Beruflich Dokumente
Kultur Dokumente
Pathway Stemi
Hochgeladen von
Intan Nurulita SariCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Pathway Stemi
Hochgeladen von
Intan Nurulita SariCopyright:
Verfügbare Formate
The State of Queensland (Queensland Health) 2012 Contact CIM@health.qld.gov.
au
(Affix identification label here)
URN:
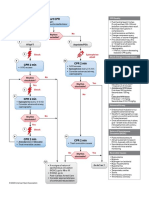
STEMI Management Plan
Family name:
ST-Elevation Myocardial Infarction
For Non-Interventional Cardiac Facilities
Given name(s):
Address:
Facility:
Date of birth:
Sex:
Clinical pathways never replace clinical judgement; Care outlined in this plan must be altered if it is not clinically appropriate for the individual patient
This management plan must be used for patients that present with ST-elevation Acute Myocardial Infarction (STEMI)
following risk stratification in the Cardiac Chest Pain Risk Stratification Pathway
Assign an individual antithrombotic regimen. Management decisions must take into consideration
the balance between ischaemic and bleeding risk for the individual patient 1
(i.e. for patients with a high ischaemic risk and a low bleeding risk, assign an intensive antithrombotic therapy or
for patients with a high risk of bleeding, assign a less intensive antithrombotic therapy)
Emergency presentation date:
time:
Onset of chest pain
time:
date:
Initial Assessment / Management Prior to Reperfusion (Tick as achieved. Record variance in patient record.)
a. If symptom onset is less than 1 hour prior to presentation then consider transfer for immediate Percutaneous
Coronary Intervention (PCI) within 60 minutes.
b. If symptom onset is 112 hours prior to presentation then consider transfer for immediate PCI within 90 minutes.
c. If patient cannot be transferred for PCI within the above timeframes, consider thrombolysis within 30 minutes.
Do Not Write in this binding margin
Reperfusion Guidelines
Persistent ST-elevation
Persistent ST-elevation
1mm in 2 contiguous limb leads (II, III, aVF / I, aVL)
2mm in 2 contiguous chest leads (V1 - V6) Persistent ST-elevation < above may represent transmural
New (or presumed new) left bundle branch block Reperfusion therapy is not routinely recommended in late presentation patients
ischaemia or pericarditis and should be considered for further investigation, including early angiography
who are asymptomatic and haemodynamically stable (ie.
12 hrs after symptom onset).
Time
Initials
Time
Initials
ECG and right-sided ECG (V4R) if inferior MI on arrival, MO review within 10 mins
Referral completed for urgent Cardiology/Medicine review
Check aspirin, 300mg administered as per MO orders, unless contraindicated or already given.
Clopidogrel 300mg to 600mg administered unless contraindicated (or consider alternative)
Cardiology Review / Management
If cathlab not available for PCI within timeframes, consider thrombolysis.
See contraindications below.
Thrombolysis contraindicated, transfer arranged for immediate PCI Omit subcut anticoagulation (consider IV anticoagulation)
Patient suitable for thrombolysis:
Informed consent obtained
Thrombolysis administered and IV Enoxaparin 30mg loading dose administered
Thrombolysis successful
Thrombolysis unsuccessful at 90mins
Mat. No.: 10217516
SW043a
SW043aV
v7.00 - 03/2012
Contraindications for Thrombolysis
Absolute:
Active bleeding or bleeding diathesis (excluding
menses)
Significant closed head or facial trauma within
3months
Patient admitted to Cardiac Monitored Unit
Referred immediatelyangiography recommended within 48 hours
Referred immediately for emergency rescue PCI
Y N
Suspected aortic dissection
Any prior intracranial haemorrhage
Ischaemic stroke within 3 months
Known structural cerebral vascular lesion
Known malignant intracranial neoplasm
Management Post-Thrombolysis
Frequent observations TPR, BP, HS, BS, SaO2, circulation
and neurological observations as per MO order
ECGs must be taken at 90 mins, 6 hours and 12 hours
Relative:
Current use of anticoagulation
Full dose GP IIb/IIIa inhibitors with fibrinolytic therapy, particularly in the elderly
Noncompressible vascular punctures
Traumatic or prolonged ( 10 min) CPR
Ischaemic stroke 3 months ago, dementia or known intracranial abnormality
(not covered in absolute contraindications)
Severe uncontrolled or chronic hypertension
Recent major surgery ( 3 weeks)
Recent internal bleeding (within 4 weeks)
Advanced metastatic cancer
Active peptic ulcer
Pregnancy
Reduction (greater than 50%) in ST
segments expected within 90mins
Continuous cardiac monitoring
Relief of symptoms expected
Haemodynamic stability achieved
If no resolution consider transfer for PCI
Signature Log (Every person documenting in this management plan must supply a sample of their initials and signature below)
Initials
Signature
Print name
Role
Initials
Signature
Y N
Print name
Role
STEMI Management Plan Non-Interventional
Continuous cardiac monitoring, ECGs as per management plan
Frequent observations temperature, pulse, resps (TPR), rhythm check, BP, heart sounds (HS), breath sounds (BS),
SaO2, circulation and neurological observations as ordered, O2 6L/min via HM if indicated (SaO2 < 93% or evidence of
shock)
Keep patient nil by mouth
ECG at 90 mins, 6 hrs and 12 hrs post thrombolysis
Repeat ECG with pain or clinical deterioration
Follow post thrombolysis protocol, then if stable Q4H (or as per
MO order*) TPR, BP, heart sounds (HS) and breath sounds (BS),
SaO2, rhythm check, circulation and pain assessment. Neurological
observations post-thrombolysis.
