Beruflich Dokumente
Kultur Dokumente
Gynecologic Oncology: Lilian T. Gien, Marie-Claude Beauchemin, Gillian Thomas
Hochgeladen von
pebripulunganOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Gynecologic Oncology: Lilian T. Gien, Marie-Claude Beauchemin, Gillian Thomas
Hochgeladen von
pebripulunganCopyright:
Verfügbare Formate
Gynecologic Oncology 116 (2010) 140146
Contents lists available at ScienceDirect
Gynecologic Oncology
j o u r n a l h o m e p a g e : w w w. e l s e v i e r. c o m / l o c a t e / y g y n o
Review
Adenocarcinoma: A unique cervical cancer
Lilian T. Gien a, Marie-Claude Beauchemin b, Gillian Thomas b,
a
b
Division of Gynecologic Oncology, Odette Cancer Centre, Sunnybrook Health Sciences Centre, Toronto, Ontario, Canada
Department of Radiation Oncology, Odette Cancer Centre, Sunnybrook Health Sciences Centre, 2075 Bayview Avenue, Toronto, ON, Canada M4N 3M5
a r t i c l e
i n f o
Article history:
Received 16 July 2009
Available online 31 October 2009
Keywords:
Adenocarcinoma
Cervix
Differences
Management
Prognosis
a b s t r a c t
Adenocarcinoma of the cervix constitutes only approximately 20% of all cervical carcinomas; therefore,
specic Level 1 evidence to guide patient management is lacking. Most trials have included this histologic
subtype but in insufcient numbers to do more than generate hypotheses from subset analyses. As a
consequence, our understanding of the natural history and optimal management of adenocarcinoma of the
cervix is limited. The optimal management of adenocarcinoma of the cervix continues to be a subject of
debate among practitioners as to whether or not it should be different from squamous cell carcinoma and
what would constitute this management. The purpose of this review was to give an overview of the current
knowledge on adenocarcinoma of the cervix and its differences from squamous cell carcinoma with regard to
risk factors, prognosis, survival rates, patterns of recurrence, and response to treatment. This article will
focus on possible specic therapeutic directions to explore in the management of locally advanced
adenocarcinomas.
2009 Published by Elsevier Inc.
Contents
Introduction . . . . . . . . . . . . . . . . . . . . .
Literature search strategy . . . . . . . . . . . . . . .
Differences in epidemiology . . . . . . . . . . . . . .
Prognostic factors and differences in survival . . . . . .
Differences in patterns of dissemination and recurrences
Differences in response to treatment in randomized trials
Differences in response to chemotherapy . . . . . . . .
Future directions and conclusions . . . . . . . . . . .
Conict of interest statement . . . . . . . . . . . . .
References . . . . . . . . . . . . . . . . . . . . . .
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
Introduction
Carcinoma of the cervix has showed a marked decline in
developed countries over the past 40 years, due to wider implementation of cytologic screening and increased detection of premalignant
disease. Although the decline is mainly attributable to a decrease in
incidence of the most common histologic variant, squamous cell
carcinoma (SCC), there has also been an increase in relative and
absolute incidence of adenocarcinoma and adenosquamous carcinoma (AC) of the uterine cervix over the same period, especially among
younger women [18]. The relative increase in the proportion of AC
Corresponding author. Fax: +1 416 480 6002.
E-mail address: Gillian.Thomas@sunnybrook.ca (G. Thomas).
0090-8258/$ see front matter 2009 Published by Elsevier Inc.
doi:10.1016/j.ygyno.2009.09.040
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
140
141
141
141
143
143
144
145
145
145
has resulted in this histology comprising more than 20% of all cervical
cancers in North America [3,5,6,9].
Most of our knowledge on the treatment of cervical cancer comes
from studies where the majority of the patients had SCC; AC only
comprised on average 10% of the cases [1021]. Very few of these
studies reported separate outcome results for AC of the cervix even on
exploratory subset analyses. No prospective study has focused on the
treatment of AC as the sole histology. As a consequence, our
understanding of the natural history and optimal management of
AC is limited. For the purposes of this review, the two most common
histologies of non-SCC, adenocarcinoma and adenosquamous carcinoma of the cervix, will be labeled as AC and analyzed together given
the scarce data separating these two histologies.
It appears that AC and SCC of the cervix behave differently. They
are different in epidemiology, prognostic factors, and patterns of
failure after similar treatments. Available data suggest that they may
L.T. Gien et al. / Gynecologic Oncology 116 (2010) 140146
also differ in their response to treatment. We postulate that new
treatment strategies specically tailored to AC should be explored.
The purpose of this review was to give an overview of the current
knowledge on AC of the cervix and its differences from SCC and to
focus on possible therapeutic directions to explore in their
management.
Literature search strategy
The literature was searched using MEDLINE (OVID: 1950 through
December 2008) and EMBASE (OVID: 1988 through December 2008),
using combined disease-specic terms (uterine cervix neoplasms/ or
cervi:.ti AND cancer:.ti or neoplasms/ or carcinoma:.ti or adenocarcinoma:.ti or adenosquamous:.ti) with outcome-specic terms (prognosis/ or treatment/). The search was restricted to English language
and humans. Additionally, Pubmed was searched with terms
adenocarcinoma or adenosquamous and cervix, and differences, prognosis, or treatment. Reference lists of related articles
and recent review articles were also screened for additional citations.
Differences in epidemiology
Over the past 40 years multiple reports have documented the
increase in relative distribution of AC compared to SCC in developed
countries [4,7]. Eifel et al. [9] reported between 1960 and 1989 the
proportion of patients with AC increased 24% to 49% while the
proportion of patients with SCC remained stable at 32%. Similar
ndings were observed from nine US-based Surveillance, Epidemiology, and End Results (SEER) registries [3]. Overall, from 1973 to 1996,
the incidence of invasive cervical cancers decreased by 37%, mainly
due to the declining incidence of SCC by 42% during that period.
Meanwhile, the AC incidence increased by 29%. From 1973 to 1977,
the proportions of SCC and AC were 88% and 12%, respectively, but
from 1993 to 1996, the proportions were 76% and 24%. Wang et al. [5],
in their analysis of SEER registries from 1976 to 2000, observed that
contrary to SCC where the rising carcinoma in situ (CIS) rates
corresponded to a decrease in invasive SCC rates, rising adenocarcinoma in situ (AIS) rates paralleled an increase in AC rates. Possible
reasons include the increased prevalence in AC risk factors such as
obesity, nulliparity, or HPV-18. Furthermore, the decrease in incidence and mortality of AC by the increased detection of AIS might not
be evident for many years because of the small numbers of AC lesions
compared to SCC in the population.
Another possible explanation for the increase in both relative and
absolute incidence of AC over time includes increased detection of
precursors with screening programs more effective in detecting SCC
than AC. SCC and CIS are mainly sampled from the exocervix, while AC
and AIS can be localized deep in the endocervical canal and be more
easily missed with the usual sampling by Papanicolaou (Pap) test. The
detection of squamous cell precursors may have led to a decrease in
invasive SCC and an increase in the relative prevalence of AC [6,7].
Besides sampling issues, there is wide inter-observer variation
from less experienced colposcopists and pathologists in recognizing
the more diverse appearance of AC compared to SCC [22,23]. Cytologic
criteria of precursor lesions of AIS have not been well validated
compared to the full spectrum of those for CIS. However, there has still
been an overall improved recognition of the disease, which can be
attributed to improved cytomorphologic description of the entity in
the 1980s prior to which AIS and AC were often classied as
endometrial or cervical cancer not otherwise specied (NOS) [24].
While AC and SCC share many similar risk factors, others have
different degrees of association with AC. According to Castellsague et
al. [8], who pooled the results from eight casecontrol studies
including 167 patients with non-SCC and 1881 hospital-based control
subjects, parity had a weaker association with AC, while obesity had a
stronger association with AC compared to SCC, similar to risk factors
141
associated with uterine cancer. Data from the International Collaboration of Epidemiological Studies of Cervical Cancer [25] included
13,541 women with cervical carcinoma, 15% of which were AC, and
23,017 women without cervical carcinoma from 23 epidemiological
studies. There was no association between smoking and the incidence
of AC with a relative risk of 0.89 (CI 0.741.06) and 0.89 (CI 0.721.10)
for current and past smokers, respectively. This is in contrast to SCC
where smoking is strongly associated, and the risk is correlated with
the number of cigarettes smoked per day and with the age of starting
smoking [25].
