Beruflich Dokumente
Kultur Dokumente
Johnson 1992 PDF
Hochgeladen von
Gabriel IonescuOriginalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Johnson 1992 PDF
Hochgeladen von
Gabriel IonescuCopyright:
Verfügbare Formate
See
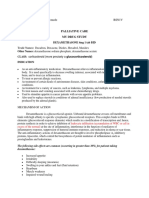
discussions, stats, and author profiles for this publication at: http://www.researchgate.net/publication/223334825
Mechanisms of stress: A dynamic overview of
hormonal and behavioral homeostasis
ARTICLE in NEUROSCIENCE & BIOBEHAVIORAL REVIEWS FEBRUARY 1992
Impact Factor: 10.28 DOI: 10.1016/S0149-7634(05)80175-7
CITATIONS
DOWNLOADS
VIEWS
432
141
164
4 AUTHORS, INCLUDING:
Elizabeth O Johnson
George Chrousos
National and Kapodistrian University of Athens
National and Kapodistrian University of Athens
143 PUBLICATIONS 4,465 CITATIONS
1,352 PUBLICATIONS 67,177 CITATIONS
SEE PROFILE
SEE PROFILE
Philip Gold
National Institutes of Health
451 PUBLICATIONS 29,501 CITATIONS
SEE PROFILE
Available from: Elizabeth O Johnson
Retrieved on: 19 September 2015
Neuroscienceand BiobehavioralReviews, Vol. 16, pp. 115-130, 1992
0149-7634/92 $5.00 + .00
Copyright 1992 Pergamon Press Ltd.
Printed in the USA. All rights reserved.
Mechanisms of Stress: A Dynamic Overview
of Hormonal and Behavioral Homeostasis
E L I Z A B E T H O. J O H N S O N , * t t T H E M I S C. K A M I L A R I S , * t G E O R G E P. C H R O U S O S * A N D P H I L I P W . G O L D t
*Developmental Endocrinology Branch, National hlstitute o f Child Health and Human Development and
"~Clinical Neuroendocrinology Branch, National hzstitute o f Mental Health, NIH, Bethesda MD 20892
R e c e i v e d 13 D e c e m b e r 1990
JOHNSON, E. O., T. C. KAMILARIS, G. P. CHROUSOS AND P. W. GOLD. Mechanisms of stress: A dynamic overview of
hormonal and behavioral homeostasis. NEUROSCI BIOBEHAV REV 16(2) 115-130, 1992.-Environmental events, both physical and emotional, can produce stress reactions to widely varying degrees. Stress can affect many aspects of physiology, and
levels of stress, emotional status, and means of coping with stress can influence health and disease. The stress system consists of
brain elements, of which the main components are the corticotropin-releasing hormone (CRH) and locus ceruleus (LC)-norepinephrine (NE)/autonomic systems, as well as their peripheral effectors, the pituitary-adrenal axis and the autonomic system, which
function to coordinate the stress response. Activation of the stress system results in behavioral and physical changes which allow
the organism to adapt. This system is closely integrated with other central nervous system elements involved in the regulation of
behavior and emotion, in addition to the axes responsible for reproduction, growth and immunity. With current trends in stress
research which focus on understanding the mechanisms through which the stress-response is adaptive or becomes maladaptive,
there is a growing association of stress system dysfunction, characterized by hyperactivity and/or hypoactivity to various pathophysiological states. The purpose of this review is to 11 define the concepts of stress and the stress response from a historical
perspective, 2) present a dynamic overview of the biobehavioral mechanisms that participate in the stress response, and 3) examine the consequences of stress on the physiologic and behavioral well-being of the organism by integrating knowledge from apparently disparate fields of science.
Stress
HPA axis
Immunosuppression
Autonomic system
Depression
Aging
Reproductive suppression
DEFINITION OF STRESS
Growth retardation
was later called by Galen "vis medicatrix Naturae.'" Psychogenic
stress was mentioned by Epicurus, who suggested that coping
with emotional stressors was a way to improve the "quality" of
life (42,65).
In the early nineteenth century, the French physiologist Claude
Bernard introduced a theory suggesting that, as organisms become more independent of their surroundings, they develop
more complex ways of stabilizing their internal environments to
counter the changes in their external environment. The importance of adaptive mechanisms was thus recognized as the constancy of the "milieu interieur,- which would be the condition
of a free and independent existence (18).
In the early 1900's, Walter Cannon expanded this theory and
coined the term "homeostasis." He demonstrated in several
seminal experiments that the sympathoadrenal system was responsible for coordinating the "fight or flight" response necessary to meet external challenges (27). Cannon was able to show
that both physical and emotional disturbances triggered the same
response from the organism. In addition, he proposed that there
was a "critical" level of stress, in terms of magnitude and duration, against which the homeostatic mechanisms fail and the
organism perishes. Cannon believed that an individual organism's susceptibility to this critical stress "varied under different
A critical problem faced by investigators lies in the definition of stress and related concepts (Table 1). The term " s t r e s s "
describes a state of threatened "homeostasis" (Greek for "'steady
state") or threatened harmony, balance, or equilibrium. The
threatening, disturbing forces are defined as "'stressors,'" while
the counteracting forces put forth to neutralize the effects of the
stressors and reestablish homeostasis are called the "'adaptive
response" (42). A major problem in stress biology is confusion
regarding the definitions for " s t r e s s , " "stressor," "'adaptive responses," and "consequences of stress."
Historical Development of Stress as a Concept
The concept of "homeostasis" goes back to the ancient
Greeks (Table 2). The natural philosopher Empedocles considered that all matter was a harmonious mixture of elements and
qualities (42,65). This early expression of homeostasis was extended to living beings by Hippocrates, who considered health
as the state of harmonious balance, and disease as the state of
dysharmony (3). Hippocrates described disturbing forces of nature as causes of disease and referred to the healing forces inherent to the organism as the "healing power of Nature." This
tRequests for reprints should be addressed to Elizabeth O. Johnson, Developmental Endocrinology Branch, National Institute of Child Health and
Human Development, NIH, Bldg. 10, Room 10N262, Bethesda, MD 20892.
115
116
JOHNSON, KAMILARIS, CHROUSOS AND GOLD
Disturbing
Forces
II
Stressors
TABLE 1
TABLE 2
THE CONCEPT OF HOMEOSTASIS
HISTORY OF THE CONCEPT OF STRESS
Harmony
Balance
Equilibrium
Homeostasis
(Steady State)
II
Threatened
Homeostasis
(stress)
~:
,c
Counteracting
Neutralizing
Forces
II
Adaptive
Responses
general conditions and during the normal and pathologic ups and
down of existence in an ordinary life-cycle" (27).
In 1936, Selye presented his concept of the "General Adaptation Syndrome," and attention shifted from the sympathetic
nervous system to the adrenal glands (183). Selye defined four
stages of the stress reaction: 1) an initial "alarm reaction,"
characterized by an immediate sympathoadrenomedullary discharge; 2) a "stage of resistance," characterized by activation
of the hypothalamic-pituitary-adrenal (HPA) axis; 3) a stage of
adrenal hypertrophy, gastrointestinal ulceration, and thymic and
lymphoid shrinkage, which he called the "General Adaptation
Syndrome"; and 4) a final stage of exhaustion and death.
Chronic alterations in the hormonal responses and abnormal
changes in several tissues were believed to cause the "diseases
of adaptation" (184,187).
Hams, a contemporary of Selye's, suggested in 1948 that
hypothalamic releasing or inhibiting factors regulate anterior pituitary function (83). Saffran and Schally demonstrated in 1955
that a factor from the hypothalamus was regulating ACTH release from the pituitary (166). They named this principle "corticotropin-releasing factor." After intensive investigation, in 1981,
Vale and others were able to isolate this factor and characterize
its structure as a 41 amino-acid peptide (207). When the chemical structure was identified, the term "factor" was changed to
"hormone."
Contemporary theory in stress biology conceptualizes an integrated "stress system" consisting of neuroanatomical and functional structures that function to produce the behavioral,
physiological and biochemical changes directed toward maintaining homeostasis (42). This theory is supported by recent findings in neurobiology demonstrating anatomical and functional
connections between the hypothaiamus, the arousal center in the
pons, and several sympathetic nuclei in the hindbrain (26, 141,
209). In the periphery, the adrenocortical and sympathetic divisions of the stress system have additional integrative actions.
These include complementary and permissive interactions of
glucocorticoids and catecholamines in the regulation and maintenance of metabolic and cardiovascular homeostasis (22,157).
Classification of Stressors--The Adaptive Response to Stress
The adaptive response to stress appears to depend upon the
quality (physical or emotional), strength, and duration (acute,
chronic) of the stimulus, as well as upon the constitution and
state of the organism (51). A stressor can be viewed as any perturbation that disrupts homeostasis. Physical stressors include
disturbances of the internal environment (anoxia, hypoglycemia,
etc.), external extremes (heat and cold), and multifaceted stressors (noxious stimuli and physical strain, such as exercise or in-
Empedocles
(500--430 BC)
Hippocrates
(460-375 BC)
Epicurus
(341-270 BC)
Claude Bernard
(1813-1878)
Walter Cannon
(1871-1945)
Hans Seyle
1907-1982)
first written reference to homeostasis.
Health is the state of the harmonious balance of the
elements, and disease is the state of
dysharmony."Nature heals disease" (Noysvn Fyseiw
Iatroi).
Coping with emotional stressors improves the quality
of life.
"Milieu interieur."
"Fight or flight" reaction; "homeostasis."
The "General Adaptation Syndrome."
jury). Psychological stressors are stimuli that affect emotion and
result in fear, anxiety, or frustration, and are among the most
potent activators of the HPA axis (113, 124, 185). It should be
noted that stressors may be mixed and act in combination.
The adaptive response to stress includes the behavioral and
physiological processes that the organism consistently musters in
its attempt to reestablish homeostasis in the face of a wide range
of stressors (183,186). In general, the adaptive response to stress
involves a redirection of both behavior and energy (43) (Table
3). Behavioral adaptation is viewed as the facilitation of adaptive, and inhibition of nonadaptive, neural pathways which enable the organism to cope more successfully with the stressful
stimulus. These behavioral responses include altered cognitive
and sensory thresholds, increased alertness, selective memory
enhancement (27), stress-induced analgesia (204), and suppression of feeding and reproductive behavior (28,191). Peripheral
adaptation is viewed as provision of the energy necessary to
overcome stressors and involves both a shift of energy substrates
from storage sites to the bloodstream, as well as appropriate
cardiovascular changes. Glucocorticoids, epinephrine (E), and
norepinephrine (NE) act to inhibit glucose uptake, fatty acid
storage, and protein synthesis at storage sites and stimulate the
release of energy substrates, including glucose, amino acids, and
free fatty acids, from muscle, fat tissue and liver (133,218).
These changes in energy availability are paralleled by the stimulation of cardiovascular and pulmonary function, which include
increased heart rate, blood pressure and respiration (218). Simultaneously, anabolic processes, such as digestion, growth, reproduction and immune function, are suppressed (105).
It appears that the ability to appropriately regulate the stress
response may be as important as the ability to initiate it. Containment of the stress response is crucial to avoid the behavioral
and physical consequences of the mobilization of behaviors and
resources. Chronic activation of the catabolic processes of the
stress response can ultimately become destructive and pathogenic. Thus metabolic (myopathy, fatigue, changes in glycemia)
and cardiovascular consequences (hypertension), compromised
growth and tissue repair, peptic ulceration, reproductive suppression (impotence and amenorrhea), as well as consequences of
immunosuppression (increased susceptibility to infection and cancer) can occur when the state of stress is unduly prolonged
(105). In addition to elimination of, or habituation to, the stressor, the containment of the stress response is assisted by various
stress-induced substances. Thus, for example, glucocorticoids
and opioids suppress both the HPA axis and the central sympa-
MECHANISMS OF STRESS
117
Psychogenic/
Emotional
Stimuli
TABLE 3
BEHAVIORAL AND PHYSIOLOGICAL ADAPTATION
DURING STRESS
Behavioral Adaptation
Altered cognition and attention span level
Increased alertness
Altered sensory threshold
Sharpened memory and sensation
Stress-induced analgesia
Suppression of feeding behavior
Suppression of reproductive behavior
Peripheral Adaptation
Oxygen and nutrients directed to the CNS and stressed body sites
Detoxification from toxic products
Altered cardiovascular tone
Containment of the stress-response
Traumatic
Stimuli ~
/
Pressure.Sensitive
/ //BaroreceptorSignals
// /
Cytokines/
/ ,/ J
Mediatorsof
ACT_.H ~ / / / n ^
nflammation
( ~ I - 1 3 - E P " "/6 -~.//E
H /~~'-'-''"NE/NPY
~~CRH~
~.,~"~ 5HT
fI
Homeostasis and the Components of the Stress Response
The HPA axis and the sympathetic system are important regulators of an animal's homeostatic functions (205). Thus the organism's response to stress is composed of behavioral, endocrine,
and autonomic components, coordinated to neutralize the disrupting effects of the "stressors" on homeostasis (42, 73, 74).
Below, we describe the mechanisms by which the various components of the stress system restore homeostasis.
MECHANISMS OF THE STRESS RESPONSE
Hypothalamic-Pituitary-Adrenal (HPA) A.ris
The function of the HPA axis has been the subject of intense
basic and clinical research which has attempted to understand
why glucocorticoids are critical for life. The response to stress
is associated with increases in the levels of plasma glucocorticoids. The secretion of glucocorticoids from the adrenal cortex
is under the control of ACTH, which in turn is released from
the anterior lobe of the pituitary. ACTH secretion is regulated
by corticotropin-releasing hormone (CRH) and other secreta-
- / ,,~
I
I
thetic system, while centrally produced norepinephrine inhibits
the sympathetic system via local a2-adrenergic receptor inhibition (203).
Although there is a stereotypic consistency of the responses
that the body activates during stress, all stressors do not result
in identical profiles of behavioral and peripheral responses.
These differences appear to be related to genetic constitution, as
well as to early-life experiences (112, 163,200). Moreover, not
all stressors should be construed as noxious or injurious. Indeed,
many stressors promote essential differentiation, growth, and
enhanced physiological and behavioral competence, which would
be markedly impaired in a relatively stress-free environment. On
the other hand, in the context of constant or inescapable stress,
or in an organism in which the usual counterregulatory elements
of the stress response are relatively inoperative, the effectors of
the generalized stress response could produce secondary changes
that interfere with adaptation, rather than promote it (181, 182,
2 1 3 , 2 1 4 ) . An analogy to this situation of an unrestrained or excessive stress response is that of the spectrum of autoimmune
diseases that occur as a consequence of excessive stimulation of
the immune response or its escape from its usual counterregulatory elements (194-196).
Diurnal
Rhythms
" GABA/BZD
/
/
/
Pituitary
//
\ ~\
ACTH
Glucocorico //
Adrenal
FIG. 1. Schematic representation of the putative regulation of the hypothalamic-pituitary-adrenal (HPA) axis. The corticotropin-releasing hormone (CRH) system is the principal central biologic effector which
facilitates a characteristic behavioral and peripheral response to stress.