Assess for resolution of chest pain and for recurrent chest pain
TnI, ELFT, FBC, COAGS and BGL on arrival, TnI repeated 68hrs
TnI, ELFT, FBC, TFT, 8hr fasting lipids and glucose next AM
Ensure patent IVC resite if necessary
Fluid balance chart commenced and patient baseline weight if
possible
Complete nursing history, Waterlow, no lift and falls
Schedule echocardiogram and chest X-ray
If signs of recurrent infarction consider emergency PCI
Daily ECG with review by MO
4 hrly obs if stable; TPR, BP, BS, HS, SaO2, rhythm check, circulation
Assess, manage and report chest pain
Bloods as ordered by MO
Daily weight and/or fluid balance chart if indicated
Review suitability for discharge with appropriate discharge planning
Daily ECG with review by MO. Bloods as ordered by MO
QID or BD if stable; TPR, BP, BS, HS, SaO2, rhythm check, circulation
Assess, manage and report chest pain
Daily weight and/or fluid balance chart if indicated
Review suitability for discharge with appropriate discharge planning
ECG with pain or clinical deterioration with review by MO.
Bloods as ordered by MO
BD/QID obs if stable; TPR, BP, BS, HS, SaO2, rhythm check,
circulation
Assess, manage and report chest pain
Daily weight and/or fluid balance chart if indicated
Review suitability for discharge with appropriate discharge planning
ECGs PRN and on day of discharge with MO review.
Bloods as ordered by MO
BD/QID observations if stable; TPR, BP, SaO2
Assess, manage and report chest pain
Daily weight and/or fluid balance chart if indicated
ECG and right-sided ECG (V4R) if inferior MI on arrival, MO review
within 10 mins
Continuous observations including neurological
Continuous cardiac monitoring (ST segments if available)
Insert IVC 2
Assessment / Investigations
If invasive intervention imminent consider IV Heparin rather than subcut Enoxaparin
For Enoxaparin dosing, calculate creatinine clearance (CrCl) using the CrCl Calculator
(http://medicationdosingcalculators.health.qld.gov.au) and follow Dosing and Monitoring
Guidelines.
In brief: If CrCl < 30 mL/min use IV Heparin (or alternative)
If CrCl 30 to 50 mL/min use IV Heparin (or alternative) or subcut Enoxaparin. If
Enoxaparin is to be used beyond 48 hours, anti-factor Xa should be monitored
according to the Guidelines
If CrCl > 50 mL/min use subcut Enoxaparin
Review need for monitoring
Mobilise independently if able
Medications reviewed by MO, review need for
anticoagulation
Remove IVC if appropriate
Discharge medications; ACE inhibitors, Aspirin, beta
blockers, Clopidogrel (or alternative), statins, Glyceryl
Trinitrate and reviewed medications
As required, travel forms/medical certificate
Patient given discharge summary and one sent to GP
Patient to book visit to GP within 1 week of discharge
For Cardiology OPD 1 month post discharge. Consider
appointments with Physician/Heart Failure service
Telemetry commenced if appropriate
Medications reviewed by MO, review need for anticoagulation
Increase ambulation around unit
Review for suitability for transfer to cardiology ward
Ensure patent IVC resite every 48hrs
Continuous cardiac monitoring
Medications reviewed by MO, review need for anticoagulation
Mobilise minimally with supervision for hygiene
Review for suitability for transfer to cardiology ward
Ensure patent IVC resite if necessary
Continue with discharge planning
Communicate with patient and NOK
Patient attends group session
Outstanding discharge requirements identified
Patient educated on new medication, angina
management, home management and plan for
prolonged chest pain
Continue with cardiac rehab
Discharge planning reviewed
Patient informed on plan of care. Reinforce
AMI, diagnostic procedures and risk factors
specifically smoking cessation strategies
ALERTS: If renal function is unstable,
calculated CrCl is unreliable - use IV
Heparin (or alternative). High bleeding
risk in elderly with low body weight consider IV Heparin (or alternative).
