Beruflich Dokumente
Kultur Dokumente
Pennsylvania Medicaid Fraud Control Unit
Hochgeladen von
Beverly Tran0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
555 Ansichten2 Seiten1) The document discusses patient neglect and Medicaid fraud, providing contact information for reporting concerns about neglect by caregivers or fraud by medical providers.
2) It defines patient neglect as knowingly failing to provide necessary treatment or care, resulting in injury, and lists indicators such as malnutrition, untreated bedsores, or failure to follow medical orders.
3) Medicaid fraud by providers is described as billing for unnecessary or more expensive services than provided, or billing multiple times for the same service.
Originalbeschreibung:
Pennsylvania Medicaid Fraud Control Unit Brochure
Copyright
© Attribution Non-Commercial (BY-NC)
Verfügbare Formate
PDF, TXT oder online auf Scribd lesen
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument melden1) The document discusses patient neglect and Medicaid fraud, providing contact information for reporting concerns about neglect by caregivers or fraud by medical providers.
2) It defines patient neglect as knowingly failing to provide necessary treatment or care, resulting in injury, and lists indicators such as malnutrition, untreated bedsores, or failure to follow medical orders.
3) Medicaid fraud by providers is described as billing for unnecessary or more expensive services than provided, or billing multiple times for the same service.
Copyright:
Attribution Non-Commercial (BY-NC)
Verfügbare Formate
Als PDF, TXT herunterladen oder online auf Scribd lesen
0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
555 Ansichten2 SeitenPennsylvania Medicaid Fraud Control Unit
Hochgeladen von
Beverly Tran1) The document discusses patient neglect and Medicaid fraud, providing contact information for reporting concerns about neglect by caregivers or fraud by medical providers.
2) It defines patient neglect as knowingly failing to provide necessary treatment or care, resulting in injury, and lists indicators such as malnutrition, untreated bedsores, or failure to follow medical orders.
3) Medicaid fraud by providers is described as billing for unnecessary or more expensive services than provided, or billing multiple times for the same service.
Copyright:
Attribution Non-Commercial (BY-NC)
Verfügbare Formate
Als PDF, TXT herunterladen oder online auf Scribd lesen
Sie sind auf Seite 1von 2
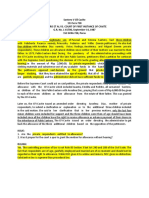
If you suspect that Medicaid Fraud is
PATIENT NEGLECT being committed by a provider, or a care
As the elderly or disabled dependent person you know is suffering
become more and more from patient neglect, write or call:
dependent on others for
their care, it becomes
increasingly important for Office of Attorney General
individuals who accept Medicaid Fraud Control Unit
the position of trust as 1600 Strawberry Square
caretakers of these Harrisburg, PA 17120
vulnerable people to be 717-783-1481
held accountable for neglecting those in their care.
Failure to provide the care and treatment Office of Attorney General
necessary to maintain the welfare of those who Medicaid Fraud Control Unit
depend on that care is every bit as dangerous and 10950 Route 30
harmful as intentional assaultive behavior.
North Huntingdon, PA 15642
Criminal neglect of a care dependent person occurs 724-861-3670
when a caregiver knowingly, intentionally or
recklessly fails to provide treatment, care, goods, Office of Attorney General
or service that is necessary to maintain the health Medicaid Fraud Control Unit
or safety of the care dependent person. The failure 106 Lowther Street
must then result in bodily injury to the care Lemoyne, PA 17043
dependent person. 717-712-1220
Office of Attorney General
INDICATORS OF PATIENT NEGLECT Medicaid Fraud Control Unit
Care dependent persons who are malnourished, 1000 Madison Avenue
dehydrated, or have untreated bedsores. Norristown, PA 19403
610-631-5920
Staff failing to follow doctors’ orders with
regard to treatment of a care dependent
person.
www.attorneygeneral.gov
Failure to seek needed medical treatment for a
care dependent person in a timely manner or
not at all.
Care dependent persons who appear unkempt,
unclean, or disheveled.
In 1978, the MEDICAID FRAUD
Pennsylvania The Medicaid Fraud Control Unit investigates Giving or accepting something of value in return
PROVIDER FRAUD. A provider is any business for providing medical services, i.e. kickbacks.
