Beruflich Dokumente
Kultur Dokumente
Pain Theories PDF
Hochgeladen von
Andreea-Alexandra LupuOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Pain Theories PDF
Hochgeladen von
Andreea-Alexandra LupuCopyright:
Verfügbare Formate
PAIN: THEORIES AND A NEW
APPROACH TO TREATMENT
Gilbert H. Coffey, MD, and Melvyn V. Mahon, MD
Washington, DC
Various theories of pain are reviewed in an
attempt to understand its mode of action. The
therapeutic effects of a new, noninvasive form
of treating pain, utilizing electrical units which
selectively stimulate the sensory nerves, are
discussed.
Patients with pain of varying degrees of severity and of many different etiologies were
treated with a new form of treatment: transcutaneous electrical nerve stimulation (TENS).
The authors' results have shown this method
to be highly successful in the treatment of patients, most of whom had been treated unsuccessfully with conventional medical and surgical approaches.
TENS affords a new dimension in the current concept of treating pain.
Pain is the most common symptom that causes
patients to seek medical treatment. In their attempt to treat pain with its complexities and various problems, physicians are often forced to recognize that most therapeutic measures used at this
time are inadequate.
Many forms of acute pain have been treated
successfully with medication, surgery, and physical therapy. Chronic pain, however, is difficult to
treat even with additional therapies such as acupuncture, hypnosis, operant conditioning and biofeedback. Physicians, in their attempts to help patients, often add to the patients' disabilities with
This paper was presented at the 85th Annual Convention
and Scientific Assembly of the National Medical Association, Dallas, August 4, 1980. Requests for reprints should be
addressed to Dr. Gilbert H. Coffey, Department of Physical
Medicine and Rehabilitation, 2041 Georgia Avenue, NW,
Washington, DC 20060.
the potential of complications which frequently
have disastrous effects.
This paper has two purposes: first, to discuss
the various theories of pain and to understand
its mechanisms of action and alleviation, especially as it relates to transcutaneous electrical
nerve stimulation (TENS); and second, to report
the authors' evaluation of the treatment of chronic
pain with a newer method, TENS, which is nonhazardous and which offers great promise.
The psychiatrist in an acute medical center is
confronted many times daily with the treatment of
patients with pain symptoms, both acute and
chronic, of varying severities and etiologies. Because of this ready access to patients who were
referred for pain relief when other treatments had
been unsuccessful and because of the desire to
evaluate this new treatment, this study was undertaken.
PAIN THEORIES
To understand the mechanism of pain and its
possible alleviation, five theories are discussed:
specificity, 1.2 pattern,1'2 gate control,"3'4 anodal
blocking and, most recently, central inhibition.2
The specificity theory proposes that a mosaic of
specific pain receptors in body tissue projects to a
main center in the brain." 2 It maintains that free
nerve endings are pain receptors which generate
pain impulses that are carried by A-delta and
C-fibers in peripheral nerves and by the lateral
spinothalamic tract in the spinal cord to a pain
center in the thalamus. This theory, however,
does not explain the inhibition or exaggeration of
pain by emotion or the continued presence of pain
after surgical removal of a body part with its receptors. Calling a nerve receptor a "pain recep-
JOURNAL OF THE NATIONAL MEDICAL ASSOCIATION, VOL. 74, NO. 2, 1982
147
PAIN: THEORIES AND TREATMENT
Central|
Stimulation
Moderate
9eses9.esa m em.s.m..;*
Large Myelinated Fast
Fibers Carrying Light
Touch
00*SS*6*a6Sgggg
Actio .
|System
\
Tett Vibration
Pain
Small Unmyelinated
Slow Fibers
Pain Stimulation
Figure 1. A schematic drawing illustrating the gate-control theory of pain. (From Ersek RA: Low back pain:
Prompt relief with transcutaneous neurostimulation: A report of 35 consecutive patients. Orthoped Rev 5(12):
28, 1976)
tor" implies that stimulation of one type of receptor elicits a single psychological or physiological
response. This has not been borne out clinically,
physiologically, or psychologically.
The pattern theory is based upon the belief that
stimulus intensity and central summation are the
critical determinants of pain.1 2 Related to theories
of central summation is the theory that a specialized input controlling system normally prevents
summation from occurring, and that destruction of
this system leads to pathological pain states. This
theory proposes the existence of a rapidly conducting fiber system which inhibits synaptic
transmission in a more slowly conducting fiber
system that carries the signal for pain. These systems are also identified as epicritic and protopathic, myelinated and unmyelinated, and phylogenetically new and old, respectively. Under
pathological conditions, the slowly conducting
system establishes dominance over the fast with
the result of slow, diffuse, burning pain or hyperalgesia. This theory has been challenged because
it does not explain the existence of specific end
organs.