Commence discharge planning
Refer to allied health staff as necessary
including cardiac rehab and physio
Communicate with patient and NOK on
treatment plan
Give My Heart My Life book or similar
Offer basic explanation of AMI, diagnostic
procedures, risk factors and social supports
Explanation of condition and treatment
Reassure patient
Communicate with Next of Kin (NOK)
Rehabilitation / Education
Inpatient cardiac rehab reviews; cardiac rehab/physio
Reinforce chest pain management with patient and NOK
Given written and personalised risk factor control information (smoking,
nutrition, diabetes, stress management, high blood pressure and
cholesterol)
Attended Healthy Eating education session (if No, refer to community
health or outpatient group session)
Review with patient and carer; current status, disease process, diagnostic
and therapeutic options and general prognosis. Review driving/
commercial/pilot licensing
Review resumption of lifestyle activities and return to work
Complete cardiac rehab OPD referral
Written information given on Consumer Medicines Information and
Discharge Medication Record (DMR)
Refer immediatelyangiography recommended within 48 hours
Anticoagulation:
Continuous cardiac monitoring (ST segments if available)
Strict rest in bed for 12 hrs post STEMI (1224 hours post successful thrombolysis, patient may
go to toilet on wheelchair with telemetry [must be supervised], provided they are pain free, and
off inotropic and oxygen therapy)
Medications charted by MO including aspirin, Clopidogrel (or alternative), beta blockers, ACE
inhibitors, statins, nitrates and consider GP IIb/IIIa inhibitors
For diabetics cease Metformin, use insulin for glycaemic control
Reperfusion
Administer thrombolysis and IV Enoxaparin 30mg loading dose unless contraindicated
If thrombolysis contraindicated, transfer to interventional cardiac facility for PCI
If reperfusion is unsuccessful at 90mins, arrange emergency transfer for PCI
For patients with right ventricular involvement, seek cardiologist advice
Ensure adequate pain relief
Management
Additional reading: Chew P, Aroney C, Aylward P et al. 2011 Addendum... Guidelines for the Management of Acute Coronary Syndromes (ACS) 2006. Heart, Lung and Circulation 2011; 20:487-502
97 hours to 7396 hours
discharge
4972
hours
2548 hours
024 hours
090
minutes
STEMI Management Plan
DO not write in this binding margin
Das könnte Ihnen auch gefallen
- Pre-Op Assessment: Dr. Ayesha Ehsan House Surgeon S-IIDokument25 SeitenPre-Op Assessment: Dr. Ayesha Ehsan House Surgeon S-IIFatima MNoch keine Bewertungen
- Stroke Clinical PathwayDokument35 SeitenStroke Clinical PathwayLaurencia Leny100% (2)
- ICU Scoring Systems A Complete Guide - 2020 EditionVon EverandICU Scoring Systems A Complete Guide - 2020 EditionNoch keine Bewertungen
- A Simple Guide to Abdominal Aortic Aneurysm, Diagnosis, Treatment and Related ConditionsVon EverandA Simple Guide to Abdominal Aortic Aneurysm, Diagnosis, Treatment and Related ConditionsNoch keine Bewertungen
- Critical Care SedationVon EverandCritical Care SedationAngelo Raffaele De GaudioNoch keine Bewertungen
- ACLS Suspected Stroke AlgorithmDokument8 SeitenACLS Suspected Stroke AlgorithmBirhane GebreegziabiherNoch keine Bewertungen
- Stemi PathwayDokument12 SeitenStemi PathwaysyifaNoch keine Bewertungen
- Initial Patient Assessment in OpdDokument4 SeitenInitial Patient Assessment in OpdLokender Goyal100% (1)
