing Disorders in Alzheimer's Disease
and Other Forms of Dementia
Article in Journal of Alzheimer's disease: JAD April 2016
Impact Factor: 4.15 DOI: 10.3233/JAD-160009
READS
19
2 authors:
Luigi Trojano
Guido Gainotti
Second University of Naples
Catholic University of the Sacred Heart
226 PUBLICATIONS 2,867 CITATIONS
337 PUBLICATIONS 9,884 CITATIONS
SEE PROFILE
SEE PROFILE
Available from: Luigi Trojano
Retrieved on: 26 April 2016
Journal of Alzheimers Disease xx (20xx) xxx
DOI 10.3233/JAD-160009
IOS Press
Review
Drawing Disorders in Alzheimers Disease
and Other Forms of Dementia
Luigi Trojanoa,b and Guido Gainottic,d
a Department
b S.
of Psychology, Second University of Naples, Italy
Maugeri Foundation, Scientic Institute of Telese Terme (BN), Italy
c Center for Neuropsychological Research, Institute of Neurology, Catholic University, Rome, Italy
d IRCCS Fondazione Santa Lucia, Department of Clinical and Behavioral Neurology, Rome, Italy
Handling Associate Editor: Jason Brandt
Accepted 16 March 2016
10
11
12
13
14
15
16
17
18
19
20
Abstract. Drawing is a multicomponential process that can be impaired by many kinds of brain lesions. Drawing disorders
are very common in Alzheimers disease and other forms of dementia, and can provide clinical information for the distinction
of the different dementing diseases. In our review we started from an overview of the neural and cognitive bases of drawing,
and from a recollection of the drawing tasks more frequently used for assessing individuals with dementia. Then, we analyzed
drawing disorders in dementia, paying special attention to those observed in Alzheimers disease, from the prodromal stages
of the amnesic mild cognitive impairment to the stages of full-blown dementia, both in the sporadic forms with late onset
in the entorhino-hippocampal structures and in those with early onset in the posterior neocortical structures. We reviewed
the drawing features that could differentiate Alzheimers disease from vascular dementia and from the most frequent forms
of degenerative dementia, namely frontotemporal dementia and Lewy body disease. Finally, we examined some peculiar
aspects of drawing disorders in dementia, such as perseverations, rotations, and closing-in. We argue that a careful analysis
of drawing errors helps to differentiate the different forms of dementia more than overall accuracy in drawing.
22
Keywords: Alzheimers disease, constructional apraxia, drawing disorders, frontotemporal dementia, Lewy body disease,
vascular dementia
23
INTRODUCTION
21
24
25
26
27
28
29
30
Different kinds of drawing disorders can be found
in Alzheimers disease (AD) and other forms of
dementia. Investigations conducted in patients with
focal brain lesions and with different forms of dementia have shown that many of these disorders can
be traced back to visual-spatial [15] or planning
disturbances [610]. These disorders are the main
determinants of constructional apraxia (CA) and are
Correspondence
to: Luigi Trojano, Dept. of Psychology, Second University of Naples, Viale Ellittico 31, 81100 Caserta, Italy.
Tel./Fax: +39 0823 274784; E-mail: luigi.trojano@unina2.it.
subsumed by lesions affecting the parietal [1114]
and frontal regions of the brain [15]. They are usually observed in copying tasks, whereas other forms
of drawing disorders, mainly due to disruption of (or
impaired access to) the pictorial representations of
objects, can be observed on tasks of drawing from
memory [1619]. The relationships between clinical forms of dementia and the corresponding patterns
of drawing disabilities stem, therefore, from the fact
that (at least in the early stages of the disease) the
brain pathology affects different brain networks preferentially. Furthermore, the need for simple tasks
with rich informational content in the assessment of
ISSN 1387-2877/16/$35.00 2016 IOS Press and the authors. All rights reserved
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
55
56
57
58
59
60
61
62
63
64
65
66
67
68
69
70
71
72
73
74
75
76
77
78
79
80
81
82
83
84
85
86
87
88
89
90
91
92
L. Trojano and G. Gainotti / Drawing Disorders in Dementia
dementia prompted the implementation of drawing
tasks, such as the clock drawing test (CDT) [2022],
in place of those classically used for assessing CA in
patients with focal brain lesions. The present review
will therefore include several sections. The first will
illustrate the neural and cognitive bases of drawing. The second will focus on the drawing tasks
more frequently used in dementia. In the third section we will pass to analyze drawing disorders in
AD, from the prodromal stages of the amnesic mild
cognitive impairment (aMCI) to the stages of fullblown dementia, both in the sporadic forms with late
onset in the entorhino-hippocampal structures and in
those with early onset in the posterior neocortical
structures. In the next section we will consider the features of drawing disorders that could differentiate AD
from vascular dementia and from the most frequent
forms of degenerative dementia, namely frontotemporal dementia (FTD) and the Lewy body disease
(LBD). In the last section we will take into account
some peculiar aspects of drawing disorders in dementia, paying particular attention to the closing-in
phenomenon [2325].
Drawing disorders in dementia are a field that is
attracting an ever-growing interest. A 2005-2015 literature search limited to Pubmed database and to
papers in English language, with the terms [drawing
OR copying OR constructional] AND dementia
as keywords, identified 793 papers. Faced with this
huge amount of studies, we realized that our work
could not be exhaustive but wanted to provide a
comprehensive review including the most relevant
clinical aspects of drawing disorders.
NEURAL AND COGNITIVE BASES OF
DRAWING
Poppelreuter [26] observed that some brain damaged patients may be impaired in a series of activities
requiring a careful control of vision on action, such
as drawing, but Kleist [27] was the first to propose the
term CA to designate a specific disturbance which
appears in formative activities (such as assembling,
building, or drawing) in which the spatial form of
the task is missed, although there is no apraxia of
the single movements. In subsequent years, drawing
became progressively more popular in neuropsychological assessment, and a lot of studies have been
aimed at comprehending its neural and cognitive
bases in brain-damaged patients and in healthy subjects [22, 28].
Studies on focal brain-damaged patients have often
provided contrasting evidence about the lateralization
and the intra-hemispheric locus of lesions provoking
drawing disabilities. Since 1962 Benton [29] underlined that the subjective nature of the clinical method,
and the large variability of the tasks used to study
constructive disorders could account for the inconsistencies found in previous literature. Benton thus
suggested using graded tests with precise scoring procedures to improve the comparability of results [29].
The ensuing authors adopted this pivotal standpoint
in trying to comprehend the neural basis of drawing
through the analysis of performance in focal brain
damaged patients. However, many studies did not
detect differences in prevalence or severity of drawing
disorders after right or left hemispheric lesions (e.g.,
[2, 6, 3032]). Then, prompted by a first systematic
survey about the relationships between visuoconstructive disabilities and hemispheric locus of lesion
[12], several authors attempted to ascertain whether
qualitative differences existed between the drawing
disorders resulting from right or left hemispheric
lesions. On one hand, correlational studies demonstrated that drawing disabilities are tightly related
with scores on visual-perceptual tasks in right but
not in left brain-damaged patients, e.g., [3, 4, 18, 33].
On the other hand, drawing disorders in left-brain
damaged patients have been ascribed to a planning
disorder [6, 7], but this interpretation has not been
supported by several empirical studies [8, 9, 17, 18,
33]. In one of the most recent systematic attempts at
identifying the neural structures involved in copying a complex figure, in a wide sample of focal
brain-damaged patients, voxel-based morphometry
revealed that different lesions in the two hemispheres
were significantly correlated with different aspects of
the drawing production [34].
Rather inconclusive results on the neural bases of
drawing in healthy individuals have also been obtained
by functional neuroimaging studies, because the latter have been constrained by the relevant artifacts
induced by the hand and arm movements, and have
often assessed drawing-related tasks rather than actual
drawing [14, 3538]. Only very recently the development of functional MRI-compatible graphic tablets
[39] allowed the analysis of hand movements during
drawing, and one recent study using such a device
reported activation within a wide network extending from the temporo-occipital to parietal and lateral
frontal areas bilaterally in healthy participants while
they were drawing faces or abstract patterns with different levels of visual details [40].
93
94
95
96
97
98
99
100
101
102
103
104
105
106
107
108
109
110
111
112
113
114
115
116
117
118
119
120
121
122
123
124
125
126
127
128
129
130
131
132
133
134
135
136
137
138
139
140
141
142
143
144
L. Trojano and G. Gainotti / Drawing Disorders in Dementia
145
146
147
148
149
150
151
152
153
154
155
156
157
158
159
160
161
162
163
164
165
166
167
168
169
170
171
172
173
174
175
176
177
178
179
180
181
182
183
184
185
186
187
188
189
190
191
192
193
Neuropsychological and functional neuroimaging
data are thus consistent with the view that the process
of drawing involves different cognitive components.
Several authors tried to single out these components
within comprehensive models [4143]. All these
models share the idea that visuospatial processes,
dedicated planning abilities, and general control processes are involved in drawing [44], although the
models differ from each other in terms of formal
characteristics, depth of analysis and some theoretical
aspects. It is worth mentioning that Grossi [43], drawing on the distinction between lexical and sub-lexical
components of language, proposed the existence of
two copying procedures: a lexical route and a lineby-line procedure. The former would consist of
motor subroutines, which could be considered as part
of a constructional lexicon, could be used to draw
well-known figures (such as a square or a face), and
would develop as a result of formal education and personal aptitudes [4546]. The latter procedure would
not rely on previously acquired constructional representations, could be used for copying novel stimuli,
and would be only based on a piecemeal spatial analysis. Both procedures could be adopted for copying
complex pictures, but some patients might be constrained to use either one or the other. For instance,
patients with visual agnosia tend to adopt a slavish
line-by-line copying procedure for familiar objects
they cannot recognize [4748]. On the contrary some
demented patients can draw simple figures successfully but fail at integrating correctly shaped simple
elements in a coherent whole, because of planning or
visuospatial defects.
the figure as a whole, with its component elements in
the correct spatial relationships. However, this task
also relies on non-constructional cognitive abilities,
particularly on lexical-semantic knowledge, pictorial
representations, and mental imagery [16, 50, 51].
A clear instance of the complexity of free drawing tasks is CDT which is widely used in the first
steps of detecting cognitive impairment and dementia
(Fig. 1), as a stand-alone neuropsychological test or
DRAWING TASKS FREQUENTLY USED IN
DEMENTIA
Drawing tasks have been widely used in patients
with dementia, but drawing performance may vary
greatly, as a function of the task (copying and free
drawing cannot be considered equivalent), of the
stimuli used in the task (more complex stimuli pose
greater load on visuospatial and planning functions),
and even of the patients pre-morbid abilities (largely
dependent on age, educational level, and even cultural
background) [49].
Free drawing, in which the patient is required to
draw a named object (e.g., a clock, a face, an animal, or a tool), can reveal information about the
patients ability to draw complete shapes or a tendency to omit parts and about their ability to organize
Fig. 1. Drawing a clock face on an empty circle, and putting the
hands at 2 : 45. Spatial distortions and errors reflecting impaired
semantic knowledge in drawings by patients with Alzheimers
disease (first row). Planning errors, perseverations, and stimulusbound responses in drawings by patients with severe forms of
vascular dementia (second row) and of behavioral vascular dementia (second row) or behavioral variant of frontotemporal dementia
(third row). Gross spatial distortions and perseverations in drawings by patients with Lewy body disease (bottom row). Often
patients with dementia are not able to draw the clock hands at
the given time, and some write numbers instead of drawings the
hands.
194
195
196
197
198
199
200
201
202
203
204
205
206
207
208
209
210
211
212
213
214
215
216
217
218
219
220
221
222
223
224
225
226
227
228
229
230
231
232
233
234
235
236
237
238
239
240
241
242
243
244
245
246
247
248
249
250
251
252
253
254
L. Trojano and G. Gainotti / Drawing Disorders in Dementia
included into composite screening batteries [20, 21,
52]. In its classical form [53], CDT requires patients
to draw the face of a clock with all the numbers
and set the two hands to 10 after 11. Many administration procedures and scoring systems have been
proposed [5457], but there is no consensus as to
which is the most useful for dementia screening [20,
54]. The scoring systems share commonalities, but
each may reflect different cognitive components and
be correlated with different areas of brain atrophy
[58]. However, independently from the scoring procedure, performance on CDT in demented patients
seems to be inversely correlated with lesion load in
medial temporal lobe, in subcortical structures and in
periventricular white matter [59, 60] and might provide prognostic information for cognitive decline [61,
62]. Some authors suggested that qualitative analysis
of errors in clock drawing might improve diagnostic accuracy for dementia screening. For instance,
errors such as inaccurate time setting, missing hands
or numbers, and number substitutions or repetitions
might be particularly useful for dementia screening
[63]. Using appropriate error classification criteria,
error analysis in CDT might be useful to differentiate different types of dementia, since conceptual
errors are quite frequent in AD [64], but in a recent
longitudinal study conceptual errors and perseverations were more frequently observed in the advanced
stages of all dementing diseases, whereas spatial
and planning errors were more frequent in mild-tomoderate dementia [65]. Errors in setting numbers
and clock hands seem to correlate with regional
hypometabolism in bilateral parietal and posterior
temporal areas and in the right middle frontal gyrus
[58]. By the same token, it has been recently observed
that different types of errors in demented patients
performance on CDT might correlate with atrophy
in different brain regions, within frontal, parietal and
temporal lobes [66].
One strategy for improving diagnostic accuracy of
CDT is to compare the drawing to command condition with a copy condition, in which subjects are
required to copy a pre-drawn clock, since in the copy
condition performance would rely only on a subset of
cognitive functions centered on visuoperceptual and
constructional skills [16]. However, although copying seems to directly assess the patients ability to
reproduce a figure, even this task can imply problem solving and executive abilities and is affected by
age, educational level, and even cultural background
[49]. In assessing copying abilities, it is therefore
necessary to adopt standardized tasks, with solid
Fig. 2. Copying of geometrical drawings: cube (model on the top).
Gross simplifications, spatial distortions, errors of perspective in
patients with Alzheimers disease (first row) and vascular dementia
(second row). Simplifications, distortions and perseverations in
patients with moderate to severe frontotemporal dementia (third
row). The bottom figures show instances of near closing-in (on the
left) and of adherent closing-in (on the right).
normative data, and to use different kinds of stimuli, well-known or novel, of graded complexity from
simple shapes, such as circles and squares, to complex
figures, such as a cube (Fig. 2), two intersecting pentagons (Fig. 3), or the Rey-Osterreith Complex Figure
(ROCF) [67, 68]. In particular, the copy of the ROCF
(Fig. 4) is often used in the assessment of drawing
abilities in individuals with dementia, and provides
an opportunity to assess copying procedures together
with copying accuracy [67]. The copy of the ROCF
has high sensitivity for detecting brain damage, since
it involves a wide network of brain areas, including
255
256
257
258
259
260
261
262
263
264
265
266
L. Trojano and G. Gainotti / Drawing Disorders in Dementia
Fig. 3. Copying of geometrical drawings: interlocking pentagons (model on the top). Simplifications and distortions in drawings by patients
with Alzheimers disease (first row); perseverations, simplifications and spatial distortions in patients with vascular dementia (second row);
simplification, distortions and planning errors in patients with moderate to severe frontotemporal dementia (third row). The bottom figures
show instances of near closing-in (on the left) and of adherent closing-in (on the right).