CRH stimulates secretion of both hypothalamic and pituitary POMC
gene-derived peptides, the latter resulting in glucocorticoid secretion.
The activation of the CRH neurons appears to be regulated by central
stimulatory and inhibitory inputs and by multiple negative feedback
loops. (Solid lines represent stimulatory effects; broken lines represent
inhibitory effects.) The latter include an ultrashort CRH-mediated loop,
a short hypothalamic POMC gene-derived peptide loop, including both
ACTH and [3-endorphin, and a long glucocorticoid-mediated feedback
loop.
gogues from the hypothalamus (99, 133, 218) (Fig. 1).
Glucocorticoids exert many different effects, including effects
on cardiovascular function, metabolism, muscle function, behavior and the immune system (43). These effects can be grouped
into two categories defined as permissive and regulatory (88).
"Permissive" effects of glucocorticoids function to " p e r m i t "
other hormones or factors to accomplish their function at a normal level, and are observed primarily in the resting state and
may span the resting and stress states. The permissive role of
glucocorticoids is crucial for maintenance of homeostasis at the
basal state (31, 103, 134, 157, 206). "Regulatory" effects of
glucocorticoids are exerted only by stress-induced levels of these
hormones. It has been hypothesized that the regulatory effects
of stress-related elevations of glucocorticoids may be necessary
118
to prevent overreaction of the central stress, immune and other
systems, which, if unchecked, lead to injury (133).
Several closed feedback mechanisms regulate the secretion of
glucocorticoids (99, 133, 218) (Fig. 1). There is a major feedback loop between glucocorticoids and the hypothalamic-pituitary axis. Thus circulating glucocorticoids act on the pituitary
directly to inhibit ACTH secretion, and on the hypothalamus to
suppress secretion of CRH (99). Additional feedback loops include the inhibitory effects of ACTH, [3-endorphin ([3-EP) and
CRH on the hypothalamic CRH neuron (34). These mechanisms
enable the organism to maintain a stable blood level of glucocorticoids at all times, while simultaneously providing an emergency override, via the central nervous system (CNS), to respond
to stressors.
Corticotropin-Releasing Hormone ( CRH)
It has long been recognized that the endocrine response to
stress is coordinated at the CNS. CRH is a 41 amino-acid peptide secreted from the hypothalamus and has a putative role in
regulating the normal response to stress. The chemical isolation
and description of CRH by Vale provided an important missing
link in the system (207). The genes encoding the CRH molecule
in the human, rat and sheep have been characterized (157, 178,
189, 207). These genes have been highly conserved throughout
evolution. In fact, the CRH peptides from humans and rats are
identical in amino acid sequence (157,189). The existence of
CRH has been known since the 1950's, but synthetic CRH only
became available recently; the availability of synthetic CRH has
opened new experimental avenues.
Anatomical distribution. CRH, localized by immunocytochemistry, is found in neuronal cell bodies in the paraventricular
nucleus (PVN) (26,141). CRH neurons project to the median
eminence, where they terminate on the capillaries of the hypophyseal portal vessels. These vessels function as a direct short
vascular pathway from the hypothalamus to the anterior pituitary. Thus CRH, which is released into the hypophyseal portal
system, is transported to the anterior pituitary, where it stimulates pituitary corticotrophs to both synthesize and secrete ACTH.
A different set of PVN CRH neurons send projections to the
hindbrain, where they stimulate the electrical activity of their
target neurons in the arousal and sympathetic centers (208).
There also are extrahypothalamic CRH neurons. Through immunocytochemical, receptor studies and the detection of CRH
mRNA, CRH has been demonstrated in the brainstem, midbrain,
striatum, hippocampus, cerebral cortex, spinal cord, sympathetic
ganglia and adrenal gland (47,199). The broad distribution of
CRH and its receptors in the CNS provides a substrate for the
wide-ranging behavioral effects of this peptide.
Receptors. The CRH receptor is highly concentrated in the
brain, anterior pituitary, adrenal medulla and sympathetic ganglia of the rat and several primates (45,209). CRH receptors in
pituitary corticotrophs appear to be sensitive to circulating levels
of glucocorticoids, as these receptors decrease shortly after adrenalectomy or during chronic stress (6,217). These conditions are
associated with increased hypothalamic CRH and vasopressin
(AVP) secretion, and decreased responsiveness to physiologic
increases in plasma glucocorticoids, respectively.
Regulation. CRH secretion can be affected by stimuli such
as emotion, pain and changes in blood pressure. The PVN has
connections with various components of the limbic system, implicated in emotions, such as fear, and anger. Pain pathways are
believed to be primarily located in the spinothalamic tracts which
project via the reticular formation of the brainstem to the PVN.
Changes in blood pressure also affect CRH release. Blood pres-
J O H N S O N , KAMILARIS, CHROUSOS A N D GOLD
sure is regulated by receptors in the carotid sinus, the aortic
arch, major chest veins, and both atria. When blood pressure
increases, impulses originating from these receptors travel to the
nucleus of the tractus solitarius in the medulla and then to the
PVN, where CRH secretion is inhibited. Conversely, CRH secretion is increased when blood pressure decreases. The latter
has been associated with a decrease in the number of impulses
reaching the PVN via the nucleus tractus solitarius (63).
Several neurotransmitter systems regulate PVN CRH release
(Fig. 1). Both NE and E stimulate CRH release. It appears that
the former stimulates CRH release via the a~-adrenergic receptor
(35). Acetylcholine and serotonin are also excitatory mediators
participating in both the circadian rhythm and stress-induced release of CRH, whereas gamma-aminobutyric acid (GABA), the
opioid peptide system, ACTH, and glucocorticoids are inhibitory
(35). Several products of the immune system such as several cytokines, including Interleukin-1 (IL-I), Interleukin-2 (IL-2), Interleukin-6 (IL-6), or inflammatory mediators, such as platelet
activating factor (PAF) and tumor necrosis factor (TNF) appear
to stimulate secretion of hypothalamic CRH in vitro and in vivo
(19, 194, 216).
Behavioral effects. The distribution of CRH within and beyond the hypothalamus provides an anatomical context for the
observation that CRH can simultaneously activate and coordinate
metabolic, circulatory and behavioral responses during adaptive
situations (59, 64, 202). CRH injected directly into the cerebroventricular system produces a number of effects that are reminiscent of the stress response (28,29). These include neuronal
activation, electroencephalographic arousal, and pronounced general behavioral activation. Behavioral changes are dependent on
the situation and dose (102). For example, when CRH is injected
ICV in rats, it produces dose-dependent locomotor activation in
familiar environments and the "'freeze" posture in foreign environments (202). At low doses, CRH-induced activation is characterized by increased locomotion, sniffing, grooming and rearing.
These changes are believed to be consistent with "'general behavioral arousal." High doses of CRH, on the other hand, produce bizarre behaviors, including repetitive locomotion, irritability,
or demonstrations of aggression (102). High doses of CRH ICV
have been shown to decrease sexual behaviors (191). Finally,
CRH decreascs food intake in the home cage and inhibits increases in food intake produced by NE and insulin, implicating
CRH as a mediator of stress-related suppression of appetite or
food intake (132).
ACTH and Endorphins
Anatomical distribution. Proopiomelanocortin (POMC) is the
prohormone for ACTH (122). POMC is synthesized in the brain
(arcuate nucleus of the hypothalamus, zona incerta, lateral septum, nucleus accumbens, periventricular thalamus, periaqueductal gray, locus coeruleus, nucleus tractus solitarius, reticular
formation, stria terminalis and medial amygdala), pituitary gland,
gastrointestinal tract and reproductive organs, and is cleaved into
different biologically active peptides (79, 84, 106, 137, 176). In
the anterior pituitary, POMC is broken down into ACTH, a 39
amino-acid fragment, and 13-1ipotropin, a 92 amino-acid fragment; in turn, 13-1ipoprotein is broken further into other smaller
active fragments, including [3-endorphin (Fig. 2). The particular
POMC fragments produced in a given tissue or cell type are believed to be specific and determined by local enzymes and pH.
ACTH is transported via the systemic circulation to the adrenal gland, where it stimulates synthesis and secretion of glucocorticoids, aldosterone and adrenal androgens. ACTH also has a
trophic or sensitizing effect on the adrenal cortex, enhancing the
M E C H A N I S M S OF STRESS
NH2
119
13-MSH
COOH
ACTH
(1-391
11-131 CLIP
~LPH
118-391
I'-LPH
~-MSH
11-5111
137-S8)
11-gl)
l~-Enclorphln
161-gl1
reduces exploration in a novel environment without influencing
locomotion (57). The increased activity produced by ACTH is
about 100 times less potent than the changes produced by CRH.
y-Endorphln (81-77 I
I
Enl(ephlllln 161-115)
FIG. 2. Schematic representation of proopiomelanocortin (POMC), the
large molecular weight precursor of ACTH, 13-1ipotropic hormone (13LPH), and [3-endorphin. CLIP represents corticotropin-like intermediate
lobe peptide, et-MSH, 13-MSH, and a- and [3-melanocyte-stimulating
hormones, respectively.
response to subsequent stimulation. Thus, if an animal is exposed to regular, fixed doses of ACTH, the glucocorticoid response to the dose increases over time, primarily as a result of
adrenocortical hypertrophy. The same occurs during chronic
stress. Conversely, if ACTH secretion is decreased or eliminated, the glucocorticoid response to ACTH is reduced, most
probably as a result of adrenal atrophy. Interestingly, ACTH
may also have neurotrophic effects. For example, ACTH can facilitate recovery after a sciatic nerve crush (51,63).
Receptors. The ACTH receptor follows a pattern of receptor
regulation and homeostasis similar to that observed in most endocrine systems. When ACTH concentrations are high, receptors are desensitized and are downregulated or disappear.
Conversely, when ACTH concentrations are low, the number or
sensitivity of the receptors increases. Although the ACTH receptor system appears to follow a normal pattern, the glucocorticoid response to ACTH does not. Rather, elevations in ACTH
result in elevations in glucocorticoid secretion. Thus it appears
that the glucocorticoid responsivity to ACTH may be regulated
at the postreceptor level (109).
Regulation. CRH is the most potent stimulator of ACTH/13endorphin secretion from the anterior pituitary corticotrophs.
ACTH response to stress, however, is partially regulated by
peptides other than CRH. These include arginine vasopressin
(AVP), oxytocin (OT), angiotensin II, vasoactive intestinal polypeptide (VIP), serotonin, and, in the rat, E and NE (8, 148,
157). The physiologic role of these peptides in the regulation of
ACTH secretion is still not clear. AVP secreted by parvocellular
regions of the PVN into the hypophyseal portal circulation stimulates ACTH release synergistically with CRH (177). Glucocorticoids inhibit stimulated ACTH secretion both in vivo and in
vitro (99). The inhibitory effects in vivo exerted at least at two
levels, via inhibition of the secretion of hypothalamic CRH and
direct suppression of ACTH release at the pituitary level (34).
Behavior. ACTH, along with vasopressin, is believed to enhance attention, motivation, learning and memory retention (50,5 i).
It appears that only a small part of the ACTH molecule, amino
acids 4-7 of the N terminal, is needed to produce these effects
(50). Besides these positive effects, ACTH also acts as an opiate antagonist, and competes with opiate-binding sites in the
brain. Thus ACTH can counteract morphine analgesia and reverse catatonic posture (immobility). ACTH administered ICV
also appears to affect social behavior in the rat by reducing social interaction and decreasing aggression. Novel or stressful
stimuli induce grooming, which has been related to the endogenous release of ACTH (69).
The behavioral response to ICV ACTH is characterized by
the "stretching yawning syndrome," in which rats display excessive grooming behavior interrupted by bouts of stretching. In
contrast to CRH, ACTH given ICV does not appear to increase
activity or exploration (58,89). When injected peripherally, ACTH
Glucocorticoids
The adrenal gland consists of at least two anatomically and
chemically distinct structures: an inner medullary area containing catecholamine-producing chromaffin cells and an outer cortical region in which glucocorticoids and other steroids are
synthesized. Glucocorticoids are released from the adrenal gland
into the general circulation. A high proportion, almost 95%, of
circulating cortisol circulates bound to an alpha globulin called
"transcortin" or "corticosteroid-binding globulin" (CBG). The
bound fraction of cortisol is considered physiologically inactive.
The small free-fraction of cortisol in plasma represents the active fraction of the hormone which exerts negative feedback effects on CRH and ACTH release (190).
Receptors. Glucocorticoid receptors are present throughout
the brain, including in the CRH neurons of the hypothalamus
(62). The actions of glucocorticoids on the central nervous system (CNS) are mediated by two separate receptor systems: glucocorticoid receptors type I and type II (155,173). Type I
("corticosterone receptors") receptors are found mainly in the
neurons of the limbic structures, such as the hippocampus and
septum (120). These receptors play a role in modulating the response to environmental and emotional stimuli, with consequent
changes in behavior and HPA axis activity. Type I receptors
have a high affinity for the primary glucocorticoid (cortisol/corticosterone), and are similar to "mineralocorticoid receptors" of
the kidney (155,173). In the limbic system, these receptors have
a high specificity for corticosterone as an agonist, whereas the
mineralocorticoid aldosterone appears to be a competitive antagonist. The Type I receptors that are found in the circumventricular organs function as mineralocorticoid receptors that respond
to aldosterone and act to regulate sodium homeostasis, cardiovascular control and salt appetite (173). With age, the hippocampus loses approximately 50 percent of its glucocorticoid type
I binding sites (172). ACTH appears to have atrophic effect on
the CNS and reverses age-related decreases in type I receptor
(156).
Type II glucocorticoid receptors are present at high concentrations in the hypothalamus, particularly in the CRH neurons.
Type II receptors also are found in the brain areas that contain
POMC, such as the hippocampus, lateral septum, amygdala, and
nucleus tractus solitarius (120). At these sites, it is likely that
the receptors participate in the behavioral, neuroendocrine and
autonomic responses to stress (173). During stress, the occupancy of type I receptor changes only minimally, whereas that
of type II receptor changes considerably (155). Glucocorticoids
exert negative feedback to terminate ACTH release in response
to stress and have long-term effects on adaptive behaviors, presumably via the type II receptors. Type II receptors diminish
with age, but are not affected by ACTH per se (156, 171-173).
Reduction of type II receptors is associated with decreases of
the negative feedback action of glucocorticoids, which may result in a more persistent elevation of circulating plasma corticosteroid levels following stress (167, 169, 171-173). In addition,
persistent elevations of circulating glucocorticoids render the
neurons of the hippocampus vulnerable to toxic influences with
consequent degeneration and death of the cells (i 10, 169-173).
Behavior. Glucocorticoids have two types of action in the
CNS. The first is associated with perception and the coordination of the circadian patterns of food intake and sleep. The second is a negative feedback effect on stress-activated neural
120
JOHNSON, KAMILARIS, CHROUSOS AND GOLD
circuits and metabolic processes. Interestingly, the acute effects
of glucocorticoids are euphorogenic, whereas chronically elevated glucocorticoids produce depression in a large number of
subjects (27).
