Beruflich Dokumente
Kultur Dokumente
Case 9 Infertility
Hochgeladen von
juliusCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Case 9 Infertility
Hochgeladen von
juliusCopyright:
Verfügbare Formate
CASE 9: INFERTILITY
INFERTILITY
Failure to conceive of 1 year of unprotected sexual
contact meaning the couple is not practicing any
artificial or natural form of family planning
IF >35: investigation should begin AFTER 6 months
Classification:
1. Primary - Never had any pregnancy
2. Secondary Had been pregnant either abnormal or
normal as G1P0 (0010) or G1P1 (1001)
As long as the woman got pregnant regardless of the
outcome of the pregnancy labeled as GRAVIDITY.
Regardless of whether it is primary or secondary, it will
follow a similar pattern.
History Taking:
First visit: Ideally should be a couple,
First part: Investigative: who is at fault?
First explain: Physiology
IMPT: Correct attitude of the couple PATIENCE
The past history may give inkling, like if the
menstrual history is very erratic chances are the
woman in anovulatory. Even if by menstrual history,
I know she is anovulatory, I cannot give outright
anovulatory drugs. Why? I will make her ovulate but
if her tubes are obstructed, ovulation is useless.
General Data:
Age
Female: Fertility rate by age 30 goes down by 50%
Male: Perhaps on the 60s related to erectile
dysfunction, esp. if diabetic becoming impotent
Occupation: Male (Hot Seats, OFW gone for
several years)
HPI:
Its not about how long have you been married but
how long have you been together? How long have
you indulge in sexual activity?
What do you do to try to get pregnant?
Sexual Hx:
Frequency of sexual contact. The normal average
should be 2 3x/week due to the 72 hours lifespan
of the sperm inside the uterine cavity for continuous
supply of sperm. It must be per week because you
are actually given a day to get pregnant in a month
(time the woman ovulates). So if you have contact
day before ovulation, the sperm is expected to live
until the day of ovulation.
Problem: Dyspareunia (Sx: Endometriosis)
After sexual contact the seminal fluid has nowhere
to go except to come out from the vagina on the
premise the sperm cells have already migrated into
the uterine cavity & perhaps into the fallopian tube.
The seminal fluid is not expected to go inside the
cervix.
OFW: be discrete in asking questions. Have you had
a child with another or STID?
Menstrual Hx:
Menarche, succeeding menstruation, interval
between the cycle (28 , 28 32, 32 35)
IMPT to know: interval of the cycles to be able to
predict when ovulation will occur.
o In 28 day cycle: Expected ovulation D14
nd
because the 2 half of the cycle is more
constant due to lifespan of Corpus luteum.
o In 35 day cycle: Expected ovulation D21
Past Personal History
Especially for the male, ask for childhood diseases
particularly "MUMPS ORCHITIS"
Past Medical History:
Previous
abdominal
&
pelvic
surgeries
(appendectomy, ovarian surgery, laparoscopy):
Assess risk for adhesions (Peritoneal factor)
Physical Exam:
Aside from pelvic examination, is there any particular
organ needed to check?
Breasts:
Breast changes During Menses
Breast changes are affected by which hormone is
predominant. Right after the menstrual cycle the
breast are non-tender & less engorged. But as you
go to the secretory phase, with the effects of E + P,
breasts become fuller & tender.
Thats why during PE, do not examine the breast
pre-menstrual. Take note when was the LMP?
Example: LMP - June 25. Today - July 23 Perhaps in a
day or so, she is expected to get her period. If she
has OVULATORY cycles, you will expect to feel more
engorged tender breast.
IMPT: PREMENSTRUAL gives inkling that her cycles
are OVULATORY.