267
268
269
270
271
272
273
274
275
276
277
278
frontal, superior temporal, posterior parietal and middle occipital cortex, more extensively in the right
hemisphere [69]. Several neurofunctional studies in
dementia showed that accuracy in copying the ROCF
is related to metabolic rate in bilateral temporalparietal cortex and occipital lobe, and in right frontal
lobe, whereas the procedure used to copy, namely the
tendency to draw first the main organizational lines of
the model, correlated with metabolism in right lateral
temporal cortex [70]. It is worth mentioning, however, that neurofunctional studies comparing copying
of different kinds of stimuli in dementia demon-
strated that the neural correlates of copying tasks,
mainly centered in the posterior brain regions, differ
as a function of task complexity [71]. Moreover, it
appears advisable to complement evaluation of accuracy in copying tasks with a qualitative analysis of
the patients production, which can provide further
relevant information. This fact has been underlined
above with respect to the CDT, and is also suggested by recent studies showing that the copy of
two intersecting pentagons (Fig. 3), included in the
Mini-Mental State Examination [72], may provide
elements for differential diagnosis of degenerative
279
280
281
282
283
284
285
286
287
288
289
290
L. Trojano and G. Gainotti / Drawing Disorders in Dementia
Fig. 4. Copying of Rey complex figure (model on the top). Gross spatial distortions and simplifications in patients with Alzheimers disease
(first row); planning errors, spatial distortions, and perseveration in patients with vascular dementia (second row) and frontotemporal dementia
(lowest row). In the left sided column are reported drawings of patients with mild forms and in the right-sided columns those of patients
with severe forms of dementia. Note in the right top figure that the reproduction of the single subcomponents is relatively spared, but spatial
relationships among them are lost; in the right bottom figure an instance of rotation.
291
292
293
294
295
296
297
298
299
300
301
302
303
304
305
306
dementias [73, 74]. Although error analysis in drawing tasks may not reveal a straightforward procedure
[22, 28, 44], several clinical phenomena observed in
drawing have been sufficiently characterized in their
possible cognitive and neural correlates, as it will be
discussed in the next sections of this paper.
It is important to stress, however, that in the diagnostic work-up for dementia performance on drawing
tasks, and qualitative error analysis should be complemented by assessment of the deficits that can
contribute to constructional apraxia. As it will be
discussed later, mechanisms inducing errors in spontaneous drawing or in copying may encompass basic
deficits in visuoperceptual abilities, spatial attention,
spatial working memory or spatial planning, and executive function [75]. Particularly crucial in this respect
seem to be visuospatial perception whose different
aspects can be impaired in dementia [44, 7578]. Visuospatial perception is often assessed by tests such as
Bentons Judgement of Line Orientation, in which
subjects are required to identify the lines that have
the same angulation as those presented as stimuli
[79], or by comprehensive test batteries assessing several aspects of visuoperceptual processing, such as
Warrington and James Visual Object and Space Perception Battery [80], or the Battery for Visuospatial
Abilities [4, 81]. The mechanisms underlying drawing
disorders can also be clarified by means of planning/executive tests, such as Trail Making test [82] or
tests for figural fluency [83], and other tests that have
been used to assess patients with focal lesions. Motor
programming deficits have also to be considered,
307
308
309
310
311
312
313
314
315
316
317
318
319
320
321
322
L. Trojano and G. Gainotti / Drawing Disorders in Dementia
323
324
325
326
327
328
329
330
331
332
333
334
335
336
337
338
339
340
341
342
343
344
345
346
347
348
349
350
351
352
353
354
355
356
357
358
359
360
361
362
363
364
365
366
367
368
369
370
because patients with dementia may be affected by
limb apraxia or optic ataxia with a strong impact on
drawing. Therefore, these types of tests have to be used
to evaluate the different forms and the different stages
of dementia. To establish an algorithm for assessing
the different abilities involved in the drawing process and the disorders than can cause constructional
apraxia might provide a powerful tool to understand
the genesis of drawing disorders and of the different
types of errors in dementia.
DRAWING DISORDERS IN ALZHEIMERS
DISEASE
The observation that many brain regions in both
hemispheres are involved in different aspects of drawing, and by implication of constructional tasks, can
provide an explanation of the classical findings suggesting that CA is related to poor intellectual abilities
in focal brain damaged patients [30], and can represent an index for diffuse cognitive deterioration, after
lesions in either left [84] or right hemisphere [85].
According to old studies, in AD drawing disorders
are present since early stages of the disease, and their
severity increases as the illness progresses [22, 28].
However, more recent investigations have shown that
in the early stages of AD simple models can be easily copied and that drawing disabilities are observed
only with rather complex tasks [86, 87].
Several variables must therefore be taken into
account in the study of drawing disorders in AD.
Among these variables we will separately consider:
(1) the drawing tasks used in AD and the corresponding kinds of errors; (2) the drawing disorders
in prodromic (aMCI) and clinical forms of AD; (3)
the drawing disabilities in early and late onset forms
of AD; (4) the drawing disorders in different stages
of evolution of AD; (5) the mechanisms giving rise
to drawing disorders in AD patients.
The drawing tasks used in AD and the
corresponding kinds of errors
An attempt at a systematic description of AD
patients errors in a free drawing task [9] has shown
frequent occurrence of simplifications, spatial alterations, and lack of perspective. However, since free
drawing poses a heavy load on semantic memory,
errors on this task (e.g., simplifications in drawing a
house) may derive from impaired access to semantic
knowledge or to impaired visuoperceptual processing [51]. For this reason, spontaneous drawing could
be impaired in the early stages of AD, while copying may deteriorate later [88]. The reproduction of
complex figures is particularly sensitive to the progression of the disease [89]. For instance, the ROCF
may be reproduced in a simplified way, with single
constitutive elements put one after the other, even in
early AD (see Fig. 4). In these cases, patients seem
able to recognize and reproduce single well-known
elements but are unable to reproduce complex spatial relationships correctly. Another simplification
error may consist in the reproduction of more familiar
or simpler figures instead of more complex ones (e.g.,
a square instead of a diamond). As the disease progresses, patients usually become unable even to draw
simple figures correctly, as they no longer had access
to well-consolidated motor subroutines and can show
peculiar patterns of behavior, such as the closing-in
phenomenon [2325, 90, 91] (see Figs. 2 and 3).
Drawing disorders in prodromic (aMCI) and
clinical forms of AD
Drawing disorders are not usually present in MCI,
at least when copying of simple figures is employed
[92]. However, a different pattern might emerge as a
function of clinical characteristics of MCI patients,
particularly if more complex tasks are used. In a
study on brain morphometric correlates of CDT
in patients with MCI or AD, Thomann et al. [86]
observed that, even though MCI patients did not differ from matched healthy controls in copying simple
geometrical drawings, CDT could discriminate MCI
from matched healthy controls and AD from MCI
patients. Analogously, in a further brain morphometric study on MCI and AD patients, accuracy in
copying the ROCF was significantly different in MCI
patients, AD patients, and healthy controls [87]. It
has also been observed that MCI patients make conceptual and graphic errors more often than matched
healthy controls, and that AD patients score lower
and make significantly more conceptual, graphic, and
spatial-planning mistakes than MCI individuals, thus
suggesting that a detailed scoring system is necessary
to differentiate individuals with MCI from healthy
adults [63, 93]. Scoring systems focusing on hand
and number placement might better differentiate MCI
individuals from healthy controls, but the solidity of
CDT as a screening tool for MCI has been questioned [94]. In this respect, it should be taken into
account that cognitive characteristics of MCI individuals might correlate with performance on CDT. It is
very important to acknowledge at this point that MCI
371
372
373
374
375
376
377
378
379
380
381
382
383
384
385
386
387
388
389
390
391
392
393
394
395
396
397
398
399
400
401
402
403
404
405
406
407
408
409
410
411
412
413
414
415
416
417
418
419
420
421
422
423
424
425
426
427
428
429
430
431
432
433
434
435
436
437
438
439
440
441
442
443
444
445
446
447
448
449
450
451
452
453
454
455
456
457
458
459
460
461
462
463
464
465
466
467
468
469
470
L. Trojano and G. Gainotti / Drawing Disorders in Dementia
patients are rather heterogeneous from the etiological
point of view and that amnesic MCI can be considered
as that most related to development of AD [95, 96].
In line with this caveat is the fact that, a recent study
contrasting MCI of the amnesic, dysexecutive, or
multi-domain type on CDT [97] confirmed that aMCI
did not differ from a matched sample of healthy controls, whereas both dysexecutive and multi-domain
MCI individuals made a significantly larger number
of errors in hand and number placement.
Poor performance on CDT might predict future
development of AD in patients with MCI [98], but
not all qualitative scoring procedures might be sufficiently sensitive to capture longitudinal changes
of CDT from MCI to AD [61]. A recent metaanalysis [99] confirmed that the CDT might reveal
a useful measure of cognitive decline over time, and
that conceptual clock drawing errors (with particular mention of hand and number placement) would
be most informative about the cognitive decline.
This meta-analysis also showed that CDT might
differentiate individuals who are going to develop
dementia in subsequent years, thus being included
among the tests helpful for predicting conversion to
dementia.
Drawing disabilities in early and late onset
forms of AD
The structural or functional neuroimaging abnormalities correlate with the clinical features in AD
patients, because typical late-onset patients (LOAD)
present with memory disorders and medial temporal lobe atrophy, whereas focal neocortical forms
of AD prevail in early-onset patients (EOAD) and
are associated with executive-behavioral disorders,
logopenic aphasia, and (in posterior cortical atrophy)
with progressive visual-spatial disorders [100, 101].
Some authors have, therefore, examined the relations
between age at onset and drawing disorders in AD
patients, and reported a high prevalence of visuoconstructional disabilities, assessed with the copy of the
ROCF, in EOAD patients [101103]. In some studies [102, 103], but not in others [101], these drawing
disorders were associated with visuospatial deficits.
Furthermore, some studies [104] have shown that
the presence and severity of drawing disorders certainly depends on the AD phenotype and not just on
age. Most frequent and severe drawing disorders are
found in posterior cortical atrophy (PCA), which is
associated with prominent visuospatial impairments
and relative preservation of memory, insight, and
judgment [105]. PCA is associated with atrophy in
the occipital, parietal, and posterior temporal lobes
[106], but recently a lesion of long white-matter
tracts, including the superior and inferior longitudinal
fasciculi and the inferior fronto-occipital fasciculus,
has also been documented [107]. This early-onset
AD-related pathology gives rise to complex visuospatial difficulties, such as visuoperceptual impairments
[108], optic ataxia, simultanagnosia, gaze apraxia
(often with the complete spectrum of Balint syndrome), and even egocentric [109, 110] or allocentric
[111] unilateral spatial neglect. All such visuospatial impairments have a strong impact on drawing
abilities, affecting both spontaneous drawing and
copying, and giving rise to severe displacements of
drawing elements, omissions, gross spatial distortions (exploded drawings) [112].
Drawing disorders in different stages of
evolution of AD
A strict relation between the progression of visuoperceptual spatial impairment and the progressive
deterioration of the performance on copying the
ROCF has been reported [89] (see Fig. 4). Mild AD
usually spares basic visual sensory processes and
affects all high-order visual processes, along both the
ventral (occipito-temporal) and the dorsal (occipitoparietal) visual streams [113]. Caine and Hodges
[114] carried out two separated studies to investigate
ventral and dorsal visual functions in a sample of
AD patients at early stages of the disease. A small
subsample of patients were impaired on visuospatial
tasks, thus suggesting that this small group of patients
with prominent visuospatial disorders might represent one end of a continuous spectrum at the other
end of which are patients affected by a focal degenerative dementia involving occipito-parietal cortex, the
so-called PCA [115118]. In the moderate stages of
AD, visuospatial impairments would become more
evident, and play a relevant role in the development of constructional disorders [89]. More recently,
Guerin et al. [119] examined the cognitive mechanisms underlying the constructional performance
of AD patients at different stages of the disease by
means of a copying task and of visuospatial tasks
measuring spatial exploration (visual search tasks),
judgment of spatial relations, and planning abilities.
The results suggested that cognitive defects underlying constructional impairment in patients with AD
involved the early phases of spatial-constructional
processing, likely exploration and judgment of
471
472
473
474
475
476
477
478
479
480
481
482
483
484
485
486
487
488
489
490
491
492
493
494
495
496
497
498
499
500
501
502
503
504
505
506
507
508
509
510
511
512
513
514
515
516
517
518
519
520
L. Trojano and G. Gainotti / Drawing Disorders in Dementia
521
522
523
524
525
526
527
528
529
530
531
532
533
534
535
536
537
538
539
540
541
542
543
544
545
546
547
548
549
550
551
552
553
554
555
556
557
558
559
560
561
562
563
564
565
566
567
568
569
570
spatial relationships, rather than the late stage of
planning.
characteristically affected in AD, as well as visuospatial cognition in general [76].
Mechanisms giving rise to drawing disorders in
AD patients
DRAWING DISORDERS IN THE
DIFFERENTIAL DIAGNOSIS BETWEEN
AD AND VASCULAR DEMENTIA OR
OTHER DEGENERATIVE FORMS OF
DEMENTIA
The drawing impairment in AD patients may stem
from different cognitive mechanisms.
In recent years, the different mechanisms giving
rise to CA in AD patients have been tackled with by
means of morphometric and neurofunctional studies.
However, such studies did not provide strongly convergent data. For instance, in a sample of AD and
MCI patients overall score on CDT was inversely
correlated with atrophy in the middle and superior
temporal gyri (BA 21 and 22) bilaterally, but more
strongly in the left hemisphere, and in the left entorhinal area (BA 28) [86], whereas in a sample of AD
patients impaired performance on the ROCF copying
task was correlated with atrophy in several frontotemporo-parietal regions in the right hemisphere [87].
In a further study [5], impaired performance on a
copying test was correlated with bilateral parietal
atrophy. The differences between such studies might
originate from different characteristic of the AD samples, and from the neuropsychological measure used
for assessing drawing. Several recent neurofunctional
studies are illustrative of these sources of variability. In a large sample of AD patients, Shon et al.
[120] found that drawing from memory or copying a clock face correlated with regional glucose
metabolism in bilateral temporo-parietal regions, but
these correlations changed as a function of dementia
severity. Matsuoka et al. [58] reported another representative instance of variability in neurofunctional
findings depending on the neuropsychological measure in a large sample of drug-nave AD patients,
in whom overall performance on CDT, the partial
score on locating numbers of the clock and the
partial score on setting the hands were correlated
with atrophy in distinct parietal, posterior temporal and frontal regions. A PET study using copying
of simple geometrical figure as a measure of constructional abilities showed, instead, an exclusive
correlation of copying performance with the left inferior parietal lobule and the left inferior frontal gyrus
[121].
These data explain why the diffuse involvement of
several areas of the brain in AD can impair drawing performance since the early clinical stages of
the diseases, particularly when drawing is assessed
by means of complex stimuli. Therefore, drawing is
The widespread involvement of several neural networks in drawing can explain the clinical observation
of frequent drawing disorders in AD, but also implies
that drawing disorders are often found in other forms
of dementia, both of vascular and degenerative nature.
