Beruflich Dokumente
Kultur Dokumente
Paternal Postpartum Depression
Hochgeladen von
jmister810 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
32 Ansichten1 SeitePaternal postpartum depression is associated with behavioral problems, hyperactivity. The prevalence of paternal depression 6 to 12 months after birth was 10%. Psychiatric diagnoses were more common in offspring of depressed fathers.
Originalbeschreibung:
Copyright
© © All Rights Reserved
Verfügbare Formate
DOCX, PDF, TXT oder online auf Scribd lesen
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenPaternal postpartum depression is associated with behavioral problems, hyperactivity. The prevalence of paternal depression 6 to 12 months after birth was 10%. Psychiatric diagnoses were more common in offspring of depressed fathers.
Copyright:
© All Rights Reserved
Verfügbare Formate
Als DOCX, PDF, TXT herunterladen oder online auf Scribd lesen
0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
32 Ansichten1 SeitePaternal Postpartum Depression
Hochgeladen von
jmister81Paternal postpartum depression is associated with behavioral problems, hyperactivity. The prevalence of paternal depression 6 to 12 months after birth was 10%. Psychiatric diagnoses were more common in offspring of depressed fathers.
Copyright:
© All Rights Reserved
Verfügbare Formate
Als DOCX, PDF, TXT herunterladen oder online auf Scribd lesen
Sie sind auf Seite 1von 1
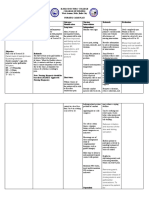
Paternal Postpartum Depression
Three main points:
Prevalence of paternal depression during the first three postpartum months is about 8 percent. Moderate
positive correlation between paternal and maternal depression
Depression in fathers (not mothers) of preterm infants was associated with significantly lower cognitive
function in the child at 2 years. Paternal postpartum depression associated with psychiatric diagnoses (eg,
oppositional defiant/conduct disorder and anxiety disorders), behavioral problems, and hyperactivity in their
children. Possible reasons why: less likely to engage with their children, are more likely to use aggressive or
harsh discipline, less parent-to-child reading, marital conflict
The EPDS is a suitable screening tool for fathers in the postpartum period, albeit cutoffs are different to
those applicable in women. It is important to note the EPDS does not diagnose depression but can alert the
clinician to the need for a full diagnostic interview
Prevalence and risk factors
The estimated prevalence of postpartum depression for mothers ranges from 8 to 15%
The prevalence of paternal depression during the first three postpartum months was 8%
The prevalence of paternal depression 6 to 12 months after birth was 10%.
The correlation between paternal and maternal depression was positive and moderate in size (r = 0.308; 95%
CI, 0.228-0.384).
Risk factors for postnatal paternal depression: Prenatal anxiety or depression, Lifetime history of severe
depression, Marital discord, Maternal prenatal depression, Other children in the family
Impact on infant outcomes
Behavioral problems and hyperactivity occurred in more children whose fathers had suffered postpartum
depression (even after controlling for maternal depression and other risk factors).
The increased risk for behavioral problems associated with depression in fathers during the infant's early
months also remains after controlling for later paternal depression.
Psychiatric diagnoses (eg, oppositional defiant/conduct disorder and anxiety disorders) were more common
in offspring of depressed fathers than offspring of nondepressed fathers (12 versus 6 percent) independent of
maternal postnatal depression.
Children of fathers with higher depressive symptoms had lower cognitive function at age of 24 months,
even after adjustment for maternal depressive symptoms and childrens biological and social risk factors.
These associations were not found for mothers.
Possible reasons why there was an association with lower cognitive function: Fathers less likely to engage
with their children, are more likely to use aggressive or harsh discipline, less likely to read to their child,
more martial conflict
Screening
A quick self-report screen
1) "Since your new baby was born, have you felt down, depressed, or hopeless?"
2) "Since your new baby was born, have you had little interest or little pleasure in doing things?"
One Yes answer constitutes a positive screen.
The Edinburg Postnatal Depression Scale (EPDS) is a reliable and valid measure of mood in fathers.
Several studies validating it in paternal postpartum depression.
One study from 2001: Screening for depression or anxiety disorders in fathers requires a two point lower
cut-off than screening for depression or anxiety in mothers (7/8), and we recommend this cut-off to be 5/6.