For many years, there were concerns that AC of the cervix was
linked with the use of oral contraceptives (OC) [26]. However, a recent
large systematic review that included 28 eligible studies and 12,531
women with cervical cancer demonstrated that although there was an
increased relative risk of cervix cancer with increasing duration of OC
use compared to never users of OC, the results were no different when
comparing SCC and AC of the cervix [27].
Finally, studies have shown that AC and SCC have slightly different
associations with HPV. Castellsague et al. [8] found that HPV-16 and
HPV-18 were the two most commonly detected HPV types in AC of the
cervix, present in 82% of their study patients. Data suggest that HPV18 accounts for about 50% of AC compared with only 15% of SCC [6].
Furthermore, the attributable fraction of HPV-18 and HPV-16 to AC is
higher relative to that of SCC, which is associated with a greater
diversity of HPV types [6].
Prognostic factors and differences in survival
Controversy exists as to whether histologic type is an independent
prognostic factor for survival. Although some studies have shown no
differences in survival between AC and SCC [2833], the majority have
shown that AC carries a worse prognosis with 10%20% differences in
5-year overall survival rates [9,3441]. The most important prognostic
factors for survival are clinical stage and lymph node status.
Clinical stage is a consistent prognostic factor for survival in all
cervix cancers. For AC, Baalbergen et al. [42] demonstrated in a study
of 305 patients that 5-year overall survival rates decreased with
advancing FIGO stage (stage I 80%, stage II 37%, stage III b11%). The
same trend was shown by Eifel et al. [1] for relapse-free survival in
367 cases of AC (stage I 73%, stage II 32%, stage III/IV 31%). As clinical
stage increases, a difference in survival between AC and SCC becomes
apparent. Comparing stage for stage, patients with AC had a
signicantly lower survival rate than those with SCC [2,9,36,37]. The
differences in survival rates according to stage are summarized in
Table 1.
Size of the tumor lesion is also a signicant prognostic factor. The
differences between AC and SCC may be negligible in small tumors,
as demonstrated by Marchiole et al. [43], where 118 radical
trachelectomy patients were compared to 139 radical hysterectomy
patients. Only tumor size and lymphvascular space invasion (LVSI),
and not histology, were shown on multivariate analysis to be
independent prognostic factors for recurrence. Thirteen of the 16
recurrences occurred in patients with tumors 2 cm. Conversely, as
the size of the tumor increases, the relative survival rate of patients
with AC signicantly decreases. Both Nakanishi et al. [38] and Eifel et
al. [9] found that tumor size N4 cm was a signicant adverse
prognostic factor for survival. The 5-year survival rate is 88%97% for
tumors b23 cm, but only 50%62% for tumors 45 cm [1,34]. In the
largest dataset, Eifel et al. [9] compared 1538 stage IB SCC to 229
stage IB AC patients, all treated with radical irradiation. Patients with
tumors N4 cm had an overall survival of 73% for SCC, but only 59%
for AC, and the estimated risk of death was 1.9 times greater for
patients with AC (p b 0.01), although the locoregional control rates
were similar in both groups. This reected the greater risk of
developing distant metastases in patients with AC (25%) compared
to those with SCC (14%) [9].
142
L.T. Gien et al. / Gynecologic Oncology 116 (2010) 140146
Table 1
Comparison of overall survival rates by histology and by stage.
Author, year [ref]
Number of patients (n)
Treatment
Stage
Hopkins et al., 1991 [36]
959 (203 AC, 756 SCC)
Pelvic RT +/ radical hysterectomy, pelvic,
and PA nodes for stage IB
Eifel et al., 1995 [9]
Chen et al., 1999 [37]
1767 (229 AC, 1538 SCC)
3678 (302 AC, 3376 SCC)
Pelvic RT +/ extrafascial hysterectomy
Stage IBIIA: radical hysterectomy,
pelvic nodes or RT
Stage IIBIV: RT +/ CT
Lai et al., 1999 [2]
891 (134 AC, 757 SCC)
Irie et al., 2000 [39]
255 (57 AC, 198 SCC)
Radical hysterectomy, pelvic nodes +/
adjuvant RT
Radical hysterectomy, pelvic nodes +/
adjuvant RT
5-Year survival (%)
p-Value
AC
SCC
I
II
III
IB
Overall
I
II
III
IV
IB & II
60
47
8
72
67
76
63
29
0
74
90
62
36
82
81
81
75
42
26
83
b 0.0001
0.01
0.002
b 0.01
0.0009
0.0039
0.0103
Overall
IB
II
78
96
61
92
94
90
0.0034
NS
0.0007
0.0136
AC, adenocarcinoma; SCC, squamous cell carcinoma; RT, radiation therapy; CT, chemotherapy; PA, para-aortic; NS, not signicant; ref, reference.
Lymph node metastases is a particularly important prognostic
factor in AC of the cervix, where the incidence has been reported to be
higher for AC compared to SCC, and rate of survival was shown to be
worse. In a study of 225 stage IBIIB cervix cancers with radical
hysterectomy, the incidence of node involvement was 32% for AC
versus 15% for SCC [39]. Not only are larger tumors associated with a
higher likelihood of lymph node metastasis, but also the incidence of
lymphadenopathy signicantly increases in AC than SCC [34,39]. Once
the nodes are positive, the survival rates worsen. Berek et al. [34] and
Baalbergen et al. [42] both found in surgically treated stage IIIB AC
that the survival rate was approximately 91% if the lymph nodes were
negative, but dropped to 10%34% if they were positive. Among
patients with positive nodes, AC has a signicantly reduced survival
compared to SCC in a number of studies [29,38,39]. Although
Shingleton et al. [29] did not nd a statistically signicant difference
in survival between the two histologies, subset analysis suggested
that AC patients with positive nodes had a worse overall survival
when compared to similar SCC patients (33% vs. 76% respectively,
p b 0.01). The differences in survival according to lymph node status
are summarized in Table 2.
The literature also suggests that certain histologic subtypes of
adenocarcinoma portend a worse prognosis. In most studies,
adenosquamous (AS) histology is included with AC. However, when
AS tumors are separated from AC, AS histology has a worse overall
survival rate [30,44,45]. Farley et al. [45] compared 185 patients with
AC to 88 with AS, and the 5-year overall survival rate was signicantly
worse for AS (65% vs. 83%, p b 0.002). Additionally, although studies
that compared SCC, AC, and AS histology found no signicant
difference in risk of death between SCC and AC, AS had death rates
1.8 times greater than SCC (p = 0.02) and 2.8 times greater than AC
(p = 0.007) [30,44]. Grisaru et al. [46] conducted a retrospective study
of 880 surgically treated stage IAIB cervical carcinomas evaluating
the prognostic signicance of histology for recurrence-free survival.
Median tumor size was 2 cm (range 0.16 cm). Pathologic data were
recorded by gynecologic pathologists at one center. Patients with AC
were divided into two groups: mucinous/endometrioid adenocarcinoma (n = 225) and adenosquamous/clear cell adenocarcinoma
(n = 81). There was a signicantly worse 5-year recurrence-free
survival on univariate analysis associated with AS compared to AC and
SCC (81% vs. 90%, p = 0.03). Despite some studies nding no
difference in survival in AS compared to AC and SCC [32,47,48], Farley
et al. [45] summarized in a specic review of the literature that on
average, AS histology had a worse overall survival compared to that of
AC alone, or AC and AS combined together (stage I, 69% vs. 80% vs.
80%; stage II, 27% vs. 59% vs. 48%, respectively). This highlights the
hypothesis that AC histology seems to have a worse prognosis
compared to SCC but could be partially attributed to AS being grouped
with AC histology.
There has been suggestion from retrospective studies that poorly
differentiated or grade 3 histology is an adverse prognostic factor for
recurrence in early stage AC of the cervix [31,49]. Eifel et al. [49]
observed that among 160 patients who had initial treatment for stage
I AC 4 cm in diameter, the 34 patients with grade 3 disease had a 5year survival rate of 67% compared to the other 126 patients whose 5year survival rate was 85% (p = 0.0018). Similarly, Kilgore et al. [31]
demonstrated that among 162 patients with AC, those with grade 2 or
3 lesions had a 5-year survival of 70% compared to 92% in those with
grade 1 lesions. Neither of these studies, however, included pathologic
Table 2
Comparison of overall survival rates by histology and by pathologic lymph node status.