In recent years a growing number of studies attempted
to ascertain whether drawing could provide additional information for refining clinical differentiation
among dementias. Here we will provide an overview
of such studies, from which it will emerge that it can
be difficult to disentangle drawing disorders in AD
from those shown by patients affected by other kinds
of progressive dementias, and that some distinctive
features might be captured by qualitative analysis
of drawing productions (see Table 1). As it will be
argued in the next section, it is possible, however,
that if patients with different etiologies share some
neural lesions or cognitive defect, they will produce
similar error types in drawing.
Drawing disorders in vascular dementia
Since AD and vascular dementia (VaD) are the
most common forms of dementia in old age, several
investigations tried to evaluate if drawing disorders can be useful to differentiate the two forms
of dementia. In particular, a few studies compared
drawing abilities in AD and VaD patients on the
CDT, without providing convergent evidence. Looi
and Sachdev [122] reviewed 11 studies comparing
the performance of VaD and AD patients in the area
of constructional apraxia, using tests such as block
design, CDT, or the ROCF copying task. Eight of
the studies showed no difference between the two
groups, while in three it was found that the AD
were less impaired. Wiechmann et al. [123] did not
find difference in accuracy on CDT between AD
and VaD. Instead, in a study on a sample of outpatients matched for general cognitive impairment VaD
scored significantly lower than AD on CDT, likely
related to poorer executive abilities in VaD patients
[124]. Kitabayashi et al. [125] stratified their patient
sample by general cognitive impairment, and found
571
572
573
574
575
576
577
578
579
580
581
582
583
584
585
586
587
588
589
590
591
592
593
594
595
596
597
598
599
600
601
602
603
604
605
606
607
608
609
610
611
612
613
614
615
616
617
618
10
L. Trojano and G. Gainotti / Drawing Disorders in Dementia
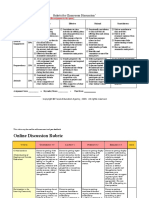
Table 1
Summary of studies comparing drawing disorders in Alzheimers Disease and in other forms of dementia
First author
Comparison AD-VaD
Wiechmann [123]
Kitabayashi [125]
Fukui [126]
Graham [127]
Comparison AD-FTD
Rascovsky [131]
Blair [132]
Razani [133]
Thompson [134]
Drawing test
CDT
CDT
CDT, figure copying
ROCF
CDT, figure copying
CDT
CDT
Figure copying
Possin [135]
Perri [136]
Gorno-Tempini [137]
Grossi [138]
Gasparini [139]
Simplified ROCF
ROCF
ROCF
ROCF
ROCF
Rascovsky [141]
Mendez [142]
Comparison AD-LBD
Nervi [152]
Crowell [153]
Tiraboschi [154]
Cahn-Wiener [156]
Hamilton [157]
Cagnin [158]
Palmqvist [159]
Gnanalingham [162]
Ala [164]
Cormack [165]
Connor [166]
Caffarra [167]
Figure copying
Figure copying
Figure copying
Figure copying
Figure copying
CDT
Clock copying
CDT
CDT, cube copying
CDT, clock copying
Pentagon copying
Pentagon copying
Pentagon copying
Figure copying,
pentagon copying
Findings
No difference in accuracy
Conceptual and spatial/planning errors in AD in all disease stages;
conceptual and graphic errors in moderate-severe VaD
No difference at mild disease stages; sVaD worse
than AD on both tasks at severe stages
No difference between AD and sVaD
AD worse than FTD on overall CDT score; no differences in figure copying
AD worse than FTD; less conceptual, spatial
and planning errors in FTD than in AD
AD worse than right- and left-onset FTD
AD worse than FTD; less spatial errors,
but more perseverations in FTD than in AD
AD worse than FTD
AD worse than FTD
AD worse than non fluent PA
No difference between AD and bvFTD
No overall difference between AD and bvFTD;
AD better than bvFTD in drawing details
Steeper decline of copying abilities in FTD with respect to AD
No 2-year decline in FTD
LBD worse than AD
LBD worse than AD
LBD worse than AD; no differences in pentagon copying
No differences in overall score, but more conceptual and planning errors in LBD
No differences, but lower scores predicted steeper decline in LBD
LBD worse than AD
LBD worse than AD
No difference in CDT; LBD worse than AD in clock copying
LBD worse than AD
LBD worse than AD
No difference
No difference in figure copying,
worse scores in LBD on an analytic scoring system for pentagon copying
AD, Alzheimers disease; VaD, vascular dementia; sVaD, subcortical VaD; FTD, frontotemporal dementia; bvFTD, behavioral variant of
FTD; PA, progressive aphasia; LBD, Lewy body dementia; CDT, Clock drawing test; ROCF, copy of Reys complex figure. Reference
numbering follows the text.
619
620
621
622
623
624
625
626
627
628
629
630
631
632
633
634
635
that CDT can well discriminate patients with AD or
VaD from healthy controls, but the main differences
between AD and VaD patients were in the relative
percentage of error types, with AD patients showing
many conceptual and spatial/planning errors independently from disease severity and VaD patients
showing conceptual errors and graphic difficulties
only in presence of moderate cognitive impairment
(see Fig. 1). Partially different findings have been
reported by Fukui et al. [126], who did not find differences between AD and subcortical VaD patients
at mild disease stages on CDT and figure copying,
whereas at later stages VaD achieved significantly
lower scores than AD in both drawing tasks. Graham
et al. [127] also found that patients with subcortical
VaD were more impaired than AD patients on executive/attentional functioning, and visuospatial and
perceptual skills. In their recent review on CDT, Tan
et al. [128] concluded that the overall accuracy on
CDT in AD versus VaD patients did not provide
consistent results, whereas qualitative analyses might
reveal useful differences between the two groups of
patients, since VaD patients tended to show more frequent executive/planning or perseveration errors than
AD patients.
Drawing disorders in frontotemporal dementia
The relative preservation of visuospatial and
constructional abilities is a feature capable of distinguishing FTD from other degenerative dementias
and, notably, AD [129, 130]. Consistent with this
idea, a few studies observed better performance on
CDT in FTD compared with AD. For instance, in
636
637
638
639
640
641
642
643
644
645
646
647
648
649
650
L. Trojano and G. Gainotti / Drawing Disorders in Dementia
651
652
653
654
655
656
657
658
659
660
661
662
663
664
665
666
667
668
669
670
671
672
673
674
675
676
677
678
679
680
681
682
683
684
685
686
687
688
689
690
691
692
693
694
695
696
697
698
699
700
701
702
a sample of autopsy-verified FTD patients, Rascovsky et al. [131] observed similar scores in copying
geometrical figures, but higher overall CDT scores
in FTD compared to AD patients. In the same vein,
Blair et al. [132] reported higher overall scores, and
fewer conceptual, spatial, and planning errors in FTD
compared to the AD group (see Fig. 1). Comparing the performance of AD patients with those of
patients with right and left FTD, Razani et al. [133]
also confirmed that the AD group displayed significant impairments in visual-constructional ability
relative to the two FTD groups. On the other hand,
Thompson et al. [134] observed that FTD patients
outperformed AD patients in copying geometrical
figures of different complexity showing a lower number of spatial errors, but were also characterized by
a higher number of perseverative errors and of poor
organization of the copy than AD patients. Thus spatial errors were highly predictive of AD, whereas
organizational errors, perseverations, or overelaborated copies were significant predictors of FTD (see
Figs. 24). Data supporting the hypothesis of a prevalence of spatial errors in the drawings of AD patients
and of executive disorders in those of FTD patients
have also been obtained in a study by Possin et al.
[135], that used quantitative morphometric evaluation of structural MRI. These authors reported that
a sample of patients with the behavioral variant of
FTD performed better than a sample of AD patients in
copying drawings, but also observed that the drawing
impairments in the two patient groups might be based
on different cognitive and neuroanatomical correlates. In AD patients poor figure copy was associated
with performance on spatial perception and attention
tasks, and correlated significantly with volumes in
the right parietal cortex. In FTD patients, instead,
performance on figure copy correlated significantly
with scores on spatial planning and working memory
tasks, and correlated with right dorsolateral prefrontal cortex volumes. These observations would fit
clinical data demonstrating that patients with prominent behavioral disorders and frontal involvement
(behavioral variant FTD, bvFTD) outperformed AD
patients on ROCF immediate reproduction [136],
and that patients with prominent language deficits
(non-fluent progressive aphasia) did not differ from
healthy controls on cube copying and ROCF immediate reproduction [137]. Therefore, several studies
confirmed the basic tenet that visuospatial skills and
drawing abilities are relatively preserved in FTD,
but at least two studies did not detect differences
in overall accuracy on ROCF immediate reproduc-
11
tion between bvFTD and AD patients [138, 139]. It
is thus possible that during the disease course FTD
patients might show relatively preserved constructional abilities in the early stages, whereas differences
between FTD and AD might blur in late stages of
the disease. This hypothesis might find support in
a meta-analysis showing that constructional abilities
assessed on copying the ROCF quickly deteriorate
as FTD progresses [140], and in a longitudinal study
showing a trend toward a steeper decline of copying abilities in FTD with respect to AD [141, but for
contrasting findings see 142].
Divergences about drawing disorders in FTD
will be reconciled by taking into account the heterogeneous clinical features and neuropathological
underpinnings of the disease [108, 143]. In this
respect, it is important to underline a distinction
between the drawing abilities of patients with bvFTD
and those of patients with the temporal variant or
semantic dementia (SD), because both are relatively
spared on copying tasks, but the latter can be either
enhanced or selectively impaired in drawing from
memory the typical shape of common objects. The
seemingly contradictory data about drawing abilities in SD are illustrated by results obtained by
Bozeat et al. [19] and by Miller et al. [144146].
Bozeat et al. [19] showed that when SD patients
are required to produce drawings of concrete objects
from dictation of their names, their drawings are
characterized by a loss of the distinctive features of
the represented objects. On the other hand, Miller
et al. [144146] showed that in the early stages of
SD, patients with left anterior temporal lobe atrophy
and severe anomia increase their drawing abilities,
copying with great precision and sometimes become
artists. In these cases, artworks show an enhanced
tendency to realism. This improvement of visuoconstructive and artistic abilities was attributed by Miller
et al. [144, 146] to the sparing of the parietal lobe
and of the right hemisphere, considered as dominant
for the three key features of visual artistry: visual
constructive ability, spatial attention, and internal representation. The apparent contradiction between data
reported by Bozeat et al. [19] and by Miller et al.
[144146] is probably due to the different stage of
evolution of SD in which observations were gathered (an early stage of SD, with unilateral left sided
atrophy in the case of Miller et al. [144146] and
a later stages of SD, with bilateral anterior temporal lobe (ATL) atrophy in the case of Bozeat et al.
[19] observations). Gainotti [147, 148] has, indeed,
recently reviewed data showing that the format of
703
704
705
706
707
708
709
710
711
712
713
714
715
716
717
718
719
720
721
722
723
724
725
726
727
728
729
730
731
732
733
734
735
736
737
738
739
740
741
742
743
744
745
746
747
748
749
750
751
752
753
754
12
L. Trojano and G. Gainotti / Drawing Disorders in Dementia
765
conceptual representations is mainly verbal in the left
ATL and mainly sensorial/pictorial in the right ATL.
In the early stages of SD the atrophy of the left ATL
can release, with a mechanism labeled paradoxical
functional facilitation by Kapur [149] the pictorial
representations stored in the right ATL, leading to an
enhancement of pictorial abilities. On the other hand,
in later stages the bilateral spread of atrophy provokes
a complete disruption of verbal and non-verbal conceptual representations of concrete entities, leading
to an inability to draw them from memory.
766
Drawing disorders in Lewy body dementia
755
756
757
758
759
760
761
762
763
764
767
768
769
770
771
772
773
774
775
776
777
778
779
780
781
782
783
784
785
786
787
788
789
790
791
792
793
794
795
796
797
798
799
800
801
802
803
804
In LBD, visuospatial difficulties are often early and
prominent [150]. Visuospatial tasks, such as object
size discrimination, form discrimination, overlapping
figure identification, and visual counting tasks, may
reveal more impaired performances in LBD than in
AD, and these defects likely contribute to the disproportionate impairment in constructional tasks in LBD
patients [151153].
In line with these observations, case series of
pathologically verified LBD [154] as well as systematic reviews [155] confirmed that an impairment
in copying geometrical figures is very common in
LBD patients since early stages of the disease. However, several studies employing CDT did not report
significant differences in overall total score in LBD
and AD patients [156, 157], likely because of the
complexity of the task (see Fig. 1), although at least
two studies reported significantly lower overall scores
in LBD versus AD patients [158, 159]. A SPECT
study showed that LBD patients with defective
performance on CDT presented more marked hypoperfusion in a frontal-subcortical network, involving
frontal eye fields and the thalamus, with respect to
LBD patients with normal CDT scores [160]. A
more recent neurofunctional investigation by PET
revealed, instead, that, after controlling for overall
cognitive impairment, there was a direct association between frontoparietal dysfunction and impaired
CDT performance in LBD [161].
The early and prominent impairment of visuospatial processing in LBD led some authors to suggest
that LBD patients may be characterized by parallel
impairments in free drawing and in figure copying
since early stages of the disease whereas AD patients
would show relative sparing of figure copying ([162],
but also see [163]). Likely because of its complexity,
copy of the ROCF has not been extensively used in
LBD, whereas some interesting observations came
from the copy of the intersecting pentagons included
in the MMSE. Ala et al. [164] found that patients with
LBD were more likely than those with AD to copy
pentagons incorrectly, and suggested that this impairment might help identifying LBD patients. Cormack
et al. [165] confirmed that LBD patients show significantly lower performance in copying pentagons with
respect to AD; moreover, while in AD the impairment in copying figures was correlated with general
cognitive deterioration, in LBD drawing was correlated with visuospatial tasks only, thus suggesting the
existence of a specific defect in this disease. Different scoring criteria can likely explain the reason why
other authors failed to detect differences between
LBD and AD in pentagon copying [108, 159], but
more extended copying tests might show significantly lower performance in LBD with respect to
AD patients [108]. Recently, it has been demonstrated
that qualitative analysis of the pentagon copy test can
provide additional information for distinguishing AD
from LBD patients, since a lower number of angles
is among distinctive features of LBD patients copies
[73, 167], and can also predict development of LBD
in MCI patients [74].
PECULIAR ASPECTS OF DRAWING
DISORDERS IN DEMENTIA
In the previous sections of this paper it has been
repeatedly underlined that qualitative observations
(i.e., errors analysis) might provide additional information about the cognitive and neural correlates of
drawing disorders in patients with different kinds
of dementia. Some qualitative phenomena observed
in drawing tasks in demented patients deserve,
therefore, some brief comments, because of their frequency and their potential clinical usefulness.
Graphic perseveration
Generally speaking, perseveration can be considered among productive (or positive) pathological
signs, since it consists in iterative behavioral
responses, not adequate to the current stimulus (see
Figs. 24) [168]. Patients may produce the same figure repeatedly, in response to only one stimulus, or
replicate stimulis elements (continuous perseveration, according to Sandson and Albert) [169]; on other
occasions, patients may inappropriately draw figures
already drawn in previous trials, instead of reproducing the current stimulus (recurrent perseveration)
[169].
