Beruflich Dokumente
Kultur Dokumente
Premolar Transplantation To Replace A Missing Central Incisor
Hochgeladen von
MaryGonzalesʚïɞOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Premolar Transplantation To Replace A Missing Central Incisor
Hochgeladen von
MaryGonzalesʚïɞCopyright:
Verfügbare Formate
CASE REPORT
Premolar transplantation to replace a missing
central incisor
a
Deise Lima Cunha, Marco Antonio Masioli, Joao~ Batista Gagno Intra, Armelindo Roldi,
Camila de Sousa Dardengo,e and Jose Augusto Mendes Miguelf
Vitoria, Esprito Santo, and Rio de Janeiro, Rio de Janeiro, Brazil
During childhood, the anterior maxilla is susceptible to injury, and the loss of incisors is one of the most
serious injuries. In many cases, autotransplantation is the best alternative for children who lose an incisor
during the growth phase. This case report describes the treatment of a boy who had a traumatic injury when
he was 8 years old that resulted in avulsion of the maxillary right central incisor. When he sought treatment
at age 10, the space was lost as was bone in the incisor region. Because he lacked space in the mandibular
arch for proper tooth alignment, extractions were planned. One extracted premolar was transplanted into the
space of the missing maxillary incisor area. The posttreatment results were good, and follow-up records 7
and 9 years after treatment showed healthy periodontal support and cortical bone gain in the transplanted
tooth's buccal area. (Am J Orthod Dentofacial Orthop 2015;147:394-401)
he incisor
root development
phase coincides
with
the
period
of childhood
in which trauma
occurs frequently
in the
anterior maxilla.1-5 During this age, tooth avulsion occurs
because the incisor roots
are still growing and do not have good bone
3
implantation. However, there are situations where the
trauma is of such a magnitude that reimplantation is
not possible. Consequently, treatment becomes limited
because it is contraindicated to place dental implants or
other restorative treatment while the patient still has
6
the potential for alveolar growth.
The transplantation of immature premolars has
become a viable method for restoring edentulous areas
because they can maintain the function and preserve
the alveolar crest; this is advantageous for young
patients when compared with dental implants that are
static and do not erupt to compensate for future
7-9
growth.
a
Private practice, Vitoria, Esprito Santo, Brazil.
Professor, Federal Esprito Santo Univertsity, Esprito Santo,
c
Brazil. Private practice, Vitoria, Esprito Santo, Brazil.
b
d
e
Private practice, Vitoria, Esprito Santo, Brazil.
Private practice, Vitoria, Esprito Santo, Brazil.
Associate professor, Department of Orthodontics, School of Dentistry, Rio de
Ja-neiro State University, Rio de Janeiro, Rio de Janeiro, Brazil.
All authors have completed and submitted the ICMJE Form for Disclosure of
Po-tential Conflicts of Interest, and none were reported.
Address correspondence to: Deise Lima Cunha, Av Nossa Senhora dos Navegantes 635/802, Enseada do Sua, Vitoria, Esprito Santo 29050-335, Brazil; email, deise@masioliodontologia.com.br.
Submitted, November 2013; revised and accepted, August 2014.
0889-5406/$36.00
Copyright 2015 by the American Association of Orthodontists.
http://dx.doi.org/10.1016/j.ajodo.2014.08.022
394
The success of autotransplanted teeth is associated
with periodontal ligament healing, no root resorption,
bone and gum healing, and pulp and root development.
To maintain this sequence of factors, atraumatic
surgery is fundamental, and multidisciplinary
participation is necessary to allow for a functional and
3
esthetic restoration.
Recent advances in computerized tomography have
allowed for the visualization of structures that were
impossible to evaluate in the past. Through these new
technologies, the visualization of the periodontal ligament and new bone formation has become a reality.
This case report presents the autotransplantation of
a premolar to the region of a central incisor through
surgery with preservation of the periodontal ligament.
The receiver site exhibited considerable bone
resorption because tooth loss occurred 2 years before
the initiation of treatment. The preservation of dental
structures (cementum and periodontal ligament)
allowed for bone formation around the transplanted
tooth. This finding was possible only with the use of 3dimensional tomography as a means of observation.