NE
Autonomic System
As previously mentioned, the two principal components of
the general adaptational response are the CRH and the locus
ceruleus-norepinephrine, (LC-NE)/autonomic (sympathetic) nervous systems (71,72) (Fig. 3). The LC-NE/sympathetic systems
are located in the brainstem (136). Activation of the LC-NE
system leads to release of norepinephrine from a dense network
of neurons throughout the brain that results in arousal, vigilance
and increased anxiety. It has been generally accepted that the
sympathetic division of the autonomic system is primarily associated with conferring an adaptive advantage during stressful situations via its effectors, the sympathetic nerves and the adrenal
medulla, located in the periphery. On the other hand, the parasympathetic division of the autonomic nervous system, which is
functionally linked to the sympathetic system, appears to produce effects antithetical to those of the sympathetic nervous system. Thus its inhibition can produce effects analogous to those
of sympathetic activation.
Cannon (37) was the first to note that a variety of stressors
resulted in an increase in sympathetic nervous system activity
and adrenal medulla output. During stress, E and NE are released into the general circulation and the activity of enzymes
that regulate catecholamines biosynthesis is stimulated. Today,
it is generally accepted that the general sympathetic and sympathomedullary systems are critical elements in the integrated
physiological response of an organism to a variety of stressors
(8, 111, 118, 124). Central regulation of this response involves
components of the central stress system in the cerebral cortex,
limbic system, hypothalamus, and brainstem (60).
Acute stress results in secretion of E and NE from the adrenal medulla and release of NE from the sympathetic nerve terminals (205). In contrast, chronic intermittent stress is associated
with changes in the adrenal medulla, including increased activity of enzymes involved in catecholamine biosynthesis, increased
rates of catecholamine synthesis and elevated tissue concentrations of catecholamines (108). Chronic intermittent stressors initially appear to affect catecholamine release during subsequent
exposures, as a function of the familiarity of the stressor (101).
Thus exposure to homotypic (familiar) stressors in a chronic intermittent fashion results in a reduced sympathetic, sympathomedullary response with time. In contrast, following chronic
intermittent stress, exposure to an acute heterotypic (novel)
stressor results in an enhanced sympathetic, sympathomedullary
response (119,197).
There is growing body of studies that demonstrate that animals subjected to inescapable, uncontrollable electric shocks
show subsequent deficits in learning to terminate the noxious
stimulus even when it is escapable. This phenomenon has been
termed "learned helplessness," suggesting that the inability of
the individual to control or terminate the stressor results from
the initial learning of inescapability (181, 182, 213, 214). Experimentally induced behavioral deficits of this type have been
seen as a model of depression. Such a "learning deficit" was
considered analogous to some of the mood/cognitive disturbances observed in patients with depression, who frequently report feelings of helplessness or powerlessness to cope with
stress. The weight of the available evidence suggests one mechanism underlying the behavioral deficits observed in animals exposed to inescapable stress is a depletion of norepinephrine
\\\ ii
ss
\ I
(~ituitary~ <
/'
\ ~
"
E/NE
\\1IW
ACTH/
G,oc/o
iooi,s
Adrenal
FIG. 3. Schematic diagram of the functional interrelations between corticotropin-releasing hormone (CRH) and locus ceruleus-norepinephrine
(LC-NE) systems. These systems are the principal central biologic effectors of the generalized stress response. In the periphery, both systems
act through glucocorticoids secreted from the adrenal cortex and the catecholamines, epinephrine and norepinephrine (E, NE) from the sympathetic and sympathomedullary systems (SS). Glucocorticoids are thought
to restrain both systems of the stress response, in order to prevent the
consequences of prolonged or excessive activation. (Solid lines represent
stimulatory effects; broken lines represent inhibitory effects.)
and/or a decrease in tyrosine hydroxylase activity (213,214).
The stress system also interacts with other CNS elements that
play a role in information processing, action initiation, as well
as setting the emotional tone. The mesocortical dopamine system which innervates the prefrontal cortex, a brain region believed to be involved in anticipatory phenomena and cognitive
function, is activated by the LC-NE/sympathetic systems during
stress. In addition, the mesolimbic dopamine system, a region
closely linked to the nucleus accumbens, which has been implicated in motivational/reinforcement/reward phenomena, is also
stimulated by the LC-NE/sympathetic systems during stress (48,
49, 136, 164). Noradrenergic neurons which originate in the
brainstem LC-NE/sympathetic system activate the amygdala/hippocampus complex during stress (75).
Finally, the LC-NE/sympathetic systems seem to respond
similarly to the CRH system to many of the same neurochemical modulators. Serotonin and acetylcholine appear to be excitatory to the sympathetic system (5, 9, 12, 36, 61, 80), while the
gabaergic (9,61) and the opioid peptidergic (9, 23, 34, 80) neurotransmissions act to inhibit the LC-NE/sympathetic systems. In
addition, the LC-NE/sympathetic systems seem to respond to
autoregulation by an alpha-2 adrenergic-mediated inhibition.
CONSEQUENCESOF STRESSON "'WELL-BEING":
THE INTERACTIONWITH OTHERPHYSIOLOGICSYSTEMS
The systems responsible for reproduction, growth and immunity are directly linked to the stress system, and each is pro-
M E C H A N I S M S OF STRESS
121
foundly influenced by the effectors of the stress response. Chronic
stress can have physiological and behavioral consequences which
affect the well-being of an individual. These include accelerated
aging, reproductive suppression, retardation of growth, and immunosuppression. In addition, some common psychiatric disorders, such as depression, panic anxiety and anorexia nervosa,
may represent dysregulation of the systems responding to stress.
Stress and Aging
There is general support for the notion that chronic stress can
accelerate aging (145) and that an aged animal has impaired
ability to terminate the stress response (171). It has been suggested that cortisol hypersecretion in aged animals is due to degenerative changes within the aging brain and loss of sensitivity
to glucocorticoid-mediated feedback inhibition. These effects are
seen specifically in the hippocampal region of the limbic system, which has been associated with inhibition of the HPA axis
(173). With age, the hippocampus loses approximately 50 percent of type I ("mineralocorticoid receptors") binding sites, as
well as some of the type II ("glucocorticoid receptors") sites
(172,173). In addition, the aged hippocampus demonstrates loss
of neurons (174). It appears that cumulative exposure to increased glucocorticoid concentrations over the lifespan might
mediate hippocampal neuron death (110). Chronic stress or
pharmacologic doses of glucocorticoid treatment accelerate this
process (170, 173, 174). This effect appears to be specific for
the hippocampus, since other areas of the brain are spared (170).
Some of the damaging effects of glucocorticoids appear to be
mediated by type II glucocorticoid receptors. Hence, RU 486, a
type II receptor antagonist, attenuates these toxic effects of glucocorticoids on the hippocampus (173).
Early neonatal experience may play a role in shaping individual patterns of stress susceptibility in later life. Meany et al.
(125,126) have demonstrated that neonatal handling of rats increases hippocampal glucocordcoid receptor levels. This is concordant with their ability to shut off the pituitary-adrenal response
to stress. One could postulate that this enhanced capability to
terminate the secretion of adrenocortical stress hormones may
attenuate the glucocorticoid-dependent degenerative changes in
regions of the brain that participate in the restraint of the stress
response, particularly the hippocampus (174).
Suppression of Reproductive Function
The state of threatened homeostasis produced by physical or
emotional stress has long been recognized as a profound disruptive factor in reproductive function. Females under stress may
demonstrate delayed puberty, lack of behavioral receptivity,
failure of ovulation or embryo implantation, spontaneous abortion, or increased infant mortality (4, 10, 30, 117). Males may
exhibit suppression of testosterone secretion, spermatogenesis
and libido (2, 44, 152, 173). The severe suppression of reproduction during stress appears to be caused by several hormones
secreted during stress (such as CRH, ACTH, beta-endorphin and
glucocorticoids) on hypothalamic-pituitary-gonadal (HPG) axis
function (54, 81, 158, 161, 191, 211). Although the mechanism(s) of these effects on reproductive function are not fully
elucidated, possible sites involved include: 1) a centrally mediated inhibition of gonadotropin-releasing hormone (GnRH) release by CRH, opioids and glucocorticoids (158,161); 2) a
glucocorticoid-mediated decrease in pituitary responsiveness to
GnRH, resulting in decreased luteinizing hormone (LH) secretion (81); 3) direct gonadal effects of glucocorticoids with subsequent alterations in sex steroid output (13,39); and 4)
/;G}
/
ACTH
LH,FSH
nal ~~'Gonad
Target
Tissues
FIG. 4. Schematic representation of the functional interrelations between
the hypothalamic-pituitary-adrenal (HPA) and hypothalamic-pituitary-gonadal (HPG) axes. CRH activates the pituitary-adrenal axis and GnRH
the pituitary-gonadal axis, respectively. The activity of the GnRHsecreting neurons during stress is inhibited by CRH directly or via hypothalamic (arcuate nucleus) [3-endorphin(~-EP). Glucocorticoids suppress
the activity of the reproductive axis at all levels, including the hypothalamus, pituitary, gonads and target tissues of sex steroids. (Solid lines
represent stimulatory effects; broken lines represent inhibitory effects.)
glucocorticoid-induced sex steroid target tissue resistance to gonadal sex steroid (153) (Fig. 4).
Stress-induced decreases in circulating LH and sex steroid
levels have been observed in both males and female rats and
monkeys (24, 55, 139, 140). Abbott (1) demonstrated that, in
marmosets, socially mediated suppression of reproduction is associated with a significant reduction in LH release, resulting in
decreased sexual behaviors in males and lack of behavioral receptiveness and complete ovarian inactivity in females. Similarly, O'Byme (139) showed that a summation of the stressful
effects of aggressive encounters and physical restraint produced
a suppression of LH secretion during estradiol-induced LH surges
in female marmosets. Although the site of action of socially induced inhibition of LH release was not addressed in this study,
the fact that exogenous GnRH administration reversed the LHdecrease in these animals supports the hypothesis that a centrally
mediated inhibition of GnRH secretion by hormones secreted
during stress could be related with the decrease of LH secretion
(1, 139, 140).
Previous studies have shown that disruptive effects of stress
on reproductive function in female animals and women may be
dependent on decreased gonadotropin secretion induced by elevated endogenous CRH and opioid levels (14, 66, 68, 138, 146,
161). From these studies, it appears that the most probable
mechanism for reproductive inhibition involves CRH released
during stress and acting within the brain to inhibit gonadotropin
122
secretion, directly and/or indirectly through opioids (13-endorphin) (Fig. 3). This hypothesis is supported by several animal
studies in which ICV administration of either CRH neutralizing
antibodies or a specific CRH antagonist prevented CRH-induced
suppression of the HPG axis (146). Recent observations in the
rat have shown that the inhibitory effect of CRH on LH secretion is blocked by anti-13-endorphin serum and by a 13-endorphin
antagonist, Blockage of [3-endorphin m and e receptors and
dynorphin k-receptors reverses footshock-induced decreases in
plasma LH levels, suggesting that multiple endogenous opiate
systems participate in stress-induced inhibition of reproduction
(146). The existence of a putative CRH-opioid interaction is
supported by the ability of nalaxone to reverse the CRH-induced
decrease in plasma LH levels in monkeys (68). Studies in amenorrheic anorexic patients showed that decreases in gonadotropin
secretion were associated with increased CRH and [3-endorphin
concentrations in the CSF (71, 86, 97, 98).
Another mechanism by which activation of the HPA axis may
influence reproductive function during stress is by direct effect
of glucocorticoids at multiple levels of the HPG axis. Glucocorticoids suppress GnRH and gonadotropin secretion at both the
hypothalamic and pituitary levels (11,96). At the gonadal level,
glucocorticoids have a direct inhibitory effect on testicular Leydig cell function. Leydig cell sensitivity to LH and hCG is decreased by glucocorticoids, probably due to glucocorticoidinduced reductions in testicular LH receptors (13,39). In cycling
females, glucocorticoid treatment decreased estradiol concentrations and caused resistance of the uterus to estradiol. The latter
has been associated with decreased estradiol receptors in the
uterus (153). Stress cannot only influence the ability of the female to conceive, but also can adversely affect the fecundity of
each conception. In rodents, stress during pregnancy has been
shown to result in smaller litter sizes (149,150). In sheep, there
also is evidence that stress and hypercortisolism are associated
with increased embryo loss following implantation and may precipitate premature labor (16, 87, 114).
Growth Retardation
In humans, linear growth and final adult stature depend on
multiple factors. These include genetic constitution (154), nutrition (I 15), systemic disease (32,78), hormones (90) and psychosocial environment (151). A putative association between stressful
psychosocial environment and subsequent physical stature, intellectual and behavioral development has been described (I 29,130).
Psychosocial dwarfism, known also as abuse dwarfism, is a
human condition thought to result from disruptions of social relationships in the neonatal environment; believed to be of particular importance is the withdrawal of normal " c a r e " by the
caregiver, which may act as an emotional stressor (151). This
syndrome is characterized by three primary reversible impairments: 1) delayed physical maturation, defined by both lower
than normal body weight and height and delayed onset of puberty; 2) retardation of intellectual age, indicated by regressive
or bizarre behaviors and retarded psychomotor development; and
3) delayed social maturation and slow psychosexual development
(7,77).
Studies of the biochemical basis of growth abnormalities in
children with psychosocial dwarfism have indicated that a "functional" growth hormone (GH) deficiency exists, which normalizes rapidly with improved psychosocial environment (76,77).
Fasting plasma GH levels and GH response to insulin-induced
hypoglycemia are abnormally low in these children (77), and
IGF-I levels are in the range characteristically found in hypopituitarism (46). Although abnormalities in thyroid and adrenal
JOHNSON, KAMILARIS, CHROUSOS AND GOLD
/I
~IV
I
I I
it,
/\,, \
iI
\\
\\\
.<...I
Adrenal ',.
/ ~
Somatomedm i
Targel
Tissues
FIG. 5. Diagrammatic outline of the putative functional interrelations
between the HPA axis and hypothalamic-pituitary-growth axis. Growth
hormone (GH) secretion is under dual hypothalamic control of growth
hormone-releasing hormone (GRH), which is stimulatory, and somatostatin, which is inhibitory. The activity of GRH neurons during stress
appears to inhibited by CRH directly and/or via hypothalamic [3-endorphin (13-EP) and somatostatin. GH exerts peripheral growth-promoting
actions directly by stimulating peripheral somatomedin-C (IGF-I) production. Somatomedin-C appears to participate in a negative feedback
regulation of GH secretion at both the pituitary and the hypothalamus.
During chronic stress or hypercortisolemic states, glucocorticoids appear
to suppress spontaneous secretion of GH at the pituitary level and probably at the hypothalamus. In addition, glucocorticoids induce major tissue resistance to somatomedin-C and other growth factors. (Solid lines
represent stimulatory effects; broken lines represent inhibitory effects.)
axis function have been reported in a few studies, they are not
typical (106).
It is a commonly hypothesized view is that glucocorticoids
and/or opioids secreted in response to chronic stress inhibit pituitary GH release at the pituitary level and decrease target tissue
sensitivity to growth hormone, somatomedin-C or other growth
factors (Fig. 5). The recent observation that the central administration of CRH decreases GH secretion in rats suggests a possible role of endogenous CRH in the modulation of GH secretion
during stress (142,159). Studies of the possible mechanisms involved in this effect suggest a central site of action, since specific CRH antagonist administration abolished the inhibitory
effect of a noxious stimuli on GH secretion (160). Additionally,
the available data suggests that release of 13-endorphin and/or
somatostatin by CRH may represent important mediators of this
effect (15,160).