Office of Attorney or individual that supplies health care goods and
General created a Providing medically unnecessary services.
services to Medicaid recipients. Providers can be
Medicaid Fraud medical doctors, dentists, hospitals, nursing homes, Falsifying cost reports.
Control Unit whose pharmacies, durable medical equipment sellers, Billing for ambulance runs to doctor
purpose was to ambulance companies, or anyone else who bills the appointments.
investigate and Medicaid Program for health care goods and services
provided to a Medicaid recipient. A provider commits In many areas of the Commonwealth, Health
prosecute fraud fraud by giving false information regarding services Maintenance Organizations (HMO’s) have contracted
committed by medical providers rendered to Medicaid recipients. The result is an with the Department of Public Welfare to administer
enrolled in the Medicaid program, as increase in the cost of the Medicaid program, which the Medicaid funded medical services.
well as to investigate patient abuse and eventually will be passed along to the taxpayers.
neglect in Medicaid funded health care
facilities pursuant to the Medicare- EXAMPLES OF MEDICAID FRAUD HEALTH MAINTENANCE
Medicaid Anti-Fraud and Abuse Billing for medical services not actually ORGANIZATIONS (HMO’s)
Amendment of 1977. performed. Although HMO’s can be defrauded by providers in
ways similar to the fraud committed in the traditional
Billing for a more expensive service than fee-for-service setting, HMO’s present unique fraud
The unit is a part of the Office of was actually rendered. issues. Whereas in standard health care
Attorney General’s Criminal Law
Billing for separate services that should be reimbursement situations the fraud is characterized
Division and is comprised of combined into one billing. by overbilling, an HMO environment creates an
prosecutors, agents and auditors incentive to deny care to patients/consumers. This
Billing twice for the same medical service.
housed in three regional offices across means that while a fee has been paid by the HMO to
the Commonwealth. The Medicaid Dispensing generic drugs and billing the provider for covered services, the services are
for brand-name drugs. denied or cut back for other than sound medical
Fraud Control Unit has the authority to
reasons. This not only defrauds the insurance
file felony and misdemeanor charges company, but also compromises patient health.
against those who defraud the
Medicaid program or commit patient
neglect.
Tom Corbett
Attorney General
Das könnte Ihnen auch gefallen
- HIPAA - FW & A ReviewDokument5 SeitenHIPAA - FW & A ReviewGiullz EuguiNoch keine Bewertungen
- ArticleDokument2 SeitenArticletdp01912Noch keine Bewertungen
- TOPICSDokument23 SeitenTOPICSLili GomezNoch keine Bewertungen
- Fraud Asuransi KesehatanDokument9 SeitenFraud Asuransi KesehatanOlivia JosianaNoch keine Bewertungen
- GI CouncilDokument7 SeitenGI CouncilHiten BhanushaliNoch keine Bewertungen
- Medical Billing Terminology and MeaningsDokument7 SeitenMedical Billing Terminology and MeaningsMarynaNoch keine Bewertungen
- Fraud: A Cancer To The Healthcare DomainDokument5 SeitenFraud: A Cancer To The Healthcare DomainSingh RobNoch keine Bewertungen
- Health Care Fraud - Physicians As White Collar CriminalsDokument4 SeitenHealth Care Fraud - Physicians As White Collar Criminalstdp01912Noch keine Bewertungen
- Health Insurance Fraud PresentationDokument10 SeitenHealth Insurance Fraud PresentationAhmed HashmiNoch keine Bewertungen