Author, year [ref]
Number of patients (n)
Stage
LN status
Berek et al., 1985 [34]
51 AC
IBIIB
Shingleton et al., 1995 [29]
Irie et al., 2000 [39]
106 (20 AC, 86 SCC)
255 (57 AC, 198 SCC)
I
IBIIB
Nakanishi et al., 2000 [38]
509 (104 AC, 405 SCC)
IB
Baalbergen et al., 2004 [42]
200
IIIA
Positive
Negative
Positive
Positive
Negative
Positive
Negative
Positive
Negative
AC, adenocarcinoma; SCC, squamous cell carcinoma; NA, not applicable; NS, not signicant; ref, reference.
5 year survival (%)
AC
SCC
10
92
33
48
92
63
94
34
91
NA
NA
76
77
90
84
98
NA
NA
p-value
b 0.0001
b0.01
b0.05
NS
b0.001
b0.067
b0.003
L.T. Gien et al. / Gynecologic Oncology 116 (2010) 140146
review of the specimens. The GOG conducted a prospective study of
732 patients evaluating surgicopathologic factors in cervix cancer
with central pathology review but only included SCC histology. The
only independent prognostic factors were clinical tumor size, depth of
stromal invasion, and presence of LVSI [50]. In GOG 92, Sedlis et al.
[12] randomized patients with a combination of these three adverse
factors post-radical hysterectomy to either observation or adjuvant
radiation and found that the risk of recurrence was reduced by 44% in
the adjuvant radiation group [12]. Therefore, although advanced
grade and presence of LVSI may potentially carry a poorer prognosis in
patients with AC, it is difcult to conclude from the literature that the
presence of either of these factors alone would warrant additional
adjuvant therapy to surgery for small AC tumors, given that the
studies demonstrating grade as an adverse factor did not have
prospective pathology review, and LVSI as a factor alone is not
considered a reason for adjuvant radiation.
Overall, differences in survival in AC compared to SCC of the cervix
seem to be related to several adverse prognostic factors. The
differences between AC and SCC further persist when evaluating
patterns of disease dissemination and recurrence.
Differences in patterns of dissemination and recurrences
Differences in patterns of disease dissemination have been
reported for patients with AC histology. Shimada et al. [51] reported
on the largest series of 3471 surgically treated stage IBIIB cervix
cancers where 52 patients (1.5%) had ovarian metastasis (23/52 SCC
and 29/52 AC). Patients with AC had a signicantly higher rate of
ovarian metastasis (5% vs. 0.8%, p b 0.01). This difference was also
observed stage for stage; in stage IB, 4% of AC had ovarian metastasis
compared to 0.2% of SCC, while in stage IIB, it was 10% of AC compared
to 2% of SCC. It is unknown, however, how often the ovarian
metastases were grossly evident at the time of surgery. The presence
of ovarian metastasis did not correlate with lymph node involvement
or parametrial invasion. The difference in 5-year survival in patients
with ovarian metastasis (AC 18% vs. SCC 44%) was not statistically
signicant probably because of the small numbers in each group.
These data may have implications for surgical management, especially
for younger women where the risks associated with loss of ovarian
function should be weighed against that of potential ovarian
metastasis.
The sites of recurrence also differed between AC and SCC in this
study [51]. Although 48 patients (92%) received adjuvant therapy,
including radiation and/or chemotherapy after radical hysterectomy,
forty patients with ovarian metastasis (16/23 SCC and 24/29 AC)
recurred. In SCC with distant recurrence, 8 of 9 patients recurred in
extrapelvic lymph nodes, namely, paraaortic, cervical and inguinal
nodes. In AC with distant recurrence, 7 of 9 patients had hematogenous metastasis, while two recurred in paraaortic lymph nodes,
suggesting that route of spread to the ovaries may differ; SCC
predominantly disseminates lymphatically, whereas AC perhaps does
so hematogenously.
A number of studies demonstrate higher rates of distant metastasis
with AC histology. Berek et al. [34] reported on 51 surgically treated
AC patients; 13 recurred, of which 12 died with diffuse distant
metastasis and/or abdominal carcinomatosis. In small retrospective
studies, higher incidences of distant recurrence occurred for AC
compared to SCC, including higher rates of ascites, abdominal
carcinomatosis, and paraaortic spread [1,33,52]. Additionally, when
AC subtypes were analyzed, AS histology had an increased risk [53]
and shorter interval of disease recurrence [48]. The rate [30] and
deaths from distant metastasis [44] were both higher for AS. Finally,
according to Eifel et al. [1], in their analysis of 367 AC patients, the
overall distant metastasis rates for stages II and III AC were
dramatically higher than similarly staged SCC (stage II 46% vs. 13%;
stage III 38% vs. 21%). Subsequently, Eifel et al. [9] reported differences
143
Table 3
Differences in pelvic and distant relapse rates at 5 years by histology and by stage (data
from Eifel et al., 1995 [9]).
Stage
IB1
IB2
Number of
patients (n)
Risk of relapse at 5 years
Pelvic (%)
p-Value
Distant (%)
113
706
106
797
6
3
17
13
b 0.01
15
7
37
21
AC
SCC
AC
SCC
0.16
p-Value
0.01
b 0.01
AC, adenocarcinoma; SCC, squamous cell carcinoma.
in local and distant recurrence rates in stage IB cancers treated with
radiation. AC had statistically signicant increased distant relapse
rates compared to SCC regardless of tumor size (Table 3), while the
pelvic relapse rates were no different from SCC, demonstrating distant
failure despite adequate local control.
The striking difference in distant recurrence rates after primary
treatment raises questions regarding the approaches to locoregional
versus systemic treatment for patients with AC. Consideration should
be given to modifying current treatment approaches for AC rather
than using a generalized approach for SCC, in the attempt to reduce
the distant recurrence rates for this histology. Provocative questions
regarding treatment continue to arise when the differential response
to treatments in previous trials are analyzed.
Differences in response to treatment in randomized trials
Current standard treatment of AC has evolved through Level 1
evidence from trials incorporating SC and AC, but with a minority
proportion of AC (from 9% to 21%). Few studies have reported
unplanned subset analyses of response rate or survival for AC [1021].
However, three randomized trials report subgroup analyses by cell
type and demonstrate that treatments can have different effects on
recurrence rates and survival.
A phase III study (GOG 92) reported by Sedlis et al. [12] and
updated by Rotman et al. [21] randomized patients with surgically
treated stage IB cervical cancer with negative nodes and at least 2
adverse prognostic features (deep stromal invasion, LVSI, tumor
diameter N4 cm) to adjuvant post-operative external beam pelvic
radiation therapy (RT) versus observation (OBS). Two hundred
seventy-seven patients were entered including 59 patients with
non-squamous cell (non-SCC) histology. Overall, there was a
signicant reduction in risk of recurrence (OBS 31% vs. RT 18%,
p = 0.007) with the use of adjuvant RT. Both local (21% vs. 14%) and
distant (9% vs. 3%) recurrence rates were lower in the RT group.
Although the overall death rate was lower in the RT group (20% vs.
29%), the difference in overall survival did not reach statistical
signicance (p = 0.074). In subset analysis by histologic type, a higher
recurrence rate was observed for non-SCC histology (both AC and AS)
in the observation group compared to the RT group (non-SCC
recurrence rate: OBS 44% vs. RT 9%). This difference was more marked
than those with SCC histology (SCC recurrence rate: OBS 28% vs. RT
20%). These hypothesis-generating data suggest that the addition of
adjuvant RT is particularly more effective for patients with AC
compared to SCC in reducing the risk of recurrence. For patients
with surgically resectable disease and negative nodes, the fact that a
locoregional treatment can impact may suggest that AC histology has
localized micro-metastases in the pelvis, which can be potentially
eradicated by RT.
Peters et al. [17] reported from GOG 109/SWOG 8797/RTOG 91-12
on chemo-radiation versus radiation therapy alone for high-risk
features (positive lymph nodes and/or positive margins and/or
microscopic parametrial invasion) following radical hysterectomy
for stage Ia2, Ib, IIa cervical cancer. The planned chemotherapy was
two cycles of concurrent cisplatin + 5-uorouracil and two additional
144
L.T. Gien et al. / Gynecologic Oncology 116 (2010) 140146
should be conducted, given that it is not clear whether the poorer
outcomes were associated with the radiation itself or with suboptimal
dosing.