DIAGNOSIS AND ETIOLOGY
A 10-year-old boy was evaluated with the chief
complaint of esthetic concerns (Figs 1-3). He was
missing a maxillary central incisor, which had been
lost in a traumatic injury at age 8. He was physically
healthy but had active caries, a sinus tract in the
maxillary left central incisor, and decay reaching the
pulp of the maxillary right first premolar. Because of
Cunha et al
395
Fig 1. Initial extraoral and intraoral photographs.
the loss of the maxillary right central incisor 2 years
earlier, the alveolar crest was atrophic because of the
large amount of bone resorption. He had a posterior
crossbite, crowding in the mandibular arch with a
discrepancy of 8 mm, and an Angle Class I
malocclusion and a Class II skeletal pattern (ANB, 7 )
(Table).
TREATMENT OBJECTIVES
The goals of treatment included orthodontic alignment and leveling of the arches, obtaining a Class I
rela-tionship of the canines and molars, maintaining a
normal contour of the marginal gingiva and bone for
the transplant, correcting the posterior crossbite, and
closing all spaces created by the dental extractions.
TREATMENT ALTERNATIVES
One treatment option was extraction of the maxillary left central incisor, which already had an associated sinus tract and was also traumatized. This would
create space for the proper alignment of the maxillary
arch. The central incisors would be replaced by the
maxillary lateral incisors, which would be moved
mesially; thus, the subsequent teeth would move
consecutively. In the mandibular arch, the first
premolars would be extracted to align and level the
teeth without the additional projection of the incisors.
After orthodontic treatment, some prosthetic treat-ment
would be needed. The disadvantages of this course of
treatment included excessive orthodontic movement
and maintenance of the maxillary right
American Journal of Orthodontics and Dentofacial Orthopedics
March 2015
Vol 147
Issue 3
Cunha et al
396
Fig 2. Initial dental casts.
first premolar, which had a poor prognosis. In addition,
the anterior esthetics would be questionable because of
the emergence profile of the lateral incisors, which was
different from that of the central incisors. The canines'
Class I relationship would not be achieved, and lateral
movements would have to be performed in group
function. Finally, the movement of the maxillary right
lateral incisor to the position of the right central incisor
would present an excessive risk of recession because
of bone deficiency in the region caused by the early
loss of this tooth.
Another alternative treatment was extraction of the
first premolars to obtain adequate space for the alignment of both arches. Thus, the teeth would be aligned
and space maintained for dental implant placement in
the maxillary right central incisor region after the
completion of the vertical growth of the maxillary
alveolar process. The advantages of this treatment
included extraction of the right first premolar, which
had pulpal involvement. The disadvantages included
difficulty in providing a definitive resolution to the
problem of the absence of the incisor. The condition
March 2015
Vol 147
Issue 3
of the area for placement of the implant would be poor
because early tooth loss also results in bone loss,
thereby generating the need for a surgical graft to
obtain a satisfactory esthetic appearance of the gingiva.
However, the chosen treatment was endodontic
therapy of the maxillary left central incisor, extraction
of the maxillary first premolars, and maxillary expansion. In addition, we assembled 4 3 2 mechanics to
make room for the transplant of the mandibular right
second premolar to the maxillary right central incisor
region, since this tooth had the ideal apical development.
All treatment options would achieve ideal Class I
molar relationship and overjet. However, the patient
and his parents wished for him to have a beautiful
smile with good esthetics and function. The risk of root
resorption from the transplant was understood and
accepted by the patient and his parents.
TREATMENT PROGRESS
Once the discrepancy on the mandibular arch reached
8 mm, tooth extraction was inevitable, and to
American Journal of Orthodontics and Dentofacial Orthopedics
Cunha et al
397
Fig 3. Initial radiographs and cephalometric tracing.
Table. Cephalometric measurements
Pretreatment Posttreatment Norm
Maxilla to cranial base
SNA ( )
Mandible to cranial base
SNB ( )
SN-MP ( )
FMA (MP-FH) ( )
Maxillomandibular
ANB ( )
Maxillary dentition
U1-NA (mm)
U1-SN ( )
Mandibular dentition
L1-NP (mm)
L1-MP ( )
Soft tissues
Lower lip to E-plane (mm)
Upper lip to E-plane (mm)
81.5
79.8
82.0
76.5
42.0
34.8
75.5
36.0
28.1
80.9
32.9
25.4
5.0
4.3
1.6
3.0
101.6
2.4
101.0
4.3
102.3
5.3
94.5
5.5
99.8
4.0
95.0
1.8
1.4
0.5
2.6
2.0
2.9
transplant the extracted mandibular premolar, the
appropriate space in the receiving site was obtained
quickly before the apical foramen was closed.