805
806
807
808
809
810
811
812
813
814
815
816
817
818
819
820
821
822
823
824
825
826
827
828
829
830
831
832
833
834
835
836
837
838
839
840
841
842
843
844
845
846
847
848
849
850
851
852
L. Trojano and G. Gainotti / Drawing Disorders in Dementia
853
854
855
856
857
858
859
860
861
862
863
864
865
866
867
868
869
870
871
872
873
874
875
876
877
878
879
880
881
882
883
884
885
886
887
888
889
890
891
892
893
894
895
896
897
898
899
900
901
902
903
904
A specific kind of perseveration is observed in CDT,
when patients produce repeatedly the same numbers,
or start numeration over and over (see Fig. 1). These
errors in clock drawings have been described in a small
proportion of AD patients [170], but would increase in
moderate to severe stages of the disease [88]. Ryan et
al. [171] compared graphic performances on the Bender visuomotor Gestalt test and on CDT in AD with or
without wandering, and observed a larger number of
both continuous and recurrent perseverative errors in
individuals showing the wandering phenomenon, thus
suggesting a relationship between perseveration and
behavioral control.
A first study specifically comparing graphic perseverations in patients with AD or VaD showed that
perseverations were more frequent in VaD than in
AD [172]. However, Cosentino et al. [173] assessed
patients on CDT and on copying clocks and observed
that perseveration and closing-in (see below) in AD
and VaD were more frequent in patients with higher
number of white matter lesions and with more marked
impairment on executive frontal tasks. These findings
suggested that the executive impairment associated
with frontal-subcortical dysfunction contributes to the
genesis of perseveration in clock drawing in dementia. Recently, in a retrospective study on a large patient
sample, De Lucia et al. [174] observed that frequency
of graphic perseverative errors was similar in AD
and VaD, and that patients with moderate-to-severe
dementia produced a significantly higher number of
perseverations than individuals with mild dementia.
In both groups graphic perseverations were related
with frontal and visuoconstructional impairments,
thus supporting the view that frontal-executive defects
canhamperinhibitionofiterativegraphicproductions.
In FTD, patients perseveration in drawing would
be often present also in early stages of the disease
while specific disturbances in reproducing spatial
relationships would become evident later during the
course of the disease [175]. In a systematic analysis
of errors observed in a wide range of neuropsychological tests, Thompson et al. [134] reported that
FTD patients outperformed a group of AD patients
in drawing tasks, but the most distinctive feature
between the two groups were perseveration and poor
overall organization (see Figs. 24). It is worth
mentioning, however, that other studies focusing on
qualitative error analysis [138, 139] did not observe
a higher proportion of graphic perseverations in FTD
with respect to AD.
In LBD, several authors suggested that less
efficient executive control might induce higher fre-
13
quency of perseveration than in AD [176, 177],
but perseverations in drawing tasks have not been
assessed specifically.
Rotation
In copying stimuli, some patients may respect
spatial relationships among constituent elements but
reproduce a model with general orientation different
from the stimulus, e.g., rotating the reproduction by
90 or 180 degrees (see Fig. 4). This behavior has been
already mentioned in early studies on constructional
apraxia [27, 178, 179] and has been reported, although
rarely, in subsequent descriptions of patients with
brain lesions. From a consecutive unselected series of
240 neurological patients, Solms et al. [180] identified
16 patients who reproduced the ROCF with its major
axis vertically rotated, independently from accuracy
in reproducing spatial relationships among inner elements. Seven of these patients had diffuse cerebral
involvement, but all remaining cases showed a lesion
involving frontal regions. The authors suggested that
this behavior could reflect the lack of planning and verification abilities of frontal patients [180]. In another
case series of patients with AD, rotation of one or
both items of the MMSE interlocking pentagons was
reported in about 5% of patients [181]. Frequency of
rotation of MMSE pentagons would not differ in AD
or LBD patients, but it could progressively increase
during the disease course in LBD patients [73].
Recent findings suggest that complex visuoperceptual and planning mechanisms might contribute to the
genesis of rotations. In a retrospective study on a large
sample of patients with MCI or degenerative dementia who underwent copy and recall of the ROCF,
Isella et al. [182] observed rotation on the copy condition in 2.7% patients and on recall in 3.3% patients.
In a subsequent prospective study on a mixed sample of patients with degenerative dementias or focal
brain lesions, rotation at the copy of the ROCF was
associated with visuospatial and selective attention
impairments, and with more severe temporo-parietooccipital atrophy or hypometabolism, whereas no
specific profile of cognitive impairment distinguished
patients with rotation at recall of the ROCF, in whom
frontal abnormalities were more frequent [183].
Closing-in
In copying tasks, demented patients often show the
tendency either to put the pencil directly over the
model, producing a scrawl, or to overlap the lines
905
906
907
908
909
910
911
912
913
914
915
916
917
918
919
920
921
922
923
924
925
926
927
928
929
930
931
932
933
934
935
936
937
938
939
940
941
942
943
944
945
946
947
948
949
950
951
952
14
953
954
955
956
957
958
959
960
961
962
963
964
965
966
967
968
969
970
971
972
973
974
975
976
977
978
979
980
981
982
983
984
985
986
987
988
989
990
991
992
993
994
995
996
997
998
999
1000
1001
1002
1003
1004
L. Trojano and G. Gainotti / Drawing Disorders in Dementia
of the model with those of the copy or to draw very
near to the models elements (see Figs. 2 and 3).
Such behavior, termed closing-in (CI), has been first
described by Mayer-Gross [23], and later reported
more often in demented patients than after focal brain
lesions [24, 90]. Among dementing syndromes, CI is
predominant in AD [88, 184], suggesting the idea
that CI might represent a neuropsychological marker
for clinical diagnosis of AD [90, 185, 186]. One
more recent study [25] confirmed that CI is more frequent in AD with respect to VaD patients, and that
the two patient groups also tended to show qualitatively different CI phenomena, as AD patients more
often overlapped at least one element of the copy onto
the model (adherent-CI), whereas VaD patients more
often drew close to the model without overlapping
onto it (near-CI). On the other hand, one retrospective study showed that CI is as frequent in AD as in
FTD patients, but did not provide qualitative observations [187]. Indeed, in a sample of patients with the
behavioral variant of FTD, near-CI has been observed
more frequently than adherent-CI, and was often (but
not obligatorily) associated with other imitation and
utilization behaviors [188]. Notably, more frequent
occurrence of near-CI than of adherent-CI has been
recently reported also in non-demented Parkinsons
disease patients [189], whereas the reverse pattern
has been observed in Parkinsons disease dementia
[190].
In his original description, Mayer-Gross [23]
ascribed CI to a disturbance in performing spatial
movements of hands and fingers correctly. In later
years, interpretative accounts of CI clustered within
two main streams. The first interpretative framework
might originate from the consideration that CI could
occur when patients who are unable to structure an
empty space look for a reference point to solve difficult constructional dilemmas [191]. Following this
suggestion, in recent years CI has been considered as
a compensatory behavior implemented to overcome
deficits of visuospatial skills or of visuospatial working memory [192]. In this compensation account,
patients with impaired ability to represent the model,
or to hold its representation for the need of reproducing it, might tend to close-in to the model in the
attempt to reduce their difficulties. Such a compensation hypothesis received support by the finding
that complex models could increase severity of CI
in AD patients [192], and by the observation that AD
patients with CI showed more severe impairments on
several visuospatial tests, compared to AD patients
without CI [193].
The alternative account might be traced back to the
hypothesis that CI might represent a primitive reflex
leading patients to be strongly attracted by the model
and be unable to detach from it [24]. In this attraction framework, CI would represent a default
behavior released by defects of attentional-executive
abilities [194, 195]. In analogy with the compensation hypothesis, the attraction hypothesis predicts
that CI would be enhanced in dealing with complex
models because they likely imply high attentional
load, and reduce available resources for monitoring graphic productions. However, this hypothesis
specifically envisages strong correlations between CI
and frontal/executive dysfunction, and foresees that
CI can be triggered by high attention-demanding task
conditions. Several converging pieces of evidence
supported this account, since a significant correlation between CI and frontal/executive dysfunction
has been reported in MCI [196], AD [191], VaD [25],
and Parkinsons disease [189], and in such diseases
copying geometrical figures in dual-task conditions
enhanced CI [25, 184, 197]. A first attempt at identifying the neural correlates of CI in AD patients
would point to bilateral orbito-frontal cortex as the
area in which atrophy was significantly associated to
presence of CI [198].
Most available evidence would thus suggest that,
independently from the diagnosis, patients sharing
similar cognitive impairment might produce CI, and
this attempt at identifying cognitive and neural correlates of specific errors might provide further insights
on drawing disorders in dementia.
CONCLUDING REMARKS
It is interesting to note, at the end of this review,
that several patients reported by Kleist [27] and
Mayer Gross [23] in the earliest studies on constructional apraxia and drawing disorders were affected by
dementia. It is also worth of note that, in one of the
first studies aiming to investigate with standardized
tests the patterns of neuropsychological impairment
shown by various diagnostic groups of dementia,
Gainotti et al. [199] showed that AD patients were
particularly impaired on memory and drawing tasks.
In another study, Villa et al. [200] showed that
the coexistence of mental deterioration was more
strongly associated with drawing disabilities than laterality of lesion, or intrahemispheric locus of lesion
in focal brain-damaged patients. More recent investigations have followed two complementary strategies
1005
1006
1007
1008
1009
1010
1011
1012
1013
1014
1015
1016
1017
1018
1019
1020
1021
1022
1023
1024
1025
1026
1027
1028
1029
1030
1031
1032
1033
1034
1035
1036
1037
1038
1039
1040
1041
1042
1043
1044
1045
1046
1047
1048
1049
1050
1051
1052
1053
L. Trojano and G. Gainotti / Drawing Disorders in Dementia
1054
1055
1056
1057
1058
1059
1060
1061
1062
1063
1064
1065
1066
1067
1068
1069
1070
1071
1072
1073
1074
1075
1076
1077
1078
1079
1080
1081
1082
1083
1084
1085
1086
1087
1088
1089
1090
1091
1092
1093
1094
1095
1096
1097
1098
1099
1100
1101
1102
1103
1104
1105
to clarify incidence and qualitative aspects of drawing disabilities observed in AD and other forms of
dementia. The first strategy consisted in adopting
short drawing tasks that could be particularly appropriate to investigate drawing disorders in demented
patients. The second strategy consisted in taking into
account the nature and the qualitative aspects of
drawing disorders that could facilitate the differential
diagnosis between AD and the other clinical forms of
dementia.
The most popular task adopted according to
the first strategic approach is CDT, which allows
obtaining different scores (e.g., graphic difficulties, related to elementary motor disorders; stimulus
bound responses, resulting from inhibition difficulties; conceptual deficits, related to semantic memory
disorders; perseverations resulting from frontal lobe
dysfunctions and visuospatial disorders), and can be
administered both under verbal command and in the
copy of a pre-drawn clock (see Fig. 1). According
to several authors [21, 88, 125, 126, 201, 202], the
CDT is able to distinguish different severity levels
and clinical forms of dementia, but other authors
reported contrasting findings with respect to both
issues [65, 123, 128, 131, 158]. These deceiving
results are probably due to two main factors. The
first is that the CTD is basically a screening test and as
such cannot provide a large and diversified amount of
clinical information. The second is that many administration procedures and scoring systems have been
proposed [20, 21, 5457], but there is no consensus
as to which is the most useful for dementia screening or for providing hints at a differential diagnosis
among different forms of dementia. It is also possible
that different diagnostic criteria and, above all, rate
of diagnostic uncertainty might have biased some of
the findings reported in the present review, and this
concern might only be overcome by gathering further well-designed and accurate studies on drawing
disorders in the different forms of dementia.
More substantial results have been obtained following the second research strategy, because several
studies have shown that the discrepancy between command and copy condition (in the CDT or in other
drawing tasks) is greater in forms of dementia, such
as the subcortical vascular dementia [127, 128] or the
bvFTD [129, 130, 134136], which are characterized
by a prominent deficit of the executive and control
functions. Furthermore, the drawing impairments in
AD and FTD patients could be based on different cognitive and neuroanatomical mechanisms in agreement
with the different prevalence of lesions in these two
15
diseases [134, 135]: in AD patients poor figure copy
was associated with performance on spatial perception and attentional tasks, and correlated significantly
with volumes in the right parietal cortex; in FTD
patients, instead, performance on figure copy correlated significantly with scores on spatial planning
and working memory tasks, and was connected with
right dorsolateral prefrontal cortex volumes. Very different from the drawing disorders of patients with
bvFTD are those of patients with semantic dementia,
because both obtain good performances on copying
tasks, but the latter are selectively impaired in drawing
from memory the typical shape of common objects.
In fact, when SD patients were given the names of
concrete objects and asked to produce the corresponding designs, these drawings were characterized by
a loss of the distinctive features of the represented
objects, resulting from disruption of the corresponding conceptual representations, stored in the right and
left anterior temporal lobes [19, 203]. Copying tasks
are, therefore, substantially spared in degenerative
diseases mainly involving the frontal (bvFTD) or temporal (SD) cortices and might be mildly impaired in the
early stages of standard forms of AD, in which atrophy prevails in the medial temporal lobes, although
neuroimaging studies repeatedly showed a pattern
of reduced metabolism in the temporo-parietal areas
[204, 205]. A much more severe impairment in copying tasks is observed in early-onset AD patients and
in PCA variant, in which severe constructive defects
are usually associated with progressive visual-spatial
disorders, including Balint syndrome and unilateral
spatial neglect [100, 101]. A very similar pattern of
drawing impairment is found in LBD, in which visuospatial difficulties are often early and prominent and
contribute to the disproportionate impairment in constructional tasks observed in these patients [151153].
We can, therefore, conclude that the pattern of
drawing disorders observed in AD and in other forms
of dementia can be explained if we take into account
the main functions of the neural networks involved
in these forms of degenerative diseases. Among
the peculiar drawing patterns that are observed in
the moderate-to-severe forms of dementia the most
important is certainly the closing-in symptom (see
Figs. 2 and 3), which is significantly more frequent
and more severe in AD than in vascular forms of
dementia [24, 25], because AD patients tend to put
the pencil directly over the model, or to overlap the
lines of the model with those of the copy (adherentCI), whereas VaD patients more often draw in close
proximity to the model without overlapping onto it
1106
1107
1108
1109
1110
1111
1112
1113
1114
1115
1116
1117
1118
1119
1120
1121
1122
1123
1124
1125
1126
1127
1128
1129
1130
1131
1132
1133
1134
1135
1136
1137
1138
1139
1140
1141
1142
1143
1144
1145
1146
1147
1148
1149
1150
1151
1152
1153
1154
1155
1156
1157
16
1158
1159
1160
1161
1162
1163
1164
1165
1166
1167
1168
1169
1170
1171
1172
1173
1174
1175
L. Trojano and G. Gainotti / Drawing Disorders in Dementia
(near-CI). If the CI might improve the differential
diagnosis between AD and VaD, it is less useful in
the distinction between AD and FTD, because the
role of the frontal lobes in its production is still under
scrutiny. From this point of view, it is important
that recent neuroanatomical data demonstrated the
selective association of atrophy in the orbito-frontal
areas, implied in inhibiting primitive reflexes, with
the closing-in phenomenon [198]. Even if several
neuropsychological and pathophysiological aspects
of drawing disorders in AD and other forms of dementia require further clarification, the clinical interest
of drawing tasks in the differential diagnosis among
different forms of dementia can, therefore, be considered as firmly established, particularly taking into
account analysis of drawing errors more than overall
accuracy in drawing.