Studies in laboratory animals and humans have shown that
disruption of the infant-caregiver relationship, as in maternal
deprivation, rejection, or abuse, contributes to marked physiological and behavioral abnormalities in the offspring. For instance, it may impair overall skeletal growth and the ease with
which social bonds are formed later in development (56,179).
The mechanism(s) that mediate the linkage between early care
M E C H A N I S M S O F STRESS
123
or emotional state and the physical and behavioral manifestations
during development are not clear.
In many species, physical contact and touch between young
animals and their caregivers appears to be necessary for normal
somatic growth (56,179). In humans, the etiology of psychosocial growth retardation has been related to unsatisfactory mother-infant relationships, often measured in terms of physical contact
(76,77). In nonhuman primates, when physical contact is restrained, even if visual, auditory and olfactory cues are mainmined, the behavioral development of the animal remains abnormal
(82). Rat pups that are separated from their mother or placed
with an anesthetized dam demonstrate decreases in tissue omithine decarboxylase activity and GH secretion and reduced tissue sensitivity to exogenous GH (179,180). These deficiencies
could be reversed with tactile stimulation (179).
Alterations in bnmunocompetence During Stress
The principal effectors of the stress response exert multiple,
complex effects on the immunologic apparatus. Conversely,
many humeral components of the immune response exert effects
on the central and peripheral components of the generalized
stress response (25,212l (Fig. 6l. These interactions are sufficiently complex, as well as dose- and context-dependent, that
no single statement can simply summarize these interactions, We
shall try, therefore, to summarize only a few principles that have
been generally established regarding alterations in immunocompetence during stress.
Among the effectors of the stress response, the hypothalamic-pituitary-adrenal axis seems to be the most influential. The
HPA axis can influence immunologic function through a variety
of mechanisms, including CRH-mediated actions on the release
of somatostatin, with subsequent inhibition of growth hormone,
CRH-mediated release of ACTH and beta-endorphin, and CRHmediated pituitary-adrenal activation (25, 210, 212). Perhaps the
best understood and most widely studied immunologic effects of
the HPA axis are those mediated by glucocorticoids (17,133).
At plasma levels generally achieved during either emotional or
physical stress, including the stress of physical injury or inflammation, glucocorticoids generally exert immunosuppressive and
antiinflammatory effects (17, 33, 133). These include inhibition
of leukocyte traffic, interference with cell-mediated immunity,
and enhancement of suppressor T-cell function (22, 67, 85, 123,
131, 133, 134). Moreover, there is a systematic decrease in the
production of cytokines and interference with their functional effects, as well as the induction of lymphopenia, thymic involution, and loss of splenic and lymph node tissue mass (17, 123,
131 ). It should be noted that, in some instances, glucocorticoids
enhance certain components of the immune response, including
the function of specific differentiated clones of lymphocytes
(194).
The CRH neuron of the HPA axis has recently been shown
to participate in a negative feedback loop, producing pituitaryadrenal activation and concomitant glucocorticoid-mediated immunosuppression in response to peripheral mediators of the
inflammatory response, such as IFN, IL-I, IL-2, and PAF. This
negative feedback loop is thought to appropriately restrain the
immune and inflammatory response so that it will not overshoot
in response to immune triggers (25, 133, 212). Interruption of
this feedback loop by the administration of glucocorticoid antagonists or an endogenous deficiency in the responsiveness of the
CRH neuron to a variety of immune mediators results in susceptibility to inflammatory disease. Hence, Sternberg et al. have
shown that the susceptibility of the LEW/N rat to a variety of
inflammatory diseases reflects a deficient responsiveness of the
CRH
~~_
P~ituitar~y~
"',.k,,.j/
CYet~ikitnes]
f
~ammation
ACTH
GlucocorticoidsJ
Adrenal
FIG. 6. A putaiive bidirectional regulatory feedback loop exists between
the immune system and the CRH system. Cytokines and inflammatory
mediators stimulate the HPA axis primarily by causing secretion of
CRH. The HPA axis, in turn, inhibits the immune/inflammatory response primarily via increases in glucocorticoid secretion. This glucocorticoid-mediated immunosuppression could prevent excessive
inflammatory/immune responses during acute stress. (Solid lines represent stimulatory effects; broken lines represent inhibitory effects.)
CRH neuron to a variety of stimuli, including cytokines (195,196).
Conversely, histocompatible F/344N rats are resistant to inflammatory disease because of a hyperresponsiveness of their CRH
neurons to inflammatory mediators, but show the susceptibility
of LEW/N rats to a variety of immunogenic stimuli if given
small doses of the glucocorticoid antagonist RU 486 (195,196).
CRH has been shown not only to be essential for the activation of the pituitary-adrenal axis, but also to possess a variety of
behavioral effects when given ICV. Specifically, the central administration of CRH not only activates the pituitary-adrenal axis,
but also sets into motion a variety of other physiological and
behavioral responses that are adaptive during stressful situations.
These include activation of the sympathetic nervous system, enhancement of pathways mediating cautious avoidance and anxiety, and inhibition of pathways subserving vegetative functions
such as feeding and reproduction. Although not yet definitively
demonstrated, the response of the CRH neuron to the humeral
mediators of immunity such as IL-I and PAF could not only
serve to restrain the immune response to prevent it from overshooting, but could also promote behavioral adaption of value
during the stress of injury (17, 19, 25, 133, 194, 212, 216). As
an example, IL-l-mediated CRH release, leading to cautious restraint and increased anxiety, could serve to protect an animal
from exposing itself to further injury during the stress of illness
of prior injury. Such a dual role of a central element such as the
CRH neuron would bring the discipline of neuroimmunology full
circle by showing that the CNS could respond to peripherally
mediated inflammatory signals by modulating both the immunologic and behavioral response of the organ to increase the likelihood of survival.
124
It has been suggested that patients with major depression
show immunosuppression as a consequence of the hypercortisolism frequently associated with this disorder (33). However. the
data have been conflicting. Although we cannot definitively account for the discrepancies, they could reflect the fact that glucocorticoids are not always immunosuppressive, but may enhance
certain components of the immune response (17,25). A second
possibility is that not all depressive syndromes are associated
with hypercortisolism (73,74). Indeed, the weight of available
data suggests that, while the hyperaroused state of melancholia
is frequently associated with hypercortisolism, the hyperphagia
and hypersomnia of certain "atypical" depressions may be associated with a subtle central adrenal insufficiency, and hence
enhancement of certain immunologic responses. In this regard,
our group has recently noted that the atypical depression often
associated with the chronic fatigue syndrome, hypothyroidism,
and seasonal affective disorder may be associated with a subtle
deficiency in the responsiveness of the CRH neuron in association with subtle adrenal insufficiency.
In addition to the CRH system, the LC-NE system is thought
to be the other major effector of the generalized stress response.
CRH is itself thought to be a potent stimulus to the LC-NE system, although many neurotransmitters participate in the regulation and counterregulation of this important stress responsive
system. NE is thought to have a variety of effects on the immunologic response, acting both as a blood-borne humeral mediator and locally (194). As an example, the spleen and lymph
nodes are replete with noradrenergic terminals and adrenergic
receptors that modulate the functional activity of these lymphoid
organs.
Psychiatric Disorders
It has been proposed that a critical factor in the pathophysiology of several psychiatric syndromes, such as major depression, anorexia nervosa and panic anxiety, stems from an
abnormality in the counterregulation of the generalized stress response, resulting in CRH and/or central catecholamine hypersecretion (192). In particular, it has been hypothesized that
abnormalities in the positive regulation of or defects in counterregulation of the central components of the adrenocortical and
adrenergic system are responsible for these disorders (73,74).
The association between stress and depression stem from
several observations: 1) individuals who are depression-prone
have a higher than expected incidence of early noxious stress or
maternal deprivation; 2) depressive episodes are often associated
with major life changes (73,74); 3) acute stress-induced hormonal and behavioral changes closely resemble the symptom
complex of depression (71); and 4) hypercortisolism is a consistent feature of the classic form of major depression, melancholia
(165).
The symptom complex of melancholia indicates that depression need not be a state of pathological inactivation or suppression, as the term depression implies, but rather a state of
pathological hyperarousal (73,74). Indeed, from a clinical perspective, one can construe melancholia as an organized state of
anxiety attached principally to the self, resulting in a profound
sense of worthlessness and hopelessness about the future, prospects of the worthless self. This anxiety about self and the future are associated with other signs of hyperarousal or activation
of the generalized stress response that include enhanced vigilance, as well as inhibition of vegetative functions such as feeding, growth, reproduction, and sleep (73,74). Our group has
advanced several lines of evidence suggesting that CRH may
play a role in the clinical and biochemical manifestations of
melancholia (40, 41, 70-74, 101L As an example, we have
JOHNSON, KAMILARIS, CHROUSOS AND GOLD
shown that the plasma ACTH responses to exogenous CRH are
blunted in melancholia and correlate negatively with the basal
glucocorticoid levels. These data indicate that the pituitary corticotroph cell in major depression is appropriately restrained by
high circulating glucocorticoids, and that hypercortisolism in
major depression reflects a defect at or above the hypothalamus
resulting in the hypersecretion of endogenous CRH (73,74). We
also showed that a continuous infusion of CRH to volunteers reproduces the pattern and magnitude of hypercortisolism seen in
major depression, while postdexamethasone cortisol levels in
patients with major depression correlate positively with CSF
CRH levels (73,74). Recently, we have advanced preliminary
data that, in CSF sampled continuously for 30 hours, the levels
of CRH measured hourly are consistently higher in depressed
patients compared to controls (101).
This evidence of activation of one of the principal effectors
of the stress response in major depression is also associated with
evidence that the other major effector of the stress response, the
LC-NE system, is also activated in melancholia. Hence, patients
with melancholia show elevated levels of NE in CSF and plasma.
while successful responses to antidepressant treatment, regardless of the class, is associated with a significant fall in the
plasma and CSF levels of the principal NE metabolite, MHPG
(70-74, 101L In addition, tricyclic antidepressants which are the
most effective agents in the treatment of melancholia reduce the
LC firing rate, while we have recently shown that chronic but
not acute imipramine treatment causes a significant decrease in
the expression of TH mRNA in the LC. Taken together, these
data suggest that the clinical and biochemical manifestations of
major depression represent an activation of the major effectors
of the generalized stress response that have escaped their usual
counterregulatory elements to become pathologically established
as a syndrome of sustained hyperarousal and organized anxiety.
The principal animal models of major depression support
such a conclusion. These include the model of inescapable shock
or learned helplessness, analogous to the clinical context in
which many major depressions develop, namely sustained helplessness or a burden of internal conflict or external stress that is
inescapable (181, 182, 213, 214). Investigators such as Weiss
have shown that inescapable shock produces a syndrome in the
rat that is very analogous to that of melancholia, consisting of
early moming awakening, anorexia, decreased libido and hypothalamic hypogonadism, shortened REM latency, and a behavioral phenotype compatible with the organism's being overwhelmed
by stress (213,214). This syndrome responds to the classic treatments for melancholia, including tricyclic antidepressants and
electroconvulsant treatment. It appears that the severity of the
behavioral disturbances following inescapable shock correlate
positively with the LC firing rate.
Although there has been a general emphasis on the role of
the aminergic systems in stress and depression, there is a growing body of evidence that suggests that supersensitivity of central muscarinic mechanisms may be involved in the pathophysiology of depressive disorders (52, 53, 91-93). Stress results in the rapid activation of the septohippocampal cholinergic
system characterized by an increase in high-affinity uptake of
choline and the release of acetylcholine (ACh). The latter has
been shown to simultaneously induce alterations in behavioral,
cardiovascular and neuroendocrine function characteristic of those
observed during stress (52, 53, 143, 144). Hence, it has been
hypothesized that stress-induced changes in affective, neuroendocrine, sleep and heart rate profiles may reflect a central muscarinic cholinergic component. In this regard, in vivo and in
vitro data suggest that the muscarinic cholinergic agonist arecoline stimulates the HPA axis and that this effect is mediated
mainly by the release of endogenous CRH (36). In addition, it
MECHANISMS
OF STRESS
125
appears that the functional activity of ACh and the secretion o f
hypothalamic CRH are increased in affective disorders. The
physiological relevance o f a CRH-mediated cholinergic stimulation o f the HPA axis is underlined by data showing the involvement o f cholinergic neurotransmission in both the stress response
and the pathophysiology o f affective disorders (52, 53, I00,
116).
Our group has recently advanced data that some forms o f
major depression may not be associated with activation o f stressresponsive neurotransmitter systems, but rather with their inactivation. This subtype, termed atypical depression and characterized
by evidence o f pathological hypoarousal such as profound lethargy, hypersomnia, and hyperphagia, occurs across the boundaries o f medical illnesses such as Cushing's disease, chronic
fatigue syndrome, hypothyroidism, and seasonal affective disorder (73,74). We have advanced several lines o f evidence that
these disorders are associated with a functional decrease in the
responsiveness o f the CRH neuron in these disorders stemming
from a variety of pathophysiological mechanisms. In Cushing's
disease, we postulate that the long-standing peripherally medi-
ated (pituitary) hypercortisolism of this disorder causes a sustained suppression o f the hypothalamic CRH neuron contributing
to an atypical depression-like syndrome that is a frequent concomitant of Cushing's disease. In experimental models o f hyp o t h y r o i d i s m , we have s h o w n that there is a decrease in
hypothalamic CRH m R N A expression and content in association
with a subtle central adrenal insufficiency (96). In chronic fatigue syndrome, we have shown that a significant decrease in
24-hour urinary free cortisol excretion is associated with several
lines of indirect evidence indicative of a subtle central adrenal
insufficiency, including robust cortisol responses to low-dose
ACTH but blunted cortisol responses to high-dose ACTH, and
ACTH responses to CRH analogous to those seen in postoperative Cushing's disease patients thought to manifest a centrally
mediated adrenal insufficiency (101). Taken together, these data
suggest that a second major subtype o f primary affective disorder, namely atypical depression, reflects a pathological inactivation rather than a pathological activation of at least one arousalproducing neurotransmitter system that is thought to be a principal
effector o f the generalized stress response.
REFERENCES
1. Abbott, D. H. Behavioral and physiological suppression of fertility
in subordinate marmoset monkeys. Am. J. Primatol. 6:169-186;
1984.
2. Abbott, D. H. Behaviorally mediated suppression of reproduction
in female primates. J. Zool. (Lond.) 213:455-470; 1987.
3. Adams, F. The genuine works of Hippocrates. Baltimore: Williams
and Wilkins Company; 1939.
4. Adams, M. R,; Kaplan, J. R.; Koritnik, D. R. Psychosocial influences on ovarian endocrine and ovulatory function in Macaca facicularis. Physiol. Behav. 35:935-940; 1985.
5. Aghajanian, G. K. Mescaline and LSD facilitate the activation of
the locus coeruleus neurons by peripheral stimuli. Brain Res. 186:
492-498; 1980.