- Preoperative EvaluationDokument47 SeitenPreoperative EvaluationCzerwin Juales100% (2)
- Standardized Emergency Color CodesDokument1 SeiteStandardized Emergency Color CodesDivya ToppoNoch keine Bewertungen
- Triage First Fast Track Guidelines 2Dokument14 SeitenTriage First Fast Track Guidelines 2Bayu Wirantika0% (1)
- In-Patient Department: Patient Nursing Staff Ratio: RMO'S: 3 - Morning 2 - NightDokument6 SeitenIn-Patient Department: Patient Nursing Staff Ratio: RMO'S: 3 - Morning 2 - NightSiddhi RaneNoch keine Bewertungen
- Toledo Code Blue PolicyDokument4 SeitenToledo Code Blue PolicySt SNoch keine Bewertungen
- Major Haemorrhage ProtocolsDokument3 SeitenMajor Haemorrhage ProtocolsleicesterbugNoch keine Bewertungen
- ATLS-9e Tetanus PDFDokument2 SeitenATLS-9e Tetanus PDFAroell KriboNoch keine Bewertungen
- Emergency Department Intubation ChecklisTDokument2 SeitenEmergency Department Intubation ChecklisTStacey Woods100% (1)
- Preoperative Assessment PolicyDokument10 SeitenPreoperative Assessment PolicymandayogNoch keine Bewertungen
- ACLS Protocols Pocket VersionDokument2 SeitenACLS Protocols Pocket Versionjohndoe1995Noch keine Bewertungen
- 5 Reducing Time To Analgesia in The Emergency Department Using ADokument10 Seiten5 Reducing Time To Analgesia in The Emergency Department Using AMegaHandayaniNoch keine Bewertungen
- Missing Patients ProcedureDokument16 SeitenMissing Patients ProcedureAgnieszka WaligóraNoch keine Bewertungen
- The Who Emergency Care System Framework and Assessment Tool: The Ethiopian Federal Moh ExperienceDokument23 SeitenThe Who Emergency Care System Framework and Assessment Tool: The Ethiopian Federal Moh ExperienceshoriatNoch keine Bewertungen
- Effects of Fast-Track in A University Emergency Department Through The National Emergency Department Overcrowding StudyDokument8 SeitenEffects of Fast-Track in A University Emergency Department Through The National Emergency Department Overcrowding StudyErvin WidhiantyasNoch keine Bewertungen
- Minimum Service Delivery Standards (MSDS) For Hospitals in Sindh ProvinceDokument3 SeitenMinimum Service Delivery Standards (MSDS) For Hospitals in Sindh Provinceimran82aliNoch keine Bewertungen
- 93 - Operating Room ProtocolDokument25 Seiten93 - Operating Room ProtocolFelix Kwenandar100% (1)
- Perioperative Anticoagulation Bridging Guideline PostedDokument6 SeitenPerioperative Anticoagulation Bridging Guideline PostedNuc Alexandru100% (1)
- Definition, Classification, Etiology, and Pathophysiology of Shock in Adults - UpToDateDokument20 SeitenDefinition, Classification, Etiology, and Pathophysiology of Shock in Adults - UpToDateEstructuración Técnica 2019Noch keine Bewertungen
- AR 3 Airway Drug Assisted Intubation Protocol Final 2017 EditableDokument2 SeitenAR 3 Airway Drug Assisted Intubation Protocol Final 2017 EditableAlejandroCabreraBustillo100% (1)
- Integrated Cath Lab Safety ChecklistDokument2 SeitenIntegrated Cath Lab Safety ChecklistwenhalNoch keine Bewertungen
- Transport of Critically Ill PatientsDokument22 SeitenTransport of Critically Ill PatientsFadil RamadhanNoch keine Bewertungen
- Wa0000.Dokument7 SeitenWa0000.benitez1228Noch keine Bewertungen
- Hypertension, Hypertensive Crisis, and Hypertensive Emergency: Approaches To Emergency Department CareDokument11 SeitenHypertension, Hypertensive Crisis, and Hypertensive Emergency: Approaches To Emergency Department CarePebrian SyahNoch keine Bewertungen