DISCLOSURE STATEMENT
[11]
[12]
[13]
[14]
[15]
[16]
[17]
[18]
[19]
1176
1177
1178
Authors disclosures available online (http://j-alz.
com/manuscript-disclosures/16-0009r2).
REFERENCES
[20]
[21]
1179
[1]
1180
1181
[2]
1182
1183
1184
[3]
1185
1186
1187
[4]
1188
1189
1190
1191
1192
[5]
1193
1194
1195
1196
1197
[6]
1198
1199
1200
[7]
1201
1202
1203
[8]
1204
1205
1206
[9]
1207
1208
1209
1210
[10]
Ettlinger G, Warrington E, Zangwill OL (1957) A further
study of visual-spatial agnosia. Brain 80, 335-361.
Arena R, Gainotti G (1978) Constructional apraxia and
visuoperceptive disabilities in relation to laterality of cerebral lesions. Cortex 14, 463-473.
Gainotti G, Tiacci C (1970) Patterns of drawing disability
in right and left hemispheric patients. Neuropsychologia
8, 379-384.
Trojano L, Fragassi NA, Chiacchio L, Izzo O, Izzo G,
Di Cesare G, Cristinzio C, Grossi D (2004) Relationships
between constructional and visuospatial abilities in normal
subjects and in focal brain-damaged patients. J Clin Exp
Neuropsychol 26, 1103-1112.
Serra L, Fadda L, Perri R, Span`o B, Marra C, Castelli
D, Torso M, Makovac E, Cercignani M, Caltagirone C,
Bozzali M (2014) Constructional apraxia as a distinctive cognitive and structural brain feature of pre-senile
Alzheimers disease. J Alzheimers Dis 38, 391-402.
Warrington EK, James M, Kinsbourne M (1966) Drawing
disability in relation to laterality of cerebral lesion. Brain
89, 53-82.
Hecaen H, Assal G (1970) A comparison of constructive deficits following right and left hemispheric lesions.
Neuropsychologia 8, 289-303.
Gainotti G, Miceli G, Caltagirone C (1977). Constructional apraxia in left brain-damaged patients: A planning
disorder? Cortex 13, 109-118.
Kirk A, Kertesz A (1991) On drawing impairment in
Alzheimers disease. Arch Neurol 48, 73-77.
Pillon B (1981) Troubles visuo-constructifs et methodes
de compensation. Resultats de 85 patients atteints de
lesions cerebrales. Neuropsychologia 19, 375-383.
[22]
[23]
[24]
[25]
[26]
[27]
[28]
[29]
[30]
[31]
[32]
Critchley M (1953) The Parietal Lobes, Hafner Press, New
York.
Piercy M, Hecaen H, Ajuriaguerra J (1960) Constructional
apraxia associated with unilateral cerebral lesions-left and
right sided cases compared. Brain 83, 225-242.
De Renzi E (1982) Disorders of Space Exploration and
Cognition, Wiley, Chichester.
Makuuchi M, Kaminaga T, Sugishita M (2003) Both parietal lobes are involved in drawing: A functional MRI
study and implications for constructional apraxia. Brain
Res Cogn Brain Res 16, 338-347.
Roth HL, Bauer RM, Crucian GP, Heilman KM
(2014) Frontal-executive constructional apraxia: When
delayed recall is better than copying. Neurocase 20,
283-295.
Price CC, Cunningham H, Coronado N, Freedland A,
Cosentino S, Penney DL, Penisi A, Bowers D, Okun MS,
Libon DJ (2011). Clock drawing in the montreal cognitive
assessment: Recommendations for dementia assessment.
Dement Geriatr Cogn Disord 31, 179-187.
Gainotti G, Silveri MC, Villa G, Caltagirone C (1983)
Drawing objects from memory in aphasia. Brain 106,
613-622.
Kirk A, Kertesz A (1989) Hemispheric contributions to
drawing. Neuropsychologia 27, 881-886.
Bozeat S, Lambon Ralph MA, Graham KS, Patterson K,
Wilkin H, Rowland J, Hodges JR (2003) A duck with
four legs: Investigating the structure of conceptual knowledge using picture drawing in semantic dementia. Cogn
Neuropsychol 20, 27-47.
Agrell B, Dehlin O (2012) The clock-drawing test. 1998.
Age Ageing 41(Suppl 3), 41-45.
Freedman MI, Leach L, Kaplan E, Winocur G, Shulman
KJ, Delis DC (1994) Clock Drawing, Oxford University
Press, Oxford.
Trojano L, Conson M (2008). Visuospatial and visuoconstructive deficits. In Handbook of Clinical Neurology, Vol.
88, Goldenberg G, Miller BL, eds. Elsevier, Amsterdam,
pp. 373-392.
Mayer Gross W (1935) Some observation on apraxia. Proc
R Soc Med 28, 1203-1212.
Gainotti G (1972) A quantitative study of the closingin symptom in normal children and in brain-damaged
patients. Neuropsychologia 10, 429-436.
De Lucia N, Grossi D, Trojano L (2014) The genesis of
closing-in in Alzheimer disease and vascular dementia: A
comparative clinical and experimental study. Neuropsychology 28, 312-318.
Poppelreuter W (1917) Die Psychischen Schaedigungen
durch Kopfschuss im Kriege 1914-1916, Vol. 1, Voss,
Leipzig.
Kleist K (1934) Gehirnpathologie, Barth, Leipzig.
Gainotti G (1985) Constructional apraxia. In Handbook of
Clinical Neurology, Vol. 45, JAM Fredericks, ed., Elsevier,
Amsterdam, pp. 491-506.
Benton AL (1962) The visual retention test as a constructional praxis task. Conn Neurol 22, 141-155.
Arrigoni C, De Renzi E (1964) Constructional apraxia and
hemispheric locus of lesion. Cortex 1, 170-197.
De Renzi E, Faglioni P (1967) The relationship between
visuo-spatial impairment and constructional apraxia. Cortex 3, 327-342.
Colombo A, De Renzi E, Faglioni P (1976) The occurrence of visual neglect in patients with unilateral cerebral
disease. Cortex 12, 221-231.
1211
1212
1213
1214
1215
1216
1217
1218
1219
1220
1221
1222
1223
1224
1225
1226
1227
1228
1229
1230
1231
1232
1233
1234
1235
1236
1237
1238
1239
1240
1241
1242
1243
1244
1245
1246
1247
1248
1249
1250
1251
1252
1253
1254
1255
1256
1257
1258
1259
1260
1261
1262
1263
1264
1265
1266
1267
1268
1269
1270
1271
1272
1273
1274
1275
L. Trojano and G. Gainotti / Drawing Disorders in Dementia
1276
[33]
1277
1278
1279
1280
[34]
1281
1282
1283
1284
1285
[35]
1286
1287
1288
[36]
1289
1290
1291
[37]
1292
1293
1294
1295
[38]
1296
1297
1298
[39]
1299
1300
1301
1302
1303
[40]
1304
1305
1306
1307
[41]
1308
1309
1310
[42]
1311
1312
[43]
1313
1314
[44]
1315
1316
1317
1318
[45]
1319
1320
1321
1322
[46]
1323
1324
1325
[47]
1326
1327
[48]
1328
1329
[49]
1330
1331
1332
[50]
1333
1334
[51]
1335
1336
[52]
1337
1338
1339
1340
[53]
Carlesimo GA, Fadda L, Caltagirone C (1993) Basic
mechanisms of constructional apraxia in unilateral braindamaged patients: Role of visuo-perceptual and executive
disorders. J Clin Exp Neuropsychol 15, 342-358.
Chechlacz M, Novick A, Rotshtein P, Bickerton WL,
Humphreys GW, Demeyere N (2014) The neural substrates of drawing: A voxel-based morphometry analysis
of constructional, hierarchical, and spatial representation
deficits. J Cogn Neurosci 26, 2701-2715.
Ino T, Asada T, Ito J, Kimura T, Fukuyama H (2003)
Parieto-frontal networks for clock drawing revealed with
fMRI. Neurosci Res 45, 71-77.
Harrington G, Farias D, Davis C (2009) The neural basis
for simulated drawing and the semantic implications. Cortex 45, 386-393.
Ferber S, Mraz R, Baker N, Graham SJ (2007) Shared and
differential neural substrates of copying versus drawing:
A functional magnetic resonance imaging study. Neuroreport 18, 1089-1093.
Ogawa K, Inui T (2009) The role of the posterior parietal
cortex in drawing by copying. Neuropsychologia 47, 10131022.
Hauptmann B, Sosnik R, Smikt O, Okon E, Manor D,
Kushnir T, Flash T, Karni A (2009) A new method to record
and control for 2D movement kinematics during functional magnetic resonance imaging (fMRI). Cortex 45,
407-417.
Miall RC, Nam SH, Tchalenko J (2014) The influence of
stimulus format on drawinga functional imaging study
of decision making in portrait drawing. Neuroimage 102,
608-619.
Roncato S, Sartori G, Rumiati R (1987) Constructional
apraxia: An information processing analysis. Cogn Neuropsychol 4, 113-129.
Van Sommers P (1989) A system for drawing-related neuropsychology. Cogn Neuropsychol 6, 117-164.
Grossi D (1991) La Riabilitazione dei Disturbi della Cognizione Spaziale, Masson, Milano.
Grossi D, Trojano L (2002) Constructional Apraxia. In
Handbook of Clinical and Experimental Neuropsychology, G Denes, L Pizzamiglio, eds. Psychology Press,
Hove.
Grossi D, Calise G, Correra C, Trojano L (1996) Selective
drawing disorders after right subcortical stroke: A neuropsychological premorbid and follow-up case study. Ital
J Neurol Sci 17, 241-248.
Trojano L, Grossi D (1998) Pure constructional apraxia
- a cognitive analysis of a single case. Behav Neurol 11,
43-49.
Trojano L, Grossi D (1992) Impaired drawing from memory in a visual agnosic patient. Brain Cogn 20, 327-344.
Wapner W, Judd T, Gardner H (1978) Visual agnosia in an
artist. Cortex 14, 343-364.
Rosselli M, Ardila A (2003) The impact of culture and education on non-verbal neuropsychological measurements:
A critical review. Brain Cogn 52, 326-333.
Trojano L, Grossi D (1994) A critical review of mental
imagery defects. Brain Cogn 24, 213-243.
Grossman M (1988) Drawing deficits in brain-damaged
patients freehands pictures. Brain Cogn 8, 189-205.
Shulman KI, Herrmann N, Brodaty H, Chiu H, Lawlor B,
Ritchie K, Scanlan JM (2006) IPA survey of brief cognitive
screening instruments. Int Psychogeriatr 18, 281-94.
Kaplan E (1988) The process approach to neuropsychological assessment. Aphasiology 2, 309-311.
[54]
[55]
[56]
[57]
[58]
[59]
[60]
[61]
[62]
[63]
[64]
[65]
[66]
[67]
[68]
[69]
[70]
17
Sunderland T, Hill JL, Mellow AM, Lawlor BA, Gundersheimer J, Newhouse PA, Grafman JH (1989) Clock
drawing in Alzheimers disease. A novel measure of
dementia severity. J Am Geriatr Soc 37, 725-729.
Scanlan JM, Brush M, Quijano C, Borson S (2002)
Comparing clock tests for dementia screening: Nave judgments vs formal systemswhat is optimal? Int J Geriatr
Psychiatry 17, 14-21.
Tuokko H, Hadjistavropoulos T, Miller JA, Beattie BL
(1992) The Clock Test: A sensitive measure to differentiate
normal elderly from those with Alzheimer disease. J Am
Geriatr Soc 40, 579-584.
Mendez MF, Ala T, Underwood KL (1992) Development of scoring criteria for the clock drawing task in
Alzheimers disease. J Am Geriatr Soc 40, 1095-1099.
Matsuoka T, Narumoto J, Okamura A, Taniguchi S, Kato
Y, Shibata K, Nakamura K, Okuyama C, Yamada K, Fukui
K (2013) Neural correlates of the components of the clock
drawing test. Int Psychogeriatr 25, 1317-1323.
Kim YS, Lee KM, Choi BH, Sohn EH, Lee AY (2009)
Relation between the clock drawing test (CDT) and structural changes of brain in dementia. Arch Gerontol Geriatr
48, 218-221.
Seidl U, Traeger TV, Hirjak D, Remmele B, Wolf RC,
Kaiser E, Stieltjes B, Essig M, Schroder J, Thomann PA
(2012) Subcortical morphological correlates of impaired
clock drawing performance. Neurosci Lett 512, 28-32.
Wang P, Shi L, Zhao Q, Hong Z, Guo Q (2014)
Longitudinal changes in clock drawing test (CDT) performance before and after cognitive decline. PLoS One 9,
e97873.
Peters R, Pinto EM (2008) Predictive value of the Clock
Drawing Test. A review of the literature. Dement Geriatr
Cogn Disord 26, 351-355.
Lessig MC, Scanlan JM, Nazemi H, Borson S (2008)
Time that tells: Critical clock-drawing errors for dementia
screening. Int Psychogeriatr 20, 459-470.
Lee AY, Kim JS, Choi BH, Sohn EH (2009) Characteristics of clock drawing test (CDT) errors by the dementia
type: Quantitative and qualitative analyses. Arch Gerontol
Geriatr 48, 58-60.
Lee JH, Oh ES, Jeong SH, Sohn EH, Lee TY, Lee AY
(2011) Longitudinal changes in clock drawing test (CDT)
performance according to dementia subtypes and severity.
Arch Gerontol Geriatr 53, e179-82.
Nakashima H, Umegaki H, Makino T, Kato K, Abe
S, Suzuki Y, Kuzuya M (2015) Neuroanatomical correlates of error types on the Clock Drawing Test in
Alzheimers disease patients. Geriatr Gerontol Int. doi:
10.1111/ggi.12550.
Rey A (1941) Lexamen psychologique dans les cas
dencephalopathie traumatique. Arch Psychol 28, 215285.
Osterrieth PA (1944) Le test de copie dune figure complexe. Arch Psychol 30, 286-356.
Biesbroek JM, van Zandvoort MJ, Kuijf HJ, Weaver
NA, Kappelle LJ, Vos PC, Velthuis BK, Biessels GJ,
Postma A, Utrecht VCI Study Group (2014) The anatomy
of visuospatial construction revealed by lesion-symptom
mapping. Neuropsychologia 62, 68-76.
Melrose RJ, Harwood D, Khoo T, Mandelkern M, Sultzer
DL (2013) Association between cerebral metabolism
and Rey-Osterrieth Complex Figure Test performance in
Alzheimers disease. J Clin Exp Neuropsychol 35, 246258.
1341
1342
1343
1344
1345
1346
1347
1348
1349
1350
1351
1352
1353
1354
1355
1356
1357
1358
1359
1360
1361
1362
1363
1364
1365
1366
1367
1368
1369
1370
1371
1372
1373
1374
1375
1376
1377
1378
1379
1380
1381
1382
1383
1384
1385
1386
1387
1388
1389
1390
1391
1392
1393
1394
1395
1396
1397
1398
1399
1400
1401
1402
1403
1404
1405
18
1406
[71]
1407
1408
1409
1410
1411
[72]
1412
1413
1414
1415
[73]
1416
1417
1418
1419
1420
[74]
1421
1422
1423
1424
[75]
1425
1426
1427
1428
[76]
1429
1430
1431
[77]
1432
1433
1434
1435
[78]
1436
1437
1438
[79]
1439
1440
1441
[80]
1442
1443
1444
[81]
1445
1446
1447
1448
[82]
1449
1450
1451
[83]
1452
1453
1454
[84]
1455
1456
1457
1458
[85]
1459
1460
1461
[86]
1462
1463
1464
1465
1466
1467
1468
1469
1470
[87]
L. Trojano and G. Gainotti / Drawing Disorders in Dementia
Forster S, Teipel S, Zach C, Rominger A, Cumming P,
Fougere Cl, Yakushev I, Haslbeck M, Hampel H, Bartenstein P, Burger K (2010) FDG-PET mapping the brain
substrates of visuo-constructive processing in Alzheimers
disease. J Psychiatr Res 44, 462-469.