- 12 - FWA-Common Type of Health Care FraudDokument4 Seiten12 - FWA-Common Type of Health Care FraudRoldan Dela CruzNoch keine Bewertungen
- Newman's Medical Billing and Coding Technicians Study GuideVon EverandNewman's Medical Billing and Coding Technicians Study GuideNoch keine Bewertungen
- FWA Provider Training - Oct 2019Dokument23 SeitenFWA Provider Training - Oct 2019Anushree PawanrajNoch keine Bewertungen
- Billing Definations 7Dokument15 SeitenBilling Definations 7Saeed ahmed100% (2)
- Newman's Billing and Coding Technicians Study GuideVon EverandNewman's Billing and Coding Technicians Study GuideBewertung: 4.5 von 5 Sternen4.5/5 (2)
- Common Medicare and Medicaid Fraud SchemesDokument11 SeitenCommon Medicare and Medicaid Fraud SchemesHemant ShahNoch keine Bewertungen
- Dwnload Full Health Promotion Throughout The Life Span 7th Edition Edelman Test Bank PDFDokument35 SeitenDwnload Full Health Promotion Throughout The Life Span 7th Edition Edelman Test Bank PDFinserve.absolve.q2oxs100% (7)
- Financial Agreement Policy Form PDFDokument2 SeitenFinancial Agreement Policy Form PDFTulika CNoch keine Bewertungen
- Different Modes of Private Health FinancingDokument20 SeitenDifferent Modes of Private Health FinancingHeme globinNoch keine Bewertungen
- 2016 National Training ProgramDokument50 Seiten2016 National Training ProgramTian Njawani100% (1)
- POD Special Fraud AlertDokument4 SeitenPOD Special Fraud AlertMichael KlinskiNoch keine Bewertungen
- Emergency NursingDokument16 SeitenEmergency NursingSwapnil Mahapure100% (2)
- Medical Billing TrainingDokument11 SeitenMedical Billing TrainingHarry Canaba100% (1)
- Fraud in InsuranceDokument54 SeitenFraud in Insurance9220501752Noch keine Bewertungen
- Godwin Ikwuakam and Yannick Pierre ComplaintDokument25 SeitenGodwin Ikwuakam and Yannick Pierre ComplaintEmily BabayNoch keine Bewertungen
- OpinionDokument3 SeitenOpinionAlma CayapNoch keine Bewertungen
- No Surprises Act FAQ 4.22Dokument4 SeitenNo Surprises Act FAQ 4.22Indiana Family to FamilyNoch keine Bewertungen
- Chapter 10: Fraud Management: Certificate in Health InsuranceDokument0 SeitenChapter 10: Fraud Management: Certificate in Health InsuranceJonathon CabreraNoch keine Bewertungen
- Textbook of Urgent Care Management: Chapter 36, Virtual CareVon EverandTextbook of Urgent Care Management: Chapter 36, Virtual CareNoch keine Bewertungen
- HHS OIG - Offshore Outsourcing OEI-09-12-00530Dokument13 SeitenHHS OIG - Offshore Outsourcing OEI-09-12-00530Michael BarbereNoch keine Bewertungen
- Insurance Fraud Detection Hints - Nebraska DPT of InsuranceDokument13 SeitenInsurance Fraud Detection Hints - Nebraska DPT of InsuranceElenaGeorgiadiNoch keine Bewertungen
- US Financial StudyDokument25 SeitenUS Financial StudysandeepNoch keine Bewertungen
- Board Review D3sa - Multiple TopicsDokument55 SeitenBoard Review D3sa - Multiple TopicsMerville HCNoch keine Bewertungen
- Health Care Code of ConductDokument4 SeitenHealth Care Code of ConductSteve Levine100% (2)
- NAHC WhitePaper Value-of-HomeHealthDokument8 SeitenNAHC WhitePaper Value-of-HomeHealthZied JemmeliNoch keine Bewertungen
- Final TPADokument40 SeitenFinal TPAkushal87100% (1)
- Detecting Medical Identity TheftDokument2 SeitenDetecting Medical Identity TheftGeorge F. Indest IIINoch keine Bewertungen
- Leveraging Big Data Analytics To Reduce Healthcare CostsDokument8 SeitenLeveraging Big Data Analytics To Reduce Healthcare Costsgary felderNoch keine Bewertungen