6. Aguilera, G. Corticotropin releasing factor receptors: Characterization and actions in the anterior pituitary gland. In: Chrousos, G,
P.; Loriaux, D. L.; Gold, P. W., eds. Mechanisms of physical and
emotional stress. Advances in experimental medicine and biology,
volume 245. New York: Plenum Press; 1988:83-105.
7. Alexlrod, J.; Reisine, T. D. Stress hormones: Their interaction and
regulation. Science 224:45--459; 1984.
8. Annecillo, C.; Money, J.; Lobatto. C.; Intelligence (IQ) lost and
regained: The psychoneuroendocrinology of failure to thrive, catch-up
growth, the syndrome of abuse dwarfism, and Munchausen's syndrome in proxy. In: Holmes, C. S., ed. Psychoneuroendocrinology: Brain, behavior and hormonal interactions. New York: SpringerVerlag; 1990:113-126.
9. Aston-Jones, G.; Foote, S, L.; Bloom, F. E. Anatomy and physiology of locus coeruleus neurons; functional implications. In: Ziegler, M. G.; Lake. C. R., eds. Norepinephrine. Baltimore: Williams
and Wilkins; 1984:92-116.
10. Bachman, G. A.; Kemmann, E. Prevalence of oligomenorrhea and
amenorrhea in a college population. Am. J. Obstet. Gynecol. 1'44:
98-102; 1982.
11. Baldwin, D. M.; Sawyer, C. H. Effects of dexamethasone on LH
release and ovulation in the cyclic rat. Endocrinology 94:13971403; 1974.
12. Bagdy, G,; Calogero, A. E.; Murphy, D.; Szemeredy, K. Serotonin agonists cause parallel activation of the sympathoadrenomedullary system and the hypothalamo-pituitary-adrenocortical axis in
conscious rats. Endocrinology 165:2664-2669; 1989.
13. Bambino, T. H.; Hsueh, A. J. W. Direct inhibitory effect of glucocorticoids upon testicular luteinizing hormone receptor and steroidogenesis in vivo and in vitro. Endocrinology 108:2142-2148;
1981.
14. Barbarino, A.; De Marinis, L.; Tofani, A.; Casa, S.; D'Amico,
C.; Mancini, A.; Corsello, S. M.; Sciuto, R.; Barini, A, Corticotropin-releasing hormone inhibition of gonadotropin release and
15.
16.
17.
18.
19.
20.
21.
22.
23.
24.
25,
26.
27.
28.
the effect of opioid blockade. J. Clin. Endocrinol. Metab. 68:523528; 1989.
Bartolome, J. V.; Barotome, M. B.; Daltner, L. A.; Evans, C. J.;
Barchas. J. D.; Kuhn, C. M.; Schanberg, S. M. Effects of [3-endorphin on ornithine decarboxylase in tissues of developing rats: A
potential role for this endogenous neuropeptide in the modulation
of tissue growth. Life Sci. 38:2355-2362; 1986.
Bassen, J. J,; Thorburn, G. D. Foetal plasma corticosteroids and
the initiation of parturition in the sheep. J. Endocrinol. '44:285286; 1969.
Bateman. A.; Singh, A.; Kral, T.; Solomon, S. The immune-hypothalamic-pituitary-adrenal axis. Endocr. Rev. 10:92-112; 1989.
Bernard, C. Les phenomenes de la vie. Vol. 1. Paris: Librairie J-B
Bailliere et Fils; 1878: 879.
Bernardini, R,; Calogero, A. E.; Ehrlich, Y. H.; Brucke, T.;
Chrousos, G. P.; Gold. P. W. The alkyl-ether phospholipid platelet-activating factor is a stimulator of the hypothalamic-pituitaryadrenal axis in the rat. Endocrinology 1:1067-1073; 1989.
Bernardini, R,; Chiarenza, A.; Calogero, A. E.; Gold, P. W.;
Chrousos, G. P. Arachidonic acid metabolites modulate rat hypothalamic corticotropin releasing hormone secretion in vitro. Neuroendocrinology 50:708-715; 1989.
Bernardini, R.; Kamilaris, T. C.; Calogero, A. E.; Johnson, E.
O.; Gold, P. W,; Chrousos. G. P. Interactions between tumor necrosis factor-a, hypothalamic corticotropin-releasing hormone and
adrenocorticotropin secretion in the rat. Endocrinology 126:2876-2881 ; 1990.
Besedovsky, J. O.; del Rey, A. E,; Sorkin, E. Neuroendocrine
immunoregulation. In: Fabris, W.; Garaci, E.; Hadden, J., eds.
Immunoregulation. London: Plenum Press; 1983.
Bird, S. J.; Kuhar, M. J. Iontophoretic application of opiates to
the locus ceruleus. Brain Res. 122:523-33; 1977.
Blake, C. A. Effects of "stress" on pulsatile luteinizing hormone
release in ovariectomized rats. Exp. Biol. Med. 148:813-815;
1975.
Blalock, J. E. A molecular basis for bidirectional communication
between the immune and neuroendocrine systems. Physiol. Rev.
69:1-32: 1989.
Bloom, R. E.; Battenberg, E. L. F.; Rivier. J.; Vale, W. Corticotropin releasing factor (CRFI: Immunoreactive neurones and fibers in rat hypothalamus, Regul. Pept. 4:43-48; 1982.
Bohus, B.; De Kloet, E.; Veldhuis, H. Adrenal steroids and behavioral adaptation: Relationships to brain corticoid receptors. In:
Ganten, R.; Pfaff, D., eds. Progress in Neuroendocrinology. vol
2. Berlin: Springer-Verlag; 1983:1.
Britton, D. R,; Koob, G. F.; Rivier, J.; Vale, W. Intraventricular
corticotropin-releasing factor enhances behavioral effects of nov-
126
elty. Life Sci. 31:363-367; 1982.
29. Britton, D. R.; Lee, G.; Dana, R.; Risch, S. C.; Koob, G. F. Activiating and "anxiogenic" effects of corticotropin-releasing factor
are not inhibited by blockade of the pituitary-adrenal system with
dexamethasone. Life Sci. 39:1281-1286; 1986.
30. Broadhurst, P. L. Experiments in psychogenetics applications of
biomedical genetics to the inheritance of behavior. In: Eysenck, H.
J., ed. Experiments in personality psychogenetics and psychopharmacology, vol. 1. London: Routledge and Keegan Paul; 1960:1102.
31. Brown, M. R.; Fisher, L. A.; Spiess, J.; Rivier, J.; Rivier, C.;
Vale, W. Corticotropin releasing factor: Actions on the sympathetic nervous system and metabolism. Endocrinology 111:928931: 1982.
32. Cacciari, E.; Salardi, S.; Lazzari, R., et al. Short stature and celiac disease: A relationship to consider even in patients with no
gastrointestinal symptoms. J. Pediatr. 103:708-711; 1983.
33. Callabrese, J. R.; Kling, M. A.; Gold, P. W. Alterations in immunocompetence during stress, bereavement, and depression: Focus on neuroendocrine regulation. Am. J. Psychiatry 144:11231134; 1987.
34. Calogero, A. E.; Gallucci, W. T.; Gold, P. W.; Chrousos, G. P.
Multiple feedback regulatory loops upon rat hypothalamic corticotropin-releasing hormone secretion. J. Clin. Invest. 82:767-774;
1988.
35. Calogero, A. E.; Bernardini, R.; Gold, P. W.; Chrousos, G. P.
Regulation of rat hypothalamic corticotropin-releasing hormone secretion in vitro: Potential clinical implications. In: Chrousos, G.
P.; Loriaux, D. L.; Gold, P. W., eds. Mechanisms of physical and
emotional stress, vol. 245. Advances in experimental medicine and
biology. New York: Plenum Press; 1988:167-181.
36. Calogero, A. E.; Kamilaris. T. C.; Gomez, M. T.; Johnson, E.
O.; Tartaglia, M. E.; Gold, P. W.; Chrousos, G. P. The muscarinic cholinergic agonist arecoline stimulates the rat hypothalamicpituitary-adrenal axis through a centrally-mediated corticotropinreleasing hormone-dependent mechanism. Endocrinology 125:2"442453; 1989.
37. Cannon, W. B. The wisdom of the body. Physiol. Rev. 9:399431; 1929.
38. Carrol, B.; Eeinberg, M.; Greden, J.; Tarika, J.; Albala, A.; Haskett, R.; James, N.; Kronfol, Z.; Lohr, N.; Steiner, M.; de Vigne,
J.; Young, E. A specific laboratory test for the diagnosis of melancholia. Arch. Gen. Psychiatry 38:15-22; 1981.
39. Charpenet, G.; Tache, Y.; Forest, M. G.: Haour, F.; Saez, J. M.;
Bemier, M.; Ducharme, J. R.; Collu, R. Effects of chronic intermittent immobilization stress on rat testicular androgenic function.
Endocrinology 109(4): 1254-1258; 198 I.
40. Chrousos, G. P.; Schulte, H. M.; Oldfield, E. H.; Loriaux, D. L.;
Cutler, G. B.; Kellner, C. H.; Gold, P. W. Hypothalmic hormones
in neuropsychiatric disease. Psychopharmacol. Bull. 19:416--421;
1983.
41. Chrousos, G. P.; Schuermeyer, T. H.; Doppman, J.: Oldfield, E.
H.; Schulte, H. M.; Gold, P. W.; Loriaux, D. L. Clinical applications of corticotropin-releasing factor. Ann, Intern. Med. 102:344358; 1985.
42. Chrousos, G. P.; Loriaux, L. D.; Gold, P. W. The concept of
stress and its historical development. In: Chrousos, G. P.; Loriaux,
L. D.; Gold, P. W., eds. Mechanisms of physical and emotional
stress, vol. 245. Advances in experimental medicine and biology.
New York: Plenum Press; 1988:3-7.
43. Chrousos, G. P.; Laue, L.; Nieman, L. K.; Kawai, S.; Udelsman,
R. U.; Brandon, D. D.; Loriaux, D. L. Glucocorticoids and glucocorticoid antagonists: Lessons from RU 486. Kidney Int. 34(Suppl.
26):18-23; 1988.
44. Collu, R.; Gibb, W.; Ducharme, J. R. Effects of stress on the gonadal function. J. Endocrinol. Invest. 7:529-537; 1984.
45. Cummings, S.; Elde, R.; Ell, J.; Lendall, A. Corticotropin-releasing factor immunoreactivity is widely distributed within the central
nervous system of the rat: An immunohistochemical study. J. Neurosci. 3:1355-1368; 1983.
46. D'Ercole, A. J.; Underwood, L. E.; Van Wyk, J. J. Serum somatomedin-C in hypopituitarism and in other disorders of growth.
J. Pediatr. 90:375-381; 1977.
JOHNSON,
KAMILARIS,
CHROUSOS
AND
GOLD
47. De Souza, E. B.; lnsel, T. R.; Perrin, M. H.; Rivier, J.; Vale, W.
W.; Kuhar, M. J. Corticotropin-releasing factor receptors are widely
distributed within the rat central nervous system: An autoradiographic study. J. Neurosci. 5:3189-3203; 1985.
48. Deutch, A. Y.; Clark, W. A.; Roth, R. H. Prefrontal cortical dopamine depletion enhances the responsiveness of the mesolimbic
dopamine neurons to stress. Brain Res. 521:311-315; 1990.
49. Deutch, A. Y.; Goldstein, M.; Roth, R. H. Activation of the locus ceruleus by selective stimulation of the ventral tegmental area.
Brain Res. 363:307-314: 1986.
50. De Wied, D. Pituitary-adrenal system hormones and behavior. In:
Schmitt, F. G.; Worden, F. G., eds. The neurosciences. Third
study program. Cambridge: MIT Press; 1974:653-666.
51. De Wied, D. Pituitary-adrenal system hormones and behavior. In:
Selye, H., ed. Selye's guide to stress research, vol 1. New York:
Van Nostrand Reinhold; 1980:252-279.
52. Dilsaver, S. C. Effects of stress on muscarinic mechanisms. Neurosci. Biobehav. Rev. 12:23-28; 1988.
53. Dilsaver S. C.; Alessi, N. E. Chronic inescapable footshock produces cholinergic system supersensitvity. Biol. Psychiatry 22:914918; 1987.
54. Doerr, P.; Pirke, K. M. Cortisol-induced suppression of plasma
testosterone in normal adult males. J. Clin. Endocrinol. Metab.
43:622-629; 1976.
55. Euker, J. S.; Meites, J.; Riegte, G. D. Effects of acute stress on
serum LH and prolactin in intact, castrate and desamethasonetreated male rats. Endocrinology 96:85-92; 1975.
56. Field, T. Supplemental stimulation of preterm neonates. Early
Hum. Dev. 4:301-314; 1980.
57. File, S. E. ACTH but not corticosterone impairs habituation and
reduces exploration. Pharmacol. Biochem. Behav. 9:161-166; 1978.
58. File, S. E.; Clarke, A. Exploration motor activity after intraventricular ACTH, morphine and naloxone. Behav. Brain Res. 2:223227; 1980,
59. Fisher, L. A.; Rivier, J.; Rivier, C.; Speiss, J.; Vale, W.; Brown,
M. R. Corticotropin releasing factor (CRF): Central effects on
mean arterial pressure and heart rate in rats. Endocrinology 110:
2222-2224; 1982.
60. Foote, S. L.; Aston-Jones, G.; Bloom, F. E. Inpulse activity of
locus coeruleus neurons in awake rats and monkeys is a function
of sensory stimulation and arousal. Proc. Natl. Acad. Sci. USA
77:3033-3037; 1980.
61. Foote. S. L; Bloom, F. E.; Bloom, F. E. Nucleus locus ceruleus:
New evidence for anatomical and physiological specificity. Physiol. Rev. 63:8'44-914; 1983.
62. Fuxe, K.; Wikstrom, A.; Okret, S.; Agnati, L.; Harfstrand, A.;
Yu, Z.; Granholm, L.; Zoli, M.; Vale, W.; Gustafsson, J., et al.
Mapping of glucocorticoid receptor immunoreactive neurons in the
rat teland diencephalon using a monoclonal antibody against rat
liver glucocorticoid receptor. Endocrinology 117:1803-1812; 1985.
63. Ganong, W. E. The stress response--a dynamic overview. Hosp.
Pract. 93:155-171; 1988.
64. Gardiner, S. M.; Compton, A. M.; Bennett, T. Cardiovascular instability induced by intracerebroventricular administration of vasopressin or corticotrophin-releasing factor in conscious Long Evans
and Brattleboro rats. J. Neuroendocrinol. 2:39--43; 1990.
65. Garrison, F. H. An introduction to the history of medicine. Philadelphia: Saunders; 1929.
66. Gilbeau, P. M.; Smith, C. G. Naloxone reversal of stress induced
reproductive effects in the male rhesus monkey. Neuropeptides
5:335-338; 1985.
67. Gillis, S.; Crabtree, G. R.; Smith, K. A. Glucocorticoid induced
inhibition of T cell growth factor production I. The effect of mitogen induced lymphocyte proliferation. J. lmmunol. 123:1624-1631 ;
1979.