The treatment began with the extraction of the
maxillary first premolars and the installation of a hyrax
device for crossbite correction and to obtain space for
transplantation. The device was removed 3 months
later when standard edgewise slot 0.022-in brackets
were placed. Thus, the space was opened with a nickeltitanium coil spring for the transplantation of the
mandibular right second premolar to the space of the
maxillary right central incisor.
The surgical procedure was performed as shown in
Figure 4 according to the protocol determined by
10
Slagsvold and Bjerck. Because the maxillary right
central incisor had been lost almost 3 years previously,
the bone edge was reabsorbed and quite constricted in
buccolingual thickness (Fig 4, A). Surgery with drills
and saline solution irrigation was performed to yield 1
socket to receive the self-transplanted premolar (Fig 4,
B-D). After that, the donor tooth was extracted
carefully, so as to not damage the structures of the
periodontal ligament (Fig 4, E). However, because of
poor bone levels, the alveolus had no cortical bone
American Journal of Orthodontics and Dentofacial Orthopedics
March 2015
Vol 147
Issue 3
Cunha et al
398
Fig 4. Surgical autotransplantation: A, receiver site ready to receive the transplanted tooth; B-D,
sur-gical procedure for the preparation of the bone socket; E, removal of the dental germ of its
original site; F-H, placement of the tooth germ into the receptor and stabilization.
Fig 5. Final extraoral and intraoral photographs.
March 2015
Vol 147
Issue 3
American Journal of Orthodontics and Dentofacial Orthopedics
Cunha et al
399
Fig 6. Final dental casts.
(Fig 4, F). After placing the tooth germ gently in this
new bone in infra-occlusion, the patient was instructed to be careful that the transplant did not receive
any pressure to prevent injury to the periodon-tium.
The gingiva covering the element was stabilized only
with a suture to hold it in position (Fig 4, G and H). A
lingual arch was placed, and the left mandibular
second premolar was extracted.
TREATMENT RESULTS
After 3 years 8 months, Class I molar and canine
re-lationships were achieved, the maxillary and
mandibular midlines were coincident, the crossbite was
corrected, the extraction spaces were closed, and
proper alignment and leveling were obtained (Figs 57). The profile was acceptable, despite the Class II
skeletal pattern; the patient had a pleasant smile and a
good incisor relationship. It was requested that the
patient undergo extraction of the third molars.
Figure 8 shows radiographs before the autotransplantation to 9 years after surgery. A computed tomography
scan (Fig 9) suggested that cortical bone had been formed
by the deposition of bone on the root of the transplanted
tooth. This new bone formation was possible only
because of the preservation of the cementum and the
periodontal ligament of the transplanted tooth.
DISCUSSION
The treatment of choice for this patient was autotransplantation. Earlier trauma in the incisor region contraindicated large movements of the anterior teeth because
resorption was a risk. One advantage of autotransplantation is that even if the transplanted tooth is lost in the
future from resorption, the presence of the transplanted
tooth while the patient is growing helps to maintain bone
in the area and allows vertical bone growth. This
characteristic of the autotransplant is extremely relevant
in this procedure. Maintaining bone should be considered,
especially when the patient loses a central incisor before
entering the growth spurt. The maintenance of bone in the
transplantation area during this stage of life will facil-itate
the replacement with a dental implant, if it is needed.
In Scandinavian countries, autotransplantation of
premolars to replace missing incisors is a widespread
11
method that has been used for over 40 years.
However, there is no description of this procedure with
the same success rates in other countries because of the
difficulty of implementing the technique. It is known
that for the procedure to be successful, it is essential to
6
ensure that the periodontium is not injured.
Some authors reported that for patients in whom tooth
loss has occurred too early, there can be resorption of the
alveolar bone crest, with insufficient bone volume
American Journal of Orthodontics and Dentofacial Orthopedics
March 2015
Vol 147
Issue 3
Cunha et al
400
Fig 7. Final radiographs and cephalometric tracing.
Fig 8. Periapical radiographs from pretreatment to 9 years posttreatment: A, initial radiography; B,
immediately after autotransplantation surgery; C, 1-year follow-up (beginning of orthodontic
treatment); D, 5-year follow-up (orthodontic treatment completion); E, 9-year follow-up.
to accommodate vestibule-palatal transplantation, as
12
described here.
For these patients, the authors
suggested bone grafts before transplantation surgery.
This protocol was not adopted because the time
required to wait for healing of the graft would
compromise the quality of the transplant since the root
of the trans-planted tooth would be in an advanced
stage of devel-opment.
The ideal stage for transplantation (3/4-4/4 formed
root with open apex) and the preservation of the periodontal structures (ligament and cementum) are funda4,13
mental to the success of this therapy.