In 1965, the gate control theory of pain was
148
suggested by Melzack and Wall' on the basis of
physiological evidence on spinal mechanisms
(Figure 1). Evidence demonstrating central control
over afferent input was consistent with concepts
of physiological specialization and central summation of input control. This theory postulates
that three spinal cord constituents are integral to
sensory recognition and modulation: substantia
gelatinosa (SG) cells in the dorsal horn, the central transmission (T) cells in the dorsal horn, and
dorsal column fibers projecting to the brain. The
SG cells act as presynaptic modulators of afferent
patterns before they influence the T cells. These
afferent patterns in the dorsal column act as a central control trigger which activates selective brain
processes influencing the modulating properties of
the gate control system. This results in activation
of neural mechanisms by the branching T cell
which comprises action responsible for perception
and response.
Gate control theory expressed in simplified
form proposes that when pain (C and A-delta) fibers
are stimulated, pain impulses are passed presynaptically in the SG and are transmitted to the
brain, and they will be perceived and will continue
JOURNAL OF THE NATIONAL MEDICAL ASSOCIATION, VOL. 74, NO. 2, 1982
PAIN: THEORIES AND TREATMENT
? THALAMUS
+
p ~~~~~~~?T-CELLS
>~SG
SGs~~~
+
Figure 2. A schematic drawing Illustrating the postsynaptic central inhibitory
balance theory of pain (author's drawing). L=Large fiber, S=Small fiber,
SG=Substantia gelatinosa, SGL=Substantia geltinosa output influenced by
L, SGs=Substantia gelatinosa output influenced by S, P= Projection neuron,
M=Marginal neuron
to be felt as pain as long as the stimulus persists.
Relief of pain is dependent on stimulation of the
large myelinated A-beta fibers which normally
transmit the perceptions of touch and pressure.
A-beta fiber stimulation results in an inhibitory effect setup in the same area of the SG where pain
fibers synapse with a decrease in transmission or
closing the gate to pain. Cessation of large fiber
stimulation would remove the inhibition of pain in
the SG and open the gate to the transmission and
perception of pain.
This theory seems to explain relief of pain by
electrical stimulation of large nerve fibers but does
not rule out the possibility of undetected postsynaptic control mechanisms.
The central inhibition theory3 suggests that
large-fiber and small-fiber activity do not result in
presynaptic effects of opposite polarity as suggested by the gate control theory (Figure 2). The
concept of inhibitory balance depends on minor
inhibitory feedback from small fiber input that activates the nociceptive marginal neuron and major
inhibitory feedback to the marginal neuron from
large non-nociceptive fibers. Modulation of painproducing input thus depends on the balance between large fiber and small fiber activity via a
postsynaptic inhibitory mechanism acting on the
nociceptive relay neurons. This theory satisfactorily accounts for pain modulation by counter irritation and large fiber stimulation.
These last two theories explain not only the effects of electrical stimulation but the effects of the
drug action site in the substantia gelatinosa, the
effects of acupuncture, and the possible accentuation or diminution of pain psychogenically via
feedback via the reticular formation.
The theory of anodal blocking proposes maintaining the absolute refractory period in the nerve
by rapidly and repeatedly stimulating the nerve
fiber, thus preventing pain impulses from being
transmitted. This theory is not accepted because it
does not explain the relief or modulation of pain by
any other means.
Transcutaneous electrical nerve stimulation
(TENS) transmits electrical stimulation cutaneously to the appropriate underlying nerves to prevent the message of pain from reaching the brain.
HISTORY
The basic technique of pain relief through use of
electricity was first reported by Roman and Greek
physicians about 254 AD, when tubs of water filled
with electric fish were used to relieve the pain of
gout, headache, and other etiologies of pain.
It was noticed many years ago that physical
therapy modalities which included muscle stimulation, ie, for peripheral nerve injuries or muscle
pain, resulted in unanticipated pain relief. It was
then thought that other modes of action from the
JOURNAL OF THE NATIONAL MEDICAL ASSOCIATION, VOL. 74, NO. 2, 1982
149
PAIN: THEORIES AND TREATMENT
TABLE 1. ELECTRICAL CHARACTERISTICS OF UNITS USED IN THIS STUDY
Unit Features
Neuromod 3271
Pulse
Rate
0-85 mamp
Width
Wave
50-400 Sec
Exponential
12-100 pulses/sec
PSL GL-106
0-2.0 mamp (peak)
16 cycles/sec; on 75% and off
25% of each cycle imposed
upon a current flow between
20 kHz and 1 MHz
Square
stimulation were present and certain wave forms
effected greater pain relief than others. However,
it was only recently that certain electrical units,
specifically designed to stimulate sensory nerves,
have been utilized exclusively for pain relief.