- Health Insurance N TPA by Poonam N Neha BhakerDokument44 SeitenHealth Insurance N TPA by Poonam N Neha Bhakerpoonam@imsNoch keine Bewertungen
- Mission Charity Care Response April 30, 2020Dokument54 SeitenMission Charity Care Response April 30, 2020Jennifer EmertNoch keine Bewertungen
- Health Insurance in KsaDokument9 SeitenHealth Insurance in KsaserlinaNoch keine Bewertungen
- Basics of Medical Billing & CodingDokument86 SeitenBasics of Medical Billing & CodingRic Sánchez100% (3)
- ER Utilization Budget AmendmentDokument2 SeitenER Utilization Budget AmendmentLia PaulineNoch keine Bewertungen
- Assignment 3 - Del MundoDokument5 SeitenAssignment 3 - Del MundoAngel Alexa Del MundoNoch keine Bewertungen
- Medicare Two-Way Claim: Purpose of This Form Private Health Insurance Member's Details 1 2 3 4 5Dokument2 SeitenMedicare Two-Way Claim: Purpose of This Form Private Health Insurance Member's Details 1 2 3 4 5lalidawatermarkNoch keine Bewertungen
- Contemporary Nursing Issues Trends and Management 5th Edition Cherry Test BankDokument39 SeitenContemporary Nursing Issues Trends and Management 5th Edition Cherry Test Bankseeressgroined3djz100% (16)
- HealthConsent CDokument1 SeiteHealthConsent CsakondathabisoNoch keine Bewertungen
- US Healthcare System Analysis v2-0Dokument31 SeitenUS Healthcare System Analysis v2-0Achintya KumarNoch keine Bewertungen
- Lesson Plan Emergency NursingDokument38 SeitenLesson Plan Emergency NursingNanaJaeNoch keine Bewertungen
- Negligence and Medical MalpracticeDokument62 SeitenNegligence and Medical Malpracticesarguss14100% (7)
- Introduction To Health Profile and Healthcare System in TaiwanDokument52 SeitenIntroduction To Health Profile and Healthcare System in TaiwanTaschiro YuliarthaNoch keine Bewertungen
- Asymmetric InformationDokument22 SeitenAsymmetric InformationSmita SinghNoch keine Bewertungen
- Ao2018 0012 PDFDokument11 SeitenAo2018 0012 PDFFlorescinda Mae NapaNoch keine Bewertungen
- Health Promotion Throughout The Life Span 7th Edition Edelman Test BankDokument11 SeitenHealth Promotion Throughout The Life Span 7th Edition Edelman Test BankJosephJohnsonfmixo100% (14)
- Georgetown University Study-Discount Medical Cards Issue Brief by Mila Kofman March2005Dokument16 SeitenGeorgetown University Study-Discount Medical Cards Issue Brief by Mila Kofman March2005Noorullah DanishNoch keine Bewertungen
- Wiggins Abduljaber IndictmentDokument29 SeitenWiggins Abduljaber IndictmentLansingStateJournalNoch keine Bewertungen
- Compliance 2017Dokument5 SeitenCompliance 2017Swisskelly1Noch keine Bewertungen
- 01 - Phil Health Care Providers v. CIRDokument1 Seite01 - Phil Health Care Providers v. CIRperlitainocencioNoch keine Bewertungen
- Healthcare BasicsDokument57 SeitenHealthcare BasicsManickavel Manoharan100% (2)
- 2.6 Negligence & MalpracticeDokument3 Seiten2.6 Negligence & MalpracticeValerie Gonzaga-Carandang100% (1)
- Central Bank Digital Currencies: Foundational Principles and Core FeaturesDokument26 SeitenCentral Bank Digital Currencies: Foundational Principles and Core FeaturesBeverly Tran100% (1)
- Juvenile Law Center - Labeled For Life August 2020Dokument76 SeitenJuvenile Law Center - Labeled For Life August 2020Beverly TranNoch keine Bewertungen
- Michigan Attorney General Clergy Abuse Investigation 705417 7Dokument7 SeitenMichigan Attorney General Clergy Abuse Investigation 705417 7Beverly TranNoch keine Bewertungen
- Protecting Our Democracy Act 2020 Fact SheetDokument3 SeitenProtecting Our Democracy Act 2020 Fact SheetBeverly TranNoch keine Bewertungen