In our patient, the tooth was transplanted with threequarters of the root formed. The advantage of perform-ing
the transplant in this situation is that the element will
provide satisfactory implementation, in addition to
March 2015
Vol 147
Issue 3
American Journal of Orthodontics and Dentofacial Orthopedics
Cunha et al
401
Tomography at the 7-year follow-up showed good
periodontal support on the transplanted buccal root,
and radiography at the 9-year follow-up showed good
periodontal support.
REFERENCES
Fig 9. Tomography at the 7-year follow-up. The longitudinal section of the maxillary right central incisor region
shows that vestibular cortical bone formed on the root of
the transplanted tooth after orthodontic treatment.
maintaining nutrition and continuing the formation
process until closure of the root apex.
The preservation of the periodontal structures
hinders the formation of ankylosed areas around the
transplanted root. In addition, the periodontal ligament
provides undifferentiated progenitor cells that are
capable of differentiating into fibroblasts, osteoblasts,
and cementoblasts. The differentiated osteoblasts can
generate bone around the transplants, filling the gap
between the walls of the alveolus and the transplant,
14,15
and causing osteogenesis.
In this patient, there was
bone formation in the vestibular region that could be
easily observed in the computed tomography scan.
Because of the great difficulty in accessing
computed tomography scanners and the high cost of
screening when this patient started treatment, no initial
tomo-graphic
documentation was made for
comparison. Nevertheless, during the surgery, it was
possible to observe the thinness of the bone in this
region and the absence of sufficient bone in the socket
created to receive the transplant.
CONCLUSIONS
A 10-year-old boy had lost his maxillary right
central incisor from dental trauma when he was 8.
Orthodontic treatment was performed, and the lost
tooth was re-placed with autotransplantation of the
mandibular right second premolar. The proposed
treatment successfully achieved all desired objectives
to the satisfaction of the patient and his parents.
1. Vilhjalmsson VH, Knudsen GC, Grung B, Bardsen A. Dental
auto-transplantation to anterior maxillary sites. Dent Traumatol
2011; 27:23-9.
2. Kindelan SA, Day PF, Kindelan JD, Spencer JR, Duggal MS.
Dental trauma: an overview of its in fluence on the manage-ment
of orthodontic treatment. Part 1. J Orthod 2008;35: 68-78.
3. Zachrisson BU. Planning esthetic treatment after avulsion of
maxillary incisors. J Am Dent Assoc 2008;139:1484-90.
4. Zachrisson BU. Management of missing maxillary anterior teeth
with emphasis on autotransplantation. Am J Orthod Dentofacial
Orthop 2004;126:284-8.
5. Kristerson L, Langerstrom L. Autotransplantation of teeth in
cases with agenesis or traumatic loss of maxillary incisors. Eur J
Orthod 1991;13:486-92.
6. Harzer W, Ruger D, Tauscher E. Autotransplantation of first premolar to replace a maxillary incisor 3D-volume tomography
for evaluation of the periodontal space. Dent Traumatol
2009;25: 233-7.
7. Keightley AJ, Cross DL, McKerlie RA, Brocklebank L.
Autotrans-plantation of an immature premolar, with the aid of
cone beam CT and computer-aided prototyping: a case report.
Dent Trauma-tol 2010;26:195-9.
8. Paulsen HU, Andreasen JO, Schwartz O. Pulp and periodontal
heal-ing, root development and root resorption subsequent to
trans-plantation and orthodontic rotation: a long-term study of
autotransplanted premolars. Am J Orthod Dentofacial Orthop
1995;108:630-40.
9. Paulsen HU, Andreasen JO, Yu Z, Schwartz O. Tooth loss
treatment in the anterior region: autotransplantation of premolars
and cryopreservation. World J Orthod 2006;7: 27-34.
10. Slagsvold O, Bjercke B. Applicability of autotransplantation in
cases of missing upper anterior teeth. Am J Orthod 1978;74:
410-21.
11. Park YS, Jung MH, Shon WJ. Autotransplantation of a displaced
mandibular second premolar to its normal position. Am J Orthod
Dentofacial Orthop 2013;143:274-80.
12. Thomas S, Turner SR, Sandy JR. Autotransplantation of teeth: is
there a role? Br J Orthod 1998;25:275-82.
13. Paulsen HU. Autotransplantation of teeth in orthodontic
treatment. Am J Orthod Dentofacial Orthop 2001;119: 336-7.