2.3% of fathers endorsed question 9 (I have been so unhappy that I have been crying)
compared to 44.1% of mothers
Das könnte Ihnen auch gefallen
- Test Upload For Scribd 6747Dokument1 SeiteTest Upload For Scribd 6747jmister81Noch keine Bewertungen
- Test Upload For Scribd 67472821Dokument1 SeiteTest Upload For Scribd 67472821jmister81Noch keine Bewertungen
- Paternal Postpartum DepressionDokument4 SeitenPaternal Postpartum Depressionjmister81Noch keine Bewertungen
- Paternal Postpartum DepressionDokument1 SeitePaternal Postpartum Depressionjmister81Noch keine Bewertungen
- HaNDL - Headaches and LymphocytosisDokument2 SeitenHaNDL - Headaches and Lymphocytosisjmister81Noch keine Bewertungen
- Psychogenic Nonepileptic SeizuresDokument3 SeitenPsychogenic Nonepileptic Seizuresjmister81Noch keine Bewertungen
- Paternal Postpartum DepressionDokument4 SeitenPaternal Postpartum Depressionjmister81Noch keine Bewertungen
- Evidence For Albumin in PreeclampsiaDokument2 SeitenEvidence For Albumin in Preeclampsiajmister81Noch keine Bewertungen
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5782)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (587)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (72)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (265)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (119)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- הוראות הפעלה Resmart Gii Auto Cpap System e 20a h oDokument37 Seitenהוראות הפעלה Resmart Gii Auto Cpap System e 20a h oAntonio AcostaNoch keine Bewertungen
- REFLEXOLOGY PresentationDokument15 SeitenREFLEXOLOGY Presentationdanielle palm100% (4)
- Icmr PPT (1) VidhiDokument32 SeitenIcmr PPT (1) VidhiVidhi GuptaNoch keine Bewertungen
- Case Studies - MIC3002Dokument28 SeitenCase Studies - MIC300217206404 STUDENTNoch keine Bewertungen
- 10.1007-S00210-008-027serotonin Pharmacology in The Gastrointestinal Tract: A ReviewDokument23 Seiten10.1007-S00210-008-027serotonin Pharmacology in The Gastrointestinal Tract: A ReviewanataeusNoch keine Bewertungen
- ResearchDokument10 SeitenResearchBea Angela Cabajar100% (1)
- What Is Systolic Blood Pressure?Dokument6 SeitenWhat Is Systolic Blood Pressure?sachinsuvarna1986Noch keine Bewertungen
- Hepatitis TableDokument2 SeitenHepatitis Tableampogison08Noch keine Bewertungen
- Deficient Fluid Volume (Vanene)Dokument7 SeitenDeficient Fluid Volume (Vanene)jajalerNoch keine Bewertungen
- Internship Manual 20-21 PDFDokument19 SeitenInternship Manual 20-21 PDFMsalik1Noch keine Bewertungen
- Lyphochek Immunology Plus Control Levels 1 and 2: 430 430X Bilevel Minipak 12 X 1 ML 2 X 1 ML Level 1 27551 Level 2 27552Dokument6 SeitenLyphochek Immunology Plus Control Levels 1 and 2: 430 430X Bilevel Minipak 12 X 1 ML 2 X 1 ML Level 1 27551 Level 2 27552Ade FeriyatnaNoch keine Bewertungen
- Alternatives To Hysterectomy: Duncan Turner MD, MBBS, Facog, October 28th 1998 Santa Barbara, CaliforniaDokument39 SeitenAlternatives To Hysterectomy: Duncan Turner MD, MBBS, Facog, October 28th 1998 Santa Barbara, Californiadekate_manojNoch keine Bewertungen
- General Parasitology L2Dokument27 SeitenGeneral Parasitology L2kayse abtidoonNoch keine Bewertungen
- Eye MD Examination Report Form - CopyrightDokument1 SeiteEye MD Examination Report Form - CopyrightsolihaNoch keine Bewertungen
- Nursing Care Plan (Acute Cholecystitis) - NAVARRADokument6 SeitenNursing Care Plan (Acute Cholecystitis) - NAVARRAami forevsNoch keine Bewertungen
- Efficacy and Safety of Rabeprazole in Children.20Dokument10 SeitenEfficacy and Safety of Rabeprazole in Children.20Ismy HoiriyahNoch keine Bewertungen
- Souvenir Book Updated Compressed-1 PDFDokument184 SeitenSouvenir Book Updated Compressed-1 PDFManju Kumari100% (1)
- Homeopathic Relief for DepersonalizationDokument4 SeitenHomeopathic Relief for DepersonalizationAnonymous dpxYTENoch keine Bewertungen
- Incentive SpirometryDokument1 SeiteIncentive Spirometry11- Nolasco, Mary Rose F.Noch keine Bewertungen
- Warfarin INR Antibx InteractionDokument3 SeitenWarfarin INR Antibx InteractionSheila UlinaNoch keine Bewertungen
- 8688 Bas Tses Winter 2020 Online pg14 15889Dokument2 Seiten8688 Bas Tses Winter 2020 Online pg14 15889Léo TavaresNoch keine Bewertungen
- Nursing Care For Patient With Wilms TumorDokument2 SeitenNursing Care For Patient With Wilms TumorAnusha Verghese100% (2)
- Diabetic Ketoacidosis - Anand Singh BrarDokument5 SeitenDiabetic Ketoacidosis - Anand Singh BrarAnand Singh BrarNoch keine Bewertungen
- Puberty and The HPG AxisDokument36 SeitenPuberty and The HPG AxiskjhkaNoch keine Bewertungen
- Tugas GinjalDokument22 SeitenTugas GinjalAnastasia MargaretNoch keine Bewertungen
- Post-Debridement Nursing Care PlanDokument2 SeitenPost-Debridement Nursing Care PlanAbdelmar SusulanNoch keine Bewertungen
- Discharge PlanningDokument1 SeiteDischarge PlanningChyNoch keine Bewertungen
- G-CFA Instructor Tab 6-2 Handout 2 Sample Adequate Nursing Care Plan-R6Dokument2 SeitenG-CFA Instructor Tab 6-2 Handout 2 Sample Adequate Nursing Care Plan-R6SriMathi Kasi Malini ArmugamNoch keine Bewertungen
- Anaesthesia - 2020 - Griffiths - Guideline For The Management of Hip Fractures 2020Dokument13 SeitenAnaesthesia - 2020 - Griffiths - Guideline For The Management of Hip Fractures 2020BBD BBDNoch keine Bewertungen
- Top Communicable Diseases in The Philippines 2019Dokument4 SeitenTop Communicable Diseases in The Philippines 2019Nicole cuencosNoch keine Bewertungen