68. Gindoff, P. R.; Ferin, M. Endogenous opioid peptides modulate
the effect of corticotropin-releasing factor on gonadotropin release
in the primate. Endocrinology 121:837-842; 1987.
69. Gipsen, W. H.; van der Poel, A.; van Wimersma Greidanus, T.
B. Pituitary adrenal influences on behavior. Responses to test situations with or without electric footshock. Physiol. Behav. 10:345350; 1973.
70. Gold, P. W.; Chrousos, G. P. Clinical studies with corticotropin
MECHANISMS
71.
72.
73.
74.
75.
76.
77.
78.
79.
80.
81.
82.
83.
84.
85.
86.
87.
88.
89.
OF STRESS
releasing factor: Implications for the diagnosis and pathophysiology of depression, Cushing's disease, and adrenal insuffiency.
Psychoneuroendocrinology 10:401-419; 1985.
Gold, P. W.; Loriaux, D. L.; Roy, A.; Kling, M. A.; Calabrese,
J. R.; Kellner, C. H.; Nieman, L. K.; Post, R. M.; Pickar, D.;
Gallucci, W.; Avgerinos, P.; Paul, S.; Oldfield, E. H.; Cutler, G.
B.; Chrousos, G. P. Responses to corticotropin-releasing hormone
in the hypercortisolism of depression and Cushing's disease. N.
Engl. J. Med. 314:1329-1335; 1986.
Gold, P. W.; Gwirtsman, H.; Avgerinos, P. C.; Nieman, L. K.;
Gallucci, W. T.; Kaye, W.; Jimerson, D.; Ebert, M.; Rittmaster,
R.; Loriaux, D. L.; Chrousos, G. P. Abnormal hypothalamic-pituitary-adrenal function in anorexia nervosa: Pathophysiologic mechanisms in underweight and weight-corrected patients. N. Engl. J.
Med. 314:1335-1342; 1986.
Gold, P. W.; Goodwin, F. K.; Chrousos, G. P. Clinical and biochemical manifestations of depression: Relation to the neurobiology of stress. (first of two parts). N. Engl. J. Med. 319:348-353;
1988.
Gold, P. W.; Goodwin, F. K.; Chrousos, G. P. Clinical and biochemical manifestations of depression: Relation to the neurobiology of stress. (second of two parts). N. Engl. J. Med. 319:413420; 1988.
Gray, T. S. Amygdala: Role in autonomic and neuroendocrine responses to stress. In: McCubbin, J. A.; Kaufman, P. G.; Nemeroff, C. B., eds. Stress, neuropeptides and systemic disease. New
York: Academic Press; 1991:37-53.
Green, W. H.; Campbell, M.; David, R. Psychosocial dwarfism:
A critical review of the evidence. J. Am. Acad. Clin. Child Adolesc. Psychiatry 23:39--48; 1984.
Green, W. H. A theoretical model for classical psychosocial dwarfism (psychosocially determined short stature). In: Holmes, C. S.,
ed. Psychoneuroendocrinology: Brain, behavior and hormonal interactions. New York: Springer-Verlag; 1990:92-112.
Groll, A.; Preece, M. A.; Candy, D. C. A., et al. Short stature as
the primary manifestation of celiac disease. Lancet 2:1097-1105;
1980.
Guillemin, R.; Vargo, T.; Rossier, J.; Minick, S.; Ling, N.; Rivier, C.; Vale, W.; Bloom, F. Beta-endorphin and adrenocorticotropin are secreted concomitantly by the pituitary gland. Science 197:
1367-1368; 1977.
Guynet, P. G.; Aghajanian, G. K. Acetylcholine, substance P and
met-enkephalin in the locus coeruleus: Pharmacological evidence
for independent sites of action. Eur. J. Pharmacol. 53:319-328;
1979.
Hagino, N.; Watanabe, M.; Goldzieher, J. W. Inhibition by
adrenocorticotrophin of gonadotrophin-induced ovulation in immature female rats. Endocrinology 84:308-314; 1969.
Harlow, H. F.; Zimmerman, R. R. Affectational responses in the
infant monkey. Science 130:421-432; 1959.
Harris, G. W. Neural control of the pituitary gland. Physiol. Rev.
28:134-179; 1948.
Hatfield, J. M.; Daikh, D. I.; Adelman, J. P.; Douglass, J.; Bond,
C. T.; Allen, R. G. In situ hybridization detection of marked differences in pre-proopiomelanocortin messenger ribonucleic acid
content of individual corticotropes and melanotropes. Endocrinology 124:1359-1364; 1989.
Haynes, B. F.; Fanci, A. S. The differential effect of in vivo hydrocortisone on the kinetics of subpopulations of human peripheral
blood thymus-derived lymphocytes. J. Clin. Invest. 61:703-707;
1978.
Hotta, M.; Shibasaki, T.; Masuda, A.; Imaki, T.; Demura, H.;
Ling, N.; Shizume, K. The response of plasma adrenocorticotropin and cortisol to corticotropin releasing hormone (CRH) and
cerebrospinal fluid immunoreactive CRH in anorexia nervosa patients. J. Clin. Endocrinol. Metab. 62:319-324; 1986.
Howarth, B., Jr.; Hawk, H. W. Effect of hydrocortisone on embryonic survival in sheep. J. Anita. Sci. 27:117-121; 1968.
Ingle, D. J. Permissibility of hormone action. A review. Acta Endocrinol. 17:172-186; 1954.
Isaacson, R. L.; Green, E. T. The effects of ACThI_24 on locomotion, exploration, rearing and grooming. Behav. Biol. 24:118122; 1978.
127
90. Isaksson, O. G. P.; Jansson, J. 0.; Gansel, A. M. Growth hormone stimulates longitudinal bone growth directly. Science 216:
1237-1241; 1982.
91. Janowsky, D. S.; El-Yousef, M. K.; Davis, J. H.; Sereke, H. S.
A cholinergic adrenergic hypothesis of mania and depression. Lancet 19:675-681; 1972.
92. Janowsky, D. S.; Risch, S. C. Acetylcholine hypothesis of stress
modulation. Integ. Psychiatry 3:3-9; 1985.
93. Janowsky, D. S.; Risch, S. C. Cholinomimetic and anticholinergic
drugs used to investigate a cholinergic hypothesis of affective disorders and stress. Drug Dev. Rev. 4:125-142; 1984.
94. Johnson. H. M.; Smith, E. M.; Torres. B. A.; Blalock, J. E. Regulation of the in vitro antibody response by neuroendocrine hormones. Proc. Natl. Acad. Sci. USA 79:4171--4174; 1982.
95. Johnson, H. M.; Toress. B. A.; Smith, E. M.; Dion, L. D.; Blalock. J. E. Regulation of lymphokine (-,/-interferon) production by
corticotropin. J. Immunol. 132:246-250; 1984.
96. Kamilaris, T. C.; DeBold, C. R.; Johnson, E. O.; Mamalaki, E.;
Listwak, S. J.; Calogero, A. E.; Kalogeras, K. T.; Gold, P. W.;
Orth, D. N. Effects of short and long duration hypothyroidism and
hyperthyroidism on the plasma adrenocorticotropin and corticosterone responses to ovine corticotropin-releasing hormone in rats.
Endocrinology 128:2567-2576; 1991.
97. Kaye, H.; Pickar, D.; Naber, D.; Ebert, M. Cerebrospinal fluid
opioid activity in anorexia nervosa. Am. J. Psychiatry 139:643645; 1982.
98. Kaye, W.; Gwirtsman, H.; George, D.; Ebert, M.; Jimerson, D.;
Tomai, T.; Chrousos, G.; Gold, P. Elevated cerebrospinal fluid
levels of immunoreactive corticotropin releasing hormone in anorexia nervosa: Relation to state of nutrition, adrenal function, and
intensity of depression. J. Clin. Endocrinol. Metab. 64:203-208;
1987.
99. Keller-Wood, M.; Dallman, M. Corticosteroid inhibition of ACTH
secretion. Endocr. Rev. 5:1-24; 1984.
100. Kennedy, S.; Thompson, R.; Stancer, H. C.; Roy, A.; Persad, E.
Life events precipitating mania. Br. J. Psychiatry. 142:398-403;
1983.
101. Kling, M. A.; Roy, A.; Doran, A. R.; Calabrese, J. R.; Rubinow,
D. R.; Whitfield, H. J.; Conrad, M.; Post, R. M.; Chrousos, G.
P.; Gold, P. W. Cerebrospinal fluid immunoreactive corticotropinreleasing hormone and adrenocorticotropin secretion in Cushing's
disease and major depresssion: Potential clinical implications. J
Clin. Endocr. Metab. 72:260-271; 1991.
102. Koob, G. F.; Bloom, F. E. Corticotropin-releasing factor and behavior. Fed. Proc. 44:259-263; 1985.
103. Kopin, I. J.; Eisenhofer, G.; Goldstein, D. Sympathoadrenal medullary system and stress. In: Chrousos, G. P.; Loriaux, D. L.;
Gold, P. W., eds. Mechanisms of physical and emotional stress.
vol. 245. Advances in experimental medicine and biology. New
York: Plenum Press; 1986:11-23.
104. Kopin, I. J.; Eisenhofer, G.; Goldstein, D. Adrenergic response
following recognition of stress. In: Breznits, S.; Zinder, O., eds.
Molecular biology of stress. New York: Alan R. Liss; 1989:123132.
105. Krieger, D. Cushing's Syndrome. vol 22. Monographs in endocrinology. Berlin: Springer-Verlag; 1982.
106. Krieger. D.; Good, M. H. Adrenocortical and thyroid function in
the deprivation syndrome. Am. J. Dis. Child. 120:95-102; 1970.
107. Krieger, D. T.; Liotta, A. S.; Brownstein, M. J. Presence of corticotropi in brain of normal and hypophysectomized rats. Proc.
Natl. Acad. Sci. USA 74:648-652; 1977.
108. Kvetnansky, R.; Nemeth, S.; Vegas, M.; Oprsalova, Z.; Jurcovicova, J. Plasma catecholamines in rats during adaptation to intermittent exposure to different stress. In: Usdin, E.; Kvetnansky,
R.; Alexlrod, J., eds. Stress: The role of catecholamines and
other neurotransmitters. New York: Gordon and Breach; 1984:537562.
109. Lamberts, S. W.; Zwiderwizk, J.; Uitterlinder, P.; Blizd, J.;
Bruning, H.; De Jong, F. Characterization of adrenal autonomy in
Cushing's syndrome: A comparison between in vivo and in vitro
responsiveness of the adrenal gland. J. Clin. Endocrinol. Metab.
70:192-199; 1990.
110. Landfield, P.; Baskin, R.; Pitier, T. Brain-aging correlates: Retar-
128
111.
112.
113.
114.
115.
116.
117.
118.
119.
120.
121.
122.
123.
124.
125.
126.
127.
128.
129.
130.
131.
132.
133.
134.
JOHNSON,
dation by hormonal-pharmacological treatments. Science 214:581584; 1981.
Landsberg, L. Catecholamines and the sympathoadrenal system.
In: Ingbar, S., ed. The year in endocrinology 1975-1976. New
York: Plenum; 1976:177.
Levine, S. Psychobiologic consequences of disruption in motherinfant relationships. In: Krasnegor, N. A.; Blass, E. M.; Hofer,
M. A.; Smotherman, W. P., ed. Perinatal development: A psychobiological perspective. New York: Academic Press; 1987:359-376.
Levine, S.; Goldman. L.; Coover, G. D. Expectancy and the pituitary-adrenal system. In: Physiology, emotion and psychosomatic
illness. CIBA Foundation symposium 8. Amsterdam: Elsevier/Excerpta Medica; 1972:281-291.
Liggens, G. C.; Fairclough, R. J.; Grieves, S. A.; Kendall, J. W.,
et al. The mechanism of parturition in the ewe. Recent Progr.
Horm. Res. 29:111-150; 1973.
Linder, B.; Cassorla, F. Short stature: Etiology, diagnosis, and
treatment. JAMA 260:3171-3175; 1988.
Lloyd, C. Life events and depressive disorder: II. Events as precipitating factors. Arch. Gen. Psychiatry. 37:541-548; 1980.
Loucks, A. B.; Mortola, J. F.; Girton, L.; Yen, S. C. Alterations
in the hypothalamic-pituitary-ovarian and the hypothalamic-pituitary-adrenal axes in athletic women. J. Clin. Endocrinol. Metab.
68:402-411 ; 1989.
McCarty, R. Stress, behavior and the sympathetic-adrenal medullary system. In: Pohorecky, L. A.; Brick, J., ed. Stress and alcohol use. New York: Elsevier Science Publishers; 1983:7.
McCarty, R.; Stone, E. A. Chronic stress and regulation of the
sympathetic nervous system. In: Usdin, E.; Kvetnansky, R.; Alexlrod, J., eds. Stress: The role of catecholamines and other neurotransmitters. New York: Gordon and Breach; 1984:563-576.
McEwen, B. S.; Weiss, J.; Schwartz, L. Selective retention of
corticosterone by limbic structures in rat brain. Nature 220:911912; 1968.
Makara, G. B. Mechanisms by which stressful stimuli activate the
pituitary-adrenal system. Fed. Proc. 44:149-153; 1985.
Mains, R.; Eipper, E.; Ling, N. Common precursor to corticotropin and endorphins. Proc. Natl. Acad. Sci. USA 74:3014-3018;
1977.
Marsh, J. T.; Rasmussen, A. F. Response of adrenals, thymus,
spleen and leukicytes to shuttle box and confinement stress. Proc.
Soc. Exp. Biol. Med. 104:180-183; 1960.
Mason, J. W. A review of psychoendocrine research on the sympatho-adrenal medullary system. Psychosom. Med. 30:576-607;
1968.
Meany, M.; Aitken, D. The effects of early, postnatal handling on
hippocampal glucocorticoid receptor concentrations: Temporal parameters. Brain Res. 22:30-304; 1985.
Meany, M.; Aitken, D.; Bodnoff, S.; Iny, L.; Tatarevicz, J.; Sapolsky, R. Early postnatal handling alters glucocorticoid receptor
concentrations in selected brain regions. Behav. Neurosci. 99:765770; 1985.
Meyer, J. Biochemical effects of corticosteroids on neural tissues.
Physiol. Rev. 65:946-1020; 1985.
Millan, M. A.; Abous Samra, A. B.; Wynn, P. C.; Catt, K. J.;
Aquilera, G. Receptors and actions of corticotropin releasing hormone in the primate pituitary gland. J. Clin. Endocrinol. Metab.
64:1036-1041; 1987.
Money, J. The syndrome of abuse dwarfism (psychosocial dwarfism or reversible hyposomatotropinism): Behavioral data and case
report. Am. J. Dis. Child. 131:508-513; 1977.
Money, J.; Annecillo, C.; Kelley, J. F. Abuse-dwarfism syndrome:
After rescue, statural and intellectual catchup growth correlate. J.
Clin. Child Psychol. 12:279-283; 1983.
Monjan, A. A. Stress and immunologic competence: Studies in
animals. In: Ader, R., ed. Psychoneuroendocrinology. New York:
Academic Press; 1985:185.
Morely, J. E.; Levine, A. S. Corticotropin-releasing factor, grooming and ingestive behavior. Life Sci. 31:1459-1464; 1982.