14. Mensink G, Karagozoglu KH, Strackee SD, van Teeseling RA,
Smeele LE, Becking AG. Autotransplantation of two maxillary
pre-molars in a free vascularized fibula reconstructed mandible.
Int J Oral Maxillofac Surg 2011;40:219-21.
15. Yau ECK. Tooth autotransplantation as a treatment option. Hong
Kong Med Diary 2009;14:21-4.
American Journal of Orthodontics and Dentofacial Orthopedics
March 2015
Vol 147
Issue 3
Das könnte Ihnen auch gefallen
- Controlled Tooth Movement To Correct An Iatrogenic Problem: Case ReportDokument8 SeitenControlled Tooth Movement To Correct An Iatrogenic Problem: Case ReportElla GolikNoch keine Bewertungen
- Ortho Bone ScrewDokument17 SeitenOrtho Bone ScrewmedicalcenterNoch keine Bewertungen
- 2014 AJODO SilveiraDokument11 Seiten2014 AJODO SilveiraJavier Farias VeraNoch keine Bewertungen
- Miyahira2008 - Miniplates As Skeletal Anchorage For Treating Mandibular Second Molar ImpactionsDokument4 SeitenMiyahira2008 - Miniplates As Skeletal Anchorage For Treating Mandibular Second Molar ImpactionsNathália LopesNoch keine Bewertungen
- Mandibular Premolar Transplantation To Replace Missing Maxillary Anterior Teeth: A Multidisciplinary ApproachDokument14 SeitenMandibular Premolar Transplantation To Replace Missing Maxillary Anterior Teeth: A Multidisciplinary ApproachRicha AhlawatNoch keine Bewertungen
- Articulo Mordida AbiertaDokument13 SeitenArticulo Mordida AbiertaLesliieYasmiinGariinRizzoNoch keine Bewertungen
- Bong 2011 PDFDokument14 SeitenBong 2011 PDFkarenchavezalvanNoch keine Bewertungen
- Atypical Extraction of Maxillary Central Incisors - AJODODokument8 SeitenAtypical Extraction of Maxillary Central Incisors - AJODOSofia PereiraNoch keine Bewertungen
- Jung 2018Dokument14 SeitenJung 2018Anonymous ckVKx4njgNoch keine Bewertungen
- AJO DO Revista ArticuloDokument10 SeitenAJO DO Revista ArticuloAngélicaLujánNoch keine Bewertungen
- Pinho2013 PDFDokument7 SeitenPinho2013 PDFammarkochiNoch keine Bewertungen
- PIIS0889540612000881Dokument11 SeitenPIIS0889540612000881Aly OsmanNoch keine Bewertungen
- Mukherjee Et AlDokument5 SeitenMukherjee Et AlSohaib ShujaatNoch keine Bewertungen
- Treatment of Maxillary Canine TranspositionDokument8 SeitenTreatment of Maxillary Canine TranspositionFabian BarretoNoch keine Bewertungen
- Case Report Lateral Open Bite Treatment Stability OMT Essential Cabrera USP Brazil AJO DO 2011Dokument11 SeitenCase Report Lateral Open Bite Treatment Stability OMT Essential Cabrera USP Brazil AJO DO 2011AndreaVanoyMartinNoch keine Bewertungen
- Orthodontic Treatment in A Periodontal Patient With Pathologic Migration of Anterior TeethDokument9 SeitenOrthodontic Treatment in A Periodontal Patient With Pathologic Migration of Anterior TeethMárcio LMSNoch keine Bewertungen
- Arvystas 1998Dokument4 SeitenArvystas 1998Саша АптреевNoch keine Bewertungen
- 16 Box Loop and 3 Impacted TeethDokument12 Seiten16 Box Loop and 3 Impacted TeethtomografiaquinNoch keine Bewertungen
- Multiloop Edgewise Archwire in The Treatment of A Patient With An Anterior Open Bite and A Long FaceDokument7 SeitenMultiloop Edgewise Archwire in The Treatment of A Patient With An Anterior Open Bite and A Long FaceKanchit SuwanswadNoch keine Bewertungen
- Space Closure in The Maxillary Posterior Area Through The Maxillary SinusDokument8 SeitenSpace Closure in The Maxillary Posterior Area Through The Maxillary SinusArsenie TataruNoch keine Bewertungen
- Attempted Traction of Impacted and Ankylosed Maxillary Canines.Dokument9 SeitenAttempted Traction of Impacted and Ankylosed Maxillary Canines.Maria Fernanda CáceresNoch keine Bewertungen