Table 5 summarizes the results from these three randomized trials
that have completed subgroup analyses based on histology. Although
these data are from small groups of patients, a similar hypothesis
emerges that patients with AC tend to respond differently to the
treatment in these trials. Further exploration of AC of the cervix in
future trials should be considered.
Differences in response to chemotherapy
Fig. 1. Progression-free survival for patients with squamous cell carcinoma (SCC) and
adenocarcinoma or adenosquamous carcinoma (Adeno) in the RT arm and the CT + RT
arm (data adapted from Peters et al., 2000) [17]. Reprinted with permission. 2008
American Society of Clinical Oncology. All rights reserved.
cycles given after radiation. 243 patients were evaluable, of which 50
were AC histology. A separate subset analysis by histology was
performed. Patients with AC and AS had worse prognosis than SCC
when treated with RT alone. However, this difference disappeared in
patients who received chemotherapy in addition to RT (Fig. 1) [17].
AC had poorer 5-year survival, local and distant recurrence rates than
SCC when chemotherapy was omitted. However, when chemotherapy
was added, results of 5-year survival, local and distant recurrence
rates between AC and SCC were comparable (Table 4) [20]. Finally,
further analyses of all patients receiving chemotherapy found higher
numbers of chemotherapy courses were associated with an improved
progression-free and overall survival (p = 0.03) [17]. From this, we
hypothesize that systemic chemotherapy plays a greater importance
in the treatment of AC, possibly because they may harbor more micrometastasis than SCC and therefore have more to gain from the added
systemic effect of the extra courses of chemotherapy.
Landoni et al. [10] reported results on AC in a study on patients
with stage Ib and IIa cervix cancer randomized between surgery
(n = 172) and radical radiation therapy (n = 171). Adjuvant radiotherapy was delivered after surgery in nearly two-thirds for those
with parametrial involvement, less than 3 mm margins, cut through
tumors, or positive nodes. Five-year overall and disease-free survival
rates were not signicantly different in the surgery and radiotherapy
groups (83% and 74%, respectively, for both groups). For those with AC
(46/337 patients, 14%), there appeared to be a signicant advantage
for patients who had surgery compared to those who had radiotherapy alone in both overall survival (70% vs. 59%, p = 0.05) and diseasefree survival (66% vs. 47%, p = 0.02). AC histology was also a signicant prognostic factor on multivariate analysis. It is important to
note the radiation dose in this study was very low by most standards
(median dose to pelvis 47 Gy, median dose to Point A 76 Gy, range 70
90 Gy) and two-thirds of patients on the surgical arm also received
adjuvant pelvic RT. Therefore, it is unclear from this study whether RT
alone for AC would be less effective than surgery if RT was
administered in optimal doses. This subgroup analysis therefore
raises the hypothesis that for early stage AC of the cervix treated by
radiation alone, careful observation post-treatment for central failure
Patients regardless of histology who present with metastatic,
persistent, or recurrent carcinomas of the cervix continue to have very
poor prognosis. Most studies evaluating chemotherapy in this setting
have insufcient numbers of patients to come to any accurate
conclusions regarding treatment of AC as a separate entity. However,
there are studies that have attempted to evaluate the response of AC
to chemotherapy.
Curtin et al. [54] reported on a series of 42 patients with
histologically conrmed persistent or recurrent AC of the cervix
with documented disease progression after standard local therapy
and administered Taxol 170 mg/m2 over 24 h IV every 3 weeks. The
overall response rate (RR) was 31%, which exceeded rates reported in
other studies using single agents in non-SCC of the cervix and was
similar to that of cisplatin and topotecan in GOG 179 (27%) [55].
Paclitaxel therefore demonstrated activity in non-SCC of the cervix
that appears comparable to that reported for other agents [54].
Similarly, Nagao et al. [56] performed a pilot study of those with no
prior platinum to receive docetaxel and carboplatin in 17 advanced or
recurrent cervix cancers. Eight of 17 were non-SCC histologies, and
the chemotherapy was neoadjuvant in 15 of the 17 patients. The
overall response rate was 76%. Seven of 10 patients (70%) with SCC
had clinical responses (2 complete response [CR], 5 partial response
[PR]), while 6 of 7 patients (86%) with non-SCC had clinical responses
(0 CR, 6 PR). Although this study had a very small number of patients,
it was encouraging to see an excellent overall response rate with this
regimen in the AC group.
Finally, Kastratis et al. [57] reported on pooled phase II results for
200 patients treated with rst-line platinum-based chemotherapy for
stage IV or recurrent cervical cancer. Twenty-nine percent (58/200)
had non-SCC histology. Overall response was 60% for non-SCC and
43% for SCC (p = 0.040), although histology was not an independent
predictor of tumor response (p = 0.797). The median survival was
19.1 months for non-SCC versus 11.6 months for SCC, but this
difference was not statistically signicant (p = 0.06) perhaps because
of the small number with non-SCC histology. Additionally, AC patients
more often received a paclitaxel-containing regimen than those with
SCC (81% vs. 58 %, p = 0.002) [57]. The non-SCC patients with
paclitaxel had a higher median survival compared to those without
paclitaxel (20.3 vs. 11.7 months). This difference was not statistically
signicant (p = 0.167), and the number of non-SCC patients in the
cohort was relatively small. Although this regimen is standard for
advanced or recurrent SCC, one can only hypothesize from these data
Table 4
Comparison of 5-year survival, local and distant recurrence rates by histology, and treatment modality (data from Monk et al., 2005 [20]).
SCC
5-Year survival
Local recurrence
Distant recurrence
AC
RT% (patients)
RT + CT% (patients)
p-Value
RT% (patients)
RT + CT% (patients)
p-Value
69
20 (19/95)
14 (13/95)
80
9 (9/98)
10 (10/98)
0.019
55
29 (6/21)
24 (5/21)
82
7 (2/29)
10 (10/98)
0.014
SCC, squamous cell carcinoma; AC, adenocarcinoma; RT, radiation therapy; CT, chemotherapy.
L.T. Gien et al. / Gynecologic Oncology 116 (2010) 140146
145
Table 5
Summary of results of randomized trials in cervix cancer with adenocarcinoma subset analyses.
Author, year [ref]
Sedlis et al., 1999 [12]/
Rotman et al., 2006 [21]
Peters et al., 2000 [17]
Monk et al., 2005 [20]
Landoni et al., 1997 [10]
Stage
Prognostic factors
Treatment arms
59 (21)
IB
243
50 (21)
IA2IIA
337
46 (14)
IBIIA
Two of the following: CLS,
N 4 cm, deep stromal invasion
+ Margin, + parametrium,
or + LN
None specied
Adjuvant pelvic RT
(4650.4 Gy)
Adjuvant pelvic RT
(49.3 Gy)
RT (pelvis 47 Gy,
point A 76 Gy)
Total
AC (%)
277
Results for AC patients
Obs
Adjuvant RT + CT
(5FU + cisplatin)
Surgery +/ adjuvant RT
RT vs. Obs: difference in
recurrences higher in AC vs. SCC
RT: worse PFS in AC N SCC
RT + CT: PFS AC = SCC
RT: worse OS
Surgery +/ RT: improved OS
AC, adenocarcinoma; SCC, squamous cell carcinoma; CLS, capillary lymphatic space; hyst, hysterectomy; LN, lymph node; RT, radiation therapy; CT, chemotherapy; Obs, observation;
OS, overall survival; PFS, progression-free survival; ref, reference.
that a taxane-containing regimen might be more effective for non-SCC
histology. Given the rarity of these tumors, this study is still one of the
largest evaluating AC histology in this clinical setting. Further separate
evaluation of the response to chemotherapy of AC needs to be
considered in future studies.
Future directions and conclusions
Based on hypotheses developed from review of limited available
data unique to AC on patterns of disease dissemination and risks of
failure after conventional treatment, several summary statements can
be made for patients with AC of the cervix.
For patients with small tumors b2 cm in size and negative LVSI, the
survival difference between AC and SCC is negligible. Surgical
management with radical hysterectomy or radical trachelectomy for
these carefully selected patients result in low recurrence rates and
high overall survival rates, with no differences in outcome related to
histologic type.