Thyroid Gland:
HYPO/ HYPERTHYROIDISM
Ask for PMH, Signs & Symptoms
There are 3 basic work-up for infertility:
1. Male Factor:
Semen Analysis
2. Tubal Factor: Test for Tubal Patency
3. Ovarian Factor: Documentation of Ovulation
MALE FACTOR (Semen Analysis):
Male Factor: 40% cause of infertility (Dr. PPP & PGH)
th
25% (Katz Book 6 Ed)
Mumps Adults: Swelling of Testes
Infections STD: Testes, vas deferens, epididymis
Diabetes Affects the nerves
Exposure to radiation & chemotherapeutic agents
1 thing to do: Semen Analysis (volume, sperm
count, motility & morphology)
st
Table 41-4 Lower Fifth Percentile Values in Fertile Men
Parameter
Value Problems
Semen volume (mL)
1.5
Sperm concentration (million/mL)
15
Total number (million/ejaculate)
39
Oligo/Azoospermia
Total motility (%)
40
Asthenospermia
Progressive motility (%)
32
Normal forms (%)
4
Teratospermia
Requirement: 2- 3 days of abstinence (natural:
sexual contact & artificial: masturbation)
GOOD:
30 M, 50% motile
NOT GOOD: 50 M, 10% motile
If abnormal: REFER to URO (Infertility Specialist)
http://www.rrc.com/docs/Testing_Male-Fact.pdf
Book:
Best to examine within 2 hours
Liquefaction: 15 20 minutes after ejaculation
Sperm morphology: Kruger Criteria
TUBAL FACTOR (Tubal Patency):
History needed for tubal patency: previous
operation like appendectomy (formation of
adhesions) or endometriosis (peritubal adhesions)
PID, Thyroid Fever, TB Salphingitis
OVARIAN FACTOR (Documentation of Ovulation)
Presumptive Evidences of Ovulation:
1. Menstrual History
To know if the cycle is ovulatory: Start by Menstrual Hx
If the cycles are regular, periodic & predictable,
these are usually preceded with PREMENSTRUAL
MOLIMINA which predicts the impending ovulation &
subsequent menstruation.
Premenstrual Molimina: are the symptoms,
sensations, feelings, & observations, such as
bloating, headaches, nausea, ovulatory pain, &
breast tenderness that many women experience
during the premenstrual phase of their cycles.
2.
Changes in Cervical Mucus: Spinnbarkeit & Ferning
There are certain predictors of ovulation. Looking
back at physiology:
After menstruation there will be a rise in estrogen in
FOLLICULAR PHASE under the effect of FSH. The
follicles will start producing Estrogen causing
proliferation of endometrium. Because of the peak
in E just before the menses (D12-D13) there will be
CHANGES IN THE CERVICAL MUCUS. The cervical mucus
will undergo 2 changes:
Spinnbarkeit reaction
Ferning test
Test for Tubal patency:
1. Hysterosalphingography, a radiologic procedure by
introduction (injection under fluoroscopy) of
contrast material (black dye) through the cervix, fill
up the uterus, traverse to the tube & out to the
pelvic cavity
Done a week AFTER menstruation
Give prophylactic antibiotics at time of HSG:
Doxycycline 100mg BID for 3 days (will last for 4
days)
http://www.rrc.com/docs/hsg.pdf
2.
3.
Sonohysterogram or sonohysterography: inject
saline to the cervix, filling up the endometrial cavity.
What will you see will be the turbulence due to the
exit of saline through the tube
UTZ: Fluid in the cul de sac
Laparoscopy + Chromotubation
Chromotubation is very similar to hysterogram
except the dye is a colored dye usually methylene
blue (need to have a vision of pelvic cavity directly)
Can also be: Laparotomy + Chromotubation- Open
abdomen
Among the 3 tests for tubal patency, the most basic
test used is HSG.
But if patient is OLDER: Age 35 36, do a more
aggressive work up, proceed straightforward to L + C to
be able demonstrate peri-tubal adhesions & outright lyse
the adhesions.