- Treatment of Facial Asymmetry and Severe Midline Deviation With Orthodontic Mini-ImplantsDokument13 SeitenTreatment of Facial Asymmetry and Severe Midline Deviation With Orthodontic Mini-ImplantsRicha AhlawatNoch keine Bewertungen
- Third Molar Autotransplant Planning With A Tooth Replica. A Year of Follow-Up Case ReportDokument6 SeitenThird Molar Autotransplant Planning With A Tooth Replica. A Year of Follow-Up Case ReportAlNoch keine Bewertungen
- MOLARDokument8 SeitenMOLARJuan Carlos MeloNoch keine Bewertungen
- 1 s2.0 S0889540622001561 MainDokument13 Seiten1 s2.0 S0889540622001561 MainPaula Heline NisanshaNoch keine Bewertungen
- Articulo Caso ClinicoDokument7 SeitenArticulo Caso ClinicoRICARDO REALPENoch keine Bewertungen
- Pucciarelli2018 PDFDokument4 SeitenPucciarelli2018 PDFAkanksha MahajanNoch keine Bewertungen
- Mi Sympheal DODokument10 SeitenMi Sympheal DOChhavi SinghalNoch keine Bewertungen
- Vertical-Dimension Control During En-MasseDokument13 SeitenVertical-Dimension Control During En-MasseLisbethNoch keine Bewertungen
- Open Bite: Diagnosis, Treatment and StabilityDokument12 SeitenOpen Bite: Diagnosis, Treatment and Stabilityjavi222222Noch keine Bewertungen
- Mermigos 11 01Dokument4 SeitenMermigos 11 01Sankurnia HariwijayadiNoch keine Bewertungen
- Use of Palatal Miniscrew Anchorage and Lingual Multi-Bracket Appliances To Enhance Efficiency of Molar Scissors-Bite CorrectionDokument8 SeitenUse of Palatal Miniscrew Anchorage and Lingual Multi-Bracket Appliances To Enhance Efficiency of Molar Scissors-Bite CorrectionTriyunda PermatasariNoch keine Bewertungen
- Impaksi 1Dokument12 SeitenImpaksi 1Floba Ika SianturiNoch keine Bewertungen
- PIIS0889540612002740Dokument13 SeitenPIIS0889540612002740Aly OsmanNoch keine Bewertungen
- Chin Remodeling in A Patient With Bimaxillary P 2018 American Journal of OrtDokument9 SeitenChin Remodeling in A Patient With Bimaxillary P 2018 American Journal of Ortchristian roblesNoch keine Bewertungen
- Atypical Extraction Treatment For Failing Replante - 2020 - American Journal ofDokument11 SeitenAtypical Extraction Treatment For Failing Replante - 2020 - American Journal ofAlejandro Aranzábal NavarreteNoch keine Bewertungen
- 1 s2.0 S2666430522000036 MainDokument12 Seiten1 s2.0 S2666430522000036 MainDANTE DELEGUERYNoch keine Bewertungen
- Content ServerDokument6 SeitenContent ServerNicoll SQNoch keine Bewertungen
- Nonsurgical Correction of A Class III Malocclusion in An Adult by Miniscrew-Assisted Mandibular Dentition DistalizationDokument11 SeitenNonsurgical Correction of A Class III Malocclusion in An Adult by Miniscrew-Assisted Mandibular Dentition DistalizationNeycer Catpo NuncevayNoch keine Bewertungen
- Maxillary Arch Distalization Using Interradicular Miniscrews and The Lever-Arm ApplianceDokument8 SeitenMaxillary Arch Distalization Using Interradicular Miniscrews and The Lever-Arm ApplianceJuan Carlos CárcamoNoch keine Bewertungen
- Ankylosed Teeth As Abutments For Maxillary Protraction: A Case ReportDokument5 SeitenAnkylosed Teeth As Abutments For Maxillary Protraction: A Case Reportdrgeorgejose7818Noch keine Bewertungen
- A Complex Facial Trauma Case With Multiple MandibuDokument6 SeitenA Complex Facial Trauma Case With Multiple MandibuIndra D KristionoNoch keine Bewertungen
- Berlin Et Al (2023) Multidisciplinary Approach For Autotransplantation and Restoration of A Maxillary PremolarDokument7 SeitenBerlin Et Al (2023) Multidisciplinary Approach For Autotransplantation and Restoration of A Maxillary PremolarISAI FLORES PÉREZNoch keine Bewertungen