It is believed that TENS selectively stimulates
and overloads the large sensory fibers, thus relieving pain as postulated by the central inhibitory
and/or gate control theories. Recently, physicians
have administered TENS to patients who have
acute and/or chronic pain which has not been
amenable to conservative therapies for relief by
local anesthesia or analgesia.5 Pain from cancer,
bursitis, ankle sprains, fractured bones, acute
back strain, tic douloureux, ruptured intervertebral disc, phantom limb, causalgia, post-herpetic
and occipital neuralgia, and parturition2,1-0 have
been treated. In addition, present uses of TENS
include reduction of the rate of postoperative atelectasis and ileus. I TENS also has been used as a
screening test to determine patient suitability for
surgical placement of dorsal column stimulators.6
To these indications the authors have added cervical sprain, myofascitis, and tendinitis. TENS
usage is contraindicated in patients with psychogenic and/or psychiatric disturbances, pregnancy,
and pacemakers.
with chronic pain not amenable to conservative
therapies and/or poor surgical risks, and later expanded to include patients with acute pain. All patients had received general medical and physical
medicine examinations along with various tests. An
attempt was made to eliminate suspected malingerers and patients with psychogenic pain syndromes.
EQUIPMENT
APPLICATION
A basic TENS unit is a constant current pulse
generator. Equipment used in this study consisted
of two units, a Medtronic Neuromod 3271 unit
with carbonized rubber electrodes and the PSL
Pain Suppressor GL-106 with carbon-impregnated
foam electrodes. Aquasonic transmission gel with
the Neuromod and H20 with the PSL, and micro-
The negative electrode placement12 for both
units was as follows: soft tissue, over the trigger
point; radiculopathy, along the nerve distribution;
and joint pain, at site of greatest pain or around the
joint. The positive electrode was placed distally to
the negative electrode, or to a corresponding spinal site, or opposite on an extremity or proximal
150
pore surgical tape or velcro straps were used for
electrode conduction and placement. Some characteristics of these units are listed in Table 1.
The Neuromod 3271 has adjustable amplitude,
rate, and pulse width, whereas the PSL unit
has an adjustable amplitude with rate and pulse
width set by the manufacturer. The other striking
difference between the two units is the generated
wave form. The Neuromod wave form is a simple
asymmetrical spike (with exponential decay characteristics); the PSL wave form is a square wave
with a pulsed frequency of 16/sec with 20,000
waves compressed into each cycle. Each cycle is
imposed upon a current flow between 20 kHz and
1 MHz.
METHODS AND PROCEDURES
Patient selection initially was limited to those
JOURNAL OF THE NATIONAL
MEDICAL
ASSOCIATION, VOL. 74, NO. 2, 1982
PAIN: THEORIES AND TREATMENT
when appropriate. Often one has to empirically
place the electrodes in a position for greatest pain
relief especially when no benefit is derived from
the initial treatment. Often an electrode was
placed around an extremity encompassing more
than one major nerve or area supplied by one
nerve. The Neuromod unit is adjusted to patient
tolerance for amplitude, rate, and pulse width and
maintained at this level. The amplitude of the PSL
is adjusted to patient perception, then decreased
to subthreshold sensory perception levels.
The treatment periods varied from one quarter
to one hour. If no pain relief was experienced or if
the treatment caused increased pain after three
sessions, even with various electrode placements,
the treatments were discontinued. The frequency
of treatments was daily, twice daily, or three
times weekly (TIW) depending on the patient's response. Usually the outpatients were treated TIW
or less, depending on the duration or absence or
decrease of pain. The treatment regimen was thoroughly explained to the patient.
Patients were loaned units for use at home and
on weekends. When possible the TENS units were
semi-permanently attached to patients who received relief from their frequent use, enabling
them to carry out their activities of daily living,
function as normally as possible, participate in
their therapy programs, and, in some cases, return
to their jobs. In many instances the need for medications was decreased or eliminated during and
between treatment periods in those who did not
obtain complete relief.
CASE HISTORIES
Case 1
A 50-year-old man had a 15-year history of histamine cluster headaches, often disabling, without
satisfactory response to various medications. He
had several medical workups including computerized axial tomography.
Treatment consisted of one half to one hour
treatment sessions with active electrodes placed
bitemporally and one referrable electrode placed
on the right posterior neck. This patient received
immediate complete relief of his headaches which
lasted up to 24 hours. Treatments were continued
every 24 hours with continued relief.
Case 2
A 48-year-old woman had a six-month history
of a constant nagging pain along the lateral side of
the right leg from below the knee to the ankle.
There were no other symptoms or signs.
Further history indicated that she had been on
anti-tuberculous therapy for longer than nine
months. This patient underwent an extensive
workup including nerve conduction velocities and
electromyography which were reported as normal.
The TENS treatment was with circular electrodes,
the active around the right ankle and the referrable
around the leg just below the knee. The treatment
took approximately 45 minutes. She obtained
complete relief with one treatment without recurrence of pain.