Other Notes:
If tubes are patent: IUI
If tubes are not patent: Microsurgery, Salphingectomy, IVF
Preovulatory
Postovulatory
Mucus is clear, watery & easily
stretched
Estrogen
Mucus is whitish/ opaque, can
break, beaded
Progesterone
If you notice these changes, then most likely you
might be having ovulatory cycles so this is the time
to schedule for contact.
These will not tell that a woman, she is going to
ovulate. It will only tell the presence of high E level
that will be the trigger for the secretion of LH.
Remember, ovulation is the effect of LH surge.
TREATMENT:
If the 3 basic workups results are normal, the treatment
may simply start by telling the couple when the RIGHT
time to have contact is/ TIMING of sexual contact.
3.
Biphasic Basal Body Temperature
Not used anymore
O
O
After menses: 36.8 C - 36.9 C
After ovulation: rise due to thermogenic effect of
PROGESTERONE,
O
If the woman will have her menses: DROP in C
If the woman will be pregnant: continuous rise
because of the progesterone coming from the
Corpus Luteum & eventually to be taken over
by the placenta
Presence of Biphasic rise in temperature will tell
most likely she has ovulatory cycle
Use: Ovulation thermometer which only have 36 O
38 C. As soon as the patient wakes up, sticks it
under the tongue & document daily (D1 to Last Day
of menses)
IF Ovarian Factor: Anovulation
PCOS (Rotterdam Criteria 2/3: Infertility,
Hyperandrogenism, Chronic Anovulation)
Thyroid, Hyperprolactinemia
TX: Induction of ovulation, Ovulatory drugs
Documentation of Ovulation:
4. Serial Follicular Monitoring
Most practical (Sonographic)
In a patient with a regular cycle, try to look at the
ovary starting D12. UTZ will tell if there is a
dominant follicle which measures: 16 mm to 18.5
mm at D14. Then if at D16: < 10 mm, that will tell
that the woman must have ovulated.
If you know at what diameter the follicle will
rupture, youll be able to predict when she is going
to ovulate. A dominant follicle measuring 18 - 22
mm will most likely ovulate.
Take note of:
i.
in Size of the Dominant Follicle
ii.
Presence of the Fluid in the Cul de sac because
with the extrusion of the egg from the ovary,
there will be a leakage of the antrum folliculi
that will stay in the cul de sac.
iii.
Change in the Endometrial Lining. If the woman
ovulated in D14 15, by D16 observe the
changes in the endometrial lining from
Proliferative to SECRETORY PHASE.
5.
6.
Endometrial biopsy
The presence of secretory endometrium telling that
a woman had ovulated because a woman will never
have a secretory endometrium in the absence of
progesterone.
Serum progesterone assay
Progesterone: woman must have ovulated
1.
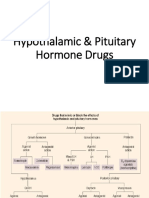
Clomiphene Citrate (ANTI-ESTROGEN)
Most popular drug to induce ovulation
Family of Tamoxifen
Works if there is ENOUGH Estrogen
Will not work IF lacks E2
Hypothalamus
GnRH
Pituitary
FSH & LH
Ovarian
Estrogen & Progesterone
Unexplained infertility/ Idiopathic
IF Normal Basic work ups
Do Laparoscopy + Chromopertubation: Check for Lesions
TX: Clomiphene, IUI, IVF (IF >35: do IVF Right Away)
Pituitary Glands will produce the gonadotropic
hormones: FSH & LH which will act on the ovaries
for the stimulation & development of the follicles.
These follicles would produce E.
Too much E would trigger the Negative Feedback
mechanism to stop the production of FSH.
Clomiphene Citrate Stimulation:
No negative feedback mechanism
Level of E will not be increase due to the antiestrogenic effect. So the hypothalamus cannot
sense the level of E & will keep producing GnRH,
increasing both FSH & LH.
Result: in the # of follicles chance of
ovulation
Drawback: Multi-fetal Pregnancy, Twinning
2.
Most will use serial follicular monitoring to
determine whether ovulation has taken place or not.