- A Case Report On Orthodontic Management of An Adolescent Cleft PatientDokument4 SeitenA Case Report On Orthodontic Management of An Adolescent Cleft PatientMichelle WibiantoNoch keine Bewertungen
- Ambard 2019Dokument4 SeitenAmbard 2019Akanksha MahajanNoch keine Bewertungen
- Root Resorption A 6-Year Follow-Up Case ReportDokument3 SeitenRoot Resorption A 6-Year Follow-Up Case Reportpaola lopezNoch keine Bewertungen
- 7 Articulo Bone-Anchored Maxillary Protraction in A Patient With Complete Cleft Lip and Palate: A Case ReportDokument8 Seiten7 Articulo Bone-Anchored Maxillary Protraction in A Patient With Complete Cleft Lip and Palate: A Case ReportErika NuñezNoch keine Bewertungen
- Open Bite: Diagnosis, Treatment and StabilityDokument11 SeitenOpen Bite: Diagnosis, Treatment and StabilityJavier Farias VeraNoch keine Bewertungen
- Caso Clinico-Ort LingualDokument11 SeitenCaso Clinico-Ort LingualRICARDO REALPENoch keine Bewertungen
- Orthodontic and Non - Orthodontic Root ResorptionDokument8 SeitenOrthodontic and Non - Orthodontic Root ResorptionGaurav PoplaiNoch keine Bewertungen
- Mandibular Implant Supported Overdenture As Occlusal Guide, Case ReportDokument5 SeitenMandibular Implant Supported Overdenture As Occlusal Guide, Case ReportFrancisca Dinamarca LamaNoch keine Bewertungen
- Absolute Anchorage With Universal T-Loop Mechanics For Severe Deepbite and Maxillary Anterior Protrusion and Its 10-Year StabilityDokument12 SeitenAbsolute Anchorage With Universal T-Loop Mechanics For Severe Deepbite and Maxillary Anterior Protrusion and Its 10-Year StabilitysmritiNoch keine Bewertungen
- CANINEDokument10 SeitenCANINEHarish Kumar.THOTANoch keine Bewertungen
- Severe Anterior Open Bite With Mandibular Retrusion Treated With Multiloop Edgewise Archwires and Microimplant Anchorage ComplementedDokument10 SeitenSevere Anterior Open Bite With Mandibular Retrusion Treated With Multiloop Edgewise Archwires and Microimplant Anchorage ComplementedLedir Luciana Henley de AndradeNoch keine Bewertungen
- Sefalo 3Dokument6 SeitenSefalo 3Aisha DewiNoch keine Bewertungen
- Corticotomia y Canteamiento Plano OclusalDokument11 SeitenCorticotomia y Canteamiento Plano OclusalKarla SolísNoch keine Bewertungen
- Correcting Severe Scissor Bite in An Adult: Case ReportDokument12 SeitenCorrecting Severe Scissor Bite in An Adult: Case ReportLikhita ChNoch keine Bewertungen
- Jced 13 E75Dokument6 SeitenJced 13 E75Ezza RezzaNoch keine Bewertungen
- Canino Ectopico A Nivel de Incisivo LateralDokument12 SeitenCanino Ectopico A Nivel de Incisivo Lateralangianny_cdNoch keine Bewertungen
- Teste Examen Anul III ENGDokument84 SeitenTeste Examen Anul III ENGdianaNoch keine Bewertungen
- Oral Lesion Description A Mini ReviewDokument7 SeitenOral Lesion Description A Mini ReviewnediaNoch keine Bewertungen
- Paranasal Sinus (Repaired) EntDokument48 SeitenParanasal Sinus (Repaired) EntDr-Firas Nayf Al-ThawabiaNoch keine Bewertungen
- Prelacrimal Approach To Maxillare SinusesDokument5 SeitenPrelacrimal Approach To Maxillare SinusesBagus Sofian AdhatamaNoch keine Bewertungen
- Local Anesthesia in Pediatric Dentistry Lecture Students 2009 MDokument88 SeitenLocal Anesthesia in Pediatric Dentistry Lecture Students 2009 MIoana DănilăNoch keine Bewertungen
- Head and NeckDokument11 SeitenHead and NeckdrsamnNoch keine Bewertungen