Folstein MF, Folstein SE, McHugh PR (1975) Minimental state. A practical method for grading the cognitive
state of patients for the clinician. J Psychiatric Res 12,
189-198.
Mitolo M, Salmon DP, Gardini S, Galasko D, Grossi
E, Caffarra P (2014) The new Qualitative Scoring
MMSE Pentagon Test (QSPT) as a valid screening tool
between autopsy-confirmed dementia with Lewy bodies
and Alzheimers disease. J Alzheimers Dis 39, 823-832.
Cagnin A, Buss`e C, Jelcic N, Gnoato F, Mitolo M, Caffarra P (2015) High specificity of MMSE pentagon scoring
for diagnosis of prodromal dementia with Lewy bodies.
Parkinsonism Relat Disord 21, 303-305.
Benton A, Tranel A (1993) Visuoperceptual, visuospatial,
and visuo-constructional disorders. In Clinical neuropsychology, KM Heilman, E Valenstein, eds. Oxford
University Press, New York.
Mandal PK, Joshi J, Saharan S (2012) Visuospatial perception: An emerging biomarker for Alzheimers disease.
J Alzheimers Dis 31(Suppl 3), S117-S135.
Quental NBM, Brucki SMD, Bueno OFA (2013) Visuospatial function in early Alzheimers disease-The use of
the Visual Object and Space Perception (VOSP) battery.
PLoS One 8, e68398.
Orsini A, Trojano L, Chiacchio L, Grossi D (1988) Immediate memory spans in dementia. Percept Mot Skills 67,
267-272.
Benton AL, Hannay HJ, Varney NR (1975) Visual perception of line direction in patients with unilateral brain
disease. Neurology 25, 907-910.
Warrington EK, James M (1991) VOSP, The Visual Object
and Space Perception Battery, Thames Valley Test Company, Bury St. Edmunds.
Trojano L, Siciliano M, Pedone R, Cristinzio C,
Grossi D (2015) Italian normative data for the Battery
for Visuospatial Abilities (TERADIC). Neurol Sci 36,
1353-1361.
Tombaugh TN (2004) Trail making test A and B: Normative data stratified by age and education. Arch Clin
Neuropsychol 19, 203-214.
Ruff RM, Light RH, Evans RW (1987) The ruff figural
fluency test: A normative study with adults. Dev Neuropsychol 3, 37-51.
Borod JC, Carper M, Goodglass H (1982) WAIS performance IQ in aphasia as a function of auditory
comprehension and constructional apraxia. Cortex 18,
212-220.
Benowitz LI, Moya KL, Levine DN (1990) Impaired verbal reasoning and constructional apraxia in subjects with
right hemisphere damage. Neuropsychologia 28, 231-241.
Thomann PA, Toro P, Dos Santos V, Essig M, Schroder
J (2008) Clock drawing performance and brain morphology in mild cognitive impairment and Alzheimers disease.
Brain Cogn 67, 88-93.
Ahn HJ, Seo SW, Chin J, Suh MK, Lee BH, Kim ST,
Im K, Lee JM, Lee JH, Heilman KM, Na DL (2011) The
cortical neuroanatomy of neuropsychological deficits in
mild cognitive impairment and Alzheimers disease: A
surface-based morphometric analysis. Neuropsychologia
49, 3931-3945.
[88]
[89]
[90]
[91]
[92]
[93]
[94]
[95]
[96]
[97]
[98]
[99]
[100]
[101]
[102]
[103]
Rouleau I, Salmon DP, Butters N (1996) Longitudinal
analysis of clock drawing in Alzheimers disease patients.
Brain Cogn 31, 17-34.
Binetti G, Cappa S, Magni E, Padovani A, Bianchetti A,
Trabucchi M (1998) Visual and spatial perception in the
early phase of Alzheimers disease. Neuropsychology 12,
29-33.
Ajuriaguerra J, Muller M, Tissot R (1960) A propos
de quelques probl`emes poses par lapraxie dans les
demences. Encephale 49, 275-401.
Gainotti G, Marra C, Villa G, Parlato V, Chiarotti F (1998)
Sensitivity and specificity of some neuropsychological
markers of Alzheimer dementia. Alzheimer Dis Assoc Disord 12, 152-162.
Gainotti G, Quaranta D, Vita MG, Marra C (2014)
Neuropsychological predictors of conversion from mild
cognitive impairment to Alzheimers disease. J Alzheimers
Dis 38, 481-495.
Parsey CM, Schmitter-Edgecombe M (2011) Quantitative
and qualitative analyses of the clock drawing test in mild
cognitive impairment and Alzheimer disease: Evaluation
of a modified scoring system. J Geriatr Psychiatry Neurol
24, 108-18.
Ehreke L, Luck T, Luppa M, Konig HH, Villringer A,
Riedel-Heller SG (2011) Clock drawing test - screening
utility for mild cognitive impairment according to different scoring systems: Results of the Leipzig Longitudinal
Study of the Aged (LEILA 75+). Int Psychogeriatr 23,
1592-1601.
Marra C, Ferraccioli M, Vita MG, Quaranta D, Gainotti G
(2011) Patterns of cognitive decline and rates of conversion to dementia in patients with degenerative and vascular
forms of MCI. Curr Alzheimer Res 8, 24-31.
Mariani E, Monastero R, Mecocci P (2007) Mild cognitive
impairment: A systematic review. J Alzheimers Dis 12,
23-35.
Ahmed S, Brennan L, Eppig J, Price CC, Lamar M,
Delano-Wood L, Bangen KJ, Edmonds EC, Clark L,
Nation DA, Jak A, Au R, Swenson R, Bondi MW, Libon
DJ (2016) Visuoconstructional impairment in subtypes of
mild cognitive impairment. Appl Neuropsychol Adult 23,
43-52.
Lee SJ, Ritchie CS, Yaffe K, Stijacic Cenzer I, Barnes
DE (2014) A clinical index to predict progression from
mild cognitive impairment to dementia due to Alzheimers
disease. PLoS One 9, e113535.
Amodeo S, Mainland BJ, Herrmann N, Shulman KI (2015)
The times they are a-changin: Clock drawing and prediction of dementia. J Geriatr Psychiatry Neurol 28, 145-155.
Llado A, Sanchez-Valle R (2011) Focusing on atypical symptoms for improved diagnosis of early-onset
Alzheimers disease. Future Neurol 6, 575-578.
Joubert S, Gour N, Guedj E, Didic M, Gueriot C, Koric L,
Ranjeva JP, Felician O, Guye M, Ceccaldi M (2016) Earlyonset and late-onset Alzheimers disease are associated
with distinct patterns of memory impairment. Cortex 74,
217-232.
Fujimori M, Imamura T, Yamashita H, Hirono N, Ikejiri
Y, Shimomura T, Mori E (1998) Age at onset and
visuocognitive disturbances in Alzheimer disease.
Alzheimer Dis Assoc Disord 12, 163-166.
Koedam EL, Lauffer V, van der Vlies AE, van der Flier
WM, Scheltens P, Pijnenburg YA (2010) Early-versus
late-onset Alzheimers disease: More than age alone. J
Alzheimers Dis 19, 1401-1408.
1471
1472
1473
1474
1475
1476
1477
1478
1479
1480
1481
1482
1483
1484
1485
1486
1487
1488
1489
1490
1491
1492
1493
1494
1495
1496
1497
1498
1499
1500
1501
1502
1503
1504
1505
1506
1507
1508
1509
1510
1511
1512
1513
1514
1515
1516
1517
1518
1519
1520
1521
1522
1523
1524
1525
1526
1527
1528
1529
1530
1531
1532
1533
1534
1535
L. Trojano and G. Gainotti / Drawing Disorders in Dementia
1536
[104]
1537
1538
1539
1540
[105]
1541
1542
[106]
1543
1544
1545
1546
1547
[107]
1548
1549
1550
1551
1552
[108]
1553
1554
[109]
1555
1556
1557
1558
[110]
1559
1560
1561
[111]
1562
1563
1564
[112]
1565
1566
[113]
1567
1568
1569
[114]
1570
1571
1572
[115]
1573
1574
[116]
1575
1576
1577
1578
[117]
1579
1580
1581
1582
1583
[118]
1584
1585
1586
1587
[119]
1588
1589
1590
1591
[120]
1592
1593
1594
1595
1596
1597
1598
1599
1600
[121]
Mendez MF, Ghajarania M, Perryman KM (2002)
Posterior cortical atrophy: Clinical characteristics and
differences compared to Alzheimers disease. Dement
Geriatr Cogn Disord 14, 33-40.
Benson DF, Davis RJ, Snyder BD (1988) Posterior cortical
atrophy. Arch Neurol 45, 789-793.
Kas A, de Souza LC, Samri D, Bartolomeo P, Lacomblez
L, Kalafat M, Migliaccio R, Thiebaut de Schotten M,
Cohen L, Dubois B, Habert MO, Sarazin M (2011) Neural correlates of cognitive impairment in posterior cortical
atrophy. Brain 134, 1464-1478.
Migliaccio R, Agosta F, Toba MN, Samri D, Corlier F, de
Souza LC, Chupin M, Sharman M, Gorno-Tempini ML,
Dubois B, Filippi M, Bartolomeo P (2012) Brain networks
in posterior cortical atrophy: A single case tractography
study and literature review. Cortex 48, 1298-1309.
Possin KL (2010) Visual spatial cognition in neurodegenerative disease. Neurocase 16, 466-487.
Andrade K, Samri D, Sarazin M, de Souza LC, Cohen L,
Thiebaut de Schotten M, Dubois B, Bartolomeo P (2010)
Visual neglect in posterior cortical atrophy. BMC Neurol
10, 68.
Silveri MC, Ciccarelli N, Cappa A (2011) Unilateral
spatial neglect in degenerative brain pathology. Neuropsychology 25, 554-566.
Zilli EM, Heilman KM (2015) Allocentric spatial
neglect with posterior cortical atrophy. Neurocase 21,
190-197.
McMonagle P, Kertesz A (2006) Exploded drawing in
posterior cortical atrophy. Neurology 67, 1866.
Rizzo M, Anderson SW, Dawson J, Nawrot M (2000)
Vision and cognition in Alzheimers disease. Neuropsychologia 38, 1157-1169.
Caine D, Hodges JR (2001) Heterogeneity of semantic
and visuospatial deficits in early Alzheimers disease. Neuropsychology 15, 155-164.
Benson DF, Davis RJ, Snyder BD (1988) Posterior cortical
atrophy. Arch Neurol 45, 789-793.
Ross SJM, Graham N, Stuart-Green L, Prins M, Xuereb
J, Patterson K, Hodges JR (1996) Progressive biparietal
atrophy: An atypical presentation of Alzheimers disease.
J Neurol Neurosurg Psychiatry 9, 191-224.
Hof PR, Vogt BA, Bouras C, Morrison JH (1997) Atypical
form of Alzheimers disease with prominent posterior cortical atrophy: A review of lesion distribution and circuit
disconnection in cortical visual pathways. Vision Res 37,
3609-3625.
Suzuki K, Otsuka Y, Endo K, Ejima A, Saito H, Fujii T,
Yamadori A (2003) Visuospatial deficits due to impaired
visual attention: Investigation of two cases of slowly progressive visuospatial impairment. Cortex 39, 327-341.
Guerin F, Belleville S, Ska B (2002) Characterization of
visuoconstructional disabilities in patients with probable
dementia of Alzheimers type. J Clin Exp Neuropsychol
24, 1-17.
Shon JM, Lee DY, Seo EH, Sohn BK, Kim JW, Park SY,
Kim SG, Jhoo JH, Woo JI (2013) Functional neuroanatomical correlates of the executive clock drawing task (CLOX)
performance in Alzheimers disease: A FDG-PET study.
Neuroscience 246, 271-280.
Teipel SJ, Willoch F, Ishii K, Burger K, Drzezga A, Engel
R, Bartenstein P, Moller HJ, Schwaiger M, Hampel H
(2006) Resting state glucose utilization and the CERAD
cognitive battery in patients with Alzheimers disease.
Neurobiol Aging 27, 681-690.
[122]
[123]
[124]
[125]
[126]
[127]
[128]
[129]
[130]
[131]
[132]
[133]
[134]
[135]
19
Looi JCL, Sachdev PS (1999) Differentiation of vascular
dementia from AD on neuropsychological tests. Neurology 53, 670-678.
Wiechmann AR, Hall JR, OBryant S (2010) The fourpoint scoring system for the clock drawing test does not
differentiate between Alzheimers disease and vascular
dementia. Psychol Rep 106, 941-948.
Heinik J, Solomesh I, Raikher B, Lin R (2002) Can
clock drawing test help to differentiate between dementia of the Alzheimers type and vascular dementia?
A preliminary study. Int J Geriatr Psychiatry 17,
699-703.
Kitabayashi Y, Ueda H, Narumoto J, Nakamura K, Kita
H, Fukui K (2001) Qualitative analyses of clock drawings
in Alzheimers disease and vascular dementia. Psychiatry
Clin Neurosci 55, 485-491.
Fukui T, Lee E, Kitamura M, Hosoda H, Bokui C, Ikusu K,
Okita K (2009) Visuospatial dysfunction may be a key in
the differentiation between Alzheimers disease and subcortical cognitive impairment in moderate to severe stages.
Dement Geriatr Cogn Disord 28, 288-294.
Graham NL, Emery T, Hodges JR (2004) Distinctive
cognitive profiles in Alzheimers disease and subcortical vascular dementia. J Neurol Neurosurg Psychiatry 75,
61-71.
Tan LP, Herrmann N, Mainland BJ, Shulman K (2015)
Can clock drawing differentiate Alzheimers disease from
other dementias? Int Psychogeriatr 27, 1649-1660.
Neary D, Snowden JS, Gustafson L, Passant U, Stuss D,
Black S, Freedman M, Kertesz A, Robert PH, Albert M,
Boone K, Miller BL, Cummings J, Benson DF (1998)
Frontotemporal lobar degeneration: A consensus on clinical diagnostic criteria. Neurology 51, 1546-1554.
Rascovsky K, Hodges JR, Knopman D, Mendez MF,
Kramer JH, Neuhaus J, van Swieten JC, Seelaar H, Dopper
EG, Onyike CU, Hillis AE, Josephs KA, Boeve BF,
Kertesz A, Seeley WW, Rankin KP, Johnson JK, GornoTempini ML, Rosen H, Prioleau-Latham CE, Lee A, Kipps
CM, Lillo P, Piguet O, Rohrer JD, Rossor MN, Warren JD,
Fox NC, Galasko D, Salmon DP, Black SE, Mesulam M,
Weintraub S, Dickerson BC, Diehl-Schmid J, Pasquier F,
Deramecourt V, Lebert F, Pijnenburg Y, Chow TW, Manes
F, Grafman J, Cappa SF, Freedman M, Grossman M, Miller
BL (2011) Sensitivity of revised diagnostic criteria for the
behavioural variant of frontotemporal dementia. Brain 34,
2456-2477.