Ovulation
TVS: Antral Follicle Count (>5 follicle/ ovary)
AMH Most sensitive, secreted by granulosa
Age: FSH AMH
LH Level: Urine Kit
Easy to administer:, 50 mg - 150 mg taken on D3 D7 of the cycle per orem (worth: P280)
Do an UTZ to monitor the response
Gonadotropins
Given if with Pituitary Failure
Exogenous FSH & LH
O
1 indicated: HYPOGONADOTROPIC (Lack FSH & LH)
Administer: Parenteral (IM/SC), No oral preparation
In practice, cannot be given to any general GYNE but
only the infertility specialist because the problem is
development of OVARIAN HYPERSTIMULATION
SYNDROME wherein the ovaries grow in size.
Usually drugs for those who will undergo IVF
SE: Multi-fetal pregnancy, TWINNING
Other Notes:
Metformin An Adjunct Insulin Sensitizer
GnRH Given if Hypothalamus is not working
PCOS oral/injectable Last Resort: Surgery IVF
Among the factors in infertility, the easiest factor to
treat is the OVARIAN factor.
IF Turner's Syndrome (Ovarian Agenesis)
Can get pregnant but not of her own
Does not have primordial follicles (atrophied)
IF Tubal Factor:
IF Distal tubal obstruction
TX: Tubal Plastic Surgery (Micro)
Salphingostomy (Ostomy: opening)
Try to open the fimbriae by invert the end of the
tube (Like a bulb becoming a flower)
If with HSG, you see part of the tube is
normal but it ends in the middle (obstruction)
TX: Supplement HSG + Laparoscopy & do anastomosis
IVF:
Nowadays. IVF discovered primarily for a patient
whose tubes are obstructed.
In Vitro (Outside), Layman: Test Tube Baby
Success Rate: 30% chance to be able to get
pregnancy
Procedure:
1. Ovarian Hyperstimulation - to produce a lot of eggs
2. Oocyte Retrieval
Via UTZ try to get an egg from the ovary then
place in the TT or petri dish with sperm (the seminal
fluid will have to undergo sperm washing or sperm
swim up) & make them fertilized on their own
3. Fertilization
4. Embryo Transfer Back into the endometrium
ICSI: Intra-cytoplasmic Sperm Injection
If there is failure of IVF
Cryopreservation
Do the fertilization directly by introducing the sperm
into the cytoplasm of the egg
This may be also the option if the problem is the
peritoneal factor. A lot of patients with
endometriosis do IVF to attain pregnancy.
OTHER FACTORS:
CERVICAL FACTOR
Character of Cervical Mucus
IF maybe laden with macrophages because of an
infection in the lower genital tract, this may be
hostile to the sperm. It will kill the sperm & none
would swim up the endometrium.
Sometimes the cervical factor is being alluded as the
cause of a woman who seems to be normal after
evaluating the 3 basic factors (Male, Tubal &
Ovarian). We may think of the wife developing
antibodies against the sperms of the husband
Test: Post-coital Test (SIM HUHNER'S TEST)
No longer used
Ask the couple to have contact at 7 am, by 10 am
retrieval of some seminal fluid from the vagina &
placed in a slide. Check whether there are still
motile sperms present
IF all the sperms are dead, most likely the cervical
factor is involved.
Treatment:
The only way is to change your husband
Try to lower the antibodies in the female by
abstinence or use condoms
Nowadays, the sperms will no longer be deposited
in the vagina but directly into the endometrial cavity
called INTRAUTERINE INSEMINATION (IUI) the
seminal fluid collected will have to go to a
processing called: sperm wash or sperm swim up
which means trying to clear the seminal fluid of
debris & will only collect best sperm cells. This is
part of ART.
UTERINE FACTOR
Presence of polyp, submucous myoma
Remember after fertilization, in a few days the egg
will go down into the endometrium which is now
going to termed as the DECIDUA for implantation.