Case 3
A 49-year-old man with T4-level paraplegia of
three years duration, secondary to a fall off a ladder, presented for therapy. He had had severe,
constant pain at the operation site and over the
upper back. The examination was negative for peripheral pain. Tests, including tomography, were
normal for his condition. Surgical intervention was
not indicated; further, the patient did not desire
any surgical procedure. Potent medications were
partially effective.
The TENS treatment consisted of a total of six
electrodes, two placed over the operative site, two
over the upper trapezius, and two on the posterior
neck. The treatments were for one hour periods.
Relief was experienced for 11/2 hours initially, with
increasing pain-free periods with subsequent
treatments. The patient has decreased his medications and can now participate fully in his exercise
maintenance program and a more complete social
life utilizing his wheelchair. He owns a home
TENS unit.
Case 4
This patient, a 39-year-old, markedly obese
woman, had a four-year history of incapacitating
low and mid back pain. She wore a high back
brace, was on potent analgesics, and could not
perform her occupation as a seamstress or sing in
her church choir.
JOURNAL OF THE NATIONAL MEDICAL ASSOCIATION, VOL. 74, NO. 2, 1982
151
PAIN: THEORIES AND TREATMENT
TABLE 2. DIAGNOSES, NUMBER OF PATIENTS, AND THE TYPE OF RELIEF ACHIEVED WITH THE PAIN
SUPPRESSOR UNIT
None
Diagnosis (Number of Patients)
1.
2.
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
16.
17.
Low Back Pain Without Radiculopathy
Low Back Pain with Radiculopathy
S/P Back Surgery with Radiculopathy
Cervical Sprain with Radiculopathy
S/P Surgery: Trigger Finger
Trigger Finger Without Surgery
S/P Surgery: Carpal Tunnel Syndrome
Histamine Cluster Headaches
Chronic Thrombophlebitis
Osteoarthritis, Severe, Both Hips
Disc Disease, Lumbar with Radiculopathy
Peripheral Pain Syndrome Etiology
Sinus Headache, Prolonged
Tension Headache, Severe
Knee Strain, Acute
Paraplegia, Low Cervical Pain
Causalgia, Left Forearm
Total
Pain Relief (Hrs)
Moderate
Complete
<12 >12 >48 <12 >12 >48
(1)
(5)
(3)
(4)
(1)
(1)
(1)
(2)
(1)
(1)
(1)
(1)
(1)
(4)
(1)
(1)
(1)
30
1
1
2
1
1
1
1
1
1
1
1
1
1
1
1*
1
1
4
1
1
1
6
11
*Initial relief-later, pain with treatment
TABLE 3. DIAGNOSES, NUMBER OF PATIENTS, AND THE TYPE OF RELIEF ACHIEVED
WITH THE NEUROMOD UNIT
None
Diagnosis (Number of Patients)
1.
2.
3.
4.
5.
6.
Low Back Pain Without Radiculopathy
Low Back Pain with Radiculopathy
S/P Back Surgery Without Radiculopathy
S/P Back Surgery with Radiculopathy
S/P Sarcoma Thigh with Causalgia
Excision Distal Fibula
Total
(5)
(6)
(0)
(5)
(1)
(1)
(18)
Because of her weight and other medical factors, surgical intervention was not considered
practicable. She was treated with TENS: two
active electrodes over the low back and two referrable electrodes paraspinal in the mid-back region.
Treatment consisted of one hour sessions TIW.
After three treatments she decreased her medications, resumed her seamstress occupation at home
and singing in the church choir. She, also, owns a
home unit.
152
Pain Relief (Hrs)
Moderate
Complete
<12 >12 >48 <12 >12 >48
1
1
2
3
2
1
1
5
1
1
RESULTS
A total of 48 pre-evaluated patients with various
diagnoses and with acute and chronic pain, surgical and nonsurgical, were treated with the PSL
(Table 2) and the Neuromod (Table 3). Thirty-five
female and 13 male patients were treated. Eighty
percent of the patients in this study reported some
relief of pain (Table 4). One patient reported an
increase in pain. All male patients received some
JOURNAL OF THE NATIONAL MEDICAL
ASSOCIATION, VOL. 74, NO. 2,1982
PAIN: THEORIES AND TREATMENT
TABLE 4. RELIEF OF PAIN, MALE AND FEMALE WITH THE TWO UNITS
Unit (Number of Patients)
PSL (30)
Neuromod (18)
PSL, Male (8)
PSL, Female (22)
Neuromod, Male (5)
Neuromod, Female (13)
degree of relief while 26 percent of the female
patients received none. A higher percentage of patients received some relief with the PSL unit while
no women received complete pain relief with the
Neuromod unit. Many patients reported some
small degree of muscle contraction with the
Neuromod and many patients reported a soothing
sensation with the PSL. Two patients incurred
superficial pinpoint burns with the PSL which
were related to the electrode application. Many
patients who did not receive complete pain relief
with treatment were able to resume near normal
social activities, return to work, engage actively in
their therapy programs, and/or decrease their dependence on medications.