Munck, A.; Guyre, P.; Holbrook, N. Physiological functions of
glucocorticoids in stress and their relation to pharmacological actions. Endocrin. Rev. 5:25-44; 1984.
Munck, A.; Guyre, P. M. Glucocorticoid physiology, pharmacol-
135.
136.
137.
138.
139.
140.
141.
142.
143.
144.
145.
146.
147.
148.
149.
150.
151.
152.
153.
154.
155.
KAMILARIS,
CHROUSOS
AND GOLD
ogy and stress. In: Chrousos, G. P.; Loriaux, D. L.; Lipsett, M.
B., eds. Steroid hormone resistance. New York: Plenum Press;
1986:81-96.
Naito, Y.; Fukata, J.; Tominaga, T.; Nakai, Y.; Tamai, S.; Mori,
K.; Imura, H. Interleukin 6 stimulates the secretion of adrenocorticotropic hormone in conscious, freely moving rats. Biochem. Biophys. Res. Commun. 155:1459-1463; 1988.
Nauta, W. J. H.; Feirtag, M. Fundamental neuroanatomy. New
York: W. H. Freeman; 1986.
Nikolarakis, K. E.; Almeida, O. S. X.; Sirinathsinghji, D. J. S.;
Herz, A. Stimulation of hypothalamic beta-endorphin and dynorphin release by corticotropin-releasing factor (in vitro). Brain Res.
399:152-155; 1986.
Nikolarakis, K. E.; Almeida, O. S. X.; Sirinathsinghji, D. J. S.;
Herz, A. Concomitant changes in the in vitro and in vivo release
of opioid peptides and luteinizing hormone-releasing hormone from
the hypothalamus following blockade of receptors for corticotropin-releasing factor. Neuroendocrinology 47:545-550; 1988.
O'Byrne, K. T.; Lunn, S. F.; Dixson, A. F. Effects of acute stress
and the patterns of LH secretion in the common marmoset (Callithrixjacchus). J. Endocrinol. 118:259-264; 1988.
O'Byrne, K. T.; Lunn, S. F.; Dixson, A. F. Naloxone reversal of
stress-induced suppression of LH release in the common marmoset. Physiol. Behav. 45:1077-1080; 1989.
Olschowka, J. A.; O'Donohue, T. L.; Mueller, G. P.; Jacobowitz,
D. M. The distribution of corticotropin releasing factor-like immunoreactive neurons in rat brain. Peptides 3:995-1015; 1982.
Ono, N.; Lumpkin, M. D.; Samson, W. K.; McDonald, J. K.;
McCann, S. M. Intrahypothalamic action of corticotrophin-releasing factor (CRF) to inhibit growth hormone and LH release in the
rat. Life Sci. 35:1117-1123; 1984.
Overstreet, D. H.; Janowsky, D. S.; Gillin, J. C.; Shiromani, P.
J.; Sutin, E. L. Stress induced immobility in rats with cholinergic
supersensitivity. Biol. Psychiatry 21:657-664; 1986.
Overstreet, D. H.; Russel, R. W.; Crocker, A. D.; Janowsky, D.
S.; Gillin, J. C. Genetic and pharmacological models of cholinergic supersensitivity. Experientia 44:465-472; 1988.
Pare, W. The effect of chronic environmental stress on premature
aging in the rat. J. Gerontol. 20:78-84; 1965.
Petraglia, F.; Vale, W.; Rivier, C. Opioids act centrally to modulate stress-induced decrease in luteinizing hormone in the rat. Endocrinology 119:2445-2450; 1986.
Petraglia, F.; Sutton, S.; Vale, W.; Plotsky, P. Corticotropin-releasing factor decreases plasma LH levels in female rats by inhibiting gonadotropin-releasing hormone release into hypo-physialportal circulation. Endocrinology 20:1083-1088; 1987.
Plotsky, P.; Bruhn, T.; Otto, S. Central modulation of immunoreactive arginine vasopressin and oxytocin secretion into the hypophysial-portal circulation by CRF. Endocrinology 116:16391641; 1985.
Pollard, I.; Dyer, S. L. Effect of stress administered during pregnancy on the development of fetal testes and their subsequent
function in the adult rat. J. Endocrinol. 107:241-245; 1985.
Pollard, I. Prenatal stress effects over two generations in rats. J.
Endocrinol. 109:239-244; 1986.
Powell, G. F.; Brasel, J. A.; Blizzard, R. M. Emotional deprivation and growth retardation simulating idiopathic hypopituitarism.
Clinical evaluation of the syndrome. N. Engl. J. Med. 276:12711278; 1967.
Rabin, D.; Gold, P. W.; Margioris, A. N.; Chrousos, G. P. Stress
and reproduction: Physiologic interactions between the stress and
reproductive axes. In: Chrousos, G. P.; Loriaux, D. L.; Gold, P.
W., eds. Mechanisms of physical and emotional stress, vol 245.
Advances in experimental medicine and biology. New York: Prenrice-Hall; 1988:377-387.
Rabin, D. S.; Johnson, E. O.; Brandon, D. D.; Liapi, C.; Chrousos, G. P. Glucocorticoids inhibit estradiol-mediated uterine growth:
Possible role of the uterine estradiol receptor. Biol. Reprod. 42:
74-80; 1990.
Ranke, M. B.; Pfluger, H.; Rosendahl, W., et al. Turner syndrome: Spontaneous growth in 150 cases and review of the literature. Eur. J. Pediatr. 141:81-88; 1983.
Reul, J.; DeKloet, E. Two receptor systems for corticosterone in
MECHANISMS
156.
157.
158.
159.
160.
161.
162.
163.
164.
165.
166.
167.
168.
169.
170.
171.
172.
173.
174.
175.
176.
177.
178.
OF STRESS
rat brain: Microdistribution and differential occupation. Endocrinology 177:2505-2511; 1985.
Rigter, J.; Veldhuis, H.; De Kloet, E. Spatial orientation and the
hippocampal corticosterone recptor systems of old rats; Effect of
ACTI-I4_9 analogue ORC2766. Brain Res. 309:393-398; 1984.
Rivier, C.; Vale, W. Modulation of stress-induced ACTH release
by CRF, catecholamines, and vasopressin. Nature 305:325-327;
1983.
Rivier, C.; Vale, W. Influence of corticotropin-releasing factor on
reproductive functions in the rat. Endocrinology 114:914-921; 1984.
Rivier, C.; Vale, W. Corticotropin-releasing factor (CRF) acts
centrally to inhibit growth hormone secretion in the rat. Endocrinology 114:2409-2411; 1984.
Rivier, C.; Vale, W. Involvement of corticotropin-releasing factor
and somatostatin in stress-induced inhibition of growth hormone
secretion in the rat. Endocrinology 117:2478-2482; 1985.
Rivier, C.; Rivier, J.; Vale, W. Stress-induced inhibition of reproductive functions: Role of endogenous corticotropin-releasing factor. Science 231:607-609; 1986.
Rose, R. M. Endocrine response to stressful psychological events.
Psychiatr. Clin. North Am. 3:251; 1980.
Rosenblum, L. A. Influences of environmental demand on maternal behavior and infant development. In: Krasnegor, N. A.; Blass,
E. M.; Hofer, M. A.; Smotherman, W. P., eds. Perinatal development: A psychobiological perspective. New York: Academic Press;
1987:377-395.
Roth, R. H.; Tam, S. Y.; Lda, Y.; Yang, J. S.; Deutch, A. Y.
Stress and the mesocorticolimbic dopamine systems. Ann. NY
Acad. Sci. 537:138-147; 1988.
Sachet, R. J.; Hellman, C.; Roffwarg, H. P.; Halpern, F. S.;
Fukushima, D. K.; Gallagher, T. F. Disrupted 24-hour patterns of
cortisol secretion in psychotic depression. Arch. Gen. Psychiatry
28:19-24; 1973.
Saffran, M.; Schally, A. V.; Bentey, B. G. Stimulation of the release of corticotropin from the adenohypophysis by a neurohypophyseal factor. Endocrinology 57:439~.44; 1955.
Sapolsky, R. Glucocorticoid toxicity in the hippocampus: Temporal aspects of neuronal vulnerability. Brain Res. 359:300-305;
1985.
Sapolsky, R. M. Endocrine and behavioral correlates of drought in
wild olive baboons (Papio anubis). Am. J. Primatol. 11:217-227;
1986.
Sapolsky, R.; McEwen, B. S. Down-regulation of neural corticosterone receptors by corticosterone and dexamethasone. Brain Res.
339:161-165; 1985.
Sapolsky, R.; Pulsinelli, W. Glucocorticoids potentiate ischemic
injury to neurons: Therapeutic implications. Science 229:13971399; 1985.
Sapolsky, R.; Krey, L.; McEwen, B. The adrenocortical stress-response in the aged male rat: Impairment of recovery from stress.
Exp. Gerontol. 18:55-63; 1983.
Sapolsky, R.; Krey, L.; McEwen, B. Corticosterone receptors decline in a site-specific manner in the aged rat brain. Brain Res.
289:235-240; 1983.
Sapolsky, R.; Krey, L. C.; McEwen, B. S. The neuroendocrinology of stress and aging: The glucocorticoid cascade hypothesis.
Endocr. Rev. 7:284-301; 1986.
Sapolsky, R.; Krey, L. C.; McEwen, B. S. Prolonged glucocorticold exposure reduces hippocampal neuron number: Implications
for aging. J. Neurosci. 5:1222-1227; 1985.
Sapolsky, R.; Rivier, C.; Yamamoto, G.; Plotsky, P.; Vale, W.
Interleukin 1 stimulates the secretion of hypothalamic corticotropin
releasing factor. Science 238:522"--524; 1987.
Sawchenko, P. E.; Swanson, L. W.; Joseph, S. A. The distribution and cells of origin of ACTH (1-39) stained varicosities in the
paraventricular and supraoptic nuclei. Brain Res. 232:365-374;
1982.
Sawchenko, P.; Swanson, L.; Vale, W. Co-expression of CRF and
vasopressin immunoreactivity in parvocellular neurosecretory neurons of the adrenalectomized rat. Proc. Natl. Acad. Sci. USA 81:
1883-1887; 1984.
Schally, A. V.; Chang, R. C.; Arimura, A.; Redding, T. W.;
Fishback, J. B.; Vigh, S. High molecular weight peptide with cor-
129
179.
180.
181.
182.
183.
184.
185.
186.
187.
188.
189.
190.
191.
192.
193.
194.
ticotropin-releasing factor activity from porcine hypothalami. Proc.
Natl. Acad. Sci. 78:5197-5201; 1981.
Schanberg, S. M.; Field, T. M. Maternal deprivation and supplemental stimulation. In: Field, T. M.; McCabe, P. M.; Schneiderman, N., eds. Stress and coping across development. Hillsdale,
NJ: Erlbaum; 1988:3-25.
Schanberg, S. M.; Kuhn, C. M. Maternal deprivation: An animal
model of psychosocial dwarfism. In: Usdin, E.; Squrkes, T. L.;
Youdim, M. B. H., eds. Enzymes and neurotransmitters in mental
disease. New York: John Wiley and Sons; 1980:372-393.
Seligman, M. E. P. Reversal of performance deficits and perceptual deficits in learned helplessness and depression. J. Abnorm.
Psychol. 85:11-26; 1976.
Seligman, M. E. P.; Maler, S. F. Failure to escape traumatic
shock. J. Exp. Psychol. 74:1-9; 1967.
Selye, H. A syndrome produced by diverse nocuous agents. Nature 138:32; 1936.
Selye, H. The general adaptation syndrome and the diseases of adaptation. J. Clin. Endocrinol. 6:117-173; 1946.
Selye, H. Stress. The physiology and pathophysiology of exposure
to stress. Montreal: Acta; 1950.
Selye, H. Hormones and resistance. New York: Springer-Verlag;
1971.
Selye, H. The evolution of the stress concept. Am. Scient. 61:692699; 1973.
Seyle, H. Selye's guide to stress research, vol 1. New York: Van
Nostrand Reinhold; 1980:v.
Shibihara, Y.; Morimoto, Y.; Furutani, Notake, M.; Takahashi,
H.; Shimizu, S.; Horikawa, S.; Numa, S. Isolation and sequence
analysis of the human corticotropin-releasing factor precursor gene.
EMBO J. 2:775-779; 1983.
Siiteri, P. K.; Mural, J. T.; Hammond, G. L.; Nisker, J. A.; Raymoure, W. J.; Kuhn, R. W. The serum transport of steroid hormones. Recent Prog. Horm. Res. 38:457-510; 1982.
Sirinathsinghji, D. J. S.; Rees, L. H.; Rivier, J.; Vale, W. Corticotropin-releasing factor is a potent inhibitor of sexual receptivity
in the female rat. Nature 305:232-235; 1983.
Smith, M. A.; Kling, M. A.; Whitfield, H. J.; Brandt, H. A.;
Demitrack, M. A.; Geracioti, T. D.; Chrousos, G. P; Gold, P. W.
Corticotropin-releasing hormone: From endocrinology to psychobiology. Horm. Res. 31:66-71; 1989.
Snyder, D. S.; Unanue, E. R. Corticosteroids inhibit murine macrophage Ia expression and interleukin q production. J. Immunol.
129:1803-1865; 1982.
Steinberg, E. M. Monokines, lymphokines, and the brain. In:
Cruse, J. M.; Lewis, R. E., eds. The year in immunology 1988:
Vol. 5. Immunoregulatory cytokines and cell growth. Basel: Karger;
1988:205-217.
195. Steinberg, E. M.; Hill, J. M.; Chrousos, G. P.; Kamilaris, T.;
Listwack, S. J.; Gold, P. W.; Wilder, R. Inflammatory mediatorinduced hypothalamic-pituitary-adrenal axis activation is defective
in streptococcal cell wall arthritis-susceptible Lewis rats. Proc.
Natl. Acad. Sci. USA 86:2374.-2378; 1989.
196. Sternberg, E. M.; Young, W. S.; Bernardini, R.; Calogero, A. E.;
Chrousos, G. P.; Gold, P. W.; Wilder, R. L. A central nervous
system defect in biosynthesis of corticotropin-releasing hormone is
associated with susceptibility to streptococcal cell wall-induced arthritis in Lewis rats. Proc. Natl. Acad. Sci. USA 86:4771--4775;
1989.
197. Stone, E. A.; McCarty, R. Tyrosine hydroxylase activity and catecholamine release. Neurosci. Biobehav. Rev. 7:29-34; 1983.
198. Stock, G.; Rupprecht, U.; Strumf, H.; Schlor, H. Cardiovascular
changes during arousal elicited by stimulation of amygdala, hypothalamus and locus cernleus. J. Auton. Nerv. Syst. 3:503-510;
1981.
199. Suda, T.; Tomori, N.; Tozawa, F.; Demura, H.; Shizume, K.;
Mouri, T.; Miura, Y.; Sasaro, N. lmmunoreactive corticotropin
and corticotropin-releasing factor in human hypothalamus, adrenal,
lung cancer and phenechromocytoma. J. Clin. Endocrinol. Metab.
58:919-924; 1984.