- Stroke Clinical PathwayDokument1 SeiteStroke Clinical PathwayKanoknun PisitpatcaragulNoch keine Bewertungen
- Blood Transfusion Single Use PathwayDokument6 SeitenBlood Transfusion Single Use PathwayropusanNoch keine Bewertungen
- Radiology Procedure Manual (AAC 6)Dokument32 SeitenRadiology Procedure Manual (AAC 6)malaramamurthyNoch keine Bewertungen
- AtlsDokument23 SeitenAtlsvivi chanNoch keine Bewertungen
- Arero Primary Hospital Triage ProtocolDokument4 SeitenArero Primary Hospital Triage Protocolsami ketemaNoch keine Bewertungen
- Cardiac EmergencyDokument56 SeitenCardiac Emergency21rayhanf100% (1)
- Anaphylaxis With Angioedema: Section I: Scenario DemographicsDokument7 SeitenAnaphylaxis With Angioedema: Section I: Scenario DemographicsharasthaNoch keine Bewertungen
- Guide To Surgical Site MarkingDokument24 SeitenGuide To Surgical Site MarkingSafiqulatif AbdillahNoch keine Bewertungen
- Modified Early Obstetric Warning Score MEOWS MID33 AO13 v4.2Dokument9 SeitenModified Early Obstetric Warning Score MEOWS MID33 AO13 v4.2indirinoor5Noch keine Bewertungen
- Disaster TriageDokument31 SeitenDisaster Triagekurnia ciptaNoch keine Bewertungen
- Deficiency of Case SheetDokument15 SeitenDeficiency of Case SheetberliyaNoch keine Bewertungen
- National Early Warning Score (NEWS)Dokument47 SeitenNational Early Warning Score (NEWS)Anonymous odb9XJWL0Noch keine Bewertungen
- Algo StrokeDokument2 SeitenAlgo Strokettrriissnnaa100% (1)
- Central Triage ProtocolDokument1 SeiteCentral Triage Protocolgechworkneh38Noch keine Bewertungen
- Flow Chart For Adult Cardio-Pulmonary Resuscitation (Adult CPR)Dokument1 SeiteFlow Chart For Adult Cardio-Pulmonary Resuscitation (Adult CPR)Lia IshakNoch keine Bewertungen
- Module 9 Mechanical Ventilation PDFDokument46 SeitenModule 9 Mechanical Ventilation PDFChabboo SutabrataNoch keine Bewertungen
- Access To Care and Continuity of CareDokument44 SeitenAccess To Care and Continuity of CareCamille Honeyleith Lanuza FernandoNoch keine Bewertungen
- Atls Approach To Pediatric TraumaDokument8 SeitenAtls Approach To Pediatric TraumaMakoto KyogokuNoch keine Bewertungen
- Antrim ED Handbook 2019Dokument238 SeitenAntrim ED Handbook 2019Chris Jardine LiNoch keine Bewertungen
- Preoperative AssessmentDokument9 SeitenPreoperative Assessment1234chocoNoch keine Bewertungen
- Evidence Based Emergency Care PDFDokument2 SeitenEvidence Based Emergency Care PDFMelissa0% (1)
- RECOVER Initiative CPR Reporting Sheet 2020. v3.2Dokument2 SeitenRECOVER Initiative CPR Reporting Sheet 2020. v3.2Mohana Preethi MNoch keine Bewertungen
- Continuous Quality Improvement IndicatorsDokument10 SeitenContinuous Quality Improvement Indicatorsaaminah tariq100% (1)
- Saudi CPR Guidlines in EnglishDokument16 SeitenSaudi CPR Guidlines in EnglishpiyushbamsNoch keine Bewertungen
- Kewal K. Jain - Textbook of Personalized Medicine-Springer (2021)Dokument770 SeitenKewal K. Jain - Textbook of Personalized Medicine-Springer (2021)youssraNoch keine Bewertungen
- Pengaruh Discharge Planning Terhadap Kecemasan Pasien Coronary Artery Desease Di Rs Usu MedanDokument11 SeitenPengaruh Discharge Planning Terhadap Kecemasan Pasien Coronary Artery Desease Di Rs Usu MedanYanis HildaNoch keine Bewertungen
- Diagnostic Criteria of Kawasaki Disease: ND RDDokument1 SeiteDiagnostic Criteria of Kawasaki Disease: ND RDJose Fernando Gregana ElpaNoch keine Bewertungen