CONCLUSIONS
As a result of this study, the authors conclude
that TENS is a valuable adjunct to pain relief therapy as it is non-invasive, easy to apply, and nonnoxious. The only absolute contraindication is in
patients with a demand-type cardiac pacemaker.
TENS can be used as a screening method for patients who may need more drastic treatment methods. The authors feel that TENS should be the
first form of treatment for evaluated pain patients.
TENS has proven to be effective in 80 percent of
patients treated by the authors. It has decreased
their dependency on medications and improved
their activity and mobility. These units may be
used independently by patients after evaluation
and electrode placement determination, since repositioning may be necessary to achieve the best
Pain Relief Percentages (Number)
None
Moderate
Complete
17 (5)
22 (4)
0 (0)
23 (5)
0 (0)
30 (4)
33
67
50
32
60
70
(10)
(12)
(4)
(7)
(3)
(9)
50 (15)
11 (2)
50 (4)
45 (10)
40 (2)
0 (0)
results. Some dramatic results have been achieved
with TENS, and with more experimentation and
usage, more definitive knowledge of its mechanism may be gained and better results achieved.
TENS is recommended for routine use in a controlled setting.
Literature Cited
1. Melzack R, Wall PD. Pain mechanisms: A new
theory. Science 1965; 150:971-79.
2. Indeck W, Printz A. Skin application of electrical impulses for relief of pain in chronic orthopaedic conditions.
Minnesota Med 1975; 58:305-09.
3. Kerr FWL. Pain-a central inhibitory balance theory.
Mayo Clinic Proc 1975; 50:685-90.
4. Stiller R. Pain: Why It Hurts, Where It Hurts, When It
Hurts. Nashville, Tenn: Thomas Nelson, 1975.
5. Kirsch WM, Lewis JA, Simon RH. Experiences with
electrical stimulation devices for the control of chronic
pain. Med Instrum 1975; 9:217-20.
6. Shealy NC, Maurer D. Transcutaneous nerve stimulation for control of pain. Surg Neurol 1974; 2:45-7.
7. Picuza JA, Cannon BW, Hunter SE, et al. Pain suppression by peripheral nerve stimulation. Part l: Observations with transcutaneous stimuli. Surg Neurol 1975; 4:
105-14.
8. Long DM. External electrical stimulation as a treatment of chronic pain. Minnesota Med 1974; 57:195-98.
9. Loeser JD, Black RG, Christman A. Relief of pain by
transcutaneous stimulation. J Neurosurg 1975; 42:308-13.
10. Meyer GA, Fields HL: Causalgia treated by selective
large fiber stimulation of peripheral nerve. Brain 1972; 95:
163-68.
11. Hymes AC, Raab DE, Yonehiro EG, et al. Acute pain
control by electrostimulation: A preliminary report. Adv
Neurol 1974; 4:761-67.
12. Ebersold MJ, Laws ER, Stonnington HH, et al.
Transcutaneous electrical stimulation for treatment of
chronic pain: A preliminary report. Surg Neurolog 1975; 4:
96-9.
JOURNAL OF THE NATIONAL MEDICAL ASSOCIATION, VOL. 74, NO. 2, 1982
153
Das könnte Ihnen auch gefallen
- Hirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsVon EverandHirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNoch keine Bewertungen
- Types of PainDokument3 SeitenTypes of PainSab IbarretaNoch keine Bewertungen
- McKenzie CONCEPT AnilDokument12 SeitenMcKenzie CONCEPT AnilSOUMYADEEP BHUINYANoch keine Bewertungen
- Old Ideas: The Specificity Theory of PainDokument8 SeitenOld Ideas: The Specificity Theory of Paingeloss23150% (2)
- Lung SurgeriesDokument43 SeitenLung SurgeriesSereinNoch keine Bewertungen
- NCLEX-Physical AssessDokument83 SeitenNCLEX-Physical AssessRoberto EsmeleNoch keine Bewertungen
- Recent Article On Long Wave Diathermy-1Dokument5 SeitenRecent Article On Long Wave Diathermy-1Asad AnZariNoch keine Bewertungen
- Origin & Conduction of Cardiac Impulse: Dr.S.Brinda MD Associate Professor PhysiologyDokument36 SeitenOrigin & Conduction of Cardiac Impulse: Dr.S.Brinda MD Associate Professor PhysiologyAtchaya ThillainatarajanNoch keine Bewertungen
- Journal On PainDokument5 SeitenJournal On PainGeevine CansinoNoch keine Bewertungen