Sometimes this endometrial lining is not fertile for
implantation If this endometrium is not suitable for
implantation, no pregnancy will happen.
Test: Endometrial Biopsy
Most common problem as a Luteal Phase Defect.
PERITONEAL FACTOR
The ability of the distal end of the tube to pick up
the egg. The distal end of the tube has fimbriae
(finger like projections), when the woman ovulates
this fimbriae will detect that there is an egg
available for pick-up. So at the time of ovulation this
fimbriae will keep on moving, trying to pick the egg
termed as TUBAL PICK-UP MECHJANISM
So if there is anything here (adhesions) that the tube
cannot move, that egg will not find its place inside the
fallopian tube
When will you suspect? In patients with
Endometriosis (adhesions around the tube) or
previous PID
CASE 9
31 year old, married G1P1 (1001), vendor, wants to be
st
pregnant. She has been married for 3 years. Her 1 child was
with another partner. Her husband is a 33 y/o, truck driver. He
also has a 10 y/o child with a previous partner. She has regular
menses. PMH: 2008 diagnosed with PID, treated as an
outpatient. PPE: Speculum: cervix pink, smooth. IE: cervix
firm, long, closed; uterus normal size: adnexa no mass/
tenderness
Category: Secondary Infertility
Possible Cause: PID
Factors involved:
Tubal: Obstructed tube from intraluminal infection
Peritoneal: Adhesions from the distal end of the
tube
Test: Laparoscopy
Look into the pelvic cavity
The tubes may be patent but if they dont move,
that egg will never find its place in the tube.
Only after knowing the cause that you will be ready
to treat the patient, otherwise youll fail.
Work-ups
Do Semen analysis (sperm count changes every 72
days)
Do HSG.
Additional Notes from Dr. Dee 2013 (KQ )
For those who will be under Dr. PPP, please hide this. She likes to
browse thru your reviewer if she sees it on your table
Das könnte Ihnen auch gefallen
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- All Shifting Final Exam Questions Complete First Shift: M Ultiple C HoiceDokument11 SeitenAll Shifting Final Exam Questions Complete First Shift: M Ultiple C HoicejuliusNoch keine Bewertungen
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Written Revalida - 2012Dokument21 SeitenWritten Revalida - 2012juliusNoch keine Bewertungen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- BurnsDokument4 SeitenBurnsjuliusNoch keine Bewertungen
- Case 11 Lower Genital UTIDokument2 SeitenCase 11 Lower Genital UTIjuliusNoch keine Bewertungen
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- Female Infertility: An OverviewDokument12 SeitenFemale Infertility: An OverviewSuhar TomiNoch keine Bewertungen
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Male Hypogonadism - Basic, Clinical, and Therapeutic Principles PDFDokument407 SeitenMale Hypogonadism - Basic, Clinical, and Therapeutic Principles PDFMansoor Abbas100% (1)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- L5 The Menstrual CycleDokument12 SeitenL5 The Menstrual CycleKatrina Salas MiclatNoch keine Bewertungen
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Biology 12 - The Reproductive System!: Name: Block: DateDokument4 SeitenBiology 12 - The Reproductive System!: Name: Block: DateLerr Real Relle100% (1)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Amenorrhea - Algorithm & DifferentialsDokument9 SeitenAmenorrhea - Algorithm & DifferentialsItharshan IndreswaranNoch keine Bewertungen
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Infertility: Presented ByDokument47 SeitenInfertility: Presented ByNilakshi Barik MandalNoch keine Bewertungen
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- CTS-3 STARS Academy Multan Campus-Secure PDFDokument14 SeitenCTS-3 STARS Academy Multan Campus-Secure PDFHanzala ShahidNoch keine Bewertungen