- Hypertrophic CardiomyopathyDokument37 SeitenHypertrophic CardiomyopathyMarko Vukovic100% (1)
- Ryujin™ Plus - RX PTCA Balloon Catheter: Product CharacteristicsDokument1 SeiteRyujin™ Plus - RX PTCA Balloon Catheter: Product CharacteristicssunanNoch keine Bewertungen
- VINNO-M86 BrochureDokument6 SeitenVINNO-M86 BrochureMedis MEDISNoch keine Bewertungen
- EKGDokument137 SeitenEKGGbariel100% (3)
- Internal Medicine - CardiologyDokument122 SeitenInternal Medicine - CardiologySoleil Daddou100% (2)
- CardiomyopathyDokument9 SeitenCardiomyopathyMinh Nguyễn Phương HồngNoch keine Bewertungen
- Myocardial Bridges Over Interventricular Branches of Coronary ArteriesDokument4 SeitenMyocardial Bridges Over Interventricular Branches of Coronary Arterieseditorjmst100% (1)
- Cardioversion For Atrial Fibrillation - ClinicalKeyDokument27 SeitenCardioversion For Atrial Fibrillation - ClinicalKeyAnthony Martin Corrales ParedesNoch keine Bewertungen
- Ischemic Heart DiseaseDokument28 SeitenIschemic Heart DiseaseLiusHarimanNoch keine Bewertungen
- Unit 7 Cardiac (S)Dokument78 SeitenUnit 7 Cardiac (S)Cheyenne SchimpfNoch keine Bewertungen
- Common - CardioDokument91 SeitenCommon - CardioHanadi UmhanayNoch keine Bewertungen
- Radiol 223008Dokument15 SeitenRadiol 223008rehan hayderNoch keine Bewertungen
- In Premature Ventricular Complex, An Impulse That Starts in A Ventricle and Is Conducted Through The Ventricles Before The Next Normal SinusDokument7 SeitenIn Premature Ventricular Complex, An Impulse That Starts in A Ventricle and Is Conducted Through The Ventricles Before The Next Normal SinushelloaNoch keine Bewertungen
- Operators Guide Zoll M SeriesDokument96 SeitenOperators Guide Zoll M SeriesAntok JegauNoch keine Bewertungen
- Clinical Practice GuidelinesDokument9 SeitenClinical Practice GuidelinesIntel AtomNoch keine Bewertungen
- Surgery List With CostDokument30 SeitenSurgery List With CostBALAJINoch keine Bewertungen
- Combined Pressure and Flow Measurements To Guide Treatment of Coronary Stenoses PDFDokument10 SeitenCombined Pressure and Flow Measurements To Guide Treatment of Coronary Stenoses PDFIsfan RialdyNoch keine Bewertungen
- A Rare Case of Peripartum CardiomyopathyDokument3 SeitenA Rare Case of Peripartum CardiomyopathyKarina PuspaseruniNoch keine Bewertungen
- Lesson Plan SampleDokument7 SeitenLesson Plan SampleSilvia RajeshNoch keine Bewertungen
- Natriuretic Peptide Measurement in NonDokument2 SeitenNatriuretic Peptide Measurement in NonAde YonataNoch keine Bewertungen
- RUNDOWN West Borneo Cardiovascular Annual Meeting (WeBCAM) 2023Dokument3 SeitenRUNDOWN West Borneo Cardiovascular Annual Meeting (WeBCAM) 2023Bayu Zeva WirasaktiNoch keine Bewertungen
- ValvopatiasDokument97 SeitenValvopatiasapi-3826574Noch keine Bewertungen
- OMI 2018, MirandaDokument14 SeitenOMI 2018, MirandaResidentes UrgenciasNoch keine Bewertungen
- Pericardial Diseases 3rd Yr BMTDokument38 SeitenPericardial Diseases 3rd Yr BMT211941103014100% (1)
- Cardiac Echocardiography Skills ChecklistDokument5 SeitenCardiac Echocardiography Skills Checklistdk15janNoch keine Bewertungen
- DR SC Manchanda - AboutDokument2 SeitenDR SC Manchanda - Aboutbluesaphire09Noch keine Bewertungen
- E.C.G Machine: by Er.U.Karthik Premkumar, H.O.D - Biomedical Engineering DepartmentDokument36 SeitenE.C.G Machine: by Er.U.Karthik Premkumar, H.O.D - Biomedical Engineering DepartmentAch ThungNoch keine Bewertungen