- Nursing Care of Clients Before and After CABGDokument46 SeitenNursing Care of Clients Before and After CABGshejila c hNoch keine Bewertungen
- BCLS AclsDokument27 SeitenBCLS AclsJanmichael FeliscuzoNoch keine Bewertungen
- Research Methodology: For All Physiotherapy and Allied Health Sciences StudentsDokument1 SeiteResearch Methodology: For All Physiotherapy and Allied Health Sciences StudentsProductivity 100Noch keine Bewertungen
- Anatomy and Physiology of The LungsDokument3 SeitenAnatomy and Physiology of The LungsMayownski TejeroNoch keine Bewertungen
- Musculoskeletal SystemDokument19 SeitenMusculoskeletal SystemDani Anyika100% (1)
- Cardiorespiratory AssessmentDokument7 SeitenCardiorespiratory AssessmentmalarvelykNoch keine Bewertungen
- Lung Expansion 1Dokument31 SeitenLung Expansion 11trindogg100% (2)
- Physiotherapy For Cardiac SurgeryDokument15 SeitenPhysiotherapy For Cardiac SurgeryMuruganNoch keine Bewertungen
- Blood Supply of BrainDokument2 SeitenBlood Supply of BrainvmagtotoNoch keine Bewertungen
- PAINLESS DELIVERY - PPDokument17 SeitenPAINLESS DELIVERY - PPrafiaNoch keine Bewertungen
- Tracheostomy Care: PhysiologyDokument2 SeitenTracheostomy Care: PhysiologyrajirajeshNoch keine Bewertungen
- Theories of Pain MechanismDokument16 SeitenTheories of Pain MechanismGithaiga KimaniNoch keine Bewertungen
- Adolescent Girls Anaemia Control ProgramDokument38 SeitenAdolescent Girls Anaemia Control ProgramKarunya VkNoch keine Bewertungen
- Urinary System Anatomy and PhysiologyDokument12 SeitenUrinary System Anatomy and PhysiologyCris Vincent Suma-oy100% (1)
- Arterial Line Arterial LineDokument13 SeitenArterial Line Arterial LineLinamaria Lozano100% (1)
- Amputation: DefinitionDokument9 SeitenAmputation: DefinitionCharaNoch keine Bewertungen
- Pathophysiology On ArrhythmiaDokument34 SeitenPathophysiology On ArrhythmiaYhr Yh100% (1)
- Case PresentationDokument44 SeitenCase PresentationSonali JoshiNoch keine Bewertungen
- Unit 1Dokument16 SeitenUnit 1reeta yadav0% (1)
- Tuberculosis of SpineDokument11 SeitenTuberculosis of SpineSepti RahadianNoch keine Bewertungen
- Case 8 NCP (Multiple Sclerosis)Dokument2 SeitenCase 8 NCP (Multiple Sclerosis)je-ann catedralNoch keine Bewertungen
- Compartment Syndrome: Return To TopDokument3 SeitenCompartment Syndrome: Return To TopSania Kamal BalweelNoch keine Bewertungen
- Prolapsed Intervertebral DiscDokument12 SeitenProlapsed Intervertebral DiscElvisNoch keine Bewertungen
- AARC Clinical Practice Guideline: Incentive SpirometryDokument10 SeitenAARC Clinical Practice Guideline: Incentive SpirometrytruptimptNoch keine Bewertungen
- Chest Trauma and Diseases: Mexigin Gayatri Akash JohannaDokument80 SeitenChest Trauma and Diseases: Mexigin Gayatri Akash JohannadidiNoch keine Bewertungen
- Myasthenia Gravis BrochureDokument2 SeitenMyasthenia Gravis BrochureMolly100% (1)
- DR - Lajja Bhagat MPT (Cardiopulmonary)Dokument49 SeitenDR - Lajja Bhagat MPT (Cardiopulmonary)Lajja Bhagat Shah100% (1)
- Types of PainDokument5 SeitenTypes of PainmariyalqibtiyahNoch keine Bewertungen
- Total Joint ReplacementDokument10 SeitenTotal Joint Replacementapi-3764215Noch keine Bewertungen
- BIOPSYDokument8 SeitenBIOPSYASHLEY DAWN BUENAFENoch keine Bewertungen
- Lab Guide: Musculoskeletal AssessmentDokument6 SeitenLab Guide: Musculoskeletal AssessmentDaisy MellaNoch keine Bewertungen
- Anatomy & Physiology of The Cardiovascular SystemDokument3 SeitenAnatomy & Physiology of The Cardiovascular SystemluaNoch keine Bewertungen
- Spinal StabilizationDokument32 SeitenSpinal StabilizationLakshita PrajapatiNoch keine Bewertungen
- SyringomyeliaDokument3 SeitenSyringomyeliaImran TagalaNoch keine Bewertungen
- Anterior Cord SyndromeDokument8 SeitenAnterior Cord SyndromeJanine Erika Julom BrillantesNoch keine Bewertungen
- Herpes ZosterDokument16 SeitenHerpes ZosterColleen De la RosaNoch keine Bewertungen