As tumor stage advances, AC has signicantly lower survival rates
compared to SCC stage for stage. The incidence of lymph node
metastasis is higher for AC compared to SCC, and survival rates are
dramatically lower in AC patients with positive lymph nodes
compared to similar SCC patients. Radiation therapy as part of the
management may be more effective in this histology for local control
in stage IB tumors as demonstrated by Sedlis et al. [12]. However, even
with adequate pelvic control in those treated with radiation, distant
relapse rates are higher in stage IB1 tumors [9], raising questions
regarding prevention of distant relapse through adjuvant systemic
treatment.
In patients with tumor size N4 cm and progressively advanced
disease, concurrent chemoradiation is the primary treatment. Very
careful post-treatment surveillance should be carried out locally to
detect central failure and identify those potentially curable with
further surgery. Distant failure rates are higher in AC tumors N4 cm [9]
and also occur more frequently when chemotherapy is omitted [20],
suggesting that sufcient courses of chemotherapy should be
administered to attempt to impact on occult disseminated disease.
The aim should be to decrease distant failure rates in AC. This could
potentially include not only the addition of a taxane to the
chemotherapeutic regimen but also additional courses of conventional chemotherapy post-concurrent chemoradiation.
The addition of biologic agents could further improve the systemic
control of disease. Recent improvements in our understanding of
molecular events in tumor cells have led to the use of agents targeting
the epidermal growth factor (EGF) and vascular endothelial growth
factor (VEGF) signaling pathways, which play critical roles in tumor
growth and angiogenesis [58]. Cetuximab, an antibody directed at the
EGF receptor, is investigated in several clinical studies in cervical
cancer, both as monotherapy or in combination with radiotherapy. A
recent phase II trial combining cetuximab with cisplatin and
topotecan for advanced cervix cancer unfortunately demonstrated
signicant toxicity [59]. Several phase II clinical trials with bevacizumab in cervix cancer, targeting the VEGF pathway, have been
initiated. The most recent publication demonstrated bevacizumab
was well tolerated with comparable response rates to other phase II
GOG studies in this setting [60]. Additionally, VEGFR tyrosine kinase
inhibitors, such as sorafenib and pazopanib, are being studied in phase
I/II clinical trials [58]. The hope is that these agents will improve
outcomes for women with cervix cancer and could potentially be of
benet particularly in patients with AC histology, which tends to
display a poorer distant recurrence rate.
Finally, the randomized phase III trials in cervix cancer have
demonstrated relatively small proportions of patients with AC
histology. The likelihood of being able to perform a phase III trial on
solely AC histology in cervix cancer is extremely low. In order to
examine the effects of therapy on AC, exploratory analyses with phase
II trials will need to take place. This will still require a signicant
number of patients with contribution from multiple centers. The data
that exist regarding AC of the cervix generate hypotheses that warrant
further examination of AC as an entity of its own. The ability to do this
depends on collaboration from the international community to
contribute patients and work towards an understanding of adenocarcinoma as a unique cervical cancer.
Conict of interest statement
The authors have no conicts of interest to declare.
References
[1] Eifel PJ, Morris M, Oswald MJ, Wharton JT, Delclos L. Adenocarcinoma of the uterine
cervix: prognosis and patterns of failure in 367 Cases. Cancer 1990;65:250714.
[2] Lai CH, Hsueh S, Hong JH, Chang TC, Tseng CJ, Chou HH, et al. Are adenocarcinomas
and adenosquamous carcinomas different from squamous carcinomas in stage IB
and II cervical cancer patients undergoing primary radical surgery? Int J Gynecol
Cancer 1999;9:2836.
[3] Smith HO, Tiffany MF, Qualls CR, Key CR. The rising incidence of adenocarcinoma
relative to squamous cell carcinoma of the uterine cervix in the United States: a
24-year population-based study. Gynecol Oncol 2000;78:97105.
[4] Sasieni P, Adams J. Changing rates of adenocarcinoma and adenosquamous
carcinoma of the cervix in England. Lancet 2001;357:14903.
[5] Wang SS, Sherman ME, Hildesheim A, Lacey Jr JV, Devesa S. Cervical adenocarcinoma and squamous cell carcinoma incidence trends among white women and
black women in the United States for 1976-2000. Cancer 2004;100:103544.
[6] Sherman ME, Wang SS, Carreon J, Devesa SS. Mortality trends for cervical squamous
and adenocarcinoma in the United States. Cancer 2005;103(6):125864.
[7] Bray F, Carstensen B, Mller H, Zappa M, Zakelj MP, Lawrence G, et al. Incidence
trends of adenocarcinoma of the cervix in 13 European countries. Cancer
Epidemiol Biomark Prev 2005;14:21919.
[8] Castellsagu X, Daz M, De Sanjos S, Muoz N, Herrero R, Franceschi S, et al.
Worldwide human papillomavirus etiology of cervical adenocarcinoma and its
cofactors: implications for screening and prevention. J Natl Cancer Inst 2006;98:
30315.
[9] Eifel PJ, Burke TW, Morris M, Smith TL. Adenocarcinoma as an independent risk
factor for disease recurrence in patients with stage 1B cervical carcinoma. Gynecol
Oncol 1995;59:3844.
[10] Landoni F, Maneo A, Colombo A, Placa F, Milani R, Perego P, et al. Randomized
study of radical surgery versus radiotherapy for stage Ib-IIa cervical cancer. Lancet
1997;350:53540.
[11] Morris M, Eifel PJ, Lu J, et al. Pelvic radiation with concurrent chemotherapy
compared with pelvic and paraaortic radiation for high-risk cervical cancer. N Engl
J Med 1999;340:113743.
[12] Sedlis A, Bundy BN, Rotman MZ, Lentz SS, Muderspach LI, Zaino RJ. A randomized trial
of pelvic radiation therapy versus no further therapy in selected patients with stage
1b carcinoma of the cervix after radical hysterectomy and pelvic lymphadenectomy:
a Gynecologic Oncology Group study. Gynecol Oncol 1999;73:17783.
146
L.T. Gien et al. / Gynecologic Oncology 116 (2010) 140146
[13] Keys HM, Bundy BN, Stehman FB, et al. Cisplatin, radiation, and adjuvant
hysterectomy for bulky stage IB cervical carcinoma. N Engl J Med 1999;340:115461.
[14] Rose PG, Bundy BN, Watkins J, et al. Concurrent cisplatin-based chemotherapy
and radiotherapy for locally advanced cervical cancer. N Engl J Med 1999;340:
114453.
[15] Whitney CW, Sause W, Bundy BN, et al. A randomized comparison of uorouracil plus
cisplatin versus hydroxyurea as an adjunct to radiation therapy in stages IIBIVA
carcinoma of the cervix with negative para-aortic lymph nodes: a Gynecologic
Oncology Group and Southwest Oncology Group study. J Clin Oncol 1999;17:133948.
[16] Landoni F, Maneo A, Cormio G, Perego P, Milani R, Caruso O, et al. Class II versus
class III radical hysterectomy in stage IB-IIA cervical cancer: a prospective
randomized study. Gynecol Oncol 2001;80:312.
[17] Peters WA, Liu PY, Barrett RJ, Stock RJ, Monk BJ, Berek JS, et al. Concurrent
chemotherapy and pelvic radiation therapy compared with pelvic radiation
therapy alone as adjuvant therapy after radical surgery in high-risk early stage
cancer of the cervix. J Clin Oncol 2000;18:160613.
[18] Eifel PJ, Winter K, Morris M, Levenback C, Grigsby PW, Cooper J, et al. Pelvic
irradiation with concurrent chemotherapy versus pelvic and para-aortic irradiation
for high-risk cervical cancer: an update of Radiation Therapy Oncology Group trial
(RTOG) 90-01. J Clin Oncol 2004;22:87280.
[19] Lanciano R, Calkins A, Bundy BN, Parham G, Lucci JA, Moore DH, et al. Randomized
comparison of weekly cisplatin or protracted venous infusion of uorouracil in
combination with pelvic radiation in advanced cervix cancer: a Gynecologic
Oncology Group study. J Clin Oncol 2005;23:828995.
[20] Monk BJ, Wang J, Im S, Stock RJ, Peters WA, Liu PY, et al. Rethinking the use of
radiation and chemotherapy after radical hysterectomy: a clinicalpathologic
analysis of a Gynecologic Oncology Group/Southwest Oncology Group/Radiation
Therapy Oncology Group trial. Gynecol Oncol 2005;96:7218.
