Beruflich Dokumente
Kultur Dokumente
Diabetes in Dentistry
Hochgeladen von
mihaella2Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Diabetes in Dentistry
Hochgeladen von
mihaella2Copyright:
Verfügbare Formate
Health Deliver y
Dentistry in diabetes
diagnosis and management
` Martin Gillis and Steven Saxon
Much attention is given to heart disease, nerve damage,
kidney disease, and eye damage which can develop in
people with diabetes. However, the mouth (oral) health
complications associated with diabetes are often
overlooked. The oral complications of prime concern are
gum (periodontal) disease, dental caries, dry mouth
(xerostomia), oral soft tissue damage, and pain in the
face and mouth (orofacial pain).
In order to diagnose the potential presence of these
conditions, it is very important for people with diabetes to
have dental examinations at least every 6 months. In this
article, Martin Gillis and Steven Saxon look at the oral
health of people with diabetes with regard to the oral
symptoms of undiagnosed diabetes, the oral health
complications which can develop in diagnosed diabetes,
the oral health-care management of people with diabetes,
and national oral health-care policy as it relates to
diabetes.
>>
September 2003
Volume 48 Issue 3
14
Diabetes manifests itself in the mouth.
Therefore, in addition to looking after
the oral health of people with
diabetes, dentists also play a role in
screening for disease in the general
population.There is a strong
relationship between a person's oral
health and their general health. In
some people, such as in those with
diabetes, the first signs and symptoms
of a medical condition can develop in
the mouth.These people can be
referred to their family physician for
further diagnostic tests.
Oral complications
The oral complications of diabetes,
like other complications associated
with the condition, are related to a
person's ability to control blood sugar
levels (glycaemic control) and their
overall health. People with wellmanaged diabetes have fewer or less
severe complications than those with
poorer glycaemic control.
Periodontal disease (periodontitis)
affects the gums and bone which
support the teeth. It is an
inflammatory disease, triggered by the
bacteria in dental plaque, which results
in the infection of gums followed by
the destruction of bone.The
symptoms of periodontitis are hardly
noticeable at first; but as the disease
Health Deliver y
Dental caries is the process of
demineralization of the tooth
surface caused by bacteria in
which the enamel is broken
down. With proper early
measures, the process can be
halted and even reversed. If
untreated, the demineralization
weakens the tooth and may lead
to fracture.
The temporomandibular joint
allows the lower jaw (mandible)
to move when the mouth opens,
articulating with the bones at
the side of the skull (temporals).
progresses, symptoms such as
bleeding gums, tooth sensitivity,
recession of gums, bad breath
(halitosis), swollen gums, itchy gums,
and loose teeth become apparent.
Scientific studies have shown that
cases of advanced periodontitis are
associated with poorly controlled
diabetes. One researcher called it
the sixth complication of diabetes.1
There is a two-way relationship
between diabetes and periodontitis:
periodontitis can affect diabetes
control and the ability to follow a
proper diet, while poor diabetes
control can negatively affect the
outcome of treatment for
periodontal disease. A healthy
treatment outcome relies on both
good oral health and good diabetes
management.
Dental caries is an oral disease
which affects everybody, but
especially those who have diabetes.
This is mainly due to higher sugar
(glucose) levels in the saliva
surrounding the teeth.
( )
Gum disease has
been called the
sixth complication
of diabetes.
Oral soft tissue damage includes
fungal infections (candidiasis),
ulcers, denture-sore mouth, and
changes in the tongue (such as
chronic fissured tongue). The
development of these conditions is
due to a dry mouth, delayed wound
healing and altered immune and
inflammatory responses.
Xerostomia, or dry mouth, occurs in
people with poor diabetes control. It
is due to decreased salivary flow
rates, alterations in saliva
composition and an increase in
salivary glucose levels. Medications
and nerve damage (neuropathies) may
further complicate the xerostomia.
Oral neuropathies can be either
painful conditions which are
debilitating to the person with
diabetes, or non-painful conditions
which alter taste and function.
Examples of oral neuropathies are:
burning mouth syndrome
burning tongue
temporomandibular joint
dysfunction (TMD)
depapillation and fissuring of the
tongue.
Dentistry and diabetes
diagnosis
There is a relationship between oral
disease and those affecting the whole
body (systemic). Diabetes is a
condition which reflects this
relationship. A person with
undiagnosed diabetes who visits the
dentist for a check-up will show oral
symptoms which could alert the >>
15
September 2003
Volume 48 Issue 3
Health Deliver y
dentist of this undiagnosed
condition. People who previously
had unremarkable check-ups may
have dry mouth, periodontitis, soft
tissue damage and dental caries. At
the same time, the person with
diabetes may talk about weight
changes, blurred vision, lethargy,
changes in mood, and frequent
trips to the toilet.
These symptoms would alert the
dentist to refer this person with
diabetes to their family physician
for diagnostic blood work to test
for diabetes. The diagnosis and
treatment of diabetes is not within
the scope of practice of the
general dentist. It is, however,
within the dentist's scope of
practice to be highly vigilant with
this aspect of care. This applies not
only to diabetes, but to all
systemic conditions that influence
oral health.