- Presented By: VIVEK DEVDokument38 SeitenPresented By: VIVEK DEVFranchesca LugoNoch keine Bewertungen
- Martha Rogers - Theory of Hunitary Human BeingDokument4 SeitenMartha Rogers - Theory of Hunitary Human BeingVictoria Castillo TamayoNoch keine Bewertungen
- Foot Anatomy Tendons and LigamentsDokument3 SeitenFoot Anatomy Tendons and Ligamentsanak_kost_aji_baungNoch keine Bewertungen
- Gi SystemDokument73 SeitenGi SystemSeema SachdevaNoch keine Bewertungen
- Rehabilitation in Spinal Cord InjuryDokument2 SeitenRehabilitation in Spinal Cord InjuryAudry ArifinNoch keine Bewertungen
- Obg CAM TherapiesDokument34 SeitenObg CAM TherapiesAGERI PUSHPALATHANoch keine Bewertungen
- 07.03.09 Chest Physiotherapy PDFDokument9 Seiten07.03.09 Chest Physiotherapy PDFRakesh KumarNoch keine Bewertungen
- Past, Present and Future Research in PhysiotherapyDokument11 SeitenPast, Present and Future Research in PhysiotherapyKiran Kumar Kalyanam100% (2)
- Devices Used in ICU: Critical Care NursingDokument95 SeitenDevices Used in ICU: Critical Care NursinghendranatjNoch keine Bewertungen
- Cholelithiasis GallstoneDokument22 SeitenCholelithiasis GallstoneBheru LalNoch keine Bewertungen
- Assessment of Musculo-Skeletal System: 2 Year B. SC NursingDokument33 SeitenAssessment of Musculo-Skeletal System: 2 Year B. SC NursingRubin100% (1)
- Discuss Nursing Interventions That Prevent Complications of ImmobilityDokument19 SeitenDiscuss Nursing Interventions That Prevent Complications of ImmobilityLilly Ann Vaughan50% (2)
- Cervical RibDokument15 SeitenCervical RibArko duttaNoch keine Bewertungen
- Modes of Mechanical VentilationDokument4 SeitenModes of Mechanical Ventilationsgod34100% (1)
- Chapter 5 - Functional Assessment & Amp Functional DeclineDokument7 SeitenChapter 5 - Functional Assessment & Amp Functional DeclineAndreea-Alexandra LupuNoch keine Bewertungen
- Chapter 3 - The Interprofessional TeamDokument8 SeitenChapter 3 - The Interprofessional TeamAndreea-Alexandra LupuNoch keine Bewertungen
- Chapter 2 - Overview of Geriatric AssessmentDokument8 SeitenChapter 2 - Overview of Geriatric AssessmentAndreea-Alexandra LupuNoch keine Bewertungen
- Dallas Pain QuestionnaireDokument1 SeiteDallas Pain QuestionnaireAndreea-Alexandra LupuNoch keine Bewertungen
- Chapter 1 - Transforming The Care of Older PersonsDokument3 SeitenChapter 1 - Transforming The Care of Older PersonsAndreea-Alexandra LupuNoch keine Bewertungen
- Effects of Low-Level He-Ne Laser Irradiation On The Gene Expression of IL-1beta, TNF-alpha, IFN-gamma, TGF-beta, BFGF, and PDGF in Rat's GingivaDokument1 SeiteEffects of Low-Level He-Ne Laser Irradiation On The Gene Expression of IL-1beta, TNF-alpha, IFN-gamma, TGF-beta, BFGF, and PDGF in Rat's GingivaAndreea-Alexandra LupuNoch keine Bewertungen
- Les Plus Belles Salles D'opéra Du Monde: Photos Prises Sur Le Net Créations Delia Florea CliquezDokument20 SeitenLes Plus Belles Salles D'opéra Du Monde: Photos Prises Sur Le Net Créations Delia Florea CliquezAndreea-Alexandra LupuNoch keine Bewertungen
- VaccinuriDokument18 SeitenVaccinuriAndreea-Alexandra LupuNoch keine Bewertungen
- The A To Z of Skeletal MusclesDokument238 SeitenThe A To Z of Skeletal MusclesAspenPharma99% (161)
- LiteracyDokument259 SeitenLiteracyAndreea-Alexandra LupuNoch keine Bewertungen
- MU151 Group Assignment 6Dokument3 SeitenMU151 Group Assignment 6Jay CadienteNoch keine Bewertungen
- Iyengar S., Leuschke G.J., Leykin A. - Twenty-Four Hours of Local Cohomology (2007)Dokument298 SeitenIyengar S., Leuschke G.J., Leykin A. - Twenty-Four Hours of Local Cohomology (2007)wojtekch100% (1)
- DLL Template MathDokument3 SeitenDLL Template MathVash Mc GregorNoch keine Bewertungen
- 39 - Riyadhah Wasyamsi Waduhaha RevDokument13 Seiten39 - Riyadhah Wasyamsi Waduhaha RevZulkarnain Agung100% (18)
- Breast Cancer ChemotherapyDokument7 SeitenBreast Cancer Chemotherapydini kusmaharaniNoch keine Bewertungen