200. Suomi, S. Genetic and maternal contributions to individual differences in rhesus monkey biobehavioral development. In: Krasnegor,
N.; Blass, E.; Hofer, M.; Smotherman, W., eds. Perinatal devel-
130
201.
202.
203.
204.
205.
206.
207.
208.
209.
JOHNSON,
opment: A psychobiological perspective. New York: Academic
Press; 1987: 397--419.
Suomi, S. J.; Kraemer, G. W.; Baysinger, C. M.; Delizio, R. D.
Inherited and experiential factors in anxious behavior displayed by
rhesus monkeys. In: Klein, D. F.; Rabkin, J., eds. Anxiety: New
research and changing concepts. New York: Raven; 1981:179-200.
Sutton, R. E.; Kooh, G. F.; Le Moal, M.; Rivier, J.; Vale, W.
Corticotropin releasing factor (CRF) produces behavioural activation in rats. Nature 297:331-333; 1982.
Szemeredi, K.; Bagdy, G.; Stull, R.; Calogero, A. E.; Kopin, I.
J.; Goldstein, D. S. Sympathoadrenalmedullary inhibition by chronic
glucocorticoid treatment in conscious rats. Endocrinology 123:
2585-2590; 1988.
Terman, G.; Shavit, Y.; Lewis, J.; Cannon, J.; Liebeskind, J. Intrinsic mechanisms of pain inhibition: Activation by stress. Science
226:1270-1277; 1984.
Tilders, F. J. H.; Berkenbosch, F. CRF and catecholamines; Their
place in the central and peripheral regulation of the stress response.
Acta Endocrinol. (Suppl. 1 (Copenh.) 276:63-75; 1986.
Udelsman, R.; Goldstein, D. S.; Loriaus, D. L.; Chrousos, G. P.
Catecholamine-glucocorticoid interactions during surgical stress. J.
Surg. Res. 43:539; 1987.
Vale, W.; Spiess, J.; Rivier, C.; Rivier, J. Characterization of a
41 residue ovine hypothalamic peptide that stimulates the secretion
of corticotropin and 13-endorphin. Science 213:1394-1397; 1981.
Valentino, R. J.; Cha, C. I.; Foote, S. L. Anatomic and physiologic evidence for innervation of noradrenergic locus coeruleus by
neuronal corticotropin-releasing factor. Soc. Neurosci. Abstr. 12:
1003; 1986.
Valentino, R. J. CRH effects on central noradrenergic neurons:
Relationship to stress. In: Chrousos, G. P.; Loriaux, D. L.; Gold,
P. W., eds. Mechanisms of physical and emotional stress. Advances in experimental medicine and biology, vol. 245. New York:
Plenum Press; 1988:47-64.
KAMILARIS,
CHROUSOS
AND GOLD
210. Van Liessum, P. A.; Swinkels, L. M.; Pieters, G. F.; Ross, A.
A.; Smals, A. G.; Benraad, T. J.; Kloppenborg, P. W. Lack of
antibody formation during long-term subcutaneous treatment with
the somatostatin analogue octreotide in acromegaly. Acta Endocrinol. (Copenh.) 122:309-312; 1990.
211. Vreeburg, J. T. M.; De Greef, W. J.; Ooms, M. P.; Van Wouw,
P.; Weber, R. F. A. Effects of adrenocorticotropin and corticosterone on the negative feedback action of testosterone in the adult
male rat. Endocrinology 115(3):977-983; 1984.
212. Weigent, D. A.; Blalock, J. E. Interactions between the neuroendocrine and immune systems: Common hormones and receptors.
Immunol. Rev. 100:79-10g; 1987.
213. Weiss, J. M.; Stone, E. A.; Hanell, N. Coping behavior and brain
norepinephrine levels in rats. J. Comp. Physiol. Psychol. 72:153160; 1970.
214. Weiss, J. M.; Goodman, P. A.; Losito, B. G.; Corrigan, S.;
Chatty, J. M.; Baily, W. H. Behavioral depression produced by
an uncontrollable stressor: Relationship to norepinephrine, dopamine and serotonin levels in various regions of rat brain. Brain
Res. Rev. 3:167-205; 1981.
215. Winokur, G.; Pfohl, B.; Sherman, B. The relationships of historically defined subtypes of depression to ACTH and cortisol levels
in depression: Preliminary study. Biol. Psychiata-y 20:751-757;
1985.
216. Woloski, B. R. M. N. J.; Smith, E. M.; Mejer, W. J. III; Fuler,
G. M.; Blalock, J. E. Corticotropin releasing activity of monokines. Science 230:1035-1037; 1985.
217. Wynn, P. C.; Jarqood, J. P.; Cart, K. J.; Aguilera, G. Regulation
of corticotropin-releasing factor (CRF) receptors with the rat pituitary gland: Effect of adrenaiectomy on CRF receptors and corticotroph responses. Endocrinology 116:1653-1659; 1985.
218. Yates, E.; Marsh, D.; Maran, J. The adrenal cortex. In: Mountcastle, V., ed. Medical physiology, 14th ed. St. Louis: C. V.
Mosby; 1980:1558-1601.
Das könnte Ihnen auch gefallen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (894)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (587)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (119)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2219)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Osprey, Men-at-Arms #246 The Romanian of Army World War 2 (1991) OCR 8.12 PDFDokument48 SeitenOsprey, Men-at-Arms #246 The Romanian of Army World War 2 (1991) OCR 8.12 PDFGabriel Ionescu100% (2)
- Osprey, Men-at-Arms #246 The Romanian of Army World War 2 (1991) OCR 8.12 PDFDokument48 SeitenOsprey, Men-at-Arms #246 The Romanian of Army World War 2 (1991) OCR 8.12 PDFGabriel Ionescu100% (2)
- Topnotch Surgery Reviewer PDFDokument81 SeitenTopnotch Surgery Reviewer PDFkat0% (1)
- Secrets of Korean MedicineDokument70 SeitenSecrets of Korean Medicineemedronho4550100% (3)
- Stress DisordersDokument1 SeiteStress DisordersGabriel IonescuNoch keine Bewertungen
- Of Mice and EthicsDokument4 SeitenOf Mice and EthicsGabriel IonescuNoch keine Bewertungen
- Viral Hepatitis - Selected Issues of Pathogenesis and DiagnosticsDokument162 SeitenViral Hepatitis - Selected Issues of Pathogenesis and DiagnosticsGabriel IonescuNoch keine Bewertungen
- 2010 Vol5 (8) No4 pg265-270Dokument6 Seiten2010 Vol5 (8) No4 pg265-270Gabriel IonescuNoch keine Bewertungen
- Mollecular Hepatic Stellate Cells Targets inDokument14 SeitenMollecular Hepatic Stellate Cells Targets inGabriel IonescuNoch keine Bewertungen
- InTech-Evolution of Viral Hepatitis Role of Psychosocial StressDokument10 SeitenInTech-Evolution of Viral Hepatitis Role of Psychosocial StressGabriel IonescuNoch keine Bewertungen
- Articol Lipide Serice Publicat PDFDokument3 SeitenArticol Lipide Serice Publicat PDFGabriel IonescuNoch keine Bewertungen
- 11 1 08 Ionescu PDFDokument5 Seiten11 1 08 Ionescu PDFGabriel IonescuNoch keine Bewertungen
- CHSJ 2012.2.5Dokument5 SeitenCHSJ 2012.2.5Gabriel IonescuNoch keine Bewertungen
- New Techniques in Gastrointestinal Endos PDFDokument322 SeitenNew Techniques in Gastrointestinal Endos PDFGabriel Ionescu100% (2)
- Rabeprazole Combined With Hydrotalcite Is Effective For Patients With Bile Reflux Gastritis After CholecystectomyDokument5 SeitenRabeprazole Combined With Hydrotalcite Is Effective For Patients With Bile Reflux Gastritis After CholecystectomyGabriel IonescuNoch keine Bewertungen
- Statins in The Treatment of Hepatitis CDokument3 SeitenStatins in The Treatment of Hepatitis CGabriel IonescuNoch keine Bewertungen
- 11 1 08 Ionescu PDFDokument5 Seiten11 1 08 Ionescu PDFGabriel IonescuNoch keine Bewertungen
- WJH 6 137Dokument8 SeitenWJH 6 137Gabriel IonescuNoch keine Bewertungen
- Mollecular Hepatic Stellate Cells Targets inDokument14 SeitenMollecular Hepatic Stellate Cells Targets inGabriel IonescuNoch keine Bewertungen
- 2161 069X S12 006Dokument6 Seiten2161 069X S12 006Gabriel IonescuNoch keine Bewertungen
- Viral Hepatitis - Selected Issues of Pathogenesis and DiagnosticsDokument162 SeitenViral Hepatitis - Selected Issues of Pathogenesis and DiagnosticsGabriel IonescuNoch keine Bewertungen
- InTech-Evolution of Viral Hepatitis Role of Psychosocial StressDokument10 SeitenInTech-Evolution of Viral Hepatitis Role of Psychosocial StressGabriel IonescuNoch keine Bewertungen
- 2980Dokument7 Seiten2980Gabriel IonescuNoch keine Bewertungen
- Reglare CSHDokument18 SeitenReglare CSHGabriel IonescuNoch keine Bewertungen
- Chir RosisDokument6 SeitenChir RosisGabriel IonescuNoch keine Bewertungen
- Leziuni Hepatice FocaleDokument4 SeitenLeziuni Hepatice FocaleGabriel IonescuNoch keine Bewertungen
- Fractal Analysis Differentiation of Nuclear and Vascular Patterns in Hepatocellular Carcinomas and Hepatic MetastasisDokument10 SeitenFractal Analysis Differentiation of Nuclear and Vascular Patterns in Hepatocellular Carcinomas and Hepatic MetastasisGabriel IonescuNoch keine Bewertungen
- Statins in The Treatment of Hepatitis CDokument3 SeitenStatins in The Treatment of Hepatitis CGabriel IonescuNoch keine Bewertungen
- Fatigue in Liver DiseaseDokument8 SeitenFatigue in Liver DiseaseGabriel IonescuNoch keine Bewertungen
- 2161 069X S12 006Dokument6 Seiten2161 069X S12 006Gabriel IonescuNoch keine Bewertungen
- Of Mice and EthicsDokument4 SeitenOf Mice and EthicsGabriel IonescuNoch keine Bewertungen
- Bourke Harrell Neigh 2012 Stress GlucocorticoidsDokument20 SeitenBourke Harrell Neigh 2012 Stress GlucocorticoidsConstanceNoch keine Bewertungen
- Kaplan All SubjectsDokument8 SeitenKaplan All Subjectssarmad_bayatliNoch keine Bewertungen
- Name: Ellaine Jhane T. Domede Bsn1VDokument9 SeitenName: Ellaine Jhane T. Domede Bsn1VNeil Floyd VenturaNoch keine Bewertungen
- Kerangka Konsep PenelitianDokument29 SeitenKerangka Konsep PenelitianGabriel KlemensNoch keine Bewertungen
- 1.endocrine and Metabolic Response To TraumaDokument35 Seiten1.endocrine and Metabolic Response To TraumaDenise JohnsonNoch keine Bewertungen
- Dr. Rishi Pal: Asstt. ProfessorDokument40 SeitenDr. Rishi Pal: Asstt. ProfessortamaNoch keine Bewertungen
- Side Effects of Drugs - Annual 33 - J. Aronson (Elsevier, 2011) WWDokument1.122 SeitenSide Effects of Drugs - Annual 33 - J. Aronson (Elsevier, 2011) WWAndrei E. HawayNoch keine Bewertungen
- Pharmacology in RehabilitationDokument682 SeitenPharmacology in RehabilitationDiana Mesquita100% (1)
- Consideration of Steroids For Endodontic PainDokument11 SeitenConsideration of Steroids For Endodontic PainArturo Trejo VeraNoch keine Bewertungen
- Topic 1 Endocrine SystemDokument140 SeitenTopic 1 Endocrine SystemmasdfgNoch keine Bewertungen
- 2 2015 Nsaid Analgetik AntipiretikaDokument65 Seiten2 2015 Nsaid Analgetik AntipiretikasekarNoch keine Bewertungen
- Effects of Dexamethasone and Low-Level Laser TherapyDokument24 SeitenEffects of Dexamethasone and Low-Level Laser TherapyAbles227 BlessNoch keine Bewertungen
- Glucocorticoid Induced Adrenal Insufficiency Prete2021Dokument20 SeitenGlucocorticoid Induced Adrenal Insufficiency Prete2021Marcos OrtizNoch keine Bewertungen
- Stress and Physiological ResponseDokument11 SeitenStress and Physiological ResponseCampbell BellNoch keine Bewertungen
- Who DrugDokument5.107 SeitenWho DrugShaila ArunNoch keine Bewertungen
- What Steroid Supplementation Is Required For A Patient With Primary Adrenal Insufficiency Undergoing A Dental Procedure?Dokument6 SeitenWhat Steroid Supplementation Is Required For A Patient With Primary Adrenal Insufficiency Undergoing A Dental Procedure?AnthonyNoch keine Bewertungen
- Disorders of AdrenalsDokument8 SeitenDisorders of AdrenalsM.PRASAD NAIDUNoch keine Bewertungen
- Shock Lecture NotesDokument5 SeitenShock Lecture Notescolek22100% (7)
- Drugs Affecting The Respiratory System: Department of Pharmacology Medical Faculty Brawijaya UniversityDokument79 SeitenDrugs Affecting The Respiratory System: Department of Pharmacology Medical Faculty Brawijaya UniversitySatya BimantaraNoch keine Bewertungen
- Sahebkar Panahi 21072017 Proof PDFDokument16 SeitenSahebkar Panahi 21072017 Proof PDFJulius PalmaNoch keine Bewertungen
- Pharm MCQ BookDokument11 SeitenPharm MCQ BookanojanNoch keine Bewertungen
- Top-200-Drug ETSYDokument31 SeitenTop-200-Drug ETSYBetsy Brown ByersmithNoch keine Bewertungen
- Tugas Anestesi Rani RevisiDokument27 SeitenTugas Anestesi Rani RevisiFahrizalNoch keine Bewertungen
- Pathophysiology of Endocrine SystemDokument39 SeitenPathophysiology of Endocrine SystemAhmad Abu Kush100% (1)
- Deborah P Merke, Stefan R Bornstein, Congenital Adrenal HyperplasiaDokument12 SeitenDeborah P Merke, Stefan R Bornstein, Congenital Adrenal HyperplasiaJakub LuszczykNoch keine Bewertungen
- Side Effects of Systemic Corticosteroids in ChildrenDokument6 SeitenSide Effects of Systemic Corticosteroids in ChildrenChamara AtukoralaNoch keine Bewertungen
- Anaemia in Dogs and Cats (Part 2) : Continuing EducationDokument6 SeitenAnaemia in Dogs and Cats (Part 2) : Continuing EducationAchmad NugrohoNoch keine Bewertungen
- Application of Recombinant DNATechnologies On Sub-Cloning of Transcriptional Co-FactorDokument6 SeitenApplication of Recombinant DNATechnologies On Sub-Cloning of Transcriptional Co-FactorInternational Journal of Innovative Science and Research TechnologyNoch keine Bewertungen