Rascovsky K, Salmon DP, Ho GJ, Galasko D, Peavy
GM, Hansen LA, Thal LJ (2002) Cognitive profiles differ
in autopsy-confirmed frontotemporal dementia and AD.
Neurology 58, 1801-1808.
Blair M, Kertesz A, McMonagle P, Davidson W, Bodi N
(2006) Quantitative and qualitative analyses of clock drawing in frontotemporal dementia and Alzheimers disease.
J Int Neuropsychol Soc 12, 159-165.
Razani J, Boone KB, Miller BL, Lee A, Sherman D
(2001) Neuropsychological performance of right- and
left-frontotemporal dementia compared to Alzheimers
disease. J Int Neuropsychol Soc 7, 468-480.
Thompson JC, Stopford CL, Snowden JS, Neary D
(2005) Qualitative neuropsychological performance
characteristics in frontotemporal dementia and
Alzheimers disease. J Neurol Neurosurg Psychiatry 76,
920-927.
Possin KL, Laluz VR, Alcantar OZ, Miller BL, Kramer JH
(2011) Distinct neuroanatomical substrates and cognitive
1601
1602
1603
1604
1605
1606
1607
1608
1609
1610
1611
1612
1613
1614
1615
1616
1617
1618
1619
1620
1621
1622
1623
1624
1625
1626
1627
1628
1629
1630
1631
1632
1633
1634
1635
1636
1637
1638
1639
1640
1641
1642
1643
1644
1645
1646
1647
1648
1649
1650
1651
1652
1653
1654
1655
1656
1657
1658
1659
1660
1661
1662
1663
1664
1665
20
1666
1667
1668
1669
[136]
1670
1671
1672
1673
1674
[137]
1675
1676
1677
1678
[138]
1679
1680
1681
1682
1683
1684
[139]
1685
1686
1687
1688
1689
[140]
1690
1691
1692
1693
[141]
1694
1695
1696
1697
1698
[142]
1699
1700
1701
[143]
1702
1703
1704
1705
[144]
1706
1707
1708
[145]
1709
1710
1711
[146]
1712
1713
1714
1715
[147]
1716
1717
1718
[148]
1719
1720
1721
1722
[149]
1723
1724
1725
1726
1727
1728
1729
1730
[150]
L. Trojano and G. Gainotti / Drawing Disorders in Dementia
mechanisms of figure copy performance in Alzheimers
Disease and behavioral variant Frontotemporal Dementia.
Neuropsychologia 49, 43-48.
Perri R, Koch G, Carlesimo GA, Serra L, Fadda
L, Pasqualetti P, Pettenati C, Caltagirone C (2005)
Alzheimers disease and frontal variant of frontotemporal dementia. A very brief battery for cognitive and
behavioural distinction. J Neurol 252, 1238-1244.
Gorno-Tempini ML, Dronkers NF, Rankin KP, Ogar JM,
Phengrasamy L, Rosen HJ, Johnson JK, Weiner MW,
Miller BL (2004) Cognition and anatomy in three variants
of primary progressive aphasia. Ann Neurol 55, 335-346.
Grossi D, Fragassi NA, Chiacchio L, Valoroso L, Tuccillo R, Perrotta C, Rapone P, Conchiglia G, Trojano L
(2002) Do visuospatial and constructional disturbances
differentiate frontal variant of frontotemporal dementia
and Alzheimers disease? An experimental study of a clinical belief. Int J Geriatr Psychiatry 17, 641-648.
Gasparini M, Masciarelli G, Vanacore N, Ottaviani D,
Salati E, Talarico G, Lenzi GL, Bruno G (2008) A descriptive study on constructional impairment in frontotemporal
dementia and Alzheimers disease. Eur J Neurol 15, 589597.
Elderkin-Thompson V, Boone KB, Hwang S, Kumar A
(2004) Neurocognitive profiles in elderly patients with
frontotemporal degeneration or major depressive disorder.
J Int Neuropsychol Soc 10, 753-771.
Rascovsky K, Salmon DP, Hansen LA, Galasko D (2008)
Distinct cognitive profiles and rates of decline on the
Mattis Dementia Rating Scale in autopsy-confirmed frontotemporal dementia and Alzheimers disease. J Int
Neuropsychol Soc 14, 373-383.
Mendez MF, Shapira JS, McMurtray A, Licht E, Miller
BL (2007) Accuracy of the clinical evaluation for frontotemporal dementia. Arch Neurol 64, 830-835.
Wittenberg D, Possin KL, Rascovsky K, Rankin KP, Miller
BL, Kramer JH (2008) The early neuropsychological
and behavioral characteristics of frontotemporal dementia.
Neuropsychol Rev 18, 91-102.
Miller BL, Ponton M, Benson DF, Cummings JL, Mena
I (1996) Enhanced artistic creativity with temporal lobe
degeneration. Lancet 348, 1744-1745.
Miller BL, Cummings J, Mishkin F, Boone K, Prince F,
Ponton M, Cotman C (1998) Emergence of artistic talent
in frontotemporal dementia Neurology 51, 978-982.
Miller BL, Boone K, Cummings JL, Read SL, Mishkin F
(2000) Functional correlates of musical and visual ability in frontotemporal dementia. Br J Psychiatry 176,
458-463.
Gainotti G (2012) The format of conceptual representations disrupted in semantic dementia: A position paper.
Cortex 48, 521-529.
Gainotti G (2015) Is the difference between right and left
ATLs due to the distinction between general and social
cognition or between verbal and non-verbal representations? Neurosci Biobehav Rev 51, 296-312.
Kapur N (1996) Paradoxical functional facilitation in
brain-behaviour research. A critical review. Brain 119,
1775-1790.
McKeith IG, Galasko D, Kosaka K, Perry EK, Dickson
DW, Hansen LA, Salmon DP, Lowe J, Mirra SS, Byrne
EJ, Lennox G, Quinn NP, Edwardson JA, Ince PG, Bergeron C, Burns A, Miller BL, Lovestone S, Collerton D,
Jansen EN, Ballard C, de Vos RA, Wilcock GK, Jellinger
KA, Perry RH (1996) Consensus guidelines for the clinical
[151]
[152]
[153]
[154]
[155]
[156]
[157]
[158]
[159]
[160]
[161]
[162]
[163]
[164]
[165]
and pathologic diagnosis of dementia with Lewy bodies
(DLB): Report of the consortium on DLB international
workshop. Neurology 47, 1113-1124.
Mori E, Shimomura T, Fujimori M, Hirono N, Imamura T,
Hashimoto M, Tanimukai S, Kazui H, Hanihara T (2000)
Visuoperceptual impairment in dementia with Lewy bodies. Arch Neurol 57, 489-493.
Nervi A, Reitz C, Tang MX, Santana V, Piriz A, ReyesDumeyer D, Lantigua R, Medrano M, Jimenez-Velazquez
IZ, Lee JH, Mayeux R (2008) Comparison of clinical manifestations in Alzheimer disease and dementia with Lewy
bodies. Arch Neurol 65, 1634-1639.
Crowell TA, Luis CA, Cox DE, Mullan M (2007) Neuropsychological comparison of Alzheimers disease and
dementia with Lewy bodies. Dement Geriatr Cogn Disord
23, 120-125.
Tiraboschi P, Salmon DP, Hansen LA, Hofstetter RC, Thal
LJ, Corey-Bloom J (2006) What best differentiates Lewy
body from Alzheimers disease in early-stage dementia?
Brain 129, 729-735.
Collerton D, Burn D, McKeith I, OBrien J (2003) Systematic review and meta-analysis show that dementia
with Lewy bodies is a visual-perceptual and attentionalexecutive dementia. Dement Geriatr Cogn Disord 16,
229-237.
Cahn-Weiner DA, Williams K, Grace J, Tremont G, Westervelt H, Stern RA (2003) Discrimination of dementia with
Lewy bodies from Alzheimer disease and Parkinson disease using the clock drawing test. Cogn Behav Neurol 16,
85-92.
Hamilton JM, Salmon DP, Galasko D, Raman R, Emond
J, Hansen LA, Masliah E, Thal LJ (2008) Visuospatial
deficits predict rate of cognitive decline in autopsy-verified
dementia with Lewy bodies. Neuropsychology 22, 729737.
Cagnin A, Gnoato F, Jelcic N, Favaretto S, Zarantonello G,
Ermani M, Dam M (2013) Clinical and cognitive correlates
of visual hallucinations in dementia with Lewy bodies.
J Neurol Neurosurg Psychiatry 84, 505-510.
Palmqvist S, Hansson O, Minthon L, Londos E (2009)
Practical suggestions on how to differentiate dementia with Lewy bodies from Alzheimers disease with
common cognitive tests. Int J Geriatr Psychiatry 24,
1405-1412.
Nagahama Y, Okina T, Suzuki N, Matsuda M (2008) Cerebral substrates related to impaired performance in the
clock-drawing test in dementia with Lewy bodies. Dement
Geriatr Cogn Disord 25, 524-530.
Perneczky R, Drzezga A, Boecker H, Ceballos-Baumann
AO, Valet M, Feurer R, Forstl H, Kurz A, Haussermann
P (2010) Metabolic alterations associated with impaired
clock drawing in Lewy body dementia. Psychiatry Res
181, 85-89.
Gnanalingham KK, Byrne EJ, Thornton A (1996) Clockface drawing to differentiate Lewy body and Alzheimer
type dementia. Lancet 347, 696-697.
Swanwick GR, Coen RF, Maguire CP, Coakley D, Lawlor
BA (1996) Clock-face drawing to differentiate dementia
syndrome. Lancet 347, 1115.
Ala TA, Hughes LF, Kyrouac GA, Ghobrial MW, Elble
RJ (2001) Pentagon copying is more impaired in dementia
with Lewy bodies than in Alzheimers disease. J Neurol
Neurosurg Psychiatry 70, 483-488.
Cormack F, Aarsland D, Ballard C, Tovee MJ (2004) Pentagon drawing and neuropsychological performance in
1731
1732
1733
1734
1735
1736
1737
1738
1739
1740
1741
1742
1743
1744
1745
1746
1747
1748
1749
1750
1751
1752
1753
1754
1755
1756
1757
1758
1759
1760
1761
1762
1763
1764
1765
1766
1767
1768
1769
1770
1771
1772
1773
1774
1775
1776
1777
1778
1779
1780
1781
1782
1783
1784
1785
1786
1787
1788
1789
1790
1791
1792
1793
1794
1795
L. Trojano and G. Gainotti / Drawing Disorders in Dementia
1796
1797
1798
1799
[166]
1800
1801
1802
1803
[167]
1804
1805
1806
1807
1808
[168]
1809
1810
[169]
1811
1812
[170]
1813
1814
1815
1816
[171]
1817
1818
1819
1820
[172]
1821
1822
1823
1824
1825
[173]
1826
1827
1828
1829
[174]
1830
1831
1832
[175]
1833
1834
1835
1836
[176]
1837
1838
1839
1840
1841
1842
[177]
1843
1844
1845
1846
[178]
1847
1848
1849
[179]
1850
1851
[180]
1852
1853
1854
1855
[181]
1856
1857
1858
1859
1860
[182]
dementia with Lewy bodies, Alzheimers disease, Parkinsons disease and Parkinsons disease with dementia. Int J
Geriatr Psychiatry 19, 371-377.
Connor DJ, Salmon DP, Sandy TJ, Galasko D, Hansen LA,
Thal LJ (1998) Cognitive profiles of autopsy-confirmed
Lewys body variant vs pure Alzheimer disease. Arch
Neurol 55, 994-1000.
Caffarra P, Gardini S, Dieci F, Copelli S, Maset L, Concari L, Farina E, Grossi E (2013) The qualitative scoring
MMSE pentagon test (QSPT): A new method for differentiating dementia with Lewy Body from Alzheimers
disease. Behav Neurol 27, 213-220.
Vallar G (1998) Spatial hemineglect in humans. Trends
Cog Sci 2, 87-97.
Sandson J, Albert ML (1987) Perseveration in behavioural
neurology. Neurology 37, 1736-1741.
Rouleau I, Salmon DP, Butters N, Kennedy C, McGuire
K (1992) Quantitative and qualitative analyses of clock
drawings in Alzheimers and Huntingtons disease. Brain
Cog 18, 70-87.
Ryan PJ, McGowan J, McCaffrey N, Terrence Ryan
G, Zandi T, Brannigan GG (1995) Graphomotor perseveration and wandering in Alzheimers disease. J Ger
Psychiatry Neurol 8, 209-212.
Lamar M, Podell K, Carew TG, Cloud BS, Resh R,
Kennedy C, Goldberg E, Kaplan E, Libon DJ (1997) Perseverative behaviour in Alzheimers disease and subcortical
ischemic vascular dementia. Neuropsychology 11, 523534.
Cosentino S, Jefferson A, Chute DL, Kaplan E, Libon DJ
(2004) Clock drawing errors in dementia: Neuropsychological and neuroanatomical considerations. Cogn Behav
Neurol 17, 74-84.
De Lucia N, Grossi D, Trojano L (2015) The genesis of
graphic perseverations in Alzheimers Disease and Vascular Dementia. Clin Neuropsychol 30, 1-14.
Snowden JS, Neary D, Mann DM (1996) Fronto-temporal
Lobar Degeneration: Fronto-temporal Dementia, Progressive Aphasia, Semantic Dementia, Churcill Livingstone, New York, pp. 49-50
Aarsland D, Litvan I, Salmon D, Galasko D, WentzelLarsen T, Larsen JP (2003) Performance on the dementia
rating scale in Parkinsons disease with dementia and
dementia with Lewy bodies: Comparison with progressive supranuclear palsy and Alzheimers disease. J Neurol
Neurosurg Psychiatry 74, 1215-1220.
Doubleday EK, Snowden JS, Varma AR, Neary D
(2002) Qualitative performance characteristics differentiate dementia with Lewy bodies and Alzheimers disease.
J Neurol Neurosurg Psychiatry 72, 602-607.
Best F (1917) Hemianopsie und Seelenblindheit bei
Hirnverletzungen. Graefes Archiv fur Ophtalmologie 93,
149-150.
Strauss H (1924) Ueber konstructive Apraxie. Mschr Psychiatr 56, 65-124.
Solms M, Turnbull OH, Kaplan-Solms K, Miller P (1998)
Rotated drawing: The range of performance and anatomical correlates in a series of 16 patients. Brain Cogn 38,
358-368.
Della Sala S, Turnbull O, Beschin N, Perini M (2002) Orientation agnosia in pentagon copying. J Neurol Neurosurg
Psychiatry 72, 129-130.
Isella V, Traficante D, Tagliabue CF, Mapelli C, Ferri F,
Caffarra P, Appollonio IM (2013) A retrospective survey
on rotated drawing in persons with mild cognitive impair-
[183]
[184]
[185]
[186]
[187]
[188]
[189]
[190]
[191]
[192]
[193]
[194]
[195]
[196]
[197]
[198]
[199]
21
ment or degenerative dementia. Clin Neuropsychol 27,
1300-1315.