- Role LibrariesDokument57 SeitenRole LibrariesGiovanni AnggastaNoch keine Bewertungen
- Electronic Devices and Electronic Circuits: QuestionsDokument51 SeitenElectronic Devices and Electronic Circuits: QuestionsRohit SahuNoch keine Bewertungen
- Di Franco Amended Factum 2021-05-03Dokument30 SeitenDi Franco Amended Factum 2021-05-03Michael BueckertNoch keine Bewertungen
- Republic Flour Mills Inc vs. Comm. of Cutoms (39 SCRA 509) Case DigestDokument3 SeitenRepublic Flour Mills Inc vs. Comm. of Cutoms (39 SCRA 509) Case DigestCamelle EscaroNoch keine Bewertungen
- Gianna Pomata (Editor), Nancy G. Siraisi (Editor) - Historia - Empiricism and Erudition in Early Modern Europe (Transformations - Studies in The History of Science and Technology) (2006)Dokument493 SeitenGianna Pomata (Editor), Nancy G. Siraisi (Editor) - Historia - Empiricism and Erudition in Early Modern Europe (Transformations - Studies in The History of Science and Technology) (2006)Marcelo Rizzo100% (1)
- Verbal Reasoning TestDokument3 SeitenVerbal Reasoning TesttagawoNoch keine Bewertungen
- National ScientistDokument2 SeitenNational ScientistHu T. BunuanNoch keine Bewertungen
- Power System Planning Lec5aDokument15 SeitenPower System Planning Lec5aJoyzaJaneJulaoSemillaNoch keine Bewertungen
- Simple Linear Equations A Through HDokument20 SeitenSimple Linear Equations A Through HFresgNoch keine Bewertungen
- IOSH Managing Safely Leaflet For Training ProvidersDokument6 SeitenIOSH Managing Safely Leaflet For Training ProvidersShakil Ahmad AligNoch keine Bewertungen
- CRM Project (Oyo)Dokument16 SeitenCRM Project (Oyo)Meenakshi AgrawalNoch keine Bewertungen
- Personal Development: Quarter 2 - Module 2: Identifying Ways To Become Responsible in A RelationshipDokument21 SeitenPersonal Development: Quarter 2 - Module 2: Identifying Ways To Become Responsible in A RelationshipTabada Nicky100% (2)
- HSE Matrix PlanDokument5 SeitenHSE Matrix Planवात्सल्य कृतार्थ100% (1)
- Episode 5 The Global TeacherDokument8 SeitenEpisode 5 The Global TeacherEllieza Bauto SantosNoch keine Bewertungen
- MK Slide PDFDokument26 SeitenMK Slide PDFPrabakaran NrdNoch keine Bewertungen
- Creativity & Innovation Brainstorming TechniquesDokument50 SeitenCreativity & Innovation Brainstorming TechniquesFirdhaus SakaffNoch keine Bewertungen
- Winifred Breines The Trouble Between Us An Uneasy History of White and Black Women in The Feminist MovementDokument279 SeitenWinifred Breines The Trouble Between Us An Uneasy History of White and Black Women in The Feminist MovementOlgaNoch keine Bewertungen
- A Guide To FractionsDokument18 SeitenA Guide To FractionsAnnelyanne RufinoNoch keine Bewertungen
- Improving Hands-On Experimentation Through Model Making and Rapid Prototyping: The Case of The University of Botswana's Industrial Design StudentsDokument6 SeitenImproving Hands-On Experimentation Through Model Making and Rapid Prototyping: The Case of The University of Botswana's Industrial Design StudentsnaimshaikhNoch keine Bewertungen
- Effect of Employee Loyalty On Customer S PDFDokument37 SeitenEffect of Employee Loyalty On Customer S PDFShailendra DasariNoch keine Bewertungen
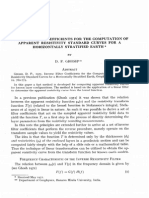
- Ghosh, D. P., 1971, Inverse Filter Coefficients For The Computation of Apparent Resistivity Standard Curves For A Horizontally Stratified EarthDokument7 SeitenGhosh, D. P., 1971, Inverse Filter Coefficients For The Computation of Apparent Resistivity Standard Curves For A Horizontally Stratified EarthCinthia MtzNoch keine Bewertungen
- 2018 UPlink NMAT Review Social Science LectureDokument133 Seiten2018 UPlink NMAT Review Social Science LectureFranchesca LugoNoch keine Bewertungen
- Sample ProposalDokument2 SeitenSample ProposaltoupieNoch keine Bewertungen
- MATH 7S eIIaDokument8 SeitenMATH 7S eIIaELLA MAE DUBLASNoch keine Bewertungen