[21] Rotman M, Sedlis A, Piedmonte MR, Bundy B, Lentz SS, Muderspach LI, et al. A
phase III randomized trial of postoperative pelvic irradiation in stage 1B cervical
carcinoma with poor prognostic features: follow-up of a Gynecologic Oncology
Group study. Int J Radiat Oncol Biol Phys 2006;65:16976.
[22] Wang SS, Sherman ME, Silverberg SG, Carreon JD, Lacey JV, Zaino R, et al.
Pathological characteristics of cervical adenocarcinoma in a multi-center U.S.based study. Gynecol Oncol 2006;103:5416.
[23] Alfsen GC, Reed W, Abeler VM. Reproducibility of classication in non-squamous
cell carcinomas of the uteterine cervix. Gynecol Oncol 2003;90:2829.
[24] The Bethesda System for reporting cervical/vaginal cytologic diagnoses: revised
after the second National Cancer Institute workshop, April 29-30, 1991. Acta Cytol
1993;37:11524.
[25] International Collaboration of Epidemiological Studies of Cervical Cancer.
Carcinoma of the cervix and tobacco smoking: collaborative reanalysis of
individual data on 13,541 women with carcinoma of the cervix and 23,017
women without carcinoma of the cervix from 23 epidemiological studies. Int J
Cancer 2006;118:148195.
[26] Peters RK, Chao A, Mack TM, Thomas D, Bernstein L, Henderson BE. Increased
frequency of adenocarcinoma of the uterine cervix in young women in Los Angeles
County. J Natl Cancer Inst 1986;76:4238.
[27] Smith JS, Green J, Berrington de Gonzalez A, Appleby P, Peto J, Plummer M, et al.
Cervical cancer and use of hormonal contraceptives: a systematic review. Lancet
2003;361:115967.
[28] Grigsby PW, Perez CA, Kuske RR, Camel HM, Kao MS, Galakatos AE, et al.
Adenocarcinoma of the uterine cervix: lack of evidence for a poor prognosis.
Radiother Oncol 1988;12:28996.
[29] Shingleton HM, Bell MC, Fremgen A, Chmiel JS, Russell AH, Jones WB, et al. Is there
really a difference in survival of women with squamous cell carcinoma,
adenocarcinoa, and adenosquamous cell carcinoma of the cervix? Cancer
1995;76:194855.
[30] Look KY, Brunetto VL, Clarke-Pearson DL, Averette HE, Major FJ, Alvarez RD, et al.
An analysis of cell type in patients with surgically staged stage IB carcinoma of the
cervix: a Gynecologic Oncology Group Study. Gynecol Oncol 1996;63:30411.
[31] Kilgore LC, Soong SJ, Gore H, et al. Analysis of prognostic features in
adenocarcinoma of the cervix. Gynecol Oncol 1998;31:13748.
[32] Alfsen GC, Kristensen GB, Skovlund E, Pettersen EO, Abeler VM. Histologic subtype
has minor importance for overall survival in patients with adenocarcinoma of the
uterine cervix: a population-based study of prognostic factors in 505 patients with
nonsquamous cell carcinomas of the cervix. Cancer 2001;92:247183.
[33] Lee KBM, Lee JM, Park CY, Lee KB, Cho HY, Ha SY. What is the difference between
squamous cell carcinoma and adenocarcinoma of the cervix? A matched case
control study. Int J Gynecol Cancer 2006;16:156973.
[34] Berek JS, Hacker NS, Fu YS, et al. Adenocarcinoma of the uterine cervix: histologic
variables associated with lymph node metastasis and survival. Obstet Gynecol
1985;65:4652.
[35] Kleine W, Rau K, Schwoeorer D, Peiderer A. Prognosis of adenocarcinoma of the
cervix uteri: a comparative study. Gynecol Oncol 1989;35:14559.
[36] Hopkins MP, Morley GW. A comparison of adenocarcinoma and squamous cell
carcinoma of the cervix. Obstet Gynecol 1991;77:9127.
[37] Chen RJ, Lin YH, Chen CA, Huang SC, Chow SN, Hsieh CY. Inuence of histologic
type and age on survival rates for invasive cervical carcinoma in Taiwan. Gynecol
Oncol 1999;73:18490.
[38] Nakanishi T, Ishikawa H, Suzuki Y, Inoue T, Nakamura S, Kuzuya K. A comparison
of prognoses of pathologic stage IB adenocarcinoma and squamous cell carcinoma
of the uterine cervix. Gynecol Oncol 2000;79:28993.
[39] Irie T, Kigawa J, Minagawa Y, Itamochi H, Sato S, Akeshima R, et al. Prognosis and
clinicopathological characteristics of Ib-IIb adenocarcinoma of the uterine cervix
in patients who have had radical hysterectomy. Eur J Surg Oncol 2000;26:4647.
[40] Takeda N, Sakuragi N, Takeda M, Okamoto K, Kuwabara M, Negishi H, et al.
Multivariate analysis of histopathologic prognostic factors for invasive cervical
cancer treated with radical hysterectomy and systematic retroperitoneal
lymphadenectomy. Acta Obstet Gynecol Scand 2002;81:114451.
[41] Davy MLJ, Dodd TJ, Luke CJ, Roder DM. Cervical cancer: effect of glandular cell type
on prognosis, treatment, and survival. Obstet Gynecol 2003;101:3845.
[42] Baalbergen A, Ewing-Graham PC, Hop WCJ, Struijk P, Helmerhorst TJM. Prognostic
factors in adenocarcinoma of the uterine cervix. Gynecol Oncol 2004;92:2627.
[43] Marchiole P, Benchaib M, Buenerd A, Lazlo E, Dargent D, Mathevet P. Oncological
safety of laparoscopic-assisted vaginal radical trachelectomy (LARVT or Dargent's
operation): a comparative study with laparoscopic-assisted vaginal radical
hysterectomy (LARVH). Gynecol Oncol 2007;106:13241.
[44] Gallup DG, Harper RH, Stock RJ. Poor prognosis in patients with adenosquamous
cell carcinoma of the cervix. Obstet Gynecol 1985;65:41622.
[45] Farley JH, Hickey KW, Carlson JW, Rose GS, Kost ER, Harrison TA. Adenosquamous
histology predicts a poor outcome for patients with advanced-stage, but not earlystage, cervical carcinoma. Cancer 2003;97:2196202.
[46] Grisaru D, Covens A, Chapman B, Shaw P, Colgan T, Murphy J, et al. Does histology
inuence prognosis in patients with early-stage cervical carcinoma. Cancer
2001;92:29993004.
[47] Harrison TA, Sevin BU, Koechili O, Nguyen HN, Averette HE, Penalver M, et al.
Adenosquamous carcinoma of the cervix: prognosis in early stage disease treated
by radical hysterectomy. Gynecol Oncol 1993;50:3105.
[48] Dos Reis R, Frumovitz M, Milam MR, Capp E, Sun CC, Coleman RL, et al.
Adenosquamous carcinoma versus adenocarcinoma in early-stage cervical cancer
patients undergoing radical hysterectomy: an outcomes analysis. Gynecol Oncol
2007;107:45863.
[49] Eifel PJ, Burke TW, Delclos L, Wharton JT, Oswald MJ. Early stage I adenocarcinoma
of the uterine cervix: treatment results in patients with tumors 4 cm in
diameter. Gynecol Oncol 1991;41:199205.
[50] Delgado G, Bundy B, Zaino R, Sevin BU, Creasman WT, Major F. Prospective
surgicalpathological study of disease-free interval in patients with stage IB
squamous cell carcinoma of the cervix: a Gynecologic Oncology Group study.
Gynecol Oncol 1990;38:3527.
[51] Shimada M, Kiwaga J, Nishimura R, Yamaguchi S, Kuzuya K, Nakanishi T, et al.
Ovarian metastasis in carcinoma of the uterine cervix. Gynecol Oncol 2006;101:
2347.
[52] Drescher CW, Hopkins MP, Roberts JA. Comparison of the pattern of metastatic
spread of squamous cell cancer and adenocarcioma of the uterine cervix. Gynecol
Oncol 1989;33:3403.
[53] Lea JS, Coleman RL, Garner EO, Duska LR, Miller DS, Schorge JO. Adenosquamous
histology predicts poor outcome in low-risk stage IB1 cervical adenocarcinoma.
Gynecol Oncol 2003;91:55862.
[54] Curtin JP, Blessing JA, Webster KD, Rose PG, Mayer AR, Fowler WC, et al. Paclitaxel,
an active agent in nonsquamous carcinoma of the uterine cervix: a Gynecologic
Oncology Group study. J Clin Oncol 2001;19:12758.