- Michigan Sex Offenders Registration Act (SORA) Second Amended Complaint 62818Dokument47 SeitenMichigan Sex Offenders Registration Act (SORA) Second Amended Complaint 62818Beverly TranNoch keine Bewertungen
- Children's Health Defense v. Facebook Complaint DKT 1-08-17 2020Dokument115 SeitenChildren's Health Defense v. Facebook Complaint DKT 1-08-17 2020Beverly Tran100% (2)
- DOJ CRIPA Request For COVID-19 Nursing Home Death Data Letter To Michigan Governor Gretchen Whitmer 08-26-2020Dokument2 SeitenDOJ CRIPA Request For COVID-19 Nursing Home Death Data Letter To Michigan Governor Gretchen Whitmer 08-26-2020Beverly TranNoch keine Bewertungen
- Yesse Yehudah Indictment - Fulfilling Our Responsibilities Unto Mankind, Also Known As FORUMDokument28 SeitenYesse Yehudah Indictment - Fulfilling Our Responsibilities Unto Mankind, Also Known As FORUMBeverly TranNoch keine Bewertungen
- Mitchell v. Dakota County Social Services Et Al.Dokument23 SeitenMitchell v. Dakota County Social Services Et Al.Beverly TranNoch keine Bewertungen
- Appointment of Jim Jones To San Francisco Housing AuthorityDokument1 SeiteAppointment of Jim Jones To San Francisco Housing AuthorityBeverly TranNoch keine Bewertungen
- Karimi v. Deutsche Bank Aktiengesellschaft Et Al., No. 20-Cv-08978karimi v. Deutsche Bank Aktiengesellschaft Et Al., No. 20-cv-08978Dokument36 SeitenKarimi v. Deutsche Bank Aktiengesellschaft Et Al., No. 20-Cv-08978karimi v. Deutsche Bank Aktiengesellschaft Et Al., No. 20-cv-08978Beverly TranNoch keine Bewertungen
- Amended Complaint in FITE V Huntington National Bank - OhioDokument17 SeitenAmended Complaint in FITE V Huntington National Bank - OhioBeverly TranNoch keine Bewertungen
- Toledo City Council Criminal ComplaintDokument41 SeitenToledo City Council Criminal ComplaintBeverly TranNoch keine Bewertungen
- Michigan Western District Stay On State Supreme Court Response On Whitmer Emergency Powers 061920Dokument7 SeitenMichigan Western District Stay On State Supreme Court Response On Whitmer Emergency Powers 061920Beverly TranNoch keine Bewertungen
- Order of Malta American Association Year of Preparation Formation ProgramDokument17 SeitenOrder of Malta American Association Year of Preparation Formation ProgramBeverly TranNoch keine Bewertungen
- High Court of Australia PELL V THE QUEEN 2020-12-2020-04-07Dokument2 SeitenHigh Court of Australia PELL V THE QUEEN 2020-12-2020-04-07Beverly Tran100% (1)
- 10 1001@jama 2020 4783Dokument8 Seiten10 1001@jama 2020 4783Maria RamosNoch keine Bewertungen
- Caritas Pro Vitae Gradu TrustDokument4 SeitenCaritas Pro Vitae Gradu TrustBeverly TranNoch keine Bewertungen
- Connecticut Attorney General Legal Opinion Letter On Religious Exemption On Immunizatoins 5-6-2019Dokument7 SeitenConnecticut Attorney General Legal Opinion Letter On Religious Exemption On Immunizatoins 5-6-2019Beverly TranNoch keine Bewertungen
- National Bank of Pakistan: Karachi (South) RegionDokument6 SeitenNational Bank of Pakistan: Karachi (South) RegionAMIR4263Noch keine Bewertungen
- A.C. Muthiah v. Board of Control For Cricket in India, (2011) 6 SCC 617Dokument1 SeiteA.C. Muthiah v. Board of Control For Cricket in India, (2011) 6 SCC 617kajkargroupNoch keine Bewertungen
- People v. Yanson-DumancasDokument20 SeitenPeople v. Yanson-DumancasBea MarañonNoch keine Bewertungen
- Rime AW: Crimes Criminals Crime Verbs Crime CollocationsDokument5 SeitenRime AW: Crimes Criminals Crime Verbs Crime CollocationsDanielNoch keine Bewertungen