In a check-up,
a person with
undiagnosed
diabetes may
show oral
symptoms which
could alert the
dentist of the
condition.
Collaborative efforts
In February 2003, the Nova
Scotia Dental Association
(NSDA), the Canadian Diabetes
Association (CDA)-Nova Scotia
Division, and Dalhousie University
held a diabetes oral consultation
clinic. The clinic was available to
people with diabetes for
consultations with dentists to
assess their oral health status with
respect to the oral complications
of diabetes. The goals of the clinic
were to:
increase public awareness of the
oral complications of diabetes
educate people with diabetes
about the importance of good
oral health and the necessity of
regular visits to the dentist
uncover the barriers which
people with diabetes face in
seeking oral health care.
In 2003, there was also a poster
campaign which was co-sponsored
by NSDA and CDA. More than
2000 posters were distributed to
dental and medical practices, and
diabetes care centres throughout
Nova Scotia. These posters are
designed to communicate to
people with diabetes the
importance of good oral health
care, and the importance of
keeping routine dental
appointments.
Posters are designed to
communicate to people with
diabetes the importance of
good oral health care.
September 2003
Volume 48 Issue 3
16
Health Deliver y
National oral health-care
policy on diabetes
The US and a number of European
countries have developed oral
health-care policies. Canada is in the
process of developing such a
policy. A national oral health-care
policy essentially involves the:
collection of current
epidemiological data
identification of a problem area
based on this data
establishment of a measurable
goal to improve the identified
problem
development of action
programmes to reach this goal.
An example is the US 'Healthy
People 2010' health-care strategy.
The document encompasses all
aspects of health care, including
oral health and diabetes. One goal
of the strategy is to increase the
percentage of people with diabetes
having at least one annual dental
check up from the current 58% to
75% by the year 2010.2
( )
The financial and
social costs of oral
disease are high.
Action programmes need to be
developed in order to reach this
and other oral health-care goals.
A second document, 'A national call
to action to promote oral health',
prepared by the office of the US
Surgeon General, outlines the
objectives necessary to attain these
goals.These objectives apply to oral
health and diabetes through the:
recognition of oral health care as
an accepted component of
diabetes management
accumulation of scientific
information to develop an
evidence base in order to
improve the oral health of people
with diabetes
removal of the barriers to care
faced by people with diabetes
through the development of oral
health-care programmes.3
` Martin Gillis and Steven
Saxon
The burden of oral disease restricts
activities in school, in the workplace,
at home, and impacts negatively
upon a person's quality of life.The
financial and social costs of oral
disease are high. A national oral
health-care policy is designed to
help society deal with oral disease.
It also deals with the relationship
between oral disease and systemic
conditions.The relationship between
oral health and systemic health is
well illustrated with diabetes.
Steven Saxon is a family dentist in
Sydney, Nova Scotia, Canada. He is a
member of the Nova Scotia Dental
Association and Vice President of the
Cape Breton Branch of the Nova Scotia
Diabetes Association. He has had
Type 1 diabetes for 30 years.
Scientific study, oral health-care
programmes, and collaborative
efforts between dental associations,
diabetes organizations, and the
private sector can create a template
which is integral for dealing with
oral health-care issues.Templates of
this kind provide a foundation for
the health-care policy makers and
educators to give health-care
providers the resources necessary
to improve the public's well being.
17
Martin Gillis is a family dentist in
Liverpool, Nova Scotia, Canada. He is
a member of the Nova Scotia Dental
Association and a clinic instructor at
Dalhousie University Dental School. He
has had Type 1 diabetes for 15 years.
References
1. Loe H. Periodontal disease: the
sixth complication of diabetes
mellitus. Diabetes Care 1993; 16:
329-334.
2. US Department of Health and
Human Services. Healthy People 2010.
2nd ed.2 vols. Washington, DC: US
Government Printing Office, November
2000.
3. US Department of Health and
Human Services. National call to
action to promote oral health.
Rockville, MD: US Department of
Health and Human Services, Public
Health Service, National Institutes of
Health, National Institute of Dental
and Craniofacial Research. NIH
Publication No. 03-5303, Spring 2003.