[55] Long HJ, Bundy BN, Grendys EC, Benda JA, McMeekin DS, Sorosky J, et al.
Randomized phase III trial of cisplatin with or without topotecan in carcinoma of
the uterine cervix: a Gynecologic Oncology Group study. J Clin Oncol 2005;23:
462633.
[56] Nagao S, Fujiwara K, Oda T, Ishikawa H, Koike H, Tanaka H, et al. Combination
chemotherapy of docetaxel and carboplatin in advanced or recurrent cervix
cancer: a pilot study. Gynecol Oncol 2005;96:8059.
[57] Kastratis E, Bamias A, Efstathiou E, Gika D, Bozas G, Zorzou P, et al. The outcome of
advanced or recurrent non-squamous carcinoma of the uterine cervix after
platinum-based combination chemotherapy. Gynecol Oncol 2005;99:37682.
[58] del Campo JM, Prat A, Gil-Moreno A, Perez J, Parera M. Update on novel
therapeutic agents for cervical cancer. Gynecol Oncol 2008;110:S726.
[59] Kurtz JE, Hardy-Bessard AC, Deslandres M, Lavau-Denis S, Largillier R, RoemerBecuwe C, et al. Cetuximab, topotecan and cisplatin for the treatment of advanced
cervical cancer: a phase II GINECO trial. Gynecol Oncol 2009;113:1620.
[60] Monk BJ, Sill MW, Burger RA, Gray HJ, Buekers TE, Roman LD. Phase II trial of
bevacizumab in the treatment of persistent or recurrent squamous cell carcinoma
of the cervix: a gynecologic oncology group study. J Clin Oncol 2009;27:106974.
Das könnte Ihnen auch gefallen
- FLAC DynamicDokument294 SeitenFLAC DynamicMaximillian KrisnadiNoch keine Bewertungen
- Yehuda Berg Satan PDFDokument77 SeitenYehuda Berg Satan PDFOswaldo Archundia100% (7)
- Adnexal MassDokument28 SeitenAdnexal MassJuan P. RuedaNoch keine Bewertungen
- AT2H - Basics - Symbolism in HinduismDokument28 SeitenAT2H - Basics - Symbolism in Hinduismapi-3764210Noch keine Bewertungen
- Breast Cancer Metastasis and Drug Resistance Progress and ProspectsDokument416 SeitenBreast Cancer Metastasis and Drug Resistance Progress and ProspectsRichard Balili100% (1)
- Drainage BasinsDokument4 SeitenDrainage BasinsDannySP10100% (1)
- (Essentials of Diagnostic Gynecological Pathology) C. Simon Herrington-Pathology of The Cervix-Springer (2017)Dokument266 Seiten(Essentials of Diagnostic Gynecological Pathology) C. Simon Herrington-Pathology of The Cervix-Springer (2017)raul gutierrez100% (1)
- Ovarian CancerDokument7 SeitenOvarian CancerAndi AliNoch keine Bewertungen
- Boil-Off Gas CalculationsDokument14 SeitenBoil-Off Gas CalculationsAlberto100% (1)
- Atlas-Complejidad Económica PDFDokument362 SeitenAtlas-Complejidad Económica PDFRafael QuiñonesNoch keine Bewertungen
- MÁY 5 Service Manual Bellavista 1000 V16 08Dokument126 SeitenMÁY 5 Service Manual Bellavista 1000 V16 08Huế TrầnNoch keine Bewertungen
- Gynecologic Oncology Reports: Olpin J., Chuang L., Berek J., Ga Ffney D. TDokument7 SeitenGynecologic Oncology Reports: Olpin J., Chuang L., Berek J., Ga Ffney D. TJheyson Javier Barrios PereiraNoch keine Bewertungen
- Free Research Paper On Cervical CancerDokument6 SeitenFree Research Paper On Cervical Cancerafedonkfh100% (1)
- Running Head: Brachytherapy: Isotopes 1Dokument20 SeitenRunning Head: Brachytherapy: Isotopes 1api-384666214Noch keine Bewertungen
- Thesis Statement On Cervical CancerDokument6 SeitenThesis Statement On Cervical Cancerbkx3abyc100% (2)
- Cervical Cancer ThesisDokument8 SeitenCervical Cancer Thesisafbteuawc100% (2)
- MM 0127 Coveragepositioncriteria Cervical Cancer Screening TechnologiesDokument21 SeitenMM 0127 Coveragepositioncriteria Cervical Cancer Screening TechnologiesHildaNoch keine Bewertungen
- 00006Dokument6 Seiten00006carlangaslaraNoch keine Bewertungen
- Cervical Cancer Literature ReviewDokument6 SeitenCervical Cancer Literature Reviewaflskeqjr100% (1)
- Research Paper About Cervical CancerDokument4 SeitenResearch Paper About Cervical Cancergw1357jx100% (1)
- Example Research Paper Lung CancerDokument8 SeitenExample Research Paper Lung Cancerafmcvhffm100% (1)
- Research Paper Topics CancerDokument4 SeitenResearch Paper Topics Cancergvzyr86v100% (1)
- Original 2Dokument6 SeitenOriginal 2medusineNoch keine Bewertungen
- Thesis Cervical CancerDokument6 SeitenThesis Cervical Cancerheduurief100% (2)
- Roe 2018Dokument11 SeitenRoe 2018mohamaed abbasNoch keine Bewertungen
- Thesis Statement Examples For Breast CancerDokument7 SeitenThesis Statement Examples For Breast CancermandyhebertlafayetteNoch keine Bewertungen
- Ductal Carcinoma in Situ: How Much Is Too Much?: Keerthi Gogineni, MD, MSHPDokument3 SeitenDuctal Carcinoma in Situ: How Much Is Too Much?: Keerthi Gogineni, MD, MSHPCarlos OlivoNoch keine Bewertungen
- Early Breast CancaerDokument17 SeitenEarly Breast CancaerDwi Arnhilah Miranda100% (1)
- Research Paper Cervical CancerDokument5 SeitenResearch Paper Cervical Cancergz8bjzmj100% (1)
- FigoDokument11 SeitenFigoPraja Putra AdnyanaNoch keine Bewertungen
- Colorectal Cancer DissertationDokument6 SeitenColorectal Cancer DissertationBestPaperWritingServicesSingapore100% (1)
- Ovarian Cancer - StatPearls - NCBI BookshelfDokument13 SeitenOvarian Cancer - StatPearls - NCBI BookshelfeeeeeeNoch keine Bewertungen
- Current Status of Knowledge, Attitude and Practice (KAP) and Screening For Cervical Cancer in Countries at Different Levels of DevelopmentDokument7 SeitenCurrent Status of Knowledge, Attitude and Practice (KAP) and Screening For Cervical Cancer in Countries at Different Levels of DevelopmentHuzaifa SaeedNoch keine Bewertungen
- Borderline Ovarian CancerDokument8 SeitenBorderline Ovarian Canceramarendra WardhanaNoch keine Bewertungen
- Breast Cancer Staging PDFDokument12 SeitenBreast Cancer Staging PDFDanu BagoesNoch keine Bewertungen
- ESGOESTROESP Guidelines For The Management of Patients With Cervical Cancer - Update 2023Dokument32 SeitenESGOESTROESP Guidelines For The Management of Patients With Cervical Cancer - Update 2023Limbert Rodríguez TiconaNoch keine Bewertungen
- Borderline Ovarian Tumors - UpToDateDokument19 SeitenBorderline Ovarian Tumors - UpToDatenoor hyNoch keine Bewertungen
- Riesgo de Ansiedad y Depresión en Mujeres Taiwanesas Con Cáncer de Mama y Cáncer de Cuello UterinoDokument9 SeitenRiesgo de Ansiedad y Depresión en Mujeres Taiwanesas Con Cáncer de Mama y Cáncer de Cuello UterinoJessNoch keine Bewertungen
- 1 s2.0 S2405844020304485 MainDokument5 Seiten1 s2.0 S2405844020304485 MainSome LaNoch keine Bewertungen
- Cancer de PeneDokument12 SeitenCancer de PeneAndelcass DellNoch keine Bewertungen
- Nims MedsDokument13 SeitenNims MedsWeng Villaverde PampoNoch keine Bewertungen
- 1019 5298 1 PBDokument11 Seiten1019 5298 1 PBm907062008Noch keine Bewertungen