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- AmenorrheaDokument41 SeitenAmenorrheadoraNoch keine Bewertungen
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- Reproductive and Endocrine System: Role of Hormones in The Male and Female Reproductive SystemDokument47 SeitenReproductive and Endocrine System: Role of Hormones in The Male and Female Reproductive Systempj100% (2)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- HY EndocrineDokument22 SeitenHY EndocrineoopsseNoch keine Bewertungen
- Exercise and The Menstrual CycleDokument14 SeitenExercise and The Menstrual CycleAndrew HaslettNoch keine Bewertungen
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Animal Biotechnology For Livestock Production 3 Springer, 2023Dokument334 SeitenAnimal Biotechnology For Livestock Production 3 Springer, 2023Gilbert MethewNoch keine Bewertungen
- 2nd Year Mcqs - Mcqs Physiology MedicalDokument4 Seiten2nd Year Mcqs - Mcqs Physiology MedicalKhadijaSarwarNoch keine Bewertungen
- Growing Pains: Problems With Puberty Suppression in Treating Gender DysphoriaDokument34 SeitenGrowing Pains: Problems With Puberty Suppression in Treating Gender DysphoriaColin Wright100% (2)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- Ob Maternity NotesDokument46 SeitenOb Maternity Notesr79cb5480100% (4)
- The Breasts Do Become Sensitive and Some Women DoDokument14 SeitenThe Breasts Do Become Sensitive and Some Women DoJaymih Santos AbasoloNoch keine Bewertungen
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- Embryo TransferDokument21 SeitenEmbryo TransferMARCO ANTONIO CABRERA PASCACIONoch keine Bewertungen
- D0679sci Part2 QR 2020 FinalDokument21 SeitenD0679sci Part2 QR 2020 FinalEND GAMINGNoch keine Bewertungen
- Birth Control Pill & Lupron Sample IVF CalendarDokument2 SeitenBirth Control Pill & Lupron Sample IVF Calendarandi hamatajNoch keine Bewertungen
- Anatomy and Physiology-Endocrine SystemDokument5 SeitenAnatomy and Physiology-Endocrine SystemEixid Enna YeLikNoch keine Bewertungen
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Bio ProjectDokument17 SeitenBio Projectsaifnkhannrahman100% (5)
- DPC-3 Word - 1Dokument42 SeitenDPC-3 Word - 1charlienitin1325Noch keine Bewertungen
- Postmenopausal Syndrome: Pronob K. Dalal, Manu AgarwalDokument11 SeitenPostmenopausal Syndrome: Pronob K. Dalal, Manu Agarwalwidya astutyloloNoch keine Bewertungen
- Reproduction in Humans: Test Yourself 18.1 (Page 335)Dokument4 SeitenReproduction in Humans: Test Yourself 18.1 (Page 335)leeNoch keine Bewertungen
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Adolescence by John Santrock - 15e, TEST BANK 0078035481Dokument38 SeitenAdolescence by John Santrock - 15e, TEST BANK 0078035481jksnmmmNoch keine Bewertungen
- Open Breast Disorders (Benign and Malignant) DoneDokument117 SeitenOpen Breast Disorders (Benign and Malignant) Donereema.saleh123Noch keine Bewertungen
- Hypothalamic & Pituitary Hormone DrugsDokument29 SeitenHypothalamic & Pituitary Hormone DrugsDylan MansillaNoch keine Bewertungen
- Body Condition and Suckling As Factor Influencing The Duration of Postpartum Anestrum in Cattle.Dokument26 SeitenBody Condition and Suckling As Factor Influencing The Duration of Postpartum Anestrum in Cattle.Raul KimNoch keine Bewertungen
- Up-To-Date Review About Minipuberty and Overview On Hypothalamic-Pituitary-Gonadal Axis Activation in Fetal and Neonatal LifeDokument9 SeitenUp-To-Date Review About Minipuberty and Overview On Hypothalamic-Pituitary-Gonadal Axis Activation in Fetal and Neonatal LifeBerry BancinNoch keine Bewertungen
- PNLE II For Maternal and Child HealthDokument13 SeitenPNLE II For Maternal and Child HealthASDF ASDF100% (1)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)