- Maxillary and Mandibular Anatomical Landmarks in Periapical Radiography - (Research by DR - Mahmoud El Masry @AmCoFam)Dokument18 SeitenMaxillary and Mandibular Anatomical Landmarks in Periapical Radiography - (Research by DR - Mahmoud El Masry @AmCoFam)AmericanCornerFamily100% (8)
- C 13 Sisteme Implantare Microlok Si SilhouetteDokument34 SeitenC 13 Sisteme Implantare Microlok Si Silhouettefabian2yoNoch keine Bewertungen
- AS RQs Day 1-2 NBDE 2 WordDokument15 SeitenAS RQs Day 1-2 NBDE 2 Wordravi guptaNoch keine Bewertungen
- Zygomatico-Maxillary OsteotomyDokument8 SeitenZygomatico-Maxillary Osteotomypratiksha malhotraNoch keine Bewertungen
- Neoplasms of Nose & para Nasal SinusesDokument171 SeitenNeoplasms of Nose & para Nasal SinusesJulian HobbsNoch keine Bewertungen
- Implant Surgical AnatomyDokument14 SeitenImplant Surgical AnatomyKo YotoNoch keine Bewertungen
- Kutkut 2011 Sinus WidthDokument5 SeitenKutkut 2011 Sinus WidthLamis MagdyNoch keine Bewertungen
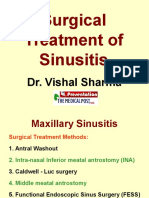
- 11 Surgical Treatment of SinusitisDokument69 Seiten11 Surgical Treatment of SinusitissevattapillaiNoch keine Bewertungen
- Parameters of Care Dentoalveolar Surgery 2012Dokument22 SeitenParameters of Care Dentoalveolar Surgery 2012api-265532519Noch keine Bewertungen
- Lec.3 Development of The FaceDokument25 SeitenLec.3 Development of The FaceDentistryNoch keine Bewertungen
- PhilHealth Circular No. 0035, s.2013 Annex 10 List of Alternative Documents For Record of Operative or Surgical TechniqueDokument14 SeitenPhilHealth Circular No. 0035, s.2013 Annex 10 List of Alternative Documents For Record of Operative or Surgical TechniqueChrysanthus HerreraNoch keine Bewertungen
- Research Article: Epidemiology of Maxillofacial Fractures at A Teaching Hospital in Malaysia: A Retrospective StudyDokument11 SeitenResearch Article: Epidemiology of Maxillofacial Fractures at A Teaching Hospital in Malaysia: A Retrospective Studydr_nadheemNoch keine Bewertungen
- Anatomy of The Nose and Sinus Paranasal, Case RhinosinusitisDokument51 SeitenAnatomy of The Nose and Sinus Paranasal, Case RhinosinusitisDera Seta SaputriNoch keine Bewertungen
- Assessment of The Use of A Dental Mouth MirrorDokument7 SeitenAssessment of The Use of A Dental Mouth MirrorIOSRjournalNoch keine Bewertungen
- Third MolarDokument19 SeitenThird MolarMike LimNoch keine Bewertungen
- Bonemorphogenetic Proteinsin Craniomaxillofacial Surgery: Sarah D. Davies,, Mark W. OchsDokument15 SeitenBonemorphogenetic Proteinsin Craniomaxillofacial Surgery: Sarah D. Davies,, Mark W. Ochshasan nazzalNoch keine Bewertungen
- Handbook of Equine Respiratory EndosDokument127 SeitenHandbook of Equine Respiratory EndosIoana Corbu CostacheNoch keine Bewertungen
- Essential Techniques of Alveolar Bone Augmentation in Implant Dentistry A Surgical Manual 2Nd Edition Len Tolstunov Full ChapterDokument68 SeitenEssential Techniques of Alveolar Bone Augmentation in Implant Dentistry A Surgical Manual 2Nd Edition Len Tolstunov Full Chapterrichard.rathbone385100% (5)
- MRI & CT of Facial Bones PDFDokument53 SeitenMRI & CT of Facial Bones PDFdr_340802071Noch keine Bewertungen
- Odontogenic Infections: Ickman Setoaji W, DRG., MMDokument66 SeitenOdontogenic Infections: Ickman Setoaji W, DRG., MMAmeliza Putri AlindNoch keine Bewertungen
- 3 RfajDokument81 Seiten3 RfajSheikhaNoch keine Bewertungen
- Oral Surgery Board 2008Dokument6 SeitenOral Surgery Board 2008Anonymous FwwfR6Noch keine Bewertungen
- ENT InstrumentsDokument71 SeitenENT InstrumentsPragnya MeduriNoch keine Bewertungen
- Lec8 Sem2 Hnsweek3 20110822Dokument9 SeitenLec8 Sem2 Hnsweek3 20110822Sazter AthiraNoch keine Bewertungen