September 2003
Volume 48 Issue 3
Das könnte Ihnen auch gefallen
- Access To Dental Care For Frail Elderly People V2Dokument5 SeitenAccess To Dental Care For Frail Elderly People V2mihaella2Noch keine Bewertungen
- Complicationsduringrootcanalirrigation LiteraturereviewandcasereportsDokument3 SeitenComplicationsduringrootcanalirrigation Literaturereviewandcasereportsmihaella2Noch keine Bewertungen
- FDI Dental Ethics ManualDokument136 SeitenFDI Dental Ethics Manualdocx1975100% (2)
- Perio DiseasesDokument116 SeitenPerio Diseasesdr parveen bathlaNoch keine Bewertungen
- Complications During Root Canal Irrigation - Literature Review and Case ReportsDokument8 SeitenComplications During Root Canal Irrigation - Literature Review and Case ReportsGavi GazNoch keine Bewertungen
- Happy Tooth Sad ToothDokument1 SeiteHappy Tooth Sad Toothmihaella2Noch keine Bewertungen
- Dentistry in Diabetes PDFDokument4 SeitenDentistry in Diabetes PDFmihaella2Noch keine Bewertungen
- Dental Pulp Functions and Responses to InjuryDokument14 SeitenDental Pulp Functions and Responses to Injurymihaella2Noch keine Bewertungen
- Pharmacology PDFDokument167 SeitenPharmacology PDFmihaella2Noch keine Bewertungen
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (587)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (265)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (119)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Respiratory Diseases of NewbornDokument93 SeitenRespiratory Diseases of NewbornTheva Thy100% (1)
- Diabetes Mellitus in Children 1Dokument89 SeitenDiabetes Mellitus in Children 1Vinay PatilNoch keine Bewertungen
- Aeromonas InfectionDokument27 SeitenAeromonas Infection周治剛Noch keine Bewertungen
- Psycho Physiological Disorders 1Dokument8 SeitenPsycho Physiological Disorders 1Cedric Jay Villegas TasicoNoch keine Bewertungen
- Stroke Risk Scorecard 2018Dokument2 SeitenStroke Risk Scorecard 2018wahyu satriaNoch keine Bewertungen
- Heart SoundDokument29 SeitenHeart Sounddianpratiwirahim100% (1)
- ZakriyaDokument6 SeitenZakriyaapi-512107573Noch keine Bewertungen
- RBC MORPH UlkaDokument53 SeitenRBC MORPH UlkaRushi WalgudeNoch keine Bewertungen
- Hematology Topics Objectives References: Our Lady of Fatima University Department of Internal MedicineDokument7 SeitenHematology Topics Objectives References: Our Lady of Fatima University Department of Internal MedicineAlmar NuñezNoch keine Bewertungen
- Patient Anita NCPDokument15 SeitenPatient Anita NCPJoshoua MalanaNoch keine Bewertungen
- DUPUYTREN'S SYNDROME TestDokument15 SeitenDUPUYTREN'S SYNDROME TestreyNoch keine Bewertungen
- Practice Test Pediatric Nursing 100 ItemsDokument17 SeitenPractice Test Pediatric Nursing 100 ItemsPaul Christian P. Santos, RN94% (87)
- 01 NGT Procedure With RationaleDokument4 Seiten01 NGT Procedure With RationaleAryaj SulitNoch keine Bewertungen
- The Floppy Infant:: Evaluation of HypotoniaDokument13 SeitenThe Floppy Infant:: Evaluation of HypotoniaminipredatorNoch keine Bewertungen
- Blood TransfusionDokument2 SeitenBlood TransfusionKomal TomarNoch keine Bewertungen
- Abdominal Wall HerniaDokument100 SeitenAbdominal Wall Herniaintandiahningrum100% (1)
- CefaclorDokument3 SeitenCefaclorAyah PaasaNoch keine Bewertungen
- Differential Diagnosis of Neck SwellingsDokument24 SeitenDifferential Diagnosis of Neck SwellingsDrArish Mahmood100% (3)
- Vocal Cord ParalysisDokument74 SeitenVocal Cord ParalysisWaqas KhanNoch keine Bewertungen
- The Natural Remedy HandbookDokument264 SeitenThe Natural Remedy HandbookRoi Trawon100% (2)
- Suppurative Lung DiseasesDokument39 SeitenSuppurative Lung Diseasesmatchees-gone rogueNoch keine Bewertungen
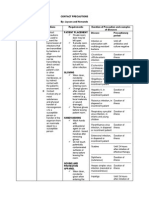
- Contact PrecautionsDokument2 SeitenContact PrecautionsCristina L. JaysonNoch keine Bewertungen
- Nursing Students Peritonitis Care PlanDokument2 SeitenNursing Students Peritonitis Care PlanJide Manuel100% (1)
- Pediatric TB Diagnosis UpdatesDokument39 SeitenPediatric TB Diagnosis UpdatesSiddhartha NandiNoch keine Bewertungen
- Harris Hip ScorHarrise - Orthopaedic ScoresDokument2 SeitenHarris Hip ScorHarrise - Orthopaedic Scoresw00tzxNoch keine Bewertungen
- HANDOUTS Brain SurgeryDokument3 SeitenHANDOUTS Brain SurgerynieltresNoch keine Bewertungen
- Lipo Contrast Cryo BrochureDokument5 SeitenLipo Contrast Cryo BrochureSerenity ZhangNoch keine Bewertungen
- HemorrhoidectomyDokument5 SeitenHemorrhoidectomydrnareshkumar3281100% (1)
- Asking-Filling in Medical ReportDokument5 SeitenAsking-Filling in Medical ReportMiss Hanay VinnyNoch keine Bewertungen
- Nursing Care Plan Assessment Nursing Diagnosis Planning Implementation Rationale Evaluation Subjective: Objective: STG: at The End of 1 DependentDokument1 SeiteNursing Care Plan Assessment Nursing Diagnosis Planning Implementation Rationale Evaluation Subjective: Objective: STG: at The End of 1 DependentThomas FarrishNoch keine Bewertungen