- 7) Shangri-La v. Developers Group Case DigestDokument2 Seiten7) Shangri-La v. Developers Group Case DigestIvan Dizon100% (1)
- Ibanez Vs PeopleDokument2 SeitenIbanez Vs PeopleEgo sum pulcher0% (1)
- Data Privacy ActDokument3 SeitenData Privacy ActsofiaqueenNoch keine Bewertungen
- 100) Coastal Subic Bay Terminal, Inc. v. Department of Labor and Employment - Office of The Secretary, 537 Phil. 459 (2006)Dokument3 Seiten100) Coastal Subic Bay Terminal, Inc. v. Department of Labor and Employment - Office of The Secretary, 537 Phil. 459 (2006)Daniela SandraNoch keine Bewertungen
- CHAPTER 1: Concept and Measurement of Development: Economic Growth Vs Economic DevelopmentDokument20 SeitenCHAPTER 1: Concept and Measurement of Development: Economic Growth Vs Economic DevelopmentAaron Justin Panganiban ArellanoNoch keine Bewertungen
- Module 4Dokument6 SeitenModule 4Phebjoszelle Cdl Jvr LibreNoch keine Bewertungen
- A Study of Environmental Dispute ResolutionDokument16 SeitenA Study of Environmental Dispute ResolutionPriyamvada YadavNoch keine Bewertungen
- 2023 Edelman Trust Barometer Global Report - 0Dokument71 Seiten2023 Edelman Trust Barometer Global Report - 0DavidNoch keine Bewertungen
- Cases On Consent Assault, CF N Hurt, GriveousDokument3 SeitenCases On Consent Assault, CF N Hurt, GriveousafiqahNoch keine Bewertungen
- Philippine Identification System: Syrill S. Cayetano AisamDokument1 SeitePhilippine Identification System: Syrill S. Cayetano AisamSai RillNoch keine Bewertungen
- Russian Rev Lesson Plan 5Dokument4 SeitenRussian Rev Lesson Plan 5api-268737485Noch keine Bewertungen
- Attendance-1 Feb 2023 To 16 Mar 2023Dokument10 SeitenAttendance-1 Feb 2023 To 16 Mar 2023Ayank NaritaNoch keine Bewertungen
- Power CommercialDokument8 SeitenPower CommercialRose Ann LascuñaNoch keine Bewertungen
- SPA SampleDokument2 SeitenSPA Samplecathy cardozaNoch keine Bewertungen
- Short Texts On MasculinityDokument6 SeitenShort Texts On Masculinityapi-522679657Noch keine Bewertungen
- Booking Number: FV86EA: PassengerDokument1 SeiteBooking Number: FV86EA: PassengerLe Cam NhanNoch keine Bewertungen
- PB NQZ K0 TACsopc DZ LW EKUEPf I6 A QRLVD OKWE4 VZKDokument91 SeitenPB NQZ K0 TACsopc DZ LW EKUEPf I6 A QRLVD OKWE4 VZKMuhammad Anees YousafNoch keine Bewertungen
- UCP - OBLICON - Obligations Part 1Dokument3 SeitenUCP - OBLICON - Obligations Part 1Joshua Umali100% (1)
- Introduction To Open InnovationDokument7 SeitenIntroduction To Open InnovationShivam PatelNoch keine Bewertungen
- Santero V CFIDokument1 SeiteSantero V CFICaroline A. LegaspinoNoch keine Bewertungen
- World Current Affairs Mcqs For NTS TEST, FPSC TEST and PMS CSSDokument3 SeitenWorld Current Affairs Mcqs For NTS TEST, FPSC TEST and PMS CSSYasin CNoch keine Bewertungen
- Public Corporation Case DistributionDokument38 SeitenPublic Corporation Case DistributionRESUELLO DIVINA MAENoch keine Bewertungen
- SS12, SS13, SS14, SS15, SS16: Vishay General SemiconductorDokument5 SeitenSS12, SS13, SS14, SS15, SS16: Vishay General SemiconductorRiiandaArifSNoch keine Bewertungen
- United States District Court For The District of ColumbiaDokument4 SeitenUnited States District Court For The District of ColumbiaLaw&CrimeNoch keine Bewertungen
- Invoice 2260, 2261, 2262Dokument4 SeitenInvoice 2260, 2261, 2262miroljubNoch keine Bewertungen
- 2023-09-14 Proposed (DCKT 496 - 0)Dokument3 Seiten2023-09-14 Proposed (DCKT 496 - 0)TélamNoch keine Bewertungen