- Cervical CancerDokument14 SeitenCervical CancerAlejandra MurilloNoch keine Bewertungen
- Jfac 142Dokument25 SeitenJfac 142Ana Paula Giolo FranzNoch keine Bewertungen
- Ca CervixDokument17 SeitenCa CervixNisa Aprilen GintingNoch keine Bewertungen
- Cervical CancerDokument18 SeitenCervical CancerErjohn Vincent LimNoch keine Bewertungen
- The Surgeon's Guide To Fibroadenomas: Katherine Kopkash, Katharine YaoDokument8 SeitenThe Surgeon's Guide To Fibroadenomas: Katherine Kopkash, Katharine YaoKarina WirajayaNoch keine Bewertungen
- International Journal of Pediatric OtorhinolaryngologyDokument22 SeitenInternational Journal of Pediatric OtorhinolaryngologyDear Farah SielmaNoch keine Bewertungen
- Oesophageal CarcinomaDokument13 SeitenOesophageal CarcinomaMichelle DefandiNoch keine Bewertungen
- Ca CervikDokument7 SeitenCa CervikHendra SusantoNoch keine Bewertungen
- Ovarian Cancer DissertationDokument5 SeitenOvarian Cancer DissertationHelpWritingPaperYonkers100% (1)
- Systematic Literature Review Breast CancerDokument7 SeitenSystematic Literature Review Breast Cancerafmzodjhpxembt100% (1)
- Ecgy 05 00131Dokument4 SeitenEcgy 05 00131Zaniru Raúl Marín MartínezNoch keine Bewertungen
- Literature Review On Knowledge Regarding Prevention of Cervical CancerDokument6 SeitenLiterature Review On Knowledge Regarding Prevention of Cervical Cancerea8p6td0Noch keine Bewertungen
- Research Paper Colorectal CancerDokument4 SeitenResearch Paper Colorectal Cancerxactrjwgf100% (1)
- ACOG 2011 Management of The Adnexal Mass June 2011Dokument16 SeitenACOG 2011 Management of The Adnexal Mass June 2011Arlen Patricia Soto LópezNoch keine Bewertungen
- Cervical Cancer Trends in The United States: A 35-Year Population-Based AnalysisDokument7 SeitenCervical Cancer Trends in The United States: A 35-Year Population-Based Analysisbehanges71Noch keine Bewertungen
- ZLJ 209Dokument11 SeitenZLJ 209afg_19Noch keine Bewertungen
- Winer2016 PDFDokument8 SeitenWiner2016 PDFAlex AdamiteiNoch keine Bewertungen
- Kader2018 Atypical Ductal Hyperplasia - Update On Diagnosis, Management, and Molecular LandscapeDokument11 SeitenKader2018 Atypical Ductal Hyperplasia - Update On Diagnosis, Management, and Molecular LandscapeLyka MahrNoch keine Bewertungen
- Cervical CA Proposal Jan152010Dokument21 SeitenCervical CA Proposal Jan152010redblade_88100% (2)
- Thesis On Cervical Cancer ScreeningDokument6 SeitenThesis On Cervical Cancer Screeningangelabaxtermanchester100% (1)
- Literature Review On Pap SmearDokument4 SeitenLiterature Review On Pap Smearbsdavcvkg100% (1)
- Axillary Node Metastases With Occult Primary Breast CancerDokument19 SeitenAxillary Node Metastases With Occult Primary Breast CanceraizatamlikhaNoch keine Bewertungen
- Anal Cancer Guidelines 2014Dokument12 SeitenAnal Cancer Guidelines 2014Alfredo Alfaro CarvajalNoch keine Bewertungen
- Literature Review Sample On Breast CancerDokument6 SeitenLiterature Review Sample On Breast Canceraflslcqrg100% (1)
- Amniotic Fluid and Its Abnormality: DefinitionDokument7 SeitenAmniotic Fluid and Its Abnormality: DefinitionpebripulunganNoch keine Bewertungen
- Maternal Social Support Predicts Birth Weight and Fetal Growth in Human PregnancyDokument11 SeitenMaternal Social Support Predicts Birth Weight and Fetal Growth in Human PregnancypebripulunganNoch keine Bewertungen
- Factors Influencing The Use of Antenatal Care in Rural West Sumatra, IndonesiaDokument8 SeitenFactors Influencing The Use of Antenatal Care in Rural West Sumatra, IndonesiapebripulunganNoch keine Bewertungen
- Prevalence of Abnormal Pap Smear During Pregnancy in A Teaching Hospital in South IndiaDokument4 SeitenPrevalence of Abnormal Pap Smear During Pregnancy in A Teaching Hospital in South IndiapebripulunganNoch keine Bewertungen
- Weekly KosongggDokument11 SeitenWeekly KosongggpebripulunganNoch keine Bewertungen
- The Modern Day Cult: by Antonio Panebianco, Jason Devine, Will RichardsDokument11 SeitenThe Modern Day Cult: by Antonio Panebianco, Jason Devine, Will RichardsAntonio PanebiancoNoch keine Bewertungen
- LESSON 2 Facilities Location StrategiesDokument2 SeitenLESSON 2 Facilities Location StrategiesElle LeeNoch keine Bewertungen
- The 50 Most Inspiring Travel Quotes of All TimeDokument4 SeitenThe 50 Most Inspiring Travel Quotes of All Timeungku1Noch keine Bewertungen
- Saberon StratMan2Dokument3 SeitenSaberon StratMan2paredesladyheart18Noch keine Bewertungen
- Orchestral Recording, January 2006Dokument10 SeitenOrchestral Recording, January 2006Rhys WilliamsNoch keine Bewertungen
- 4th Six Weeks RecoveryDokument8 Seiten4th Six Weeks RecoveryAshley HighNoch keine Bewertungen
- PrionDokument22 SeitenPrionAnushkaNoch keine Bewertungen
- Chapter 4 TurbineDokument56 SeitenChapter 4 TurbineHabtamu Tkubet EbuyNoch keine Bewertungen
- Monitoring:: Steps of Adding New SiteDokument8 SeitenMonitoring:: Steps of Adding New SiteMohammad ZakoutNoch keine Bewertungen
- AE451 Aerospace Engineering Design: Team HDokument140 SeitenAE451 Aerospace Engineering Design: Team HÖmer Uğur ZayıfoğluNoch keine Bewertungen
- EclipseDokument6 SeitenEclipsetoncipNoch keine Bewertungen
- Unit-3 DC Machines IMP QuestionsDokument30 SeitenUnit-3 DC Machines IMP Questionskrishna Sai Atla VenkataNoch keine Bewertungen
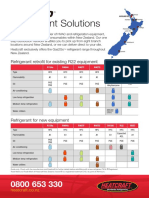
- Refrigerant Solutions: Refrigerant Retrofit For Existing R22 EquipmentDokument2 SeitenRefrigerant Solutions: Refrigerant Retrofit For Existing R22 EquipmentpriyoNoch keine Bewertungen
- Em - Animals A To ZDokument9 SeitenEm - Animals A To ZgowriNoch keine Bewertungen
- Presentation On Anther Culture: Submitted To Submitted byDokument22 SeitenPresentation On Anther Culture: Submitted To Submitted byvishnu0751Noch keine Bewertungen
- Modeling The Dynamic and Static Behavior of Chemical ProcessesDokument4 SeitenModeling The Dynamic and Static Behavior of Chemical ProcessesFatma CahyaniNoch keine Bewertungen
- Conduit 5Dokument42 SeitenConduit 5dediNoch keine Bewertungen
- Oplan Tumbler ProposalDokument3 SeitenOplan Tumbler ProposalKay Tuppil ManzanillaNoch keine Bewertungen
- HandbikeDokument10 SeitenHandbikeLely JuniariNoch keine Bewertungen
- SpeedFace M4 DatasheetDokument2 SeitenSpeedFace M4 DatasheetRENJITH K NAIRNoch keine Bewertungen
- JCB R135 & R155-HD Skid Steer-New BrochureDokument8 SeitenJCB R135 & R155-HD Skid Steer-New BrochureAshraf KadabaNoch keine Bewertungen
- Igorot Village: Get To Know..Dokument11 SeitenIgorot Village: Get To Know..Elain RagosNoch keine Bewertungen
- Edrolo ch3Dokument42 SeitenEdrolo ch3YvonneNoch keine Bewertungen