Molteni F, Traficante D, Ferri F, Isella V (2014) Cognitive profile of patients with rotated drawing at copy
or recall: A controlled group study. Brain Cogn 85,
286-90.
Ober BA, Jagust WJ, Koss E, Delis DC, Friedland RP
(1991) Visuoconstructive performance and regional cerebral glucose metabolism in Alzheimers disease. J Clin
Exp Neuropsychol 13, 752-772.
Gainotti G, Parlato V, Monteleone D, Carlomagno S
(1992) Neuropsychological markers of dementia on visuospatial tasks: A comparison between Alzheimers type
and vascular forms of dementia. J Clin Exp Neuropsychol
14, 239-252.
Kwak YT (2004) Closing-in phenomenon in Alzheimers
disease and subcortical vascular dementia. BMC Neurology 26, 1-7.
Ambron E, Allaria F, McIntosh RD, Della Sala S (2009)
Closing-in behaviour in fronto-temporal dementia. J Neurol 256, 1004-1006.
Grossi D, De Lucia N, Milan G, Trojano L (2015)
Relationships between environmental dependency and
closing-in in Patients with Fronto-temporal Dementia.
J Int Neuropsychol Soc 21, 1-7.
De Lucia N, Trojano L, Vitale C, Grossi D, Barone
P, Santangelo G (2015) The closing-in phenomenon in
Parkinsons disease. Parkinsonism Relat Disord 21, 793796.
De Lucia N, Grossi D, Mauro A, Trojano L (2015)
Closing-in in Parkinsons disease individuals with dementia: An experimental study. J Clin Exp Neuropsychol 37,
946-955.
De Renzi E (1959) Osservazioni semeiogenetiche in
tema di aprassia costruttiva. Riv Sper Freniat 58,
231-256.
Lee BH, Chin J, Kang SJ, Kim EJ, Park KC, Na DL (2004)
Mechanism of the closing-in phenomenon in a figure copying task in Alzheimers disease patients. Neurocase 10,
393-397.
Serra L, Fadda L, Perri R, Caltagirone C, Carlesimo GA
(2010) The closing-in phenomenon in the drawing performance of Alzheimers disease patients: A compensation
account. Cortex 46, 1031-1036.
McIntosh RD, Ambron E, Della Sala S (2008) Evidence
for an attraction account of closing-in behaviour. Cogn
Neuropsychol 25, 376-394.
Kwon JC, Kang SJ, Lee BH, Chin J, Heilman KM, Na DL
(2002) Manual approach during hand gesture imitation.
Arch Neurol 59, 1468-1475.
Ambron E, McIntosh RD, Finotto S, Clerici F, Mariani C,
Della Sala S (2012) Closing-in behavior in mild cognitive
impairment: An executive deficit. J Int Neuropsychol Soc
18, 269-276.
De Lucia N, Grossi D, Maria Fasanaro A, Carpi S, Trojano L (2013) Frontal defects contribute to the genesis of
closing-in in Alzheimers disease patients. J Int Neuropsychol Soc 19, 802-808.
Kwon SY, Lee ES, Hong YJ, Lim SC, Ahn KJ, Yoon D,
Shim YS, Yang DW (2015) Anatomical correlates of the
Closing-In phenomenon. Dement Neurocogn Disord 14,
17-23.
Gainotti G, Caltagirone C, Masullo C, Miceli G (1980)
Patterns of neuropsychological impairment detected in
various diagnostic groups of dementia. In Aging of
1861
1862
1863
1864
1865
1866
1867
1868
1869
1870
1871
1872
1873
1874
1875
1876
1877
1878
1879
1880
1881
1882
1883
1884
1885
1886
1887
1888
1889
1890
1891
1892
1893
1894
1895
1896
1897
1898
1899
1900
1901
1902
1903
1904
1905
1906
1907
1908
1909
1910
1911
1912
1913
1914
1915
1916
1917
1918
1919
1920
1921
1922
1923
1924
1925
22
1926
1927
1928
[200]
1929
1930
1931
1932
[201]
1933
1934
1935
1936
1937
1938
[202]
L. Trojano and G. Gainotti / Drawing Disorders in Dementia
the brain and dementia, L Amaducci, AN Davison, P
Antuono, eds. Raven Press, New York, pp. 245-250.
Villa G, Gainotti G, De Bonis C (1986) Constructive
disabilities in focal brain-damaged patients: Influence of
hemispheric side, locus of lesion and coexistent mental
deterioration. Neuropsychologia 24, 497-510.
Libon DJ, Malamut BL, Swenson R, Sands LP, Cloud
BS (1996) Further analyses of clock drawings among
demented and nondemented older subjects. Arch Clin Neuropsychol 11, 193-205.
Cacho J, Garca-Garca R, Fernandez-Calvo B, Gamazo
S, Rodrguez-Perez R, Almeida A, Contador I (2005)
Improvement pattern in the clock drawing test in early
Alzheimers disease. Eur Neurol 53, 140-145.
[203]
[204]
[205]
Patterson K, Nestor PJ, Rogers TT (2007) Where do you
know what you know? The representation of semantic
knowledge in the human brain. Nat Rev Neurosci 8, 976987.
Rapoport SI (1991) Positron emission tomography in
Alzheimers disease in relation to disease pathogenesis: A
critical review. Cerebrovasc Brain Metab Rev 3, 297-335.
Schroeter ML, Stein T, Maslowski N, Neumann J
(2009) Neural correlates of Alzheimers disease and
mild cognitive impairment: A systematic and quantitative meta-analysis involving 1351 patients. Neuroimage
47, 1196-1206.
1939
1940
1941
1942
1943
1944
1945
1946
1947
1948
1949
1950
Das könnte Ihnen auch gefallen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Comparison of Two TDCS Protocols On Pain and EEG Alpha 2 Oscillations in Women With FibromyalgiaDokument7 SeitenComparison of Two TDCS Protocols On Pain and EEG Alpha 2 Oscillations in Women With FibromyalgiaIcaroNoch keine Bewertungen
- The Evolution of The Brain, The Human Nature of Cortical Circuits, and Intellectual Creativity Javier DeFelipe1,2,3Dokument17 SeitenThe Evolution of The Brain, The Human Nature of Cortical Circuits, and Intellectual Creativity Javier DeFelipe1,2,3Bliss Tamar LoladzeNoch keine Bewertungen
- Neuropsychology and Neuropsychiatry of Neurodegenerative DisordersDokument192 SeitenNeuropsychology and Neuropsychiatry of Neurodegenerative DisordersIcaroNoch keine Bewertungen
- PRISMA 2009 Flow DiagramDokument1 SeitePRISMA 2009 Flow DiagramKou YashiroNoch keine Bewertungen
- Luria's Three-Step Test: What Is It and What Does It Tell Us?Dokument5 SeitenLuria's Three-Step Test: What Is It and What Does It Tell Us?IcaroNoch keine Bewertungen
- 10 1016@j Clinph 2018 03 020Dokument9 Seiten10 1016@j Clinph 2018 03 020IcaroNoch keine Bewertungen
- Comparison of Two TDCS Protocols On Pain and EEG Alpha 2 Oscillations in Women With FibromyalgiaDokument7 SeitenComparison of Two TDCS Protocols On Pain and EEG Alpha 2 Oscillations in Women With FibromyalgiaIcaroNoch keine Bewertungen
- 82 534 3 PBDokument10 Seiten82 534 3 PBIcaroNoch keine Bewertungen
- Using Latent Class Analysis To Model Prescription Medications in The Measurement of Falling Among A Community Elderly PopulationDokument7 SeitenUsing Latent Class Analysis To Model Prescription Medications in The Measurement of Falling Among A Community Elderly PopulationIcaroNoch keine Bewertungen
- Trajectories of Decline in Cognition and Daily FunctioningDokument10 SeitenTrajectories of Decline in Cognition and Daily FunctioningIcaroNoch keine Bewertungen
- Statistical Procedures For Determining The Extent of Cognitive Change Following ConcussionDokument7 SeitenStatistical Procedures For Determining The Extent of Cognitive Change Following Concussionpsyquis2Noch keine Bewertungen
- Vancouver Condensed Guide 2015Dokument8 SeitenVancouver Condensed Guide 2015Sameer SharmaNoch keine Bewertungen
- Kos Toulas 2017Dokument11 SeitenKos Toulas 2017IcaroNoch keine Bewertungen
- Test-Instructions - Category Fluency TestDokument14 SeitenTest-Instructions - Category Fluency TestIcaroNoch keine Bewertungen
- 1980 5764 DN 11 01 00006Dokument9 Seiten1980 5764 DN 11 01 00006IcaroNoch keine Bewertungen
- Criteria Lewy 2017 Neurology McKeith BlancDokument15 SeitenCriteria Lewy 2017 Neurology McKeith BlancIcaroNoch keine Bewertungen
- Bozeat2000 PDFDokument9 SeitenBozeat2000 PDFIcaroNoch keine Bewertungen
- Example How To Write A ProposalDokument9 SeitenExample How To Write A ProposalSpoorthi PoojariNoch keine Bewertungen
- Brain and Cognitive Reserve Translation Via NetworkDokument48 SeitenBrain and Cognitive Reserve Translation Via NetworkIcaro100% (1)
- Cancellation Task in Very Low Educated PeopleDokument9 SeitenCancellation Task in Very Low Educated PeopleIcaroNoch keine Bewertungen
- LSDDokument2 SeitenLSDI-Sun Deep Mohan TeaNoch keine Bewertungen
- Dee 0006 0020Dokument8 SeitenDee 0006 0020IcaroNoch keine Bewertungen
- How Effective Is The Trail Making TestDokument5 SeitenHow Effective Is The Trail Making TestIcaroNoch keine Bewertungen
- Indications For NeuropsychologicalDokument5 SeitenIndications For NeuropsychologicalIcaroNoch keine Bewertungen
- The Clock Drawing TestDokument13 SeitenThe Clock Drawing TestIcaroNoch keine Bewertungen
- New Scoring Methodology Improves The Adas CogDokument17 SeitenNew Scoring Methodology Improves The Adas CogIcaroNoch keine Bewertungen
- Sleep and Human AgingDokument18 SeitenSleep and Human AgingIcaroNoch keine Bewertungen
- Sleep and Executive Functions in Older Adults - A Systematic ReviewDokument14 SeitenSleep and Executive Functions in Older Adults - A Systematic ReviewIcaroNoch keine Bewertungen
- Living With Chronic Illness ScaleDokument6 SeitenLiving With Chronic Illness ScaleIcaroNoch keine Bewertungen
- Effects of Age, APOE ε4, Cognitive Reserve and Hippocampal Volume on Cognitive InterventionDokument8 SeitenEffects of Age, APOE ε4, Cognitive Reserve and Hippocampal Volume on Cognitive InterventionIcaroNoch keine Bewertungen
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Bala Songs - English VersionDokument40 SeitenBala Songs - English Versionasha manoharanNoch keine Bewertungen
- Test 1A- Lê thị thanh xuânDokument4 SeitenTest 1A- Lê thị thanh xuânGia Minh Lý TrầnNoch keine Bewertungen
- CLMS Teacher Guide PDFDokument27 SeitenCLMS Teacher Guide PDFmatheus_aurelio123Noch keine Bewertungen
- Live Project of Business Research MethodsDokument11 SeitenLive Project of Business Research Methodsmuthu_voilaNoch keine Bewertungen
- Elapsed Time LessonDokument3 SeitenElapsed Time Lessonapi-2492380990% (1)
- Open Forum 1 Transcript Chapter 1Dokument1 SeiteOpen Forum 1 Transcript Chapter 1sh100% (1)
- Various PurposesDokument22 SeitenVarious PurposesLJNoch keine Bewertungen
- Irregular Verbs PDFDokument1 SeiteIrregular Verbs PDFSeckin CicekNoch keine Bewertungen
- CBSE Class 8th English 2016 17Dokument7 SeitenCBSE Class 8th English 2016 17cxsdvNoch keine Bewertungen
- Demotic Dictionary Project: Stephen VinsonDokument4 SeitenDemotic Dictionary Project: Stephen VinsonLoly AliNoch keine Bewertungen
- Discussion Rubric ExamplesDokument6 SeitenDiscussion Rubric ExamplesDilausan B MolukNoch keine Bewertungen
- Introduction To Git: Architecture of CVCSDokument34 SeitenIntroduction To Git: Architecture of CVCSamit guptaNoch keine Bewertungen
- Lecture 5: Graphs: IIT KanpurDokument7 SeitenLecture 5: Graphs: IIT KanpursevroussnapeNoch keine Bewertungen
- CE 2 UNIT 1 NotesDokument8 SeitenCE 2 UNIT 1 NotesRoshan MallipeddiNoch keine Bewertungen
- Business Communication Lecture PPTs Unit-1Dokument40 SeitenBusiness Communication Lecture PPTs Unit-1Amit KumarNoch keine Bewertungen
- WEEK 1 Affirming and Negating Words and ExpressionsDokument108 SeitenWEEK 1 Affirming and Negating Words and ExpressionsCarmelita Lim DabuetNoch keine Bewertungen
- Simple ApprehensionDokument1 SeiteSimple ApprehensionAllan MacacapagalNoch keine Bewertungen
- Tu FuDokument2 SeitenTu FuRyan Bustillo85% (13)
- Insite MES (Manufacturing Execution System) : ChannabasappaDokument15 SeitenInsite MES (Manufacturing Execution System) : Channabasappabalamurugan_abapNoch keine Bewertungen
- Shuklaambara Dharam VishnumDokument115 SeitenShuklaambara Dharam VishnumNeelesh Kamath100% (4)
- Trinity Sunday: Proper Prayers of The Mass in The Extraordinary FormDokument2 SeitenTrinity Sunday: Proper Prayers of The Mass in The Extraordinary FormGottfried Zedfihar Flave TarihoranNoch keine Bewertungen
- Shaivism - Wikipedia, The Free EncyclopediaDokument6 SeitenShaivism - Wikipedia, The Free EncyclopediaShree Vishnu ShastriNoch keine Bewertungen
- Ubc 2004-0342 PDFDokument136 SeitenUbc 2004-0342 PDFDario JimenezNoch keine Bewertungen
- The Cambridge Encyclopedia of Language: Third EditionDokument7 SeitenThe Cambridge Encyclopedia of Language: Third Editionjashan singhNoch keine Bewertungen
- SnapTwain ManualDokument17 SeitenSnapTwain ManualKaijNoch keine Bewertungen
- Sequence and SeriesDokument97 SeitenSequence and SeriesArindam PrakashNoch keine Bewertungen
- Intro To Poetry 1Dokument51 SeitenIntro To Poetry 1Rhonel Galutera100% (1)
- CT Routine Std-IVDokument2 SeitenCT Routine Std-IVMd Masud RanaNoch keine Bewertungen
- CS251 SE-1 (شعبة عامة لائحة قديمة) Midterm Exam (Spring 2023) ANSWER KEYDokument2 SeitenCS251 SE-1 (شعبة عامة لائحة قديمة) Midterm Exam (Spring 2023) ANSWER KEYعمرو جمالNoch keine Bewertungen
- Suggested Solutions To Test: Email Address: Ymei@math - Cuhk.edu - Hk. (Any Questions Are Welcome!)Dokument3 SeitenSuggested Solutions To Test: Email Address: Ymei@math - Cuhk.edu - Hk. (Any Questions Are Welcome!)Bryan Steve PichuchoNoch keine Bewertungen